Tools, Not Schools, of Therapy
188 70 11MB
English Pages [1420] Year 2020
CONTENTS
Introduction
Part 1 - JOIN THE A-TEAM!
Chapter 1: Transforming Therapeutic Failure Into Success
Checklist of Cognitive Distortions
Cost-Benefit Analysis*
Chapter 2: How the A-TEAM Model Works
Part 2 - ASSESSMENT
Chapter 3: What's Wrong with the DSM?
Chapter 4: The Easy Diagnostic System for DSM-IV
Chapter 5: How to Take a Really Good Clinical History
Part 3 - TESTING
Chapter 6: The Clinician's Illusion
Chapter 7: How to Track Therapeutic Progress
Brief Mood Survey*
Evaluation of Therapy Session
Chapter 8: Suicide Assessment and Prevention
Suicide Assessment Interview Form
Part 4 - EMPATHY
Chapter 9: The Five Secrets of Effective Communication
EAR chart
Chapter 10: Learning to Use the FiveSecrets in Real Time
Chapter 11: Common Empathy Errors—And How to Avoid Them
Feeling Words Chart*
Chapter 12: "This Therapy Sucks!" How to Develop Trust and Rapport with theAngry, Mistrustful Patient
Good vs. Bad Communication Checklist
Chapter 13: "Doctor, I can tell that you're secretlyattracted to me."
Part 5 - AGENDA SETTING
Chapter 14: Motivating the Unmotivated Patient
The Five Steps in Agenda Setting
Chapter 15: Eight Types of Therapeutic Resistance
Why Our Patients Resist*
Chapter 16: The Defiant Veteran with PTSD
Chapter 17: "Life stinks! What do youintend to do about it?" Additions & Habits
Chapter 18: 50 Ways to Untwist Your Thinking
Chart wt pg#
Part 6 - METHODS
Chapter 19: The Daily Mood Log and Recovery Circle
Quick Chart - 50 Ways to Untwist Your Thinking*
Chapter 20: Basic Techniques
1. Empathy
2. Agenda Setting
3. Identify the Distortions
4. Straightforward Technique
Chapter 21: Cognitive Techniques
Compassion-Based Techniques
5. Double Standard Technique
The Straightforward Double Standard Technique
The Paradoxical Double Standard Technique
The Role-Playing Double Standard Technique
Truth-Based Techniques
6. Examine the Evidence
7. Experimental Technique
8. Survey Technique
9. Reattribution
Logic-Based Techniques
10. Socratic Method
11. Thinking in Shades of Gray
Semantic Techniques
12. Semantic Method
13. Let's Define Terms
14. Be Specific
Zigzag Technique
Quantitative Techniques
15. Self-Monitoring
16. Negative Practice / Worry Breaks
Humor-Based Techniques
17. Paradoxical Magnification
18. Shame-Attacking Exercises
Role-Playing Techniques
19. Externalization of Voices
20. Feared Fantasy
Philosophical / Spiritual Techniques
21. Acceptance Paradox
Visual Imaging Techniques
22. Time Projection
23. Humorous Imaging
24. Cognitive Hypnosis
Chapter 22: Uncovering Techniques
25. Individual Downward Arrow
26. Interpersonal Downward Arrow
27. What-If Technique
28. Hidden Emotion Technique
Chapter 23: Motivational Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
Cost-Benefit Analysis
Attitude Cost-Benefit Analysis
30. Devil's Advocate Technique
31. Stimulus Control
32. Decision-Making Form
33. Daily Activity Schedule
34. Pleasure Predicting Sheet
35. Anti-Procrastination Sheet
Other Anti-Procrastination Techniques
Chapter 24: Exposure Techniques
Classical Exposure Techniques
36. Gradual Exposure and Flooding
My Fear Hierarchy
37. Response Prevention
38. Distraction
Cognitive Exposure Techniques
39. Cognitive Flooding
40. Image Substitution
41. Memory Rescripting
Other Cognitive Exposure Techniques
Interpersonal Exposure Techniques
42. Smile and Hello Practice
43. David Letterman Technique
44. Self-Disclosure
45. Flirting Training
46. Rejection Practice
Other Interpersonal Exposure Techniques
Chapter 25: Interpersonal Techniques
46. Relationship Cost-Benefit Analysis (CBA)
47. Revise Your Communication Style
Good vs. Bad Communication Checklist
48. Five Secrets of Effective Communication
Worksheet- Revise Your Communication Style
12 GOOD Reasons NOT to Listen
12 GOOD Reasons NOT to Express Your Feelings
12 GOOD Reasons NOTto Treat the Other Person with Respect
49. One-Minute Drill
Part 7 - TREATMENT PROGRAM
Chapter 26: Selecting the Most EffectiveTechniques
Chapter 27: Comorbid Depression and Anxiety
Chapter 28: Borderline Personality Disorder
Chapter 29: Public Speaking Anxiety
Common Self-Defeating Beliefs
Chapter 30: Driving Phobia
Chapter 31: Performance Anxiety
Chapter 32: Feeling Better vs. Getting Better—Relapse Prevention Training
Part 8- HEALING YOURSELF
Chapter 33: "I Don't Like You Either!"Countertransference
Common Self-Defeating Beliefs
Part 9 - A-TEAM REVISITED
Chapter 34: The Therapist's Report Card
Appendix
References
2020 NEW Materials Section
NEW Flowcharts & Outlines
TEAM Therapy Session Flow Sheet
Sample Session Flow Chart
Depression Recovery Map
Anxiety Recovery Map
Anger/Relationship Recovery Map
Habit/Addiction Recovery Map
NEW - More Methods
51 Additional Methods
Comparing the Role-Playing Techniques*
Strategies for Defeating Dysfunctional Negative or Positive Thoughts*
Method List with Book Page Numbers
Methods List with Book Page Numbers Alphabetical Order
NEW Advanced Empathy
Advanced Empathy Techniques
Change the Focus
NEW Assessment of Resistance Expanded
Assessement of Resistance or Agenda Setting
5 Steps in Agenda Setting
Why Our Patients Resist
Basic Concepts
01 Empathy
02 Straightfordard Invitation
03 Paradoxical Invitation
04 Sitting with Open Hands
05 Fallback Position
06 Changing the Focus
07 Dangling the Carrot
08 The Miracle Cure
09 Magic Button
10 Acid Test
11 Postitive Reframing
12 Magic Dial
13 CBA
14 Externalization of Resistance
15 Devil's Advocate
16 Gentle Ultimatum
17 Paradoxical Inquiry
Positive Reframing Detailed Overview
Posititve Reframe Ideas
Tips on Agenda Setting
What to Say at Each Step
Agenda Setting FLowchart
Positive Reframing for Relationships
PAS Relationships Flow chart
PAS Relationships Invitation Dialetics
NEW Habit & Addictions Materials
Treating Habits & Addictions Handout
Checklist of Positive Distortions
PAS for Complex Cases
Heal Yourself Habit Log
Relapse Prevention Mood Log for Addiction
Feeling Great Additional "Chapters"
Chapter 32 Ending Habits & Addictions
Chapter 33 How to Make Difficult Decisions
Recommend Papers

- Author / Uploaded
- David Burns
- Commentary
- decrypted from 8391D65350AC03B8042B64C061A19E94 source file
File loading please wait...
Citation preview
Therapist’s ebook, “Tools Not Schools” Expanded 2020 Edition By. Dr. David Burns See bookmarks for easy navigation. NEW Appendix with 150 additional pages • • • • •••• • •• • • • •• • •• •
Tools, Not Schools, of Therapy
(Formerly Strategies for Therapeutic Success— My 50 Most Effective Techniques)
By David D. Burns, M.D. With Signe L. Burns
CONTENTS
Page Introduction
vi
Disclaimer
xi
Illustrated Forms and Charts
xiii Part I
Join the TEAM 1. Transforming Therapeutic Failure Into Success
2
2. How the A-TEAM Model Works
44
Part 2 A = Assessment: How to Do a World-Class Intake Evaluation 3. What's Wrong with the DSM?
65
4. The Easy Diagnostic System for DSM-IV
83
5. How to Take a Really Good Clinical History
107
Part 3 T = Testing: A Boring Topic with Exciting Implications 6. The Clinician's Illusion
157
7. How to Track Clinical Progress and Monitor the Therapeutic Alliance
196
8. Suicide Assessment and Prevention
224
Part 4 E = Empathy: Does It REALLY Make a Difference? 9. The Five Secrets of Effective Communication
233
10. Learning to Use the Five Secrets in Real Time
284
Contents
iv
11. Common Empathy Errors—And How to Avoid Them
291
12. "This therapy sucks! You're a dickhead!"—How to Develop Trust and Rapport with the Angry, Mistrustful Patient
326
13. "Doctor, I can tell that you're secretly attracted to me!"
360
Part 5 A = Agenda Setting: The Key to Therapeutic Success 14. Motivating the Unmotivated Patient
376
15. The Eight Types of Therapeutic Resistance
406
16. The Defiant Veteran with PTSD
451
17. "Life stinks! What do you intend to do about it?"
474
Part 6 M = Methods: My Fifty Most Effective Techniques 18. 50 Ways to Untwist Your Thinking
514
19. The Daily Mood Log and the Recovery Circle
532
20. Basic Techniques
564
21. Cognitive Techniques
578
22. Uncovering Techniques
727
23. Motivational Techniques
769
24. Exposure Techniques
832
25. Interpersonal Techniques
880
Part 7 How to Create a Cutting Edge Treatment Program for Any Patient with Any Axis I or II Disorder 26. Selecting the Most Effective Techniques for Your Patients
940
27. Comorbid Depression and Anxiety—The Student Who Was Afraid of Being Average
979
28. Borderline Personality Disorder—The Woman Who Thought She Deserved to Suffer Forever
1021
29. Public Speaking Anxiety—The Woman Who Was Afraid to Faint
1063
30. Driving Phobia—The Woman with Rubbery Legs
1091
31. Performance Anxiety—The Therapist Who Thought She
1112
Contents
v
Was a Fraud 32. Feeling Better vs. Getting Better—Relapse Prevention Training
1135
Part 8 Healing Yourself 33. "I don't like you either!" Countertransference from a CBT Perspective
1164
Part 9 TEAM Revisited 34. The Therapist's Report Card
1200
Appendix References
1231
NEW BONUS Materials TOC for NEW Materials
1248
Session Flow Charts & Recovery Maps
1250
Additional Tool Lists & Definations
1257
Advanced Empathy Tools Overview
1294
Change the Focus Updated - Agenda Setting - Assessment of Resistance
1303
Postive Reframe Table Habits
Additions
Making Difficult Decisions
1358 1386
Introduction When I was on the voluntary clinical faculty at the University of Pennsylvania in Philadelphia, I supervised a psychiatric resident named Neal Stolar. Neal had two doctoral degrees—in medicine and psychology—so his title was Neal Stolar, M.D., Ph.D. I felt intimidated about supervising someone who already had so much training. The first time we met for supervision, I told Neal that it was too bad that he hadn't worked with me earlier in my career, when I still knew a great deal. I explained that it seemed like the older I got, the less I knew, and that sometimes, I felt like I didn't really know anything at all. I explained that if I was stuck with a really tough patient, and came to him for a consultation, he could probably help me just as much as I could help him with his difficult patients. I said that I'd pretend to be the expert if he'd pretend to be the student. That way, we could hang out and talk about his clinical work during his weekly supervision hour, and we might even have a good time as long as we didn't take our roles too seriously. Neal said he was okay with that, and told me that he was a student of Buddhism. He said that the Buddhists prefer an empty cup to a full cup. That's because you can pour wine into an empty cup. But if you try to pour wine into a full cup, it will simply overflow. Similarly, in this book, I'll pretend to be the expert. I have lots of ideas and methods to share with you, and I'll try to convey them with enthusiasm and conviction. At times, I might say something that seems inconsistent with your
Introduction
vii
own clinical experience or understanding of the literature. If this were a seminar or workshop, you could raise your hand and challenge me. Then we could have a productive dialogue and come to a consensus. In fact, this is the type of interaction that makes teaching so dynamic and rewarding. But since this is a book, we don't have that option. Therefore, I'd urge you to read with some skepticism, but try to keep an open mind at the same time. The field of mental health is still in its infancy, and we're just beginning to develop a true science of human behavior. Unfortunately, we still have a long way to go in that regard. There are hundreds of competing schools of therapy, and every school claims to have the best approach. I'm convinced that many of our most cherished theories about the causes of emotional distress will eventually be proven false, and that our best treatment techniques will be eclipsed by vastly more effective methods in the future. So we really are empty cups. If we can work together with a spirit of humility, mutual respect, and creativity, I'm convinced that we can do some good work—and maybe even brilliant work at times—to relieve the intense suffering of the people who come to us for help. Some ideas are relatively easy to communicate in words. In Feeling Good: The New Mood Therapy, I described ten common cognitive distortions that trigger painful mood swings, such as All-or-Nothing Thinking, Overgeneralization, Jumping to Conclusions, Should Statements, and Blame, to name just a few. Many readers have told me that those ideas rang true immediately, and helped them overcome mood problems that had troubled them for years.
Introduction
viii
Other ideas are considerably more difficult to communicate. Some of the techniques I'll describe appear to be simple, but can be very challenging in reallife situations, especially when you're struggling with an oppositional or mistrustful patient. That's why I've created an interactive book. Reading is a good first step, but to get to the next level, you'll have to do the written exercises. I've used these exercises with my Stanford students and in my workshops for mental health professionals all over the country. Believe me, they really work. They can cause a dramatic change in the way you do therapy. If you do the exercises, you'll get far more out of this book than if you just read the problems and look at the answers. For example, let's imagine that you're treating an angry, oppositional teenager named Jimmy. During a session, Jimmy says, "You're a dickhead! This therapy sucks!" What would you say next? In Chapter 9, I'll ask you to write down exactly what you'd say in response to a variety of tough criticisms you might hear from angry patients. I'll urge you to do this before you read my analyses. Although there's a natural human urge to turn the page and peek at the answer, I hope that you'll resist the urge. Instead, pick up a pen or pencil and write something down on the blank lines I've provided. The practice will be invaluable, even if you later decide that your response was flawed or ineffective. It's the same as with any new skill you're trying to master, like tennis. You can watch a tennis match, read about tennis, and talk to a tennis coach, but your tennis game won't improve. If you want to learn to play skillfully, practice will be necessary. Your body won't do what your brain tells it to do at first. I'm not just
Introduction
ix
aiming for a tune-up in your work with challenging patients, but a major shift in your thinking and clinical techniques. In addition to the written exercises, I've included a number of role-playing exercises you can try with colleagues. You'll need at least one person to practice with. The more you practice, the easier it will be to respond effectively when you're actually confronted with angry, critical patients or colleagues. There's no other way to learn these techniques at the tissue level. This is where the rubber meets the road. One word of caution is in order. When you do these exercises, you may discover that your own intuitive ways of responding to patients are lame, defensive, and off-putting. Repeated failure will be inevitable at first. If your pride gets in the way, and you find negative feedback from colleagues threatening, you're going to have a tough time of it. But if you're willing to fail shamelessly when you do these exercises, they can be tremendously rewarding and fun. In fact, I hope that you'll laugh many times while you're reading and doing the exercises in the book. In my seminars at Stanford, my students and I laugh a great deal, and that's when some of the deepest learning occurs. I've written this book with both novice and advanced practitioners in mind. If you're a student, I hope to provide you with a superb foundation in the basic concepts and techniques of effective psychotherapy so you can quickly become a world-class therapist. If you're an experienced therapist, I hope this book will cause a radical shift in your philosophy of how to help people who are suffering. Of course, the goal is more than just a change in your understanding. I will
Introduction
x
provide you with many powerful techniques that you can use right away in your clinical work. You'll notice that I tend to illustrate each technique with a patient for whom that technique was effective. If I didn't do this, you'd get the impression that the technique wasn't any good, and you wouldn't feel very motivated to learn about it. But at the same time, it may appear that all my patients were magically cured by a single technique. This impression would be very misleading. Most patients are complex and difficult to treat. They've often been suffering for years, and many previous therapists have tried to talk them out of their self-defeating behavior patterns, with little success. If we're going to help these patients, we'll have to use creative new techniques they've never been exposed to before. So while I'll focus on the method that worked for each patient I describe, keep in mind that I usually had to try 10 or 15 techniques that didn't work before I found the one that did. If I described all the methods that weren't effective, you'd soon be asleep! I believe that nearly every depressed and anxious patient can recover, but it usually takes lots of persistence and hard work to bring this result about. In fact, the acceptance of failure is one of the most important keys to therapeutic success. That's because the faster you fail, the faster you'll find the method that works for each patient. Now, let's get started!
Disclaimer Although the vignettes in the book are based on real patients, I've disguised their identities to such an extensive degree that any resemblance to any person, living or dead, is purely coincidental. In fact, many of the cases represent composites of several patients with similar problems. I've done this to protect patient confidentiality, and to try to maintain the highest ethical standards. However, I've attempted to preserve the spirit of the work we did together. Hopefully, these stories will ring true and resonate with your own clinical experience. In most cases, I've also disguised the names and identities of students and colleagues, for similar reasons. I do not want to embarrass anyone or provide any information that might identify a patient. As you read this book, you'll note that I use the word, "patient." I'm a psychiatrist, and I use this word because of my medical training. Psychologists and clinical social workers often object to this word, and feel that we should call the people we work with "clients." They think that the word, "patient," is a putdown. In contrast, when I've presented psychotherapy workshops for psychiatrists and other physicians, I've sometimes gotten into trouble for using the word, "clients." Once, I was even warned that it amounts to an ethics violation! I was informed that prostitutes have "clients," whereas physicians have "patients." Perhaps we should simply refer to the people we treat as human beings
Disclaimer
xii
who are suffering and coming to us for help, and let it go at that. Still, as a convention in this book, I'll use the word, "patient," and I'll trust you to make the necessary translation, depending on your training and inclination.
Forms and Charts
xiii
Illustrated Forms and Charts Cognitive and Behavioral Tools
Page
The Five Steps in Agenda Setting
384
Blank Daily Mood Log
534
Daily Mood Log (cont'd)
535
Checklist of Cognitive Distortions
535
Recovery Circle
1133
Recovery Circle (cont'd)
1134
50 Ways to Untwist Your Thinking (long list)
522
50 Ways to Untwist Your Thinking (one-page list)
1027
Cost-Benefit Analysis
1043
Common Self-Defeating Beliefs
1183
Decision-Making Form
805
Therapist's Report Card
1227
Scoring Key: Therapist's Report Card
1228
Interpersonal Tools Interpersonal Decision-Making Form
889
Relationship Cost-Benefit Analysis
899
Revise Your Communication Style Form
330
Good vs. Bad Communication Checklist
332
The Bad Communication Checklist
332
The Five Secrets of Effective Communication
242
Feeling Words Chart
315
Assessment Instruments Burns Depression Checklist
72
Speedy Screening for Anxiety Disorders, Shyness Test
98
Shyness Survey and Shyness Scale
105
Brief Mood Survey, weekly version
202
Brief Mood Survey, before and after session version
208
Scoring Key: Brief Mood Survey
204
Relationship Satisfaction Scale
202
Disclaimer
xiv
Scoring Key: Relationship Satisfaction Scale
204
Evaluation of Therapy Session
203
Scoring Key: Evaluation of Therapy Session
205
Part One JOIN THE A-TEAM!
1*
Transforming Therapeutic Failure Into Success
If you're like most clinicians, 50% of your patients are reasonably cooperative, motivated, and willing to do what it takes to get better. All they need is some supportive listening and a bit of guidance, and they're on their way. But the other 50% can be far more challenging. Do you have a patient who— Makes you feel anxious, overwhelmed, and frustrated? Constantly "yes-buts" you? "Forgets" to do the self-help assignments between sessions? Is critical and demanding, but no matter how hard you try, it's never good enough? Complains endlessly, but rejects all your helpful suggestions? Pouts and refuses to talk? Cancels at the last minute, or fails to show up at all? * Copyright
2003 by David D. Burns, M.D.
Chapter 1
3
Claims that you don't care—when you feel like you really do? These challenging moments in therapy—when failure seems inevitable and personal feelings of frustration and despair are the most intense—often present us with opportunities for therapeutic breakthroughs. In fact, our worst therapeutic failures are nearly always our greatest therapeutic successes in disguise. It just doesn't feel that way at the time! In my psychotherapy workshops, I often ask therapists to tell me about the most upsetting statements they've heard from their most difficult patients. Here are some examples: "Don't give me any more of your psychobabble shit! Was that supposed to help?" "I'm pregnant and it's all your fault!" "You don't care about me. You don't even understand how I feel." "Aren't you just a student here? I thought I was going to see one of the staff doctors." "My wife thinks I'm not making any progress!" "I'd prefer to talk to someone with an intact brainstem." "I just read an article about Prozac. Do you think I need a real doctor? Or should I stick with you?" "How would you know how I feel? You've never had to live on the streets. You've never been addicted to heroin." "You're bored with me. You're going to kick me out, just like all my other therapists did."
Chapter 1
4
"What's the worst thing that ever happened to you? Did you break a fingernail?" "Doctor, I can sense that there's a special chemistry between us. Do you ever give private sessions after hours?" "I've tried everything and nothing works. What are you going to do that's so different?" Have you ever had a patient who said something like this to you? Try to recall an upsetting interaction with one of your most challenging patients. Was the patient critical of you? Demanding? Angry? Overwhelmed? Hopeless? Write down one thing that this patient said to you. If you're drawing a blank, simply write down the type of thing you've heard from your most difficult patients, or make up the most difficult statement you can imagine hearing during a therapy session. If you prefer, you can just select one of the statements from the list above and write it here: Step 1. S/he said:
Now write down exactly what you said next. If you can't recall exactly
Chapter 1
5
what you said, simply write down the type of thing you'd usually say. Put your response here: Step 2. I said:
Have you completed the exercise? Did you write something down? If not, please do it now before you continue reading. The written exercises will make all the difference in the world, especially if you want to experience tangible improvements in your therapy skills. There's a crucial difference between intellectual understanding and the capacity to transform that understanding into dynamic, effective work with real patients. The written exercises will help you bridge that gap. Without the written exercises, true understanding of these methods will be impossible. Later on, I'll ask you to review what you just wrote down. This will provide us with a baseline assessment of how you ordinarily deal with conflicts in the therapeutic alliance. We'll also diagnose any errors you might have made, so you can see whether your skills are improving as you read this book. Most therapists make the same kinds of errors when they're under attack
Chapter 1
6
from difficult patients. Some get defensive. Others sound patronizing. Many resort to formulaic responses that don't sound genuine. Nearly all therapists carefully avoid acknowledging the patient's anger. And very few know how to find the grain of truth—or the Mount Everest of truth—in the patient's criticisms. As a result, the tensions escalate. These errors aren't limited to novice practitioners. Seasoned clinicians make the same kinds of mistakes. It makes no difference whether you're male or female, or whether you're a clinical social worker, addiction counselor, psychologist, or psychiatrist. I've observed hundreds of therapists in role-playing exercises and real-life interactions with difficult patients, and I've seen defensive, off-putting reactions to hostile patients more than 90% of the time. These reactions seem to be as automatic as the jerk of your leg when the doctor taps your knee. However, there's a light at the end of the tunnel. You can nearly always transform therapeutic failure into success, but you'll have to learn to respond in a radically different way from how you normally respond, or how you were trained to respond. If you respond skillfully, an angry, mistrustful patient will suddenly see you in a far more positive light. This can happen much more quickly than you might imagine. Empathy failures aren't the only kinds of therapeutic challenges we're confronted with. Your patients could pour their hearts out at every session and think that you're the most wonderfully understanding therapist in the world, but they still won't improve if they aren't motivated to solve the problems that brought
Chapter 1
7
them to therapy. This is not a trivial problem. Many patients are deeply ambivalent about change. On the one hand, they're suffering and desperately want relief, but on the other hand, they resist change. They yes-but you. They "forget" to do their psychotherapy homework between sessions. Sometimes, it seems like they're addicted to complaining and won't lift a finger to solve the problems that are bugging them. I'm sure you know what I'm talking about. What are you supposed to do when the patient isn't motivated? Agenda Setting will be a major focus of this book. When you set the agenda, you identify a specific problem the patient wants help with, conceptualize the nature of the problem, and head off the resistance at the pass. You make the patient accountable before you begin to implement any therapeutic interventions or techniques. Agenda Setting is so simple and basic that it seems like the arithmetic of psychotherapy. Most therapists wrongly believe they understand the concept. In fact, you may have learned about the importance of asking about the patient's goals for the treatment goals in your very first psychotherapy class in graduate school. However, Agenda Setting is far more difficult and sophisticated than it seems. It's more like the advanced calculus of psychotherapy. In fact, some of the therapists I've trained have not been able to comprehend or implement Agenda Setting in their clinical work, even after several years of trying. This is unfortunate, because nearly all therapeutic failure results from Agenda Setting errors, or from the complete failure to establish a meaningful therapeutic agenda with your patient.
Chapter 1
8
Even if you have a warm, empathic therapeutic relationship, and a reasonably motivated patient, therapy can still fail. In fact, in this book I'm going to show you how to fail as fast as you can. That's because change is rarely easy, and you'll nearly always have to try a variety of techniques until you discover the one that's helpful to you patient. For example, I once treated a divorced grammar school teacher named Daniel who was suffering from depression and Borderline Personality Disorder. Daniel went to his first therapist when he was 12, and had worked with many therapists since that time. He'd also taken numerous antidepressant medications, but nothing had ever helped. He was constantly miserable. From a cognitive therapy perspective, our feelings result from our thoughts or perceptions. And to corollary is—when you change the way you think, you can change the way you feel. This is very fundamental, and every cognitive therapist is familiar with this notion. However, getting patients to change their thoughts can be incredibly challenging. One of Daniel's negative thoughts was, "I'm a defective human being. I'm defective at the core." Daniel believed this thought 100%. He insisted that this wasn't a distorted thought, but a fact, and he had lots of evidence to back up his conviction. Put yourself in Daniel's shoes for a moment. If you believed that you were a defective human being, how would you feel? What negative emotions would you have? You might have actually felt that way at some time or another during your life. Most of us have experienced dark moments of despair or intense selfdoubt. I know I have! But Daniel had been stuck in that mindset almost his entire
Chapter 1
9
life. Put checks ( ) to the right of all the feelings that Daniel, or anyone, might have, if they believed they were defective:
Emotion
( )
Emotion
( )
Emotion
Depressed
Inferior
Worthless
Hopeless
Anxious
Lonely
Frustrated
Angry
Guilty
Ashamed
Humiliated
Resentful
( )
Chapter 1
10
Answer The best answer would probably be all of the above. Daniel was flooded with every conceivable kind of negative emotion, and said that he'd felt this way for as long as he could remember. Sometimes he felt angry. Sometimes he felt worthless, depressed, and hopeless. Sometimes he felt anxious and insecure. Like most individuals with Borderline Personality Disorder, his feelings were constantly in turmoil, and all his feelings were negative. I believe that the goal of therapy should be tangible change at the gut level, and not just talking about your problems indefinitely. I also believe that change should occur as quickly as possible so patients can complete their therapy and get on with their lives. For Daniel, recovery would mean that his feelings of defectiveness would disappear. He'd wake up each morning feeling happy and worthwhile, looking forward to the day. He'd also understand exactly what technique led to his recovery, so he could use that same technique whenever he fell into a black hole again in the future. As long as Daniel keeps beating up on himself and telling himself that he's "defective at the core," he'll feel miserable. How can we get him to put the lie to this thought, so he can stop thinking about himself in such a negative way? None of his previous therapists have been able to help him. His parents and family had also tried to persuade him to think more positively, but that didn't help, either. We'll need some innovative new strategies if we want to show Daniel how to change his life.
Chapter 1
11
On pages 15 – 24, you'll find a list of 50 CBT techniques, along with brief descriptions of how they work. They're grouped into six categories: Basic Techniques, Cognitive Techniques, Uncovering Techniques, Motivational Techniques, Exposure Techniques, and Interpersonal Techniques. Later on, I'll show you how all of these techniques work, and how to select the ones that are the most likely to be effective for each patient you see. Most therapists don't use nearly this many techniques. They just use a few favorite approaches they learned during their training, such as Socratic questioning or empathic listening. Do we really need all of the techniques on pages 15 – 24? I think we do, for several reasons. First, it simply isn't the case that one or two therapy techniques will work for everyone. People are different, and we all respond to different approaches. Second, different kinds of problems require different kinds of techniques. For example, cognitive restructuring techniques can very effective, even curative, for patients suffering from depression and low self-esteem, but they'll rarely ever be sufficient for patients who are suffering from anxiety disorders. Although cognitive techniques are invaluable for anxiety, a variety of exposure techniques, plus the new Hidden Emotion technique, will nearly always be needed. And if you're treating a relationship problem, such as marital conflict, I almost never use cognitive techniques. In my experience, they just don't work. The resistance to change is far too intense. So I use a radically different approach. The same is true for habits and addictions. Motivational methods are they key to successful treatment.
Chapter 1
12
Finally, you can never predict what technique will work for a particular patient, and two patients with nearly identical problems will rarely ever respond to the same technique. Trial and error will usually be needed. If you have many techniques available, you won't panic when a technique doesn't seem to be working for a particular patient. There will be lots of others you can try. Imagine that you're treating Daniel. How many of the 50 CBT techniques on pages 15 – 24 do you think you'll have to try before Daniel stops believing that he's "defective at the core"? Use a check ( ) to indicate your best guess:
( )
( )
1
7–9
2–3
10 – 20
4–6
> 20
No matter how many techniques you try, you probably won't be able to help Daniel.
Chapter 1
13
Answer There's no single correct answer to this question, but in my experience, 11 – 20 techniques is a good range. For an easy, cooperative patient who's never had any previous therapy, two or three techniques will often be enough. For a difficult patient like Daniel, you may even need to try more than 20 techniques. But on average, it's good to think in terms of 10 – 20 techniques. That way, you won't get frustrated if the first few techniques you try don't work. Let's assume that the 15th technique you try is helpful to Daniel. He suddenly stops believing that he's defective at the core and feels enormous relief. This means that you'll have to fail 14 times before Daniel makes a breakthrough. Suppose that you and Daniel try three or four new techniques each time you meet. For example, during one session, you try Identify the Distortions, Examine the Evidence, the Double Standard Technique, and Let's Define Terms. At the end of the session, Daniel still feels miserable and totally convinced that he's defective at the core. The next time you see him, you try three or four more techniques, but they aren't helpful either. How many sessions will it take before Daniel recovers? Think about it for a moment before you continue reading. The math is pretty simple. If the 15th technique works, and you try three or four new techniques every session, then Daniel's mood should improve within four or five sessions. Now imagine that you have only two or three techniques that you use these techniques with your patients. You use these techniques because you believe in them, and because your clinical supervisor in graduate school believed
Chapter 1
14
in them. How many sessions will it take for Daniel to recover? Think about it for a moment before you continue reading. Once again, the math is simple. Daniel may never get better, since the technique that will help him is not likely to be one of the two or three techniques that you use. As the treatment drags on, you'll get more and more burned out because nothing changes, and your patient just keeps complaining endlessly about his life. You may even begin to buy into his belief that he's hopeless and worthless, and doomed to a life of misery. That's why I use many techniques with every patient. The original title of this book was Strategies for Therapeutic Success, but what we're really talking about are strategies for therapeutic failure. The faster you fail, the faster you'll find the method that works for your patient. So the goal of therapy is to fail as fast as you can. If you learn to fail at high speed, you'll be well on your way to becoming a world-class therapist. Any of the techniques listed on pages 15 – 24 might conceivably help Daniel. You won't know if a technique works until you try it. See if you can select at least fifteen techniques that might help Daniel. Put one technique in each of the boxes around the Recovery Circle on page 25. Don't worry if you don't know how many of the techniques work. All you have to do is to skim through the list on pages 15 – 24. If a technique looks like it might be helpful, put the name of the technique in one of the boxes. I always try to four basic techniques first, so I've listed them in the first four boxes. This should make your job easier. When you're done, turn to page 25 and I'll describe a few of the techniques that I used.
Chapter 1
15 50 Ways to Untwist Your Thinking* Basic Techniques
1.
Empathy (page 564)
When we're upset, we need someone to listen and see the world through our eyes without trying to cheer us up, help us, or give us advice. Although this won't usually lead to a cure, it can be a tremendous relief to know that someone's listening. Similarly, you can learn to empathize when you're trying to help a friend or family member who feels upset. Usually, all they really want is for you to be a good listener.
2.
Agenda Setting (page 566)
Agenda Setting is the most basic and important technique of all. First, try to define the problem you want help with. It must be real and specific as to person, place, and time. Ask yourself, "When was I upset? What time of day was it? Where was I? Who was I interacting with? What was going on?" Now ask yourself if you're willing to roll up your sleeves and work on it now, rather than just talking about it endlessly. Ask yourself, "What would it be worth to me to solve this problem? How hard would I be willing to work on the solution?"
3.
Identify the Distortions (page 568)
Use the Checklist of Cognitive Distortions to identify the distortions in each negative thought.
4.
Straightforward Technique (page 572)
Try to substitute a more positive and realistic thought for each negative thought. Ask yourself, "Is this negative thought really true? Do I really believe it? Is there another way to look at the situation?" Compassion-Based Techniques
5.
Double Standard Technique (page 582)
Instead of putting yourself down, talk to yourself in the same compassionate way you might talk to a dear friend who was upset. Ask yourself, "Would I say such harsh things to a friend with a similar problem? If not, why not? What would I say to him or her?" Truth-Based Techniques
6.
Examine the Evidence (page 591)
Instead of assuming that your negative thought is true, examine the evidence for it. Ask yourself, "What are the facts? What do they show?"
7.
Experimental Technique (page 599)
Do an experiment to test the validity of your negative thought, in much the same way that a scientist would test a theory. Ask yourself, "How could I test this negative thought to find out if it's really true?" For example, if you believe you're on the verge of losing control and cracking up during your panic attacks, you can test this belief by trying to drive yourself crazy though willful effort. You can roll around on the floor, flail your arms and legs in the air, and speak gibberish. It can be a relief to discover that you can't go crazy, no matter how hard you try.
8.
Survey Technique (page 602)
Conduct a survey to find out if your thoughts are realistic. Ask yourself, "How do other people think and feel about this? Could I ask some friends and get some feedback?" For example, if you believe that social anxiety is rare or shameful, you could simply ask several friends if they've ever felt that way.
* Copyright
2000 by David D. Burns, MD. Revised 2004.
Fifty Ways to Untwist Your Thinking 9.
Reattribution (page 609)
16
Instead of blaming yourself entirely for a problem, think about the many factors that contributed to it. Ask yourself, "What caused this problem? What did I contribute and what did others contribute? What can I learn from the situation?" Logic-Based Techniques
10. Socratic Method (page 614)
Ask yourself questions that will lead to the inconsistencies in your negative thoughts. For example, you might ask yourself, "When I say that I'm a 'failure at life,' do I mean that I fail at some things some of the time, or all things all of the time?" If you say, "some things some of the time," you can point out that this is true of all human beings. If you say, "all things all of the time," you can point out that this isn't true of anyone, since no one fails at everything.
11. Thinking in Shades of Gray (page 618)
Instead of thinking about your problems in black-and-white categories, you can evaluate them in shades of gray. When things don't work out as well as you'd hoped, you can think of the experience as a partial success or learning opportunity. Pinpoint your specific errors instead of writing yourself off as a total failure. Semantic Techniques
12. Semantic Method (page 620)
Substitute language that's less colorful and emotionally loaded. Instead of thinking, "I shouldn't have made that mistake," you can tell yourself, "It would be preferable if I hadn't made that mistake." This method is especially helpful for Should Statements and Labeling.
13. Let's Define Terms (page 625)
When you label yourself as "inferior," "a fool," or "a loser," ask yourself what those labels mean. What's the definition of "a fool" or "a loser"? When you try to define these terms, you'll discover there's no such thing as "a fool" or "a loser." Foolish behavior exists, but "fools" and "losers" do not.
14. Be Specific (page 632)
Stick with reality and avoid judgments about reality. For example, instead of thinking of yourself as defective or worthless, you can focus on your specific strengths and weaknesses. Quantitative Techniques
15. Self-Monitoring (page 636)
Keep track of repetitious negative thoughts or anxiety-producing fantasies by counting them. You can keep a 3x5 card in your wallet or pocket and put a tick mark on it each time you have a negative thought. Alternatively, you can wear a wrist-counter like the ones golfers use to keep track of their scores. Record the total number of negative thoughts each day on your calendar. Often, the upsetting thoughts will diminish or disappear within two to three weeks.
16. Negative Practice / Worry Breaks (page 642)
Schedule time to intentionally worry or criticize yourself. For example, if you constantly beat up on yourself because of your shortcomings, you can schedule several five-minute periods each day to berate yourself and feel miserable. At those times, you can be as selfcritical as you want and rip yourself to shreds with gusto. Use the rest of your time for positive, productive living.
Fifty Ways to Untwist Your Thinking
17
Humor-Based Techniques
17. Paradoxical Magnification (page 647)
Instead of trying to refute your negative thoughts, you can buy into them and exaggerate them. Try to make them as extreme as possible. For example, if you feel inferior, you could tell yourself, "Yes, it's true. In fact, I'm probably the most inferior person in California at this time." Paradoxically, this can sometimes provide objectivity and relief. Of course, if you're really upset, this technique may have the unintended effect of making you feel even worse. If so, try another method.
18. Shame-Attacking Exercises (page 651)
If you suffer from shyness, you probably have intense fears of looking foolish in front of other people. Shame-Attacking Exercises are a specific and potent antidote to these kinds of fears. You intentionally do something foolish in public so you can get over this fear. For example, you could stand up and announce each stop on a bus or shout out the time in a crowded department store. When you make a fool of yourself on purpose, you discover that the world doesn't come to an end after all, and that people don't really look down on you. This discovery can be liberating. Role-Playing Techniques
19. Externalization of Voices (page 660)
This technique transforms intellectual understanding into emotional change at the gut level. It's the most powerful of all the CBT techniques, but it can be quite challenging and even a bit upsetting at first. You and another person will take turns playing the role of your negative thoughts and the role of your positive thoughts. The person playing the negative thoughts attacks, and the person playing the positive thoughts defends. Use role-reversals when you get stuck. In the "I-I" version of the Externalization of Voices, both of you will speak in the first person, "I." In the "You-I" version, the person playing the negative thoughts will speak in the second-person, "You," and the person playing the positive thoughts will speak in the first person, "I." The "I-I" method is gentle and safe, but less effective. The "You-I" method is more intimidating and challenging, but has far greater healing power.
20. Feared Fantasy Technique (page 670)
Other Role-Playing Methods
Like the Externalization of Voices, this is a two-person technique. You and the other person act out your worst fears, such as being rejected by an exceptionally hostile critic because you aren't smart enough or good enough. When you face your worst fear, you often gain liberation from it. Your worst fears don't usually turn out to be real monsters, but figments of your imagination that you can defeat with a little logic, compassion, and common sense. Many techniques are much more effective in a role-playing format. They include Cognitive Techniques like the Double Standard Technique (#5) and, Acceptance Paradox (#21), Motivational Techniques like the Devil's Advocate (#30), and Exposure Techniques like the David Letterman Technique (#43) and Flirting Training (#45). The Interpersonal Techniques, such as the Five Secrets of Effective Communication (#49) and OneMinute Drill (#50) also work extremely well in a role-playing format.
Fifty Ways to Untwist Your Thinking
18
Philosophical / Spiritual Techniques
21. Acceptance Paradox (page 683)
Instead of defending against your own self-criticisms, you can find truth in them and accept your shortcomings with tranquility. Tell yourself, "It's true that I have many inadequacies. In fact, there is very little, if anything, about me that couldn't be improved considerably." Visual Imaging Techniques
22. Time Projection (page 700)
Future Projection. If you're depressed, you can take a mental trip into the future and imagine that you've recovered. The current self who feels worthless and defeated can have a conversation with the future self who feels joy and self-esteem. The outpouring of emotion will often have a cathartic effect. Past Projection. You can also take a mental trip into your past and have a conversation with someone who hurt or abused you. This will give you the chance to express thoughts and feelings that have been bottled up and eating away at you for many years.
23. Humorous Imaging (page 702)
When you feel consumed with anxiety or anger, it can sometimes help to visualize something humorous. A depressed woman obsessed about the fact that she'd gotten screwed in her divorce settlement. She could barely make ends meet, and became furious every time she fantasized about her ex-husband cavorting with his new trophy wife on his yacht and living in the lap of luxury. The constant feelings of anger and resentment were making her miserable. She found that picturing him at a board meeting in his underpants made her giggle. This was a useful antidote to the feelings of rage that were plaguing her.
24. Cognitive Hypnosis (page 703)
You'll need a therapist who uses hypnosis if you want to try this technique, and you'll have to be hypnotizable—this includes about a third of us. After inducing a trance, the hypnotist may suggest that you're standing in a special library with two sets of shelves. The shelves on the left contain intensely negative books, like "The Book of Rape" and "The Book of Despair," and the shelves on the right contain positive books, like "The Book of Joy" and "The Book of Self-Esteem." When you take a book from the shelf on the left, you'll discover that it's about you. It contains descriptions of all your negative thoughts, memories, and fears. When you read from this book, you'll feel overwhelmed with feelings of depression, anxiety, hopelessness and shame. Your hypnotist will guide you as you destroy this book. You can burn it, bury it, or shred it. Then you'll find yourself in the library again, where you'll take a book from the shelf on the right. Once again, you'll discover that it's all about you, but this time, it's filled with positive messages of self-esteem, creativity, and optimism. As you read from this book, you'll be flooded with feelings of inner peace.
Other Visual Imaging Techniques
Cognitive Flooding (#39), Image Substitution (#40), and Memory Rescripting (#41) are also Visual Imaging Techniques, but they're categorized as Cognitive Exposure Techniques because they're extremely useful in the treatment of anxiety.
Fifty Ways to Untwist Your Thinking
19
Uncovering Techniques
25. Individual Downward Arrow (page 731)
Draw a downward arrow under a negative thought on your Daily Mood Log and ask yourself, "Why would it be upsetting to me if this thought were true? What would it mean to me?" A new negative thought will come to mind. Write it down under the arrow and repeat this process several times. When you review the chain of negative thoughts, along with the list of Common Self-Defeating Beliefs (SDBs) on page 1183, you can pinpoint the attitudes and beliefs that make you vulnerable to depression and anxiety, such as Perfectionism, the Achievement Addiction, or the Brushfire Fallacy.
26. Interpersonal Downward Arrow (page 740)
Draw a downward arrow under a negative thought on your Daily Mood Log and ask yourself, "If that were true, what would it tell me about the type of person s/he is? The type of person I am? The type of relationship we have?" A new negative thought will come to mind. Write it down under the arrow and repeat this process several times. The thoughts you generate will help you uncover the Self-Defeating Beliefs that lead to problems in your relationships with other people, such as Entitlement, Truth, or Submissiveness.
27. What-If Technique (page 749)
This Uncovering Technique was developed specifically for anxiety. Draw a downward arrow under a negative thought on your Daily Mood Log and ask yourself, "What if that were true? What's the worst that could happen? What do I fear the most?" A new negative thought or fantasy will come to mind. Write it down under the arrow and repeat this process several times. You'll generate additional thoughts that will lead to the fantasy that frightens you the most. Then you can ask yourself, "How likely is it that this would happen? And could I live with it if it did?"
28. Hidden Emotion Technique (page 757)
This technique is based on the idea that when you're anxious, you may be avoiding a personal problem that you don't want to face. Bringing the problem to conscious awareness and expressing your feelings will often eliminate your anxiety. Ask yourself, "Am I focusing on my anxiety to avoid dealing with something upsetting? What's the real problem that's bothering me? Do I secretly resent my spouse or my job? Am I unhappy about being in school? How do I really feel?" Motivational Techniques
29. Straightforward and Paradoxical CostBenefit Analysis (CBA) (page 772)
When you do a Straightforward CBA, you list the advantages and disadvantages of a negative thought ("I'm such a loser") or Self-Defeating Belief ("I should be perfect"). You can also do a CBA for a negative feeling (like anger, guilt, inferiority or anxiety), a habit (such as drinking, using drugs, overeating or procrastinating), or a relationship problem (such as blaming your spouse for your marital problems). Ask yourself, "What are the advantages and disadvantages of this belief, feeling or habit? How will it help me, and how will it hurt me?" After you list all the advantages and disadvantages, balance them against each other on a 100-point scale so you can see whether the costs or the benefits of your mindset are greater. When you do a Paradoxical CBA, you list only the advantages of a negative thought, belief, feeling, habit, or relationship problem. Now ask yourself, "Given all these advantages, why should I change?" This will make you aware of the powerful forces that keep you stuck.
Fifty Ways to Untwist Your Thinking 30. Devil's Advocate Technique (page 798)
20
This is a Role-Playing Technique. Another person plays the role of the Devil who tempts you to drink, overeat, procrastinate, or date the wrong person. Your job is talk back to those thoughts in real time. Use role-reversals when you get stuck. For example, if you're struggling to stick with your diet, imagine being in a mall where fast food is sold. The Devil might say, "Gee, why don't you go and get one of those hot, buttery cinnamon buns? They just came out of the oven. It would taste so good. You deserve it!" You can fight back and say, "I don't need a cinnamon bun, and I'll feel terrible if I give in. I'm determined to stick with my diet, and I'm looking forward to fitting into more attractive clothes." The Devil will try to break you down again, and you can fight back. This method can be surprisingly challenging, especially if the Devil is familiar with your own rationalizations and expresses them in a seductive and persuasive manner.
31. Stimulus Control (page 802)
If you're trying to break a bad habit, such as alcoholism or overeating, you can reduce temptation rather than struggling with it. For example, if you drink too much, you can get rid of all the alcoholic beverages in your house and avoid going to places where alcohol is served. Stimulus Control is not a complete treatment for any addiction, but it can be an important part of a more comprehensive program.
32. Decision-Making Form (page 803)
If you're stuck on the horns of a dilemma, the Decision-Making Form can help you sort out your options and get unstuck. It won't tell you what you should do, but will show you what the real issues are and how you feel about them.
33. Daily Activity Schedule (page 803)
When you're depressed, everything seems overwhelming. Nothing seems worth doing, so you may give up on life. The Daily Activity Schedule can help you overcome donothingism. Record what you do each hour from the time you get up in the morning to the time you go to bed at night. Rate how satisfying each activity was on a scale from 0 (not at all satisfying) to 5 (the most satisfying). A review of the schedule will show you which activities boost your mood the most.
34. Pleasure Predicting Sheet (page 811)
Schedule a series of activities with the potential for pleasure, learning, or personal growth. Indicate who you plan to do each activity with. Include activities you can do by yourself (such as jogging) as well as activities with other people. Predict how satisfying each activity will be on a scale from 0% (the least) to 100% (the most). After you complete each activity, record how satisfying it actually turned out to be on the same scale. Now compare your actual satisfaction ratings with your predictions. Many depressed people find that lots of activities turn out to be more rewarding than they predicted. This discovery can boost your motivation to become more actively involved in life again. You can also compare the satisfaction you get from being alone to the satisfaction you feel from being with other people. This can help you test Self-Defeating Beliefs such as, "If I'm alone, I'm bound to feel miserable."
35. Anti-Procrastination Sheet (page 823)
Rather than telling yourself you have to do everything all at once, break an overwhelming task down into tiny steps that you can tackle one step at a time. List each step in the lefthand column of the Anti-Procrastination Sheet. In the next two columns, predict how difficult and how satisfying each step will be on a scale from 0% – 100%. After completing each small step, record how difficult and how satisfying it turned out to be in the last two columns. Now compare your predictions with the outcome. Many people discover that each step is far easier and more rewarding than they expected.
Fifty Ways to Untwist Your Thinking Other AntiProcrastination Techniques
21
Socratic Method. If you're struggling with procrastination, you can ask yourself a series of questions that will lead to the absurdity of your claim that you just "can't" seem to get started on the task you've been avoiding. First, break the task down into tiny steps. What's the first thing you'd have to do? The second thing? Then ask yourself, "What do I mean when I claim that I can't do the first step? Or the second step?" Problem-Solution Method. Schedule a time when you can do five minutes of the task you've been avoiding. Let's say you decide to start organizing the mess on your desk at 3:00 PM. Draw a line down the center of a piece of paper and list all the problems that will get in your way and all the excuses you'll give yourself for not getting started at 3:00 in the left-hand column. You might put, "A friend may call and need to talk," or "It may seem too anxiety-provoking," or "I may decide that I need to rest for a while first." You can put solutions to each problem in the right-hand column. Classical Exposure Techniques
36. Gradual Exposure and Flooding (page 833)
When you use Gradual Exposure, you expose yourself to the thing you fear in small steps. For example, if you have an elevator phobia, you could get on an elevator, go up one floor, and get off. Once you're comfortable with that, you could ride the elevator for two floors. You can gradually increase the length of time you spend in the elevator. You can use Gradual Exposure for any phobia, such as the fear of heights, needles, or dogs, as well as other forms of anxiety, such as shyness or Obsessive-Compulsive Disorder. You can also create a Fear Hierarchy, listing the least threatening situation as +1, and the most threatening as +10. You can record the type and amount of exposure you perform each day, as well as how anxious you felt, between 0% and 100%. When you use Flooding, you expose yourself to the thing you fear all at once. For example, if you have an elevator phobia, you can force yourself to get on an elevator and ride up and down, no matter how anxious you feel, until your fear disappears. Flooding is more frightening than Gradual Exposure, but it works more rapidly. Both approaches have been used successfully in the treatment of nearly all forms of anxiety, so you can use the approach that appeals to you the most.
37. Response Prevention (page 844)
Response Prevention is an important key to the treatment of all forms of anxiety. It's often combined with exposure. For example, let's say you have a powerful urge to check the mailbox over and over after you drop a letter in. Using Response Prevention, you would drop the letter in the mailbox and walk away without checking it as you usually do. Your anxiety will temporarily get worse, and you'll feel compelled to check it. But if you refuse to give in to this urge, your anxiety will eventually disappear.
38. Distraction (page 846)
If you feel anxious, you can distract yourself from the upsetting thoughts by concentrating intensely on something else. For the best results, you can combine Distraction with Gradual Exposure or Flooding. For example, if you feel panicky during an airplane flight, you can work on a crossword puzzle or engage the passenger next to you in conversation. Some therapists recommend moving the eyes back and forth from left to right during exposure. This is called EMDR (Eye Movement Desensitization and Reprocessing). Others recommend tapping rhythmically on some part of your body, like your clavicle or eyebrow, during exposure. This is called TFT (Thought Field Therapy). Although these techniques are controversial, there's no harm in trying them, and they might make the exposure somewhat less upsetting.
Fifty Ways to Untwist Your Thinking
22
Cognitive Exposure Techniques
39. Cognitive Flooding (page 849)
Cognitive Flooding is useful when you can't expose yourself to the thing you fear in reality. For example, if you have a fear of flying, you can't expose yourself to an actual airplane crash in order to overcome your fears! However, you can confront this fear in your mind's eye using Cognitive Flooding. Visualize your worst fear, such as feeling trapped in a plane that's crashing toward the earth in a ball of flames while all the passengers scream in terror. Try to endure the anxiety for as long as you can. If you become panicky, don't fight it! Instead, try to make the panic even worse. Eventually, the anxiety will burn itself out because your body simply cannot create anxiety indefinitely.
40. Image Substitution (page 854)
Substitute a more positive or peaceful image for a frightening one. For example, during an airplane flight, you can fantasize landing safely or relaxing on a beach instead of imagining the plane crashing in flames.
41. Memory Rescripting (page 859)
If you've been a victim of sexual or physical abuse, you may experience flashbacks with vivid memories of the traumatic episode. These mental pictures can be likened to a horrifying internal movie that you replay over and over, in exactly the same way every time. You can edit the frightening scenes in this movie in much the same way that you can change your negative thoughts. For example, if your best buddy was killed by a hand grenade when you were fighting together in Vietnam, you may be haunted by horrifying memories of his body being blown apart. You can bring him back to life in your mind's eye and tell him all the things you never got to say before he died. Then you can give him a proper burial and say goodbye. Changing the images can create a sense of mastery and help you overcome the feelings of helplessness that resulted from being a victim. In addition, the intentional exposure will desensitize you, and the traumatic memories will lose their power to intimidate you.
Other Cognitive Exposure Techniques
Negative Practice / Worry Breaks (#16), the Feared Fantasy (#20) and the Acceptance Paradox (#21) are all forms of Cognitive Exposure. Interpersonal Exposure Techniques
42. Smile and Hello Practice (page 865)
If you're shy, you can force yourself to smile and say hello to 10 or 20 strangers each day. Use a 3x5 card to record how many people respond positively, neutrally, and negatively. You'll often discover that people are much friendlier than you expected. This discovery can help you overcome your fears of rejection or looking foolish.
43. David Letterman Technique (page 866)
You can learn how to make casual conversation with anyone by using the Five Secrets of Effective Communication (#49), especially the Disarming Technique, Inquiry, and Stroking. These are the same skills used by successful talk-show hosts like David Letterman and Jay Leno. They appear charming, personable and relaxed because they always keep the spotlight on the other person. Instead of trying to impress people by talking about yourself, you can focus on them in a friendly way. Find truth in what they say. Express curiosity and admiration. Ask questions and encourage them to open up. You'll find that most people are somewhat bored and lonely, and love to be the center of attention.
Fifty Ways to Untwist Your Thinking
23
44. Self-Disclosure (page 870)
Instead of shamefully hiding your feelings of shyness or nervousness in a social situation, you can disclose them openly. This technique requires a good sense of self-esteem to be effective. If it's done skillfully, it will allow you to form real relationships with people instead of trying to put on a show and pretend to be something that you're not. This technique is based on the rather unintuitive idea that shyness without shame is actually an asset, because it makes you seem more human and personable.
45. Flirting Training (page 872)
You learn to flirt in a playful, light-hearted way, rather than interacting with others in such a formal, heavy manner. Paradoxically, when you lighten up and learn to stop taking people so seriously, they're more likely to find you attractive and may even start chasing you.
46. Rejection Practice (page 875)
If you're shy and afraid of rejection, you can try to accumulate as many rejections as you can instead of trying so hard to find someone to love you. Although this takes tremendous courage, you'll discover that the world doesn't actually come to an end when you're rejected. Paradoxically, when you stop fearing rejection, you stop getting rejected.
Other Interpersonal Exposure Techniques
Shame-Attacking Exercises (#18) are categorized as Humor-Based Techniques, but they're also Interpersonal Exposure Techniques. The Rejection Feared Fantasy is a variation of the Feared Fantasy Technique (#20). Let's say that you're intensely shy and afraid of rejection. You can enter an Alice-in-Wonderland nightmare world where your worst fears come true. A friend or therapist can play the role of the most rejecting, hostile person you can imagine. She or he will be far worse than any real human being would ever be, and will try to rip you to shreds. If you respond with the Acceptance Paradox, you'll discover that you can easily handle anything the Hostile Critic throws at you without getting perturbed. Use role-reversals if you get stuck. Interpersonal Techniques
47. Relationship CostBenefit Analysis (CBA) (page 894)
List the advantages and disadvantages of blaming the other person for the problems in your relationship. You'll discover that there are lots of advantages: You can feel morally superior. You won't have to examine your own role in the problem. You'll feel like truth is on your side. You can get back at the other person without feeling guilty. You can feel powerful. You can tell your friends what a loser the other person is, and they'll probably agree with you. There may also be some disadvantages. You won't be able to resolve the problem or get close to the person you're mad at. The conflict will go on and on, and you'll feel consumed by feelings of frustration and anger. Your friends may get tired of your constant complaining. And there won't be any room for personal or spiritual growth. Once you've listed all the advantages and disadvantages on the CBA form, balance them against each other on a 100-point scale. Ask yourself whether the costs or the benefits of this mind-set are greater. If you decide to keep blaming the other person, the prognosis for the relationship will be extremely poor. The willingness to stop blaming them and examine your own role in the problem is the key to developing a more satisfying relationship.
Fifty Ways to Untwist Your Thinking 48. Revise Your Communication Style (page 904)
24
The Revise Your Communication Style form can help you improve your relationships with family members, friends and colleagues. There are five steps: Step 1. Write down one thing the other person said to you. Step 2. Write down exactly what you said next. Step 3. Analyze what you wrote down in Step 2. Was it an example of good or bad communication? Step 4. Think about the consequences of what you wrote down in Step 2. How will the other person think and feel? What will she or he say next? Will your response make the situation better or worse? Step 5. Generate a more effective response using the Five Secrets of Effective Communication.
49. Five Secrets of Effective Communication (page 913)
The Five Secrets of Effective Communication can help you resolve virtually any relationship problem quickly. These techniques require considerable practice and must come from the heart or they'll backfire. 1. The Disarming Technique. Find some truth in what the other person is saying, even if it seems totally unreasonable or unfair. 2. Empathy. Try to see the world through the other person's eyes. Paraphrase their words (Thought Empathy) and acknowledge how they're probably feeling, based on what she or he said (Feeling Empathy). 3. Inquiry. Ask gentle, probing questions to learn more about what the other person is thinking and feeling. 4. "I Feel" Statements. Express your own ideas and feelings in a direct, tactful manner. Use "I Feel" Statements, such as "I'm feeling upset," rather than "You" statements, such as "You're making me furious!" 5. Stroking. Convey an attitude of respect, even if you feel angry with the other person. Find something genuinely positive to say, even in the heat of battle.
50. One-Minute Drill (page 894)
You and your partner take turns playing the roles of Talker and Listener. The Talker spends 30 seconds expressing his or her feelings about a relationship problem. The Listener paraphrases what the Talker said as accurately as possible. The Talker rates the Listener's accuracy from 0% – 100%. Once the Listener receives a rating of 95% or better, you can do a role-reversal. This technique ensures nearly perfect communication. It quickly breaks the pattern of accusation, self-defense, and hostility, and shifts the dialogue to a level of greater vulnerability and intimacy.
Other Interpersonal Techniques
Interpersonal Decision-Making. When you're at odds with someone, you have three choices: you can settle for the status quo, work to make the relationship better, or leave the person you're not getting along with. Most of time, people know what they want, but sometimes it's confusing. You may ask yourself: "Should I get engaged or break up and look for someone more exciting?" Or, "Should I get divorced or try to make my marriage better?" The Decision-Making Form (#32) can help you sort out your options when you're having a tough time making up your mind. A wide variety of patterns can emerge, and each one will lead to a unique solution.
Daniel's Recovery Circle
Empathy
16
15
Agenda Setting
1
14
2
13
Identify the Distortions 3
12
4
11
Straightforward Technique
5
10 6 9
Chapter 1
8
7
Page 25
Chapter 1
26
Answer You can see the techniques I selected on page 27. There's nothing magical about this choice of methods, and your selections were undoubtedly different. The important thing is to select at least 15 techniques. This will get you off to a good start. Once you get started, more techniques will come to mind. Empathy and Agenda Setting will be vitally important with every patient. In fact, they're so important that I've devoted several chapters to each of them, so I'll only mention them briefly here. When Daniel tells you that he's defective at the core, you'll need to listen so that he feels you can see the world through his eyes. This means acknowledging how he feels—hopeless, defeated, and worthless, and ashamed—without trying to "help" him. It also means finding the truth in what he's saying. In fact, Daniel has had far more of his share of suffering and disappointments. His marriage had only lasted a couple months, his career as a grammar school teacher isn't considered very prestigious in our culture, and he's struggled with feelings of depression, resentment and worthlessness nearly every minute of his life. It's little wonder that he feels defective. Paradoxically, Daniel won't be able to let go of this perception until he's convinced that his therapist really understands and accepts the validity of what he's trying to say. Empathy alone won't be enough. Agenda Setting is at least as important. What's Daniel's goal? Of course, he wants you to listen and understand, but does he want more than that? Does he want you to help him change his life? What would it be worth to Daniel if you agreed to help him challenge this thought and overcome his depression? What would he bring to the table? Would he be willing to do psychotherapy homework between sessions? Chapter 1
Daniel's Recovery Circle
Feared Fantasy
Acceptance Paradox Externalization of Voices
Empathy
16
15
1
14 Anti-Procrastination Sheet
Agenda Setting
2
13
Identify the Distortions 3
12
Semantic Method
4
11 Cost-Benefit Analysis
Straightforward Technique
5
10
Examine the Evidence
6 Individual Downward Arrow
9
8
7
Double Standard Technique
Thinking in Shades of Gray
Let's Define Terms
Reattribution Chapter 1
Page 27
Chapter 1
28
And what's his idea of what getting better might mean? If you had a magic wand and could "cure" him in today's session, what would it look like? Would he no longer be "defective?" Would he suddenly be earning a quarter million dollars a year and have solved all the problems in his life? Or would he have learned to accept himself, with all his flaws? And would he really be willing to experience joy and self-esteem, if you could show him how, given the fact that he does have lots of real shortcomings? Or does he feel that his suffering is more "morally correct," or "inevitable," given the facts of his life. To put it in a nutshell, what is Daniel really looking for, and what would he be willing to pay if you could deliver the goods? This is a vitally important question that has to be answered to the satisfaction of the patient and the therapist. If you jump in and try to "fix" Daniel without addressing his resistance to change and negotiating a meaningful agenda, the therapy is almost certain to fail. In fact, nearly all therapeutic failure results from Agenda Setting errors, or the complete failure of the therapist to establish a meaningful agenda with the patient. Identify the Distortions was the next technique I tried. Let's do it together now. On page 29 you'll find the familiar list of ten cognitive distortions. How many distortions can you identify in Daniel's negative thought? Check off all the distortions you can find in this thought in the checkbox on page 30. When you're done, you can review my analysis on page 31.
Chapter 1
29
Checklist of Cognitive Distortions * 1.
All-or-Nothing Thinking. You look at things in absolute, black-and-white categories.
2.
Overgeneralization. You view a single negative event as a never-ending pattern of defeat.
3.
Mental filter. You dwell on the negatives and ignore the positives. This is like the drop of ink that discolors the entire beaker of water.
4.
Discounting Positives. You insist your positive qualities don't count.
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts. Mind-Reading. You assume that people are reacting negatively to you. Fortune-Telling. You predict that things will turn out badly.
6.
Magnification or Minimization. You blow things way out of proportion or shrink them.
7.
Emotional Reasoning. You reason from your feelings: “I feel like an idiot, so I must be one.” Or "I feel hopeless. This means I'll never get better."
8.
Should Statements. You criticize yourself or other people with “shoulds,” “shouldn'ts,” “musts,” “oughts,” and “have tos.” Self-Directed Shoulds lead to feelings of guilt and inferiority. Other-Directed Shoulds lead to feelings of bitterness, anger and frustration. Hidden Shoulds are rules and should statements that are implied by your negative thoughts.
9.
Labeling. Instead of saying, “I made a mistake,” you tell yourself, “I'm a jerk” or “I'm a loser.”
10. Self-Blame and Other-Blame. You find fault instead of solving the problem. Self-Blame. You blame yourself for something you weren't entirely responsible for. Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright
1977 by David D. Burns, M.D. Revised 2006.
Chapter 1
30
Instructions. Check off all the distortions you can find in Daniel's negative thought, "I'm a defective human being. I'm defective at the core." Distortion
( )
Distortion
1. All-or-Nothing Thinking
6. Magnification or Minimization
2. Overgeneralization
7. Emotional Reasoning
3. Mental Filter
8. Should Statements
4. Discounting the Positive
9. Labeling
5. Jumping to Conclusions
10. Blame
( )
Chapter 1
31
Answer I think you can make a pretty good case that Daniel's thoughts contain all 10 distortions. Distortion
( )
Explanation
1.
All-or-Nothing Thinking
Daniel thinks that there are two kinds of people: the "defective" people and the "normal" people.
2.
Overgeneralization
Daniel generalizes from his shortcomings and problems to his entire self.
3.
Mental Filter
Daniel constantly thinks about his faults, and filters out anything positive about himself or his life.
4.
Discounting the Positive
Daniel tells himself that his good qualities don't count and tells himself that there's nothing special or interesting about him.
5.
Jumping to Conclusions
Daniel assumes that no one else could care about him (MindReading) and tells himself that things could never change (Fortune-Telling). He sees himself as a radio that's broken beyond repair.
6.
Magnification or Minimization
He blows his flaws out of proportion (Magnification) and tell himself that his good qualities don't count (Minimization). He also magnifies the importance of other people's strengths and minimizes the importance of their flaws. This allows him to conclude that he's inferior to other people.
7.
Emotional Reasoning
Daniel feels defective so he concludes that he must really be defective.
8.
Should Statements
Daniel tells himself that he shouldn't be the way he is.
9.
Labeling
Daniel labels himself as defective.
10. Blame
Daniel constantly beats up on himself and blames himself for not being better than he is. He also secretly blames God, and his fate, for his misery.
Chapter 1
32
Daniel could easily identify the distortions in his thoughts, but didn't find this especially helpful. He insisted that his thoughts weren't really distorted, and that he was simply facing the truth about himself. He told me that his problem was not with his thinking, but rather with reality. This reaction isn't unusual. Most depressed patients cannot easily comprehend that their thoughts are the source of their misery, and that the thoughts that upset them are actually distortions and subtle mental cons. Still, Identifying the Distortions in a negative thought can be useful for a variety of reasons. First, it sometimes helps you open the door, just a crack. If a thought contains 8 or 10 distortions, could it really be 100% valid? Second, it sometimes gives you ideas about other techniques that may be helpful, because some of the techniques listed on pages 15 – 24 will be especially helpful for certain distortions. For example, the Semantic Method can be especially helpful for Should Statements, and the Survey Technique is often helpful when the negative thought involves Mind-Reading. We'll come back to the theme of how to select techniques for different kinds of problems and distortions later in the book. Notice that I've used four techniques already, and Daniel is still 100% convinced that he's defective at the core. That's what I meant when I said that you should expect to try 10 – 20 techniques before you find the one that works, especially when you're working with a difficult patient like Daniel. I tried Examine the Evidence next. I asked Daniel, "What's the evidence that you're defective at the core? How did you come to this conclusion?" Daniel explained that he'd been constantly depressed, angry, or anxious
Chapter 1
33
every minute of every day since childhood, and couldn't recall even one minute of happiness. He said this showed that he was "emotionally defective." I said it I could see that he'd suffered a great deal, but I wondered if this was the only evidence he had that he was "defective at the core." Daniel said he had lots of additional evidence. He pointed out that he couldn't get along with women, and reminded me that he'd gotten divorced two months after his first and only marriage. He said that he had no male friends, either. He said he even had to pay psychiatrists to talk to him, and he was pretty sure that they couldn't stand him, either. He said this showed he was "interpersonally defective." I acknowledged that he'd had lots of problems with his relationships, but that many people had relationship problems. What was the evidence that he was "defective at the core"? How had he come to this conclusion? Daniel explained that he had no hobbies or interests, and spent most of his free time staring at walls or watching television. This proved that he was a "boring person" as well. I said, "So you've had emotional problems and difficulties in your relationships with people, and you don't have any hobbies or interests. A loss of interest in life is actually one of the cardinal symptoms of depression. Is that all the evidence you have that you're defective at the core?" He said, "Oh, no, there's a lot more evidence. I'm also a defective teacher. In fact, I'm the worst teacher in the entire school district." At this point, I realized that I'd finally caught Daniel in the distortion of Jumping to Conclusions, so I swooped in for the kill. I asked, "Where's the
Chapter 1
34
evidence that you're the worst teacher in the entire district?" He handed me a letter he'd received earlier that day from the Superintendent of Schools. The letter stated that he'd gotten the lowest ratings of any teacher in the entire school district, and that if his teaching didn't shape up within six weeks, he'd lose his job. Clearly, Examine the Evidence wasn't working very well! Of course, I wanted Daniel to see that his thinking, and not his "defectiveness," was the cause of his depression. But he wasn't buying it. Notice that we've already failed five times. What are we going to do next? You just go on to the next technique on your Recovery Circle. Keep failing as fast as you can. That's the key to success. I decided to try the Double Standard Technique next. This technique capitalizes on the fact that many of us operate on a double standard. When we think about our own problems, we rip ourselves to shreds. But if we were talking to a dear friend who had the same problem, we're usually far more objective and compassionate. I told Daniel to imagine that he was talking to a dear friend who was just like himself. This man has also had problems with his moods, relationships, and career. He's been feeling worthless and depressed for years and doesn't have any close friends, interests or hobbies. His marriage ended in divorce after just two months, and he's totally convinced that he's "defective at the core." I asked Daniel what he'd say to his friend. Daniel said he'd probably tell him that he should face the facts and jump off the Golden Gate Bridge. I had the distinct impression that we weren't hitting
Chapter 1
35
the ball out of the park with the Double Standard Technique, either! I tried many other techniques but couldn't dislodge Daniel's overwhelming conviction that he was "defective at the core." And week after week, his depression score remained unchanged. He was still severely depressed, and hadn't improved one iota. One night while I was jogging, it dawned on me that a motivational technique, like the Cost-Benefit Analysis (CBA), might be worth a try. I also reminded myself that the Semantic Method is nearly always the best technique for Should Statements. You'll learn more about these techniques later in the book, but when patients do a CBA, they weigh the advantages against the disadvantages of a particular thought, feeling, or behavior. For example, maybe there were some advantages in Daniel's thought, "I'm defective at the core." The Semantic Method simply involves changing the emotionally charged, pejorative language that patients use when they think about themselves and their problems. I called Daniel at home around 9:00 PM and apologized for calling so late. I explained that I'd been concerned about the fact that he was still struggling with feelings of worthlessness, and wondered if he might have time to do a special homework assignment before our session the next afternoon. He seemed pleased that I'd been thinking about him and asked what I wanted him to do. I told him to draw a line down the middle of a piece of paper and to write this at the top: "I'm a defective human being." I asked him to label the left-hand column "Advantages of believing this," and the right-hand column "Disadvantages of believing this," as you can see on page 38. Then he could list
Chapter 1
36
all the ways this belief helped him in the left-hand column, and all the ways it hurt him in the right-hand columns. When he was done, he could weigh the advantages against the disadvantages on a 100-point scale, and put his ratings in two circles at the bottom of the page. For example, if the advantages of the belief seemed a lot greater than the disadvantages, he might put a 70 in the circle on the left and a 30 in the circle on the right. If the advantages and disadvantages were about the same, he could put a 50 in each circle. And if the disadvantages seemed somewhat greater, he might put a 45 in the circle on the left and a 55 in the circle on the right. I told Daniel that when he finished the CBA, I wanted him to take a second piece of paper and repeat the exercise, only this time, he'd write this statement at the top: "I'm a human being with defects." Once again, he could list all the advantages and disadvantages of this belief, and weigh them against each other on a 100-point scale, just as he'd done before. Rewording the negative thought in this way is an example of the Semantic Method. You simply change the language you use when you think about your problems, using words that are less insulting and demoralizing. Daniel said that he appreciated my call and would do his best to finish the assignment before our session. As an exercise, please complete the CBA on page 38. Put yourself in Daniel's shoes and see how many advantages you can come up with for the thought, "I'm a defective human being." What are the benefits of this belief? How might this mindset reward you?
Chapter 1
37
Then ask yourself if there's a price you'll have to pay for this belief. What are the disadvantages of telling yourself that you're a defective human being? When you're done with your lists, weigh the advantages against the disadvantages on a 100-point scale and record your ratings in the circles at the bottom.
Chapter 1
38
Cost-Benefit Analysis* Describe the thought or feeling you want to evaluate: "I'm a defective human being."
Advantages of Believing This
* Copyright
Disadvantages of Believing This
1984 by David D. Burns, M.D.
Chapter 1
39
Daniel's first CBA appears on page 40. As you can see, he rated the advantages of believing he was a defective human being as 40, and the disadvantages as 60. Even though there were more advantages, the disadvantages felt greater to him. This meant that the belief was not really working for him. His second CBA appears on page 41. The results were even more lopsided. The advantages of believing, "I'm a human being with defects," greatly outweighed the disadvantages. When I saw Daniel the next afternoon, he told me that he'd done exactly what I'd asked him to do, but nothing in his life had changed. He said he was still the worst teacher in the district, still had no friends, and still had no interests or hobbies. "But," he said, "you might be interested in this." Daniel handed me the depression test he'd been taking once a week between sessions. His score had dropped into the normal range for the first time. In fact, he was completely free of any symptoms at all. He explained: "Even though the facts of my life haven't changed, my perceptions changed when I did the two Cost-Benefit Analyses. I realized that if I say, 'I'm a human being with defects,' I can still be honest with myself. The fact is, I do have lots of flaws and shortcomings. But this new mindset made me feel like I was a member of the human race again. I realized that I can work on my teaching, improve my relationships with people, and develop some hobbies and interests. My problems don't seem so overwhelming or impossible any more. In fact, I'm excited to be alive!"
Chapter 1
40
Cost-Benefit Analysis* Describe the thought or feeling you want to evaluate: "I'm a defective human being."
Advantages of Believing This
Disadvantages of Believing This
1. I'll have an excuse for failure.
1. Things will never change.
2. I can feel sorry for myself.
2. I'll feel hopeless and defeated.
3. I can feel like a victim.
3. I'll feel worthless.
4. I can feel angry and resentful.
4. I'll feel bitter and frustrated.
5. I won't have to get my hopes up and risk failure.
5. I'll drive people away and irritate anyone who tries to get close to me.
6. I won't have to try.
6. I'll feel lonely.
7. I can feel special because I'll be unique and different.
7. I'll never experience any happiness or self-esteem.
8. I'll have a sense of identity.
8. I'll feel helpless.
9. I can frustrate my therapist and defeat the people who try to help me.
9. I'll feel envious and jealous when others succeed.
10. I can blame my problems on factors that are beyond my control. 11. I won't have to do things that are anxiety-provoking, like dating. 12. I'll feel like I'm being incredibly honest and facing the truth about myself. 40 *
* Copyright
60
1984 by David D. Burns, M.D.
Chapter 1
41
Cost-Benefit Analysis* Describe the thought or feeling you want to evaluate: "I'm a human being with defects."
Advantages of Believing This
Disadvantages of Believing This
1. I can be honest with myself about my shortcomings.
1. I won't be able to feel sorry for myself all the time!
2. I'm allowed to make mistakes.
2. I won't be able to hide out and avoid people.
3. I'll feel like a member of the human race again.
3. I won't feel so special and unique any more.
4. I won't feel so depressed and resentful all the time.
4. I won't have a built-in excuse for failure.
5. I'll feel like I can work on my problems, little by little. 6. I'll feel hopeful and optimistic.
90
* Copyright
10
1984 by David D. Burns, M.D.
Chapter 1
42
What had happened? Well, I'd tried lots of techniques that hadn't worked, including the four Basic Techniques, a couple Truth Based Techniques, a Compassion-Based Technique, a Log-Based Technique, and others. But they didn't work because there was a side of Daniel that was hanging onto his symptoms. He was in pain, but he was reluctant to change. He had one foot in the water, and one foot on the shore, and he wasn't about to let me, or anyone else, push him all the way into the water. When we did the CBA, we suddenly brought all those hidden motivational forces to conscious awareness, and he could see that there were lots of good reasons not to change. The moment he saw this, those forces lost their hold over him, and he no longer felt the need to resist change so intensely. Was Daniel miraculously and permanently cured as a result of the CBA and the Semantic Method? Obviously, he has more work to do, since there are still some real problems in his life. For example, he'll need to work on his relationships and his teaching, and he may want to develop some new hobbies and interests. But this work will be far easier and more rewarding now that he's feeling good about himself and his life. In addition, we'll have to do some Relapse Prevention Training because those negative forces will gather and plan for another attack before too long. In essence, we'd finally made an important breakthrough that completely transformed the nature of our work. You might feel skeptical that such a simple technique could possibly help someone who'd struggled with low self-esteem for decades. I've found that the technique that works for any patient almost always comes as a surprise. The
Chapter 1
43
opposite is also true. Sophisticated techniques that seem like they should work usually aren't effective. Usually, the answer is quite simple. But the process of getting to that simple solution is always challenging. Daniel and I had struggled together unsuccessfully for two months before we found the techniques that worked for him. This is not unusual. In fact, frequent failure is the key to therapeutic success. If you think a technique is supposed to work, you'll feel anxious and frustrated when the patient says, "This isn't helping me. I still feel like a loser." Then you'll push harder, because you'll think the patient is being difficult, and you'll soon be enmeshed in a power struggle. But if you have many techniques available, you won't be afraid of failure. You can just keep failing as fast as you can. And when you find the technique that does work, you'll always see a dramatic change in the way the patient is thinking and feeling.
2*
How the A-TEAM Model Works
We know that effective therapy cannot simply consist of a bag of tricks or techniques you impose on patients, based on their diagnoses. People are far too complex and challenging for that. If you want to do cutting edge work, you'll need a shrewd, comprehensive assessment of the patient's problems, a warm and trusting therapeutic alliance, and a highly motivated patient who's willing to work hard to change his or her life. When you've got these ingredients, you can use a variety of creative techniques to help practically any patient, including those who seem the most difficult and refractory at first. However, bringing these ingredients together may be easier said than done. Most patients are ambivalent and may not be motivated to change their lives. Some have hidden agendas and are more interested in disability payments than recovery. Others seem addicted to the role of victim, and although they're suffering, they fear and resist change. Others may not trust you or feel cared * Copyright
2004 by David D. Burns, M.D.
Chapter 2
45
about, in spite of your best efforts to convey compassion and support. And even if you have a solid therapeutic alliance, you're still faced with the daunting task of showing your patients how to overcome the relentless feelings of depression and inferiority, the terrifying panic attacks, their troubled relationships, or their addictions. In this book, I'm going to show you how to use a flexible, systematic, and highly individualized approach to therapy that I call the TEAM model. This acronym will help you remember the keys to effective psychotherapy with any patient: T = Testing E = Empathy A = Agenda Setting M = Methods You can use the TEAM acronym to organize your learning while you read this book. It will also help you diagnose and reverse therapeutic failure. Let's examine how this model works. T = Testing Testing refers to the initial evaluation the session-by-session testing of symptoms so you can track progress throughout the treatment in a variety o dimensions. Therapeutic failure often results from errors that therapists make at the very first session. A good initial evaluation includes the clinical history as well as the Axis I and Axis II diagnostic screening. These are not the most exciting aspects of the treatment, but they can have a huge impact on the outcome, and
Chapter 2
46
there are lots of errors that therapists typically make when they're doing their initial evaluation. For example, you may take an abbreviated history and simply scribble some diagnostic term, like "Major Depression" or "Adjustment Disorder," on the chart. Sometimes you can get away with this, and sometimes you can't. Although patients often come to treatment with a single complaint, like depression, most of them will fulfill the criteria for many Axis I and II disorders. If you simply focus on the presenting complaint, you may overlook important factors that affect the way the patient thinks, feels and behaves. For example, a pleasant young man seeking treatment for depression may be secretly abusing drugs or alcohol and struggling with intense shyness as well as some symptoms of PTSD because of sexual abuse he endured as a child. He may also have narcissistic tendencies along with Borderline Personality Disorder, and could be flirting with self-destructive or violent urges. If you only focus on his depression, you could miss the boat, with disastrous consequences. At my clinic in Philadelphia, we administered a structured diagnostic interview for Axis I and II disorders to all new patients, along with psychological testing and a detailed clinical history. This provided us with excellent information, but required several hours. Therapists and patients alike hated this experience. We felt so guilty about it that we only charged patients for half of the time we spent. For years, I struggled to develop a faster and more user-friendly intake procedure that wouldn't sacrifice accuracy or thoroughness. Recently, I've come
Chapter 2
47
up with a new approach that I'm excited about. I call it the Easy Diagnostic System for DSM-IV. I'll show you how it works in Chapter 4. In most cases, you can complete a comprehensive screening for a wide variety of Axis I and II disorders fairly quickly, and carefully document all the symptoms of all the disorders in your chart. Although a top-notch initial assessment obviously won't guarantee successful treatment, you'll know that you've gotten the therapy off to a great start and laid the groundwork for superb clinical work. Of course, diagnostic issues aren't the only factors we have to evaluate at the intake evaluation. Sometimes, you have to read between the lines and ask yourself questions like this: Is this patient coming to see me because of external coercion, like an arrest for a DUI or pressure from his spouse or parents to come to therapy? Are there hidden agendas the patient hasn't revealed? For example, is the patient coming to therapy in an effort to get disability payments or a bigger settlement in a lawsuit? Is the patient withholding vitally important information, such as drug abuse or suicidal urges, due to feelings of shame, or the fear of being judged or punished? Is the patient really committed to solving the problem she or he described? For example, the patient may complain bitterly about his wife, colleague, or neighbor. Does he want to develop a better relationship with the person he's angry with, or does he simply want you to listen and agree that the other person is a loser?
Chapter 2
48
Is the patient ready, willing, and able to do what's going to be necessary to solve the problem she or he has described? The failure to confront these issues at intake may set you up for therapeutic failure and frustration later on. In contrast, learning how to make patients accountable before you initiate the actual therapeutic process can empower you and your patients, and will greatly increase your chances for therapeutic success. I once treated a 73 year-old man named Ezekiel who'd suffered from more than 40 years of depression ever since fleeing from Nazi Germany during WWII. Ezekiel had arrived in Manhattan as a young man, penniless and without a family, and had to shine shoes for several years just to survive. But he was extremely determined. He worked hard and eventually became a successful businessman. When he came to me for treatment, he was wealthy and owned his own box manufacturing plant. In spite of his success, Ezekiel had never been able to shake the conviction that he was a worthless human being. Over the years, he'd received numerous courses of psychotherapy and taken all kinds of antidepressant medications, but nothing had helped. I tried many cognitive therapy techniques, but couldn't put a dent in his belief that he was worthless. At the time, jogging was receiving a great deal of media attention and was being touted as having strong mood elevating effects because of the "runner's high." I told Ezekiel that he probably needed to boost his endorphins, and encouraged him to participate in a rigorous jogging program. He
Chapter 2
49
was desperate for relief, so I pushed him hard. Before long, he was running 5 miles a day. On one occasion, he'd even pushed himself to go nearly twice that far. Not bad for a 73 year-old man! One day, I asked Ezekiel how he felt at the beginning of his run that morning. He replied, "I felt like a totally worthless human being." Then I asked him how he felt at the end. He replied, "I felt like a totally exhausted, worthless human being." Several sessions later, Ezekiel revealed the true cause of his feelings of worthlessness. He confessed that he'd had two phobias since he was a little boy: claustrophobia and a fear of the dark. He was intensely embarrassed and so ashamed of these "weaknesses" that he'd never told anyone about them before, even a therapist. I could suddenly see why my previous interventions had been ineffective, and proposed a homework assignment specifically designed to target Ezekiel's phobias. I suggested that he could set his alarm clock for 3:00 AM, when it would be completely dark outside, and go down into his basement with all the lights off. Then I wanted him to lie down on the carpet and roll himself up in it, with his hands at his sides, so he'd feel trapped. I instructed him to stay there, no matter how terrified he felt, until his anxiety disappeared. That way, he could defeat his claustrophobia and fear of the dark at the same time. I also suggested that he could set up a tape recorder near his head. That way, he could dictate his negative thoughts and fantasies every minute, and we could find out what he was really afraid of.
Chapter 2
50
Ezekiel was terrified and refused to try the assignment. He insisted that he'd lose control and have a nervous breakdown if he attempted anything that extreme. He even went to another psychiatrist for a second opinion. Fortunately, the other psychiatrist told him that exposure was the treatment of choice for phobias, and encouraged him to continue working with me. Ezekiel finally agreed to bite the bullet. He set his alarm for 3:00 AM, went down into his basement with all the lights off, rolled himself up in the carpet, and began dictating. At first, he was terrified, and estimated his anxiety at 100% on a scale from 0% (no anxiety at all) to 100% (the worst anxiety possible). He was convicted that a "fat ghost" would suddenly come out of the darkness, sit on his chest, and suffocate him. He had an overwhelming urge to run from the basement and turn on the lights, but he resisted, just as he'd promised. After 30 minutes of intense fear, it began to dawn on him that the fat ghost hadn't yet appeared. Suddenly, he shouted, "Come on, I'm waiting for you! I'm not running! Let's get it over with!" Still, nothing happened. The whole notion suddenly began to seem ludicrous. Within two minutes, his anxiety disappeared completely, along with his depression and his conviction that he was a worthless human being. This is why an accurate assessment and conceptualization of the patient's problems is so vitally important. Obviously, there's no way to hit the bull's eye if you don't even know where the target is located! For a long time, we'd been spinning our wheels. Once I finally understood what was really going on with Ezekiel, the rest was relatively easy.
Chapter 2
51
T = Testing Following my psychiatry residency at the University of Pennsylvania School of Medicine, I spent two years as a research fellow at the Affective Diseases Research Unit of the Philadelphia Veterans Administration Hospital. My colleagues and I administered assessment instruments like the Hamilton Rating Scale for Depression (HRSD) every day to the depressed veterans on our unit, so we could test hypotheses about the biology of depression and publish our studies in scientific journals. When I went into clinical practice, I decided to measure my patients' depression levels at every session because I felt that the information could be useful in guiding the treatment. However, I didn't want to use the HRSD because it was so time-consuming to administer and so poorly constructed. If you've ever taken a close look at this test, I think you'll see what I mean. It's a mishmash of confusing items that don't effectively address the most important symptoms of depression. As an alternative, I decided to use the Beck Depression Inventory (BDI), because patients could fill it out on their own between therapy sessions. They handed me the completed BDI at the start of each session, and I recorded their score on a flow sheet in the chart. This only took about 15 seconds, and allowed me to track changes in their symptoms at every therapy session. The changes in the scores from week to week showed me what was working, and what was not. There were a number of problems with the BDI, but it was convenient, easy to use and free. However, in the mid-1980s, I received a letter stating that
Chapter 2
52
the BDI had been sold, and that I would now have to pay a royalty of $1 each time I administered it. Shortly after that, I received another letter stating that the same thing had happened to the Hopkins Symptom Checklist-90 (SCL-90). If you failed to pay the royalties for these tests, you were threatened with stiff fines and other legal actions. By that time, I'd developed a large outpatient practice, and most of my patients were taking three or four tests between sessions so I could track several kinds of symptoms. It dawned on me that if I kept using these tests, I'd have to pay nearly $10,000 a year in royalties. Furthermore, my patients sometimes complained about the tests because many of the test items were poorly worded, and the response options were often confusing as well. In addition, the psychometric properties of these instruments were less than optimal. It seemed like a good time to explore other options. I decided to see if I could develop some new instruments that would be more useful for therapists and patients alike. I hoped to develop instruments with the following properties: Brief. I wanted 5-item self-assessment tests that my patients could complete, score and interpret in less than 30 seconds. User-friendly. I wanted pleasant tests with clear instructions, logical response options, and no psychological jargon or big words. Educational. I wanted tests that would have immediate therapeutic value. Valid and reliable. I wanted valid and exceptionally accurate instruments that had psychometric properties that were superior to other popular
Chapter 2
53
instruments like the BDI, the Zung scales, and HRSD. In particular, I was hoping to develop instruments with reliabilities of at least 90%, or even 95%, if possible, as compared with reliabilities in the high 70s or low 80s of most comparable measures. Practical. I wanted tests that would assess any psychological dimension of potential interest to a clinician, such as depression, suicidal urges, every type of anxiety including shyness, relationship satisfaction, physical pain, and therapeutic empathy, as well as positive feelings such as happiness, intimacy, and self-esteem, to name just a few. To date, my colleagues and I have developed a wide variety of brief, userfriendly tests that fulfill these criteria. In all cases, we've been able to develop instruments with reliabilities greater than 90%, and some as high as 99%. We've validated them against many of the most widely used scales, such as the Beck Depression and Anxiety Inventories, the Zung Depression and Anxiety Tests, the Hamilton Rating Scale for Depression, the SCL-90, the Locke-Wallace Marital Adjustment Test, the Quality of Marriage Index, and others. These instruments can revolutionize your practice in just the same way that the development of the x-ray machine and MRI transformed the practice of medicine. You can track progress and monitor the quality of the therapeutic relationship accurately at every therapy session. But because patients fill out these tests on their own outside of sessions, the testing takes virtually no therapy time at all. For the first time, you'll see exactly how your patients feel and how much progress they're making—or not making. You'll also discover how they
Chapter 2
54
really feel about you. This will allow you to detect the tiniest failures in the therapeutic alliance immediately, before the negative feelings mushroom out of control. E = Empathy The cognitive and behavioral therapies have sometimes been criticized as lacking sufficient focus on emotion as well as the therapeutic alliance. I don't know whether this criticism is fair, because I've seen therapists of all persuasions who don't deal with their patients' feelings very skillfully, especially if the feelings are negative and directed at them! But there's no doubt that therapy without emotion and trust is going to be superficial and ineffective, no matter what school of therapy you belong to. Without a vibrant, caring therapeutic alliance, you won't get anywhere, even if you have the best techniques in the world. During the late 1990s, I helped to develop a daily CBT group therapy program for the inpatient unit at the Stanford Hospital as part of my volunteer work for the Department of Psychiatry. The psychiatric residents had tipped me off to the fact that there was a heavy biological emphasis on the unit, so most of the patients didn't get nearly as much psychotherapy as they needed. In all fairness, I think that nearly every inpatient program in the United States suffers from this difficulty. Drugs and ECT seem to be the main therapeutic solutions for whatever ails the patient. I was pleased that our inpatient staff were excited about developing a more robust psychotherapy program. Once the CBT group program got rolling, I used to come in once a week to direct the groups. That way, I could see if the groups were effective and do some
Chapter 2
55
teaching as well. At the start of a group, I noticed that one of the patients had a big bandage around his head. His name was Bart. He explained that he'd been feeling discouraged about his marriage, and had discovered that his wife was having an affair. He was devastated, and when he confronted her, she threatened to divorce him. Bart felt like he couldn't survive without her love, so he walked several miles into the woods behind his house with an automatic pistol. He stuck the barrel of the gun in his mouth, tilted it up toward his brain, and pulled the trigger. Apparently, two bullets came out. The first one ripped his left eye out, and the second one shattered on his skull. He passed out instantly, but woke up 24 hours later in a pool of blood, still alive. Then he passed out again. After another 24 hours had passed, he briefly woke up again, and passed out. He woke up a third time 24 hours later. This time, he didn't pass out, so he began crawling out of the woods. After several hours of agony, he made his way to the edge of the highway and collapsed on the shoulder of the road. A passing motorist spotted him lying there, covered in blood, with a portion of his face missing, and rushed him to the Stanford emergency room. Bart was admitted for emergency neurosurgery, where they removed the bullet fragments from his brain and reconstructed his shattered skull and face. After he recovered from the surgery, they transferred him to the psychiatric unit to treat his depression and assess his suicidal urges. In fact, he'd just arrived on our locked unit an hour earlier. When I asked Bart how he was feeling, he said he
Chapter 2
56
felt utterly hopeless, alone, and ashamed, and began sobbing. The woman next to him was in a wheelchair. Her name was Sybil, and she seemed to be about 45 years old. She was receiving intravenous fluids through a catheter in her arm and she had a feeding tube in her nose. She looked emaciated, much like the photos of concentration camp victims in Nazi Germany. Sybil explained that she was receiving treatment for anorexia nervosa. I asked how she was doing. She seemed pretty chipper and said that she was doing great, and that everyone on the staff had been wonderful to her. In fact, she'd gained 10 pounds in just three weeks. I asked how much she weighed now. She proudly exclaimed, "I'm up to 58 pounds now!" Whether or not you can see it in their faces, the people who come to us are often in great pain. They may be experiencing intense feelings of desperation, hopelessness, and fear. Before we can gain their trust, we'll have to enter into the darkness with them. Empathy alone will not be enough to cure most patients, but you won't get anywhere without it. What is empathy? The psychoanalysts define empathy as the therapist's subjective feelings and experiences while interacting with the patient. I think this definition is problematic, because our feelings result from our own thoughts and perceptions, and usually won't be correlated with our patients' thoughts and feelings. Certainly, your feelings are an important source of data. If you feel anxious, guilty, frustrated or annoyed during a session, it can tip you off that there are problems in the therapeutic alliance that need to be explored. However, your feelings won't provide you with accurate information about how your patients
Chapter 2
57
are really thinking and feeling. I prefer to define empathy as the capacity to accurately understand what the patient is thinking and feeling at any given moment. If you attempt to summarize what the patient is thinking and feeling, and the patient says, "That's exactly right, Doctor. You've got it," then I'd say you're empathizing with that patient. In addition, the understanding must be conveyed with kindness and compassion. You could accurately summarize the patient's thoughts and feelings in a condescending, defensive or sarcastic manner. This would not be true empathy, but a put-down. More than 100 published studies have documented a positive correlation between patients' ratings of therapist empathy and recovery from emotional distress (Orlinsky, Grawe, & Parks, 1995). Patients who rate their therapists as warm and trustworthy seem to improve the most. Using structural equation modeling techniques, I've shown that this correlation results from a modest direct causal effect of empathy on recovery from depression (Burns & NolenHoeksema, 1992). In other words, if you convey warmth and understanding, it will often boost a patient's mood. However, research studies have also shown that therapists' ratings of their own empathy are not correlated with recovery. In fact, our perceptions of our own warmth and understanding are barely correlated with our patients' perceptions of us, if at all. This means that you may think you're coming across in a warm and compassionate way when your patient doesn't see you that way. In contrast, you may think you're doing a lousy job when your patient has high regard for you.
Chapter 2
58
These studies indicate that our patients are highly qualified to judge how empathic we are, but we're not! How can we find out how they really feel about us? If you ask a patient how the therapy is going, they'll usually say you're doing fine, even when you're not. It can be very difficult to be assertive, especially when there's a power imbalance in a relationship, and psychotherapy certainly fits into that category. However, there is a way to find out. I've developed a Therapeutic Empathy scale that's exquisitely sensitive to even the tiniest failures in the therapeutic alliance. Patients can indicate how warm, respectful, trusting and understanding you were in the most recent session. I require all patients to fill this scale out after every therapy session so we can review their feelings at the start of the next session. Therapists are sometimes skeptical when they first learn about the Therapeutic Empathy scale. They think patients won't be honest when they fill it out, and will only tell them what they want to hear. But in fact, the truth is just the opposite. Patients are brutally honest when they fill it out and will tell you what you don't want to hear! In fact, most novice and experienced therapists get failing grades from nearly every patient at every session when they first begin to use this instrument. This can be a disturbing discovery, particularly if you're used to thinking of yourself as reasonably sensitive and empathic. But if you're willing to look at the way your patients rate you, and try some new ways of processing the feedback you'll receive when you use this instrument, your ratings will soar, and your
Chapter 2
59
satisfaction and clinical effectiveness will improve substantially. We'll talk about how you can develop warm and trusting relationships with even the most angry, mistrustful patients in Part IV of this book. A = Agenda Setting You can have the best assessment tools in the world and a wonderful therapeutic alliance, but your patients won't change one iota if they're not motivated to change. This means working hard both during and between sessions. But many patients seem to have one foot in the water and one foot on the shore. They may be perfectly willing to talk about all the problems in their lives, but may not want to roll up their sleeves and work on solving them. Others aren't clear about what they want help with. They express their complaints in abstract terms, using buzzwords such as "self-esteem," "codependency," and "ADHD." Many patients seem to have given up on life. They say: "I really am worthless." "I'm hopeless. Nothing could help." "I'm such a fat pig. I just can't control my eating." Others are openly defiant. They say: "Why should I have to change? It's not my fault!" "Life stinks! What makes you think that you can help me?" Patients may resist our efforts to help them for many different reasons. Depressed patients may resist because they feel hopeless and convinced that nothing could help them, or they may feel worthless and think that they don't
Chapter 2
60
deserve to feel joy or self-esteem. Anxious individuals may resist confronting their fears because it seems so terrifying. Angry patients may feel convinced that they're innocent victims, and that others are to blame for the problems in their relationships. And patients with bad habits or addictions won't want to give up their goodies. From our perspective, the addiction may look like a problem, but it may be working just fine for the patient. Most therapists try to overcome resistance with logic or persuasion, but that never works. Others jump in and try to help the patient, but the patient says, "Oh, I already tried that. It didn't work." Sometimes it seems like the harder you try, the more passive or oppositional the patient becomes. You feel like you're doing all the work while the patient sits back and complains that you're not helping. Before long, you feel like a trained dog jumping through a hoop. No matter how high you jump, the patient says, "That's not good enough," and holds the hoop even higher. Every session starts to feel like an energy drain, and you become frustrated and burned out. You dread seeing the patient and may begin to label him or her as "difficult," "resistant," "unmotivated," or "borderline." In Part V, I'll show you a radically different way of overcoming resistance with powerful Agenda Setting techniques. Agenda Setting strikes many therapists as basic or obvious, but it's actually the most challenging and rewarding component of psychotherapy. Most therapeutic failure is the result of Agenda Setting errors on the part of the therapist, or the failure to set the agenda in the first place. Once you understand Agenda Setting and begin to implement it
Chapter 2
61
systematically in your clinical work, you'll have a powerful new tool available for understanding and reversing therapeutic failure. M = Methods Throughout history, gurus have promoted the idea that you can treat emotional problems with a single method or technique that will cure what ails you. Experts have advocated cocaine, prayer, mindfulness meditation, relaxation training, aerobic exercise, psychoanalytic free association, dream analysis, antidepressants, EMDR, TFT, bioenergetics, hugging your inner child, getting in touch with your "true feelings," St. John's wort, Prozac, and a mind boggling array of fixes for every conceivable emotional problem. Mental health professionals, and the general public alike, routinely fall for each new brand of snake oil. I call this therapeutic reductionism. It's the attempt to reduce a complex process—psychotherapy—to one simple gimmick or formula. When you think about it, this doesn't make much sense. There are more than 50 different kinds of pneumonia, and they all respond to different kinds of antibiotics, as well as a variety of other treatments. In addition, there are many other kinds of lung disorders, such as pneumothorax, asthma, emphysema, pulmonary edema and lung cancer, to name just a few. You can't treat all these disorders with a single antibiotic. The brain is vastly more complex than the lung. The number of genes required for the creation of the human brain is far larger than the number required to create a lung. When you think about it that way, the idea that we'd
Chapter 2
62
need hundreds of different treatments for pulmonary problems, but only one treatment for emotional problems, seems absurd. For example, the cognitive therapy techniques that can be so effective for depression probably won't help an angry patient with a marital conflict. And the techniques that can quickly cure Panic Disorder won't be at all helpful for alcoholism or an eating disorder. In addition, every person we treat is unique. Different patients will respond to different techniques, even if they have the same diagnosis. For example, the Cost-Benefit Analysis (CBA) and Semantic Method ended years of suffering for Daniel, the man we discussed in Chapter 1. However, these techniques may not do a thing for the next depressed patient you see, who may respond to the Acceptance Paradox, the Externalization of Voices, or some other technique. In Part VI, I'll describe 50 CBT techniques and teach you the tricks of the trade so you'll be able to use all of them effectively in your clinical work. In Part VII, I'll show you how to select the most effective techniques for each patient, so you can develop an individualized, world-class treatment program for any patient with any Axis I or II disorder. We'll also talk about the differences between feeling better and getting better, so you can create an effective relapse prevention program for every patient before you discharge them at the end of treatment. Finally, in Part VIII, we'll talk about countertransference from a CBT perspective. What do you do when you feel anxious, inadequate or frustrated because you have a challenging or critical patient who isn't responding to your efforts? We'll talk about how you can use CBT to heal yourself, so you can
Chapter 2 develop a personal understanding of how these techniques work.
63
Part Two A = ASSESSMENT How to Do a World-Class Intake Evaluation A-TEAM
Assessment
Testing
Methods
Empathy Agenda Agenda Setting Setting
3*
What's Wrong with the DSM?
Although the Diagnostic and Statistical Manual of the American Psychiatric Association represents an important step forward, it contains a number of significant shortcomings. On the positive side, DSM-IV provides a common language for describing emotional and behavioral problems. If you've developed a promising new treatment for shyness, you can publish an outcome study of individuals who fulfill the DSM-IV criteria for Social Anxiety Disorder. Now, independent investigators can attempt to replicate your findings in another group of individuals who also fulfill the criteria for Social Anxiety Disorder. Diagnostic clarity is also important when we test our theories. Let's say that you want to find out whether gender, heredity, or childhood trauma plays a role in the development of some disorder such as schizophrenia, bipolar manicdepressive illness, phobias or panic attacks. Once you've defined the disorder you're studying in a fairly precise manner, you can test your theory empirically. If
* Copyright
2003 by David D. Burns, M.D.
Chapter 3
66
you look at the psychology and psychiatry journals that existed before the development of the DSM, you may be surprised by how quaint, metaphysical and non-empirical the articles are. If you don't know what you're talking about, science can't move forward. Diagnostic precision helps us clinically as well, because we can identify the types of interventions that are the most helpful for different kinds of problems. This allows us to match treatment techniques to disorders. In the old days, therapists used to think that a single treatment, like psychoanalysis, or psychodynamic psychotherapy, would be good for whatever ailed you. This type of reductionism seems incredibly naïve, and has never led to a single meaningful advance, at least none that I'm aware of. Unfortunately, many clinicians still seem to believe this. They think that their one method of treatment will be effective for a wide variety of disorders, so they don't bother to learn new, empirically validated treatment methods. When I do workshops on the treatment of anxiety around the country, I always ask the clinicians in the audience how many of them use exposure techniques when treating anxiety. Only about 20% of the hands go up. This boggles my mind! Exposure is probably the most extensively researched and validated psychotherapy technique in human history. And when I ask how many use Response Prevention, or have even heard of this technique, I get the same response—less than 30% of the hands go up. Now clinicians and researchers are beginning to understand that different kinds of emotional problems respond to radically different kinds of interventions.
Chapter 3
67
For example, the techniques that are so helpful for someone suffering from feelings of depression and inferiority are very different from the techniques that will help a patient who's struggling with panic attacks. Those techniques, in turn, will not be helpful someone struggling with a marital problem, or an addiction. That's one reason why we need sharp, sound thinking about the kinds of problems our patients have, and that's why the DSM has been so vitally important to our field. In spite of these advances, there are still a number of problems with the DSM-IV. To my way of thinking, these problems are severe. They include: Many of the diagnostic criteria seem arbitrary, unnecessarily complicated, and counterintuitive. The diagnostic criteria for various "disorders" tend to be non-specific, with lots of item-overlap. There's an excessive emphasis on the biological symptoms of many disorders, such as Major Depressive Disorder. There's a constant attempt to transform inherently continuous variables, such as feelings of shyness, worrying, or depression, into dichotomous variables, or "illnesses," that you can either "have" or "not have," such as "Social Anxiety Disorder," "Generalized Anxiety Disorder," or "Major Depressive Disorder." This requires the introduction of arbitrary criteria that don't map on to human experience in any meaningful way. Performing an adequate Axis I and II diagnostic screening interview on a new patient is time-consuming and frustrating for patient and therapist alike.
Chapter 3
68
The diagnostic system appears to be influenced far more by politics, and subjective impressions and preferences, than by science. The existence of the ten Axis II personality disorders has not been confirmed with rigorous statistical methods, such as factor analysis. In fact, some of the personality disorders, such as "Obsessive-Compulsive Personality Disorder," seem to represent a miscellaneous hodgepodge of symptoms that don't seem to hang together in a unified pattern. Before I comment on these problems, let me emphasize that the DSM system is of tremendous importance to our field. I don't want to sound overly negative, or like a know-it-all. I want to encourage critical, creative thinking about how we assign diagnoses and think about our patients' problems. I'm hopeful that our diagnostic system will evolve and become more sophisticated and userfriendly as future revisions of the DSM begin to address the conceptual and statistical problems I describe here. All these problems are easily solvable, but the solution may require a major paradigm shift. Now, let's review some of the problems with the DSM. Continue editing here Confusing Diagnostic Criteria The diagnostic criteria for most of the Axis I and II disorders are complicated, arbitrary, and difficult to remember. For example, to have a "Major Depressive Episode," you have to have a depressed mood or a loss of interest or pleasure, or both, every day for two weeks, along with at least 5 out of 9 additional symptoms that are listed as "Group A." I've been treating depression
Chapter 3
69
for 30 years, and I still can't remember exactly what symptoms are included in Group A. Can you? You also have to fulfill criteria B through E. You've probably reviewed the diagnostic criteria for mood disorders in the DSM-IV. Can you remember what the 9 symptoms in Group A are? Can you remember what criteria B through E are? Even if your patient fulfills all the criteria for a Major Depressive Episode, you still can't diagnose depression, or any mood disorder, for that matter. To diagnose a "Major Depressive Disorder," you have to fulfill several additional criteria. I won't ask if you remember what they are, because I'm pretty sure you don't. If you do remember, more power to you. The diagnosis of depression should be fairly simple and straightforward, but it has become incredibly convoluted. Overemphasis on Biological Symptoms If you review the DSM-IV, you'll see that many of the symptoms listed in Group A aren't specific or valid indicators of depression. Let's consider insomnia. If I were to create a list of the nine most important symptoms of depression, I definitely would not include insomnia. Here's why. There are at least 50 different causes of insomnia. They include drinking too much alcohol or coffee in the evening, jet lag, anger, anxiety, drug abuse, excitement, environmental noise, physical illness, pain, a cat that meows loudly and persistently in the middle of the night, having to study for final exams, coyotes outside that scream and yowl, and so forth. So when you ask patients if they've been having trouble sleeping,
Chapter 3
70
you're asking about a whole host of problems, and not simply depression. Weight loss and weight gain aren't very valid or reliable indicators of depression, either. Most depressed patients don't lose weight, and most of the people who gain or lose weight aren't depressed. Weight gain and weight loss have a host of causes other than depression. And many symptoms that are absolutely central to depression, such as feelings of hopelessness, aren't even included in the Group A symptom list for a Major Depressive Episode. I recently created a 25-item depression test that lists practically every symptom of depression in user-friendly language, with no psychological jargon or big words. I call it the Burns Depression Checklist. You can review it on page 72. As you can see, patients indicate how much they've experienced each symptom recently, with response options ranging from "Not at all" (0) to "Extremely" (4). Someone who answers "Not at all" on all 25 items will score 0 (no depression), and someone who answers "Extremely" on all of them will score 100 (the worst possible depression). I've administered this test to many individuals, along with other, well-established depression tests. Some of the people who took the test were not depressed, some were moderately depressed, and others were severely depressed. I analyzed the data with Structural Equation Modeling techniques. This is a sophisticated type of statistical analysis that allows you to determine the validity and reliability of a test, a portion of a test, or even single items, with a high degree of accuracy. Taken as a whole, the test had outstanding psychometric properties, substantially better than any of the well-known depression tests I
Chapter 3
71
compared it to. However, the analyses also indicated that the biological symptoms, such as "difficulty sleeping or sleeping too much," and "decreased or increased appetite," were not good indicators of depression. In fact, they're so non-specific that they will actually lower the reliability and validity of any assessment test or diagnostic system for depression. The symptoms that were absolutely central to depression included feeling sad or down in the dumps, discouraged or hopeless, worthless or inadequate, and a loss of self-esteem. A loss of pleasure or satisfaction in life was also a core symptom. Once you've created a brief scale that assesses these symptoms, you've accurately measured depression. If you add more and more symptoms to your scale, the reliability of your instrument will not increase, but may actually decrease, especially if you include non-specific biological symptoms. The emphasis on biological symptoms in the DSM-IV probably results from the fact that psychiatrists want to view emotional and behavioral problems as brain diseases that can be treated with pills. We want to tell our patients, "Oh, your depression results from a chemical imbalance in your brain. Let me write you a prescription for Prozac."
4—Extremely
3—A lot
Instructions. Use checks ( ) to indicate how much you've experienced each symptom during the past week, including today. Please answer all 25 items.
2—Moderately
Burns Depression Checklist*
1—Somewhat
72
0—Not at all
Chapter 3
Thoughts and Feelings 1. Feeling sad or down in the dumps 2. Feeling unhappy or blue 3. Crying spells or tearfulness 4. Feeling discouraged 5. Feeling hopeless 6. Low self-esteem 7. Feeling worthless or inadequate 8. Guilt or shame 9. Criticizing yourself or blaming yourself 10. Difficulty making decisions Activities and Personal Relationships 11. Loss of interest in family, friends or colleagues 12. Loneliness 13. Spending less time with family or friends 14. Loss of motivation 15. Loss of interest in work or other activities 16. Avoiding work or other activities 17. Loss of pleasure or satisfaction in life Physical Symptoms 18. Feeling tired 19. Difficulty sleeping or sleeping too much 20. Decreased or increased appetite 21. Loss of interest in sex 22. Worrying about your health Suicidal Urges ** 23. Do you have any suicidal thoughts? 24. Would you like to end your life? 25. Do you have a plan for harming yourself? Total Items 1 – 25
* Copyright
63
1984 by David D. Burns, M.D. Revised, 1996. ** Anyone with suicidal urges should seek help from a mental health professional.
Chapter 3
73
There's a comparable problem in internal medicine. At least 25% of the patients seen by physicians for complaints such as dizziness, pain, or fatigue don't have any real medical problems that could explain their symptoms. Instead, they're suffering from human problems, such as depression, anger, anxiety, or a broken heart. But doctors feel so much pressure to diagnose and treat medical disorders that they may not take the time to ask their patients about what's going on in their lives. Instead, they order more diagnostic tests and hand the patient a prescription. As a result, the patient never gets to identify or address the problems that are actually triggering the symptoms. This is the downside to overly high-tech medicine, and the same problem is now creeping into psychiatry. There's a push to make everything a biological disease. Arbitrary and Nonsensical Temporal Criteria The temporal criteria for various disorders seem arbitrary and misleading. The DSM-IV tells us that a patient cannot qualify for a "Major Depressive Episode" unless the symptoms have been present for at least two weeks. Well, what if the patient has been feeling severely depressed and suicidal for 13 days? Does that mean he doesn't have a "Major Depressive Episode"? And what happens at midnight of the 14th day? Does the "Major Depressive Episode" suddenly appear? Does the patient now have a new problem that he didn't have a few hours earlier? And now that he finally "has" a Major Depressive Episode, it would seem reasonable to ask, "When did the episode begin?" Obviously, it began two weeks ago. But how could this be, since according to our definition, the patient didn't
Chapter 3
74
have a Major Depressive Episode for the last two weeks. If you say, "But he really had a Major Depressive Episode the whole time," then why weren't we allowed to diagnose it earlier? It would seem like a good diagnostic system should allow us to diagnose the problem quickly and accurately. The temporal criteria for other disorders, such as Generalized Anxiety Disorder (GAD), are just as confusing. To qualify for GAD, the patient has to have "at least six months of persistent and excessive anxiety and worry." Let's assume that the patient has been worrying about things for 180 days. That's a couple days short of six months, so presumably, we can conclude that the patient definitely doesn't have GAD. On midnight of the last day of the sixth month, the patient finally fulfills the criteria for GAD. Does this mean that she or he now has a problem or "disorder" that she or he didn't have a day or two earlier? This seems almost as nonsensical as Alice in Wonderland! If I were working as an emergency room doctor, and you came in with a high fever, shortness of breath, and a productive cough, I'd strongly suspect pneumonia and order an x-ray. If the x-ray confirmed that your lungs were filled with bacteria or viruses, I'd diagnosis pneumonia, even if you'd only had the symptoms for a few hours. The duration of your symptoms wouldn't influence my diagnosis. I wouldn't say, "Oh, I'm not allowed to diagnose a case of pneumonia, because you haven't had the symptoms for seven days yet! But if you're still alive in a week, come on back and then I'll be permitted to diagnose and treat your pneumonia. Right now, you only have a case of 'non-pneumonia,' also called 'acute lung stress reaction.' Best of luck to you."
Chapter 3
75
You might ask, "Well, could you start me on antibiotics in the meantime?" I might have to reply, "No, that's a treatment for pneumonia. You have non-pneumonia. But we can probably start you on antibiotics next week, because then you'll have pneumonia." Symptom Overlap At the request of a colleague, I recently developed a brief, self-diagnostic screening instrument for Posttraumatic Stress Disorder (PTSD). The test maps precisely onto the DSM-IV criteria, but with two important differences. First, the test items are written in clear language, using words that are easy to understand, with no psychological jargon, much like the Burns Depression Checklist. Second, the response options are continuous, rather than "Yes-No." For example, one of the items on anhedonia reads, "Have you lost interest in activities you used to enjoy?" The response options are "Not at all" (scored 0), "Somewhat" (scored 1), "Moderately" (scored 2), "A lot" (scored 3), and "Extremely" (scored 4). Patients who strongly endorse the majority of the items on this test will have high scores, and yet they may have no symptoms of PTSD whatsoever. How can this be? It's because so many of the DSM-IV criteria for PTSD are symptoms of other problems, such as depression or Generalized Anxiety Disorder. So although the test I created is absolutely valid from the perspective of the DSM-IV, and has been an extremely useful diagnostic tool, it isn't valid in any real sense because it produces so many false-positive results. Of course, the problem is not with the test I created. It maps faithfully and accurately onto the DSM-IV criteria. The problem is with the criteria themselves.
Chapter 3
76
The Transformation of Human Suffering into Brain Diseases Suppose we could measure how depressed a group of people were every day, with a high degree of accuracy, from the moment of birth to the present. Then we could plot each person's mood over time on a graph. We'd see that our moods constantly fluctuate, much like oscilloscope patterns. Furthermore, we'd all have our own unique "moodprints." Some people would be happy most of the time, and when they got upset, they'd quickly recover. Other people would be mildly depressed a good bit of the time, with occasional periods of severe depression and occasional periods of happiness. Some people's moods would frequently go up and down, while others would be relatively steady. The psychiatrists who create the DSM have taken certain areas under these mood curves and given them names. So a two-week period of severe depression would be called a "Major Depressive Episode," and a fairly steady two-year period of mild depression would be called a "Dysthymic Disorder," and so forth. Of course, there are lots of other names for other varieties of "mood disorders," because there are so many different patterns. But what they're doing, literally, is trying to force square pegs into round holes. You lose a tremendous amount of information when you do this, and you create confusion, but you don't gain anything. Once you know how severe the feelings of depression are, and how they fluctuate over time, you know exactly how depressed that person has been. You now have all the information. Adding a dichotomous term, like "Major Depressive Episode," simply muddies the waters and creates confusion.
Chapter 3
77
The same is true with nearly any kind of emotion. We could create an accurate scale that measures how anxious and worried a person feels, and we could use this scale to assess the severity of worrying every day. Or, we could create a brief scale that measures feelings of shyness, and we could administer that scale every day. Or, we could create a scale that measures panic attacks, and determine how often a person has a panic attack, and how severe each attack is. Once you do this, you've got all the available information. When you try to apply a diagnostic label, such as Generalized Anxiety Disorder, Social Anxiety Disorder, or Panic Disorder, you have to start creating arbitrary cut-off criteria. This is the source of most of the difficulties with the DSM-IV. You can create any set of diagnostic criteria you want, but they'll always be arbitrary. For example, how long do the feelings of depression have to last before someone has a real "Major Depressive Episode"? Why did they settle on two weeks? Why not one week? Or five weeks? Or 12 weeks? And how severe does the depression have to be, on average, during that two-week period? What's the cut-off score going to be? In other words, the DSM conceptualizes human suffering as a series of disorders that you can either "have" or "not have." For some problems, like schizophrenia or bipolar illness, this seems justified. Although we don't yet know the cause of these disorders, they're definitely not normal experiences that we can all relate to. Most of us have never experienced the symptoms of schizophrenia, such as hearing voices coming from outside your head or
Chapter 3
78
believing that you're receiving secret messages from radio and television programs. And most of us will never experience the overwhelming euphoria or bizarre, impulsive behavior of a full-blown manic episode. Schizophrenia and Bipolar I (Manic-Depressive) Disorder do seem to reflect profound brain abnormalities of some type. They probably are true brain diseases. But dichotomizing doesn't work for most of the Axis I and II disorders, because they're based on common human feelings that most people experience from time to time. I recently completed a book for the general public on anxiety disorders. While I was writing it, I counted up at least 10 distinct forms of anxiety I've personally experienced at some time or another during my life. They include the fear of heights, bees, and blood, as well as public speaking anxiety, generalized anxiety, panic, shyness, and hypochondriasis, among others. The same considerations apply to depression. Most of us have known what it's like to feel sad, worthless, inadequate, discouraged, panicky or shy, at least for short periods of time. What happens when we tell a patient, "You have an illness called Social Anxiety Disorder. It results from a chemical imbalance in your brain. But you're in luck. Paxil will correct the problem for you"? There are some problems with this message. In the first place, I'm not aware of any evidence whatsoever that shyness results from any type of chemical imbalance in the brain. In fact, there is no test for a chemical imbalance in the brain. So we're telling patients something that's not likely to be valid, and
Chapter 3
79
something that can't be confirmed with a test of any type. Would a medical doctor be allowed to operate like this? If you came to me because of fatigue, and I suspected iron-deficiency anemia, I'd order a series of tests to confirm that you really were anemic and to pinpoint the cause of it. I wouldn't tell you that you had iron-deficiency anemia until I'd confirmed my impressions with lab work and systematically ruled out dozens of other potential causes of fatigue. Then why are mental health professionals allowed to tell depressed or anxious patients that they have a "chemical imbalance" in their brains? It's beyond me! You might say, "Well, haven't researchers already proven that depression and anxiety result from a chemical imbalance in the brain? Doesn't everyone know that these problems result from a brain serotonin deficiency?" I don't know that. I'm not aware of a single study in the world literature that's ever demonstrated a causal link between brain serotonin and any psychiatric disorder. This is just a theory, and nothing more. There's another problem. Recent studies suggest that antidepressants may have few, if any, actual antidepressant effects above and beyond their placebo effects (Antonuccio, Burns, & Danton, 2002; Hypericum depression trial study group, 2002; Kirsch & Sapirstein, 1998; Kirsch, Moore, Scoboria, & Nicholls, 2002). The evidence for their efficacy in the treatment of most anxiety disorders, such as shyness, is even weaker (Westra & Stewart, 1998). It's simply not true that individuals suffering from shyness are likely to be cured by Paxil, or
Chapter 3
80
any other medication. It would be great if this were true, but it's not. Perhaps the biggest problem with the transformation of human problems into illnesses is that patients may wrongly conclude that they're the victims of forces beyond their control. A young man who's struggling with shyness has just been told by a doctor that he has a brain disease. Very few patients have the critical training or capacity to see through this message. But if this patient really wants to overcome his shyness, he'll have to take the bull by the horns and use a variety of cognitive and behavioral techniques. Being passive and waiting for a pill to cure him is not going to cut it. He's still going to be shy, and he still won't know how to flirt with women. The Axis II Diagnostic Criteria are Equally Confusing The diagnostic criteria for the Axis II disorders are plagued by similar conceptual problems. Are they really "disorders," or simply descriptions of emotional and behavioral symptoms that sometimes cluster together? And are they really distinct from each other? If you do a statistical analysis of the diagnostic criteria, you'll discover that the 10 so-called " personality disorders" don't even exist as distinct patterns in the way they're conceptualized in the DSM. The temporal requirements for Axis II disorders are also confusing. For example, to qualify for Narcissistic Personality Disorder, you need to have the characteristic symptoms of the disorder, such as the belief that you're more important than other people, a lack of empathy, and a tendency to exploit others. In addition, the pattern has to begin in early adolescence or early adulthood.
Chapter 3
81
Well, what if someone becomes extremely narcissistic later in life, perhaps as the result of acquiring great fame and wealth? Would we say they're not allowed to have "Narcissistic Personality Disorder"? And if so, then what do they have? Here's another problem. The narcissism has to cause "clinically significant distress or impairment in social, occupational, or other important areas of functioning." These criteria are problematic because narcissism often works in a person's favor. What if the narcissistic individual is perfectly happy exploiting other people? I'm sure you can think of many extraordinarily narcissistic people who aren't at all bothered by their narcissism, from brutal, grandiose political leaders like Hitler or Saddam Hussein, to high-profile professional athletes, CEOs, and entertainers. Would we have to conclude that they do not have Narcissistic Personality Disorder? This is like saying that if someone gets away with murder, then they didn't really commit a crime! In summary, the reliabilities and validities of practically all the Axis I and II disorders are poor, even if you administer meticulous, time-consuming, structured diagnostic interviews. Of course, you can train two researchers to ask the diagnostic questions in the exact same manner, so they'll almost always agree on whether or not a patient has a particular disorder. This is called "interrater reliability." But this does not mean that the diagnoses the researchers assigned are valid or reliable, because they've simply been trained to make the same kinds of nonsensical errors when they assign the diagnoses. Where do the DSM diagnostic criteria come from in the first place? A
Chapter 3
82
group of politically influential psychiatrists get together in committees and vote. They decide on what diseases do or don't "exist," and how we're going to diagnose them. These decisions are usually far more political than scientific. One year, homosexuality is a disease. The next year, it's not. Few of the psychiatrists who create the DSM have had the training in the statistical modeling techniques that would be necessary to develop a robust and reliable diagnostic system. I'm hopeful that as the DSM continues to evolve, many of these problems will be corrected. However, that may take a decade or more. In the meantime, we're under an ethical, professional and legal obligation to diagnose every new patient we treat according to strict DSM-IV criteria. In the next chapter, I'll suggest a practical solution to this dilemma, and show you how to do a comprehensive and accurate Axis I and II diagnostic screening without getting bogged down in the process.
4*
The Easy Diagnostic System for DSM-IV
Doing a comprehensive diagnostic screening for Axis I and II disorders, according to strict DSM-IV criteria, can be time-consuming, frustrating, and boring, but it's a necessary part of a competent and professional intake evaluation. If you do it properly, it can take two to three hours. As a result, very few therapists do an adequate job of it. Instead, most therapists just scribble some likely diagnosis in the chart at the end of the intake evaluation. This is tempting but dangerous, because you may overlook problems that will be vitally important to the treatment, such as the presence of substance abuse, Borderline Personality Disorder, or potentially dangerous suicidal or violent urges. Furthermore, it's very unusual for patients to have a single disorder. In fact, most patients will have many probable or definite Axis I and II disorders at the same time. If you had to defend your work in court, a hostile attorney could easily put you on the defensive if you hadn't done a thorough * Copyright
2004 by David D. Burns, M.D.
Chapter 4
84
diagnostic screening at intake and documented your findings in the chart. I was recently speaking to a Stanford resident named Aaron about this problem. He explained that he and the other residents were under intense timepressure, and could only afford to budget a few minutes for diagnostic screening during the intake interview. He added that if there were a way to do a thorough diagnostic screening interview in five or ten minutes, he'd be happy to do it. I thought, "That's impossible! There's no way you could possibly do a systematic Axis I and II screening interview in less than two hours." Several weeks later, a solution suddenly came to me in a dream and I woke up feeling excited. The solution seemed so obvious that I wondered why I hadn't thought of it sooner. For a number of years, I'd been developing brief, highly reliable selfassessment instruments for a wide range of emotional problems, such as mood disorders, anxiety disorders, and a variety of other Axis I problems. It occurred to me that if I created just a few more instruments, and bundled them, I'd have a reasonably complete DSM-IV self-diagnosis assessment package that covered most of the common Axis I disorders. I decided to call it the Diagnostic Survey for Axis I Disorders. I thought that patients might be able to complete this survey on their own in the waiting room before the intake evaluation, or at home between their first and second therapy sessions. Then my colleagues and I could simply look through the patient's answers, note which tests had elevated scores, and ask a few additional questions to find out if the patient fulfilled the official DSM-IV
Chapter 4
85
criteria for a possible or definite diagnosis. It dawned on me that this type of diagnostic screening process could be very systematic and comprehensive, but would only require a few minutes of the therapist's time. I began to work on the project immediately, and soon developed the first version of the Axis I Diagnostic Survey. I began to test it right away. Sure enough, my residents found that they could accurately screen for more than 40 Axis I disorders in less than five minutes. At the time, my resident, Aaron was treating an attorney named Harold who was suffering from recurrent major depressive episodes as well as anxiety. He was also having difficulties forming intimate relationships and struggling with impulsive, risky sexual behavior. Aaron thought that Harold might also have Narcissistic Personality Disorder (NPD). I asked Aaron if he could remember the DSM-IV diagnostic criteria for NPD, and whether he’d gone through them with his patient. Aaron confessed that he couldn't remember the criteria for a diagnosis of NPD, or for any of the Axis II disorders. I was relieved because I couldn’t remember what they were, either! I wondered if it might be possible to develop a self-assessment test for NPD that mapped directly onto the DSM-IV criteria. That would make our diagnostic task much easier. Narcissistic patients could also take this test once a week so we could assess their progress, just as we were doing for depression and anxiety. After all, if we're treating people for NPD, wouldn't it make good sense to track their improvement over time? Aaron was enthusiastic about this idea, so I created the first draft of my
Chapter 4
86
self-assessment test for NPD. I used familiar, non-technical words to create two assessment items for each of the required symptom dimensions, such as: The sense of being special Fantasies of unlimited success The need for admiration Feelings of entitlement Exploitation of others A lack of empathy Envy A sense of superiority You can see the two statements that assess the first dimension, the sense of being special, on page 87. I labeled the test, "Narcissistic Tendencies," rather than "Narcissistic Personality Disorder," because the "disorder" label sounded fatalistic and judgmental, as if the patient were irreversibly defective. I also decided on continuous response options that ranged from "Not at all true" (rated 0) to "Completely true" (rated 4) for several reasons. First, I knew that continuous response options would make it far easier to respond to these kinds of items. After all, most of us have a few Axis II symptoms from time to time. I know I do! But to diagnose a personality "disorder," such as NPD, the symptoms have to be fairly intense and persistent. Second, you can simply total the score and see exactly how severe the symptoms are. And finally, tests with continuous response options are more meaningful and have vastly superior psychometric properties than tests that artificially dichotomize symptoms and diagnoses into
Chapter 4
87
"yes" vs. "no" categories. The idea wouldn't be, “Do you have this disorder?” but
Sense of Being Special 1. I sometimes have a tremendous sense of my own importance or talents. 2. I sometimes feel like I'm extremely special. Total Items 1 - 2
I had no idea whether the test would work, but I was excited to find out. Would Harold answer the items honestly? Clearly, if patients know that their therapists will look at the answers, this could lead to a response bias, because some patients might try to make themselves look better, or worse, than they really are. I was also wondered whether he'd find the test upsetting, since it was fairly blunt. I showed Aaron the test at our next supervision session, and asked he'd be willing to give it to Harold. Aaron said he was afraid that Harold might feel insulted and fly into a rage. But he said that if I'd join them for a session, I could personally ask Harold to fill it out.
* Copyright
1998 by David D. Burns, M.D. Revised 2002.
4—Completely true
3—Very true
Please answer all the items.
2—Moderately true
Instructions: Use checks ( ) to indicate how much each statement describes how you have felt or behaved during most of your life since your teenage years.
0—Not at all true
Narcissistic Tendencies*
1—Somewhat true
rather, “How strong are these tendencies at any point in time?”
Chapter 4
88
The next week, Aaron introduced me to Harold in the waiting room. He explained that I was his supervisor and wanted to join them for a session, with Harold's permission. Harold seemed pleased and said he’d love to have me join them. Once we sat down in the office, Aaron explained that I'd created a new psychological test that I wanted to show him. Harold was intrigued, and seemed eager to fill it out. I could see his answers as he was checking them off, and noticed that he was answering "Completely true" or "Very true" on every item. I braced myself, and my heart began to beat rapidly, because I was aware that narcissistic individuals often react with intense anger to any hint of criticism or disapproval. About two-thirds of the way through, Harold looked up at me with a broad smile and exclaimed, “I think you must have created this test just for me!" And the funny thing was that I had. Harold had almost a perfect score on the test, consistent with a diagnosis of definite Narcissistic Personality Disorder. Every item seemed to fit him to a tee. This experience was encouraging, but an N of 1 is hardly sufficient to validate a new test. In addition, I was concerned about false-positive results, and wondered if most people would score this high on the test. To find out, I administered my narcissism test to the 10 psychiatric residents who were attending my weekly psychotherapy seminars. Fortunately, they responded with "Not at all true" or "Somewhat true" on nearly all the items on the test, indicating very few symptoms of Narcissistic Personality Disorder. It
Chapter 4
89
seemed that the test was extremely discriminating, since their scores were at the opposite end of the spectrum from Harold’s. I wondered whether it might be possible to create valid self-assessment tests for the other Axis II disorders as well. Next, I created a user-friendly test for Borderline Personality Disorder (BPD). Once again, I translated the DSM-IV criteria into understandable, nonpejorative items with continuous response options. Patients with obvious BPD endorsed nearly all the items, and had high scores. In contrast, individuals without BPD endorsed only a few of the items to a slight degree, and had low scores. The pilot version of the BPD test was also surprisingly discriminating. I was so encouraged that before long, I'd created tests for all 10 personality disorders, and had my first Axis II self-assessment package. I decided to call the Axis I and II screening tests the Easy Diagnostic System for DSM-IV. Since then, the Easy Diagnostic System has undergone considerable refinement and revision, and continues to do so. Patients can complete the current Axis I package in about 25 minutes. The Axis II package takes about 10 minutes. Therapists can usually complete the face-to-face diagnostic screening for Axis I and Axis II in five to eight minutes, or less, depending on how complex the patient is. I've also created a Diagnostic Guidebook that tells therapists what questions to ask in order to confirm a possible or definite diagnosis, using DSM-IV criteria, when patients have elevated scores. On pages 92 – 93, you can see a copy of the Axis I and II Diagnostic
Chapter 4
90
Summary Sheet. It lists more than 50 Axis I and II disorders that you can automatically screen for, along with their diagnostic codes. They're all "No" by default. When you review the patient's answers on the Axis I and II surveys, you can simply check off “Possible” or “Yes” on this sheet. You can include the Diagnostic Summary Sheet in the chart, along with the Axis I and II surveys the patient filled out. That way, all the patient's diagnoses will be clearly documented. Most patients have multiple possible or definite Axis I and II diagnoses at intake. For example, let's say that the chief complaint is chronic depression. The patient may qualify for an Axis I diagnosis of definite Major Depressive Disorder as well as Dysthymic Disorder. However, the patient may also have several anxiety disorders, along with substance abuse, relationship problems, and a few possible or definite Axis II diagnoses as well. The Easy Diagnostic System has been quite helpful because you can do a competent and thorough diagnostic screening without getting bogged down in the process. It's also been helpful to me as a clinical supervisor. When residents present new cases to me, they show me the Diagnostic Summary Sheet and I can see all the diagnoses at a glance. If I'm unclear on why the resident did or didn't assign a particular diagnosis, we look at the way the patient filled out the relevant self-assessment test, and I can immediately see which symptoms formed the basis for the resident's conclusions. Of course, you should never rely on a test to do your thinking for you. The Easy Diagnostic System will usually provide you with information that might not otherwise be available to you, but your own expertise will always be the gold
Chapter 4 standard whenever you assign a diagnosis or interpret any test a patient completes.
91
Chapter 4
92
Axis I Diagnostic Summary Sheet*
Code
No ( )
Possible ( )
Yes ( )
Relational Problems and Other Conditions V62.3x Academic Problem V62.2x Occupational Problem 313.82 Identity Problem V61.20 Parent-Child Relational Problem V61.1x Partner Relational Problem V61.8x Sibling Relational Problem V62.81 Relational Problem NOS V61.9x Psychiatric or Medical Condition in Family Member V62.82 Bereavement Mood Disorders 309.0 Adjustment Disorder with Depressed Mood 291.8x Substance-Induced Mood Disorder 293.83 Mood Disorder due to a General Medical Condition 309.28 Mixed Episode 296.2x Major Depressive Disorder, Single Episode 296.3x Major Depressive Disorder, Recurrent 300.4x Dysthymic Disorder 296.xx Bipolar I Disorder 296.89 Bipolar II Disorder 301.13 Cyclothymic Disorder Anxiety Disorders 300.02 Generalized Anxiety Disorder (GAD) 300.01 Panic Disorder Without Agoraphobia 300.21 Panic Disorder With Agoraphobia 300.22 Agoraphobia Without History of Panic Disorder 300.29 Specific Phobia Describe type: 300.23 Social Phobia (Social Anxiety Disorder) 309.81 Post-Traumatic Stress Disorder (PTSD) 300.3x Obsessive-Compulsive Disorder (OCD) 309.24 Adjustment Disorder with Anxiety Somatoform Disorders 300.7 Hypochondriasis 300.7† 307.8
Body Dysmorphic Disorder (BDD) Pain Disorder Gambling
312.31 Drug and Alcohol Problems 305.00 Alcohol Abuse 303.90 Alcohol Dependence 304.xx Psychoactive Substance Dependence 305.xx Psychoactive Substance Abuse Pathological Gambling
*
See the Therapist's Diagnostic Guidebook or Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) for additional help. † DSM-IV assigns the same code to hypochondriasis and BDD for compatibility with ICD-9-CM.
Chapter 4
93
Axis I Summary (cont'd)
Code
No ( )
Possible ( )
Yes ( )
No ( )
Possible ( )
Yes ( )
Eating Disorders 307.50 Binge Eating Disorder (Eating Disorder NOS) 307.51 Bulimia Nervosa 307.1x Anorexia Nervosa Schizophrenia 295.30 Paranoid Type 295.10 Disorganized Type 295.20 Catatonic Type 295.90 Undifferentiated Type 295.60 Residual Type 295.70 Schizoaffective Disorder Other Axis I Disorders
Axis II Diagnostic Summary Sheet*
Code
Cluster A Paranoid Personality Disorder Schizoid Personality Disorder Schizotypal Personality Disorder
301.0 301.20 301.22 Cluster B
Antisocial Personality Disorder Borderline Personality Disorder Histrionic Personality Disorder Narcissistic Personality Disorder
301.7 301.83 301.50 301.81 Cluster C
*
Avoidant Personality Disorder Dependent Personality Disorder Obsessive-Compulsive Personality Disorder
301.82 301.6 301.4
Other Personality Disorder NOS (Not Otherwise Specified)
301.9
See the Therapist's Diagnostic Guidebook or Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) for additional help.
Chapter 4
94
This is true in medicine as well. When I was a medical intern, we treated a man named Gregory who was running temperatures as high as 104. No one had been able to track down the cause of the fever. Gregory had been hospitalized on numerous occasions and subjected to test after test, but they always came back normal. As a last resort, we were planning exploratory abdominal surgery to see if he had an occult lymphoma, such as Hodgkin’s Disease. However, we decided on one last “test” before the surgery. We moved Gregory to a room with a one-way mirror for a few days so we could observe him when there were no medical personnel in the room. We were surprised to discover that when the nurse left the room, Gregory would furtively remove the thermometer from his mouth and place it next to the light bulb. Then he'd quickly place it back in his mouth and lay there innocently, waiting for the nurse to return. This led to the correct diagnosis—Munchausen’s Syndrome, or the pathological faking of illness. The moral of the story is that the results of any medical or psychological test must be interpreted by a shrewd health professional, because even an instrument as valid and reliable as a thermometer can be misleading. All that being said, I’ve been pleased by how accurate and helpful the Easy Diagnostic System has been. The vast majority of patients seem to be honest and open in their responses to the questions. Although a top-notch initial assessment will not guarantee successful treatment, you'll know that you've gotten the therapy off to a great start and laid the groundwork for superb clinical work. Many experts have tried to streamline the diagnostic process, and have
Chapter 4
95
developed a number of approaches that you might want to consider, including: Structured Clinical Interview for DSM-IV® Axis I Disorders (SCID-I). This structured clinical interview for Axis I disorders is based on substantial research, so the data you obtain will be suitable for publication. However, it's time-consuming (90 minutes for Axis I alone) and can be a bit frustrating to administer, since you constantly have to force symptoms and diagnoses into dichotomous "yes" versus "no" categories. This can create statistical and conceptual confusion. At my clinic in Philadelphia, we evaluated the reliabilities and validities of the SCID-I diagnostic categories using confirmatory factor analysis, and found that they were low. You can purchase Axis II booklets as well, but they'll require even more time. In addition, the SCID system can be costly. You can purchase the User's Guide, Administration Booklet, and 5 scoring sheets for Axis I disorders for approximately $90 through American Psychiatric Publishing, Inc. They can be found online at: http://www.appi.org/group.cfm?groupid=SCID-I. THE CIDI-Auto: A Computerised Diagnostic Interview for Psychiatry. This automated diagnostic system is somewhat costly ($500) and requires special hardware and computer training courses. You will also have to purchase and learn how to use SPSS, a sophisticated and costly statistical analysis program. You can learn more about the CIDI system by checking out the Clinical Research Unit for Anxiety and Depression website at: http://www.crufad.unsw.edu.au/cidi/cidi.htm.
Chapter 4
96
The Mini-International Neuropsychiatric Interview (MINI). The MINI is a short, structured diagnostic interview for DSM-IV and ICD-10 psychiatric disorders. It was designed for use in multi-center clinical trials, epidemiology studies and clinical settings. On the advantages side, the MINI is not overly time-consuming, has been validated against the SCID-I, and has been translated into many foreign languages. On the disadvantages side, it still conforms to the frustrating "yes" versus "no" dichotomous system of the DSM-IV and only screens for a limited number of disorders. A more comprehensive version called the "MINI Suite" is available, but requires several hours of interview time. You can learn more about it by visiting the website for Medical Outcome Systems, Inc. at: http://medicaloutcomes.com/minisuite.asp. The following references, which can be obtained from online booksellers such as Amazon.com, could be useful as well: American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision). Arlington, VA: American Psychiatric Association. Zimmerman, M. A. (1994/96). Interview Guide for Evaluating DSM-IV Psychiatric Disorders and the Mental Status Examination. East Greenwich, RI: Psych Products Press. I now view diagnosis and testing as a three-stage process. In Stage 1, you do your preliminary symptom screening, using the Axis I and II self-assessment packages. Because the patient completes them on their own, no therapy time is
Chapter 4
97
required. In Stage 2, you assign diagnoses, based on DSM-IV criteria. This takes five to eight minutes. In Stage 3, you measure the relevant symptoms on a session-by-session basis so you can track the patient’s progress during the treatment. This takes less than one minute, since patients will complete these tests on their own between sessions as part of their psychotherapy homework. Let's assume that your new patient, Sharon, has completed the Axis I and II self-assessment tests. When you review them, you notice that she has a score of 18 out of 20 on the Shyness screening test on page 98. Can we reasonably conclude that she has a DSM-IV Axis I diagnosis of Social Phobia (Social Anxiety Disorder, diagnostic code 300.23)? Indicate your answer with a check ( ) before you turn the page. ( ) 1. Sharon definitely has Social Anxiety Disorder. 2. Sharon does not have Social Anxiety Disorder. 3. Needs further discussion.
4—Completely true
Please answer all of the items.
3—Very true
Instructions. Use checks ( ) to indicate how you've been feeling recently.
2—Moderately true
Speedy Screening for Anxiety Disorders*
1—Somewhat true
98
0—Not at all true
Chapter 4
Shyness 1. I often feel nervous or embarrassed in social situations. 2. I often feel anxious or insecure in social situations. 3. I often feel shy or uncomfortable around others. 4. I avoid social situations because they make me so uncomfortable. 5. I'm afraid of being humiliated or judged in social situations. Total Items 1 – 5
* Copyright © 2003 by David D. Burns, M.D.
18
Chapter 4
99
Answer Even though Sharon seems to have all the symptoms of Social Anxiety Disorder, we can't make a definite or possible diagnosis yet. The Diagnostic Guidebook reminds us that we need to find out the answers to these questions first: Does exposure to social situations nearly always provoke feelings of shyness and anxiety? Does Sharon realize that her fears are excessive or unreasonable? If she's suffering from paranoid schizophrenia, she may experience anxiety in social situations because she thinks that people are conspiring with the FBI to spy on her. In this case, her discomfort in social situations would result from paranoia, not shyness. Do the feelings of shyness cause problems in her life? For example, do they interfere with her social life or performance at work? Sharon will almost definitely give you a strong yes. Do the feelings of anxiety in social situations result from some other problem, such as drug intoxication or Body Dysmorphic Disorder? In this case, you would not need the additional diagnosis of Social Anxiety Disorder. In the vast majority of cases, you'll assign a diagnosis of definite Social Anxiety Disorder after you ask these three additional questions. You'd probably think about these additional criteria even if you did not have the Diagnostic Guidebook available, because they're pretty obvious. Let's assume that the situation is not quite as clear-cut. Sharon's score on
Chapter 4
100
the Shyness screening test is only 11, and she's coping with her shyness fairly well. Does she fulfill the criteria for Social Anxiety Disorder? Or doesn't she? You don't have to try to figure out the correct answer to this question, since there isn't one. The confusion results from the fact that the DSM-IV insists on conceptualizing continuous variables, like shyness, as dichotomous variables, such as "Social Anxiety Disorder." It's a little like asking how many angels can dance on the head of a pin! Instead of wasting time and energy worrying about whether Sharon "does" or "does not" have Social Anxiety Disorder, you can simply check off "Possible" on the Diagnostic Summary Sheet. Let's assume that you assign a diagnosis of definite Social Anxiety Disorder. Does this mean that Sharon is suffering from an "illness" called "Social Anxiety Disorder"? If you read the last chapter, you know that there's no such "thing" as "Social Anxiety Disorder." Shyness definitely exists, but "Social Anxiety Disorder" probably does not. It's just a more severe degree of shyness, and not a true entity or disease. Although we've assigned this diagnosis correctly from a medical-legal perspective, I'll be helping Sharon overcome her shyness. I won't be treating a true "brain disease." The same is true of the Axis II Disorders. Once I've measured a patient's narcissistic or borderline tendencies, I would prefer not to have to assign the additional label of "Narcissistic Personality Disorder," or "Borderline Personality Disorder." To my ear, these labels make the problem seem hopeless, as if you had some kind of inherent defect. Furthermore, I can evaluate and treat the patient's problems perfectly well and monitor session-by-session progress far
Chapter 4
101
more accurately without the use of these labels. For the record, I want to be absolutely clear that I'm not advocating the elimination of concepts such as "depression," "narcissism," "panic," or "shyness." These problems are real, and they cause a great deal of suffering. What I am objecting to is the "disorder" tag, because it involves the transformation of continuous variables into dichotomous ones, and carries strong political implications that are not based on scientific considerations. Furthermore, if I don't use these all-or-nothing labels, I won't have to ask the question, "Has this patient recovered yet?" This question is meaningless because you have to create arbitrary cut-off points for recovery. How much improvement is needed for true recovery? Is it ten points? Fifteen points? Would a 50% reduction in symptoms be enough? Or would you need a 90% reduction? Once again, this is like arguing about how many angels can dance on the head of a pin. Instead, you can ask this question: "How much has this patient improved so far?" This question can be answered with precision. If you administer a brief, reliable self-assessment test at every therapy session, you'll see exactly how much progress the patient has made, and how much work remains to be done. The beauty of the Easy Diagnostic System is that you can have it both ways. You can evaluate the problems you're treating in a sensible way, as continuous variables, and you can assign the DSM-IV diagnostic categories at the same time. That way, you'll be fulfilling your ethical and legal responsibilities. Many therapists have questioned whether patients will be honest when
Chapter 4
102
completing the Axis I and II surveys. I think that we sometimes make a big error in assuming that people cannot, or will not, fill out these instruments accurately. I've been pleasantly surprised by how honest people actually are. In the vast majority of cases, you'll get an immense amount of valuable information that would not ordinarily be available to you. As you can see on page 103, I've also created an honesty scale patients can fill out when they've completed the diagnostic surveys. Patients can indicate whether they found any test items upsetting, or felt they couldn't be completely honest in responding to any test items. Sometimes patients indicate that they didn't answer some items honestly. If you ask which ones they had trouble with, they'll usually say, "Oh, I had trouble with this one and this one." Then you can ask them to explain the problems they encountered. Of course, there are exceptions to every rule, and you always have to be shrewd and alert to intentional deception, and to potentially false positive or negative responses. That's why you have to confirm the diagnoses yourself. Patients who have hidden financial motives can be particularly problematic. For example, if patients know that they'll receive monthly disability payments for severe depression or PTSD, it may be hard for them to fill out the tests honestly, since a great deal of money is on the line. We're all human and potentially corruptible. I'm not trying to be critical of people who are suffering from depression or PTSD, but simply pointing out a basic fact of human nature. In my opinion, clinicians should not attempt to treat patients who have competing financial interests that might interfere with their ability to be honest, as
Chapter 4
103
well as their ability to recover. Experts who aren't involved in treatment are in the best position to do forensic evaluations, and clinicians who aren't involved in forensic evaluations are in the best position to treat patients. If you try to do both, you're asking for trouble! I don't believe there's any way around this problem. Once you've completed the intake evaluation and assigned the diagnoses, you can track the patient's progress from week to week with brief selfassessment tests. I measure different kinds of mood problems in slightly different ways. Let's assume that Sharon has a diagnosis of Social Anxiety Disorder. Shyness is a bit tricky to measure because it's so context specific. If you measure how shy Sharon has been feeling over the past week, she might report few or no symptoms at all. Does this mean that you've cured her? Low scores on a shyness test could simply reflect her avoidance of feared situations, rather than any progress in the therapy.
Difficulties with the Test 1. This test was upsetting. 2. This test was frustrating. 3. This test was hard for me. 4. Sometimes I felt confused by the questions. Openness and Accuracy 5. Some of my answers were not very accurate. 6. It was hard to answer some of the questions honestly. 7. It was hard to be completely open when I answered some questions. 8. My answers weren't always completely correct. 9. Sometimes I tried to make myself look better than I really am. 10. Sometimes I tried to make myself look worse than I really am.
Similarly, you could measure how shy Sharon feels when she's with you, but this could be misleading as well. Once she gets to know you, she may feel relaxed when she's with you, but may still experience crippling shyness in other situations. You can see my solution to this problem on page 105. On the Shyness Survey, you can see how shy Sharon feels in a variety of situations on a scale from 0 (not anxious or shy) to 10 (extremely anxious or shy). Her scores on this test will provide you with one way of assessing the severity of her shyness from week to week.
* Copyright
1989 by David D. Burns, M.D.
4—Completely true
Please answer all the items.
3—Very true
Instructions. Use checks ( ) to indicate how well each statement describes your feelings about this survey.
0—Not at all true
Feelings About the Test*
2—Moderately true
104
1—Somewhat true
Chapter 4
Chapter 4
105
Shyness Survey* Instructions. Some people feel anxious or shy around others. Please put a number between 0 (not anxious or shy) and 10 (extremely anxious or shy) to indicate how much discomfort you usually feel in each of the following social situations. Please answer all the items. 0 = not anxious or shy; 10 = extremely anxious or shy Family
0
Friends
5
Boss
8
Talking to strangers
10
People in general
8
Colleagues
8
Introducing or being introduced
10
The opposite sex
10
Authority figures
10
Social occasions
10
The same sex
5
Teachers
5
Clerks or other people in stores
10
Dating
10
Public speaking
10
Medical doctor
5
Therapist
5
Other situations
8
1.
I'd feel nervous or embarrassed.
2.
I'd feel anxious or insecure.
3.
I'd feel shy, inferior or uncomfortable.
4.
I'd have fears of looking awkward or foolish.
5.
I'd avoid or leave the situation because I felt so anxious.
4—Extremely true
Please answer all the items.
3—Very true
Indicate how you'd be feeling if you were in that situation RIGHT NOW, at this very moment.
2—Moderately true
Talking to attractive men.
0—Not at all true
Instructions. Think about ONE of the situations listed above. Briefly describe the situation here:
1—Somewhat true
Shyness Scale
Total 1 - 5
18
On the Shyness Scale, Sharon has selected a particularly challenging situation—talking to attractive men—and indicated how shy she'd be feeling if she were in that situation right now. If she selects the same situation each week, it will provide you with an accurate measurement of her progress. The Easy Diagnostic System doesn't solve all the problems with the DSM* Copyright
1989 by David D. Burns, M.D. Revised 2004.
Chapter 4
106
IV that I described in the previous chapter, but it will provide you with a convenient work-around.* You'll be able to use the DSM-IV in a professional and competent way without getting bogged down by a tedious, structured diagnostic interview. In addition, you'll be able to track your patients' progress quickly and accurately at every therapy session throughout the treatment. We'll talk more about this important topic in Chapter 7.
* To learn more about the Easy Diagnostic System, send an email to [email protected].
5*
How to Take a Really Good Clinical History
Taking a clinical history probably isn't the most exciting topic, but it is important to do it properly. If you're in a private practice setting, your clinical work will usually begin with a phone call. The patient will ask about your availability and set up the initial appointment. Sometimes, someone else will call on the patient's behalf. For example, a woman might call because her husband is depressed, or because she's concerned about her 19 year-old son. I would strongly recommend against setting up this type of appointment. You can provide empathic support, but it's unwise to make an appointment unless the prospective patient personally calls to request it.† There are many reasons for this. In the first place, the patient might not be motivated to seek treatment, and might not even show up for the appointment. But even if he does, he may only be there because of external coercion. I'd prefer
* Copyright
2004 by David D. Burns, M.D.
† Of course, there are exceptions to every rule. For example, if the prospective patient is a child, then the parents will have to call to set up the appointment.
Chapter 5
108
not to get involved in any pattern of manipulation that may be occurring in the family. Ultimately, the patient has to ask for help himself, and has to be willing to work hard if the therapy is to be successful. We'll discuss this idea throughout the book, but it's important to understand that the therapeutic process begins with the initial call. When the prospective patient calls, I ask for a brief description of the type of problem they want help with. They may be struggling with depression, panic attacks, marital problems, procrastination, substance abuse, or a combination of problems. If the problem sounds suitable for the type of treatment I offer, I tell them that I'd love to meet with them to learn more about them and make a treatment recommendation. I explain that the type of therapy I do is a little different from what they might expect, and that they'll have to do self-help assignments between sessions throughout the therapy. I tell them that the psychotherapy homework will be crucial to the success of the treatment, and ask whether they have any concerns about this. I also answer any questions they might have about the treatment, including the fees and office hours, and explain that I'll mail them a package that includes several assessment instruments that I want them to read and fill out prior to the initial evaluation, along with some information about the treatment. The package you send can include any information or assessment instruments that seem relevant to you. Here's what I include: A welcoming letter. This letter thanks patients for deciding to see you for a consultation, and reminds them about the location and time of the first
Chapter 5
109
appointment. The letter explains a little bit about the therapy, and asks them to review the enclosed memos and bring the completed assessment instruments to their first session. The Brief Mood Survey.* This one-page instrument accurately assesses feelings of depression, suicidal urges, anxiety, anger, and relationship satisfaction. Patients can complete it in approximately one minute, and it will show you precisely how severe their symptoms are at the initial evaluation. The Concept of Self-Help memo. This memo explains that self-help assignments between sessions will be an essential part of the therapy, and briefly describes the ten most common types of homework the patient may be asked to do between sessions. For example, they may be asked to complete the Brief Mood Survey every week to track their progress, record their negative thoughts and feelings every day, schedule more rewarding activities, or analyze an upsetting interaction with a friend or family member. The memo then asks them to complete the Self-Help Contract that appears on page 110. It finishes with a list called "25 GOOD Reasons NOT to Do the Psychotherapy Homework." This list includes the best excuses patients have given me over the years for not doing psychotherapy homework between sessions, such as feeling hopeless, overwhelmed, or angry. Patients can indicate how strongly each reason maps onto their feelings, on a scale from "Not at all" to "Extremely."
* There are many assessment instruments to choose from, and your choice will depend on the nature of your clinical practice. If you're interested in learning more about the Brief Mood Survey, you can send an email to: [email protected].
Chapter 5
110
Self-Help Contract* Instructions. Use checks ( ) to indicate how you think and feel about doing self-help assignments between sessions.
Yes
No
Needs Discussion
1.
I'm aware that my therapist emphasizes a self-help program as an important key to personal growth.
2.
I'm willing to complete self-help assignments consistently between therapy sessions.
3.
How many days per week are you willing to do self-help assignments between sessions?
days
4.
How much time are you willing to spend on self-help assignments each day?
minutes
5.
How many weeks will you agree to continue doing self-help assignments between sessions?
weeks
At the end of the Concept of Self-Help memo, patients are asked once again whether they're willing to do psychotherapy homework consistently throughout the treatment, or whether they'd prefer a form of therapy that does not involve any homework assignments. The How to Make Therapy Successful and Rewarding memo. This memo informs patients that negative feelings often arise during treatment. For example, they may sometimes feel angry or mistrustful because you said something that upset them. If they discuss these feelings with you, it will often lead to a far more rewarding and productive therapeutic relationship. However, many patients drop out of therapy when this occurs, because the conflict feels uncomfortable, or because they want to punish their therapists, so they miss out on important opportunities. The memo describes some of the most common reasons for premature termination,
Chapter 5
111
such as conflict phobia, shame, excessive therapeutic niceness, or a sudden upsurge in feelings of hopelessness, and asks patients how well each reason maps onto the way they sometimes think and feel. The memo concludes by asking patients whether they'd be willing to come in for one additional session to discuss their feelings if they have the urge to drop out of therapy between sessions, or whether they'd prefer to maintain the option of simply dropping out of therapy at any time, without discussing the problem with you. The administrative memo. This memo describes basic information about how payments are handled and outlines the policy for last minute cancellations. It also reassures the patient about confidentiality, but points out that if the patient expresses any suicidal intentions, or plans to hurt another person, the therapist has the duty to protect any potential victims. This might include informing the authorities as well as any potential victims of any credible and specific threats. The therapist may also be obligated to inform the authorities if the patient discloses any ongoing abuse of a child or elderly person who's under their care. The administrative memo also explains that the therapist cannot receive gifts from patients or their families, and will not read books, letters, or other written materials patients give them between sessions. However, the therapist can review these kinds of materials with the patient during sessions, as long as they're relevant to the treatment. In addition, the therapist cannot meet with the patient outside of
* Copyright © 2004 by David D. Burns, M.D.
Chapter 5
112
therapy sessions or engage in any business dealings with the patient. If friends or family members of the patient call to inquire about the patient, the therapist will not discuss the case or even acknowledge who his or her patients are. However, if the patient requests it, the therapist can speak with other individuals, including previous therapists, to obtain information, and will share all such information with the patient. I kept packets of these documents in 9 x 12 envelopes with my return address preprinted on them. All I had to do was write the patient's address on the envelope while I was on the phone with them, and drop the package in the mail. I advised patients that they would have to fill out all the forms completely and bring them to their first session or else I would not be able to meet with them. I processed patients' responses on the Concept of Self-Help memo and the How To Make Therapy Successful and Rewarding memo at the end of the initial evaluation. I also discussed each point on the administrative memo. The way you do this will be crucial to the success of the treatment. We'll discuss this process later in the chapter. In the early days, my colleagues and I used to include a four-page pamphlet called, "Coping with Depression." This pamphlet briefly described the cognitive model and included a few simple self-help techniques that patients could start using right away. Now I recommend a book like Feeling Good, The Feeling Good Handbook, or Ten Days to Self-Esteem instead. Of course, I'm a bit biased towards these books because I wrote them, but there are lots of good self-help books to choose from. The Authoritative Guide to Self-Help Books is an
Chapter 5
113
excellent resource that rates many self-help books and lists the most popular titles for every conceivable type of emotional problem (Santrock, Minnett, & Campbell, 1994). Prescribing a good book on Cognitive Behavior Therapy (CBT) can help you in many ways. First, patients will find out if they like the cognitive model and want to be treated with this approach. Second, a book like Feeling Good will do much of the educational work and basic training for you. That way, you won't have to explain basic concepts, such as the ten cognitive distortions, or how the Daily Mood Log works, over and over to every new patient. Instead, you can focus on individualizing the treatment to each person's specific problems. Third, it's a good test of motivation. Motivated patients will usually purchase one of the books and begin to work with it. Unmotivated patients won't. Finally, you're giving the message that therapy is collaborative, and that the patient will be expected to do his or her share of the work, including self-help assignments between sessions, starting right away. Several recent controlled outcome studies have indicated that Feeling Good actually has fairly potent antidepressant effects (Scogin, Hamblin, & Beutler, 1987; Scogin, Jamison, & Davis, 1990; Scogin, Jamison, Floyd, & Chaplin, 1998; Scogin, Jamison, & Gochneaut, 1989; Smith, Floyd, Jamison, & Scogin, 1997). In fact, two-thirds of patients suffering from Major Depressive Episodes have recovered or improved substantially within four weeks of being given a copy of the book, even if they received no other treatment during that period of time, and have maintained these gains without significant relapses in
Chapter 5
114
long-term follow-up studies. So you'll be speeding your patients along the road to recovery before you've even met with them for the first visit. I'd recommend a two-hour initial appointment for history-taking, although I realize this may not be possible in some settings. Tell the patient to come at least 30 minutes early so they can fill out the Easy Diagnostic System for Axis I and Axis II in the waiting room prior to seeing you. I warn the patient that the initial evaluation may feel a bit tedious, and that I'm eager to complete it so we can get on to the actual therapy work, which is usually far more rewarding. You may want to set up the first therapy session in the same week that you do the initial evaluation, so that you can get the therapeutic process moving as quickly as possible. I fill out a structured Clinical History form during the intake evaluation. This ensures that I cover all the bases systematically. The chart on page 116 describes the information that I include in a comprehensive or brief initial evaluation. These guidelines are flexible. For example, you might not need to perform a formal mental status examination on a mildly depressed college student. In contrast, the mental status exam could be crucial in your evaluation of a psychotic or confused patient in an emergency room setting. Personal Information The first section of my Clinical History form includes information such as: 1.
Name, address, home, work and cell phone numbers, email, and fax
2.
Living situation i)
Marital status
Chapter 5
115
ii)
Type of home
iii)
Who lives there
iv)
Number, names and ages of children
3.
Education
4.
Type of work
5.
6.
i)
Income
ii)
Length of employment
iii)
Satisfaction / problems at work
Payment arrangements i)
Who will pay?
ii)
Insurance / disability status
Religious preference Although this information might sound unimportant or dull, it's often very
relevant to the treatment. For example, in the early days of my practice, some patients asked me to bill a third party, such as their parents. Over the years, I learned that these arrangements often led to problems. Instead, I told patients that I was working for them, and not their parents. If their parents wanted to pay, that was fine with me, but their parents had to pay them, and they had to pay me at each session. This made it clear that I was working for them, and that they were accountable to me as well.
Chapter 5
116
Types of Clinical Histories Comprehensive History
Type of Information
Brief History
Basic Data Personal Information Emergency Contact Information
Reason for Seeking Treatment Initial Symptom Screening Referral Source Current Problems Motivation for Treatment
Treatment History History of Previous Psychotherapy Current Medications Past Medication Survey
Personal History Family History of Psychiatric Problems Childhood History Relationship Assessment Sexual History History of Abuse or Trauma Other Information Quality of Information Patient's Goals for Therapy
Diagnostic Assessment Mental Status Exam
Optional
Optional
Axis I and II Diagnostic Screening
Optional
Axis III: Medical Problems
Optional
Axis IV: Stressful Events
Optional
Optional
Axis V: Global Assessment of Functioning
Optional
Optional
Preparation for Treatment Administrative Checklist Initial Formulation and Treatment Plan
Optional
Optional
Chapter 5
117
In contrast, if a third party is paying for the therapy, the power dynamic shifts in a subtle way. Now the contract is between you and someone the patient may be in conflict with. This can set up lots of problems. If negative feelings develop, neither the patient nor the person who's paying the bill may feel responsible for the bill, and you may be left with several months of therapy that you cannot collect for. It may sound overly mercenary to be so focused on financial matters. However, the fee is a part of the treatment, and financial issues often arouse strong feelings, so you'll need to deal with the payment arrangements in a responsible way at the beginning of the treatment. Furthermore, the way patients approach financial arrangements will sometimes tell you important things about how they approach other people, and life in general. Over the years, I learned to require payment at each session. If you don't do this, some patients may slip behind in payments and act out their negative feelings indirectly, by refusing or "forgetting" to pay their monthly bill. In contrast, if you require payment at the start of each session, you'll know immediately if a problem has developed, and you can nip it in the bud before it gets out of hand. This empowers you to be honest and direct with the patient. If you have to confront a patient about something unpleasant, you'll feel free to do so. You won't have to act overly "nice" to make sure you get paid each month! I also never agreed to bill insurance companies. I told patients that if there was any paperwork they needed me to fill out, I'd be happy to fill it out for them, but it was their job to mail in the forms and collect the reimbursement from the
Chapter 5
118
insurance company. I advised them to call their insurance company to find out how much they'd be reimbursed for each session. This was because most patients had the fantasy that their medical insurance would cover the lion's share of the treatment. In fact, the reimbursement was often far less than patients expected. For example, patients often told me that their policy covered 80% of the cost of psychotherapy. But when they called to confirm this, they sometimes discovered that the insurance only paid 80% of a fee of $25 per hour, or $20 per session! That was another reason why I refused to bill insurance companies directly for the treatment. Finally, I wanted to find out if they could comfortably afford the treatment. If patients were paying out of pocket, I asked how many sessions they anticipated seeing me for. Some patients have unrealistic expectations. For example, they might budget $500 for the entire course of therapy, based on the assumption that the treatment would only require five sessions at $100 per hour, or something along those lines. I never agreed to this type of arrangement, since I didn't want to be under that kind of pressure. At my clinic in Philadelphia, I usually had several clinical psychology graduate students and psychiatric residents working as trainees. This allowed us to offer a sliding fee scale so we could accommodate people with limited resources. The top fee in our clinic was $150 per session, but some patients were seen for as little as $5 per session. Our research indicated that the novice therapists were often as effective as the most senior therapists, so this was a
Chapter 5
119
good deal for our patients. It was also good for us, since the graduate students and residents had the chance to work with real people with real problems. Emergency Contact Information Next, I ask the patient for the name and phone number of a friend or family member I can contact in case of an emergency. I also ask for the names and phone numbers of other medical or mental health professionals they're working with, and record this information on the form. This information can be tremendously important. For example, patients with Borderline Personality Disorder can be manipulative and oppositional. It's not unusual for them to skip appointments when they're feeling angry or depressed, or to make subtle or obvious suicide threats and then refuse to answer the phone. This puts you in a tremendously awkward position, because you have no way to contact the patient to find out what's going on. That's why you need the phone number of someone else you can call in the event of an emergency. This prevents the patient from having a certain kind of leverage over you. Many patients with Borderline Personality Disorder refuse to provide this information at the initial assessment. They come up with all kinds of excuses, claiming the need for confidentiality or whatever. I learned to respond along these lines: "I need this information, or I can't ethically accept you as my patient. If you're not comfortable with any of these arrangements, it might be better for you to find another therapist whose approach would be more consistent with your expectations." This may sound harsh, but will protect you from enormous stress and heartbreak later on if you're faced with a crisis and
Chapter 5
120
absolutely have to contact the patient or intervene to save the patient's life. The therapy has to be set up in a way that protects the patient and the therapist alike. You have to be able to go home at night and feel relaxed, knowing that your patients are safe. If you're constantly anxious and stressed by a manipulative patient, the work you do with that patient probably won't be very therapeutic. It's common knowledge that well-meaning family members often enable patients to maintain destructive behavior patterns, but well-meaning therapists will often fall into the same trap because of the fear that the patient will get upset if you try to set any limits. But in fact, you'll encounter many more problems if you fail to establish reasonable limits up front. Initial Symptom Screening Next, I review the scores on the Brief Mood Survey that I mailed to the patient before the intake evaluation. You may recall that this instrument assesses: Depression Suicidal Urges Anxiety Anger Relationship Satisfaction You'll see exactly how severe these symptoms are, and how satisfied or dissatisfied the patient feels in a close personal relationship. The suicidescreening test asks about suicidal thoughts as well as suicidal plans and urges. Suicidal thoughts are common, and they're not generally dangerous. However,
Chapter 5
121
any suicidal urges need to be explored right away. If the patient is feeling actively suicidal, and there's no credible deterrent, then immediate hospitalization may be indicated. Referral Source Next, I ask questions like these: Who referred you to me, and why? Why are you seeking treatment right now? The goal is not simply to get this information, but to read between the lines. Is the patient coming to see you because she or he wants help, or because of external coercion? This information will be relevant to your understanding of the patient's motivation. Current Problems This portion of the Clinical History focuses on the patient's primary problem or complaint. This is the patient's opportunity to tell you his or her story and explain why they're coming for therapy. Try to conceptualize the type of problem the patient needs help with. It might be an individual mood problem, like depression or anxiety, a marital conflict, a bad habit like procrastination, an addiction such as alcohol or drug abuse, or an eating disorder. If the patient is depressed or anxious, ask for specific examples. Can they describe a moment when they were feeling upset? What was going on? How were they feeling? What were they thinking? Ask about previous episodes as well. If they're feeling depressed, is this their first episode of depression? How many episodes of depression have they
Chapter 5
122
experienced in the past? How long have they been feeling depressed this time? Did the depression come on suddenly or gradually? Is there anything that seems to make the symptoms better or worse? If they're having problems in their relationships with other people, ask for some specific examples of the problem. What does the other person say to them? What do they say next? What are they thinking, and how do they feel, during these conflicts? What's the theme of these problems? Are they sensitive to criticism? Do they feel victimized by other people? Do other people always seem to use them or let them down? Do they feel lonely or rejected? Does the same type of relationship problem happen over and over again with lots of different people? You can ask about other kinds of stressful events as well. Has the patient experienced a loss or career reversal? Are they having problems at work? Health problems? Are they having trouble making an important personal decision, like whether or not to get married? If the patient becomes emotional during the history, it's usually a good thing. Tears can be the patient's way of showing vulnerability and asking for help. If you sense the patient is close to tears, encourage him or her to let the feelings out. Once the patient begins to cry, I tell them to try to notice what they're thinking and feeling. What thoughts and images cross their minds? This information will often provide important clues about what's bothering them the most. Empathy will be vitally important. Try to see the world through the patient's
Chapter 5
123
eyes, find truth in what the patient is saying, and acknowledge the patient's feelings. It's usually not a good idea to attempt any type of problem-solving or therapeutic interventions while you're taking the history. The patient needs to have the chance to talk and feel accepted. Finally, ask if they're looking for a solution to the problems they've described, or whether they simply want to talk and get their feelings off their chest while you listen. Ask what a solution to the problem would look like. How would their life be different if the therapy were tremendously helpful? How would they be thinking, feeling, and behaving? And how hard would they be willing to work to bring that solution about? Motivation for Treatment When the patient describes the problem that brought them to therapy, try to detect any hidden agendas that may sabotage the treatment later on. For example, the patient may have problems with alcohol abuse, but you may discover that he's only there because of pressure from his wife or boss. In addition, even if he wants to be there, he may feel ambivalent about change. Although alcohol may be causing all kinds of problems for him, such as depression, violence, missed work, or a DUI, he probably enjoys drinking, and it may be his only real source of happiness and relaxation. To find out where he stands, you might say something like this: "Ned, I think it's great that you want to quit drinking, but I can imagine that you might have mixed feelings about giving it up. Let's look at the other side of the coin, and talk about all the reasons you might not want to stop drinking."
Chapter 5
124
In addition, you can ask him what he'd be willing to bring to the table if you agreed to work with him. For example, would he agree to do regular psychotherapy homework with the Daily Mood Log? Would he agree to go to AA meetings regularly, assuming you felt this was indicated? These types of questions will help you focus on motivational issues right away. Remember that you don't have to try to persuade the patient to work with you. Instead, the patient has to persuade you to work with him or her. This represents an important shift from the way most therapists work, and may be difficult to grasp at first. We'll discuss this idea throughout the book. History of Previous Psychotherapy Next, I ask about the dates of any previous treatments, including hospitalizations, as well as the name of each therapist the patient has worked with. I also ask about the kinds of problems the patient sought help for, the type of therapy they received, and the helpfulness of the treatment. At my clinic in Philadelphia, many of our patients had undergone as many as 8 – 12 unsuccessful courses of therapy before seeking treatment with us. Patients with many unsuccessful treatment experiences will often be more challenging than patients who've never sought treatment before, because they may feel hopeless and may have given up. Sometimes, they're afraid to try again for fear of yet another disappointment. Asking what went wrong can tip you off about problems you may run into if you're not careful. A mildly depressed, angry physician with Borderline Personality Disorder told me that she'd had to fire her three previous therapists because they'd
Chapter 5
125
wrongly and foolishly implied that she might be contributing to the problems in her marriage. She explained that her husband was a self-centered jerk who was entirely to blame for the problems in their relationship. She expressed these ideas in a sharp, defensive tone of voice that tipped me off about an ocean of narcissism and hostility that would sabotage the therapy if I wasn't extremely careful in my interactions with her. Recording the patient's experiences with previous therapists at the initial evaluation may seem tedious, but it's a necessary part of responsible historytaking. I sometimes get restless and wish we could get on to the actual treatment, which is far more enjoyable. I wish I knew a way around this problem, but I don't. Of course, you can skip some or all of the history, and most therapists do, but it's risky because you may get burned and regret it later on. Unfortunately, asking patients to fill out this type of information on their own on a history form is not a solution. Skillful history-taking has to be an interactive process, because the patient's answers to each question will prompt you to ask additional questions that relate to what they just told you. In addition, reviewing a form that the patient filled out can be even more time-consuming and frustrating than simply asking them the questions and writing down what they tell you. Current Medications The next section of my Clinical History form contains a chart for recording all the patient's current medications, doses, and side effects. You should list psychiatric and non-psychiatric medications as well. This information will be
Chapter 5
126
absolutely relevant to any psychiatrist who's prescribing drugs, but a non-medical therapist should also be aware of any medications the patient is taking. Feeling Good and The Feeling Good Handbook (1999 revised versions) contain detailed consumer's guides to psychiatric medications. You and the patient can look up any drugs the patient is taking and learn about the doses and side effects, as well as any drug interactions the patient should be aware of. These books also contain considerable information about responsible and irresponsible ways to prescribe psychiatric medications. Of course, if you look online, you'll find numerous websites containing updated information about medications and their side effects as well. Past Medication Survey Record any previous psychiatric drugs the patient has taken, including the dates, doses, side effects, and therapeutic effects. This information will be especially relevant to prescribing physicians, because your choice of drugs will be influenced by patients' reactions to the medications they've taken in the past. For example, if the patient had an outstanding response to a particular antidepressant in the past, the same medication might be a good choice for the patient now. Family History of Psychiatric Problems Next, I ask about any psychiatric problems that seem to run in the family. Have any relatives experienced problems with anxiety, depression, mania, or schizophrenia? How about drug or alcohol abuse? Mental retardation? Criminal or antisocial behavior?
Chapter 5
127
Your job is not to sort out genetic from environmental influences. That's obviously a job for researchers. In addition, patients' perceptions of the nature or severity of the relative's problems may not be accurate. Your job is simply to list the person's relationship to the patient (e.g., parent, grandparent, sibling, etc.) and the type of problem they experienced. Childhood History You can ask questions like these: What was your father like? How would you describe your relationship with him? What was your mother like? How would you describe your relationship with her? What kind of relationship did your parents have? Were they loving and supportive? Did they fight a lot? How did they treat you? What were your brothers and sisters like? How would you describe your relationships with them? Do you think any of your current problems were influenced by your experiences when you were growing up? In what way? Did you have many friends when you were growing up? How would you describe your relationships with other kids? How did you do in school? Did you have any problems with your schoolwork, with the authorities, or with other children? Were you a happy child? Did you have any problems with depression, anxiety, anger, antisocial behavior, or substance abuse?
Chapter 5
128
Were there other important experiences you had when you were growing up that you'd like me to know about? Once again, we're not trying to make causal inferences about childhood experiences that may be contributing to the problems the patient is experiencing now, because that kind of information is not yet known, even to researchers. However, patients' perceptions clearly have a huge influence on the way they feel and behave, including their perceptions of the experiences they had when they were growing up. Relationship Assessment Ask the patient to describe his or her closest relationship. Are there any problems in the relationship? Has the patient experienced similar problems in other relationships in the past? How are the patient's relationships with friends, family, and colleagues? Does the patient get along well with people? Are there any problems in his or her relationships with others? Sexual History The best time to take a sexual history is at the initial evaluation. Therapists may feel inhibited or awkward about asking direct, personal questions about a patient's sexual fantasies, experiences or problems. But patients expect these kinds of questions from therapists, and it will be easier to have this discussion at the intake evaluation. Ask about the patient's sexual orientation and current sexual partners. Has the patient ever had any problems or difficulties with sex, such as difficulties
Chapter 5
129
getting aroused or having orgasms? Has the patient ever engaged in sexual practices or fantasies that were troublesome or upsetting to them? My Clinical History form makes the sexual history a bit easier because it lists all the questions you need to ask each new patient. That way, you won't avoid or tiptoe around any questions that seem overly intrusive or embarrassing. History of Abuse or Trauma Ask if the patient has ever witnessed any traumatic events such as rape, murder, or violence. Ask if the patient has ever been abused, sexually, physically, or psychologically. Was the patient ever raped or beaten up? If so, what are the patient's thoughts and feelings about that experience? Do the memories of the event create problems for the patient now? What kinds of problems? Has the patient ever abused anyone else, including rape, violence, or murder? Who was it? How does the patient feel about these experiences now? Other Information Ask the patient if you've covered all the relevant areas and problems, or if there are other things you should be aware of. Does the patient have any emotional or behavioral difficulties you didn't cover, such as loneliness, marital conflict, substance abuse, procrastination, or other work or legal problems that she or he did not mention? Ask if there's anything that the patient might have difficulty telling you, due to feelings of shame. Ask if the patient felt that she or he could be completely candid and open with you during the interview. Quality of Information
Chapter 5
130
Did the patient seem reliable, honest and open with you? Was she or he vague or evasive at times? Did the patient seem to be intoxicated or confused? Did you have the impression that the patient was just telling you what you wanted to hear? Try to be alert to hidden agendas or other pressures that could influence the reliability of the information you obtained. Several things could be red flags here. Some patients will be vague or evasive when you ask about sensitive topics such as suicidal impulses, violent impulses, or substance abuse. Was the patient referred by someone else, such as a family member, employer, or the judicial system? Is the patient trying to get addictive substances, such as painkillers, sleeping pills, or benzodiazepines? Is the patient involved in a lawsuit or disability claim? Patient's Goals for Therapy At this point in the history, I say something like this: "If we had a magic wand, and you knew that all your problems could be solved, what would you put on your wish list? What would you like to accomplish in therapy? If we were completely successful, how would we know? How would your life be different?" Most patients will describe a number of goals, such as: I'd get over my depression. I'd develop better self-esteem. I'd lose weight. I'd look for a better job. I'd overcome my shyness and public speaking anxiety.
Chapter 5
131
My wife and I wouldn't argue so much. I usually tell patients that these all sound like excellent goals. I list the goals in the chart and ask patients what it would be worth to them if we could achieve them. If I agreed to help them solve these problems, how long would they be willing to work on them? And how hard would they be willing to work? For example, would they do psychotherapy homework consistently? If one of the goals involves overcoming anxiety, I'd ask if they'd be willing to use Exposure Techniques, even if the exposure was anxiety-provoking at first. The motivational questions you ask will depend on the patient's goals for treatment. I also ask how they imagine therapy works. For example, the patient may want to overcome depression, shyness, or panic attacks, or develop a more loving marriage. What do they believe happens in therapy to bring these results about? Patients who have trouble coming up with any meaningful or specific goals probably have mixed feelings about being in therapy, or they may be confused by your question and feel put on the spot. You can sometimes prime the pump by summarizing the problems they've described and transforming them into goals. For example, you could say: "Karl, you told me that you've felt depressed and inferior ever since you were a child. Certainly, I can't tell you what to aim for in therapy, but one goal might be to overcome the depression, and another might be to develop better self-esteem, so that you no longer felt inferior to other people. Would this make sense?
Chapter 5
132 "You've also mentioned that you feel lonely and don't have any
close friends. That might be another goal we could work on—improving your relationships with people. But these are just suggestions. The goals can be anything as long as they're realistic and meaningful to you, and you're willing to work hard to achieve them." Alternatively, you can point out that the patient doesn't seem to have any goals for therapy, and express your confusion about this. Why is it that they don't have any goals for therapy? Why are they coming to see you? Ask if they have mixed feelings about being in treatment, or if someone else is pressuring them to be there. The questions in this section are designed not only to focus the therapy on something specific and real, but also to assess the patient's suitability for treatment, educate the patient about how therapy works, and make the patient accountable. If patients have no goals or don't seem motivated to work hard to overcome the problems that brought them to therapy, they may not be good candidates for CBT. You may save yourself a lot of frustration later on if you bring these issues out into the open at the intake evaluation, when you and the patient are both deciding whether or not working together would be indicated. Mental Status Exam When I was a resident, I evaluated lots of extremely disturbed individuals in our psychiatric emergency room. In that setting, there was a strong emphasis on the Mental Status Exam. Once I developed my outpatient clinical practice, it rarely seemed relevant, so I didn't routinely include it in my intake evaluation.
Chapter 5
133
The Mental Status Exam consists of your observations of the patient's appearance, speech, feelings and behavior, and includes some specialized tests of mental functioning as well. Look for gross, obvious abnormalities and patterns that may suggest the presence of: Mood problems. Does the patient seem depressed, anxious, or angry? Psychosis. Does the patient seem to be suffering from schizophrenia, mania, or psychosis secondary to drugs or medications? Brain damage. Does the patient appear to be suffering from an organic brain impairment, such as Alzheimer's disease, encephalitis, or drug intoxication or withdrawal? If the findings are confusing, you can refer the patient for more refined neuropsychological testing or for a neurological evaluation. A formal Mental Status Exam includes information about the patient's appearance, behavior, affect, and speech patterns, as well as an assessment of psychotic thought processes, other unusual experiences the patient may have had, and cognitive functioning: 1. Appearance Describe any features that may reflect emotional state. Does the patient look neat and well-dressed? Disheveled? 2. Behavior Describe the patient's behavior, speech and body language. Is the patient hyperactive and constantly moving about, with pressured speech, suggesting mania? Is the patient agitated, suggesting extreme anxiety or depression? Is the
Chapter 5
134
patient quiet and withdrawn? Friendly and warm? Hostile and defensive? Are the patient's arms folded defiantly across his or her chest? Look for abnormal body movements, such as lip smacking, tremors, or hand wringing. 3. Affect Does the patient seem to be happy? Sad? Anxious? Angry? Suspicious? Histrionic? Is the patient's affect consistent with what he or she is saying? A flat and drab affect, with no emotional color, may suggest schizophrenia. 4. Speech patterns Patients with schizophrenia often speak in word salad, which is defined as, "an incomprehensible mixing of meaningless words and phrases" (Talbott, Hales, & Yudofsky, 1988, p. 89). Their speech may include neologisms, which are words that the patient makes up, or clang associations, where the patient speaks nonsensically, using constant rhyming and punning. Echolalia refers to the patient's "irrelevant parroting of what another person has said" (Talbott et al., 1988). Look for circumstantial, tangential, distractible, or pressured speech. Patients with mania may have circumstantial speech. If you ask a question, they jump from subject to subject, expanding on each topic in great detail, but eventually come back to the original topic. In contrast, patients with schizophrenia often have tangential speech. They also jump from topic to topic, but never return to the original question. The pacing of the speech is also important. Manic patients speak rapidly, in an excited, non-stop fashion, and they're easily distractible. Thought blockage
Chapter 5
135
means that the patient stops talking halfway through a sentence and cannot complete the thought. Patients with alcoholic brain damage may confabulate. I once treated a hospitalized alcoholic man with a massively enlarged abdomen due to liver failure. He'd been bedridden for months. During the Mental Status Exam, I asked if he'd attended the party at the mayor's house the previous evening. He excitedly described partying with the mayor, without any awareness that he was making it all up. 5. Psychotic thought processes. Patients suffering from schizophrenia usually exhibit the so-called Shneiderian "first-rank" symptoms. They may hear voices coming from outside their heads or believe that secret electrical forces or devices are controlling them. They may believe that others can read their minds, or that their private thoughts are being broadcast out loud so that everyone can hear them. They may believe that others can control their minds, or insert thoughts into their brains. They may think that they receive special messages from television or radio broadcasts. Although these symptoms are most often associated with schizophrenia, you will have to rule out other possible causes of psychosis such as severe mania or psychosis secondary to drug intoxication or withdrawal. Visual hallucinations can also be observed in schizophrenia, but are more commonly associated with organic brain syndromes, such as drug intoxication or alcohol withdrawal. Other psychotic processes include: Paranoia. Patients with paranoid schizophrenia often believe that others are
Chapter 5
136
plotting against them. A schizophrenic patient once accused me of kidnapping her dog to force her to marry me. She was also convinced that I was involved in a conspiracy with the local police, and that we'd hidden television cameras in her bedroom so we could spy on her and watch her having sex. Delusions. Delusions are bizarre, fixed beliefs that aren't affected by other people's perceptions of reality. Patients may have grandiose delusions that they receive special messages from God or have special powers to save mankind. These delusions are often associated with schizophrenia, but can be seen in other conditions such as drug intoxication, bipolar disorder or psychotic depression. A schizophrenic man named Albert was convinced that my receptionist, Lucretia, could read his mind and knew exactly what he was thinking and saying during our sessions. I suggested we might test this belief by putting five $20 bills on my desk, and instructed Albert to concentrate on them intensely so Lucretia would know they were there. I told him that if she knocked on the door, I'd give her the money. I told him that she really needed the money, and would definitely knock on the door if she could read his mind. Albert agreed to the test. He concentrated on the $20 bills for several minutes, but fortunately, Lucretia didn't knock on the door. I asked Albert what he concluded. He said, "Oh, she's very sneaky. She doesn't want us to know that she can read my mind. This proves that I was right about her." Proverbs. Ask the patient to interpret the meaning of two or three simple
Chapter 5
137
proverbs, such as "A stitch in time saves nine," "Look before you leap," "A bird in the hand is worth two in the bush," or "People in glass houses shouldn't throw stones." You may have to explain that each proverb has a meaning, or contains a kind of wisdom, and you want the patient to tell you what the meaning is. Patients with schizophrenia nearly always interpret proverbs concretely, and cannot seem to comprehend the abstract meaning. They typically say things like this: "A stitch in time means that if you're stitching some clothing, then you should try to do your stitching in time, so you can save nine." Or, "If you live in a house made of glass, and you throw a stone through the window, the glass might break." Or, "Look before you leap means you should look and see where you're jumping before you leap." Sometimes, a floridly schizophrenic patient will respond with bizarre interpretations. For example: "Birds fly—one bird flies, two birds fly—fly away birdy—chirp, chirp" (Talbott et al., 1988). 6. Other unusual experiences Ask patients if they've had other unusual experiences that normal people might not understand, such as seeing things that aren't there, or feeling like they're unreal or the world is unreal. Have they ever had any blackouts, or the experience of not knowing where they were or what they'd been doing for prolonged periods of time? This information could tip you off to the existence of a dissociative disorder. 7. Cognitive functioning Tests of cognitive functioning are important in the evaluation of confused
Chapter 5
138
elderly individuals, or patients who might have an organic brain problem, such as encephalitis or delirium. Cognitive functions are not usually impaired in patients with psychotic conditions, such as schizophrenia. Here are a few simple tests you can use: Orientation to person, place and time. Ask the patient questions like this: Do you know what year it is? What's today's date? What day of the week is it? What city are we in? Where are you right now? What's your name? Patients with organic brain damage, such as Alzheimer's disease, may not be able to answer these questions. Insight. Ask the patient: Why are you here? What are we doing right now? A woman with Alzheimer's disease appeared in one of my CBT groups at the Stanford Hospital. She was from the geropsychiatric unit. She thought it was her high school reunion, and was convinced that she and I were old friends who had gone to high school together. Immediate memory. Tell the patient you are going to give him or her three things to remember, such as a number, a color, and an object (e.g., 37, yellow, telephone), and that you'll ask what they were in a few minutes. A few minutes later, ask the patient what the three things were. You can also ask the patient to repeat a string of digits. Start with three digits, such as "4, 9, 2." Then try four digits, five digits, and six digits, until the patient makes an error. You can then repeat the procedure, asking the patient to repeat the numbers backwards. Patients with dementia or other forms of brain damage may have difficulties with this task. Of course, performance on this task will be
Chapter 5
139
influenced by IQ, and possibly by mood as well. For example, an agitated, anxious or severely depressed patient may perform poorly due to impaired concentration. An angry, uncooperative patient may refuse to try or may attempt to thwart you. Recent memory. Can the patient recall what she or he was doing a few days earlier? What she or he read in the newspaper yesterday? The name of the President of the United States? The Vice President? Past memory. Can the patient recall where she or he was born? What his or her first job was? Who the last President of the United States was? Counting backwards from 100 by 7s. Tell the patient to start with 100, and count backwards by 7s, like this: 100, 93, 86, 79, 72, 65, etc. Patients with organic brain damage may have difficulty with this task. Bender Gestalt cards. If you suspect brain impairment, you can ask the patient to copy a set of patterns from the Bender Gestalt cards. The patterns are composed of basic shapes such as rectangles, circles, and triangles. This test takes about 15 minutes. Patients with organic brain damage usually have significant difficulties copying the patterns correctly. The interpretation of the test is simple and depends on the number of errors the patient makes. Axis I and II Diagnostic Screening My Clinical History form includes a diagnostic summary sheet that lists more than 40 common Axis I disorders as well as all 10 Axis II disorders, along with their DSM-IV codes. Response options include "No," "Possible," or "Yes." All the diagnoses are "No" by default, unless I put a check mark in the "Possible" or
Chapter 5
140
"Yes" diagnostic columns. You can assign diagnoses with a systematic interview technique, asking the patient a few screening questions for each category of symptoms. If the patient says "yes" or "maybe" on the screening questions, you can zero in on specific diagnoses within that category. For example, here are some reasonable screening questions for alcohol or drug abuse: How many days per week do you drink at least some alcohol or use a recreational drug? How much do you drink? What are the drugs that you use most frequently? Have you ever used drugs or alcohol in the past? Do you feel that drug or alcohol abuse has ever been a problem for you? Do you take pain pills, sleeping pills, or minor tranquilizers like Xanax or Valium? How many per day? Has anyone else, such as a doctor, friend, or family member, ever suggested that you had a drug or alcohol problem? These are not definitive diagnostic questions, but simply probes. If you get a clear-cut no on all the questions, and the patient seems reliable, you can move on to the screening questions for the next diagnostic category. In contrast, if you get a yes, or suspect that the patient is minimizing their symptoms, such as the extent of their substance abuse, you can ask additional questions that focus on the DSM-IV criteria for substance abuse or dependence. For example, if the patient tells you he drinks, ask him what he drinks, how often he drinks, how many drinks he has each day, and how large each drink is.
Chapter 5
141
For example, a patient told me that he typically had just one drink each evening before dinner, and occasionally a second drink for dessert. When I asked him to describe his drinks, he said that he usually filled up a 12-ounce glass with vodka and added a couple ice cubes. Most experts suggest that you can double the patient's estimate and come close to the actual amount of alcohol consumed. One difficulty with the interview method is that it can be time-consuming, particularly if you try to do a reasonably comprehensive and accurate job. Alternatively, you may want to try one of the self-assessment diagnostic systems, like the Easy Diagnostic System described in Chapter 4. This approach is more systematic and comprehensive. It's also extremely quick and easy for the therapist. Remember, however, that you can never rely on a test to do your thinking for you, and that your own clinical judgment will always be the gold standard for assigning any diagnoses. Axis III: Medical Problems Ask about any current illnesses, as well as any symptoms that might require medical attention, such as fever, pain, or unexplained weight loss, and write a brief description on your history form. If you're concerned about an undiagnosed medical problem that might contribute to the patient's psychiatric symptoms, you can explain your thinking and suggest an evaluation by the patient's medical doctor, or contact the patient's doctor directly. For example, I once evaluated a depressed man who'd experienced substantial recent weight loss. He was concerned that he might have a malignancy. I was suspicious and referred him to the internal medicine clinic at
Chapter 5
142
our hospital. He was quickly diagnosed with kidney cancer and scheduled for immediate surgery. However, I would have to say that this case represents the exception, rather than the rule. In my entire career, I saw only a handful of patients with undiagnosed medical problems that might have contributed to their psychiatric complaints. Axis IV: Stressful Events Ask about any stressful events that may affect the diagnosis, treatment or prognosis. Try to evaluate the severity of the problem as well as how the patient is reacting. For example, an individual may fail to react to the loss of a loved one, even though you might judge this to be very stressful. In contrast, a perfectionistic patient might feel devastated after receiving a B on an examination, even though you might judge this event to be only mildly stressful. Write a brief description of the nature of the stress, as well as the patient’s response, for any yes answers on the chart on page 143. Axis V: Global Assessment of Functioning (GAF) I'm not a big fan of the DSM-IV GAF scale because it's not really a continuum, as claimed by the authors. One of the many problems is that the GAF includes a qualitative description of heterogeneous types of symptoms or behaviors (such as flat affect, suicidal ideation, or theft) with a quasi-quantitative assessment of the patient's level of functioning (such as "good functioning in all areas.") As a result, you're mixing apples and oranges.
Chapter 5
143
Stressful Events
Check ( ) if yes
1. Family problems: divorce, death, abuse, or conflicts with family members 2. Relationship problems: living alone, conflicts with friends 3. Educational problems: illiteracy, academic or peer problems 4. Work problems: job loss, conflicts with boss or coworkers 5. Housing problems: homelessness, unsafe neighborhood 6. Economic problems: extreme poverty, insufficient welfare support, bankruptcy 7. Health care problems: inadequate insurance, poor access to health care 8. Legal problems: arrest, litigation, victim of crime 9. Other social or environmental problems: disasters, war, etc.
Here's another problem: "inadequate information" is rated as a 0—worse than actively homicidal or catatonic—whereas it should be treated as missing data. I doubt the GAF has been subjected to a great deal of psychometric assessment, and I'd be shocked if its reliability or validity ratings were high. Of course, you can obtain inter-rater reliability by creating strict rules, and training two therapists to apply those rules in the exact same way when they assign the GAF, but this process does not create true validity, since the rules may be rigid or arbitrary. In other words, you may sacrifice validity in the push to obtain interrater reliability. Still, we're obligated to assign GAF ratings at intake and discharge. As a compromise, I've attempted to transform the GAF into a more meaningful, userfriendly, and continuous measure, while still mapping onto the DSM-IV GAF scale reasonably well. My version of the GAF appears on page 144. You'll see that my current version leaves a lot to be desired, and if it didn't have to map onto
Chapter 5
144
DSM-IV, it could be improved much further. For example, a depressed lawyer who's feeling actively suicidal may still exhibit "superior functioning in a wide range of activities." Should we give him a 95, or a 5, on the GAF? He'd qualify for both ratings! After you assign a number between 0 and 100 that reflects your best assessment of the patient's level of functioning, you can write a brief description of any impairments you've observed.
Assessment of Overall Functioning
Circle One
Superior functioning in a wide range of activities
91-100
Absent or minimal symptoms, with good functioning in all areas
81-90
Transient symptoms, with only slight impairment in work or social functioning
71-80
Mild symptoms or impairment in functioning
61-70
Moderate symptoms or impairment in functioning (few friends, significant conflicts with peers or coworkers)
51-60
Serious symptoms (suicidal ideas, severe obsessional rituals) or impairment in functioning (no friends, unable to keep a job)
41-50
Some impairment in reality testing or communication (speech illogical) or major impairment in functioning, judgment, thinking, or mood (e.g., a depressed man who avoids friends, neglects family, and is unable to work)
31-40
Behavior considerably influenced by delusions or inability to function in almost all areas (e.g., stays in bed all day) with serious impairments in communication (sometimes incoherent) or judgment (grossly inappropriate)
21-30
Some danger of hurting self or others (suicide attempts; frequently violent; manic excitement), failure in hygiene (e.g., smears feces), or gross incapacity to communicate (e.g., largely incoherent or mute)
11-20
Persistent danger of severely hurting self or others
0-10
Inadequate information
Administrative Checklist At the end of my Clinical History form, I include a checklist of
Missing data
Chapter 5
145
administrative topics I review with the patient. This will save you a great deal of frustration later on. Therapists often have the fantasy that patients will understand and respect the rules of the therapy, and are sometimes phobic about reviewing them with the patient. Furthermore, when you first meet the patient, you may both be in a honeymoon phase and fantasize that nothing could go wrong. But this is rarely the case. It's best to discuss the administrative issues at the intake evaluation, before any problems have developed. After I review each topic, I check it off on the Clinical History form. This guarantees that I'll cover all the bases as quickly and efficiently as possible. You may consider the following list overly time-consuming or anxietyprovoking. You may be reluctant to discuss some of these issues with patients, fearing they'll get upset and not want to work with you. I'd encourage you to review all of these topics with every new patient in spite of this, because they'll be vital to the success of the therapy. If you skip them, you may be asking for trouble. You'll notice that we discussed some of these administrative issues earlier in the chapter. This section will provide you with tips about how to review them with new patients in the most effective manner. I'll also be referring to some of the tools I described earlier. You may want to develop some similar tools that are specifically geared to your practice. If you want to obtain copies of the tools I've developed, feel free to send an email to: [email protected]. The Concept of Self-Help memo (page 109). Did the patient read it and fill it out completely? Did they check off "Needs Discussion" on any of the items
Chapter 5
146
on the Self-Help Contract? I review the patient's responses, and ask how they feel about doing psychotherapy homework between sessions. If they protest or seem reluctant to do homework, I offer to give them a list of therapists in the community who do not require homework so they can work with a therapist whose approach is more consistent with their expectations. At the same time, I emphasize my eagerness to work with them, but let them know that the homework issue is absolutely not negotiable, and that if they have the slightest doubts about it, it would be better for them to work with someone else. Surprisingly, very few patients ever take me up on this offer. When I offer to refer them to someone else, they suddenly discover that they are willing to do the psychotherapy homework, and that I'm the therapist they want to work with. This is the only method I've ever found that's been consistently effective in motivating patients to do psychotherapy homework. The How to Make Therapy Successful and Rewarding memo (page 110). You may recall that this memo asks patients if they'll agree to come in for one additional session if they get upset and decide to drop out of therapy between sessions. Did the patient read this memo and fill it out completely? If their responses indicate that they want the privilege of dropping out of treatment without notice, I explain that I don't offer that type of arrangement. I also explain that I wouldn't suddenly decide to stop working with them between sessions without meeting with them face-to-face to explain my reasons, and that I'd hope they'd extend the same courtesy to
Chapter 5
147
me. However, I can offer to refer them to someone else if they'd prefer to have the right to drop out of therapy at any time they want without discussing their reasons with their therapist. Once again, nearly all patients suddenly discover that they're very willing to agree to this. I recently reviewed the world literature on premature termination with one of my students. We discovered that in nearly all treatment settings, including research studies as well as clinical practice, the dropout rates are high, ranging from 25% to more than 85%. Most therapists simply ignore this problem, hoping for the best. The How to Make Therapy Successful and Rewarding memo is not a perfect solution, since some patients will drop out no matter what they agreed to. However, I've had many patients who did decide to drop out, but then decided to come in and talk with me instead because they remembered our discussion about premature termination. Sometimes, they'd decided to drop out because they were feeling better and thought they didn't need any more treatment. In those cases, we reviewed the progress they'd made, pinpointed the techniques or concepts that had been the most helpful to them, and did the Relapse Prevention Training that you'll learn about in Chapter 32. I also let them know that relapse was not unusual, and that I'd be happy to see them again in the future if they ever needed additional treatment. Other patients had decided to drop out because of negative feelings about something I'd done or said in the previous therapy session. In nearly
Chapter 5
148
all cases, these discussions led to immediate improvements in the quality of the therapeutic alliance. Legal problems. You can ask about any legal issues, including a lawsuit or disability claim, that may cause a conflict of interest. A referral to a forensic psychiatrist or psychologist may be indicated. When in doubt, check with your forensic consultant so you don't get into hot water. A patient asked me if I could schedule some sessions with him and his wife together, because he was planning to seek a divorce and wanted me to observe her irrational behavior first-hand. He was hoping that I'd testify on his behalf in case things got ugly during the divorce proceedings. I explained that if I saw her, it would represent a conflict of interest. Anyone I see becomes my patient, and I can't do therapy simultaneously for two individuals who are involved in a legal battle with each other. Financial arrangements. Ask about any financial problems the patient may have. Does the patient understand the cost of the treatment? Can she or he afford the treatment? I explain that patients pay for each session at the start of the session. I avoid billing patients on a monthly basis, because all kinds of slippage can and will occur. I record the date, length of session, payment, and any current balance in a flow sheet in the patient's chart. This is easy, and your billing records will always be up to date. Furthermore, if there's a problem, you'll know right away and can discuss it with the patient. Last minute cancellations. I tried a variety of arrangements over the years that weren't very effective. Eventually, I told patients that they could cancel
Chapter 5
149
and reschedule a session for any reason whatsoever as long as they gave me at least 24 hours notice. If they gave me less than 24 hours notice, I would charge them the full fee for the session, regardless of the reason for the cancellation. However, if I had a waiting list, and could fill their slot with another patient at the last minute, I would not charge them. I explained that my policy was the same as if they'd purchased a ticket to a concert or baseball game. If they didn't show up, they wouldn't be entitled to a refund. Some therapists tell patients that they will not be charged for a missed or cancelled session as long as they have a good reason, such as sickness. This sounds good on paper but never works because patients always have a good excuse! For example, a businessman once called two hours before his session to cancel. He explained that he was feeling so good that he'd decided to treat himself to an impromptu trip to Switzerland to go skiing. He said it would be unfair to charge him for the session, since he'd be out of the country and unable to attend! There were times when I decided not to charge a patient, even though they cancelled at the last minute and did not give the required 24-hour notification. For example, if there was a death in the family, billing seemed clearly inappropriate and insensitive. But I wanted to be the one to make this determination. Otherwise, there was simply too much room for manipulation by patients. I also told patients that if they could not come in person due to bad weather conditions, I'd be happy to have a phone session with them, and bill
Chapter 5
150
them for it. All they had to do was call my office at their regularly scheduled time and have a paper and pencil ready, along with their psychotherapy homework, so we could proceed just as we would if we were meeting faceto-face. Some of my best psychotherapy sessions were conducted over the phone. If patients weren't happy with my cancellation policy, I didn't negotiate the issue or explore their feelings. I told them that I'd love to work with them, but if they felt strongly about not having to pay for skipped or cancelled sessions, it might be better for them to seek treatment from a therapist whose policies were more consistent with their expectations. I also explained that it works both ways, and that I held myself equally accountable. For example, if I ever forgot a session, I'd give them a free session to compensate for their inconvenience. This only happened two or three times in my entire career. You might wonder why I put so much emphasis on administrative arrangements. Many of the patients we treat are unassertive or hostile and act out their negative feelings indirectly. For example, if they're upset with you, they might "forget" to show up for their sessions. Novice therapists are often idealistic and do not comprehend how common these problems can be. Good therapy involves handling these contingencies effectively. If you let patients take advantage of you, because you're unassertive or conflictphobic, you'll be reinforcing your patients' dysfunctional behavior patterns. Emergencies. I always explain my emergency on-call policy. This will vary,
Chapter 5
151
depending on the nature of your practice. Are you available for emergencies? What types of emergencies? If not, who should the patient call? I did not give out my home phone number, which was unlisted, but I let patients know that I always carried my on-call beeper and that they could reach me at any time if they had to. I explained that because I was in private practice, I wasn't in a position to be able to handle lots of emergency calls. However, if they felt suicidal, or were having a serious medication problem, they should definitely call me. I emphasized that there might be times when they would need to speak with me on the phone to receive support in the here-and-now, and that I'd be happy to give them a phone session and bill them for the time. This approach worked well. If an overly needy patient needed some phone support, I felt a lot better about providing it, knowing that I would be compensated for my time and effort. Negative feelings. I remind patients that negative feelings are very common in therapy, and that they may feel unhappy about me, or the treatment, from time to time. I tell them that I want them to express these feelings, and emphasize that these discussions often lead to therapeutic breakthroughs. In addition, I explain that I will ask them to fill out the Evaluation of Therapy Session form on page 203 after every session, so they can rate how warm and understanding I was and how helpful the session was. They can also write out what they liked and disliked about the session. I emphasize that a frank discussion of these feelings is sometimes uncomfortable, but vitally
Chapter 5
152
important. Consultations. I tell the patients that if they have doubts or questions about the strategy I'm using, or feel that we're stuck, I'd be happy to obtain a consultation with a colleague on their behalf at any time, and that there will be no charge for this. They can also seek a face-to-face consultation with another mental health professional at any time to assess the treatment. Of course, I am hopeful that they will share their feelings with me first, because we can usually resolve any concerns they might have. Contacts outside of sessions. I explain that I never meet with patients outside of therapy sessions, and that doing so amounts to an ethics violation. However, we might run into each other outside of sessions at a shopping center. I ask patients if they'd want me to say hello, or if they would prefer it if we simply ignored each other's presence. Most patients are pretty relaxed about this and are happy to say hello, or even to chat briefly, if they run into you. Confidentiality. I tell patients that the information they provide will be kept confidential, and that I won't supply information to any outside person without their written consent. I tell them that if someone calls to inquire about how they're doing, I won't provide any information about them, or even acknowledge that they're my patient. However, if the patient would like a friend or family member to meet with us during a session, that would be fine. I remind the patient that if a friend or family member calls to provide information about them, I won't speak with that person unless the patient asks
Chapter 5
153
me to do so. In addition, I inform the caller that I'll share the information they provide with the patient and will never withhold any information from my patients. Confidentiality exceptions. I tell the patient that there are some emergencies where I may have to violate the rule of confidentiality. For example, if the patient makes suicidal or violent threats, I may have to contact family members, the authorities, or the potential victim. Or, if I learn that the patient has been involved in abusing others, including children, I may be required to report the problem to the authorities as well. Other ethical issues. I remind the patient that I will not accept gifts from them or from their family, as this can create a conflict of interest. I also remind them that I don't read any books or other written materials they might give me between sessions, but we can review them during sessions. I explain that I don't touch or hug patients, aside from shaking hands, as this may constitute an ethics violation.* Some younger therapists object to this regulation, thinking that's it's too cold. The problem is that patients are vulnerable, and sexual or romantic feelings can easily get fired up during the treatment. Some patients will misinterpret any hugging or touching, with potentially disastrous consequences. I have found that I can nearly always create a warm and accepting therapeutic alliance without having to resort to touching. Initial Formulation and Treatment Plan
Chapter 5
154
You can summarize your conceptualization of the patient's problems, along with your treatment recommendations, at the end of the clinical history. Ask the patient if your understanding and suggestions make sense, and how they feel about working with you. A comprehensive clinical history can be time-consuming and demanding, but it's necessary and will protect you from a legal and ethical perspective. In certain treatment settings, such as an emergency room, you'll be limited to a far more streamlined evaluation that focuses on the patient's main complaints. For this purpose, you may want to use the Brief History outlined on page 116. Remember that good therapy is collaborative, and the patient has to be accountable. At the initial assessment, the patient is not yet your patient from a legal perspective. Patients are there to decide whether they like you and want to work with you. Your job is to determine whether you're able to treat the problems they describe, and whether you're willing to accept them into treatment. If a patient doesn't want to work with you, or if you don't feel comfortable treating that individual, you can offer to refer them to someone else or encourage them to seek a therapist who will provide a better fit. Of course, you can also offer to send a summary of your intake evaluation to any other mental health professional if the patient requests it. The initial assessment involves many critical issues. If you handle them skillfully and shrewdly, you'll develop an in-depth understanding of your patient and you'll be getting the therapy off to an excellent start. This is your chance to * If you have any questions about this, you can check with the ethics committee of your
Chapter 5
155
get to know the patient and show that you're a responsible and compassionate therapist.
professional association or contact your professional liability carrier for more information.
Part Three T = TESTING A Boring Topic with Exciting Implications A-TEAM
Assessment Assessment
Testing Testing
Methods Methods
Empathy Empathy Agenda Agenda Setting Setting
6*
The Clinician's Illusion
Our field consists of numerous schools of therapy that compete with each other, much like religions. Many of us are convinced that we've found the one true religion. We tend to believe that our theories are valid and that our methods are more sophisticated than those used by therapists from other schools of therapy. If you ask a psychoanalyst or psychodynamic therapist what they think about cognitive behavioral therapy (CBT), they'll probably tell you that it's superficial and doesn't get at the "true causes" of patients' problems. They may tell you that there's not enough emphasis on emotion or on the therapeutic alliance, and that these are the keys to recovery. They may also say that the idea of rapid recovery is naïve, since real change necessarily takes a long time. Now ask a cognitive therapist what they think about psychoanalysis. They may tell you that:
* Copyright
2003 by David D. Burns, M.D.
Chapter 6
158
Psychoanalysis is based on superstitious thinking rather than the scientific method. Psychoanalysts are opposed to measurement, so their theories and methods can never be tested. Psychoanalysis attracts controlling, authoritarian people. Psychoanalysis is ineffective in the treatment of depression, anxiety, and all other Axis I and II disorders. Psychoanalysis is not based on valid knowledge about the causes of psychiatric problems. Mucking around in the past is a waste of time that addicts patients to endless rumination and prevents them from taking charge of their lives. Patients deserve effective, empirically validated treatments. Now ask psychopharmacologists what they think about psychotherapy. They'll probably tell you that psychotherapy is a just a form of handholding, and that depression and anxiety result from a chemical imbalance in the brain and must be treated with medications. We've been engaged in these kinds of territorial wars for decades. Why haven't we converged on a true science of human behavior and moved forward like other sciences, such as biology, chemistry and physics? It's partly because powerful political and financial forces dominate our field. I was trained as a physician. Because I believed in the biological model that was emphasized during my residency training, I was an esteemed member of my fraternity. I felt like I had a leg up on all the mental health professionals
Chapter 6
159
who weren't empowered to prescribe drugs. And I knew that if I treated patients with this model in my clinical practice, I'd make significantly more money. A psychiatrist can see many patients every hour for brief medication management sessions, and can charge as much or more for these visits as a non-medical therapist charges for a full hour of psychotherapy. So if you define yourself as a "psychopharmacologist," your income will double or triple. Furthermore, you don't have to master any challenging psychotherapy techniques or get involved in lengthy discussions with your patients about their most intimate problems. In addition, you'll enjoy occasional drug-company perks, such as free continuing education conferences at the finest hotels, complete with gourmet meals. And if a drug company identifies you as a frequent prescriber of one of their new medications, you may be rewarded with trips to exotic places like the Bahamas, and you may even get to take your spouse. Political and financial pressures are not the only difficulty. We also get fooled by what I call the "Clinician's Illusion." As clinicians, we see things every day that appear to confirm our beliefs about depression, anxiety, personality disorders, addictions, and relationship problems. We tell ourselves that seeing is believing, but our perceptions and reasoning can be extremely misleading. Some of the most common sources of self-deception are listed on page 160. Let's examine them in more detail. '
Chapter 6
160
How Clinicians Fool Themselves 1. The Placebo Effect. You attribute your success to your theory and methods when the improvement you observed may have actually been a non-specific placebo effect.
5. Therapeutic Solipsism. You assume you know how your patients are thinking and feeling, and you're not aware that your perceptions are completely off base.
2. Self-Fulfilling Prophecies. You feel so certain that something will happen that you subconsciously make it happen. Then you conclude you were right all along.
6. Therapeutic Arrogance. You assume that your theories and methods are valid a priori, and that you don't really need to test them empirically.
3. Sample Selection Bias. You generalize about the effectiveness of your treatment based on your experiences with the highly selected group of patients who seek you out and continue to work with you.
7. Coupling. You couple a new technique, such as rapid eye movement, with an established method, such as gradual exposure or flooding, and attribute the improvement you observe to the new technique.
4. Selective Recall. You selectively remember the patients who respond well to your interventions, and selectively forget or discount those who don't.
8. The Confirmation Paradox. You assume that your theories are valid because they're consistent with your clinical observations.
Chapter 6
161
The Placebo Effect Imagine this scenario: a man who's been feeling worthless and discouraged for several months seeks treatment from his family physician, or from a local psychiatrist. The doctor explains that he's suffering from an episode of depression that results from a chemical imbalance in his brain. The doctor reassures him and gives him a prescription for an antidepressant that will correct the imbalance. Four weeks later, the man reports that he's feeling much better. He's sleeping better, his mood has lifted, and he's productively involved in life again. He and his psychiatrist attribute his dramatic improvement to the antidepressant medication. Is this sound reasoning? Can we reasonably conclude that: His depression resulted from a chemical imbalance in his brain? The antidepressant corrected this chemical imbalance? He responded to the antidepressant? Although many health professionals and patients do draw these kinds of conclusions, his rapid improvement does not provide convincing evidence for any of them. All we can say for sure is that he was depressed and now he's feeling better. That's great, but we don't know what caused his depression or what triggered his improvement. His improvement could have resulted from the passage of time, unexpected events that lifted his mood, the fact that he became more active, the medication, or other factors, including the placebo effect. What is the placebo effect, and why is it so important? We know that our expectations can have powerful influences on the way we think, feel, and
Chapter 6
162
behave. If you're convinced that something will help, there's a good chance that it will help, even if it has no real effects at all. Let's say that you and I work as marketing executives for a pharmaceutical company. One day, at a press conference, we announce the synthesis of a wonderful new antidepressant called "Placebin." We emphasize the superior antidepressant effects of Placebin and explain that it has few or no side effects, and virtually no toxic effects. In fact, we're so excited by this new breakthrough that we're going to give Placebin to a million depressed people absolutely free of charge in a huge, nationwide clinical trial. There's tremendous enthusiasm for Placebin and our stock goes up by more than a billion dollars overnight. Of course, we don't tell anyone that our new drug is just a placebo, with no active chemical ingredient. How many of the million depressed patients who take Placebin will recover? Numerous research studies have shown that if you give an inert placebo to people who are suffering from depression, 30% – 50% of them will recover. The precise percentage will depend on how severe or refractory the patients are. This means that within a few weeks, 300,000 – 500,000 of the patients in our clinical trial will have recovered. They'll swear by the drug and tell all their friends about it. Some may even appear on Oprah and give glowing testimonials about how Placebin changed their lives. Tens of thousands of people will rush to their doctors to get prescriptions for this remarkable new medication, and controversial books will appear, asking whether it's ethical to prescribe "happiness pills." But of course, Placebin didn't really do anything for anyone. It was the
Chapter 6
163
patients' expectations, and not the pills, that got them better. The patients actually healed themselves, but didn't realize it. Why are placebos so powerful? A few possibilities jump to mind: Hope. Hopelessness is one of the cardinal symptoms of depression. The belief that things can't change acts as a self-fulfilling prophecy, because the patient gives up. Then nothing changes, so the patient concludes that she or he really is hopeless. Hope works in the opposite way. If you expect to get better, you'll become more productive and your outlook will change, so you'll start to feel better. That's why patients who believe in any new "treatment" for depression or anxiety have such a good chance of recovering, even if the treatment only has placebo effects. In many cases, the belief that you'll recover, and not the treatment itself, causes the improvement. Hope is the most potent antidepressant in existence. Warmth and empathy. Positive correlations between therapeutic empathy and recovery have been reported in more than 100 psychotherapy outcome studies (Orlinsky, Grawe, & Parks, 1995). Patients who perceive their therapists as warm and understanding recover more rapidly than patients who do not feel accepted or understood by their therapists. Of course, a correlation does not necessarily imply causality. However, my own research, using Structural Equation Modeling techniques, suggests that the correlation results from a direct causal effect of therapist empathy on recovery from depression (Burns & Nolen-Hoeksema, 1992).
Chapter 6
164
Hope and empathy are important keys to recovery, but these variables create confusion about how and why therapy works. You can test any kind of unusual therapeutic intervention you want, and if you can convince people that your treatment will be effective, it probably will be reasonably effective, even if it involves blatant quackery. Whatever we do will be somewhat effective for some of our patients, and amazingly effective for a number of them. As a result, we may conclude that our theories are valid and that our treatments have specific antidepressant or anti-anxiety effects. We'll attribute the positive outcomes we observe to our theories and to the methods we're using, and not to the placebo effect. We'll tell ourselves, "Bob recovered because of the antidepressant I prescribed," or "the EMDR* I used," or "the family of origin work we did," or whatever method we tried. This is not a trivial concern, because new treatments for depression and anxiety emerge all the time. Many of the new schools of therapy attract large numbers of followers, especially if they're skillfully marketed. I don't mean to imply that the placebo effect is a bad thing, or that it's unimportant. It's been one of the physician's strongest medicines for thousands of years, and it deserves more research. If we can learn more about how the placebo effect works, we can develop more potent placebos. But if you had a ruptured appendix, wouldn't you want the help of a skillful surgeon? If the surgeon had a warm, reassuring bedside manner, so much the better, but you'd need more than just the placebo effect to save your life. * EMDR is a treatment for anxiety that involves rhythmic movement of the eyes back and forth
Chapter 6
165
Now, you may be thinking, "Well, this is all rather academic, because we do have empirically validated treatments for depression and anxiety. Drugs and psychotherapy have been proven to be effective." In fact, the situation isn't so clear-cut. Recent studies suggest that antidepressants may have very few real therapeutic effects, if any, above and beyond their placebo effects. For example, in a well-controlled, multi-university study funded by the National Institute of Mental Health, 320 patients with major depression were randomly assigned to treatment with St. John's wort, sertraline (Zoloft), or placebo. As you can see in the chart on page 166, 32% of the patients who received placebo recovered, as compared with only 25% of the patients who received sertraline and 24% of the patients who received St. John's wort (Hypericum depression trial study group, 2002). This study clearly showed that St. John's wort has no real antidepressant effects above and beyond its placebo effects, a result that was widely publicized by the pharmaceutical industry. However, they didn't publicize the fact that the antidepressant didn't fare much better than St. John's wort! The authors of the study concluded that "the overall response to sertraline on the primary measures was not superior to that of placebo, an outcome which is not uncommon in trials of approved antidepressants" (NIH, 2002).
during exposure to upsetting memories and images.
Chapter 6
166
These results are not consistent with the widely held notion that the chemicals called "antidepressants" have strong, specific antidepressant effects. In fact, based on their review of the world literature, as well as the data that has been submitted to the FDA by drug companies over the past several decades, Kirsch and his colleagues have concluded that at least 75% – 80% of the effects we attribute to antidepressant medications clearly result from their placebo effects (Kirsch & Sapirstein, 1998; Kirsch, Moore, Scoboria, & Nicholls, 2002).
NIMH Depression Study
Percent of Patients Who Recovered
35
32%
30 25
25%
24%
Zoloft St. John's Wort
20
Placebo
15 10
On page 168, you can see a graph that represents the kinds of results you'll find in the most favorable drug company studies that have been conducted. In this study, patients with scores averaging 25 on the Hamilton Rating Scale for Depression (HRSD) were randomly assigned to treatment with placebo versus an SSRI antidepressant.* A 25-point reduction in HRSD scores would be needed
* This table, and the ones on pages 169 and 170 were adapted from Preskorn, S. H. (1997). Clinically relevant pharmacology of selective serotonin reuptake inhibitors: an overview with
Chapter 6
167
for full recovery. As you can see, the SSRI group experienced a 10-point reduction in HRSD scores, while the placebo group experienced an 8-point drop. There are two striking things about these results. First, the difference between the drug and placebo groups was only 2 points. This is the most improvement you could attribute to the drug itself, and it's small. Some recent researchers have suggested that such a tiny effect may not justify prescribing antidepressants, given the significant side effects, toxic effects, and hazards associated with these agents (Antonuccio, Danton, & DeNelsky, 1995; Antonuccio, Danton, DeNelsky, Greenberg, & Gordon, 1999; Kirsch, Moore, Scoboria, & Nicholls, 2002). Second, 8 of the 10 points of improvement in HRSD scores in the drug group, or 80%, appears to have resulted from the placebo effect, and not from the drug itself. In other words, if the people in the drug group had been in the placebo group instead, they still would have improved by 8 points. Keep in mind that the figure on page 168 represents the best studies that drug companies published. However, drug companies suppress the results of many studies that don't come out in the "right" way. If you look at the figure on page 169, you'll see the results of a study in which there were no differences whatsoever between the antidepressant and the placebo. Industry insiders will tell you that studies like this are very common, but the results are never published. As a result, there's a highly misleading pro-drug bias in the world literature. This leads to false perceptions about the efficacy of these agents.
emphasis on pharmacokinetics and effects on oxidative drug metabolism. Clinical Pharmacokinetics, 32 Suppl. 1: 1-21.
Chapter 6
168
Antidepressants vs. Placebos—The "Best" Studies
30 25 Changes in Hamilton Depression Scores
25
Placebo
20 Medication
15 10 5 0
8
10 Needed for Recovery
Chapter 6
169
Antidepressants vs. Placebos—A Typical Study
30 25 Changes in Hamilton Depression Scores
25
Placebo
20 Medication
15 10 5 0
8
8
Needed for Recovery
Chapter 6
170
Change in Hamilton Depression Scores Depression
Paroxetine (Paxil) vs. Placebo *
12
*
*
30 mg
40 mg
ns
10 8 6 4 2 0 Placebo
10 mg
20 mg
Chapter 6 I've included some actual drug company data on Paxil in the figure on page 170. You can see that the patients who received the 10 mg per day dose of Paxil actually did worse than the patients who received placebo, and the patients on the higher doses of Paxil only improved about 1 or 2 points more than the placebo group. The results with other SSRI antidepressants are similar. Recent researchers have argued that the tiny differences between antidepressants and placebos in the most "favorable" outcome studies may result from flaws in the way drug companies conduct these studies (Antonuccio, Burns, & Danton, 2002; Antonuccio, Danton, & DeNelsky, 1995; Antonuccio, Danton, DeNelsky, Greenberg, & Gordon, 1999; Kirsch, Moore, Scoboria, & Nicholls, 2002). One problem is called the "placebo washout" period. Prior to randomizing patients to the drug or placebo group, drug companies put all the patients on placebos for a one to two-week period. During this phase of the study, they carefully monitor the patients' depression scores. Any patients who improve are selectively removed from the study. At the end of the "placebo washout" period, the researchers randomly assign the remaining patients to the placebo or drug groups. In this way, they stack the deck in favor of their new drug. Can you imagine what would happen if they set the study up in the opposite way? Suppose they put everyone on their new antidepressant for one or two weeks, and then removed all those who began to improve before randomly assigning them to the placebo versus drug conditions. The drug companies would cry foul, because you'd be biasing the study against their drug. But that's
Chapter 6 exactly what they do when they selectively remove the placebo responders from their studies! Why do drug companies do this? Their motives are financial rather than scientific. If they can come up with two studies that demonstrate a statistically significant difference between their new drug and a placebo, they'll receive FDA approval to market the new drug. As a result, their stock will increase in value by more than a billion dollars overnight. They use other tricks to try to stack the deck in their favor as well. For example, patients who enlist in a drug company study of a new antidepressant are informed that they'll either receive the new drug or a placebo. They're also informed that the placebo will be chemically inactive and will have no side effects. However, if they receive the new antidepressant, there will be certain side effects they should expect. For example, if they receive Prozac, they may experience upset stomach, diarrhea, nervousness, a loss of sexual drive, and so forth. Once the study begins, patients who experience the anticipated side effects usually conclude they got the new drug. In contrast, patients who don't experience any side effects usually conclude that they're in the placebo group. Studies indicate that if you ask patients which group they're in, they'll be correct as often as 90% of the time. So the studies aren't really "double blind" at all, because the patients know very well whether or not they're receiving the new "antidepressant." This flaw tends to bias the results because the patients who think they're getting the new
Chapter 6 antidepressant become more hopeful and optimistic, so their depression scores improve. In contrast, the patients who think they're only getting the placebo tend to feel disappointed, so their depression scores may worsen. This can create statistically significant differences between the drug and placebo groups, even when no differences exist in reality. Another problem is the use of badly flawed assessment instruments like the HRSD. This scale is one of the worst psychometric instruments ever developed and it boggles my mind that anyone would take it seriously, much less use it in research! There are many fatal flaws with this instrument, including the fact that it focuses almost exclusively on non-specific somatic symptoms, which are poor indicators of depression. For example, three of the16 items on the HRSD ask about insomnia. As noted earlier, many factors other than depression can cause insomnia. Furthermore, any medication with sedative properties will cause an apparent "improvement" on the HRSD, even if the medication has no antidepressant properties at all! This is not a trivial problem, because many antidepressants have significant sedative side effects. These flaws are particularly egregious because all these problems are easily solvable from a research perspective. For example, you could simply ask patients what group they think they're in soon after the study begins, and control for this variable when you analyze the data. Or, you could use active placebos rather than inactive placebos. For example, if the drug being tested causes sedation, you could use an antihistamine like Benadryl for the placebo, since this
Chapter 6 medication causes sedation. Or, if the drug causes speediness and diarrhea, like Prozac, you could use caffeine for the placebo. But drug companies refuse to use more refined assessment instruments or implement any corrective strategies because they know they've got a good thing going and don't want to rock the boat. In fact, the only studies in the world literature that have used active placebos have failed to show any differences whatsoever between placebos and antidepressants (Kirsch & Sapirstein, 1998; Moncrieff, Wessely, & Hardy, 1998; Moncrieff & Double, 2003). Clearly, drug companies don't want to wander into this territory! Recent reports have dealt even stronger blows to the psychopharmaceutical industry. Investigators have shown that all the new antidepressants, including the SSRIs, appear to cause substantial increases in the rates of successful suicide in children (Garland, 2004; Jureidini et al., 2004; Whittington et al., 2004) and in adults (Healy, 2003). On page 175, you can see the rates of successful suicide in depressed adults who were randomly assigned to SSRIs (such as Prozac) or placebos in drug company studies. If these were true antidepressants, why would they cause an increase in suicide rates?* Many people find these studies hard to swallow, and simply cannot believe them at first. We all know someone who's said, "Prozac really worked for me. It saved my life. The effect has to be real!" But remember that 30% – 50% of the people who receive a placebo will say exactly the same thing. * The increase in suicide may result from the stimulating effects of these antidepressants. Some patients become more agitated and anxious or even experience akathisia when taking SSRIs, and this may trigger suicidal feelings. Another possibility is that the lack of antidepressant effects
Chapter 6
Incidence of Suicide In Worldwide Phase 1 – 3 Antidepressant Studies* Percent of Patients
2.0 1.55% 1.5 1.0 0.5
.48%
.66%
0 All Placebo Studies N = 4,140
SSRI Placebo Studies N = 2,401
All SSRI Studies N = 10,611
My reading of the literature, as well as my clinical experience over the years, has led me to conclude that true antidepressant medications may not yet exist. We have chemicals with side effects that are called "antidepressants," such as Prozac and Paxil, but the antidepressant effects of these kinds of drugs appear to be underwhelming at best. I don't want to throw too many stones at the drug companies, because a critical reading of the psychotherapy outcome literature reveals similar problems. Many forms of psychotherapy do not seem to have any strong or specific antidepressant effects above and beyond their placebo effects, either in the short-term or the long-term. This suggests that most of the effects we attribute to may make some patients feel more desperate. They may reason, "Even this powerful new drug
Chapter 6 each "brand" of therapy may be non-specific placebo effects as well. Self-Fulfilling Prophecies Many of our patients have a negative view of themselves, the world, and the future. They feel so convinced that bad things will happen that they inadvertently cause the very outcomes they predict. For example, a man who feels bitter and lonely may subconsciously provoke hostility and rejection. Then he'll conclude, "I knew this would this happen! I predicted it all along." He'll feel like a victim and be unaware that he's the puppeteer who's pulling the strings.As mental health professionals, we sometimes make the same kinds of mental errors. We may subconsciously cause the results that we predicted and conclude that our theories were right all along. For example, traditional psychoanalytic techniques are based on the assumption that real recovery requires deep uncovering techniques and an analysis of the patient's character structure over a period of many years. Historically, the therapist assumes a passive role and does not intervene actively with interpersonal skill-building or cognitive restructuring techniques. Of course, the belief that change will require many years can function as a self-fulfilling prophecy, because the patient is unlikely to change, given the lack of aggressive, empirically validated interventions. Then the analyst assumes that change must always be a slow process that requires many years of daily psychoanalytic treatment. Sample Selection Bias Let's say you want to find out whether or not AA is really effective, so you attend an AA meeting and ask one of the participants about it. He's extremely isn't helping me. I must be a hopeless case."
Chapter 6 enthusiastic and tells you that AA has changed his life. He explains that he's been coming to meetings for 17 years and hasn't had a drink for 15 years. You ask several other members as well. They all offer glowing testimonials about the benefits of AA. All of them have successfully quit drinking and maintained their sobriety for extended periods of time. Based on your informal survey, you might conclude that AA is 99% effective. Is this conclusion valid? There are a couple of potential problems with this reasoning. In the first place, very few people who abuse alcohol ever attend a single AA meeting. They're simply not interested or motivated. But to be generous, let's assume that 5% of the people who abuse alcohol eventually attend at least one AA meeting. Now, how many of them will be there five years later? There's a significant attrition rate among AA participants. According to some estimates, only 5% of the people who attend one AA meeting still attend meetings one year later. Over the long haul, even more will eventually drop out and start drinking again. This means that less than 5% stick with the program. So the true percentage of people with alcohol problems who have achieved abstinence because of AA isles than 0.25%, and not 99%! How did we manage to inflate our estimates of AA's effectiveness by a factor of 400? Simply by reasoning from the data we obtained at the AA meeting. Statistically, this is called a "sample specification error." In other words, we may be generalizing from a highly biased sample that does not reflect the population as a whole. In fact, the people who are helped by AA have these characteristics:
Chapter 6 They're ready and willing to stop drinking. This is a tiny percentage of the people who abuse alcohol. They're looking for help and support, so they go to an AA meeting. This is a tiny percentage of the alcoholics who want to stop drinking. They like what AA has to offer, so they attend more than one meeting. This is a small percentage of those who attend at least one AA meeting. They stick with the program and attend meetings consistently for a prolonged period of time, in spite of temptations to drink. This is a small percentage of those who get started with AA in the first place. I'm definitely not trying to be critical of AA. I think AA is a godsend. If I were treating an alcoholic patient, I might even insist that they attend AA meetings regularly in addition to coming to therapy, or else I'd refuse to treat them. All I'm saying is that we can easily be misled when we generalize about the effectiveness of our treatment methods, based on the patients who come to us for help and continue working with us. Selective Recall We're far more likely to remember and report positive outcomes than treatment failures. Therapists, patients and the media alike prefer to publicize interventions that appear to work, especially if the recovery was dramatic. When a national television show features an emotional problem like OCD or depression, and you see a patient who was helped by some medication or form of therapy, the network receives tens of thousands of calls and letters from desperate individuals who want to know how to get that form of therapy. At the
Chapter 6
Estimated and Actual Dropout Rates at Two Midwestern Clinics 70%
64.1% 57.0%
60% 50% 40%
30.3%
30% 20%
16.8%
10% 0% What's Your What's Your Actual Actual Own Dropout Colleagues' Dropout Rate Dropout Rate Rate? Dropout Rate? at Urban Clinic at Rural Clinic
same time, we're quick to discount or ignore negative results. When a patient fails to improve or drops out of treatment, we say that she or he was resistant, unmotivated, "borderline," atypical, or non-responsive. In one study, therapists from 43 Midwestern mental health clinics were asked to estimate how many of their patients dropped out of treatment prematurely (Pekarik, 1987). The actual dropout rates were also obtained at two of the clinics. As you can see in the figure above, the therapists at the urban clinic estimated that 16.8% of their own patients dropped out of therapy
Chapter 6 prematurely. The same therapist's estimated that the dropout rate for their colleagues was 30.3%, or almost twice as high. But this was impossible, since all their colleagues were involved in the same study! The findings suggested a selfserving bias in the way therapists evaluate their own performance. However, the degree of self-deception by the therapists was even greater than what those data would suggest, since the true dropout rate at the clinic was 57.0%! At the rural clinic, the exact same pattern was obtained, but the true dropout rate was even higher—64.1%! The extreme discrepancy between the therapists' perceptions of their own performance and the reality of the situation illustrates how easily we can fool ourselves when we think we're being objective about our clinical work and skills. Therapists were also asked to select the most common reason why their patients dropped out prematurely. As you can see on page 183, the top reason cited by therapists was, "Problem solved or improved." 59% of the therapists chose this option and only 7% of the therapists selected, "dislike of the therapist or the therapy" as the reason for premature termination. In other words, these therapists interpreted premature termination as a sign that they were doing a good job and that their patients liked them. In fact, only 39% of the patients indicated that they dropped out of therapy because they improved or their problem was solved, while 26% of the patients indicated they dropped out because of dislike for the therapist or the therapy. Once again, the therapists' perceptions were at odds with the actual data. Finally, the therapists were asked to estimate the average number of visits
Chapter 6 their clients had. As you can see on page 184, the therapist's estimate was 15 sessions, but the actual number of visits was only 5! The investigators concluded that many therapists consistently perceive the therapy as far more positive than it actually is. They underestimate dropout rates as well as levels of client dissatisfaction and overestimate continuance rates. You can see the percent of the therapists' errors in the chart on page 184.* The investigators speculated that one possible reason for these gross errors might be that although only 30% of their clients attended six or more clinic visits, these clients accounted for 75% of all the clinic visits. As a result, the therapists spent most of their time with the patients who didn't drop out of treatment, thus creating the illusion that most clients attended many sessions. Therapeutic Solipsism The study of premature termination how we can make profound errors in our understanding of even the most basic facts about our patients. But we're usually unaware of just how off base our perceptions can be. We've talked about the fact that therapist and patient ratings of symptom severity, the quality of the therapeutic relationship, and therapeutic helpfulness are barely correlated, if at all. This means that our beliefs about how our patients think and feel may not be even vaguely accurate. However, most of us assume that our perceptions are valid. This can result in grossly misleading conclusions about how our patients feel and how effective our treatments are.
* In each case, I used this type of formula to calculate the percent error: % Error = (true value / therapists' estimate) * 100%. For example, the true value of 15 sessions divided by the therapists' estimate of 5 sessions & 100% = 300%.
Chapter 6
Chapter 6
183
Reason for Premature Termination: Didn't Like Therapist
Reason for Premature Termination: Patient Recovered 30%
70% 60%
59%
25%
50% 40% 30% 20%
26%
39%
Therapists' Estimate Actual Value
20%
Therapists' Estimate
15% 10%
10%
5%
0%
0%
Actual Value 7%
Chapter 6
184
Percent Therapist Error
Estimated vs. Actual Number of Therapy Sessions 400%
16
15
14
371%
339%
300%
300%
12 Therapists' Estimates
10 8 6
5
Actual Value
200%
151%
100%
4 2
0%
0 Sessions
Actual vs. Im provem ent Estim ated / Problem Dropout Rate Solved
Dislike of Therapist
Num ber of Sessions
Chapter 6
185
While I was living in Philadelphia, I supervised a psychiatric resident named Brett who asked for guidance in his treatment of a severely depressed bipolar patient named Evie. Evie had been in treatment for more than 15 years, and had been seen by a number of staff psychiatrists and residents. Throughout her treatment, she'd received numerous antidepressants and mood stabilizers, usually three to five different medications at once. I'm not in favor of this practice, but it's quite common, and perhaps more the rule than the exception. Unfortunately, Evie experienced a severe reaction to one of the drugs and nearly died. She went into a coma and spent several weeks in the intensive care unit. Following recovery, she was placed on five new psychiatric medications and was assigned to Brett for follow-up treatment. I asked Brett why Evie was taking so many medications, given the fact that she'd almost died from one of them. He explained that the attending physician had assured him that the medications were absolutely necessary to correct the chemical imbalance in Evie's brain, and that she'd be much worse off without them. I pointed out that our perceptions of how our patients feel are barely correlated with how they actually do feel, if at all, and asked if he or any of the attending psychiatrists had ever given her a reliable self-assessment test to measure her symptoms or monitor her progress from week to week. Brett admitted that she'd never been given any self-assessment tests. I asked Brett how the therapeutic relationship was. He said that even though Evie was quite depressed, she seemed to like him a lot and they had an
Chapter 6
186
excellent therapeutic alliance. I pointed out that our perceptions about how warm and empathic we are sometimes aren't correlated with our patients' perceptions, either, and that it might not hurt to check this out as well. Brett agreed to give Evie the Brief Mood Survey and Evaluation of Therapy Session on pages 202 – 203 at their next session. He was shocked by the results. Evie scored a 20 out of 20 on the depression, anxiety, and anger scales. These are the worst possible scores, and indicate overwhelming levels of emotional distress. These scores were not consistent with Brett's belief that the medications were helping Evie. When patients improve, you see sharp reductions in their scores on the Brief Mood Survey. When their scores drop all the way to zero, they generally feel happy and joyous. If a treatment doesn't produce substantial and measurable results, then it isn't working, no matter how strongly you believe in it. It would be pretty hard to argue that Evie's antidepressant medications were helping her, when her scores on the tests showed that she was one of the most severely depressed individuals in North America! Next, we reviewed Evie's scores on the Evaluation of Therapy Session. Her responses on the Therapeutic Empathy scale showed that she didn't feel that Brett was warm, compassionate, or trustworthy. She also indicated that Brett didn't comprehend how she felt inside, and that she found the sessions frustrating and upsetting. At the bottom, patients can indicate what they liked and disliked the most about the session. Evie had simply scribbled, "No comment!" Brett was eager to improve his relationship with Evie. I suggested we do
Chapter 6
187
some role-playing so he could learn how to respond more empathically. I played Evie's role, and ripped into Brett. He did a superb job at responding to my criticisms, and didn't get at all defensive. At the next session, Brett reviewed the tests with Evie, and told her that he was surprised to discover how intense her feelings of depression, anxiety and anger still were, and sad to discover how badly he'd let her down. He urged her to express her negative feelings. She began to talk about all the frustration, hopelessness, and loneliness that she'd been bottling up, and started to cry. Brett had the feeling that they were finally connecting in a meaningful way. At the end of the session, he asked her to complete the Brief Mood Survey and Evaluation of Therapy Session again in the waiting room before she left. Brett was relieved when he reviewed her scores a few minutes later. She'd given him perfect scores on the Therapeutic Empathy and Helpfulness scales. At the bottom of the form, she wrote: "I've been coming here for over 15 years, and you're the only psychiatrist who's ever listened. This session meant so much to me!" Evie's responses on the Brief Mood Survey were equally encouraging. Her scores on the depression, anxiety and anger tests had all dropped by 60% – 70%, indicating only mild levels of distress. This was vastly more improvement in a single 45-minute session than she'd experienced in over 15 years of aggressive psychopharmacologic treatment—simply because the doctor had finally listened. Therapeutic Arrogance
Chapter 6
188
I had the chance to supervise a number of outstanding psychiatric residents when I was teaching at the University of Pennsylvania School of Medicine. Another real standout was a resident named Roy. Roy was enthusiastic and had a great sense of humor. He was particularly excited about the Brief Mood Survey and Therapeutic Empathy scale. At the beginning of our supervision sessions, he'd often say, "Oh, Dr. Burns, I'm so excited to see you because I got horrible scores from three patients on the Therapeutic Empathy scale this week. I can't wait to find out what I'm doing wrong." Then we'd laugh and have a terrific supervision session. Toward the end of the year, all the residents were required to give a presentation in one of their psychotherapy classes about something they'd learned that was particularly helpful to them. Roy decided to talk about the value of the assessment instruments, because most of the residents in his class weren't familiar with them. He prepared several overheads that illustrated how improvements in therapeutic empathy scores were correlated with improvements in patients' mood scores. During his talk, Roy emphasized that his perceptions of his patients were frequently off base, and that their ratings of him often came as a surprise. He concluded by saying that the assessment instruments had made a huge impact on his clinical work, and that he couldn't even imagine treating patients without them. When Roy finished his presentation, he expected some animated discussion, and was surprised when not a single hand went up. Everyone sat in
Chapter 6
189
stony silence. Then the professor, who was a psychoanalyst, said: "Honestly, Doctor, I'm shocked and deeply disappointed by your presentation. Do you think so little of your interviewing skills that you've had to lower yourself to this? And have you stopped to consider the devastating—and possibly irreversible—damage you're inflicting on your patients?" Roy was speechless! He wanted to say, "As a matter of fact, Doctor, I do think that little about the accuracy of my perceptions, and I do need these tools. Do you think so highly of your own interviewing skills that you think you don't need them?" Fortunately, Roy bit his tongue and didn't say that, because he wanted to graduate! Of course, clinical intuition and sensitivity are invaluable, but this professor's refusal to use any assessment instruments would be comparable to a physician who refused to order blood tests, x-rays, or EKGs because he thought he didn't really need the information, or because he thought the lab tests would upset the patient. He'd soon lose his license! But most mental health professionals still seem to think that they can shoot from the hip and don't like to be held accountable. If there were an unforgivable sin among mental health professionals, I think this is it. It's the arrogant idea that we know the truth about our patients and don't need to confirm our perceptions with accurate assessment instruments or put our theories to the test. This position might be forgivable if our perceptions were as valid as we thought they were. But the research does not support this
Chapter 6
190
notion. When we think that we already know "the truth," and refuse to test our claims empirically, we end up with competing cults rather than a true science of human behavior. Coupling During a break at one of my recent Scared Stiff workshops, a therapist named Melinda asked for some help with her flying phobia. She felt some urgency about overcoming this problem because she'd recently gotten engaged, and she and her fiancé were planning to get married at his parents' home in France. This meant a long airplane trip, and Melinda was petrified. I explained that I couldn't ethically try to treat someone during a break at a workshop, but that I'd be glad to show her how a few of the Cognitive Exposure Techniques worked. I told Melinda to close her eyes and imagine she was just taking off on the airplane to France. Did any frightening fantasies or images come to mind? What was she afraid of? She said that she could picture herself on the plane. Suddenly, the pilot frantically announces that everyone needs to fasten their seat belts because the plane is about to run into heavy turbulence. Melinda told me that this image triggered intense feelings of panic. She estimated her anxiety at 90%. I asked her to try to make it even worse, and to tell me what she saw in her mind's eye. She imagined that the plane was shaking violently, and that luggage was flying out of the baggage compartment and hitting the passengers on the head. People were bleeding and screaming in terror as the plane was being tossed about in the air. As this point, she said that her anxiety had jumped
Chapter 6
191
to 95%. I encouraged Melinda to try to push it all the way up to 100%. What did she see in her mind's eye? She said that the plane had just been hit by lightning and was plummeting toward the earth in a ball of flames. All the passengers were screaming and flying through the air. At this point, Melinda estimated her anxiety at 100%. I asked her to remain as anxious as possible for several minutes. I was planning to illustrate Image Substitution, but an odd thing happened. Melinda said her anxiety was fading. I told her to try to push it back up to 100% because I wanted to show her how Image Substitution worked. I suggested she could imagine the worst possible outcome, such as the plane crashing into the earth, and people's arms and legs getting ripped apart. She said that the harder she tried to make herself anxious, the less anxious she felt. Suddenly, she opened her eyes and said that her anxiety had disappeared completely. She said she didn't feel any fear whatsoever about flying, and thought she was cured. The entire intervention took less than three minutes.* Now, let's suppose that I'd been using one of the new anti-anxiety techniques, like Eye Movement Desensitization and Reprocessing (EMDR) or Thought Field Therapy (TFT). During EMDR, you wave your finger back and forth during the exposure and instruct the patient to follow the movement of your finger with their eyes. During TFT, patients tap on a variety of acupressure points during the exposure. The proponents of EMDR and TFT say that these * You might feel that a 3-minute cure isn't believable. In fact, most patients with phobias require far more time and effort before they experience tangible improvement. However, some patients do respond quickly to exposure techniques. Remember, too, that her sudden
Chapter 6
192
techniques often lead to rapid, almost miraculous cures, and have elaborate explanations about how these methods work. EMDR and TFT have lots of enthusiastic advocates, and some harsh critics as well. Personally, I'm skeptical about these techniques, but I'm open to the possibility that distraction may enhance the effectiveness of exposure by making the exposure less traumatic. There may also be a hypnotic effect of staring at the finger moving back and forth, back and forth. In fact, patients with anxiety disorders are among the most hypnotizable people in the world. I think the jury is still out about these methods, and believe that more research will be needed to determine whether and how they work. Let's suppose, for the sake of argument, that the rhythmic movement of the eyes during exposure—the unique feature of EMDR—has no real effect other than the placebo effect, as suggested by some studies (Pitman, Orr, Altman, Longpre, Poire, & Macklin, 1996; Devilly, 2001a; 2001b). But one day, I decide to try EMDR with a few patients. Let's also suppose that Melinda was one of those patients, and that I'd encouraged her to follow the movement of my finger during the Cognitive Flooding. What would I have concluded? Clearly, I would have observed a sudden miraculous cure, since that's exactly what I observed with Cognitive Flooding alone. And I probably would have been instantly converted to EMDR. If I'd been using TFT, I would have been instantly converted to TFT. Either way, I would have become a true believer in the new technique.
improvement she experienced occurred while she was sitting safely in the lecture hall. To be of value, the improvement during cognitive flooding will have to translate to the real situation.
Chapter 6
193
I call this type of clinical illusion "Coupling." You couple your favorite new technique with a powerful, empirically validated technique like exposure. Then you can attribute the improvement you observe to the new technique, and presto, you have a new school of therapy you can market. Coupling is similar to the placebo effect, but there's an important difference. When we're fooled by the placebo effect, we attribute the patient's improvement to the specific methods we used, but the patient's improvement actually resulted from non-specific factors, such as hope, empathy, or the passage of time. When we're fooled by the Coupling effect, we pair a new technique with an older, well-established technique with a proven track record. Then we attribute the improvement to our new technique, rather than to the established technique we coupled it with. The Confirmation Paradox You can disprove a theory, but you can never prove that a theory is correct. This is one of the classic problems in the philosophy of science. For example, let's say that theory X predicts outcome Y, and you observe outcome Y. Does this mean that you've confirmed theory X? Unfortunately, you haven't confirmed that theory X is valid, because an indefinite number of competing theories would have made the same exact prediction. So you're really confirming an infinite number of theories at the same time. This may sound overly abstract, but it has practical implications. For example, many therapists believe that growing up in an unloving household
Chapter 6
194
causes perfectionism and low self-esteem, particularly if the parents push the child to achieve, achieve, achieve. We can call this theory X. Let's say your patient, Luke, is very perfectionistic and suffers from low self-esteem. He's relentlessly self-critical and believes that he must impress people with his achievements in order to be loved and accepted. This is outcome Y. In this case, theory X has predicted outcome Y, and we've observed outcome Y. Can we conclude that theory X is correct? In other words, can we safely assume that Luke experienced a lack of love and acceptance as a child, and that the pressures from his parents to achieve triggered his perfectionism and low self-esteem? Not really. Scientists don’t yet know the cause of perfectionism or low selfesteem, and a large number of competing theories would have led to the same prediction. For example, Luke's problems could be entirely genetic, entirely learned, or some combination of the two. The good news is that we have powerful methods to help Luke overcome his perfectionism and develop better self-esteem, but we should be very cautious about assuming that we know how or why any patient's emotional problems developed. Although a positive result cannot confirm a theory, a negative result can prove that a theory is wrong. If theory X predicts outcome Y, but outcome Y is not observed, then we can conclude that theory X is probably not valid. That's why negative studies are so important in any field of science. In fact, Einstein's Theory of Relativity was the direct result of a study that didn't pan out. Unfortunately, clinicians and researchers in the behavioral sciences don't
Chapter 6
195
like negative outcomes. When a study doesn't come out in the "right" way, researchers feel like they've failed. Journal editors and reviewers are reluctant to publish papers with negative results, even when the studies were carefully conducted and honestly reported. Similarly, as clinicians, we feel threatened when our clinical experience doesn't seem to support our theories and methods, or when patients fail to respond to our favorite techniques. But in fact, these "failures" present us with unique opportunities to refine our thinking about the causes of emotional problems. In this chapter, we've reviewed many ways that we fool ourselves into thinking we know more than we do. The bottom line is this: seeing is not always believing, and our most cherished beliefs may not be valid. Is there a solution to the Clinician's Illusion? Part of the answer might be to provide more courses on critical thinking and research methodology in psychotherapy training programs, including psychiatric residency training. In addition, I'm convinced that the use of simple assessment instruments can help us see more clearly what's really going on with our patients, so we don't continue to operate on false perceptions. For example, you've seen how the Brief Mood Survey and Evaluation of Therapy Session revolutionized the treatment of a woman named Evie who'd been severely depressed and stuck for nearly 15 years. I believe that instruments like these can transform our clinical work and help us move toward a true science of human behavior. We'll review these tools in the next chapter.
7*
How to Track Therapeutic Progress and Monitor the Therapeutic Alliance
In my workshops for mental health professionals, I sometimes ask this question: "How many of you require your patients to take at least one psychological test between every therapy session?" Usually, only two or three hands go up, even in a group of 200 therapists. Then I ask this question: "If you had pneumonia, how many of you would go to an internist who didn't believe in the use of the thermometer, x-rays, or blood tests?" No hands go up. I point out that most of us are operating on a double standard. When we go to the doctor, we demand scientific treatment based on laboratory testing. But when we're the doctors, we fly by the seat of our pants and rely on our own subjective impressions. In the old days, before reliable, user-friendly assessment instruments were available, this position was probably justified. But in this era, I don't think it's * Copyright
2003 by David D. Burns, M.D.
Chapter 7
Page 197
ethical to treat patients without session-by-session assessments. It doesn't make much sense from a practical perspective, either, because our clinical impressions are often misleading. I once treated a woman named Alice who worked for the CBS television station in Philadelphia. Although she was happily married and doing well at work, Alice was severely depressed. At the time, I was using the Beck Depression Inventory (BDI), and Alice's score at intake was 42, indicating extremely severe depression.* This was surprising, since Alice seemed chipper and happy, and had a good sense of humor. Most patients with scores this high are hospitalized and look totally down and out. Alice and I had a positive therapeutic alliance, and she seemed to appreciate my efforts. She was very perfectionistic, and we worked hard on this problem using a variety of cognitive techniques. She always did her psychotherapy homework on the computer, and brought elegantly formatted printouts of her negative thoughts, and her attempts to challenge them, to every session. She appeared to be making tremendous progress. At the start of the eighth therapy session, I asked Alice to give me her honest assessment of how we were doing so far. Did she have any negative or positive feelings about the treatment? She said she loved the therapy and that it was exactly what she needed. She looked great and seemed to be radiating feelings of self-esteem. I felt a sense of pride and thought, "Alice is just the type of person I should present in workshops, because she's made so much progress
Chapter 7
Page 198
so quickly, even though she was so severely depressed at intake." I asked her to fill out the BDI so I could find out how much she'd improved so far. I wondered if her score might have fallen all the way to zero, which would indicate a complete elimination of her symptoms. But when she handed me the completed test, I was shocked to see that her score was 46, indicating almost unbelievably severe depression. This score was actually 4 points worse than her score at intake. I said: "Alice, I'm glad you like the therapy, and I've enjoyed working with you as well. However, the purpose of the therapy is not just to learn how to talk back to your negative thoughts, but to change how you feel at the gut level. Your score on the BDI indicates that you're still suffering terribly. I'm concerned that I've overlooked something important, and that maybe we haven't really focused in on the right problem yet." Alice hung her head and looked profoundly sad for the first time. After a long silence, she quietly said that maybe she needed to tell me something that she'd never told anyone before, including her husband. She hesitantly explained that when she was a little girl, her parents fought constantly. She was terrified by all the screaming and yelling, and would run and hide in her bedroom. Then her parents would charge into the bedroom, still screaming at each other, and her father would pick her up and throw her against the wall. After she fell to the floor, he'd pick her up again and throw her against another wall.
* Scores on the BDI range from 0 (no depression) to 63 (the worst possible depression). Scores above 30 indicate severe depression. Scores above 40 indicate extremely severe depression.
Chapter 7
Page 199
As she spoke, she began sobbing. She no longer looked like the happy and chipper person she'd appeared to be just a few minutes earlier. She told me about all the feelings of fear, anger, shame, and humiliation she'd been hiding for so many years. Then she told me she was afraid she'd been disloyal to her parents by revealing a family secret. Over the next several weeks, Alice and I worked together using the same kinds of CBT techniques we'd been using all along, but the therapy had a completely different quality to it. Within two weeks, her BDI score had fallen all the way to 12, and the following week, it had fallen all the way to 3. She said she was feeling truly happy and worthwhile for the first time in her life. Alice is a perfect example of how misleading our clinical impressions can be, and how a simple assessment instrument can radically change your understanding of your patient. If I hadn't been using the BDI, I would have believed I was doing a terrific job with someone who hadn't been helped at all.
Insert the two-page Brief Mood Survey and Evaluation of Therapy Session about here. It will require two full book pages.
Over the years, I began to notice some problems with the BDI, and decided to develop and validate several user-friendly self-assessment tests, such as the Brief Mood Survey on page 202. This instrument assesses depression, suicidal urges, anxiety, and anger, as well as relationship satisfaction, with a surprising degree of accuracy. The Evaluation of Therapy Session on page 203 assesses the patient's perceptions of therapeutic empathy as well as the helpfulness of their most recent session. Patients can also indicate what they
Chapter 7
Page 200
liked the least and the most about the session. The scoring keys for the Brief Mood Survey and Evaluation of Therapy Session appear on pages 204 – 205.
Insert scoring key for Brief Mood Survey about here
I like to photocopy the Brief Mood Survey and Evaluation of Therapy Session on two sides of a single sheet of paper, and I require all my patients to complete these tests on their own between sessions. * Most patients can easily complete them in five minutes or less. When patients hand their completed tests to me at the beginning of the next session, I record their scores on a flow sheet at the front of the chart. This requires less than one minute of therapy time, and allows me to track even the smallest fluctuations in their symptoms with a high degree of accuracy. I can also see exactly how they feel about me, and whether or not the therapy seems helpful and relevant to their problems. The young man who filled out the test on page 202 was an electrical engineering graduate student named Jonathan who was receiving outpatient treatment at Stanford for a major depressive episode. His score of 13 on the Depression scale indicated that he was feeling moderately depressed. His score the previous week had been 12, indicating that he was feeling a tad worse. He scored 2 on the first item on the Suicidal Urges scale, indicating some suicidal thoughts. Most depressed patients have occasional thoughts of death or suicide. This is not dangerous per se. However, if a patient scores 1 or higher on
* If you'd like to obtain a license for unlimited reproduction of these and many other tools in your clinical practice, you can obtain further information along with an order form for the Therapist's Toolkit by sending an email to [email protected].
Chapter 7
Page 201
the second item on the Suicidal Urges scale ("Would you like to end your life?"), you should explore the problem immediately. The patient may be contemplating a suicide attempt, and your intervention could be lifesaving. Jonathan's score of 0 on this item indicated that he was not feeling actively suicidal. Although he felt hopeless and desperate at times, he said that he would never consider a suicide attempt because it went against his religious beliefs and would devastate his family. In addition, he believed that he'd eventually recover because he'd recovered from a similar episode of depression when he was in high school. Jonathan's score of 11 on the Anxiety scale indicates that his anxiety is almost as strong as his depression. This is not unusual. Most depressed individuals experience some anxiety, and most patients who seek treatment for anxiety disorders will also report some feelings of depression. Jonathan's score of 16 on the Anger scale is interesting, since his anger appears to be even more intense than his depression. Freud believed that depression was actually "anger turned inwards." Although that theory is controversial, there's no doubt that anger and depression often go hand-in-hand. If you ask your patients about their angry feelings, it will give you a much better picture of what's bothering them. Of course, if they're angry with you, and you don’t address the problem, they may drop out of therapy.
1. 2. 3. 4. 5.
4—Extremely
Depression
3—A lot
Instructions. Use checks ( ) to indicate how you've been feeling over the past week, including today. Please answer all the items.
2—Moderately
Brief Mood Survey*
1—Somewhat
Date: 0—Not at all
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem Worthless or inadequate Loss of pleasure or satisfaction in life Total
13
Total
2
Total
11
Total
16
Suicidal Urges
1. 2.
Do you have any suicidal thoughts? Would you like to end your life? Anxiety
1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated
Relationship Satisfaction*
Dissatisfied
Satisfied
Total
* Copyright © 1997 by David D. Burns, M.D. Revised, 2004.
6–Very
5–Moderately
4–Somewhat
3–Neutral
2–Somewhat
1–Moderately
Use checks ( ) to indicate how satisfied or dissatisfied you feel about this relationship. Please answer all five items. 1. Communication and openness 2. Resolving conflicts and arguments 3. Degree of affection and caring 4. Intimacy and closeness 5. Overall satisfaction
0–Very
Put the name of someone you care about here:
8
1. 2. 3. 4. 5.
Therapeutic Empathy My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside.
1. 2. 3. 4. 5.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems.
1. 2.
Satisfaction with Today's Session I believe the session was helpful to me. Overall, I was satisfied with today's session.
1. 2.
4–Completely true
3–Very true
Instructions. Use checks ( ) to indicate how you felt about your most recent therapy session. Please answer all the items.
2–Moderately true
Evaluation of Therapy Session*
1–Somewhat true
Page 203 0–Not at all true
Chapter 7
Total
18
Total
13
Total
6
Total
5
Total
3
Total
4
Your Commitment I plan to do therapy homework before the next session. I intend to use what I learned in today's session.
1. 2. 3.
Negative Feelings During the Session At times, my therapist didn't seem to understand how I felt. At times, I felt uncomfortable during the session. I didn't always agree with my therapist.
1. 2. 3.
Difficulties with the Questions It was hard to answer some of these questions honestly. Sometimes my answers didn't show how I really felt inside. It would be too upsetting for me to criticize my therapist.
What did you like the least about the session?
What did you like the most about the session?
* Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
Chapter 7
Page 204 Scoring Key: Brief Mood Survey
Score
5–Item Depression, Anxiety, and Anger Tests
0-1
Few or no symptoms: the best possible score
2-4
Borderline symptoms
5-9
Mild symptoms
10 - 14
Moderate symptoms
15 - 17
Severe symptoms
18 - 20
Extreme symptoms
2–Item Suicidal Urges Test* Item 1
Elevated scores on this item are not unusual. Most depressed patients have some suicidal thoughts or fantasies at times.
Item 2
Here, any elevated score is dangerous. This item assesses suicidal urges. You will need to do a careful suicide assessment, and may need to hospitalize the patient if he or she seems to be in danger of making a suicide attempt.
Score
5–Item Relationship Satisfaction Test (RSAT)
0-5
Extremely dissatisfied
6 - 10
Moderately dissatisfied
11 - 14
Somewhat dissatisfied
15 - 18
Neutral
19 - 22
Slightly satisfied
23 - 26
Moderately satisfied
27 - 28
Very satisfied
29 - 30
Extremely satisfied
* I've also created a brief structured interview that can assist in your evaluation of patients with suicidal urges. We'll discuss it in Chapter 10.
Chapter 7
Page 205 Scoring Key: Evaluation of Therapy Session Therapeutic Empathy (Items 1 – 5)
Score
Interpretation
20
Outstanding! An excellent job!
19
There's a problem that should be explored.
17 - 18
Fair, but there's considerable room for improvement.
15 - 16
Poor. The patient doesn't feel supported or understood.
11 - 14
Warning! This patient is very dissatisfied.
0 - 10
Extreme problems with the therapeutic alliance. Call your attorney!
Note: You don't need to interpret the total scores on the following scales, but you may wish to track changes in the scores over time. Scale
Interpretation The patient's responses will indicate how helpful the session was. Ask the patient which techniques were the most and least helpful.
Helpfulness of the Session
Satisfaction with Today's Session
Toward the beginning of therapy, your scores on this scale will probably indicate that your interventions are only somewhat or moderately helpful. Once you develop a collaborative relationship, and the patient begins to improve, your scores will increase. However, it will be easier to get perfect scores on the Therapeutic Empathy scale than on the Helpfulness scale. The responses will show how satisfied or dissatisfied the patient felt about the session.
Your Commitment
The responses will indicate whether the patient intends to do psychotherapy homework and whether the session will have an impact on his or her life.
Negative Feelings During the Session
Any score of 1 ("Somewhat true") or above on this scale indicates that the patient had some negative feelings during the session. You can explore these feelings using the Five Secrets of Effective Communication.
Difficulties with the Questions
Any score of 1 ("Somewhat true") or above on this scale indicates that the patient had trouble answering some of the items honestly. If you ask which items they had trouble with, most patients will tell you! If they had trouble answering the questions about suicidal urges honestly, you'll need to do a careful suicide assessment immediately. An emergency intervention, such as hospitalization, may save the patient's life.
Chapter 7
Page 206
You can also ask if they have any violent fantasies or urges to hurt anyone. Most of the time, the answer will be no. However, on rare occasions, angry individuals do become violent. If you ask about any violent feelings, your intervention could prevent a catastrophic event. Jonathan was extremely upset with his wife and fearful about the future of his marriage. His low score on the Relationship Satisfaction scale confirmed that there were significant marital problems, and it turned out that the conflict with his wife was fueling his depression, anxiety, and anger. Although Jonathan sought treatment for his depression, he was suffering in many ways. The Brief Mood Survey will provide you with a much broader picture of how the patient feels, and how those feelings change from session to session. That way, you won't simply focus on the presenting complaint, such as depression, like a horse with blinders on. You'll notice that the instructions at the top of the Brief Mood Survey ask patients to indicate how they've been feeling "over the past week, including today." This version of the Brief Mood Survey is suitable for once a week outpatient therapy. Patients can fill out this form on their own between sessions, and give it to you at the start of the next session. If you record the scores on a flow sheet in your chart, one glance will give you a bird's-eye view of all the fluctuations in the patient's feelings since the initial evaluation, and you'll be able to track therapeutic progress in several dimensions with great accuracy. If you use the Brief Mood Survey regularly with all your patients, you'll be light years ahead of your colleagues, and you'll have a crystal-clear, accurate understanding
Chapter 7
Page 207
of how much progress each patient is making. I've recently created a new version of the Brief Mood Survey that I'm quite excited about. As you can see on page 208, patients indicate how they're feeling "right now," rather than "over the past week." In addition, there are two separate response regions marked "Before Session" and "After Session." We photocopy the Evaluation of Therapy Session on the back of the new Brief Mood Survey, just as we did with the older version. Here's how it works. We ask patients to make copies of the new Brief Mood Survey and Evaluation of Therapy Session for their personal use, and to bring a blank copy to each session. They come to each session five minutes early and fill out the "Before Session" ratings in the waiting room, based on how they're feeling at that moment. They hand us the Brief Mood Survey at the start of the session so we can copy the "Before Session" scores on the flow sheet in the patient's chart and discuss any changes in their scores from the previous week. At the end of the session, we hand the partially completed Brief Mood Survey back to the patient and ask them to fill it out again in the waiting room before they go home, using the "After Session" answer section, based on how they're feeling at that moment. They also complete the Evaluation of Therapy Session form on the back, while the session is still fresh in their mind. They leave the completed tests with the receptionist so we can review their scores while the session is still fresh in our minds, and record the "After Session" scores in the flow sheet in your chart.
Name:
Date:
1. 2. 3. 4. 5.
How depressed do you feel right now? Sad or down in the dumps Discouraged or hopeless Low self-esteem Worthless or inadequate Loss of pleasure or satisfaction in life
After Session
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Instructions. Use checks ( ) to indicate how you're feeling right now. Please answer all the items.
Before Session
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Brief Mood Survey*
Total
15
Total
3
Total
2
Total
0
Total
13
Total
8
Total
8
Total
3
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life?
How anxious do you feel right now? 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous
How angry do you feel right now? Frustrated Annoyed Resentful Angry Irritated
Total
* Copyright
17
2004 by David D. Burns, M.D.
Total
6—Very Satisfied
5—Moderately Satisfied
4—Somewhat Satisfied
3—Neutral
2—Somewhat Dissatisfied
1—Moderately Dissatisfied
0—Very Dissatisfied
6—Very Satisfied
After Session 5—Moderately Satisfied
4—Somewhat Satisfied
Please answer all five items. 1. Communication and openness 2. Resolving conflicts and arguments 3. Degree of affection and caring 4. Intimacy and closeness 5. Overall satisfaction
1—Moderately Dissatisfied
Use checks ( ) to indicate how satisfied or dissatisfied you feel about this relationship.
0—Very Dissatisfied
Put the name of someone you care about here:
3—Neutral
Before Session
Relationship Satisfaction*
2—Somewhat Dissatisfied
1. 2. 3. 4. 5.
17
Chapter 7
209
This procedure requires almost no therapy time, but will provide you with accurate information about: Mood changes during sessions. Each therapy session will be sandwiched between two here-and-now assessments of how depressed, anxious and angry the patient feels. The changes in the scores will indicate whether the patient improved, stayed the same, or got worse during the session. You can see on page 208 that this patient's depression score fell from 15 at the start of the session, indicating severe depression, to 3 at the end. This degree of improvement in one 45-minute session is remarkable, and is comparable to, or better than, the degree of improvement in 12 – 15 weeks of treatment with antidepressant medications or psychotherapy in the most favorable studies ever published in the world literature. This patient also reported impressive reductions in his suicidal feelings, anxiety, and anger. However, there was no improvement in his marital satisfaction score. The Brief Mood Survey on page 208 was from a session one of my students conducted recently. He was excited when he saw how much the patient had improved from the beginning to the end of the session. Obviously, he'll want to ask the patient which techniques or ideas were the most helpful, so they can do more of the same at the next session. Most of us became mental health professionals because we wanted to help people. It can be extremely rewarding to help someone change their life. But most of us don’t know when this is happening, or whether it's happening at all, because our perceptions of our patients' feelings are woefully
Chapter 7
210
inaccurate. This new version of the Brief Mood Survey allows you to see exactly how effective you are at every single session. Of course, if there isn't any change in the mood scores, it's important to know that as well. You can discuss this with the patient at the next session and try a different approach. This will prevent you from getting stuck in a rut and will keep the therapy moving in a positive direction. Mood changes between sessions. When you compare the After Session mood ratings from the previous week with the Before Session mood ratings from today's session, you'll see exactly what happens to your patients when they're not with you. Did they get better during the session and relapse after they got home? If so, what triggered the increase in depression, anxiety, or anger? Alternatively, did they improve further after the last session? If so, why? Was it because of the psychotherapy homework they were doing? Or something else that happened? One glance at the flow sheet in the patient's chart will show you every change in the patient's mood in multiple dimensions since the first time you met. This information has never before been available to therapists. For example, when do patients improve? Do they improve when they're with us, or when they're not with us? Do they improve suddenly, or gradually? What are the factors that facilitate rapid recovery? Or therapeutic failure? The answers to these basic questions will have tremendous clinical and research importance. Now I'm going to give you an exercise that will provide you with a deeper understanding of how the Evaluation of Therapy Session would work in a clinical
Chapter 7
211
setting. The first scale assesses Therapeutic Empathy. Patients indicate how warm, trustworthy, and understanding you were during the most recent session, with response options ranging from "Not at all true" (scored 0) to "Completely true" (scored 4). Let's assume that you received the Evaluation of Therapy Session on page 203. You can see that your ratings on the Therapeutic Empathy scale were 3, 4, 4, 4, and 3. In other words, your patient checked "Very true" or "Completely true" for all five items, so your total score was 18 out of 20. Keep in mind that a perfect score on this test would be 20. What would you think if you received a score of 18? How would you assess the quality of the therapeutic alliance with this patient? Please write your answer here:
Don't turn the page until you've written something!
Chapter 7
212
Answer When I ask this question in workshops, most therapists say, "Oh, that's a great score. It indicates an excellent therapeutic alliance." Is that what you thought? Most therapists would be pleased with a score of 18 out of 20. Others are concerned that the patient may simply be telling you what you want to hear. There's some evidence for this. Look at the Difficulties with the Questions section at the bottom of the form. This patient is admitting that it was hard to answer some of the questions honestly, that some answers did not reflect how he was really feeling inside, and that it would be hard to criticize you. You should interpret all his scores with this in mind, because he probably softened his responses on certain items out of a sense of politeness or because he typically avoids conflict. So what do his responses on the Therapeutic Empathy scale really mean? He rated items 2, 3, and 4 as "Completely true." This means he thought that you were completely trustworthy, treated him with respect, and did a good job of listening to what he said. However, he only rated items 1 and 5 as "Very true." These items assess how warm and caring you were, and how well you understood how he was feeling inside. Ask yourself, "Why did he mark me down on these two items?" He's really telling you that you didn't seem completely warm, supportive, or concerned during the session. In addition, he didn't think you always understood how he was feeling. In other words, a score of 18 is actually a poor score on this test. In fact,
Chapter 7
213
any score below 20 indicates a significant failure in the therapeutic alliance that needs to be explored. You won't know how serious the failure is until you discuss the problem with the patient. What would happen if you weren't aware of this problem and didn't process these concerns with him? His feelings of dissatisfaction would probably increase and sabotage your efforts. He'd continue to feel that you weren't particularly warm or caring, and that you didn't really understand him. However, the odds are overwhelming that he won't be assertive enough to tell you. And when negative feelings aren't expressed and resolved, they have a way of eating away at people and getting worse. That's about as basic as the law of gravity. Now, let's suppose that you weren't using this form and you simply asked him, "How are we doing?" What would he tell you? He'd say, "Oh, just fine, doctor." Now, let's imagine that you said, "If there were a problem, would you tell me?" He'd say, "Oh, certainly doctor." So you'd never find out. It's the same as when you're in a restaurant and the food isn't very good. When the waiter says, "How was everything?" you say, "fine," because you don't want to hurt his feelings. That's why the written evaluations will provide you with far more accurate information about how your patients feel about you. Most patients will be extremely reluctant to criticize you verbally, but they're very willing to mark you down on paper.
Chapter 7
214
When therapists first see the Evaluation of Therapy Session, many of them have the thought, "Oh, I wouldn't want to use that form because my patients will just tell me what they think I want to hear." This is not a valid concern! When my psychiatric residents and psychology students use the Evaluation of Therapy Session for the first time, most get failing grades from every patient at every session. This is also true of seasoned clinicians. When they use the Evaluation of Therapy Session with their patients for the first time, most of them are surprised to discover that they also get failing grades from every patient at every session. So the real problem with the Evaluation of Therapy Session is not that our patients will tell us what we want to hear, but what we don't want to hear! This can be bruising to the ego. A clinical social worker from Harrisburg, Pennsylvania told me that she received failing grades from her patients about half of the time when she first started using the Evaluation of Therapy Session. Those are about the best scores that any student or seasoned clinician has ever received initially. After using the Evaluation of Therapy Session and processing her patients' responses for several weeks, she began to receive perfect scores about 80% of the time. This degree of improvement is typical of most of the clinicians who've used the form consistently and worked to improve their interpersonal skills using the techniques I'll describe in Part IV of this book. You wouldn't want to get perfect scores more than 80% of the time, because some friction and confrontation is an inherent part of good therapy. It can be upsetting to discover that we're missing the mark with so many
Chapter 7
215
people, especially when we had the idea that we were reasonably sensitive and compassionate. However, if you keep your ego out of the picture, the information you receive can be invaluable. In an earlier version of the Evaluation of Therapy Session, "Very true" was the highest possible category. This created a ceiling effect. Therapists often received "perfect" scores when there were significant problems in the therapeutic alliance. This difficulty has been corrected in the current version of the test. Patients don't mind using the category, "Very true," to indicate a therapeutic problem, because it allows them to hint at the difficulty without having to insult you. Patients can condemn you through faint praise, so to speak. As a result, the test is sensitive to even the tiniest failures in the therapeutic alliance. When I first started using the Evaluation of Therapy Session, I also received failing grades from many of my patients. This was painful. I experienced considerable shame and embarrassment. I also felt annoyed, because I often received the lowest ratings from the patients I was trying the hardest with. It seemed unfair. But eventually, I got so many poor scores that it stopped bothering me. I developed thicker skin, like emotional asbestos. When I stopped fearing these criticisms, and began to explore them with my patients, something odd happened. These discussions began to lead to meaningful therapeutic breakthroughs. My empathy scores increased dramatically, and I began to look forward to low ratings instead of dreading them. Many of my best therapy sessions have been when I processed this kind of feedback with my patients.
Chapter 7
216
That's when we hit the real home runs. Your sensitivity and empathy will increase quickly if you use assessment instruments like the Brief Mood Survey and Evaluation of Therapy Session with all your patients at every therapy session. In Part IV, I'll show you how to respond effectively to virtually any critical comment a patient or colleague might make. Of course, effective therapy involves far more than just empathic listening. Patients have problems they need to resolve. This will require the skillful use of specific therapeutic techniques, and hard work on the part of therapist and patient alike. The five items on the Helpfulness of the Session scale will show you how effective your therapeutic interventions are. Once again, your patient's perceptions will often be radically different from your own. The man who filled out the test on page 203 indicated that he didn't get the chance to talk about the feelings that were bothering him during the session. At the same time, he thought that the therapist's techniques and approach were moderately helpful, and that he learned some new techniques to deal with his problems. However, his responses indicate that there's room for improvement. This may explain his less than stellar ratings on the Satisfaction and Commitment scales. The Negative Feelings During the Session scale can be an eye-opener. Many patients do not acknowledge negative feelings that surface during the session, especially if they feel angry, frustrated, intimidated, bored, or turned off by something you said. It can be hard for them to tell you directly, but they'll let you know when they fill out the scale.
Chapter 7
217
We've already discussed the last scale, called Difficulties with the Questions. If the patient scores 1 or above on any of these items, ask which items on the Brief Mood Survey or Evaluation of Therapy Session they had the most trouble with. If you do this in a friendly, respectful way, patients will nearly always tell you. For example, the patient may have minimized the intensity of suicidal urges for fear that you'd hospitalize him. So in some cases, this information can be life-saving. You can also ask if they felt concerned about hurting your feelings when they filled out the Evaluation of Therapy Session. This can open the door for a discussion of their fantasies about what might happen if they did criticize you. For example, they may have the fear that you'd get upset and reject them. The avoidance of conflict may be a pervasive problem for the patient. At the bottom of the Evaluation of Therapy Session, patients can let you what they liked the least and the most about the session. Their perceptions will often be very different from your own understanding of the session, and the discussion of these feelings can be invaluable. I once treated an intensely depressed social worker named Yvette who'd been depressed for years, and had worked with several therapists prior to seeing me. She commuted a great distance for sessions, so I scheduled her for double sessions every other week. That way, she wouldn't have to spend so much time commuting. Yvette was very intelligent, but seemed judgmental. I was aware that she could be critical of herself and others, and I felt intimidated by her. I tried
Chapter 7
218
numerous CBT techniques but nothing seemed to help. Every week, her scores on the Brief Mood Survey indicated that she was feeling just as depressed and angry as the first day she came to see me. One day, I noticed that Yvette had given me low empathy ratings for our previous session. When I asked about her feelings, she took the opportunity to rip me to shreds. Her bitter diatribe continued for the entire, two-hour session. I was embarrassed and felt like I was letting down a horribly depressed colleague who desperately needed my help. Furthermore, she was very perceptive, and most of her criticisms seemed valid. I felt like a bug, pinned and wriggling on the wall. At the end of the session, I didn't bother to schedule another therapy session because it seemed clear that she wouldn't want to continue working with me. I received a letter from Yvette two days later. It came by overnight mail and I had to sign for it. I was gripped by a sense of panic, thinking that she might have filed an ethics complaint or a lawsuit because of my inept treatment. As I opened it, I braced for more criticism. I was taken aback when I read the letter. Yvette said that our last session had been by far the best one we'd ever had. She said that as she walked to the train station after the session, her depression suddenly lifted and she began to experience her first real feelings of happiness in over 20 years. Yvette explained that she'd been angry at the world for years, and that I was the first person who'd cared enough to listen. In her letter, she included a completed copy of the Brief Mood Survey and
Chapter 7
219
Evaluation of Therapy Session. Her depression score was nearly zero for the first time, and she'd given me perfect ratings on the Therapeutic Empathy and Helpfulness scales. She added that she'd felt so relieved at the end of the session that she'd completely forgotten to schedule her next session, and wanted to know if she could come back in one week rather than two because she was so excited about the progress we were making. I was flabbergasted. My perceptions had been totally off base. And yet, I'm convinced that this phenomenon occurs in varying degrees in practically every therapy session with every therapist, regardless of gender, therapeutic orientation or experience. Here's a simple experiment you can do to test this idea. Ask several patients to fill out the Brief Mood Survey and Evaluation of Therapy Session in the waiting room after their sessions and leave them for you. At the same time, you can fill out the same scales, guessing how the patient will fill them out. When you're done, compare the patient's answers with your own. Therapists who have done this experiment have been shocked to discover almost unbelievable discrepancies between how they think their patients feel and how their patients actually do feel. You may be convinced that a patient isn't depressed, anxious or angry when they're extremely depressed, anxious or angry, or vice versa. You may feel that you came across in a warm, empathic way, only to discover that your patient didn't feel cared about or understood during the session. Or, as in Yvette's case, you may think that you did a poor job, only to discover that the patient has given you excellent ratings. If you keep your
Chapter 7
220
ego out of the picture, this information can be illuminating. At the start of a recent cognitive therapy group at the Stanford Hospital, a woman named Missy reported moderate levels of depression, anxiety, and anger on the Brief Mood Survey. During the group, I helped her challenge her negative, self-critical thoughts using a variety of CBT techniques. It seemed like we really clicked, and I couldn't wait to look at her Brief Mood Survey and Evaluation of Therapy Session at the end. I was surprised to see that Missy put 4's on every item on the Depression, Anxiety, and Anger scales. These ratings indicated that she was feeling much worse—in fact, horrible—at the end of the session. I was even more surprised to see that she put 0's on all the items on the Therapeutic Empathy and Helpfulness scales. I'd never seen scores nearly that bad before! I was sure that Missy had made a mistake. I ran out into the hall and asked her to come back into the group therapy room for a moment. I said, "Missy, I'm wondering if you'd be kind enough to review your answers on the assessment instruments, just to make sure that you didn't make a mistake when you filled them out. You see, on the mood tests, the good answers are on the left, and on the Evaluation of Therapy Session, the good answers are on the right." Missy glanced at the test and said, "I don't think there are any mistakes here, Doctor." I said, "But I thought we just had a really good session." She scowled and said, "Good for you, maybe!"
Chapter 7
221
I asked Missy what she meant. She explained that I'd said something during the session that had really hurt her feelings. It dawned on me that I'd made a comment that sounded judgmental and cutting. She'd been feeling devastated, but had covered up her feelings. Missy and I sat down and had a good meeting of the minds that cleared the air. If I hadn't been using the assessment tests, I would have wrongly concluded that I'd done a great job and that the group had been extremely helpful for Missy. At the start of the next cognitive therapy group, I noticed that a newly admitted patient named Rose had also scored 4s on every item on the Depression, Anxiety and Anger scales. She explained that she'd just been hospitalized on our locked unit for a nearly successful suicide attempt, and defiantly announced that she intended to complete the job at the first chance she got. She explained that she'd been treated for Borderline Personality Disorder and depression for many years, but still felt horrible every minute of every day. She said that she'd also struggled with a crack cocaine habit for years, and was living in a recovery house in San Francisco. She'd been clean and sober for several months, but had slipped up and used crack again following an argument with her roommate. The staff threatened to kick her out of the facility, so she tried to kill herself. She said she felt utterly worthless and hopeless, and had decided it was time to face the facts about her life and cash it in. I asked how many of the other patients in the group felt worthless and
Chapter 7
222
hopeless at times. Every hand went up. I said that these were feelings that everyone could identify with, and asked Rose if she'd like to work on them during the group. She practically bit my hand off. She said I sounded like every other stupid f___ing shrink she'd ever wasted time with and loudly announced that she had no interest in any of my f___ing goddamned help. I felt about two inches tall and thought, "Mmmm. Maybe Rose isn't going to be the best person to work with during today's group." I backed off and decided to work with a woman on the other side of the room who also felt hopeless and worthless. Rose didn't utter another word the entire time. I was afraid to look in her direction but could sense that she was staring at me with daggers in her eyes. We had a reasonably productive group, but I dreaded having to look at Rose's Brief Mood Survey and Evaluation of Therapy Session at the end. I was puzzled when I saw that all her scores on the Depression, Anxiety and Anger scales had fallen to zero, and that she no longer felt suicidal. It was as if all her negative feelings had vanished. I was even more surprised to see that she'd given me perfect scores on the Therapeutic Empathy and the Helpfulness scales. She indicated that I'd been completely warm, understanding, and trustworthy, and that the session had been incredibly helpful. At the bottom, where patients describe what they liked the least about the session, Rose had simply written, "Nothing." In the section where patients describe what they liked the most about the session, she wrote: "Doctor Burns, when you worked with that other woman, I felt like
Chapter 7
223
you were working with me. Her feelings were just like mine. I've never had any cognitive therapy before, but now I can see how distorted and unfair my negative thoughts are. I've never even thought about this before, because I always thought the problem was that I really was worthless. I can hardly believe it, but I'm suddenly feeling real selfesteem. In fact, I think this is the first happiness I've experienced since I was a child. Thank you so much! The last hour and a half has changed my life." If I hadn't been using the tests, I would have had no idea that the group had been so helpful to her, and probably would have gone out of my way to avoid her in the future. If you have the courage to use these kinds of assessment tools regularly, you may also be in for some surprises. The instruments that I've developed may or may not be suitable for your clinical practice, and there are lots of assessment tools currently competing in the marketplace. I'd strongly encourage you to select at least one or two that you like and start to use them regularly. It's not easy at first, but over time, your sensitivity and effectiveness will increase considerably. And you may discover, as I have, that your patients are really the best teachers you've ever had!
8*
Suicide Assessment and Prevention
Experts tell us that as many as 10% of chronically depressed patients eventually commit suicide, even if they're receiving treatment. I'm convinced that the vast majority of suicide attempts can be prevented--but it may require a slight shift in how you usually approach the problem. You'll notice that the Brief Mood Survey on page 208 includes two suicidescreening items along with a five-item depression scale. If you require all your patients to complete the survey at the beginning and end of every therapy session, you'll know the moment that they develop any suicidal urges. Then you can evaluate these feelings and take any steps that may be necessary to prevent a suicide attempt, such as hospitalization. Even if the patient wasn't suicidal at the start of the session, there could be an upsurge in suicidal feelings during the session because you touched on a sensitive topic. But the patient may not verbalize those feelings, and you
* Copyright
2003 by David D. Burns, M.D.
Chapter 8
225
probably didn't ask. When you review the patient's response on the Brief Mood Survey following the session, you'll immediately spot any increase in suicidal feelings. If necessary, you can get on the phone and contact the patient immediately. This is rare, but it can occur, and your intervention could save the patient's life. An attorney told me that he had to defend a psychiatrist in a malpractice suit. Apparently, the patient committed suicide several hours after his therapy session, so the family sued. When the attorney was reviewing the chart, he discovered that the patient had filled out the 15-item version of the Burns Depression Checklist the day that he committed suicide, and indicated that he had no suicidal fantasies or urges at the time. The attorney showed the test to the judge, who ruled that one of two things must have happened. Either the patient intentionally deceived the psychiatrist, or something upsetting happened immediately after the session that triggered the suicide attempt. The judge ruled that patients have the right to fool their psychiatrists, but when they do, psychiatrists cannot be held responsible for the patient's death. The judge threw the case out of court. Most patients are honest when they fill out the Depression test and Suicidal Urges scale, and these instruments can prevent many needless tragedies. But even if the tests fail to protect the patient, because of willful deception, they may still protect you. Make sure you record the patient's scores on these tests in the chart, and document your thinking in case there's an emergency. When in doubt, obtain a consultation from a colleague and document
Chapter 8
226
the consultation in the chart. You can see the Suicide Assessment Interview I've developed on pages 229 – 231. It takes about 15 minutes and is well worth the time. If you have any doubts about the patient, the interview could be life saving. I keep photocopies available in my office so I can grab one and fill it out while I'm asking the questions. It helps me clinically, because it reminds me of the most important questions to ask. I put the completed form in the patient's chart, where it serves as documentation of the fact that I did a thorough job of assessing the patient's suicidal feelings. Remember that the questions on the interview are just general guidelines. Ultimately, you'll have to rely on your own clinical judgment whenever you assess a suicidal or homicidal patient. Any structured interview is only intended to guide you through some of the most relevant topics you'll need to explore. Pay careful attention to items #19 – #21. Patients must persuade me that they will not make a suicide attempt, no matter what, if they want to work with me as outpatients. I don't feel that it's my job to persuade them not to make a suicide attempt. It's the other way around. They have to persuade me to work with them. If they can't convince me that they're completely safe, then outpatient treatment is not indicated, because it's simply not safe. In this case, I would pursue other treatment options with the patient, such as voluntary or involuntary hospitalization. Of course, patients have to feel free to discuss suicidal or homicidal fantasies during treatment. Trust and openness are crucial to successful
Chapter 8
227
treatment, and there are many CBT techniques that can help patients overcome feelings of hopelessness, worthless, desperation, or anger. However, I can only do this kind of work if I'm convinced that the patient and I are both safe, and that we're not playing Russian roulette. I want to go home at night with peace of mind, and not worrying that the patient may do something self-destructive or violent in the middle of the night. That's why all my patients have to convince me that they will not, under any circumstances, make a suicide attempt, if they want to work with me. When you've completed the Suicide Assessment Interview, you can summarize your recommendations. When in doubt, check with a colleague who has expertise in treatment of depression and in the evaluation of patients with suicidal urges, and document your consultation in the chart. This is another form of malpractice insurance. It's my understanding that you can't be successfully sued for coming to the wrong conclusion about a patient. You can only be sued for failing to do sound, competent work. Although there's a great deal you can do to drastically reduce the probability of a suicide, you can never provide any absolute guarantees. That's why the documentation of your assessment is vitally important. It will help you clinically and legally. You'll be head and shoulders above the majority of your colleagues who do not approach this problem nearly so systematically. Although violent fantasies are not as common, they do occur. Remember that your perceptions of how patients feel won't usually be accurate. That's why assessment instruments can be so vitally important. If the patient has an
Chapter 8
228
elevated score on the Anger scale on the Brief Mood Survey, you can ask who they're mad at and determine whether they have any violent fantasies or urges to do something violent. Violent fantasies are common, and they're not usually dangerous. However, if the patient is struggling with the urge to hurt someone, then you'll have to do a thorough violence assessment and document your impressions in the chart. If the patient threatens to hurt someone, you may have to contact the authorities and warn the victim as well. If in doubt, get a consultation immediately from a colleague with expertise in the assessment of violence, and document the consultation in the chart.
Chapter 8
229 Suicide Assessment Interview*
Patient's Name
Date
Risk Factors 1.
How hopeless does the patient feel?
2.
How angry does the patient feel?
3.
How strong is the desire to die?
4.
Any previous suicidal impulses?
5.
Does the patient abuse alcohol or drugs?
6.
Any severe anxiety, panic, agitation or insomnia?
Not at all
Somewhat
Moderately
A lot
Describe any positive responses. For example, why does this patient want to die? Are the suicidal impulses hard to resist? Does the patient have any plans to make a suicide attempt? Explore substance abuse as well as severe anxiety, panic attacks, or insomnia, since these factors may increase the risk of suicide.
Protective Factors 7.
How much hope does the patient feel?
8.
How strong is the desire to live?
9.
Any deterrents to a suicide attempt?
Not at all
Somewhat
Moderately
A lot
Describe the positive and negative responses. For example, how credible are the deterrents to suicide? Can this patient convince you that they will not make a suicide attempt, no matter how desperate they feel?
* Copyright © 2004 by David D. Burns, M.D.
Chapter 8
230 Suicide Assessment (p. 2)
10. Describe any previous suicide attempts. How serious were they?
11. Have any family members, friends or relatives committed suicide?
12. When does the patient intend to commit suicide? Are there certain situations, such as being rejected or losing his or her job, which might trigger a suicide attempt?
13. Has the patient decided on a method? What is the method?
14. Has the patient made any specific plans or preparations (e.g. obtained a gun or pills)?
15. Has s/he made any other preparations for suicide, like preparing a will or writing a suicide note?
16. Does the patient need or desire hospitalization at this time? Why or why not?
17. Will the patient call and ask for help if he or she feels suicidal?
Chapter 8
231 Suicide Assessment (p. 3)
18. Does the patient have a reliable support network? Does she or he live alone?
19. Does the patient seem trustworthy and reliable?
20. Does the patient wish to maintain the right to commit suicide?
21. Can the patient give you an absolute guarantee that she or he will not make a suicide attempt, no matter how desperate or discouraged she or he feels?
22. Describe any other factors that seem relevant:
Conclusions and Recommendations
Part Four E = EMPATHY Does it Really Make a Difference?
Assessment Assessment
Testing Testing
Methods Methods
Empathy Empathy Agenda Agenda Setting Setting
9*
The Five Secrets of Effective Communication
The 1970s was a decade of tremendous creativity and innovation for cognitive therapy. During that era, my colleagues and I developed many of the techniques that are still gaining popularity today. However, no matter how many techniques I tried, there were always patients I couldn't seem to connect with. They were skeptical, angry, or mistrustful, and many had the diagnosis of Borderline Personality Disorder. One day, I received a telephone call from Dr. Aaron Beck. He said he was in a jam and needed some help. He explained that he'd recently given a lecture on cognitive therapy at the Maudsley Hospital in London. Following the lecture, a medical student named Stirling Moorey asked if he could come to the Center for Cognitive Therapy in Philadelphia and study for a month during his psychiatry rotation. Dr. Beck said he'd be happy to have Stirling come anytime he wanted. Apparently, Dr. Beck forgot about the conversation. That morning, Stirling * Copyright
2003 by David D. Burns, M.D.
Chapter 9
234
had suddenly shown up at the center for his month of training. Dr. Beck was embarrassed because they didn't have any training program set up for Stirling, so he told Stirling that he could sit in on my sessions and observe me doing therapy during the month. That way, Stirling would get a feel for how cognitive therapy worked. I was taken aback by this proposal, since I'd always been trained to view therapy as sacred. Furthermore, I was just starting my private practice, and didn't think that my patients would want to feel like guinea pigs, with a medical student watching while they spilled out their innermost feelings. Still, I didn't want to disappoint a colleague, so I said that it might be okay for Stirling to sit in on a session or two. I wasn't sure I could offer more than that, because it might seem disruptive to my patients, but I was willing to give it a try. Dr. Beck thought this was an excellent idea and sent Stirling down to my office immediately. His Center for Cognitive Therapy was on the fifth floor of the Girard Bank Building, and my office was on the third floor, so Stirling appeared in my office a minute later. He seemed nervous, and explained that he hadn't yet had any psychiatric training in medical school. In addition, he hadn't taken any psychology courses in college, and was afraid the patients would find out that he didn't know anything about psychiatry. He asked if he could just sit in the corner and watch, so he wouldn't have to interact with the patients. I told Stirling that the idea of him watching from the corner felt uncomfortable to me, and that it might feel less intimidating if we all sat down together. I assured him that I'd carry the ball during the session and not put him
Chapter 9
235
on the spot. He said he felt extremely anxious but was willing to give it a try. My next patient was a college student named Phil who was referred to me by his dorm advisor at Temple University. Phil was suffering from paranoid schizophrenia. Apparently, he'd written "DEATH" on his door and often screamed in the middle of the night, which frightened the other students. He was outraged because he was convinced that his sexual thoughts were being broadcast on loudspeakers throughout the campus, and that all the other students could hear his most private thoughts. I hadn't made any progress with him, in spite of the fact that I was prescribing neuroleptics and attempting to do cognitive therapy. I thought, "This might be a good opportunity for Stirling to sit in on a session. Phil's pretty psychotic and I'm totally stuck, so it probably couldn't hurt." I introduced Stirling and explained that he was a medical student visiting from London for a month. I asked Phil if he'd mind having Stirling sit in on our session so he could share his ideas about the treatment. Phil seemed excited and said he was grateful that Stirling had been sent as a special messenger all the way from London just to help with his therapy. After we sat down together, Phil became agitated and explained that he had a terrible problem he needed my help with. On his way to the session, he'd passed an Episcopal Church. The front door was open, and he took this as a sign that he was supposed to go inside. Lo and behold, he discovered John the Baptist standing in the aisle waiting for him. Phil said he immediately realized that God had sent John the Baptist to earth with secrets about the spiritual future of the human race, and that he was
Chapter 9
236
the one who was supposed to receive them and distribute them to everyone on earth. He knelt at the feet of John the Baptist, who began to reveal the secrets to him. As he was talking, Phil became excited and exclaimed: "But then the minister got jealous, because he wanted to talk to John the Baptist, but John the Baptist wanted to talk to me. So the minister called the police and they forced me to leave. They warned me not to come back to the church again. I know there's a conspiracy to prevent me from seeing John the Baptist, and I want to know what you intend to do about it, Dr. Burns!" This was the way all our sessions had been going, and I had thought, "I know he's not taking his Stelazine. I'm going to have to raise the dose again." I didn't know how to respond, so I turned to Stirling and said, "Tell me, Stirling, what would the British approach be?" Sheer terror swept across poor Stirling's face. He looked like a deer caught in the headlights, and said nothing for nearly 30 seconds. It was so quiet you could have heard a pin drop. Stirling's eyes seemed to be spinning like a slot machine. The longer the silence went on, the more excited Phil became. He leaned forward in eager anticipation, as if he were thinking, "What's the expert from London going to say?" Finally, Stirling leaned forward and said, "You know, Phil, in England we have a great interest in religion." Phil seemed surprised and said, "You do?"
Chapter 9
237
Stirling replied, "Oh, absolutely! In fact, I took two courses on religion in college. So if John the Baptist told you secrets about the spiritual future of the human race, I'd be extremely curious to hear what he said. What, exactly, did John the Baptist tell you?" Phil seemed excited and said, "Do you really want to know?" Stirling replied, "Yes! I can't wait to find out! Please tell me. What did John the Baptist say to you?" Phil began to explain and soon, the two of them were enmeshed in an animated discussion about the spiritual future of the human race. They talked on and on, and I was completely shut out of the interaction. However, I noticed that the longer they talked, the less psychotic Phil sounded. He even began calling Stirling "Dr. Moorey." After a while, he said, "Dr. Moorey, you've helped me so much with my religion problem." I was thinking, "He did? How did he do that? What did he do, exactly?" Then Phil said, "Dr. Moorey, I'm wondering if you can help me with another problem." "Oh, absolutely," Stirling replied. "I'd be happy to help you with any problem at all. What is it?" Phil said, "Well, I'm horny all the time." Stirling looked puzzled and asked, "Why is that a problem for you?" Phil said: "I don't seem to have anything in common with any of the kids my age, and I don't know how to get a date. I wouldn't even know how to talk
Chapter 9
238
to a girl, much less get a date. In fact, I don't have a single friend. All day long, I notice how different I am from everybody else. In fact, I've heard them saying that they think I'm crazy, or something like that. I just don't seem to fit in." Stirling replied, "Phil, you're absolutely right. I noticed that about you right away when I met you." Phil said, "Really? What did you notice about me?" Stirling said, "I noticed that you are very special and unique. And I'll bet I know something else about you, too." Phil replied, "You do? What do you know about me?" Stirling said, "I have a feeling that when you're around other people, you're always thinking about how different you are, and noticing all the things you don't have in common with them." Phil seemed excited and said, "That's right. That's exactly how I feel! How did you know that, Doctor?" I was thinking, "Well, you just told him! It didn't exactly take a genius to figure that out!" Stirling replied, "And I'll bet I know something else about you, too!" Phil said, "You do? What's that?" Stirling said, "I'll bet you don't ever bother to notice what you do have in common with other people. Take you and me, for example. We're both really interested in religion, and when we talk about religion, we have a terrific time." Phil said, "You're right. I never thought about it like that before. Mmmm.
Chapter 9
239
Where do you think I could find some really horny girls I have something in common with?" Then they started talking intensely again, and before long, the session was over. I'd barely said a single word the entire time. Phil seemed relaxed and didn't sound nearly as crazy as he had at the start of the session. As I was scheduling his next appointment, he said, "Dr. Burns, I want you to know that this was by far the best therapy session we've ever had! Will Dr. Moorey be here again next week?" "Oh, absolutely," I replied. "He'll be here for the entire month. You can bank on it!" I wasn't exactly sure what had happened, but it was obviously positive, so I decided to try Stirling out with my next patient, Madge. Madge was a 50 yearold single woman with Schizoaffective Disorder. She'd had more than a dozen hospitalizations for floridly psychotic episodes at the state hospital before she was referred to me. Madge worked as a painter, and had won numerous awards at art shows. But from time to time, she'd deteriorate and become confused and suicidal. She'd started going downhill about two weeks earlier. I was seeing her twice a week and prescribing large doses of anti-psychotic medications, but nothing was working. I'd decided to hospitalize her that day because a suicide attempt seemed imminent. I thought, "It couldn't hurt to have Stirling sit in. He can talk to her while I call the inpatient unit and make the arrangements for her hospitalization." Madge
Chapter 9
240
had no objection to having Stirling join us. At the start of the session, Madge sounded delusional and disorganized. She rambled on and on about the voices that were commanding her to commit suicide. I could barely engage her in a productive dialogue, so I turned to Stirling and said, "Tell me, Stirling, what would the British approach be?" Stirling leaned forward and began to talk to Madge. They were soon involved in an intense conversation about art, and before I knew it, the session was drawing to a close. Madge turned to me and said, "Dr. Burns, I'm feeling so much better. In fact, I'm not hearing the voices any more. Do you think I really need to go to the hospital today?" I asked her to fill out the Beck Depression Inventory so I could see how severe her depression was. I was shocked to see that her score was near the normal range, and she didn't seem to be suicidal any more. I told her that since she was feeling so much better, I didn't see any reason for hospitalization. Then she said, "Will Dr. Moorey be joining us next week?" "Oh, definitely!" I replied. "Dr. Moorey will be here for the whole month." I realized that I was witnessing something very special. Stirling may have been a novice, but he was one of the most effective therapists I'd ever seen, right out of the starting gates. I told myself, "I may be the 'expert' here, but Stirling is doing something that I need to learn." I told Stirling that I was seeing about 70 patients a week in back-to-back sessions because I was trying to save up enough money for a down payment for a house. I explained that it was a grueling schedule, but I wondered if he might
Chapter 9
241
want to sit in with me on all of my sessions for the month. Stirling was excited about that, so we worked together as a team for the next month. It was one of the greatest months of my career. Whenever I was stuck with a particularly oppositional patient, I'd turn it over to Stirling, and when he got stuck, he'd turn it over to me again. Our "tag team" therapy seemed amazingly effective, even with manipulative patients with Borderline Personality Disorder. Of course, I was teaching Stirling how to do cognitive therapy, and he learned quickly. But at the same time, I was trying to figure out what he was doing. It seemed like no matter what a patient said, or how upset the patient was, they'd soon be feeling relaxed and eating out of his hands. He had the capacity to form a warm and trusting therapeutic alliance with almost any patient instantly. He had the knack of seeing the world through the other person's eyes and could always find truth in what they were saying, no matter how irrational or hostile their comments were. I started giving names to the different techniques Stirling was using, so I could try to learn to do what he was doing. When I'd go home at night on the commuter train, I'd write out imaginary dialogues with difficult patients. I'd come up with outrageous criticisms and ask myself, "What would Stirling say? How would he respond to this comment?" Then I'd attempt to write out more effective responses that incorporated the communication techniques I was beginning to systematize. Over time, I discovered that I could respond in much the same way that Stirling did, and my therapeutic effectiveness increased substantially.
Chapter 9
242
The Five Secrets of Effective Communication* (EAR) E = Empathy 1. The Disarming Technique (DT). Find some truth in what the other person is saying, even if it seems totally unreasonable or unfair. 2. Empathy. Put yourself in the other person's shoes and try to see the world through his or her eyes. Thought Empathy (TE). Paraphrase the other person's words, so that she or he will see that you listened and got the point. Feeling Empathy (FE). Acknowledge how the other person is probably feeling, based on what she or he said. 3. Inquiry (IN). Ask gentle, probing questions to learn more about what the other person is thinking and feeling.
A = Assertiveness 4. "I Feel" Statements (IF). Express your own ideas and feelings in a direct, tactful manner. Use "I Feel" Statements, such as "I feel upset," rather than "You" statements, such as "You're wrong!" or "You're making me furious!"
R = Respect 5. Stroking (ST). Convey an attitude of respect, even if you feel frustrated or angry with the other person. Find something genuinely positive to say to the other person, even in the heat of battle.
*Copyright
1991 by David D. Burns, M.D. Revised 2001.
Chapter 9
243
Since the late 1970s, many of these methods have been popularized for professionals and for the general public. You may already be familiar with several of them, possibly with different names. I call them the Five Secrets of Effective Communication, and they appear on page 242. When you use these techniques skillfully, you can quickly transform almost any failed relationship into a warm and trusting one. The acronym, EAR, may help you remember them. E stands for Empathy, or good listening skills. A stands for Assertiveness, or good selfexpression skills. R stands for Respect. These are the techniques that master communicators have used for centuries. For example, when you use the Disarming Technique, you find truth in what the other person is saying, even if they're attacking you in a hostile, unreasonable manner. Nearly 2,000 years ago, the Greek philosopher, Epictetus, said that if someone criticizes you, you can tell them that if they knew you better, they'd have far more than just that to criticize! Let's talk about each technique, and how to avoid some of the most common pitfalls you might encounter when you're learning how to use them. The Disarming Technique. When angry, critical patients attack you, you may feel convinced that their criticisms are distorted and unfair. Certainly, patients will say all kinds of things that sound irrational, and you may have a powerful urge to defend yourself or to correct them. When Phil said, "I just saw John the Baptist, and he had important secrets to share with me about the spiritual future of the human race," I had the thought, "No, Phil, you didn't see John the Baptist. You were hallucinating again, and you need more medication."
Chapter 9
244
There's something about that message that isn't exactly going to warm the patient's heart! In contrast, Stirling agreed that the human race was having serious spiritual problems. He sincerely wanted to know what John the Baptist had said, and what Phil thought about it. The moment he validated what Phil was saying, Phil relaxed and opened up. I decided to call this the Disarming Technique. You find genuine truth in what the patient is saying, even if it seems totally illogical, distorted, unfair, or off the wall. Stirling was an absolute master at this. The Disarming Technique is based on what I call the Law of Opposites:
Law of Opposites If you argue or defend yourself against a criticism that's totally irrational or unfair, you'll instantly prove that the criticism is valid.
In contrast, if you genuinely agree that the criticism is valid, you'll instantly put the lie to it.
This is a paradox.
Chapter 9
245
For example, let's say a defiant patient named Jennifer says, "What's the worst thing that ever happened to you? Did you break a fingernail?" Jennifer is saying that you've never had any real problems and couldn't possibly understand how she feels. Maybe she's been living on the streets and struggling with drug abuse, and senses that you may be looking down on her. But you want to show that you do understand, so you say, "It may seem like I've had it easy, but I know what it's like to struggle, too." You may think you're using the Disarming Technique, but you're actually being defensive. You're conveying this message: "You may feel like I don't understand, but you're wrong!" Jennifer will feel put down and conclude that her criticism was valid, since you're talking about yourself and ignoring how she feels. Instead, you might say: "Gosh, Jennifer, I'm feeling kind of taken aback right now. There's a sharp tone in your voice, and I'm concerned that I've offended you and failed to convey any real understanding of what you've been through. Can you tell me more about how you're feeling, and what I've done or said that sounded judgmental or uncaring?" In this example, you're validating Jennifer's criticism. You're agreeing that she's right, and that you've failed her in some important way. Paradoxically, this message will put the lie to her criticism and she'll suddenly perceive you as humble, respectful and genuinely concerned about her. You can think of this as the Zero Technique. When you're attacked, put
Chapter 9
246
your own agenda aside. Make yourself a zero, a nothing. Instead, zero in on what the other person is saying. Become their advocate. Then you'll end up on the same team. Most people want respect. They want to be listened to. The people who criticize you are generally convinced that they've got a good point. They want you to acknowledge that what they've said has merit. The Disarming Technique is the most powerful communication technique of all, but it's difficult to learn. There are at least three reasons for this. First, we all want to feel competent and professional. When an angry patient is ripping into you, you may feel ashamed and embarrassed. It can be awfully hard to say, "You're right. I can see that I've been letting you down." This hurts our pride. Second, fear gets in the way. When a patient criticizes you, you may feel like something terrible is about to happen. You may be afraid that the patient will drop out of therapy, sue you, or file an ethics complaint, so you defend yourself. Paradoxically, this casts you in a more negative light and the patient's frustration escalates. In contrast, when you treat your patients with respect and find truth in what they're saying, they'll usually feel more relaxed and trusting. Third, our own perceptions of the truth get in the way. I believe that every criticism contains a tremendous amount of truth, no matter how outrageous it sounds. But we sometimes get trapped in our own view of the situation, so we can't see that the patient really is right about something important. Unfortunately, our professional training reinforces the notion that the patient is wrong. We're taught that their negative feelings about us are distorted projections of childhood experiences. We label it as their "transference neurosis."
Chapter 9
247
This lets us off the hook, because the failure in the therapeutic alliance becomes their problem. Certainly, our patients will sometimes perceive us in a distorted way. But even their most distorted perceptions about us will contain an important grain of truth. You can either emphasize what's wrong with the criticism, or find the truth in it. Paradoxically, when you respectfully validate the patient's criticism, they'll stop believing it, and they'll be far more willing to focus on their own role in the problem. But when you defend yourself, they'll be all the more convinced about your culpability—and they'll usually be right! I recently described the Disarming Technique to a new crop of psychiatric residents at Stanford. Most of them were working with delusional, hostile patients on the locked unit of the Stanford Hospital, and were trying to learn how to set limits with patients who act out and make unreasonable demands. The idea that you could agree with an angry patient seemed foreign to them. A resident named Juan asked, "What if the patient's criticisms are blatantly false?" I asked for an example. Juan explained that he'd just seen an angry teenage boy named Jorge who'd shouted at him and said he was stupid. Juan exclaimed, "Obviously, someone in the Stanford psychiatric residency program isn't stupid. I have an M.D. and a Ph.D. So how could I possibly agree with him?" How would you reply to Jorge if you were his therapist? Put your ideas here:
Chapter 9
248
Chapter 9
249
Answer You could say something like this: "As a matter of fact, Jorge, I am feeling kind of stupid right now, and it seems like you're really ticked off at me. Can you tell me what I did that turned you off? I really want to hear what you have to say." Jorge's criticism of his doctor was valid. There had obviously been a failure in the alliance. Juan had done or said something that rubbed Jorge the wrong way, and he clearly hadn't connected with him. But if he conveys respect and agrees that he's misread the situation, he won't look so stupid any more! Now examine the response that you wrote down on page 248. Did you find the truth in Jorge's criticism? If so, you're off to a good start. Let's say that your patient, Serena, has a diagnosis of Borderline Personality Disorder. You notice that after last week's session, she gave you a poor score on the Therapeutic Empathy scale. When you ask her about it, she says, "You don't really care about me." Serena may feel this way about lots of people, possibly everyone, and may frequently provoke hostility and rejection. How would you disarm Serena? Remember that the Disarming Technique literally means, "to agree with." It will not be sufficient to acknowledge her feelings. You'll need to tell her that her statement is valid. But at the same time, you'll need to express yourself in a way that won't hurt or threaten her. How are you going to do that? Put your ideas here before you turn the page:
Chapter 9
250
Chapter 9
251
Answer Therapists who try this exercise in workshops usually have a hard time responding effectively. They often avoid disarming and use Inquiry instead. For example, they may say, "Can you tell me more about that?" Inquiry isn't a bad thing to do, but it's not the same as disarming, because they're not agreeing with Serena. Other therapists resort to a subtle put down. They say, "I can see how you might feel that way." This is almost like anti-disarming, and it's definitely not going to defuse Serena's anger. Some therapists simply contradict the patient. They say, "As a matter of fact, Serena, I do care about you." This may sound compassionate, but Serena will feel discounted, as if her perceptions are somehow psychotic and not to be taken seriously. She'll conclude that you're definitely not very caring because you're defending yourself and talking about how wonderful you are! I've seen many therapists resort to psychobabble formulas, such as, "I'm glad you told me that, Serena, and I'm proud of you for having the courage to be open and honest with me. Thank you for sharing." There are so many problems with this response that it's hard to know where to begin. In the first place, there's no disarming. This therapist has not agreed that Serena's statement is true. In the second place, it's phony, because this therapist doesn't really feel "glad" or "proud." He probably feels frustrated and defensive. Finally, "thank you for sharing" is a formulaic response that's guaranteed to irritate anyone. Although Serena's criticism may sound distorted, it does contain a great
Chapter 9
252
deal of truth. She's telling you that she didn't feel cared about or supported during the last session. Otherwise, she wouldn't be attacking you in the first place. If you defend yourself and insist that her criticism isn't true, Serena will feel even more annoyed and intensify her attack in an effort to get you to listen. If, in contrast, you acknowledge the truth in her criticism and convey respect, she may suddenly discover that you do care. This will make it far easier for her to examine her own role in the problem, and her defenses will begin to melt. How can you use the Disarming Technique effectively? First, you have to ask yourself, "Is there some truth in what she's saying?" If you think back on your last session with Serena, you may realize that it wasn't very rewarding and that you weren't working together very collaboratively. In fact, there was probably some tension in the air, with lots of "yes-butting," intellectual jousting, and talking past each other. If so, you could respond along these lines: "As a matter of fact, Serena, I've been thinking about our last session and it dawned on me that I didn't do a very good job of listening or providing warmth and support. Instead, I felt like we were doing battle. I could sense you were feeling frustrated, and it was uncomfortable for me, too. I felt badly about that, and was concerned that I'd let you down. Can you tell me more about how you're feeling?" How will Serena feel if you say this, and what will she conclude? She'll probably feel cared about because you're validating her complaints in a respectful way and opening the door for dialogue. Paradoxically, when you agree that you've failed her, you won't be failing her any more. In all likelihood, she's
Chapter 9
253
feeling hurt, lonely and angry, because she's so used to driving everyone away. This time, something very different happened, and she's finally connected to you. Failures in the therapeutic alliance may be frustrating and anxietyprovoking, but they present us with opportunities to do some of our most satisfying and productive work. When you're under attack, you're actually on the verge of a therapeutic breakthrough. But you won't experience that breakthrough until you can see that the patient's criticisms really are valid. Thought and Feeling Empathy. When you use Thought Empathy, you summarize the patient's words so that he or she can see that you got the message. When you use Feeling Empathy, you acknowledge how the patient is probably feeling, given the words she or he used. First, I want you to try Thought Empathy. Imagine that your patient, Omar, lashes out at you in an extremely irate tone of voice: "I've been coming to see you for 18 goddamned months, doing all your stupid homework assignments, and paying you good money, and I'm more depressed today than the first day I came to see you!" What would you say next, using Thought Empathy? Your job is to summarize what Omar just said. Repeat his words, so that he'll know you got the message. You don't have to acknowledge his feelings yet. We'll do that in a minute. Put your response here:
Chapter 9
When you've written something down, turn the page and I'll share my thinking with you.
254
Chapter 9
255
Answer Using Thought Empathy, you could say: "Wow, Omar, I can see that you're really upset, and I want to make sure that I understood what you said. You say you've been coming here for 18 months, doing all the stupid homework assignments, and paying me good money, but you're feeling more depressed today than the first day you came to see me." As you can see, I simply paraphrased what Omar said, using his exact words. I edited out the adjective, "goddamned," because I wanted to avoid sounding sarcastic or patronizing. Thought Empathy may look easy on paper, but when I do this exercise in workshops, most therapists leave out one or two of the things the patient said. They filter out the portions of the patient's message that made them feel the most anxious, embarrassed or ashamed. These are the most commonly ignored complaints, in this order: 1. "I'm paying you good money." 2. "I've been doing all your stupid homework assignments." 3. "I've been coming to see you for 18 months." 4. "I'm more depressed today than the first day I came to see you." Dodging a criticism is a huge error, because it's like cutting off one of the patient's fingers. The patient will feel discounted and annoyed, and will intensify the attack to try to get the message across. Review what you wrote down on page 253. Did you acknowledge all four
Chapter 9
256
of Omar's criticisms? If not, which ones did you miss? Now we'll try Feeling Empathy. Given what Omar just said, how is he probably feeling? You can say something like, "Omar, I can imagine that you might be feeling X, Y, and Z," where X, Y, and Z are words that refer to specific types of emotions. Please give it a try now:
Don't look at the answer until you've written something down. Remember, the best time to learn and make mistakes is now, and not later on, when you're being confronted by an angry patient.
Chapter 9
257
Answer You could simply say: "Omar, given what you just said, I can imagine that you might be feeling frustrated, disappointed, discouraged, or even a bit angry with me, and for good reason. Am I on the right track?" Notice that I've said, "you might be feeling . . . ." We never know for sure how someone's feeling, and we want to open the patient up. Avoid making accusations or putting the patient on the defensive. In addition, I said, "a bit angry." In spite of all the aggression in our society, most people are anger-phobic and feel an intense need to deny their anger. If you say, "a bit angry," it makes it easier for the patient to own up to these feelings. Finally, I said, "angry with me, and for good reason." This makes your statement more accurate and far more palatable. If you were to say, "Omar, you sound like a very angry fellow," he'd feel defensive and get even angrier because it sounds like you're accusing him of having some kind of anger problem. But when you respectfully acknowledge that the anger is directed at you, he'll find it much easier to go with the flow. In fact, the anger will often diminish the very moment you acknowledge it, if you acknowledge it skillfully. The biggest error therapists make when using Feeling Empathy is to ignore the patient's anger. In role-playing exercises, and in real-life confrontations, therapists tend to overlook anger nearly 100% of the time. Therapists will acknowledge any kind of feeling except for anger. This is true
Chapter 9
258
even when the patient is explosively angry. You may find this hard to believe, but when you practice with colleagues, you'll see exactly what I mean. Inquiry. The Feeling Empathy response above ends with the question, "Am I on the right track?" This is an example of the third listening skill, Inquiry. The goal of Inquiry is to open the patient up and encourage further dialogue, so you can learn more about how the patient is thinking and feeling. The most common error therapists make when using Inquiry is to say something like this to a critical patient: "I can see that you've been feeling stuck. What do you think would be more helpful to you?" This is a huge error. When patients are upset or angry, they need to express their feelings and want you to listen. But when you ask, "What would be more helpful to you?" it's like saying, "Hey, let's be nice. I can't tolerate your anger. Please stop attacking me so we can work on the solution and feel better." Furthermore, patients don't know what would be more helpful to them. The patient's job is to express how they're feeling. It's your job to listen and figure out what techniques or interventions might be more helpful. In general, you should avoid problem-solving when patients are upset. When people are angry, you'll almost never be able to solve the problem that's bothering them. That's because they need to have their feelings validated. Later on, when you and the patient feel better about each other, you can solve any real problems that need to be solved. Other reasonable Inquiry questions might be, "Can you tell me more about how you see the situation?" Or, "Can you tell me more about how you're feeling,
Chapter 9
259
and about how I've been missing the boat in my work with you. What are some of the problems that I've been overlooking that we should be focusing on?" "I Feel" Statements. Psychoanalysts believe that therapists must never express their feelings. Instead, you're supposed to respond with silence, or simply mirror back what the patient has said to you. There's some wisdom in this. Certainly, too much self-disclosure on the part of the therapist could be off-putting, and could violate the boundaries of an ethical professional relationship. In spite of this limitation, I believe there are times when it is helpful—in fact, crucial—for therapists to express their feelings during sessions. For example, let's say that you're feeling defensive or uncomfortable because a patient has just criticized you in a harsh tone of voice. You could say, "Gee, I'm feeling a bit awkward right now because your criticism really seems valid. What you're saying is important, and talking about it could help us get back on track. Could you tell me a bit more about how you're feeling?" In this case, the statement, "I'm feeling a bit awkward," conveys a sense of vulnerability without being unprofessional. If the patient is resentful because you seemed stiff, phony, or holier-than-thou, this statement will go a long way toward transforming the interaction. When you express your discomfort in a kindly, lowkey, respectful way, you appear far more human and genuine. There are three guidelines to keep in mind when you express your feelings during a therapy session. First, use "I Feel" Statements rather than "You" statements. "You" statements will put the patient on the defensive. For example,
Chapter 9
260
if you say, "You're making me angry, too," the patient may feel blamed or frightened. Your goal is to inform the patient of your feelings in a gentle, nonthreatening manner. Second, make sure you convey your feelings using low-key, professional language, rather than street-talk. For example, instead of saying, "I'm feeling pissed off," you could say, "I'm feeling a bit uncomfortable," or "I'm feeling some frustration as well. Let's talk this out." The statement, "I'm feeling a bit uncomfortable," is not an overly powerful declaration, but it lets your patient know that you're upset. Remember that you have the upper hand in the therapeutic relationship. The patient may view you as an authority figure, so any disclosure of your feelings may have a strong effect. Finally, remember that the goal of self-disclosure is to help the patient, and not to help yourself. Let's say that a patient is angry and ripping you to shreds, and says that your therapy is a total waste of time and you don't know what you're doing. In response, you say: "Oh, what you say is so true, but things are even worse than you think. You're actually my best patient. None of my patients are getting better and managed care doesn't pay squat. My wife is divorcing me and even my dog won't hang out with me any more." Obviously, this is just tongue in cheek, but there is a point. It's unprofessional to try to get the patient's sympathy. When you express your feelings, your goal is to open the patient up and create a warm, human connection.
Chapter 9
261
Most therapists have a great deal of trouble using "I Feel" Statements. When we're attacked, most of us feel defensive and appear uncomfortable. You can't really disguise it, because it will show in your body language, even if you don't verbalize it. If you try to cover up your feelings so you can look polished and professional, you'll look like a phony. Your patient will see through the façade every time. I can't emphasize strongly enough how common this type of error is. Therapists even try to cover up their feelings in role-playing exercises. This makes them look bad. It's also unfortunate because your vulnerability allows you to connect with the patient in a far more meaningful way. Why do we compulsively hide our feelings from our patients? One reason is that we think we're supposed to "have it all together." The popular stereotype is that we're so wise and objective that we never feel threatened by our patients' criticisms. We also tell ourselves that we shouldn't feel anxious, inadequate, defensive, frustrated, annoyed, angry, guilty, ashamed or confused. These are "bad" emotions, and acknowledging them is an admission that we've failed and that we're less than we should be. We may also have the idea that we're supposed to be totally neutral when we're with patients, and should only discuss our real feelings with a colleague or supervisor outside of the therapy session. Of course, there's nothing wrong with getting advice and support from a colleague when you feel overwhelmed or upset because of a logjam with a patient. In fact, working through these reactions can be a rich source of learning and personal growth. But there are many times when
Chapter 9
262
you can gain mileage by allowing yourself to be human during sessions, instead of trying to cover up your emotions or act totally cool, calm, and collected. Stroking. This is the last of the five communication techniques. You convey admiration or respect, even in the heat of battle. Stroking is based on the work of the 20th century theologian, Martin Buber. He described two types of relationships: "I-It" relationships and "I-Thou" relationships. "I-It" relationships are characterized by competition, battle, and a lack of respect. You view the other person as an object, and your goal is to manipulate, hurt or defeat them. In contrast, in an "I-Thou" relationship, you treat the other person with respect, even if you both feel angry or deeply hurt. An "I-Thou" relationship has a spiritual component. You view other people, and human relationships, with awe, reverence, and respect. Your goal is not to hurt the other person, but rather to connect with them on a deeper level. Many patients experience relationship problems that occur over and over again. For example, they may feel angry and frustrated because the people they care about always seem to reject them or let them down. The patient comes to expect this type of failure in nearly all their relationships, and may set you up to play the same role. All too often, we take the bait. Although we fight against it, it's almost impossible to avoid the traps our patients set for us. Some patients sense your weaknesses and stick the knife into your most vulnerable area within minutes of meeting you. Suddenly, you feel angry and resentful, or anxious and ashamed, and wish you didn't have to deal with them.
Chapter 9
263
I once asked the Stanford psychiatric residents to describe the most upsetting criticisms they'd heard from their patients. They uniformly agreed on the same scenario. As you greet your new patient for the first time, she or he looks disappointed and says, "Aren't you just a student here? I thought I was going to see one of the staff doctors." Certain patients can almost smell your insecurity. They lay down the gauntlet and invite you to get do battle from the start. Instead of getting defensive, you can treat the patient with genuine respect. This doesn't mean you have to repress your negative feelings or act like a Pollyanna. It's often crucial to express your feelings, including feelings of frustration. But you can always do this in a way that won't convey hostility or rob the patient of self-esteem. I believe that you can make any interpretation you want, any time you want, no matter how brutal it is—but you have to do it in a way that will make the patient feel flattered and respected. You can convey positive feelings verbally or nonverbally, through body language, but your expression has to be genuine or it will backfire. Like any of the Five Secrets of Effective Communication, Stroking is easily abused and prone to misapplication. Let's say that a 6'7" heroin addict named Stan begins to verbally attack you during a group therapy session. He gets in your face and says, "You're a total f___ing phony! You have no idea how I feel, or what my life is like!" You reply, "Thank you for sharing. I know that must have been hard for you, and I'm grateful." What do you think about this response?
Chapter 9
264
In the first place, Stan isn't "sharing" with you. He's ripping you to shreds in front of your other patients. In the second place, you don't feel grateful. It's more likely that you're feeling intensely annoyed, embarrassed, and defensive. In the third place, Stan wasn't being especially courageous, and it probably wasn't hard for him to put you down. In fact, it was probably deeply rewarding for him! Can you think of a more effective response? Put your ideas here:
Chapter 9
265
Answer You might say something like this: "Wow, Stan, I'm embarrassed because I was sounding phony just now. I realize that I haven't done a very good job of understanding how you feel, or what your life has been like. I can imagine that you're pretty ticked off at me, and I really want to hear more about this. I respect you a lot, and feel badly that I haven't tuned in better." This response serves several purposes. First, you're making Stan the hero instead of getting involved in a power struggle with him. This will lift the morale of the other group members because they'll feel like they can express their feelings and criticize you without any negative consequences. Second, you'll appear human, and your humility will create a bond between you and all the members of the therapy group. And finally, when you agree with a criticism, you put the lie to it. This response is not what you'd expect to hear from a "phony." However, tone will be important. If you come across in a self-effacing way, it will backfire. Effective responses convey self-respect and respect for the patient at the same time. Now that we've reviewed all five communication techniques, let's practice weaving together. Imagine that your patient, Troy, has just said this to you: "I can see through your head games!" What would you say next? Write your response below. After each sentence you write, put the communication techniques you used in parentheses. To save a lot of writing, you can simply use the two letter abbreviations on page 242.
Chapter 9
When you're done, I'll share my thinking with you.
266
Chapter 9
267
Answer Troy sounds mistrustful and angry, and has accused you of playing headgames. There's clearly been a profound failure in the therapeutic alliance, and Troy is shooting you down. You can acknowledge the truth in his criticism and let him know that you feel uncomfortable. You can also acknowledge his anger and bring the conflict to conscious awareness, rather than continuing to play games with him. Try to do this in a warm, respectful way so you don't sound hurt or defensive. This approach might work: "Gee, Troy, I'm feeling awkward right now, but you've got a good point. (IF; DT) It's embarrassing to admit it, but I think I probably was playing head games just now. (IF; TE; DT) I feel like I haven't been connecting with you in a very meaningful or genuine way. (IF; DT) There was a sharp edge in your voice just now, and it sounds like you're pretty ticked off at me. (FE) Do I have it right? (IN)" Now examine what you wrote down on page 265. How did you do? Did you share your feelings openly? Did you find genuine truth in Troy's criticism? Did you acknowledge his anger? Did you put the names of the techniques you used in parentheses at the end of each sentence? If your response seemed lame or ineffective, that's good. It means that you can see that there are problems in the way you respond to attacks from angry patients. Trying and failing many times will be necessary if you want to learn how to respond skillfully. If the first thing you wrote down doesn't seem
Chapter 9
268
effective, try again. Often, several responses will be necessary before you come up with something really good. On pages 270 – 273, you'll find 11 additional exercises to help you master these techniques. In each case, write down how you'd respond to the patient's criticism using the Five Secrets of Effective Communication. After each sentence you write, indicate which communication techniques you used in parentheses, using the abbreviations on page 242. Don't try to cram all five techniques into each response. That would be too long-winded, and it would probably sound artificial. After you've completed each problem, you can review my answer before going on to the next problem. That way, you'll learn as you go. Remember that this is more of an art than a science, and there's no simple formula you can use. The Five Secrets are like five strings on a musical instrument. Your job is to create music, and there are an infinite number of melodies you can create. For example, you can't always start with Thought Empathy, and then add the Disarming Technique, Feeling Empathy, Inquiry, and so forth. That would be formulaic and it wouldn't sound natural. Here's what I'm talking about. Your patient shouts, "You suck!" You really want to do a good job so you decide to use all five techniques. You reply: "I can hear you saying that I suck. (TE) In fact, I do suck. (DT) I can imagine that you might be feeling angry with me. (FE) Are you? (IN) I feel embarrassed, but I like you, and want to hear more! (IF; ST; IN)" Obviously, this isn't going to be a winner! If you try to do all 11 problems in one sitting, you'll probably feel
Chapter 9
269
overwhelmed. Instead, try a couple of them, and think about any errors you might have made. Tomorrow, you can try a couple more. Over time, your skills will increase. Please don't skip ahead and read the answers without trying the exercises! All the growth comes from trial and error, just as with any new skill you're learning. The exercises will be invaluable, even if your initial responses aren't very effective. Remember that there's no single correct response. These are problems that every therapist struggles with, and there will always be many effective or ineffective responses to any criticism from a patient. In some cases, you may think that my responses aren't effective, and you may be able to come up with something better. The ultimate test will be the way your patients respond during actual therapy sessions. If you use the Therapeutic Empathy scale regularly, you'll know exactly how you're doing. Good luck!
Chapter 9
270 Written Exercises
1. "How would you know how I feel? You're not living on the streets. You've never been hooked on drugs!" (Answer on page 274)
2. "My wife thinks I'm not getting anywhere. She thinks I'm wasting my time here." (Answer on page 274)
3. "You're bored with me. You're going to throw me out like everyone else did." (Answer on page 275)
4. "I'm pregnant and it's all your fault!" (Answer on page 276)
Chapter 9
271
5. "Don't give me any more of your psychology B.S. Was that supposed to help?" (Answer on page 277)
6. "You don't care about me. You're just in it for the buck." (Answer on page 278)
7. "I don't have anything to say! Nothing's bothering me!" (Answer on page 279)
Chapter 9
272
8. "I saw an article about Prozac. Do you think I need a real doctor? Or should I stick with you?" (Answer on page 281)
9. "You're not helping! You don't even understand me!" (Answer on page 281)
10. "What makes you so sure you can help me? I've tried everything and nothing works. My problems are hopeless." (Answer on page 282)
Chapter 9
11. "Aren't you just a student here? I thought I was going to see Dr. Koran!" (Answer on page 282)
273
Chapter 9
274 Answers to Written Exercises
1. "How would you know how I feel? You're not living on the streets. You've never been hooked on drugs!" (Problem on page 270) The patient is right. You simply need to acknowledge this and show your human side. This approach might work: "You know, you're right. (DT) I'm not living on the streets and I haven't struggled with many of the things you've had to face. (TE; DT) It sounds like you're in a lot of pain, and like you're angry with me as well. (FE) Maybe you think that I couldn't understand or help you because I haven't been through what you've been through. (TE) I feel sad that I've let you down so badly. (IF; DT) Can you tell me about some of the problems and feelings I haven't tuned in to? (IN)" Now that you've read my response, I have a question for you. Did you write out an answer to this exercise, or skip it and just read my solution? I'd like to encourage you to do the written exercises. It will make all the difference if you'd like to learn how to use these skills in real-life situations. 2. "My wife thinks I'm not getting anywhere. She thinks I'm wasting my time here." (Problem on page 270) This patient may think that the therapy is going well, and his wife may be feeling annoyed about something. But it's more likely that the patient feels stuck and is afraid to criticize you, so he's telling you indirectly. You may be able to tell which of these options is more accurate if you review his recent scores on the Brief Mood Survey and the Evaluation of Therapy Session. His responses will
Chapter 9
275
nearly always tip you off about how he feels. Let's assume that his mood scores have not been improving, and his scores on the Evaluation of Therapy Session indicate a lack of empathy and progress. You could respond along these lines: "I've had that feeling, too. (DT) I think your wife may be onto something. (DT) It seems like we have been stuck in the last few sessions, and I'd like to find out more about what you think. (DT; IN) Maybe I haven't been tuning in to how you're feeling, or what you really need help with. (DT) In fact, your scores on the Therapeutic Empathy and Helpfulness scales indicate that I haven't been doing a good job of supporting you or helping you. (DT) Can you tell more about how you've been feeling? (IN)" 3. "You're bored with me. You're going to throw me out like everyone else did." (Problem on page 270) You may have been feeling bored or unhappy with this patient. Instead of defending yourself, you can acknowledge the problem in a way that won't threaten the patient or rob her of self-esteem. Here's one approach: "I've also had the feeling that we're not working together nearly as well as we could. (DT) You're obviously suffering a great deal, and if I've seemed bored or conveyed the idea that I'm going to reject you, I can imagine that you might be feeling anxious and hurt, or even angry with me. (TE; FE) As awkward as it is to hear this, it's also exciting because this is the exact conversation that could get us back on track again. (IF;
Chapter 9
276
ST) Can you tell me a bit more about how you've been feeling, and what I might have said that upset you or conveyed a lack of interest? (IN)" Occasionally, I use a few other techniques in addition to the Five Secrets of Effective Communication. When I said, "This is the exact conversation that could get us back on track again," I was using Positive Reframing. I reframed the conflict as an opportunity for a therapeutic breakthrough. Positive Reframing can be a useful tool. It's easy to become consumed by shame and resentment when you're confronted by therapeutic failure. But you can just as easily conceptualize the conflict as an opportunity to make the relationship more meaningful and genuine. However, Positive Reframing can be abused, just like any communication technique. For example, you may try to cast the conflict in a positive light without encouraging the patient to express the anger and disappointment they feel. If you use Positive Reframing as a defensive maneuver to avoid the patient's anger, the tension will escalate. But when you embrace the conflict and accept the validity of your patient's anger and disillusionment, something very positive will often emerge. 4. "I'm pregnant and it's all your fault!" (Problem on page 270) At a workshop in San Francisco, I asked the therapists in the audience to describe the most anxiety-provoking criticism they'd ever heard from a patient. This statement won the award! The therapist was treating a depressed teenager who made this statement at the beginning of a session. Patients sometimes blame their therapists when they feel angry, upset or
Chapter 9
277
ashamed. If you defend yourself, you'll appear guilty. Instead, you can try to support the patient: "Gosh, Rose, I'm surprised to hear that you're pregnant, and I'm concerned about you as well. (IF; TE) I'm worried that I may have said something that had a negative effect. (IF; DT) Can you tell me more about what's happened? (IN)" Obviously, we need more information. Maybe the therapist said something that the patient took as license to become sexually active, or to have sex without adequate protection. At this point, it's all speculation, because we don't know what happened. In the vast majority of cases, listening and validating the patient's criticisms will calm the troubled waters. After all, if she were planning a lawsuit or an ethics complaint, she probably would have dropped out of therapy and wouldn't be sitting in your office telling you about her pregnancy. She may be blaming you because she feels guilty and ashamed about her sexual activities. Your warmth and support could be invaluable. 5. "Don't give me any more of your psychology B.S. Was that supposed to help?" (Problem on page 271) Sometimes we do lapse into B.S. when there's tension in the room and we feel defensive or anxious. It can often be helpful to acknowledge your feelings, using an "I Feel" Statement, and to admit that the criticism is true, using the Disarming Technique. This will often make you appear genuine and real again. Here's one way to do this:
Chapter 9
278 "Gosh, Mark, I'm taken aback! (IF) I was feeling a bit
uncomfortable just now, and I think I did get into some ridiculous psychological B.S. (IF; DT) I can see that you're feeling annoyed with me and I apologize. (FE; DT)" Apologizing is generally a therapeutic error because it prevents the patient from expressing any additional anger, but there are exceptions to every rule. In this case, the apology works because of the "I Feel" Statements and the Feeling Empathy. 6. "You don't care about me. You're just in it for the buck." (Problem on page 271) This criticism is hard to disarm because we don't want to think of ourselves as mercenary or uncaring. It seems shameful. And yet, the patient is at least partially right. If you look at the patient's responses on the Therapeutic Empathy and Helpfulness scales, you'll see the proof of this. His answers will show that he's been feeling a lack of warmth and support, and that your recent sessions have not been particularly helpful to him. You may also be feeling frustrated and annoyed. If you respond skillfully, it could lead to a therapeutic breakthrough. Here's one approach: "You know, Duane, it's a bit embarrassing to hear you say that, but I think you're right. (IF; DT) During our last session, I asked about the bill and didn't tune in to how you were feeling. (DT) I don't think I was very supportive, and I sensed some tension in the air. (DT; FE) I can imagine that you might be feeling hurt and angry with me. (FE) Let's talk
Chapter 9
279
about it. (IN)" This response has to be delivered with warmth and genuineness. Your discussion with Duane could lead to a breakthrough if you listen to all the anger and mistrust that he feels. If you sincerely agree that you haven't been very warm or caring, without any sense of shame or disrespect, you'll suddenly convey warmth and caring. When you agree that you've failed, you actually succeed. 7. "I don't have anything to say! Nothing's bothering me!" (Problem on page 271) This criticism came from a teenager who sounds defiant and upset. If you push her to talk to you, she'll clam up even more. The key is to empathize with why she's reluctant to talk, as follows: "Audrie, you say that you've got nothing to say, and that nothing's bothering you. (TE) And yet, I sense that you may be feeling angry or upset with me. (FE) I can see that your arms are crossed, and you're glaring at me. (FE) "I have a feeling you've got some good reasons not to want to talk to me. (DT) I'm concerned that I haven't done a very good job of listening or making you feel like you can trust me. (DT) Maybe you're afraid that if you told me about the problem, I'd be judgmental or get defensive, or say something really lame. (TE; IN) Am I reading you right? (IN)" In this response, I'm commenting on the impasse that has developed and taking the blame for Audrie's reluctance to talk. This is quite different from pushing her to talk about the problems that are bothering her. Of course, this has
Chapter 9
280
to be done in a genuine way, and not as a gimmick. When I said, "I can see that your arms are crossed, and you're glaring at me," I labeled it as Feeling Empathy (FE) because I was empathizing with Audrie's anger by commenting on her body language. Of course, this type of statement must be conveyed in a friendly and non-confrontational manner, or Audrie will feel cornered and will defiantly insist that you're wrong. Alternatively, you could make a statement like this: "Audrie, it seems like you're not in the mood to talk right now. (DT) I'm wondering if there's something you're ashamed about, or if you're mad at me but don't feel like you can talk about it. (FE; IN) Or perhaps I haven't been a very good listener in the past, so you may feel like you don't even want to bother to try. (FE; IN) Do any of these ideas ring true? (IN)" Notice that you're focusing on why she doesn't want to talk to you, and you're giving her some choices, rather than pressuring her to open up. I call this technique Multiple Choice Empathy. It often works surprisingly well. Multiple Choice Empathy can be difficult to grasp and master at first because there's a natural tendency to get into a power struggle with a patient who refuses to talk. This nearly always makes the patient clam up even more. Instead, when you use Multiple Choice Empathy, you're siding with the patient and agreeing that she or he has a darn good reason not to talk. If you do this skillfully, the patient will nearly always open up. 8. "I saw an article about Prozac. Do you think I need a real doctor? Or should I
Chapter 9
281
stick with you?" (Problem on page 272) Non-medical therapists frequently hear this complaint. The patient's request for Prozac needs to be taken at face value. Any depressed patient who wants an antidepressant is entitled to an evaluation by a physician to see if a medication might be indicated. However, this patient's question sounds like a thinly disguised criticism of you. You'll need to bring this out so you can explore the patient's negative feelings about the treatment. You might say: "You know, some people are enthusiastic about antidepressants, and if you'd like one, I can refer you to a colleague who can write you a prescription and monitor the medication. (DT; TE) At the same time, when you ask if you need a 'real doctor,' I get the feeling that you may be a bit annoyed or disappointed. (TE; FE) I really like you and I'm hopeful that we can continue our work together, even if you decide to try an antidepressant, but I'd also like to hear about any negative feelings you're having. (ST; IN) Can you tell me about where I've been missing the boat? (IN; DT)" 9. "You're not helping! You don't even understand me!" (Problem on page 272) This is one of the most common complaints we hear from patients. If you learn how to handle this type of complaint skillfully, it can make a significant difference throughout your career. Here's one way to respond: "You know, Maurice, you're absolutely right. (DT) I feel like I haven't done a very good job of understanding how you feel, and my efforts clearly haven't been helpful. (TE; DT) I can imagine you must be
Chapter 9
282
feeling frustrated and misunderstood, or even angry with me. (FE) I have a lot of respect for you, and I'd like to hear more about how you're feeling. (ST; IN) This is exactly what we need to talk about so we can back on the same team. (Positive Reframing)" 10. "What makes you so sure you can help me? I've tried everything and nothing works. My problems are hopeless." (Problem on page 272) This patient feels put off and is challenging you. Ask yourself why the patient is putting up a wall. You could reply: "I'm concerned that I haven't acknowledged how desperate you feel, and how hard you've been struggling without any tangible success. (IF; DT; FE) You've told me that you've gone to many therapists, and taken drug after drug, and that nothing has helped you. (TE) I can imagine that you might not want to trust me and get your hopes up after all the disappointments you've told me about. (DT; TE) I'm also wondering if you might be feeling frustrated or annoyed with me. (IN; FE)" You'll also want to assess this patient for suicidal impulses, because the patient is feeling angry, desperate and hopeless, and these feelings often trigger suicidal fantasies and urges. 11. "Aren't you just a student here? I thought I was going to see Dr. Koran!" (Problem on page 273) As threatening as this criticism may sound, it's not too difficult to respond if you simply use the Five Secrets of Effective Communication:
Chapter 9
283 "Mr. Adams, you're right. (DT) I am a psychiatric resident, and it
sounds like you were expecting to see one of the attending psychiatrists. (TE; DT) I can see that you're feeling disappointed, and I'm wondering if we can sit down and talk about your concerns. (FE; IN) If you decide that I'm not the right person for you, I'd be happy to refer you to one of the other doctors, because I want you to get the best possible treatment. (ST) But if you decide that you and I can work together, it would be great, because I'd love to have the chance to work with you. (ST) Does that seem reasonable? (IN)" The paradox here is that by admitting that you're young—without shame— and by encouraging Mr. Adams to voice his criticisms and doubts, you convey the wisdom and expertise of a sophisticated therapist. You're telling Mr. Adams that you would like to work with him, but you won't try to trap or coerce him. He'll probably decide that you're the person he wants to work with!
10*
Learning to Use the Five Secrets in Real Time
Now that you've had the chance to work through a number of alliance failures on paper, I'm going to show you a more advanced exercise that will help you learn how to use the Five Secrets in real-life situations. It's one of my favorite training techniques, but it can be a bit traumatic at first. You'll need at least one colleague or friend to practice with. You and your partner should sit in chairs facing each other. One of you will play the role of a difficult patient, and the other will play the role of the therapist. You'll do lots of role-reversals, so it doesn't make much difference who takes which role first. Instructions for the Difficult Patient. Your role is easy, and quite rewarding, as it turns out. All you have to do is attack your therapist. Your aim should be to make your therapist crawl with humiliation. You can be as hostile and obnoxious as you want. Try to force the therapist to get defensive.
* Copyright
2004 by David D. Burns, M.D.
Chapter 10
285
There are only two rules to keep in mind. First, try to limit your comments to a few sentences. An attack that lasts 10 – 15 seconds will be plenty. Even one barbed criticism can be difficult to handle. Don't overload your therapist with too many hostile remarks all at once. Second, after you've attacked your therapist, give him or her the chance to respond. The odds are high that your therapist will appear lame, defensive, or phony, and you'll have a powerful urge to interrupt and keep attacking your therapist. Resist that urge! Once the therapist has responded, STOP and provide feedback. Do not keep attacking your therapist. The role-playing is over, and it's time to give the therapist some feedback on his or her response. It's always interesting to see how hard it is for the "patient" to follow this rule. There seems to be a kind of sadistic gratification in ripping into the "therapist." When therapists get defensive, there's an almost irresistible urge to keep attacking them. When you play the role of a difficult, challenging patient, you'll begin to understand why these therapeutic impasses develop so quickly. You'll become more aware of the errors that nearly all therapists make when they're under attack. Instead of continuing to rip into your therapist, give him or her three specific kinds of feedback: 1. First, what was the therapist's overall grade? Was it an A, a B, a C, or a D? Try to be honest. You won't do the therapist any favors by being overly nice or avoiding negative feedback.
Chapter 10
286
Some therapists object to giving each other grades, but this is a huge mistake. Here's why. Even though the "therapist" probably didn't do a very good job, you may feel inhibited about criticizing a colleague, so you may become rather vague when you give feedback. This allows for too much slippage. But when you're forced to give a grade, it will be clear whether or not the therapist's response was up to speed. For example, if you give a B+, your colleague will know that he or she did some things well, but fell short in one or two areas. Then you can give specific feedback about what worked and what didn't. 2. What did you like or dislike about the therapist's response? Did you feel like opening up, or did you feel subtly pushed away? Did the therapist seem warm and open, or defensive and anxious? Did the therapist appear genuine or phony? Did the therapist convey genuine respect? 3. How skillfully did the therapist use the Five Secrets of Effective Communication? Did she or he: Use the Disarming Technique properly, and find genuine truth in your criticism? Paraphrase your statements accurately and acknowledge your feelings, including anger? Use Inquiry effectively? Express his or her feelings in a spontaneous, natural and professional manner? Convey warmth and respect?
Chapter 10
287
This third type of feedback is especially important. The goal of this exercise is to learn how to use the Five Secrets of Effective Communication skillfully. If the therapist's response was ineffective, it will usually be because she or he used the techniques in a clumsy way, or failed to include a technique that was crucial. Here's the type of feedback I've provided to the "therapist" when observing colleagues and students doing this exercise: "Gerry, I thought you did a great job with Thought Empathy, but you didn't acknowledge the patient's anger. He seemed enraged, but you didn't comment on that at all. When you forget to acknowledge his anger, he'll feel the urge to escalate his attack." "Shannon, you did a nice job with Feeling Empathy, and you conveyed a lot of warmth, but you forgot to use the Disarming Technique. As a result, your response sounded a bit formulaic. The patient's criticism had a lot of truth in it, and she needs to feel validated. "In addition, it might be good to include an 'I Feel' Statement to show your vulnerability. That patient sounded pretty upset and aggressive. How were you feeling when she attacked you?" This type of specific feedback can be invaluable when you're in the therapist's role, because you'll know exactly what you did right and wrong, and will quickly learn how to improve your responses. The feedback will demystify something that seems mysterious, confusing and difficult, so you won't be left with vague feelings of inadequacy or frustration.
Chapter 10
288
After you've provided feedback for the therapist, you can do a rolereversal. This time, you'll be the therapist, and your colleague will be the angry patient. Instructions for the Therapist. While the "difficult patient" is attacking you, listen respectfully without interrupting. Lean forward and look directly at your patient. Try to convey a receptive, compassionate, welcoming attitude. Avoid negative body language such as pulling back, grimacing, sighing, shaking your head, or rolling your eyes in disgust. When you respond, use the Five Secrets of Effective Communication. I would recommend that you keep the list of techniques on page 242 handy. Both you and your "patient" should have a copy available so you can refer to it during the exercise. You don't need to use all five techniques every time you respond, but weaving two or three together may be desirable. Thought Empathy can be important—paraphrase what the "patient" said so she or he will see that you got the message. Acknowledge how she or he is probably feeling, given what was said. Remember that therapists almost never acknowledge anger. This is a huge mistake, because the patient will simply get angrier and the attack will escalate. It will also be important to include the Disarming Technique in your response. No matter how illogical or unfair the criticism may seem, there's always a grain of truth in it. Once you see the grain of truth, you'll usually find a mountain of truth. If you can acknowledge this truth, it will have an immediate, beneficial impact on the interaction. Inquiry can be very useful at the end of your response. Instead of
Chapter 10
289
promising to try harder or offering to fix the problem, ask the patient to tell you more about how she or he is feeling. If you're feeling upset or defensive, try to include an "I Feel" Statement. Your discomfort will be obvious. If you hide your feelings, and attempt to come across in a professional, unemotional way, you may look like a phony and the patient's attack will escalate. Finally, try to convey warmth and respect, even if you're feeling frustrated or resentful. You don't have to hide your negative feelings. The important thing is to convey your feelings in a way that will not rob the patient of self-respect. After you've responded, the "patient" will critique your response. If you're doing this in a group, you can get feedback from the other observers as well. You'll probably discover that you made all kinds of errors. This can be embarrassing and humiliating. Try to avoid getting defensive or justifying your response. This will definitely turn your colleagues off! Instead, try to find some truth in what they're telling you. If you're willing to set your pride aside, the feedback you receive will be invaluable. If your response wasn't optimal, you can do a role-reversal. Now you can play the role of the patient, and your colleague will play the role of the therapist. Continue doing role-reversals until you're both satisfied that you've come up with a superb response to the patient's criticism. Be patient with yourself. This exercise will be hard at first. Part of the problem is that you'll be in a Catch-22 situation. On the one hand, I've warned you that your spontaneous responses will sound defensive and ineffective. We
Chapter 10
290
tend to have knee-jerk reactions that get us into trouble. But on the other hand, if you don't sound spontaneous and natural, you'll sound artificial and gimmicky, and that will backfire, too! The only solution to this seemingly impossible dilemma is practice, practice, practice. If you're willing to fail ten or twenty times in a row, you'll suddenly get it, and it will seem incredibly easy. Then you'll have awesome new skills that can transform your interactions with your patients, as well as your relationships with colleagues, friends, and family members. Learning the Five Secrets of Effective Communication requires humility, determination and goodwill. If you have the genuine desire to improve your relationships with difficult patients, these tools can boost your therapeutic skills and self-confidence considerably.
11*
Common Empathy Errors— And How to Avoid Them
If you want to use the Five Secrets of Effective Communication skillfully, several things will be required. First, this approach will have to make sense to you from an intellectual perspective. Certainly, there are many schools of therapy, and many ways of handling conflict. This is just one approach among many. Second, you'll have to be pretty strongly motivated. It was clear to me that Stirling Moorey, the British medical student I supervised in Philadelphia, was especially skillful in the art of empathy, and I wanted to acquire that skill if I could. I was tired of conflicts with critical, mistrustful patients, and I was eager to learn a more effective approach. Third, you'll have to back up your motivation with lots of practice. Have you been doing the written exercises? Have you tried the role-playing exercise
* Copyright
2003 by David D. Burns, M.D.
Chapter 11
292
yet? If you're just reading about these methods, you won't be able to use them effectively in real-life situations. Reading is a great first step, but you'll get a radically different perspective when you do the exercises. Finally, you'll need humility. It can be hard to disarm an angry, critical patient. Pride gets in the way. In addition, when you begin to practice with colleagues, you'll make lots of errors and look foolish at times. This can be embarrassing. Most of us are blind to the way we relate to other people, and we fancy ourselves to be far more sensitive and empathic than we actually are. The truth that comes out during the role-playing exercises can be upsetting. If your colleagues are honest, they'll give you bad grades at first, and they'll point out all kinds of errors you made. You'll suddenly realize that your response to a patient who was upset sounded phony and formulaic. If you're struggling to maintain your sense of self-esteem or trying to impress your colleagues, you'll be in for some rough sledding. But if you check your ego at the door, the process can be extremely rewarding. During the role-playing exercises, you may discover that you tend to make the same kinds of mistakes over and over. Most therapists have one major blind spot. For example, some therapists aren't very good at expressing their own feelings. They have trouble with "I Feel" Statements, so they appear stiff, formal, flat or phony during conflicts with patients. Other therapists have trouble with the Disarming Technique, Thought or Feeling Empathy, Inquiry, or Stroking. When I was first developing these methods, I had the most trouble with
Chapter 11
293
the Disarming Technique. I sometimes responded defensively because I couldn't imagine how there could possibly be any truth in the criticisms my patients leveled at me! In addition, I could always see a hundred reasons why the patient was "wrong." I found it helpful to tell myself, "Win through losing," or "Victory through surrender," whenever I was under attack from an angry patient. This reminded me to use the Disarming Technique instead of giving in to my usual knee-jerk responses. When I disarmed the patient skillfully, I noticed an almost instantaneous change in the patient's attitude and in the quality of the therapeutic alliance. This was so surprising and reinforcing that I quickly became captivated by the technique that had been so difficult for me initially. For practice, I'd make up the most preposterous criticisms I might ever hear from a patient, colleague, or family member. Then I'd try to find some truth in each criticism so I could disarm it. At first, it was difficult, but over time, it got easier and easier. Before long, I could find a great deal of truth in practically any criticism, no matter how unfair or off base it sounded. In this chapter, I'll highlight the most common errors therapists make when learning the Five Secrets of Effective Communication. I'll also give you some tips that will help you avoid these errors so you can respond warmly and effectively to even the most outrageous criticisms. Disarming Technique Errors The Disarming Technique is the most valuable of all the Five Secrets of Effective Communication, but it's the hardest to learn. Most therapists have a great deal of trouble finding truth in the criticisms of an angry, critical patient.
Chapter 11 Why is this? List at least three reasons why therapists struggle with the Disarming Technique: 1.
2.
3.
Please don't continue reading until you've answered this question!
294
Chapter 11
295
Answer There are many reasons, including: Pride and shame. You may not want to acknowledge the truth in the patient's criticism because you don't want to look bad. You may be afraid that your patients would look down on you if you agreed that you'd made a therapeutic error or treated them in an insensitive manner. Truth. You may find it hard to let go of your own version of the "truth," so you can't see that there really is truth in what the patient is saying. The Disarming Technique means that you literally agree that the patient's criticism is true. This concept is mind-boggling for some therapists. They can't see how the patient's criticism could possibly be true. Fear. When you genuinely agree with a criticism, you strip away your own defenses. Some therapists find this threatening because they think they have to keep their patients in a one-down position and never relinquish their role as "expert." They think that something terrible will happen if they agree with a critical patient, so they defend themselves. For example, you may think you'll get sued. I once treated a man named Jeffrey who was one of America's most successful medical malpractice attorneys. I taught Jeffrey how to use the Five Secrets of Effective Communication so he could deal more effectively with conflicts in his work and marriage. I asked Jeffrey whether he thought these techniques would make a therapist more vulnerable to a malpractice suit. After all, when you use the
Chapter 11
296
Disarming Technique, you're agreeing that the patient's criticisms are valid. Jeffrey said that if all doctors and psychotherapists used these techniques, he'd soon be out of business, because so few patients would ever feel like suing. He said that the main cause of malpractice suits is, "The doctor didn't listen." Most patients file malpractice suits because the doctor got defensive and put up a wall. When the doctor doesn't listen, the patient goes to an attorney, because attorneys have a way of getting doctors to pay attention! If you use these techniques skillfully, your patients' respect for you will increase, and the probability of a malpractice suit will go down. In addition, the Evaluation of Therapy Session on page 203 will allow you to track your patients' perceptions of you at every single session. You'll see precisely how caring and helpful you were, and you can spot any negative feelings or problems before they mushroom out of control. If you process the feedback non-defensively with your patients, they'll realize that they can discuss problems openly with you. That's the best malpractice insurance you can get! Therapists often ask this question: "Won't my patients just get mad and keep dumping on me if I agree with their criticisms? I'm afraid of opening Pandora's box." You usually won't open Pandora's box if you acknowledge the truth in what your patient is saying, but you'll almost definitely open Pandora's box if you don't! Fear can operate as a self-fulfilling prophecy. If you perceive the patient as your enemy, then you'll automatically put up a wall and defend yourself. Paradoxically, this forces the patient to keep attacking you.
Chapter 11
297
Patients escalate when they feel like: You're not listening or validating what they're saying. You're not acknowledging their anger. You're not conveying genuine respect. You sound defensive. You're hiding your feelings of vulnerability or awkwardness and trying to maintain a professional facade. If a patient escalates and gets more upset with you during a therapy session, write down one thing she or he said to you, and exactly what you said next. You'll nearly always see that you didn't use the Five Secrets of Effective Communication skillfully. I can't emphasize the importance of this enough. As therapists, we have the same kinds of blind spots as our patients, and it's not easy to learn to use these techniques. A therapist named Shauna told me that her patient, Aldous, became upset when she asked about his role in the conflict he was having with his wife. She was confused, because she was pretty sure that she'd been using the Disarming Technique. Let's take a closer look at what happened. Shauna's patient, Aldous said: "You're siding with my wife!" Shauna replied, "Aldous, you seem to think that I'm supporting your wife. (TE) I can imagine that you might be feeling annoyed. (FE) Are you? (IN)" At this point, Aldous became enraged and said, "Damn straight I'm annoyed! How the hell would you feel? Am I supposed to pay for this so-called
Chapter 11 'help'?" Why did Aldous' attack suddenly escalate? Can you pinpoint Shauna's communication errors? Put your ideas here before you turn the page:
298
Chapter 11
299
Answer Using the EAR system, we'd have to conclude that Shauna didn't acknowledge Aldous' feelings (Empathy), express her own (Assertiveness), or convey any genuine warmth (Respect). Shauna didn't really acknowledge the truth in what he was saying. Instead, she simply repeated his words, like a parrot. She didn't really try to see the world through his eyes, so he didn't feel validated. In fact, she subtly discounted what he was saying. He felt put-down, and this was exactly what he was complaining about in the first place. Shauna didn't use an "I Feel" Statement, either. She felt awkward, but hid behind a professional façade and struggled to maintain control. Aldous felt like no one was supporting him. His felt like his wife and his therapist were both ganging up on him, and Shauna's condescending response confirmed this feeling. Shauna fell right into the trap he set for her. You can't disarm a patient effectively until you can see that there really is truth in what the patient is saying. In fact, Shauna had been scapegoating Aldous during the previous session. She told herself that she was just trying to get him to see his role in the conflict, but she secretly sided with his wife and felt like he was to blame the problems in their marriage. Aldous picked up on this and was trying to talk about the problem. He'll need genuine empathy and support before he'll be willing to examine his role in the marital conflict. During role-playing exercises, I sometimes ask therapists to respond to patient criticisms using only the Disarming Technique. One person plays the role of a difficult patient who attacks the therapist relentlessly and verbalizes all kinds
Chapter 11
300
of outrageous statements like, "You're a jerk," "You're not helping me," "I'll never get better," "You obviously don't know what you're doing." You can try this exercise with a colleague. Most therapists have lots of trouble finding any truth in these statements. Instead, they respond with Thought Empathy and Inquiry without really agreeing with anything the patient said. For example, they might say, "It sounds like you think I'm a jerk. Can you tell me a bit more about how you're feeling?" This may not be the worst possible response, but it's definitely not the Disarming Technique because you haven't found any truth in the patient's criticism. The Disarming Technique is far more powerful. You go far beyond Thought Empathy or Inquiry and agree that the criticism is correct. If you do this skillfully, you'll put the lie to the criticism. Some therapists use the Disarming Technique in a brutal and overly literal manner during the role-playing exercises. They agree with the patient's statement in a hurtful way. Consider this example: Patient: You don't like me! Therapist: You're right. (DT) I don't like you. (IF) This statement would destroy the therapeutic alliance. When you agree with a patient's criticism, you have to convey warmth and respect at the same time. Let's assume that you've been treating a man named Johan, and the last couple sessions didn't go very well. There's a lot of tension in the air, and you notice that you got a poor score on the Therapeutic Empathy scale. When you
Chapter 11 ask Johan about it, he says, "You don't like me!" How would you use the Disarming Technique? Put your response here:
301
Chapter 11
302
Answer Here's one approach: "Johan, this is a bit awkward, but I'm glad you brought it up. (IF; Positive Reframing) I have been feeling frustrated during the last couple therapy sessions, and I've sensed that you may be feeling the same way. (IF; FE) I think I was too hard on you last week, and I feel like I haven't been nearly as helpful or supportive as I'd like to be. (DT; ST) In fact, sometimes I feel like I'm more in the role of your enemy than your ally, and it's uncomfortable for me, too. (IF; DT) I'm wondering if you're feeling angry or hurt or judged. (FE; IN) Can you tell me more about how you're feeling? (IN) " Notice that you're acknowledging the tension the air, but you're not literally agreeing with the statement, "I don't like you." You're finding the truth in the criticism without buying into the distortion in what the patient said. The patient is telling you that there's a lack of warmth in your relationship. He doesn't feel cared about or accepted. His perception is valid. You probably have been feeling frustrated or annoyed with him, so you can acknowledge it. However, Johan is involved in All-or-Nothing Thinking. He assumes that people either "like" or "dislike" each other. He may not understand that negative feelings are an inherent part of any good relationship. Your discussion of the negative feelings you're both experiencing could be an excellent opportunity to model how a meaningful relationship develops, and it can greatly strengthen the therapeutic alliance.
Chapter 11
303
Surprisingly, most therapists avoid any discussion of the negative feelings that have developed during therapy sessions. It may seem like the feelings are shameful and forbidden. When you try to avoid the tension in the air, your feelings of dislike for the patient will intensify, along with the patient's distrust and resentment. But I've never had a patient I didn't begin to like once we discussed the negative feelings that had developed. In fact, the patients I felt the most uncomfortable with were often the ones that I ended up enjoying the most. Many therapists have asked this question: What if there isn't any truth in the patient's criticism? How can you possibly agree with a criticism that's just plain wrong? I'm convinced that there's always a huge amount of truth in any criticism. Suppose a patient named Ivan told you, "You're a totally worthless, horrible human being." How would you disarm this statement? Remember, your response must be 100% true. You're not allowed to rationalize. You have to agree that Ivan is essentially right about something important. Put your ideas here before you turn the page:
Chapter 11
304
Answer Before you can effectively disarm someone, you have to think about what they're saying and find the truth in it. Even if they express themselves in a hostile or exaggerated manner, there will still be a grain of truth in the message. If a patient said that you were totally worthless and horrible, you'd want to ask yourself why they said that. Is there some truth in what they're saying? Maybe you said something that hurt their feelings, so they don't feel like they can trust you. On some level, they're absolutely right. To make the situation even tougher, Let's assume that you thought things were going fine and don't know what Ivan talking about. You could disarm him by saying something along these lines. "Ivan, when you say that I'm a totally worthless and horrible you sound pretty ticked off. (TE; FE) I must have done or said something that really hurt your feelings, and I feel badly about that. (DT; FE; IF) I'm surprised, because I don't even know what I said or did that hurt you so badly. (IF; IN) I'm very committed to you, I'd be grateful if you'd tell me what happened. (ST; IF; IN)" Of course, the details will differ in every situation. There are no formulas to memorize, and you must always respond genuinely or none of the communication techniques will be effective. In this case, I simply acknowledged that I didn't know what I'd done that bothered Ivan. Obviously, you wouldn't say that if you did know what was going on! Some patients might say you're horrible because they're trying to
Chapter 11
305
manipulate you. They feel ticked off because you didn't give them what they wanted. If so, the Disarming Technique will still be useful. They're complaining that you've let them down, and they're right. You have let them down. Some therapists are afraid to disarm manipulative patients because they sense the power struggle. They're afraid to empathize or express any warmth because they don't want to give in. Paradoxically, you'll usually gain far more control if you use the Disarming Technique, Feeling Empathy, "I Feel" Statements, and Stroking. Of course, the context will influence how you use these techniques. Let's say that a patient named Waldo is trying to manipulate you. Waldo is on the locked unit of your hospital because of a suicide attempt. He's wants you to give him a pass to leave the unit, but the staff believes he may still be suicidal. When you tell him you can't give him the pass, he says that you're horrible, insensitive and totally incompetent. He says that you're being cruel and unfair, and that if you don't give him the pass, he'll get fired and lose his job. What will you say to him? Remember, you have to use the Disarming Technique. That means that you must agree that what he's saying is correct in some way. Put your ideas here:
Chapter 11
306
Answer Here's one approach: "Waldo, I think you've got every right to feel frustrated and upset with me. (DT; FE) I don't like having to keep you here against your will, and I wish I didn't have to do it. (IF) Personally, I'd hate to be hospitalized against my will. (IF; DT) At the same time, I'm concerned about your safety. (IF; ST) You made a serious suicide attempt, and this morning you said you'd be better off dead. (TE) I think you have a lot to live for, and I'd have an awfully hard time forgiving myself if I gave you a pass and lost you. (ST; IF)" In this case, you're disarming Waldo while conveying respect and letting him know how you feel. Keep in mind that you don't have to use the Disarming Technique in every sentence, because that would sound unnatural. You'll need to incorporate some of the other techniques in your response as well. Waldo has complained that you're holding him against his will, like a caged animal. He's right, so you can agree with him, but you can express compassion at the same time, and let him know how you feel. You don't have to get involved in a power struggle or accept his invitation to do battle. If you can't find any truth in what the patient is saying, you can describe the patient's criticism to a colleague and ask if they can see some truth in it. Colleagues can often see the problem more objectively. Remember that when our patients feel hurt or angry, they may be thinking about your shortcomings in an illogical way and they may make exaggerated
Chapter 11
307
statements when they criticize you. Your patient may say that you're always late, that you never understand how they feel, or that all you really care about is money. These are classic examples of Overgeneralization, one of the ten cognitive distortions. Of course, it's not true that you're always late, that you never understand them, or that all you care about is money, so you feel the urge to defend yourself. But that will be about as helpful as pouring gasoline on a fire! You can easily disarm these criticisms if you focus on one or more specific errors that you've made. For example, you could say something along these lines: "Enrique, you're right. (DT) I was late for the last two sessions, and I know how annoying and disrespectful that can be. (DT; FE)" "Joel, I totally agree. (DT) I haven't done a very good job of understanding you during the past couple sessions. (DT) Can you tell me a bit more about how you're feeling? (IN)" "George, when I asked about the bill last session, it felt awkward to me, too. (IF) After the session, I got to thinking about how awful you must have felt when you learned that you were laid off at work. (DT; FE) I feel like I let you down. (DT; FE; IF)" When you use the Disarming Technique, you have to make valid statements, and you have to convey self-respect and respect for the patient as well. That's why the technique is so challenging. Sometimes you'll feel caught offguard, and for the life of you, you can't figure out how the patient's criticism could possibly be valid. If so, you can simply tell the patient that you're confused and
Chapter 11
308
need more information, but that you know that you must have done or said something that was upsetting to him or her. On page 310, you'll see five extreme challenging criticisms from angry patients. These are criticisms from narcissistic or schizophrenic patients that may seem like they couldn't possibly be true. Try to disarm each criticism in the space provided. Then examine your response. Did you acknowledge genuine truth in the criticism, or were you just giving it lip service? Did you get defensive and imply that the patient was wrong? Did you resort to Thought Empathy, Feeling Empathy, or Inquiry without finding any truth in what the patient said? Feel free to include any of the Five Secrets of Effective Communication in your responses, but make sure you always include the Disarming Technique. When you're done, you can review my answers on page 311. You may find the exercise difficult because you don't have many facts to go on. It may be easier if you imagine the context. For example, the first problem is: "I know you're involved in a conspiracy with the FBI to have me killed!" Imagine that the patient is suffering from paranoid schizophrenia, and you're treating him on the inpatient unit. At the start of your therapy session, he makes the accusation that you're out to get him. How will you respond? How will you agree with him? Keep in mind that there has to be some kernel of truth in what he's saying. What is he trying to tell you? When you've completed these problems, you can make up some extreme criticisms of your own. List the most preposterous or threatening criticisms a patient, colleague, friend or family member could conceivably level at you. See if
Chapter 11
309
you can find genuine truth in each criticism. Once you feel comfortable with the answers you've written down, you can practice responding in real time, using the role-playing exercise described in Chapter 10. Ask your colleagues to tell you if your responses sound phony or defensive. Over time, you'll develop the ability to use the Disarming Technique skillfully when you're under the fire of real criticism.
Chapter 11 Patient Criticism 1. I know you're involved in a conspiracy with the FBI to have me killed!
2. You're the worst therapist in the world!
3. You don't care about anybody. You're like a robot!
4. My father didn't think I was special. I need you to tell me I'm special. But you never tell me I'm special because you don't really think I'm special. 5. You're raping me, just like my brother did when I was nine years old.
310 Disarming Response
Chapter 11
311
Patient Criticism
Disarming Response
1. I know you're involved in a conspiracy with the FBI to have me killed!
"Butch, I'm glad you brought this up, and I feel the same way. (IF; ST; DT) I don't think I did a very good job of making you feel safe or understanding how you were feeling during our last session. (FE; DT) It would be awful to feel like people were plotting against you, even your own therapist. (FE; TE; DT) You wouldn't know who you could trust, or who really cared about you. (DT) Can you tell me more about what I did that was upsetting to you? (IN; FE)"
2. You're the worst therapist in the world!
"Jerome, I've had the same thought. (DT) I feel like I haven't been at all helpful to you during our last few sessions, and I don't feel like I've been connecting with you very well, either. (DT) Can you tell me what I've said or done that's turned you off? (IN; FE)"
3. You don't care about anybody. You're like a robot!
"Earl, I feel so sad to hear that, and you're right. (IF; DT) Last session, you told me how devastated you felt when your sister committed suicide. (TE; FE) I was stunned, but didn't tell you how much that affected me. (IF) I can imagine you might have felt hurt when I responded in such a cold way. (FE) Is that why you're feeling upset with me right now? (IN)"
4. My father didn't think I was special. I need you to tell me I'm special. But you never tell me I'm special because you don't really think I'm special.
"Mary, I totally agree that haven't done a very good job of making you feel special or cared about. (TE; DT) I'm sensing a lot of tension in the air right now, and I'm really concerned that you may be feeling rejected and hurt, or even angry with me. (IF; IN; FE)"
5. You're raping me, just like my brother did when I was nine years old.
"Jodi, it really hurts me to hear that, because I've been working so hard to make the therapy feel safe and helpful. (IF) But I must have failed you in some important way, and I know that trust is absolutely crucial to our work together. (DT) Can you tell me more about what I've done or said that felt so damaging and hurtful? (IN; FE)"
Chapter 11
312
Thought and Feeling Empathy Errors The most common Thought Empathy error is to get so panicky when you're criticized that you forget most of what the patient has just said. Instead of listening carefully, so you can accurately summarize the patient's words, you may get spaced out because you're trying desperately to think of an effective way to respond. Then when you attempt to summarize what the patient said, you get it wrong because you didn't really hear it. This will be insulting to the patient, because it will be clear that you weren't listening. The patient may conclude that you don't care about what she or he was trying to tell you, and the tension will escalate. One of my psychiatric residents had difficulties with Thought Empathy. She'd get so nervous that she couldn't remember most of what the patient had just said to her. Then, when she replied, it was off-putting because it was clear that she hadn't really listened. Of course, the more anxious she became, the harder and harder it was to focus on what the patient was saying to her. She became so upset about this that she began to cry during one of the role-playing exercises during our weekly training session. One effective solution is simply to take notes during sessions or roleplaying exercises with colleagues. Jot down the main points the patient has made. Then you can summarize them accurately. This nearly always works extremely well. Once you've done this consistently five or ten times, you'll probably be able to summarize the patient's statements reasonably well without taking notes.
Chapter 11
313
This helped the psychiatric resident relax and focus. In addition, I suggested that it was sometimes okay to say something like this: "Gee, Merv, I'm feeling blown away by what you just said, but I'm not sure I got all of it. (IF) You said the psychotherapy homework was a stupid and a waste of time because it's not helping. (TE) Can you tell me the other part again? (IN) I apologize for asking you to repeat what you just said, but I want to make sure that I understand exactly how you're feeling. (IF; IN)" She also found it helpful to record the negative thoughts and feelings that flooded her mind when patients, colleagues, or family members criticized her. Then she'd identify the distortions in the thoughts and put the lie to them using a variety of CBT techniques. As her anxiety diminished, she was able to concentrate more on what her patients were saying, and less on her own feelings of anxiety. During the next several months, she blossomed into a superb therapist. We'll talk more about how you can use CBT to deal with your own feelings of insecurity later in the book. The best way to learn Thought and Feeling Empathy is to ask a colleague to play the role of a hostile patient or a patient who's extremely depressed and anxious. For example, your colleague could say something like this: Sometimes, I feel so ashamed. I feel like a bad person, but nobody knows what I'm really like inside. I feel so hopeless. I feel like things will never change. Nobody could ever really understand me.
Chapter 11
314
I feel like such a loser. Concentrate on what your colleague said and try to summarize it as accurately as possible from two perspectives. First, summarize precisely what your colleague said. This is Thought Empathy. Then summarize how your colleague was likely to be feeling, based on what she or he said. This is Feeling Empathy. You can say something along these lines: "Given what you just said, I'm wondering if you're feeling X, Y or Z." X, Y and Z refer to feeling words from the chart on page 315. Now ask your colleague to tell you how accurate you were, between 0% and 100%. Try for a score of at least 95%. If your score is lower than that, ask your colleague what you missed. Then try to summarize that piece. Remember that most common Feeling Empathy error is the failure to acknowledge the patient's anger, even when the patient is obviously ticked off or enraged. You may need lots of extra practice learning to acknowledge angry feelings. This is surprising, given the fact we dedicate our careers to dealing with emotions and interpersonal conflict! However, I see it over and over again in roleplaying exercises. It's seems like it's almost impossible for most therapists to acknowledge the "patient's" anger, even when the anger is obvious. If the patient is upset, you may have the urge to try to straighten out the problem, or to focus on something else, instead of acknowledging how angry and hurt they feel. What I just wrote may not seem very important. You may think, "Well, that wouldn't happen to me!" If you do some role-playing exercises, I think you'll be amazed by how common this error is. It's really quite mind-boggling!
Chapter 11
315
Feeling Words Chart* Blue
Down
Unhappy
Disheartened
Sad
Disappointed
Despairing
Low
Hurt
Lost
Dejected
Miserable
Ashamed
At fault
Bad
Responsible
Discouraged
Pessimistic
Desperate
Defeated
Inferior
Inadequate
Worthless
Flawed
Second-rate
Useless
Undesirable
Incompetent
Defective
Tired
Exhausted
Weary
Fatigued
Sleepy
Drained
Worn out
Lethargic
Wiped out
Uninterested
Bored
Turned off
Burdened
Abandoned
Alone
Rejected
Unloved
Unwanted
Isolated
Lonesome
Friendless
Worried
Afraid
Scared
Nervous
Apprehensive
Uptight
Tense
Terrified
Panicky
Fearful
Frightened
Alarmed
Foolish
Self-conscious
Flustered
Awkward
Humiliated
Mortified
Embarrassed
Timid
Overworked
Burned out
Tense
Frazzled
Pressured
Strained
Besieged
Overwhelmed
Mad
P. O.'d
Ticked off
Irate
Resentful
Irritated
Incensed
Annoyed
Upset
Furious
Enraged
Aggravated
Picked on
Put down
Insulted
Judged
Blamed
Intimidated
Defensive
Condemned
Stuck
Thwarted
Stymied
Envious
Mistrustful
Suspicious
Depressed
Depression
Guilty Hopeless
Unmotivated Lonely
Anxiety
Anxious
Shy Stressed
Anger
Angry
Criticized Frustrated Jealous
* Copyright
Paranoid
1989 by David D. Burns, M.D. Revised 1992, 2000, 2003.
Chapter 11
316
To overcome this blind spot, ask a colleague to play the role of an angry patient and attack you over and over. For example, your colleague might say: "I hope you get suicidal some day, and have to talk to someone like you!" "I hate you!" When you respond, see if you can acknowledge the patient's anger. This can be far more difficult than it sounds. Acknowledging anger requires considerable practice, and it's easy to miss the mark. Another common error is to acknowledge the anger in a way that provokes denial and additional attack. For example, when a hostile patient criticizes you, you might say, "Gary, you really sound angry." This comes across as a "gotcha" statement. Most people don't like to feel cornered or blamed. If you accuse Gary of being angry, he will angrily insist that he's not angry. Or, he may say, "Well, asshole, how did you think I was supposed to feel?" Instead, you could acknowledge his anger like this: "Gary, based on what you just said, I can imagine that you might be feeling a bit annoyed with me, and for good reason. (FE; DT) Let's talk about it. (IN)" In this example, you've made Gary's anger acceptable, and you've also given him some wiggle room. You've said, "I can imagine you might be feeling a bit annoyed with me, and for good reason." Now he won't feel attacked or defensive because you're validating how he feels. You're also using a euphemism, "a bit annoyed." This will make it easier for Gary to own up to his angry feelings. Of course, if Gary is enraged, it wouldn't be appropriate to minimize his
Chapter 11
317
feelings, because it will seem like you're avoiding his anger. In this case, it might be better to say, "Gosh, Gary! (IF) It sounds like you're feeling furious with me, and I really want to hear what you've got to say. (FE; DT) Let's talk about it. (IN)" The phrase, "with me," makes you the target of Gary's anger. He won't feel like you're deflecting his anger toward the system, the clinic, or the world in general, and he won't feel like you're labeling him as an "angry person." You're projecting the message, "Gary, the buck stops here. I want to hear about what I've done or said that irritated you." When you express respect and skillfully encourage Gary to tell you about how he's feeling, his anger will probably soften. That's because you're listening and showing that you're receptive, so he won't feel the need to smash through your defenses. This strategy is based on the Buddhist notion that your worst enemy is often your greatest ally in disguise. When patients are enraged, you're usually at the edge of a significant therapeutic breakthrough. Once you've experienced this in your clinical work, it will no longer seem like mystical mumbo-jumbo, but a practical reality. Many therapists have asked this question: "Can't you just say, 'I'm sorry,' if the patient is mad and feels let down?" Occasionally, apologies can be helpful, but they often represent a subtle form of conflict phobia. Consider this exchange: Patient: "I was upset when you took a call from that other patient during our session last week. I'm paying good money for your time." Therapist: "Mae, I'm really sorry. I took the call because the patient was
Chapter 11
318
suicidal, and I'd do the same for you. But I'll remind the receptionist to hold any calls during our sessions from now on, unless it's an absolute emergency." On the surface, this response looks reasonable. You've apologized and proposed a solution to the problem. However, this response may backfire because you're avoiding Mae's anger. Mae may be trying to tell you that she feels hurt, angry, and ignored. This may be a central theme in her life. You're avoiding these feelings and trying to "make nice." You're really saying, "Let's solve this problem and move on. I can't tolerate your anger." This response might be more effective: "Mae, I apologize. That call was from a patient who was suicidal. I felt like I had to take it, but I also felt bad about interrupting our session. I'd be glad to offer you some extra time to make up for the time we missed. "I'm wondering how you were feeling when I took that call. I recall that you were talking about the pain you felt when you discovered that your husband was having an affair. I can imagine that you might have felt ignored, hurt or angry with me. Were you?" In this case, you've apologized and offered to solve the problem, but you've also encouraged Mae to talk about what's going on under the surface. In the long run, that will probably be more important to her than simply getting some extra time with you. If she expresses feelings of anger or disappointment, you could ask about other things you might have said or done that upset her as well.
Chapter 11
319
Find truth in what she says and acknowledge how she feels. This could be an excellent opportunity to process those feelings and develop a stronger therapeutic alliance. Inquiry Errors When patients criticize you or complain that they're not getting anywhere, you may offer to fix the problem or ask, "How can I do better?" On the surface, this response may sound kind, but it's usually counterproductive. When patients are upset, they need to express their feelings and have them validated. They don't want solutions dumped on their head right now, and it's not their responsibility to tell you how to do better. This statement may be more effective: "Can you tell me about some of the things I've done or said that turned you off?" You can ask patients to tell you more about how they're feeling, and how they view the situation. In other words, you want to open the patient up like a book. Don't shut their feelings down with offers to fix things. Of course, sometimes there are real problems that need to be solved, but it's a matter of timing. Initially, patients need the chance to vent while you listen. Later on, when they trust you and feel connected with you again, you can work together to solve the problem, if it's still appropriate. In most cases, once you listen skillfully, you won't need any further solutions. The listening is the solution. "I Feel" Statement Errors Most therapists have trouble expressing their own feelings during sessions. Feelings of shame, defensiveness, inadequacy, anger or frustration
Chapter 11
320
may seem forbidden or inappropriate. During problematic encounters with difficult patients, you may hide behind jargon or formulaic expressions because you're afraid of looking foolish, vulnerable, or unprofessional. However, when you try to cover up your feelings, you may appear phony, and the patient's attack will usually escalate. In contrast, if you share your feelings skillfully, the conflict will usually deescalate. Write down several potentially upsetting criticisms from patients and see if you can come up with effective responses that include "I Feel" Statements. Once you've gotten good at using "I Feel" Statements on paper, you can role-play with a colleague. Ask your colleague to play the role of an angry, critical patient, or a patient who feels overwhelmed and desperate. For example, your colleague may say something like, "At least my last therapist cared about me. That's more than I can say for you!" See if you can respond with an "I Feel" Statement. You might say, "Wow! I'm feeling pretty awkward right now." You would not say, "I'm ticked off," because that would be too strong, too aggressive. The Feeling Words Chart on page 321 can help. When your colleague attacks you during the role-playing, you can simply say, "I'm feeling X," where X is a word from the Feeling Words Chart. For example, you might make statements like this:
Chapter 11
321
Feeling Words Chart* Blue
Down
Unhappy
Disheartened
Sad
Disappointed
Despairing
Low
Hurt
Lost
Dejected
Miserable
Ashamed
At fault
Bad
Responsible
Discouraged
Pessimistic
Desperate
Defeated
Inferior
Inadequate
Worthless
Flawed
Second-rate
Useless
Undesirable
Incompetent
Defective
Tired
Exhausted
Weary
Fatigued
Sleepy
Drained
Worn out
Lethargic
Wiped out
Uninterested
Bored
Turned off
Burdened
Abandoned
Alone
Rejected
Unloved
Unwanted
Isolated
Lonesome
Friendless
Worried
Afraid
Scared
Nervous
Apprehensive
Uptight
Tense
Terrified
Panicky
Fearful
Frightened
Alarmed
Foolish
Self-conscious
Flustered
Awkward
Humiliated
Mortified
Embarrassed
Timid
Overworked
Burned out
Tense
Frazzled
Pressured
Strained
Besieged
Overwhelmed
Mad
P. O.'d
Ticked off
Irate
Resentful
Irritated
Incensed
Annoyed
Upset
Furious
Enraged
Aggravated
Picked on
Put down
Insulted
Judged
Blamed
Intimidated
Defensive
Condemned
Stuck
Thwarted
Stymied
Envious
Mistrustful
Suspicious
Depressed
Depression
Guilty Hopeless
Unmotivated Lonely
Anxiety
Anxious
Shy Stressed
Anger
Angry
Criticized Frustrated Jealous
* Copyright
Paranoid
1989 by David D. Burns, M.D. Revised 1992, 2000, 2003.
Chapter 11
322
"Jack, you just told me that you feel totally hopeless, and that life is not worth living. (TE) I'm feeling sad and concerned about you right now. (IF)" "April, I can see how frustrated you feel. (FE) I'm also feeling a bit uncomfortable. (IF) Let's talk this out. (IN)" "Susan, I'm surprised to hear that you're feeling so disappointed in the work we've been doing. (IF; FE)" These gentle "I Feel" Statements are designed to show the patient that you have feelings, too. Your tone of voice and body language will also be important. If you convey warmth, humility, dignity, and respect for the patient, "I Feel" Statements can be invaluable. I realize that this advice is not consistent with all schools of therapy. When I was a psychiatric resident, my psychoanalytic supervisors advised me never to reveal my feelings. I was told to be like a mirror, and only to reflect back what my patients said to me. I found this rule unnatural, and too restrictive. At times, it seemed hurtful to the patient, too. It can often be helpful to show patients that you're human, but you have to do this skillfully and ethically. Remember the three ethical guidelines when you use "I Feel" Statements: Avoid "You" statements, such as, "You're making me upset." Remember to use low-key, professional language, such as "I'm feeling a bit awkward right now," rather than "I'm feeling pissed off!" Your goal should always be to help the patient, and not to help yourself. Stroking Errors
Chapter 11
323
When you're at odds with a patient, it's easy to use Stroking in a phony way that doesn't ring true, as a way of avoiding the patient's anger. Like any other technique, Stroking is one of the most powerful communication tools, but it will backfire if it's used as a gimmick and doesn't come from the heart. I once illustrated the Five Secrets of Effective Communication for a group of therapists in Boston. A young psychologist volunteered to play the therapist in a role-playing exercise, and one of his colleagues volunteered to play the role of an angry, critical patient with Borderline Personality Disorder. I warned the therapist that the patient would probably be angry and critical, and told him to try hard to acknowledge her anger. I also predicted that he'd be unable to do this, but advised him to try to do it anyway. The moment we started the exercise, she absolutely shredded him. The room fell silent as everyone waited to see whether he'd remember to acknowledge her anger. He turned bright red, leaned forward and said, "Thank you for sharing. I'm so proud of you for being so open and honest!" Everyone started laughing, because his pat response sounded about as genuine as a wooden nickel. And he carefully avoided any mention of her anger. Of course, this will infuriate her even more. You can't just stick your head in the sand and hope the anger will go away! In addition, he was engaged in a kind of interpersonal deception, because he wasn't feeling thankful or proud. He later admitted that he was actually feeling embarrassed, defensive and annoyed, a message that you could easily read in his body language. As a result, his response sounded patronizing and
Chapter 11
324
condescending, and certainly didn't convey any real liking or respect. I'm aware that some therapists may feel like they've already learned this material in graduate school. They may imagine they're too advanced for this kind of basic training. However, I've observed over and over that these techniques can be extremely difficult to implement in a skillful way at first, and there are a thousand ways to fail with each of them. Even the top experts sometimes have trouble. I once did a workshop on empathy training at the annual meeting of one of the Canadian psychological associations. Before the workshop began, a woman introduced herself and said she'd be attending my workshop that afternoon. She wanted me to know that she'd written several books on therapeutic empathy and would be available to help with the teaching or demonstrations during the workshop. I told her that was great, and I needed all the help I could get, since the participants were sometimes reluctant to volunteer for the role-playing exercises with angry, difficult clients. When I asked for volunteers for role-playing, she eagerly raised her hand and said she'd be happy to play the role of the therapist. Another therapist offered to play the role of the patient. Unfortunately, her responses were terrible, and she got a poor grade from the therapist who played the role of the difficult patient. She sounded stilted and artificial. And to make matters worse, when the other participants attempted to point out her errors, she tried to justify her responses in terms of the theories in her books, instead of simply acknowledging her errors and thanking them for the good feedback.
Chapter 11
325
It isn't easy for any of us to screw up in front of our colleagues or patients. If you keep your ego out of the picture, the training can be exciting as well. If you practice consistently and pinpoint the kinds of errors you typically make, your skills will rapidly improve. Before long, you'll get outstanding grades from your colleagues during the role-playing exercises, and vastly improved scores from your patients on the Therapeutic Empathy and Helpfulness scales as well. You'll enjoy your clinical work much more and you'll no longer be afraid of angry, critical patients, or failures in the therapeutic alliance.
12*
"This Therapy Sucks! You're a Dickhead!"— How to Develop Trust and Rapport with the Angry, Mistrustful Patient
In this chapter, we're going to talk about transference and countertransference from a CBT perspective. Traditionally, we're taught that patients often have distorted thoughts and feelings about their therapists. For example, they may feel hurt and angry because they're convinced that the therapist doesn't care, or is being judgmental and critical of them. This is sometimes referred to as "transference." This term means that the patient is redirecting unconscious negative feelings about their parents onto the therapist. For example, they may have felt that their father or mother was rejecting and didn't love them when they were growing up, so they expect the same from the therapist. "Countertransference" refers to our own negative feelings in reaction to
* Copyright
2004 by David D. Burns, M.D.
Chapter 12
327
the patient's transference. For example, we may feel frustrated, guilty, or annoyed with the patient for misjudging us. In this chapter, I'm going to argue that when our patients claim that we're failing them, we really are. Their perceptions of us may be distorted, but they're completely valid at the same time. I'll also show you how to understand and resolve these transference and countertransference problems using a new tool called the Revise Your Communication Style form. Think of a conflict you've had with a difficult patient. Maybe you've worked with someone who was relentlessly critical, or constantly angry and resentful. It could be any difficult interaction with a patient, including the example you recorded in Chapter 1. Once you've thought of a patient, write down one thing she or he said to you on Step 1 on the blank Revise Your Communication Style form on page 330. Try to keep it brief, and quote the patient verbatim. Don't say, "I have a patient named George who's always whining and complaining." Instead, write down one specific thing that George said to you. For example, he might have said, "Nobody understands me," or "You're not helping me." This exercise will work best if you come up with a specific, real example that didn't go well. Try to think of patient who said something that made you feel anxious, frustrated, angry, ashamed, or inadequate. If you're drawing a blank, you can simply make something up. Write down the worst thing that a difficult patient might say to you. If you prefer, you can also use a personal example that's based on a difficult interaction with a family member, friend, neighbor or
Chapter 12
328
colleague. Now write down exactly what you said next on Step 2 of the Revise Your Communication Style form on page 330. How did you respond to the patient? Write out your response verbatim. If you can't remember exactly what you said, just write down what you'd usually say. Try to keep it brief. Please take a moment now and write down what the patient said to you, and what you said next, on the Revise Your Communication form on page 330. This exchange will be absolutely invaluable as you read this chapter, and we'll come back to it shortly. I recently asked therapists at a workshop in San Diego to do this exercise. A therapist named Geoff described his interaction with an angry teenager named Jimmy he'd seen the previous day. At the start of their session, Jimmy said, "This therapy sucks! You're a dickhead!" I asked Geoff what he said next. Geoff said, "This session is over!" You can see their exchange on the Revise Your Communication Style form on page 331. When we're at odds with someone, we often see ourselves as victims and feel overwhelmingly convinced that the problem is the other person's fault. Even therapists feel this way. Although few therapists would applaud Geoff's comment, we sometimes do have a tendency to blame our patients for failures in the therapeutic alliance. We feel like we aren't responsible for the tension and conflict that the patient is complaining about. We tell ourselves that their perceptions are distorted and unreasonable. This lets us off the hook, and allows us to feel like
Chapter 12
329
we aren't responsible for the failure in the therapeutic alliance. In this chapter, we're going to assume that the opposite is true. We're going to examine our own role in the conflict. When patients are angry with us, it's almost always because we haven't really been listening or seeing the world through their eyes. In the last two chapters you learned that if you validate your patients' complaints with humility and respect, they'll suddenly see you in a new light. If you do this skillfully, they'll usually lower their defenses and begin to examine their own role in the conflict. At the top of page 332, you'll see the Good vs. Bad Communication Checklist. This table lists the three characteristics of good and bad communication. You can remember them more easily if you think of the EAR acronym, which stands for Empathy, Assertiveness, and Respect. Review Geoff's response to Jimmy on page 331 and ask yourself these three questions: Yes E = Empathy
Did Geoff acknowledge Jimmy's feelings?
A = Assertiveness
Did Geoff express his own feelings in an open, direct, and non-threatening way?
R = Respect
Did Geoff convey respect?
No
Once you've check of your answers here, summarize your analysis of Geoff's response in Step 3 on page 331. When you're done, turn to page 333.
Chapter 12
330
Revise Your Communication Style* Step 1. S/he said. Write down exactly what your patient said. Be brief:
Step 2. I said. Write down exactly what you said next. Be brief:
Step 3. Good vs. Bad Communication. Was your response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist to analyze what you wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did your response in Step 2 make the problem better or worse? Why? What will your patient think and feel?
Step 5. Revised Response. Revise what you wrote down in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
* Copyright
1991 by David D. Burns, M.D. Revised 2002.
Chapter 12
331
Revise Your Communication Style* Step 1. S/he said. Write down exactly what the other person said. Be brief: "This therapy sucks! You're a dickhead!" Step 2. I said. Write down exactly what you said next. Be brief: "This session is over!" Step 3. Good vs. Bad Communication. Was Geoff's response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist to analyze what Geoff said to Jimmy. Summarize your thinking here:
Step 4. Consequences. Did Geoff's response in Step 2 make the problem better or worse? Why? What will Jimmy think and feel?
Step 5. Revised Response. Revise Geoff's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
* Copyright
1991 by David D. Burns, M.D. Revised 2002.
Chapter 12
332
Good vs. Bad Communication Checklist* Instructions. Review what you wrote down in Step 2. Was your statement an example of Good Communication or Bad Communication?
Good Communication
Bad Communication
Empathy
1.
You acknowledge the other person's feelings.
1.
You ignore the other person's feelings.
Assertiveness
2.
You express your feelings openly and directly.
2.
You fail to express your feelings openly.
Respect
3.
Your attitude is respectful and caring.
3.
Your attitude is not respectful or caring.
The Bad Communication Checklist Instructions. Review what you wrote down in Step 2 of the Revise Your Communication Style form. How many of the following communication errors can you spot?
Communication Error
( )
Communication Error
1.
Truth – You insist that you're "right" and the other person is "wrong."
10. Diversion – You change the subject or list past grievances.
2.
Blame – You imply the problem is the other person's fault.
11. Self-Blame – You act as if you're awful and terrible.
3.
Defensiveness – You argue and refuse to admit any imperfection.
12. Hopelessness – You claim you've tried everything and nothing works.
4.
Martyrdom – You imply that you're an innocent victim.
13. Demandingness – You complain when people aren't as you expect.
5.
Put-Down – You imply that the other person is a loser.
14. Denial – You imply that you don't feel angry, sad or upset when you do.
6.
Labeling – You call the other person "a jerk," "a loser," or worse.
15. Helping – Instead of listening, you give advice or "help."
7.
Sarcasm – Your tone of voice is belittling or patronizing.
16. Problem-Solving – You ignore the feelings and try to solve the problem.
8.
Counterattack – You respond to criticism with criticism.
17. Mind-Reading – You expect others to know how you feel without telling them.
9.
Scapegoating – You imply the other person is defective or has a problem.
18. Passive-Aggression – You say nothing, pout or slam doors.
* Copyright
1991 by David D. Burns, M.D. Revised 2001.
( )
Chapter 12
333
This was Geoff's analysis of his response to Jimmy: Step 3. Good vs. Bad Communication. "My response was an example of bad communication because I didn't acknowledge Jimmy's anger or find any truth in what he was saying. In addition, I didn't express my own feelings of anger or frustration. Instead, I acted them out by kicking Jimmy out of my office. I certainly didn't convey any warmth or respect!" The Bad Communication Checklist on page 332 will help you spot the specific communication errors you made. Geoff's response in Step 2 involved Blame, Defensiveness, Put-Down, Counterattack, Scapegoating, Demandingness and Denial. Selecting communication errors from this list is more of an art than a science, so you don't have to be overly precise. The next step on the Revise Your Communication Style form is called Consequences. This is where things really get interesting. Ask yourself, "What are the consequences of the statement Geoff wrote down in Step 2? What will Jimmy think? How will he feel? How will he behave?" Please complete Step 4 on page 331 now. When you're done, turn to page 334.
Chapter 12
334
Here's Geoff's assessment of how his statement probably affected Jimmy: Step 4. Consequences. "Jimmy felt that I wasn't supporting him or helping him. He was mad and trying to tell me that the therapy wasn't working for him. I thought that his hostility was inappropriate, so I kicked him out of the office. This showed that I couldn't tolerate his anger and wouldn't listen to what he had to say. He probably felt rejected, discounted, and furious. "My response confirmed what Jimmy was complaining about because I really did act like 'dickhead.' Jimmy will conclude that the therapy really does suck because he can't even be spontaneous and open during our sessions. He'll feel like he can't trust me, because I'll punish him if he says the wrong thing." Notice that we're focusing on Geoff's errors in Steps 3 and 4, and the impact of these errors on Jimmy. It's not always easy for therapists to do this type of analysis. We may think of ourselves as empathic, but it can be tough to see the world through the patient's eyes, particularly when we're under attack. It can be especially upsetting to discover that we're triggering the very feelings and behaviors that we find so distasteful. At the same time, this discovery can be empowering. Once you see what you're doing wrong, you can fix it. This brings us to Step 5, where you revise your response to the patient, using the Five Secrets of Effective Communication on page 242. What could Geoff have said to Jimmy that would have been more effective? Remember, Jimmy has just said, "This therapy sucks! You're a
Chapter 12
335
dickhead!" Write down your Revised Response on page 331. Remember to put the techniques you're using in parentheses at the end of each sentence, using the abbreviations on page 242. If your initial effort doesn't seem very good, try again. You may have to revise your response several times before you come up with something really good. You'll have to be patient with yourself. When you've completed Step 5, turn to page 336.
Chapter 12
336
This was the Revised Response that Geoff and I came up with: Step 5. Revised Response. "You're right, Jimmy. (DT) I've actually been feeling like a dickhead in our last couple sessions, and it seems like you're pretty ticked off at me. (IF; DT; FE) Can you tell me more about how you're feeling? (IN)" Some therapists may think that it was appropriate for Geoff to set limits and to punish Jimmy for lashing out. But Geoff has repeatedly tried to set limits with Jimmy, and they're at an impasse. Everyone else tries to control Jimmy as well, and this triggers more aggressive behavior. Jimmy is being brutally open with his feelings. He's telling Geoff that he feels hurt, ticked off, and let down. Geoff could decide to view this as a gift instead of an attack. Of course, Jimmy expresses himself in a clumsy, aggressive way, so it doesn't feel like a gift! But think about it this way—Jimmy probably lashes at everybody when he feels let down or frustrated, so he never gets close to anyone. This could be Geoff's golden opportunity to change the pattern. Now I want you to return to the problem you provided on page 330 and complete the Revise Your Communication Style form. Examine what you said to the patient, and see how many communication errors you made (Step 3). Ask yourself what the impact of your response will be (Step 4). Then see if you can come up with a more effective response (Step 5). If you're like most of the therapists I've trained, you'll find that you made all three communication errors when you responded to the patient's attack. This can be disconcerting, especially when we've devoted our lives to dealing with conflict.
Chapter 12
337
It's jarring to discover that we've made every conceivable communication error— we didn't listen, express our own feelings, or convey respect to our patient. Once you come up with a more effective response in Step 5, try the roleplaying exercise in Chapter 10. Ask a colleague to play the role of the difficult patient and attack you in much the same way that the patient did. After you've responded, ask your colleague to critique you. Did you get an A, a B, a C, or a D? What did you say that was effective or ineffective? How skillfully did you use the Five Secrets of Effective Communication? Starting on page 338, you'll find ten additional problems illustrating conflicts between patients and therapists. These are real examples that therapists have provided at my workshops. Complete Steps 3 – 5 for each problem that interests you. Then you can review my answer before going on to the next problem. In these problems, I used the EAR technique when analyzing the communication errors in Step 3. However, you can use the Bad Communication Checklist if you prefer. They'll both get the job done. Don't try to do all ten problems at once! That would be overwhelming. Just try one or two and see what you think. Then you can come back to them in a couple days and try a couple more. You can learn a tremendous amount that way.
Chapter 12
338
You're a zombie! Problem. A therapist named Tom was treating a depressed 17 year-old boy named Ned. Step 1. Ned said: "I wish I could be a therapist so I could be a zombie and not have feelings, like you." Step 2. I said: "It's important for me to help you take care of your feelings." Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 348.
Chapter 12
339
Stop probing me! Problem. A therapist described an impasse with a patient named Lorraine who was suffering from Borderline Personality Disorder. Step 1. Lorraine said: "It drives me crazy when you probe me with questions over and over. You're not helping me." She looked tired, discouraged, and angry. Step 2. I said: "I ask questions because I can't just open up your head and see what's inside your mind!" This led to an argument about whether or not the therapy was helping. I wanted to say: "I can't exactly open up your head and look inside, but if I had an axe, perhaps I could give it a try!" Fortunately, I bit my tongue. Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 348.
Chapter 12
340
I don't like you. Problem. A therapist named Frieda described a typical conflict with Janine, a challenging 15 year-old patient. Step 1. Janine said: "I don't like you or want you to be my therapist." Step 2. I said: "Fine! I don't want to be your therapist. No one can deal with you!" Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 350.
Chapter 12
341
I'm a mistake. Problem. A therapist described a self-deprecating statement from a man named Chris who was suffering from depression. Step 1. Chris said: "I'm a mistake." Step 2. I said: "Is that statement rational or irrational?" Chris' head fell and he lapsed into silence. Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 351.
Chapter 12
342
I hope your father dies! Problem. A therapist described a challenging interaction with her most aggressive patient, an angry man named Richard who was suffering from Borderline Personality Disorder. Step 1. Richard said: "I hope your father dies soon, along with your mother. I hope your brother gets Parkinson's disease. I hope your husband f___s you in the ass and gives you AIDS." Step 2. I said: "Sounds like you've got all the bases covered. Did you leave anything out?" Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 352.
Chapter 12
343
You know how those blacks are. Problem. A psychologist was treating a 56 year-old patient named Walter who often made racial slurs. Walter described how frightened and upset he felt when he walked past a group of African-American teenagers who were talking in a loud and boisterous way. Step 1. Walter said: "You know how those blacks are." Step 2. I said: "I find it hard to stereotype people." Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 353.
Chapter 12
344
Don't give me that psychobabble shit! Problem. A therapist described an unpleasant interaction with a 33 year-old patient named Wayne. Step 1. Wayne said: "Don't give me that psychobabble shit!" Step 2. I said: "Help me understand exactly what you mean by that." Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 354.
Chapter 12
345
I'm dropping out. Please don't call. Problem. A therapist was taken aback when he received an unexpected phone call from his patient, John. Step 1. John said: "I'm grateful for your help but I've decided not to continue with therapy. Please don't call me at home." Step 2. I said: "It's not a good idea to leave therapy without discussing your thoughts and feelings. The effective work we've done so far deserves to be discussed in person, so we can come to closure." Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 355.
Chapter 12
346
You sided with my sister! Problem. A clinical social worker described an interaction she'd had with her patient, Lily, after she'd met with the entire family. Step 1. Lily said: "In the last session I was angry. You took my sister's side." Step 2. I said: "I'm so glad you told me. I could see how ineffective I was. I was frustrated in my search to find a way to get you to see how this pattern repeats itself over and over." Lily folded her arms across her chest and clammed up. Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 357.
Chapter 12
347
I'm not getting anywhere. Problem. A therapist described an awkward moment during his third session with a depressed patient named Diane. Step 1. Diane said: "I'm not getting anywhere." Step 2. I said: "Where did you expect to be at the end of three sessions?" Step 3. Good vs. Bad Communication. Was this response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist on page 332 to analyze what the therapist wrote down in Step 2. Summarize your thinking here:
Step 4. Consequences. Did the therapist's response in Step 2 make the problem better or worse? Why? What will the patient think and feel?
Step 5. Revised Response. Revise the therapist's response in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
You'll find the answer to this problem on page 358.
Chapter 12
348
You're a zombie! (problem on page 338) Problem. A therapist named Tom was treating a depressed 17 year-old boy named Ned. Step 1. Ned said: "I wish I could be a therapist so I could be a zombie and not have feelings, like you." Step 2. I said: "It's important for me to help you take care of your feelings." Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge Ned's feelings. He was obviously feeling frustrated and annoyed. I didn't acknowledge any truth in what Ned was saying, but implied he was wrong. A = Assertiveness. I struggled to sound professional so I could avoid being vulnerable and keep Ned in the patient role. I felt flustered, defensive, panicky and embarrassed, but I tried to hide my feelings. This is exactly what he accused me of in the first place. Furthermore, when I say I'm going to "help" him "take care" of his feelings, it sounds like he's some kind of invalid, and I'm going to try to save him! R = Respect. I sounded condescending and phony. Step 4. Consequences. Ned was trying to tell me that I wasn't being warm or real, and I responded in a stiff, wooden way. My response will make him feel even more convinced that what he's saying is true, because I sound like a bucket of psychobabble. He'll realize that I'm being fake and evasive. I'm acting like a zombie without any feelings! Step 5. Revised Response. "Wow! (IF) I'm embarrassed to admit it, but I think I was acting fake and trying to sound professional instead of just admitting that I was feeling uncomfortable. (DT; IF) I can imagine you're pretty annoyed with me. (FE) Let's talk about it. (IN)" Comment. This young man wants his therapist to act like a human being. The challenge is to express your feelings in a way that maintains professionalism but conveys warmth, respect and vulnerability at the same time.
Stop probing me! (problem on page 339) Problem. A therapist described an impasse with a patient named Lorraine who was suffering from Borderline Personality Disorder. Step 1. Lorraine said: "It drives me crazy when you probe me with questions over and over. You're not helping me." She looked tired, discouraged, and angry. Step 2. I said: "I ask questions because I can't just open up your head and see what's inside your mind!" This led to an argument about whether or not the therapy was helping.
Chapter 12
349
I wanted to say: "I can't exactly open up your head and look inside, but if I had an axe, perhaps I could give it a try!" Fortunately, I bit my tongue. Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge Lorraine's feelings. She was clearly frustrated and fed up with me. A = Assertiveness. I didn't express my own feelings of frustration. Instead, I got defensive. R = Respect. My response sounded patronizing. I accused Lorraine of being wrong. Step 4. Consequences. My response convinced Lorraine that I really wasn't helping her. We ended up arguing, and the session went downhill from there. I fell into the rejecting, distancing role I'd been trying so hard to avoid. This proved that her criticism was valid, and she left the session feeling like she'd been right all along. Step 5. Revised Response. "You're right, Lorraine, it seems like I have been asking a lot of questions, and it must be driving you nuts. (DT; FE) I'm also frustrated because I feel like I haven't done a very good job of connecting with you. (DT; IF) Let's talk about it and see if we can get back on track. (IN; Positive Reframing)" Comment. In the Revised Response, the therapist agrees that things haven't been going well and that her questions haven't been helpful. This will be music to Lorraine's ears. Lorraine is aggressive. She pushes people away, and they always take the bait. They get defensive, and the relationship deteriorates. When the therapist agrees with Lorraine's criticisms, it will open the door to a more meaningful relationship. Most therapists try to hide their feelings when they feel defensive or awkward. This can be a mistake because you may look like a phony, and your patient will intensify the attack in order to try to knock you off your high horse. When the therapist says, "I'm also frustrated because I feel like I haven't done a very good job of connecting with you," she sounds human. She's expressing her feelings in a low-key manner that won't threaten Lorraine. You could argue that it may be premature for the therapist to express her own feelings of frustration, because Lorraine feels so raw and angry right now. Perhaps the statement, "I feel like I haven't been connecting with you nearly as well as I'd like," would be sufficient for the moment. Later on, when Lorraine feels more relaxed and trusting, the therapist can be more open. Of course, she'll still need to express her feelings in a non-threatening, respectful way. At the end of the Revised Response, the therapist reframes the alliance failure as an opportunity to talk and get things back on track. Like any technique, Positive Reframing has to be used in a genuine way, or it will backfire. If you're trying to hide your own feelings of defensiveness or frustration, Positive Reframing may fail, because you'll sound phony.
Chapter 12
350
I don't like you. (problem on page 340) Problem. A therapist named Frieda described a typical conflict with Janine, a challenging 15 year-old patient. Step 1. Janine said: "I don't like you or want you to be my therapist." Step 2. I said: "Fine! I don't want to be your therapist. No one can deal with you!" Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge Janine's feelings. She was feeling frustrated and angry with me. A = Assertiveness. I didn't express my feelings. I was feeling exasperated. R = Respect. My response was disrespectful and rejecting. It was a strong put-down. Step 4. Consequences. I confirmed that Janine's criticism was valid. She implied that I wasn't effective, and I counterattacked. She'll feel hurt and alienated, since even her therapist won't listen or tolerate her anger. Her attack will probably escalate, since I haven't acknowledged how she's thinking or feeling. Janine may be a challenge, but I'm provoking her to become even more hostile and unreasonable. Step 5. Revised Response. "Janine, it sounds like you're really ticked off. (FE) Can we talk about it? (IN) I agree that the therapy hasn't been going very well, and I want to know what I did that turned you off. (DT; IN) If you still want to leave after we've talked things over, I can help you find someone else to work with, but I'm hoping that you'll decide to stay, because I'm very committed to you. (IF; ST)" Comment. Janet has invited Frieda to engage in battle, and Frieda has accepted the invitation. Janine seems to be saying that they're not working together in a meaningful way. She may also be saying that she doesn't feel accepted. These messages sounded so threatening to Frieda that she lashed out at Janine. Her initial response sounded hostile and unprofessional, and confirmed what Janine was saying. Most of us struggle to resist the negative roles our patients cast us in, but we end up taking the bait. In the Revised Response, Frieda agrees that she hasn't done a good job and encourages Janine to talk. Janine will probably relax and open up because Frieda is listening. Frieda emphasizes her desire to work with Janine, but expresses a willingness to refer her to another therapist if she still feels upset after they've discussed the problem. Janine will probably want to stay because she'll see that her therapist is easy to talk to, and isn't trying to control her. Frieda's tone of voice and body language will be crucial. If she sounds defensive or hurt, even the right words will fail. But if she conveys warmth, humility, and genuine curiosity, the likelihood of a positive outcome is high.
Chapter 12
351
I'm a mistake. (problem on page 341) Problem. A therapist described a self-deprecating statement from a man named Chris who was suffering from depression. Step 1. Chris said: "I'm a mistake." Step 2. I said: "Is that statement rational or irrational?" Chris' head fell and he lapsed into silence. Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge how worthless and hopeless Chris was feeling. Instead, I implied that his feelings were irrational or "wrong." A = Assertiveness. I felt sad and concerned when Chris said he was "a mistake." I didn't express my feelings, but struggled to maintain an emotionally distant, professional facade. R = Respect. My response was disrespectful because I didn't acknowledge how demoralized Chris was feeling. Instead, I pretended to be the expert. Step 4. Consequences. My response lacked compassion. It will convince Chris that he is, in fact, a "mistake," since I implied that he'd just made another "mistake." He'll feel even more depressed and lonely, since even his therapist ignores his feelings. Something real was happening in the room. We were both feeling awkward. But instead of talking about these feelings, I put up a wall and pushed him away. Chris probably felt belittled and discounted. In fact, he hung his head. Step 5. Revised Response. "Chris, it makes me sad to hear you say that. (IF) It must feel awful to feel like you're a mistake. (TE; FE) I can imagine that you're probably struggling with feelings of worthlessness, loneliness or emptiness. (FE) Did something happen since I last saw you that made you feel overwhelmed or frustrated, or is it simply the depression eating away at you? (FE; IN) I'm really concerned, and want to hear more about how you're feeling. (IF; IN; ST)" Comment. Family members and therapists alike often make the mistake of trying to argue with a depressed person's irrational self-criticisms. This strategy is doomed to failure, because you'll overlook the intensely painful feelings and problems the person is struggling with. Many people make the equally bad mistake of trying to cheer the person up or point out his or her strengths. This almost never works, because it sounds patronizing. When people are overwhelmed, they need a listening ear, and not advice, logic, or reassurance. Once Chris has had the chance to get his feelings off his chest, and he feels validated, he and his therapist can work together to attack the problems he's struggling with. But we need more information first. Why is Chris so despondent today? Does he feel upset about something that happened at school? Did he have an argument
Chapter 12
352
with a friend? What's happening? Right now, we have nothing to go on. You may think that this therapist's initial response was incredibly inept, and feel like you'd never respond in such a cold manner. However, I've seen many therapists make similar errors when confronted by patients who are self-critical or upset. Chris sounded desperate. His therapist got panicky and thought he had to say something therapeutic, when all he really had to do was tune in to how Chris was thinking and feeling.
I hope your father dies! (problem on page 342) Problem. A therapist described a challenging interaction with her most aggressive patient, an angry man named Richard who was suffering from Borderline Personality Disorder. Step 1. Richard said: "I hope your father dies soon, along with your mother. I hope your brother gets Parkinson's disease. I hope your husband f___s you in the ass and gives you AIDS." Step 2. I said: "Sounds like you've got all the bases covered. Did you leave anything out?" Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge Richard's feelings. He sounded extremely angry. A = Assertiveness. I felt attacked. Instead of expressing my feelings, I fought back with sarcasm. R = Respect. I tried to put Richard down. I was competitive, and didn't convey any respect. Step 4. Consequences. I played the game that Richard invited me to play. Instead of asking about why he was so upset with me, I engaged him in a childish battle. I must have done something that enraged him. Maybe he felt that I wasn't treating him with respect. When I attacked him, I showed that I didn't respect him, and wasn't worthy of his respect. I accepted his invitation to play the role of enemy. Step 5. Revised Response. "Richard, I'm feeling blown away by what you just said. (IF) I can see that you're really ticked off, and I know that I must have said or done something that upset you. (DT; FE) Can you tell me what happened? (IN)" Comment. This therapist felt hurt and angry. Her initial response was defensive and passive-aggressive. The Revised Response is short. Richard feels enraged, and it will be important to give him some space so he can get his feelings off his chest. If she gets defensive, he is attack will escalate. In contrast, if he feels validated and listened
Chapter 12
353
to, he'll be far more receptive to her thoughts and feelings.
You now how those blacks are. (problem on page 343) Problem. A psychologist was treating a 56 year-old patient named Walter who often made racial slurs. Walter described how frightened and upset he felt when he walked past a group of African-American teenagers who were talking in a loud and boisterous way. Step 1. Walter said: "You know how those blacks are." Step 2. I said: "I find it hard to stereotype people." Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. Walter was feeling threatened by the teenagers, but I didn't acknowledge his feelings. A = Assertiveness. I was feeling uncomfortable and annoyed. I was unsure about how to respond, so I didn't express my feelings. Instead, I put him down and implied that I was morally superior. My anger came out indirectly. R = Respect. My response was not respectful. I sounded judgmental and holier-than-thou. Step 4. Consequences. Walter will sense that I'm putting him down, and he'll probably feel defensive. He sees people in a polarized way, and yet I'm polarizing my interaction with him. He thinks black people are inferior, and I'm letting him know that I feel the same way about him. This won't win him over to my point of view, and it won't lead to any teamwork or trust. Step 5. Revised Response. "Walter, I'm feeling a bit uncomfortable. (IF) It sounds like you had an upsetting interaction with those kids, and that you have some negative feelings about people who are black. (TE; FE) This is a little hard for me to hear, but I know those kinds of feelings can be powerful. (IF) Can you tell me what happened when you passed the kids on the street, and how you were feeling? (IN)" Comment. You may be thinking that you shouldn't have to accept someone who's so prejudiced, and may feel the urge to reject Walter. Of course, you're not obligated to work with any patient if your own feelings are getting in the way of effective therapy. When in doubt, obtain a consultation from a colleague with expertise in ethics. Make sure that you document the consultation and the basis for your decision in the chart. At the same time, we often have to work with people who are different from us, and most of our patients will express all kinds of illogical beliefs. You can't put him down and expect to do effective therapy. The therapist's initial response was an attempt to censure Walter. We sometimes fall into the trap of preaching or lecturing our patients. This is rarely effective because patients feel judged and put up walls.
Chapter 12
354
In the Revised Response, the therapist acknowledges some discomfort without sounding judgmental or moralistic. Walter will be able to save face and they can continue working together. Ultimately, you'll have the greatest leverage if your patients like you and feel accepted.
Don't give me that psychobabble shit! (problem on page 344)
Problem. A therapist described an unpleasant interaction with a 33 year-old patient named Wayne. Step 1. Wayne said: "Don't give me that psychobabble shit!" Step 2. I said: "Help me understand exactly what you mean by that." Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge Wayne's frustration and anger, or acknowledge that what he was saying was true. I used Inquiry. While this might have sounded professionally "correct," it was defensive. My response implies that Wayne hasn't made himself clear. But his statement was crystal clear! A = Assertiveness. I was feeling cornered and embarrassed. Instead of expressing my feelings, I gave Wayne more psychobabble. I might just as well have said, "Thank you for sharing." I tried to hide my feelings and resorted to a formulaic response I learned in graduate school. R = Respect. My response sounded condescending and evasive. Wayne was annoyed, and I knew exactly what he meant—he was trying to tell me that I sounded phony and that I wasn't being real. Step 4. Consequences. Wayne will conclude that I'm not very genuine, and that all he can expect from me is more "psychobabble shit." Step 5. Revised Response. "Wayne, I'm embarrassed to have to admit that you're right. (IF; DT) I was lapsing into psychobabble just now. (TE; DT) I was feeling awkward, but instead of admitting it, I tried to sound professional. (IF; DT) I can imagine that you're feeling pretty annoyed with me. (FE) Can we back up and try again? (IN)" Comment. Therapists frequently respond to critical patients with trite expressions like, "You say that . . . " or "I hear you saying that . . . " or "I can see how you might feel that way." This is not genuine empathy, but a gimmick, an evasion, or a subtle put-down. When patients accuse you of sounding like a parrot, it's nearly always because you didn't use an "I Feel" Statement. If you tell the patient how you're feeling, you'll no longer sound like a phony.
I'm dropping out. Please don't call. (problem on page 345)
Chapter 12
355
Problem. A therapist was taken aback when he received an unexpected phone call from his patient, John. Step 1. John said: "I'm grateful for your help but I've decided not to continue with therapy. Please don't call me at home." Step 2. I said: "It's not a good idea to leave therapy without discussing your thoughts and feelings. The effective work we've done so far deserves to be discussed in person, so we can come to closure." Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge John's feelings. He may have been feeling anxious, disappointed, depressed, frustrated, or annoyed. A = Assertiveness. I felt surprised and upset, but didn't express my feelings. Instead, I implied that John was wrong. R = Respect. I tried to sound professional, but didn't convey any real respect. I put up a wall instead of listening to what John was trying to tell me. My response was condescending. Step 4. Consequences. John is saying that he doesn't want to continue his therapy with me. Obviously something happened. Maybe I did or said something that upset him. Maybe he feels like the therapy hasn't been especially helpful, in spite of his polite statement of gratitude. Perhaps he feels that I'm too controlling or intrusive, since he says he doesn't want me to call him at home. Maybe he feels like I can't tolerate any criticism, so he's decided to avoid the conflict rather than talking it out. Possibly there's been some kind of crisis at home, or a family member doesn't like the fact that he's in therapy. He may even be feeling suicidal and calling me to say goodbye. When John said he was dropping out of therapy, I sounded patronizing and implied that I knew what was best for him. I lectured him instead of asking for more information. I confirmed that his criticism was valid because I'm attempting to control him, and I'm not listening. He'll almost certainly conclude that dropping out is the right decision! Step 5. Revised Response. "John, I'm surprised. (IF) I had no idea you were thinking about dropping out of therapy. (IF; TE) I'd hate to see you disappear without knowing what had happened or having the chance to talk things over. (IF; ST) Can you tell me what's going on? (IN) Did I say or do something that turned you off? (IN) Have you been feeling stuck or frustrated? (IN) Is there a crisis at home? (IN) Are you feeling desperate or hopeless? (IN)" Comment. The Revised Response begins with a gentle "I Feel" Statement. This will be more effective than lecturing the patient. The Revised Response also utilizes Multiple Choice Empathy. When you have no idea where the patient is coming from, and they're reluctant to tell you, you can suggest several possibilities. It's like priming a pump. You have to do this in a way that sounds supportive and concerned, and not demanding. There's no guarantee that this approach will be effective, but you'll have an excellent chance
Chapter 12
356
of finding out what's going on. If John responds positively to your inquiry, you can propose an additional session to try to resolve the problem. You can agree to terminate the therapy or refer John to a different therapist if he's still dissatisfied after you've talked. Premature termination is common. In most clinical settings, 25% – 75% of patients drop out of therapy unexpectedly. Many of them simply stop showing up, and their therapists never find out what happened. This is a serious problem. Obviously, the therapy cannot be effective if the patient drops out. If you educate patients about premature termination at the beginning of therapy, you won't have to struggle so hard to pick up the pieces after the fact. You may recall the discussion of the "How to Make Therapy Successful and Rewarding" memo on page 110. I send this memo to every new patient prior to the initial evaluation, along with the Brief Mood Survey and some other educational materials. The memo describes several common reasons why patients might feel the urge to drop out of therapy, including: Lack of Rapport. You may not like or trust your therapist. Feeling Judged. You may feel like your therapist is too judgmental. Conflict Phobia. You may not be comfortable with conflict and may have the urge to drop out of therapy if you develop some negative feelings about the therapist. Therapeutic Niceness. If your therapist seems too "nice," you may drop out of therapy because you don't want to hurt his or her feelings. Therapeutic Defensiveness. Your therapist may have gotten defensive when you tried to express doubts or negative feelings about the treatment. Shame. You may feel ashamed about some problem that you haven't disclosed, like drug abuse or a sexual difficulty. Hopelessness. You may feel stuck or discouraged and think that the therapy couldn't possibly help. Sudden Improvement. You may suddenly improve and conclude that you don't need any more treatment because your problems seem to be gone for good. Relapse. You may improve and then experience a relapse, and suddenly feel frustrated, hopeless and defeated again. Financial Problems. The therapy may seem too expensive or burdensome. Coercion. You might have been pressured to come to treatment by a friend or family member, but weren't completely committed to the idea in the first place. Patients indicate which reasons seem like they might apply to them. For example, here are the response options for Conflict Phobia:
Chapter 12
357
Conflict Phobia Some people avoid conflict and sweep their feelings under the carpet. Is it hard for you to talk things over when you feel upset with someone? 1. ____
I do not find it difficult to express negative feelings.
2. ____
It's somewhat difficult for me.
3. ____
It's moderately difficult for me.
4. ____
It's extremely difficult for me.
If you felt mistrustful or upset with your therapist, would you be inclined to drop out of therapy between sessions? 1. ____
I would not drop out between sessions if I felt upset.
2. _____
There's a slight chance I'd drop out if I felt upset.
3. ____
There's a moderate chance I'd drop out.
4. ____
It's very likely that I'd drop out.
At the end of the memo, patients are asked whether they'd be willing to agree to come in for one additional session if they have the sudden urge to drop out of therapy between sessions. If patients seem perplexed, I explain that therapists and patients should both be bound by the same kinds of ethical considerations, and that I wouldn't abruptly terminate them between sessions and then refuse to meet with them to discuss why. Very few patients have ever declined treatment after this discussion. Although this approach is not foolproof, it has reduced premature terminations significantly. Over the years, quite a few patients have told me that they had the urge to drop out of therapy, and then remembered that they'd agreed to come in for one additional session to discuss what was going on. These sessions were nearly always very productive.
You sided with my sister! (problem on page 346) Problem. A clinical social worker described an interaction she'd had with her patient, Lily, the week after she'd met with the entire family. Step 1. Lily said: "In the last session I was angry. You took my sister's side." Step 2. I said: "I'm so glad you told me. I could see how ineffective I was. I was frustrated in my search to find a way to get you to see how this pattern repeats itself over and over." Lily folded her arms across her chest and clammed up. Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I ignored Lily's anger and subtly discounted her claim that I
Chapter 12
358
was taking her sister's side. A = Assertiveness. I said I was feeling "glad," but I was really feeling defensive. Then I implied that she was causing the conflicts in her relationships, and made it sound like it was her fault. My response was passive-aggressive, since I was annoyed, but pretended that I was trying to be helpful! R = Respect. My response didn't ring true, because I was putting Lily down and pretending to be on her side at the same time. Step 4. Consequences. I confirmed Lily's claim that I don't support her, since I failed to support her again. I implied that she really was to blame, but hadn't yet seen the light. When she crossed her arms and clammed up, she was showing that my comment made her feel frustrated, hurt, and angry. Step 5. Revised Response. "I think you're right, Lily. (DT) I think I did take your sister's side during the last session, and that's not fair. (TE; DT) I can see why you're feeling angry with me. (FE; DT) Let's talk about it. (IN)" Comment. The first two sentences of the therapist's initial response sounded phony, and the third sentence sounded blaming and condescending. What the therapist meant was, "Lily, I've been frustrated in my attempts to get you to see how wrong you are. But being a very stubborn and defensive person, you can't stand to hear the truth about yourself." Lily heard this message loud and clear. Of course, this is the kind of scapegoating that she was complaining about in the first place. Although the therapist's statement, "I could see how ineffective I was," may sound disarming, it wasn't genuine. The therapist implied that her only real "ineffectiveness" resulted from the fact that she couldn't get Lily to stop being so stubborn. Of course, Lily does provoke hostility when she interacts with her sister and family members. She may have trouble getting along with nearly everyone. But she's highly defended and isn't ready to examine her role in these conflicts at this moment. When a patient is angry and resisting, empathic listening is the only effective response. Once Lily feels supported and trusts her therapist, they can negotiate the therapeutic agenda. What does Lily want to work on, and how motivated is she to work on it? Does she really want to work on the conflict with her sister, or is there some other problem that she'd prefer to work on?
I'm not getting anywhere. (problem on page 347) Problem. A therapist described an awkward moment during his third session with a depressed woman` named Diane. Step 1. Diane said: "I'm not getting anywhere."
Chapter 12
359
Step 2. I said: "Where did you expect to be at the end of three sessions?" Step 3. Good vs. Bad Communication. This was bad communication because: E = Empathy. I didn't acknowledge Diane's feelings. She was probably feeling stuck, discouraged, frustrated, and disappointed. A = Assertiveness. I felt surprised, confused, and defensive. Instead of admitting how I felt, I reminded Diane that I was the expert and she was the patient. R = Respect. My response was patronizing and disrespectful. It was a thinly veiled put-down. Step 4. Consequences. Diane was trying to tell me that she was disappointed in the therapy. I implied that her expectations were unrealistic. I showed her that I wasn't very compassionate or willing to listen. She'll conclude that she was right, and that we're not really getting anywhere. Step 5. Revised Response. "Diane, it sounds like you're feeling discouraged and frustrated right now. (FE) I agree that I haven't been very helpful to you yet, and I'd like to hear more about some of the problems and feelings that are bugging you. (DT; IN) The discussion may help us get back on track. (DT)" Comment. On some level, the therapist's initial response was valid. Most patients haven't made a great deal of progress by the third session. But the therapist sounded defensive and patronizing. When he defended himself, he proved that her criticism was valid, since his response wasn't at all helpful to her. Remember the Law of Opposites: when you defend yourself against the patient's criticism, you'll actually validate it. In the Revised Response, the therapist agrees with Diane and encourages her to air her feelings. If he listens respectfully, they'll end up on the same page, and then they can begin to work together more effectively. In fact, the patient's criticism is really an opportunity to make some significant progress right now.
13*
"Doctor, I can tell that you're secretly attracted to me."
In this chapter, I'll show you how to use the Five Secrets of Effective Communication to resolve some of the most difficult problems you'll ever encounter in your career, including patients who are: Violent Sexually Provocative Boring Disgusting or repulsive When I was at the University of Pennsylvania Medical School, I supervised a psychiatric resident named David who was doing a rotation at the Philadelphia VA Hospital. One night, he received an emergency call from the locked psychiatric unit on the seventh floor. Apparently, a psychotic patient named Mohammed had gone berserk. He was shouting and threatening the staff.
* Copyright
2004 by David D. Burns, M.D.
Chapter 13
361
David rushed up to the seventh floor, along with three medical students who were assigned to work with him that evening. They found Mohammed standing in the corner of the day room next to a glass bookcase. He was a tall, muscular African-American man who was holding a wooden chair above his head and glaring at them. David asked Mohammed what the problem was. Mohammed bellowed that his doctor had promised to talk to him every day, but hadn't seen him today. The medical students were eager to help. They reassured Mohammed that his doctor was a good doctor, but was out of town for a conference and would undoubtedly see him when she returned later that week. What do you think the result of this statement was? He started screaming and smashed the bookcase with his chair. The chair and glass panels shattered. Now he was holding two broken legs of the chair in his hands like clubs. Put yourself in David's shoes. What would you say if you were in this situation? Think about it for a moment, and put your answer below. Use the Five Secrets of Effective Communication, and indicate which techniques you're using in parentheses after each sentence, using the abbreviations on page 242:
Chapter 13
362
Answer David turned to Mohammed and said, "Mohammed, I agree with you. (DT) If your doctor was going out of town, she should have told you. (DT) You have every right to feel angry. (DT; FE) I'd feel exactly the same way. (ST)" Mohammed seemed surprised and softly said, "You would?" "Of course I would," David replied. "I'm with you on this, and I want to hear about what's been happening. (ST; IN)" Mohammed sighed and said, "Well, it's about time!" He set the two broken chair fragments on the floor, sat down, and began to talk about all the things that were bothering him. When someone is angry or abusive, it's natural to feel alarmed. Most of us feel the need to contain or control that person. Of course, if you're working on a locked unit, sometimes it will be necessary to call the security guards, and you may even have to put a violent patient in leather restraints from time to time. But ask yourself why the patient became violent and abusive in the first place. Usually, a person who's exploding feels exasperated because no one is listening, validating them or treating them with respect. In most cases, violence is just a last futile attempt to get someone to listen. As patients become more threatening and aggressive, your selection of methods becomes more restricted. "I Feel" Statements may not help your cause very much, unless you're awfully skillful. That's because the person who's enraged wants you to listen to them. They're usually not very interested in how you feel.
Chapter 13
363
Thought and Feeling Empathy may not be effective, either. If the patient is shouting or acting out in an obvious way, a comment like, "I can see how angry you feel," may sound patronizing and provoke more hostility. Of course, this will depend on your tone of voice to some extent. But the bottom line is this: the Disarming Technique and Stroking will usually be the most important techniques when someone is on the verge of exploding. Once they begin to calm down and trust you, you can weave the other communication techniques in again. Theory is one thing, practice is quite another. The best way to learn how to use these techniques is with the role-playing exercise described in Chapter 10. Ask a colleague to play the role of a patient who's enraged and to attack you verbally. Then respond as effectively as you can, and ask your colleague for feedback, so you can see exactly what you did right and what you did wrong. Do role-reversals until you can both come up with outstanding responses. Although anger can be challenging, sexual transference can be even more anxiety-provoking because it feels embarrassing and shameful. Furthermore, this topic is almost never included in psychotherapy training programs. When the patient makes a sexually provocative statement, it may come as a shock. In fact, sexual transference may be the most difficult and sensitive problem that therapists have to confront. Learning how to respond effectively requires about four hours of small group training. My Stanford students have told me that this topic isn't covered in any practical way in their textbooks or classes, so they appreciate this kind of training. Let's say that your patient says, "I can see that you're secretly attracted to
Chapter 13
364
me." What would you say next? This is a difficult problem, but I'd strongly encourage you to give it a try before you turn the page. Feel free to review the Five Secrets of Effective Communication on page 242. Remember to put the names of the techniques you're using in parentheses after each sentence:
Chapter 13
365
Answer You could respond like this: "Roxy, I know that your relationships with men have been a source of pain and disappointment for you, and that you've often felt exploited by the people you cared about. (FE; DT) I want to reassure you that I have great respect for you and I have no intention of taking advantage of you or hurting you in any way. (IF; ST) Still, I'm concerned that I may have projected the wrong message and made you feel uncomfortable. (IF; DT; FE) Can you tell me more about how you're feeling, or what I might have done or said that made you uncomfortable? (IN; FE)" Of course, your response will depend on the patient and on the nature of your interaction. Roxy needs to be reassured that you're not trying to seduce or exploit her. At the same time, you're using the Disarming Technique in a sophisticated way. You're acknowledging that you've failed to make her feel safe, since she senses a lack of trust and feels like you may be trying to take advantage of her. It would be easy to use the Disarming Technique inappropriately. For example, the statement, "As a matter of fact, I do find you attractive," might lead to an ethics complaint or a malpractice suit! In an attempt to avoid that error, you might make the opposite mistake and say, "No, I don't find you attractive." This would be hurtful. It sounds like a put-down, and implies that if she were more attractive, you might have a sexual interest in her! It's also defensive, and misses
Chapter 13
366
the point. There are several patterns of sexual transference, each involving slightly different dynamics. You could have a male patient with a female therapist, a female patient with a male therapist, or a patient and therapist of the same gender. In each case, the patient could express an attraction to the therapist or claim that the therapist is attracted to him or her. Imagine that a male patient expresses sexual feelings for a female therapist. He might say, "I feel like there's some special chemistry between us. Perhaps we can get together for a private session tonight when you're done with your patients." How would you respond if you were the therapist? Put your ideas here before you continue reading:
Chapter 13
367
Answer Notice that some hostile feelings may be lurking behind comments like these. The patient is demeaning his therapist and reducing her to a sex object. You could respond along these lines: "You know, Lars, I'm flattered, but therapy is different from other kinds of relationships. (ST) At the same time, I want you to know that it's okay to talk about any feelings that come up during our work together. You've told me about your difficulties forming rewarding relationships with women, and I can imagine that you might be feeling lonely and frustrated. (TE; FE) Can you tell me more about how you're feeling right now? (IN)" This response creates a clear boundary without putting Lars down or pushing him away. If you just issue a stern rejection or rebuff, he'll feel hurt, and you'll be recreating the scenario that brought him to therapy in the first place. He may even feel the urge to pursue you more intensely because you'll seem desirable and unavailable. Here's another scenario. A female patient expresses sexual or romantic feelings for her male therapist. She might say, "I'm wondering if you ever meet with your patients socially? Maybe we could get a cup of coffee together sometime." What would you say next? Put your ideas here before you continue reading:
Chapter 13
368
Chapter 13
369
Answer This patient may tend to seek out inappropriate romantic relationships, such as with married men. Why is she so strongly attracted to men who are unavailable to her? Her attraction to her therapist may provide an opportunity to focus on this issue. Here's one approach: "Laura, I don't meet with patients socially, but it's natural for all kinds of feelings to surface in a therapeutic relationship. Sometimes, it takes courage to talk about these feelings, but it can be helpful. (Positive Reframing) You've told me that you've fallen into the trap of developing relationships with men who weren't available, and then ended up feeling hurt and disappointed. (TE; FE) Can you tell me more about how you're feeling right now? (IN)" You can practice these scenarios with the help of a colleague, using the role-playing exercise described in Chapter 10. Ask your colleague to play the role of a sexually provocative patient, and you can play the therapist. After you respond, ask your "patient" to critique your response using these three criteria: Did you get an A, a B, or a C? Did you blow it and get an F? What did you say that was effective or ineffective? How did your "patient" feel when you responded? Did you use the Five Secrets of Effective Communication skillfully? At first, you may panic and find it extremely difficult to come up with effective responses. Use lots of role-reversals. It usually takes considerable trialand-error before you learn to respond skillfully. If you maintain a sense of humor
Chapter 13
370
while you're learning, it will make the process a lot less traumatic. At one of my intensive workshops in Philadelphia, I asked a female therapist to play the role of the patient, and invited four male therapists to try to respond to one sexually provocative statement. She said this to each of them, one at a time: "I've sensed a special kind of chemistry between us. I find you very attractive." The first three therapists found the statement intensely embarrassing and responded lamely. The fourth therapist was a shy, handsome young psychologist who was training at the Center for Cognitive Therapy. When it was his turn to respond, he turned bright red and seemed to get excited. He said, "Really? What is it about me that you find especially attractive?" Everyone in the room laughed. Although it was funny, it wouldn't exactly be a home run with the local ethics committee! What would you have said if you were the therapist? Sexual transference and countertransference can be tough to handle because they're so emotionally charged. But sometimes, you have the opposite problem. What do you do when you're stuck with a boring patient? This question often comes up in workshops. I believe that honesty is the best policy. If you express your feelings in a respectful way, the problem will instantly disappear. However, you'll have to do this in a way that will be flattering to the patient, so she or he won't lose face. Let's say that you've been treating a stockbroker named Tony. The therapy started out pretty well, and Tony began to open up about a number of
Chapter 13
371
personal issues. But for the past few sessions, he's been rattling on about the stock market, and you're bored. You're not even interested in the stock market, and your mind is wandering. You could say something like this: "Tony, I've noticed that during the past couple sessions, we've been talking about things that don't seem entirely relevant to your problems, like the stock market. Sometimes, I've even had trouble concentrating, and I find that my mind is wandering. This is surprising, since the problems you described at your initial evaluation several weeks ago were so compelling. You mentioned tremendous feelings of grief over the death of your daughter. You also mentioned the conflict with your wife and your struggles with alcohol. I felt very connected to you. Now I'm wondering why we've drifted away from those issues. Have you noticed this?" Once you've respectfully acknowledged that the therapy has drifted into unproductive territory, the conversation will immediately become dynamic and you won't feel bored any more! Make sure that your comments don't sound hurtful or insulting. The trick is to reframe your feelings of boredom in a positive way so you can explore why it's happening. Is Tony feeling ashamed about something? Did he give in and have a drinking binge he hasn't told you about? Does he feel like he can't trust you? Is he ambivalent about changing? Why aren't you rolling up your sleeves and working together productively? Addressing feelings of boredom will require courage, but what should you say or do if you have a patient who's totally repulsive or disgusting? Most
Chapter 13
372
therapists try to hide their negative feelings, but this may not be effective because you won't come across in a warm and spontaneous way. There will be tension in the air. You can't really fake it, and your feelings of annoyance or dislike may come out indirectly. For example, you may say or do things that subtly push the patient away, and you may miss out on an opportunity for an important therapeutic breakthrough. Some experts would argue that you should simply refer the patient to a colleague, and there may be times when this is necessary because you simply can't work with a particular patient. But I've found that when I discuss these feelings with patients in a respectful way, I nearly always start to enjoy working with them. Of course, that's not always easy! How are you going to share your feelings in a way that isn't threatening to your patient? You can't exactly say, "Hey, Jimbo, I find you totally disgusting!" Connecting with a patient who turns you off requires a bit more thoughtfulness and courage. I once treated an obese 23 year-old man named Hank who suffered from feelings of loneliness and depression. Hank worked as a construction laborer. He drank heavily, had few friends, and lived with his parents. Hank looked disheveled and came to his sessions reeking of urine. When he left the office, the chair he was sitting on smelled of urine. In fact, patients started hinting that my office had a bit of a strong smell, and I was worried that they might think I'd peed in my pants. It usually took a week for the smell to clear and by then, Hank would return for his next session.
Chapter 13
373
In addition, Hank talked about things that I found abhorrent. For example, he'd laugh about how much fun it would be if he and I could hang out together and rape women. I felt disgusted, but was struggling to get up the courage to discuss the problem. What could I say to Hank that wouldn't hurt his feelings or cause him to drop out of therapy? After procrastinating and feeling anxious for several weeks, I finally bit the bullet and forced myself to say something along these lines: "Hank, there's something that I need to tell you. This is hard for me to say, and I definitely don't want to hurt your feelings, but here it is. I don't know how often you bathe, or if you're even aware that sometimes you have a pretty strong odor. It even stays on the furniture after you leave, and some of my patients have complained about it. It's bothered me, too. "In addition, when you say how much fun it would be for us to go out and rape women, I'm not sure if you've considered how I might feel about that. In fact, I find the topic pretty upsetting. "I've also noticed that you're not doing any of the psychotherapy homework assignments, and I'm concerned that we're not making the kind of progress you came here for. "But then I got to thinking about this, and something really intriguing popped into my mind. Here you are, struggling with feelings of loneliness, and I like you, but I feel pushed away and I sometimes dread our sessions. Do you see what I mean? I got kind of excited when I
Chapter 13
374
thought about it like that. "I want to emphasize how much I respect you and appreciate the chance to work with you. But at the same time, I felt like it was important to clear the air so we could start to work together as a team." Hank accepted this message gracefully, and didn't seem at all perturbed. Much to my surprise, he came to his next session all cleaned up and looking good, and had been working hard on his psychotherapy homework for the first time. I began to look forward to our sessions, and our work together suddenly became productive and successful. I suspect this happened because I became genuinely excited when it dawned on me how paradoxical his behavior was. On the one hand, Hank was asking for help with loneliness, and yet he was pushing me away. This insight allowed me to reframe the conflict in terms of the core problem that had brought him to therapy in the first place. In addition, when I conveyed my negative feelings in a direct and respectful way, without any hostility, I think Hank felt cared about. He could see that I wasn't going to judge or reject him, and I wasn't going to act fake and hide my feelings. Most human beings have a deep need for acceptance and respect. However, if it doesn't come from the heart, your words won't be effective, no matter what techniques you use.
Part Five A = AGENDA SETTING The KEY to Therapeutic Success A-TEAM
Assessment Assessment
Testing Testing
Methods
Empathy
Agenda Agenda Setting Setting
14*
Motivating the Unmotivated Patient
Let's assume that you've taken a superb clinical history and completed the Axis I and II diagnostic screening. You're using the Brief Mood Survey or some comparable instrument to track therapeutic progress at every session, and your scores on the Therapeutic Empathy scale confirm that you've developed a warm, trusting therapeutic alliance. The patient trusts you and expresses feelings openly at every session. So far, so good. However, your patients still won't make any progress unless they're motivated and working hard to change their lives, both during and between sessions. This brings us to the fourth component of our A-TEAM model—Agenda Setting. When you set the therapeutic agenda, you move beyond the talking and listening phase of the treatment into the active, problem-solving phase. You pinpoint one specific problem the patient wants help with, conceptualize the nature of the problem, head the resistance off at the pass, and select the tools * Copyright
2003 by David D. Burns, M.D.
Chapter 14
377
that are most likely to be helpful for that problem. Agenda Setting may sound easy or trivial, but it's the most challenging and powerful psychotherapy technique of all. I once treated a woman named Jackie who became severely depressed after she discovered that her husband, Lyle, was having an affair with his secretary. She felt worthless and hopeless, and was convinced that she could never be happy without Lyle's love. In spite of the desperation she felt, Jackie was strongly motivated to overcome her depression, and agreed to do an unusual experiment to test her belief that she needed Lyle's love to feel happy and fulfilled. One Saturday afternoon, she imagined that she was having a special and important guest over for dinner, even though she knew she'd be eating by herself. She prepared a gourmet meal, lit candles and played her favorite music while she ate. After dinner she danced alone in the living room. Jackie was surprised to discover that she enjoyed the evening a lot and was perfectly capable of feeling happy and fulfilled without her husband's love. This experience caused a profound change in the way Jackie was thinking and feeling. She began to feel more confident and started dating. Within a few weeks, she met a handsome, divorced college professor named Joshua, and fell in love. Joshua was crazy about her as well. As you might predict, the moment that Lyle heard about Jackie's new love affair, he had a sudden change of heart. He lost all interest in his secretary, and begged Jackie to forgive him and take him back. He said he couldn't live without her. But it was too late. Jackie filed for divorce and married Joshua.
Chapter 14
378
Jackie recovered rapidly because she was highly committed to the treatment, and worked hard to change her life. She consistently did her psychotherapy homework between sessions, and came to every session with a clear agenda. I believe that almost any therapist could have done outstanding work with Jackie, because she was so capable, determined, and easy to work with. Unfortunately, many of our patients aren't like Jackie. They "yes-but" us, blame the world for their problems, and refuse to assume any responsibility for solving them. They may not even be clear about what they want. For example, they may say: "I'm in pain all the time. Sometimes I feel dizzy and tired, too. Nobody cares about me." "I'm having an identity crisis. Can you help me figure out who I really am?" "I just can't seem to get my life together. I'm totally overwhelmed. What should I do?" You may feel anxious when you hear statements like these, because you don't know how to help anyone figure out who they "really are," or "get their life together." In fact, I don't even know what these statements mean. When you try to help these patients, they typically ignore you and just keep complaining. Other patients seem passive, hopeless and overwhelmed. They say: "I'm a mistake. My life will never amount to anything." "I've tried everything, but nothing works." "I tell myself all the right things, but I still feel like a loser."
Chapter 14
379
Some are defiant. They say: "Doctor, you don't seem to understand that I really am worthless. Nothing could help me!" "Why should I have to change? It's not my fault!" "You're not helping me!" These kinds of therapeutic logjams nearly always result from Agenda Setting errors, or the complete failure to set the agenda in the first place. If you notice that you're feeling frustrated, drained or burned out in your work with a particular patient, you've almost definitely made an Agenda Setting error. Agenda Setting can save you enormous grief and frustration, and can help you get the therapy back on track when you feel stuck. However, Agenda Setting isn't included in most psychotherapy training programs. Certainly, nobody taught me about it when I was a resident. In addition, I've never seen a single NIMH psychotherapy outcome study that controlled for this crucial variable. And yet, it's by far the most important factor that determines a favorable or unfavorable result. I can clearly recall how I first learned about Agenda Setting. I was struggling with a depressed patient named Donald who was suffering from severe Borderline Personality Disorder (BPD). Donald was demanding, critical, and exhausting. He always put me on the spot, and frequently called me at home between sessions demanding attention for the latest emergency. Sometimes, he'd issue ultimatums and threaten to commit suicide or murder people with his automobile at the local mall if I didn't comply with his demands. It seemed like no matter what I did, it was never enough.
Chapter 14
380
One weekend, I decided to try a rather outlandish strategy to prove that I really did care. Every time Donald called with an emergency, I decided to call him back 15 minutes later to make sure he was okay. That way, he'd see that I really was there for him, and was willing to go the extra mile. Sure enough, Donald called me first thing Saturday morning because he'd gotten achy after going jogging. He was in a panic and demanded to know what he should do. We spoke for about 30 minutes, and by the end of our talk he seemed to be feeling somewhat better. I called him back 15 minutes later to see how he was doing. He seemed to appreciate the follow-up call, but called me again an hour later with a new emergency. I used the same strategy, and called him back to check up on him soon after our phone chat. Unfortunately, he started calling more and more, and I ended up spending most of the weekend talking to him on the phone. I didn't charge him for any of these phone sessions. By Sunday evening, we'd exchanged more than 20 phone calls, but he seemed even more critical of me than ever. He finally insisted that I didn't care about him and hung up on me. I reluctantly concluded that my creative paradoxical strategy hadn't been quite as effective as I'd hoped! At the time, Dr. Windy Dryden was visiting me from England. He was a psychologist who was very active in the development of CBT and a colleague of Dr. Albert Ellis. I told Windy about my problems with Donald and asked if he had any suggestions for me. Windy asked me why I was working so hard. He explained that at his clinic in England, they limited patients with BPD to one
Chapter 14
381
three-minute phone call per week, and made this limitation crystal clear at the intake evaluation. I said, "Well, what if they won't go for it?" He replied, "Then they can go somewhere else for treatment. We explain that this is how our clinic works, and we hope they will decide to work with us, but the phone rules are not negotiable. Most of the time, they do decide to work with us." Suddenly, I saw everything from a totally different perspective. I'd never considered the idea that I had the right to make my patients accountable. This insight transformed my treatment philosophy and my entire therapeutic approach changed almost overnight. When I saw Donald the next day, I explained that I'd been thinking about the fact that we didn't seem to be working together as well as we might. I pointed out that he seemed dissatisfied with the treatment, and that I was getting a bit frustrated and burned out as well. I told Donald that I liked him, was committed to him, and felt convinced that he could improve a great deal if we worked together as a team. But I was concerned because he almost never did any of the psychotherapy homework assignments, and was still feeling as depressed and discouraged as the first day he came to see me. I explained that I wanted to continue working with him, but that from now on, I could only offer one three-minute emergency phone call per week. In addition, if he decided to continue working with me, he'd have to start doing the psychotherapy homework assignments consistently, and he'd also have to
Chapter 14
382
convince me that he wouldn't make a suicide attempt or threaten to do something violent, no matter how desperate, angry, or hopeless he felt. If he was feeling desperate, and needed more input from me, he could schedule additional sessions during my normal hours. If he was willing to work along these lines, then he'd have my total commitment, and I'd be excited about working with him. But if this approach was not acceptable to him, and he felt that he needed a therapist with a different treatment philosophy, I'd be willing to provide him with a copy of my referral list and continue to provide support for a couple of weeks while he looked for his new therapist. I braced for an angry, defiant reaction. To my surprise, Donald said that this was the message he'd needed to hear all along, and that I was the person he wanted to work with. We began to work together much more effectively, and Donald's depression finally began to improve. I was excited about this new discovery and began to use the concept of Agenda Setting with all my patients. Agenda Setting begins at the end of the initial evaluation. This part is easy. I ask patients why they've come for therapy, and what they hope to achieve if the therapy is successful. I list their goals in the chart, and tell them that I'd be happy to work with them on all of them. The next phase of Agenda Setting occurs at every subsequent therapy session. This part is far more challenging. There are five steps: The Invitation. You shift from the talking and listening phase of the session to the active, problem-solving phase.
Chapter 14
383
Specificity. You identify one specific problem that the patient wants help with in today's session. Conceptualization. You determine the nature of the problem the patient wants help with. Motivation. You anticipate the most likely forms of resistance and make the patient accountable. Methods. You select the therapeutic strategies that are most likely to be helpful for the problem the patient has described. These five steps are described in greater detail on pages 384 – 384. You'll have to complete all five steps at every therapy session if you want to do productive work. Let's examine them. Step 1. The Invitation You'll need to use empathy at the beginning of every therapy session. Encourage patients to express their feelings, and try to see the world through their eyes. If you don't empathize skillfully, most patients will resist, because they won't feel that you've listened or accepted them. Once patients have told you how depressed, anxious, or angry they feel, and you've validated their feelings, ask if they feel ready to roll up their sleeves and work on one of the problems they've described, or if they need more time to talk while you listen and provide support. Although the Invitation step may seem humble, you're conveying a powerful message. Talking and listening will not be enough. If patients want to change their lives, active effort will be required.
Chapter 14
384 The Five Steps in Agenda Setting*
1.
The Invitation. At the beginning of each session, patients need the chance to tell you how they've been feeling. After you've listened for a while, you can ask if they're ready to roll up their sleeves and get to work on the problems that are bothering them, or if they need you to listen for a while longer. This conveys the idea that listening alone won't be sufficient, and that active effort will be required if they really want to change their lives.
2.
Specificity. If the patient accepts the invitation, ask them what problem they'd like to work on first. They may want help with depression, anxiety, a marital conflict, or a bad habit. Then ask them to describe one specific moment when they were struggling with that problem. For example, can they tell you about a time when they were feeling depressed, anxious, or angry with their spouse? It could be anything, but the problem must be specific as to: Person. Who were they with? What was going on? Place. Where were they? Time. What time of day was it? Vague complaints, like "I need better self-esteem," "Life stinks," or "I think I'm codependent," won't work. The problem must be real, and it must be something that the patient wants help with.
3.
Conceptualization. Once the patient describes the problem, ask yourself what type of problem it is. Is it: An individual mood problem, such as anxiety or depression? A relationship problem, such as anger or a conflict with a family member, friend, or colleague? A habit or addiction, such as an eating disorder, drug or alcohol abuse, smoking, or procrastination? A non-problem, such as healthy sadness or grief, where no therapeutic techniques other than empathic listening are required? Some problems will fall into more than one category. For example, a woman may be depressed because of a problem in her marriage. Or, a man may be struggling with shyness and substance abuse.
4.
Motivation. Does the patient really want to get better, or does he simply want to talk about the problem while you listen? How hard will he work to solve the problem, if you agree to help him with it? How many sessions is he willing to spend on it? Will he do homework assignments between sessions? Your conceptualization of the problem will help you predict the most likely forms of resistance you're likely to run into. Depression, anxiety, anger and addictions are all associated with unique forms of Process Resistance and Outcome Resistance. Together, you and the patient can think about all the reasons why he may not want to change (Outcome Resistance) or why he may not want to do what it's going to take to get better (Process Resistance). Then you can let him try to persuade that he really does want to change, even though there are many good reasons to maintain the status quo.
5.
Methods. Depression, anxiety, anger and addictions all respond to different kinds of techniques. The techniques you use will depend on the way you conceptualize the problem.
IMPORTANT: NEW and UPDATED several pages of Agenda Setting information in the Appendix starting on page 1248 of this document with flow charts, tips, and expanded help. Learn more about the Magic Button, Magic Dial, Dangling the Carrot, Gentle Ultimatum, and much more!
Chapter 14
385
Step 2. Specificity If patients accept the invitation to move forward, ask them what problem they'd like to work on first. Encourage them to describe one specific moment when they were struggling with that problem. The problem could be anything. It might be when they got out of bed this morning or when they walked out of their boss's office yesterday. It could be the painful memory of a traumatic experience, such as sexual abuse they endured many years ago, or something as simple as sitting with you during today's session, feeling inadequate, overwhelmed or anxious. No matter what the patient describes, it must be real and specific as to: Person. Who were they with when they were feeling upset? What was going on? Place. Where were they? Time. What time of day was it? In addition, it must be a problem that the patient wants help with. These questions will help you focus patients with vague complaints, such as, "My life has no meaning," or "I have low self-esteem." These problems cannot be solved because they do not exist. From a Buddhist perspective, there is no "meaning of life" and no such thing as "self-esteem," or even a "self." The patient has become trapped in abstractions. We couldn't possibly help anyone with these problems because they aren't real. However, our patients are suffering, and the suffering is real. We can ask patients to describe one specific moment when they were struggling with the
Chapter 14
386
meaning of life or feelings of low self-esteem. Then we can conceptualize the nature of the problem they've described and think about some strategies to help them solve it. The Specificity step may seem trivial, unimportant, or obvious, but it's not. All the patient's problems will be embedded in what was going on at any one moment when they felt upset. When you understand how the patient was thinking, feeling, and behaving at that one moment, you'll probably understand the cause of all their problems. And when you show them how to change the way they were thinking, feeling and behaving at that single moment, they'll usually discover the solution to all the problems that are bothering them. I think of this as the Hourglass Effect. Patients complain about all the problems they face, all the people who've let them down, and all the injustices that they've endured. This is like being at the top of the hourglass, and it can feel overwhelming. To work productively, the patient will have to focus on one specific moment when she or he felt depressed, anxious, or angry. This may feel like a deprivation. Most patients don't want help with one problem. They want help with all their problems. When you ask them to focus on just one moment when they felt upset, and to work on solving it, it may be upsetting. They'll suddenly have to give up the victim mindset and assume responsibility for changing their lives. The Specificity step of Agenda Setting is like the neck of the hourglass. It's narrow and uncomfortable. Getting through is difficult, but it can be exhilarating, because once one problem has been resolved, all the patient's problems will
Chapter 14
387
often topple like a house of cards. Some patients will get irritated when you ask them to zero in on one specific moment when they were upset. They may have the fantasy that therapy involves talking endlessly in an unstructured way while a wise and caring therapist listens attentively, nods, and occasionally mutters, "Mmm, tell me more." Others may squirm or become indignant when you ask them if they want help with the problem they've described. If this happens, you'll have to empathize again, and then try to develop a meaningful therapeutic agenda later on. Now let's practice. Imagine that you're treating a college freshman named Joan. Joan is mildly depressed and tells you that she thinks she's "too needy and dependent." How would you help her with this problem? On the table below, check any interventions you might select if you were working with Joan. You can select as many as you like. Treatment Options 1. Encourage her to exercise more, such as daily jogging. 2. Encourage her to do more activities with others. 3. Encourage her to do more activities on her own, so she can overcome her fears of being alone. 4. Use mindfulness meditation, deep breathing, or systematic desensitization to help her overcome the anxiety she feels. 5. Use Primal Scream therapy so she can vent her repressed anger. 6. Mutter, "Tell me more." 7. Encourage her to become more assertive.
Chapter 14 8. Use CBT techniques to help her develop greater self-esteem and change her negative thoughts and Self-Defeating Beliefs. 9. Explore the childhood experiences that made her dependent. 10.
Reassure her that dependency can be healthy, and that she'll feel more independent and self-confident as she gets older.
388
Chapter 14
389
Answer To my way of thinking, these answers are all incorrect. Swooping in with any therapeutic plan before you understand Joan's problem or elicit her cooperation is a waste of time. I don't have the vaguest notion what Joan is talking about. What does she mean when she says that she's too needy and dependent? You could ask Joan questions like these: "Can you give me an example of a specific time when you felt like you were too needy and dependent? When was it? What was going on? Who were you with?" Joan might tell you that she got into an argument with her mother when she visited her parents the previous weekend. If so, what were they arguing about? What did her mother say, and what did she say next? Why was this a problem for her? Does she want some communication training so she can develop a better relationship with her mother, or does she just want to talk while you listen and provide support? Here are some examples of what you might say to patients at the Specificity step: Depression. "Jenny, can you think of one moment when you were feeling depressed and discouraged that you'd like some help with?" Agoraphobia. "David, can you give me an example of a time when the agoraphobia was causing problems for you?" Shyness. "Greg, can you think of one moment when you were feeling shy, so I can get an idea about what was going on, and how you were thinking
Chapter 14
390
and feeling?" An addiction. "Jerry, can you think of a particular time when you were struggling with the temptation to drink?" An eating disorder. "Barnaby, can you tell me about a time that you were struggling with the urge to overeat?" A marital conflict. "Sandy, can you give me an example of a time when you were having trouble getting along with James? What kinds of things do you say to each other, and how does it feel? I'd like to know one thing James said to you that you found upsetting, and exactly what you said next." Step 3. Conceptualization Once the patient describes the problem, ask yourself what type of problem it is. I like to keep things simple, so I conceptualize most problems in terms of the following categories: An individual mood problem, such as depression or anxiety. A relationship problem, including anger, marital problems, or conflicts with others. A habit or addiction, such as overeating, drug or alcohol abuse, or smoking. This category also includes habits like procrastination, or consistently dating the wrong people. For example, a woman might typically fall for married men who are simply looking for a fling. A non-problem. This category includes healthy sadness and grief. The term, "non-problem," may be something of a misnomer, since the death of a loved one is clearly a real problem. However, people who are experiencing healthy
Chapter 14
391
grief that's not complicated by depression usually don't need any antidepressant medications or psychotherapeutic techniques other than empathic listening. Let's assume that Joan, the college student who said she was too needy and dependent, tells you, "My mother is so critical. She's always telling me what to do." How would you conceptualize this problem? Put a check to the right of any conceptualization that seems relevant to Joan. There might be more than one correct answer.
1. An individual mood problem, such as depression or anxiety 2. A relationship problem 3. A habit or addiction 4. A non-problem
Chapter 14
392
Answer We could think of this as a relationship problem because Joan and her mother seem to be locked into a power struggle. We could also conceptualize it as an individual mood problem because Joan's difficulties handling criticism may result from her tendency to base her self-esteem on other people's love and approval. As a result, she may experience anxiety and a loss of self-esteem whenever she's criticized, and may protect herself from these feelings by lashing out at anyone who criticizes her. Of course, these are just hypotheses. Our conceptualization of Joan's problems might evolve in other directions as we get more information about the problem she wants help with. For example, she may be feeling shy and lonely, and having a hard time developing meaningful relationships with guys she's attracted to. She may drive people away with her neediness, because she does all the chasing, or she may get used for sex and then get rejected. The Conceptualization phase will help you with the Motivation and Methods steps. Different kinds of problems are associated with different kinds of motivational difficulties. Once you've conceptualized the problem, it will be easier to anticipate why the patient may resist change. Of course, if the patient is struggling with several different kinds of problems at the same time, such as depression and a relationship problem, several types of resistance may be operating, and several different types of treatment techniques may be needed. Imagine that you're treating a software engineer named Rameesh who says he needs help with his low self-esteem. You ask him to describe a specific
Chapter 14
393
moment when he was experiencing low self-esteem. He tells you that he got upset during his performance evaluation earlier in the week. He received a poor evaluation because his coworkers complained that he was hard to work with. Rameesh told his boss that his colleagues were prejudiced against him because he was from India, and that they were jealous of him because he had superior programming skills. Rameesh's boss wasn't at all sympathetic. In fact, she put him on probation. Now he feels worthless, discouraged and frustrated. How would you conceptualize Rameesh's problem? Put a check to the right of any conceptualization that seems relevant. There could be more than one correct answer.
1.
An individual mood problem, such as depression or anxiety
2.
A relationship problem
3.
A habit or addiction
4.
A non-problem
Chapter 14
394
Answer You could certainly conceptualize this as a relationship problem. Rameesh is angry and seems to have a lot of trouble getting along with people. He clearly handles criticism poorly and sounds a bit paranoid. You could also conceptualize this as an individual mood problem, because Rameesh is feeling depressed, inadequate and anxious. It may be easier for him to improve his relationships with other people if you show him how to overcome his depression and develop unconditional self-esteem. On page 395, you'll find a short series of conceptualization exercises. When you've completed them, you can turn to the answers on page 396.
Conceptualization Exercises
7. Describes the sudden death of her mother from a ruptured aortic aneurysm 30 years earlier, when she was 13. Her father told her and her sister that their mother wouldn't want them to cry.
6. Shouts obscenities at other drivers.
5. Feels shy in social situations.
4. Was kicked out of a drug rehabilitation facility for using drugs again.
3. Flunked a test and is falling way behind in his or her studies.
2. Feels lonely and inferior to other students.
1. Complains of panic attacks during class.
Your patient:
(Depression or anxiety)
Individual Mood Problem Habit or Addiction (Substance abuse, procrastination)
Relationship Problem (Anger or interpersonal conflict)
Type of Problem
Instructions. What type of problem is each patient suffering from? Check all that seem to apply.
Chapter 14
(Sadness, unexpressed grief)
NonProblem
395
Chapter 14
396
Answers Mood Problem 1. Panic attacks
Relationship Problem
Habit or Addiction
Possible
Possible
NonProblem
2. Lonely / inferior 3. Doesn't study 4. Drug relapse 5. Shyness 6. Road rage 7. Death of mother
Possible
Remember that there are no "correct" or "incorrect" answers, because we don't have enough information yet. As you get to know the patient, your conceptualization may evolve. Let's examine the first problem, panic attacks in classes. I used to be the referring psychiatrist for the University of Pennsylvania Law School. The Associate Dean referred many first-year law students to me, most of whom wanted to drop out of school because of panic attacks during classes or test anxiety prior to final exams. On the surface, they had an obvious individual mood problem, primarily anxiety, and CBT techniques were often helpful. But when I dug a bit deeper, I discovered that they often had mixed feelings about being in law school. Some of them had applied to law school to please their parents, or because they couldn't think of anything else to do after college. Their panic attacks were a way of saying, "I'm not sure that I really want to be here." But because they were unassertive and preoccupied with pleasing other people, they'd never admitted these feelings to themselves or expressed them to their parents.
Chapter 14
397
Once they began to deal with the interpersonal issues lurking under the surface, the panic attacks and test anxiety usually improved or disappeared completely. Of course, panic attacks in classes could also result from procrastination, and that's why I put "possible" in the "Habit or Addiction" category on the chart above. Step 4. Motivation Once you've conceptualized the problem, you can assess the patient's motivation and anticipate any resistance you may encounter when you try to help that patient. Different kinds of problems are associated with specific and predictable types of resistance. The resistance of a depressed patient will be different from the resistance of a patient with an anxiety disorder. The resistance of an angry patient with a marital conflict will be different from the resistance of a patient who's struggling with an addiction. I find it helpful to think in terms of Outcome Resistance and Process Resistance. Outcome Resistance means that the patient is reluctant to change because the status quo seems to be working. Although the patient may be in pain, she or he may be rewarded by the problem, or may feel that the suffering is necessary and appropriate. For example, a perfectionistic student who suffers from test anxiety may be reluctant to give up his anxiety because he thinks it motivates him to study hard. He may fear that his academic performance will deteriorate if he doesn't constantly beat up on himself and worry about failure. So he may resist when you try to show him how to give up his perfectionism and compulsive worrying.
Chapter 14
398
Process Resistance means that the patient wants to change, but doesn't want to do the hard work that will be necessary to bring the change about. For example, a woman with a contamination phobia may want to get better, but may be reluctant to use Exposure and Response Prevention because of the intense anxiety she'll have to endure. To assess the patient's motivation, you can ask questions like this: If we could work together to solve this problem, what would it be worth to you? How badly do you want that result? Would you be willing to do self-help exercises between sessions in order to solve this problem? How many minutes would you be willing to work each day? How many days per week would you be willing to do homework assignments? How many sessions can we devote to working on this problem? In order to solve this problem, who do you think should change? Do you think you should change, or do you think that someone else should do the changing? These types of questions will show you whether the patient really wants to change, or just wants to talk. If the patient shows signs of ambivalence, it's crucial not to proceed to the Methods step. Don't try to help patients with any problem until they've convinced you that they're ready, willing, and able to do what it's going to take to change. Most mental health professionals seem to have a hard time avoiding this mistake. When the patient describes a problem, they jump in and try to help
Chapter 14
399
without making the patient accountable. Nearly all therapeutic failure results from this error. Let's think about Joan again, the young woman who said she was too needy and dependent. We conceptualized her conflict with her mother as a relationship problem, at least in part. Is she ready to roll up her sleeves and solve this problem? Remember that Outcome Resistance means that she may not be looking for a solution to the problem. Process Resistance means that she may not want to do what it will take to solve the problem. She could have Outcome Resistance, Process Resistance, both, or neither. Can we assume that Joan wants to solve this problem? Describe at least one probable source of Outcome Resistance:
Chapter 14
400
Answer Does Joan really want a more loving relationship with her mother? Or does she simply want you to listen while she complains about how unreasonable and difficult her mother is? These are very different agendas! If Joan says she does want a better relationship with her mother, we'll have to find out what she means by this. What would a better relationship with her mother look like? And what's her idea of how the improvement in the relationship is going to come about? Does she think that her mother is supposed to change? Or would she be willing to pinpoint on her own role in the conflict and learn how to communicate with her mother more skillfully? These are not trivial issues. If you try to swoop in and help Joan before you've clarified her goals and negotiated what she's willing to do, you may run into stiff resistance. She may protest and say, "Why should I have to change? My mother is the one who's acting like a jerk! Why does she always have to be so controlling?" Joan may not really be asking for help with her relationship with her mother. On some level, she may actually enjoy the conflict. It allows her to stay connected to her mother, in a negative way, and to feel morally superior to her mother at the same time. She can play the role of victim, and get others to side with her. If you jump in with a solution, but Joan isn't committed to solving the problem, you'll both get frustrated. You'll do all the pushing while she does all the resisting. This is as certain as the law of gravity. How about Rameesh? We decided that he has an individual mood
Chapter 14
401
problem and a relationship problem, since he feels depressed, anxious, and inadequate, and seems to alienate his colleagues. We could use cognitive therapy techniques to help him develop greater self-esteem, and interpersonal techniques to help him develop more rewarding relationships with his boss and colleagues. So it would seem that we have a marriage made in heaven. Rameesh has the problems, and we've got the solutions. But what will happen if we offer to help Rameesh with these problems? Is it possible that we may run into some Outcome Resistance or Process Resistance? Put your ideas here before you turn the page:
Chapter 14
402
Answer If we swoop in and try to help Rameesh at this point, he'll almost definitely resist and may even drop out of therapy. He's convinced that there's a conspiracy against him, and believes that his problems aren't his fault. We don't know what kind of help he's looking for, or if he wants help at all. What would you say to Rameesh, in order to set the agenda for today's session? How will you address his resistance at the Motivation step of Agenda Setting? Put your ideas here:
Chapter 14
403
Answer Rameesh was an actual patient I treated. Here's what I said to him: "Rameesh, I can see that you're tremendously intelligent. I really like you, and hope we can work together. However, there's a problem that you'll need to help me with first. You've said that your colleagues treat you unfairly and that they're jealous of you. That must feel extremely unfair, and I can imagine that you must be feeling incredibly angry and frustrated with them. "But if we work together, you're the one who will have to do all the changing. You'll have to learn to change the way you think and feel, as well as the way you communicate with them. But that seems rather unfair, since they're the ones who are screwing up. What are your thoughts about this? Can you help me solve this dilemma?" I had several goals in making this statement. First, I wanted to find the grain of truth in Rameesh's complaints, so he'd feel accepted. Second, I wanted to convey liking and respect. I suspected that he had a narcissistic streak and knew that if he felt judged or belittled, he'd probably put up a wall and drop out of therapy before we even got started. Finally, I wanted to head off his resistance at the pass and let him know that he'd have to persuade me to work with him, and not vice versa. Rameesh told me that he definitely wanted to work with me, and would do practically anything if I could help him overcome the problems that had been plaguing him. He actually did more cognitive therapy homework than anyone I'd
Chapter 14
404
ever worked with, and I greatly enjoyed the work we did together. Agenda Setting was the key to our success. When I presented Rameesh with powerful reasons why he probably didn't want to change, he suddenly discovered that he did. The rest was fairly easy. Step 5. Methods After you've conceptualized the type of problem the patient wants help with and made the patient accountable, you can select the most effective techniques for treating that problem. Different kinds of problems respond to different kinds of techniques. I used cognitive therapy techniques to help Rameesh develop better self-esteem, and interpersonal techniques to help him develop better relationships with other people. The 50 CBT techniques on pages 522 – 531 are arranged in six major categories. Your conceptualization of the problem will influence your choice of techniques. We'll talk more about individualizing the treatment and selecting the most effective techniques for each patient in Chapter 26. Combining Agenda Setting with Empathy I've described Empathy and Agenda Setting as separate techniques, in much the same way that you might learn one technique at a time in a martial arts class. However, you'll have to integrate them seamlessly, because certain kinds of patients will get extremely upset when you try to set the agenda. For example, patients with Borderline Personality Disorder may not take kindly to the idea that they'll have to be accountable, do psychotherapy homework consistently, and work hard to solve their problems. Some of them seem to convey this message:
Chapter 14
405
"I demand that you help me against my will while I stubbornly resist and fight you." If patients become upset or enraged when you try to set the agenda, you'll need to back off and empathize immediately. Go with the flow. Give the patient a chance to talk while you listen and provide support. Then, when the patient feels relaxed and trusts you again, you can try the Invitation step of Agenda Setting again. Empathy won't guarantee success, and definitely won't be sufficient for a cure, but it's the only thing that works when there's a failure in the therapeutic alliance.
UPDATE NOTE: See updated version of agenda setting including more on positive refreaming, dangling the carrot, sitting with open hands, and more in the Appedix!
15*
The Eight Types of Therapeutic Resistance
Patients come to us because they're suffering and desperately want relief, but sometimes, they seem more committed to the status quo than to changing their lives. I once treated a depressed and bitter anesthesiologist from Dallas who complained about all the injustices in her life and in her relationships with men. In spite of her misery, she seemed reluctant to take any steps to solve these problems and had an intense aversion to psychotherapy homework. One day, she issued this ultimatum: "If you ever ask me to do any psychotherapy homework assignments again, I'll commit suicide in the operating room of the hospital. And believe me, I know how to get the job done. Furthermore, they'll find a copy of your book, Feeling Good, displayed on my stomach when they discover my body!" As you might imagine, I backed off and decided I better not push too hard. * Copyright
2003 by David D. Burns, M.D.
Chapter 15
407
I thought that if I listened and provided enough warmth and support, she might eventually take some steps to change her life. Two years later, we were still working together, and the good news was that she hadn't committed suicide. The bad news was that nothing had changed, and she was still complaining bitterly about all the injustices in her life. About a year ago, I attended a conference with several colleagues who were discussing difficult cases. Everyone was using the word, "resistance." I'd heard this word ever since I was a psychiatric resident, but suddenly realized that I didn't know exactly what it meant. It dawned on me that resistance probably wasn't one thing, but many things. I said, "Wouldn't it be neat if we listed the five or ten most common types of resistance? Then we could teach the psychiatric residents about all the different kinds of resistance, and we might even be able to describe the most effective ways of dealing with each one." Everyone got excited and agreed that we should definitely develop this list. So I waited. And waited. But no one came up with a list. A few weeks later, a system for categorizing the eight common types of therapeutic resistance came to me in a dream in the middle of the night. I felt excited about it, and shared my idea with my students and colleagues. I began to describe it in my workshops as well. In the last chapter, I touched on the idea there are two basic types of resistance, Outcome Resistance and Process Resistance. Outcome Resistance means that patients have powerful reasons not to get better, even if they could push a button and be magically cured in today's session. Process Resistance
Chapter 15
408
means that they want to get better, but don't want to do what it's going to take to get better because it’s too hard or it makes them uncomfortable. There are four targets for each type of resistance. They correspond to your conceptualization of the patient's problem. It could involve: Depression Anxiety A relationship conflict A habit or addiction Since we have four targets for Outcome Resistance and Process Resistance, we have eight types of resistance in all. They're all completely different from each other. For example, the Outcome Resistance for depression is different from the Outcome Resistance for anxiety, a marital problem, or an addiction. Although these eight forms of resistance are internally generated, our patients sometimes resist because we force them to. Dr. Henny Westra, a brilliant Canadian psychologist, recently visited my Wednesday evening psychotherapy seminar at Stanford and presented some of her work on motivational interviewing for anxiety disorders. At the beginning of her talk, Dr. Westra asked us to pair off in twos. She explained that one person in each dyad would play the "therapist," and the other person would play the "patient." She told the "patients" to describe something they felt ambivalent about, like getting caught up on filing, cleaning the garage, buying a new car, dieting, or quitting smoking. She told the "therapists" to try to persuade the patient to change.
Chapter 15
409
As you might expect, most of the dyads quickly got into power struggles. The harder the therapists tried to persuade the patients to change, the more strenuously the patients resisted. Full-blown resistance only took a few seconds to emerge. Those of us who were in the "patient" role experienced our therapists as lacking in understanding or compassion. We felt frustrated and resentful, because our therapists seemed so pushy and narcissistic. Of course, the therapists also felt frustrated because their patients seemed stubborn and unreasonable. Although it was set-up as a role-playing exercise, it felt real. Nearly all patients will bring some ambivalence to the table. When they express reluctance to change, we may respond with logic or persuasion. This is like a knee-jerk reaction, and it's hard not to give in to it. But the harder we try to persuade patients that they can or should change, the more strenuously they resist. That's why most persuasive strategies are doomed to failure. I've summarized the eight basic patterns of resistance in the table on pages 410 – 411. The left-hand column lists several types of Outcome Resistance for depression, anxiety, relationship problems, and addictions. These are some of the reasons why patients may not want to change, even if change were instantaneous and required no effort whatsoever. The right-hand column lists several types of Process Resistance for each type of problem. These are some of the reasons why patients may be reluctant or unwilling to do what's going to be required to change, even if they really want to change.
Chapter 15
410 Why Our Patients Resist*
Outcome Resistance— Why Patients Cling to the Status Quo
Process Resistance— Why Patients Resist Working Hard To Change
Depression
Depression
Worthlessness. I don't deserve to feel good because I really am inferior or defective.
Hopelessness. Nothing will ever change, so why try? If I don't get my hopes up, I won't be disappointed.
Guilt. I don't deserve any happiness or self-esteem because I'm bad and I deserve to suffer.
Motivational Paralysis. I don't feel like doing any self-help assignments between sessions. I'll wait until I'm in the mood.
Realism of Depression. Life really is awful. People who feel happy are stupid and naïve.
Overwhelmed. The psychotherapy homework assignments are just too much work. I'm drowning in commitments and don't have time to do more.
Perfectionism. If I beat up on myself relentlessly whenever I fall short, it will motivate me to achieve great things. Achievement Addiction. I couldn't possibly feel happy or fulfilled until I've accomplished something outstanding. But I've never done anything special, so I could never feel any real joy or self-esteem. Love Addiction. I couldn't possibly feel happy or fulfilled without a loving relationship.
Entitlement. I shouldn't have to work so hard to recover. Medical Model. My doctor said that I have a chemical imbalance in my brain, so a pill should cure me. Traditional Psychiatric Model. I thought that all I had to do was come to sessions, talk about all the problems in my life, and explore the past.
Self-Pity. I like being a victim and feeling sorry for myself. Anxiety Magical Thinking. My fears protect me or my loved ones. If I stop worrying, something terrible may happen. No Pain, No Gain. My constant worrying is the price I have to pay to do superb work. If I stop worrying, I'll get complacent and fail. Conflict / Anger Phobia. I don't want to face the problem that's triggering my anxiety in the first place.
Anxiety Avoidance. Facing my worst fears will be dangerous and uncomfortable. I shouldn't have to do that. There has to be an easier way. Medical Model. The ad I saw on TV said that my shyness results from a chemical imbalance in my brain, and that an antidepressant will solve the problem.
* Copyright © 2005 by David D. Burns, M.D. Do not copy or distribute without written permission.
Chapter 15
411 Why Our Patients Resist (cont'd)* Outcome Resistance— Why Patients Cling to the Status Quo
Process Resistance— Why Patients Resist Working Hard To Change
Anger / Relationship Problems
Anger / Relationship Problems
Low Desire. I don't really want to get close to you. I just want to complain about you and keep you at a distance!
Truth. I'm right and you're wrong.
Martyrdom / Heroism. I like the role of victim.
Blame. Our problems are all your fault, so why should I have to change?
Moral Superiority. I enjoy feeling superior and looking down on you. You're a loser.
Pride. I can't stand the humiliation of examining my own role in the problem.
Gossip / Scapegoating. It's rewarding to talk to my friends about what a loser you are. They all agree with me, too!
Entitlement. I deserve better treatment. I shouldn't have to work so hard to solve the problems in our relationship.
Power. I want to control you.
Fear. Something bad will happen if I try to get close to you. You might hurt me or make me look bad. It's safer to keep you at a distance.
Revenge. I have every right punish you because of the way you've treated me. Anger addiction. I like feeling angry and bitter. It's rewarding. Violence. Aggression is exciting. I enjoy hurting you.
Hopelessness. You're such a stubborn, self-centered jerk that nothing could possibly work. Why should I bother to try?
Self-Righteousness. I treat you badly because you deserve it. It's the right thing to do. Habits and Addictions Instant Rewards. My habit is pleasurable. Why give it up? Entitlement. I shouldn't have to change. Narcissism. I'm special. I deserve this donut (or drink). Denial. I don't have a problem!
Habits and Addictions Deprivation. Giving up my habit will be painful and uncomfortable. Ugh! Who wants that? Hopelessness. I've tried over and over but nothing works, so why get my hopes up? I'll just end up feeling frustrated and disappointed again.
Conflict Phobia. I'd rather get high than face the problems that are bothering me.
* Copyright © 2005 by David D. Burns, M.D. Do not copy or distribute without written permission.
Chapter 15
412
Let's examine how Outcome Resistance and Process Resistance work for each type of problem. Once you understand these resistance patterns, you'll be able to anticipate motivational difficulties much more quickly. You'll comprehend each patient's ambivalence from the first moment they describe the problem they want help with. Then you can negotiate a far more effective therapeutic contract. Depression Some depressed individuals believe that they don't deserve to feel happy and fulfilled because they feel like worthless, inferior, or bad human beings. They may think they deserve to suffer, or believe that their depression helps them in some way. Imagine that your new patient, Mei-Ling, is a depressed college freshman from Hong Kong. Mei-Ling tells you she's upset because she's getting B's, rather than the A's that she expected. As she's gotten more and more depressed, she's lost her motivation and self-confidence. She spends most of her time alone doing nothing. She says she can't concentrate on her assignments and constantly procrastinates. She feels overwhelmed, inadequate, frustrated, ashamed, anxious, discouraged and mad at herself. She beats up on herself relentlessly, and her mind is flooded with self-critical thoughts all day long. Can you think of at least one reason why Mei-Ling might resist treatment? Why might she cling to her depression and not want to get better? Imagine that there's a magic button on your desk, and if she pushes it, she'll immediately recover from her depression and walk out of today's session feeling joyful and optimistic. Will she push the button? Why or why not?
Chapter 15
413
Of course, we don't know Mei-Ling very well yet, and our understanding will become more refined as we get to know her better. But it can be helpful to formulate some hypotheses about resistance as early in the treatment as possible. Put your ideas here before you turn the page:
Chapter 15
414
Answer On the one hand, Mei-Ling is coming to you because she feels worthless, desperate and overwhelmed. But she may be reluctant to let go of her depression for any number of reasons. First, she probably bases her feelings of self-worth on her accomplishments, and may feel that it wouldn't be possible or morally justified to feel happy and fulfilled until after she's accomplished something tremendous or gotten the straight A's she supposed to get. But she's struggling just to get B's. From her point of view, happiness may not seem realistic or even acceptable. In addition, Mei-Ling may feel like she's a huge disappointment to her parents, and think that she's obligated to suffer until she's doing superb work. She may feel like her depression and guilt are the punishments she deserves. Paradoxically, when she beats up on herself, she shows the world that she's strong and conscientious. In addition, she may think that she's avoiding criticism from others. After all, she's giving herself such a hard time that they won't need to. Mei-Ling's depression might also give her an excuse for procrastinating and slacking off. It's painful, but easy. She doesn't have to discipline herself or dig into the academic work that seems so difficult. Maybe everything came easily in grammar school and high school, so she never had to learn to be patient and persistent, or to tolerate frustration. Finally, Mei-Ling may believe that her self-loathing will motivate her to work harder and achieve more academically. So if you show her how to talk back
Chapter 15
415
to her self-critical thoughts, she may feel the need to fight you, because she may think you're taking away her crutch. These aren't insurmountable problems. If you do a good job of empathizing, and Mei-Ling likes and admires you, you can explore her resistance before you jump in and try to help her with CBT techniques. You might say something like this: "Mei-Ling, I can see that you're suffering terribly and having a horribly difficult time, and that the more depressed you get, the harder it is to study and do your best. It must feel like sinking into quicksand. If I could show you how to overcome your depression right now, so you could walk out of today's session feeling self-esteem and happiness, would you go for it? I'm not saying that I could do that. Successful treatment always takes time and hard work. But I'm wondering—would you be willing to feel joy right now if it were possible?" Mei-Ling will probably say yes, definitely. Then I'd say, "So I take it, MeiLing, that you'd be willing to be way behind in your school work and getting B's, rather than A's you'd hoped for, and still feel perfectly happy?" At this point, she'll almost certainly say, "No!" Then I might say, "I can see lots of reasons why you might not want to give up your depression. Let's talk about them." This will give her the opportunity to tell you why she feels reluctant to change. Mei-Lei believes that she's letting her parents down and feels like she should be doing better. She thinks that if she beats up on herself, it will motivate
Chapter 15
416
her to work harder. Then you could ask questions like these: "Are you saying that you want to keep beating up on yourself, and don't want to feel better until your grades and study habits have improved?" "Is that strategy working for you? Do you feel especially motivated? Is the depression helping you as much as you'd hoped?" You can also talk about how most of us have a natural tendency to beat up on ourselves when we're not living up to our hopes and expectations. This becomes a vicious cycle, because the depression and self-abuse rob you of motivation, and your performance gets even worse. In contrast, if you give yourself permission to feel good, in spite of the fact that you're not doing as well as you'd like, it may be easier to correct the problem and get back on track. If Mei-Ling grasps this formulation, you can proceed with the treatment without running into so much resistance and yes-butting. When you explore Mei-Ling's resistance, unexpected things may surface. You may discover that her parents are pressuring her to pursue a career in electrical engineering, but she has a secret desire to pursue an artistic career. In this case, her depression may be a kind of protest. She may be on strike. But instead of verbalizing these feelings to her parents directly, she may be trying to convey this message: "This career path isn't working for me. It's killing me." CBT is rich in powerful techniques to help depressed individuals change the way they're thinking and feeling. But in order to use these techniques effectively, you and your patient will have to be working hard together on the same team. If the depression is serving a purpose the patient hasn't verbalized,
Chapter 15
417
then she or he may resist your efforts. That's why it can be so useful to anticipate the resistance and develop a solid sense of teamwork before you use any CBT techniques. So far, we've focused on Mei-Ling's Outcome Resistance. Some depressed patients want to get better, but resist doing the things they'll have to do to recover, such as the psychotherapy homework assignments. Can you list at least five possible reasons for this? 1.
2.
3.
4.
5.
Chapter 15
418
Answer Patients may resist psychotherapy homework for many reasons, including: Putting the Cart Before the Horse. Depressed patients often procrastinate because they tell themselves, "I don't feel like it right now. I'll do it later, when I'm more in the mood." But of course, the mood never comes. Motivational paralysis is one of the cardinal symptoms of depression. Sometimes I ask a patient who procrastinates what comes first, motivation or action? Most patients will tell you that motivation comes first. They think they should feel like doing something before they do it. But they're putting the cart before the horse. Highly productive people know that it's the other way around. Action comes first, and motivation follows. You're not entitled to feel motivated until after you've gotten started. If you wait for the motivation, you may have to wait forever, because you'll probably never feel like doing the things you've been putting off. Hopelessness. Hopelessness is another cardinal symptom of depression. Many depressed individuals develop the illogical belief that nothing could ever help them, so they give up and do nothing. Of course, this functions as a self-fulfilling prophecy. Things don't change, and they conclude that things really are hopeless. Coercion Sensitivity. Some patients, especially adolescents, believe that if someone asks them to do something, they must refuse or lose face. So if you ask them to do self-help assignments between sessions, a power struggle develops. They see you as a controlling authority figure and feel the need to
Chapter 15
419
defeat you. You may inadvertently fall into the trap, and pressure them to do the homework. Of course, this always triggers more intense resistance. Worthlessness. Some patients believe they really are worthless, inferior, or defective. They're convinced that their negative thoughts about themselves are entirely realistic, and can't see how the psychotherapy homework could possibly help. Aversion to Psychotherapy Homework. Some patients may have bad memories of being pressured to do homework every night when they were in school. They may be turned off by the idea of psychotherapy homework because it reminds them of all the stress and tension they experienced when they were growing up. Cultural View of Therapy. Some people feel that just taking a pill or talking to their therapists and getting their problems off their chests should be enough to make them feel better. Others believe that if they explore their childhood experiences enough, they'll suddenly develop some insight that will solve their problems and change the way they feel. This model of therapy is reinforced by the media, including movies like Good Will Hunting and Ordinary People, as well as popular TV shows like The Sopranos. Now, I have a question for you. How will you deal with Process Resistance for depression? Or to be more specific, how will you persuade Mei-Ling to do the psychotherapy homework assignments that will be vital to successful treatment? Put your ideas here before you turn the page:
Chapter 15
420
Chapter 15
421
Answer The answer to this question cuts to the very heart of Agenda Setting. I don't try to persuade patients to do anything, because it never works! I don't believe it's my job to persuade any patient to work with me. Instead, I think it's their job to persuade me to work with them. My research and clinical experience confirm that all the improvement is with the patients who do the psychotherapy homework (Burns and Spangler, 1998). In contrast, depressed patients who refuse to do the homework, or consistently "forget" to do it, rarely improve, and may actually deteriorate during treatment with CBT. Therefore, I don't want to engage them in any treatment contract that isn't likely to be effective. If patients are willing to do the homework, then the prognosis for recovery is bright. If patients aren't comfortable with this idea, we'll probably need to consider other options, such as looking for another therapist who wouldn't ask them to do any homework. You may be reluctant to deliver that message, because it seems too tough-minded, and you may be afraid that the patient will drop out of therapy. I used to have the same concerns, and it was hard to make patients accountable at first. But I discovered that when I did this with firmness and compassion, the vast majority of patients suddenly decided that they wanted to work with me and were perfectly willing to do the homework after all. Anxiety Disorders Outcome Resistance for anxiety means that the patient doesn't want to recover, even if they could be cured instantly and without effort in today's
Chapter 15
422
session. Why in the world would any anxious patient want to be anxious? And why would they seek treatment if they didn't want to recover? Let's think about some common forms of anxiety and see if we can get a feel for how Outcome Resistance functions. A 23 year-old graduate student named Gloria developed symptoms of OCD shortly after her younger brother was diagnosed with bipolar manic-depressive illness. She began to have frightening fantasies of murdering her family, and found knives terrifying because she was afraid she might lose control, grab one and start stabbing her parents to death. Can you think of one possible source of Outcome Resistance? Remember, if she could be cured in today's therapy session, all her fears of going on a murder rampage would suddenly disappear, and she'd walk out of the session with no anxiety or obsessions whatsoever. Would she want that? Put your ideas here before you turn the page:
Chapter 15
423
Answer The Outcome Resistance for anxiety usually results from magical thinking. Patients are suffering, but may think that their anxiety protects them or helps them in some way. Gloria feels like she really is dangerous, and may think that she has to be vigilant and worry constantly to make sure she doesn't spiral out of control! So if she were "cured" in today's session, she might paradoxically think she was in great danger of harming her loved ones. Most mental health professionals would view OCD, or any anxiety disorder, as an illness, and assume that the patient wants relief. But many anxious patients subconsciously view their anxiety as a good thing. If you rush in to treat them without exploring this, you may run into resistance. Let's talk about Process Resistance. Assume that Gloria wants to get better. Is there something that she'll have to do that she probably won't want to do? The psychotherapy homework assignments will obviously be necessary, just as they are in the treatment of depression, but I'm thinking about something different. See if you can think of one powerful source of Process Resistance. Put your ideas here before you continue reading:
Chapter 15
424
Answer Anxious patients will have to confront their fears if they want to recover. In the treatment of OCD, Exposure and Response Prevention will be mandatory. We have numerous tools in addition to these, but Exposure and Response Prevention must be included in any effective treatment package. For example, we might ask Gloria to intentionally imagine slashing family members to death with a knife instead of struggling to push these fantasies out of her mind. This is called Cognitive Flooding. It may be intensely anxiety-provoking for her, but could be one of the keys to her recovery. If she sticks with these fantasies, they'll probably lose their power to upset her after a period of time.* We might also ask her to intentionally handle knives and other "weapons" she's been avoiding. Once again, this may be intensely anxiety-provoking, but sooner or later, she'll probably become desensitized to them. Anxious patients almost never want to do these things. In fact, avoidance is at the very heart of anxiety. How will you persuade Gloria to use Exposure and Response Prevention? Put your ideas here before you continue reading:
* Of course, you'll have to do a violence assessment first, and make sure that Gloria isn't actually planning to do something harmful. In most cases, OCD patients are not dangerous. The real problem is nearly always the way they constantly torment themselves.
Chapter 15
425
Answer Once again, it's not your job to persuade Gloria to use Exposure and Response Prevention. Instead, you can say something like this: "Gloria, I can see how miserable you feel, and really want to work with you because I'm convinced that the prognosis is positive. However, I want you to know what successful treatment will require, so you'll understand the kinds of things I may ask you to do. For example, I may ask you to schedule periods of time to intentionally fantasize about killing your family. That type of thing is bound to be pretty anxiety-provoking for you, but could be extremely helpful. How you feel about it?" You can also let Gloria know that you have lots of other tools available that will not be frightening to her, but the Exposure will be a mandatory part of the treatment. If you agree to work with her, would she be willing to use these techniques, in spite of the anxiety she'll have to endure? A woman named Betsy was suffering from GAD. She constantly worried that something terrible would happen to her children, like getting sick or being mangled in an auto accident. Describe one possible source of Outcome Resistance. Put your ideas here before you continue reading:
Chapter 15
426
Answer Betsy may think that her worrying protects her loved ones from danger. She may equate worrying with love, and believe that's what a good mother is supposed to do. She may think that something bad will happen if she stops worrying about them. Let's think about Outcome Resistance for a phobia. Why would someone with a phobia not want to be cured? I once treated a woman named Latasha who had an airplane phobia. Latasha had to make frequent airplane trips with her husband, and worried constantly that the plane would crash, so every flight was a miserable ordeal. Can you pinpoint one possible source of Outcome Resistance? Put your ideas here before you continue reading:
Chapter 15
427
Answer Latasha was convinced that her worrying protected the passengers and kept the plane in the air. She was afraid that if she relaxed during a flight, the plane would suddenly fall out of the sky like a rock. Latasha wasn't delusional or naïve. In fact, she was studying for a Ph.D. in psychology at the University of Michigan. However, she had the same kind of superstitious thinking that plagues most people who suffer from anxiety. I asked Latasha how much worrying she thought was necessary to keep the plane in the air. Was 60 minutes out of every hour necessary? Or would a smaller dose of worrying be sufficient to keep the passengers safe? Latasha thought this was funny, and agreed that five minutes of worrying per hour would probably be enough. She agreed to worry as intensely as she could for five minutes every hour on the next flight. During the next 55 minutes, she could relax and get caught up on her reading for one of her classes. She even set the alarm on her watch so she'd know when it was time to worry again. She was surprised that five minutes of worrying per hour seemed sufficient, since she had a smooth, safe flight! I once treated a psychologist named Maria who was suffering from test anxiety. Her psychology licensure examination was only six weeks away, and she was paralyzed by fear. Her mind was flooded with distorted negative thoughts, like, "I just know I'm going to flunk the test," and "They'll ask about all the things I don't know, and none of the things I do know." Of course, some candidates do flunk the licensure examination and have to take it again, but
Chapter 15
428
Maria was an excellent student and had never once flunked a test in her entire life. When I encouraged her to identify the distortions in her negative thoughts and talk back to them, she fought me tooth and nail and insisted that I just didn't understand. On the one hand, she was stuck, miserable and asking for help. But when I offered to help, I suddenly became her enemy. Why was Maria resisting me so intensely? I asked her to list all the advantages of worrying about the exam on a Cost-Benefit Analysis. She listed several: The worrying will motivate me to prepare carefully for the licensure exam. If I stop worrying, I may get complacent and flunk the test. If I don't get my hopes up, I won't be so disappointed if I do fail. I can tell myself that I knew it would happen all along. I told Maria those seemed like important benefits, and asked if there were any disadvantages. Was there a price to pay for her worrying? She listed these three disadvantages: I've been so nervous about the test that I haven't been able to study for a single minute in the previous two months! If I keep telling myself that I'll study all the wrong things, freeze up and flunk the test, it might actually function as a self-fulfilling prophecy. All the worrying is making the process of review and preparation a miserable experience, because I constantly feel inadequate, worried, and resentful. Maria decided that the disadvantages outweighed the advantages by a 70
Chapter 15
429
– 30 margin. She said that the first disadvantage—being unable to study—really tipped the scales. At this point, her attitude changed radically. I acknowledged that some anxiety might motivate her to prepare carefully and do the best possible job, but pointed out that she'd estimated her anxiety at 95% out of 100%. I asked her how much anxiety she thought she really needed to study hard. Would 50% be enough? Or 30%? She said that 10% or 15% would be plenty. I suggested that we could use CBT to lower her anxiety to that level, but if it got any lower than that, she could practice giving herself the frightening messages again so she could bring it back up to the optimal level! Maria liked this formulation, and was quickly able to put the lie to the negative thoughts that had been plaguing her. Her anxiety vanished and she said she enjoyed reviewing the material. Several weeks later, she passed the examination with flying colors on her first try. Anger and Relationship Problems Outcome Resistance for a relationship problem means that you don't really want to get close to the person you're at odds with. Process Resistance means that you want to get close, but you don't want to do what you're going to have to do to bring that result about. You're not willing to pay the price of intimacy. Individuals with troubled relationships may have Outcome Resistance, Process Resistance, or both. Can you think of some possible reasons why a patient with a relationship problem might not want to get close to the person they're complaining about? Put your ideas here before you continue reading:
Chapter 15
1.
2.
3.
4.
5.
430
Chapter 15
431
Answer There are many potential sources of Outcome Resistance. Someone with a troubled relationship may not desire greater trust and love because: They feel rewarded by the conflict. Anger and conflict can be addictive. They enjoy feeling morally superior to the person they're not getting along with. They like the role of victim and enjoy feeling sorry for themselves. They want to punish or hurt the person they're mad at, especially if they feel that they've been hurt by that person. Revenge may seem far more appealing than intimacy. They feel that the costs of getting close outweigh the benefits. They no longer care about the person they're mad at, and may want to develop a new and more rewarding relationship with someone else. They have hidden agendas. For example, a lousy marriage may be the perfect excuse to have affairs behind your partner's back. They enjoy scapegoating the other person and complaining about them. They believe that it's impossible to get close to the other person, so there's no point in trying. They feel that the other person is bad and doesn't deserve a more loving relationship. They're more attracted to power and control than intimacy and trust. They're determined to prove that they're "right" and the other person is "wrong."
Chapter 15
432
They see the relationship as a competition and more preoccupied with winning and putting the other person down than getting close. Feelings of pride and shame get in the way. I'm sure you can add to that list. If you don't take Outcome Resistance and Process Resistance into account, your interventions may be doomed to failure. Sometimes, the most important question is not, "How can I help the patient with this problem?" but rather, "Does the patient want help with it?" Experts have created a wide variety of relationship enrichment packages for troubled couples. These packages include methods to help couples resolve conflicts more skillfully, communicate more effectively, treat each other in a more positive and loving way, and modify the negative thinking patterns and selfdefeating attitudes that trigger interpersonal conflicts. The shelves of popular bookstores are flooded with self-help books on how to develop more loving relationships, many of which have achieved bestseller status. However, outcome studies indicate that none of the current approaches are particularly effective (Epstein & Baucom, 2002). At most, 50% of the couples who enter marital therapy experience meaningful or lasting improvements in their relationships. Attempts to refine these treatment programs by including even more creative and powerful techniques have not led to better outcomes. Ultimately, many troubled couples seem to go down the road of hostility, dissatisfaction, and divorce. Treatment programs directed at individuals with relationship problems have been just as ineffective. I believe these results stem from the fact that most, if not all, of these
Chapter 15
433
treatments are based on the hypothesis that people with troubled relationships desire greater intimacy and more loving marriages, and only lack the skills they need to achieve this goal. This idea sounds encouraging and creates feelings of hope and optimism. If we simply provide people with troubled relationships with more effective interpersonal skills and more adaptive attitudes, we might expect to see significant improvements in their relationships. Presumably, they'd listen and express themselves more skillfully, and treat each other with greater understanding and respect. Unfortunately, this hypothesis may not be realistic, especially if the patient feels ambivalent about getting close to the person they're mad at. Although they may say, "I want a better relationship with my spouse," or mother, brother, or boss, what they often really mean is, "I want to complain while you listen and agree that the other person is a loser." Most therapists have a charitable view of human nature. It's tempting to believe that humans are basically good, and will choose joy and intimacy over hostility and conflict. We may see violence and aggression as frustrated attempts to develop greater love and understanding. As a result, we may have a hard time resisting the urge to jump in and offer to help patients who describe problems in their relationships, and may have trouble accepting the idea that they may not really want a more loving relationship with the person they're at odds with. I often made this error during the first few years of my practice. When patients described their troubled marriages or difficulties getting along with a family member, neighbor, friend or colleague, I naively thought they were asking
Chapter 15
434
for help and wanted to solve the problem they were complaining about. I was surprised when they seemed to sabotage my efforts. The solution to the problem they described was usually pretty straightforward—but they just didn't seem interested! If you've ever treated angry individuals or couples, you probably know what I'm talking about. The patient may say: My wife is so critical. She nags me all the time. The moment I walk in the door, she starts telling me what to do. Why doesn't she appreciate all the things I do for her? My husband always says that I don't ever listen. I just ignore him when he says that! My partner said that I can't handle feelings or emotions. I told her that I had no idea why she'd say that! My husband is so stubborn. He always has to be right and won't ever listen to me! My ex is such a jerk! My sister thinks she's so high and mighty! All she cares about is herself. My husband won't ever talk about his feelings. Why are men like that? When a patient describes a relationship problem, I try to listen and see the world through their eyes, and ask for some specifics. What did the other person say to you during the argument? What did you say next? How were you feeling? What were you thinking? How would you characterize the nature of the problem you're running into?
Chapter 15
435
During this empathy phase, I don't try to help or offer any suggestions. I simply find some truth in what the patient is saying, even if their complaints sound self-serving or unreasonable. I encourage them to express their negative feelings and try to provide as much support as possible. I want the patient to feel that I'm on his or her side. Then I ask the patient if they're looking for help, or simply wanted me to know how irritating and frustrating their spouse, brother, neighbor or colleague is. Did they just want to talk while I listened, or did they want to roll up their sleeves and try to develop a better relationship with the person they're complaining about? If they don't want to work on the problem, I say something like this: "Laurel, I think I understand you, but I want to make sure I have it right. (TE) You say that you've felt lonely and unhappy in your marriage for years because your husband, Ted, doesn't express his feelings. (TE; FE) You've also said that you're not interested in trying to develop a more loving relationship because you feel convinced he's a hopeless case. (TE; FE) You've said that he's a cold fish, and that you've tried everything, but nothing works, so there's no point in trying. (TE) You told me that you're not interested in leaving him, but just wanted me to know how frustrated and annoyed you feel. (TE; FE) Did I get it right? (IN)" I call this technique Paradoxical Inquiry. If Laurel agrees that she doesn't want any help with her marital problems, I'd accept what she's saying and ask if there's some other problem she wants to work on instead. This can feel like a disappointing outcome, since you can see a solution to the problem she's
Chapter 15
436
describing. But if you give in to the urge to help Laurel, you'll run into resistance. You may be convinced that you have a great deal to offer, but if the patient hasn't asked for help, you simply can't work your magic. Now let's think about Process Resistance. Assume that Laurel does want a more loving and satisfying relationship with Ted. What's one thing she's going to have to do that she's not going to want to do? Put your ideas here before you turn the page:
Chapter 15
437
Answer Laurel is going to have to give up the idea that it's all Ted's fault and examine her own role in the problem. But she's probably not going to want to do that because it will be painful, and completely inconsistent with her view of the problem. After all, she's been cataloguing his faults for years. As far as she's concerned, she's an innocent victim. As long as she maintains this mindset, the prognosis is poor at best. That's why anger can be so much more difficult to treat than depression or anxiety. If you come to me for help with your depression, you'll probably feel worthless and convinced that you're a loser. Your mind will be flooded with negative thoughts about yourself, like "I'm defective," and "I should be better than I am." When we work together, I'll have good news for you. You'll discover that your negative thoughts about yourself are false. To recover, you won't have to face some horrible truth about yourself. In fact, you'll suddenly see that all those "horrible truths" about yourself were just illusions and distortions. This is one of the greatest discoveries that a human being can make. Recovery from depression can feel phenomenal. In contrast, if you come to me for help with a relationship problem, you'll probably feel convinced that there's nothing wrong with you, and that the person you're not getting along with is the loser. You'll feel certain that everything is the other person's fault, and your mind will be flooded with negative thoughts about them, such as, "Why does he have to be such a self-centered, dishonest jerk?
Chapter 15
438
He's got no right to say something like that!" When we work together, I'll have bad news for you. You're going to discover that you've been provoking the problem all along, and that you're not a helpless victim after all. This can feel humiliating. Of course, the goal of the treatment is not humiliation, but intimacy and joy. If patients are willing to examine their own role in the problem, we can show them how to develop more rewarding, loving relationships with the people they're not getting along with. But there's definitely going to be some pain along the way. You can deal with Process Resistance by asking questions like this: "In your opinion, who's more to blame for the problems in your relationship? Is it you, or the other person? And who should do most of the changing in order to make this relationship better?" If the patient says, "the other person," I'd say that it might be better to work on a different problem, since the other person isn't available. I'd point out that successful interpersonal therapy would require giving up the idea that it's the other person's fault, focusing on their own role in the problem, and assuming complete responsibility for doing all the changing themselves. But since they feel convinced it's the other person's fault, that approach might not be appealing, or even acceptable, to them. The goal is to use paradox rather than persuasion. If you use logic and point out that it takes two to tango, or any other logical argument, you're simply asking for resistance. As an aside, I use this approach in couple's therapy as well. During the
Chapter 15
439
initial evaluation, I meet with them together to take their history, and separately as well. Of course, I inform them that I can't keep secrets or withhold information from their spouse. But I do want to know where they stand, and what it would be worth to them if I agreed to take them on as my patient. During the individual session, I try to find out how committed they are to their marriage, or whether they have any secret agendas, such as getting divorced, having an affair or scapegoating their spouse. I also ask them who they think is the most to blame, and who should do most of the changing. Often, they insist that they're not doing anything wrong, and explain that the problems they're having are all their partner's fault. I tell them that I can't accept them into couple' therapy as long as they see it this way, since there wouldn't be any reason for them to change. Sometimes, they say that they're willing to participate in the couples' therapy, because they can help me see what their partner's doing wrong. I explain that each partner must be willing to assume complete responsibility for the conflict and focus exclusively on changing themselves, including doing regular homework assignments designed to help them change they way they feel and relate to the other person. But since they're convinced that they're not doing anything wrong, I'm not convinced that this would be productive for them. Once again, I'm trying to make each partner accountable and establish an effective therapeutic dynamic before getting involved in any actual marital therapy. This can save you from considerable frustration later on. I can only help individuals who ask for help, and even then, it takes a tremendous amount of
Chapter 15
440
creativity and determination! The Relationship Cost-Benefit Analysis is another way to deal with Process Resistance. You can ask the patient to list all the advantages of blaming the other person for the problems in their relationship. How will the blame help them? And how will it hurt them? They can balance the lists against each other on a 100-point scale, and record their ratings in the two circles at the bottom. I've included a comprehensive Relationship Cost-Benefit Analysis on pages 441 and 442. It lists almost every conceivable advantage and disadvantage of blame. You'll notice that for every advantage there's a corresponding disadvantage. Although your patients won't be able to come up with nearly this many advantages or disadvantages, you can ask them to review it as a way of priming the pump when they do their own CBA.
Chapter 15
441
Relationship Cost-Benefit Analysis* Instructions. List all the advantages and disadvantages of blaming the other person for the problems in your relationship. Balance the list against each other on a 100point scale, and put two numbers that reflect your ratings in the circles at the bottom. Advantages of Blaming the Other Person
Disadvantages of Blaming the Other Person
1. I won't have to feel guilty or ashamed.
1. I may feel guilty and ashamed anyway.
2. I won't have to feel vulnerable. I'll feel like I'm protecting myself.
2. I may feel anxious anyway, because I'll be at war with the other person.
3. Truth will be on my side. I'll feel convinced that I'm right and the other person is wrong.
3. The other person won't accept the blame and will insist that I'm wrong and that everything is my fault.
4. I can feel self-righteous and morally superior.
4. I won't experience any spiritual or emotional growth.
5. I can feel like a victim and a martyr.
5. The role of victim can get pretty tiresome.
6. I can feel sorry for myself.
6. I may get addicted to self-pity.
7. Blaming the other person will protect my self-esteem and my pride.
7. I'll be depriving myself of love, joy, and happiness.
8. I can hide my faults.
8. I'll be blind to my role in the problem.
9. I won't have to experience the pain and humiliation of self-examination.
9. I won't experience the joy of intimacy.
10. I won't have to be honest with myself.
10. I'll deny my flaws and have an overly positive view of myself.
11. It's familiar and easy. No hard work will be necessary.
11. I'll become rigid and lose the capacity for flexible thinking.
12. Everything will be predictable.
12. Nothing will change.
13. I'll feel powerful and in control.
13. I'll be powerless to resolve the conflict.
14. I'll show that I can't be pushed around 14. The other person can control me and or taken advantage of. push my buttons. 15. I can fantasize about getting revenge on the other person.
* Copyright
15. The other person may fantasize about getting revenge on me!
2004 by David D. Burns, M.D.
Chapter 15
442
Relationship Cost-Benefit Analysis (cont'd) Advantages of Blaming the Other Person
Disadvantages of Blaming the Other Person
16. I can justify petty behavior, and tell 16. The other person may not put up with myself that the other person deserves it and will probably retaliate. it. 17. I can be passive-aggressive and do nasty things behind their back.
17. I may feel lonely and ashamed.
18. I can insist that I have the right to be angry.
18. It can be exhausting to feel angry all the time. I also have the right to feel happy.
19. The anger will give my life purpose and meaning.
19. I'll get trapped by my anger and enmeshed in the conflict.
20. Life will seem dramatic and exciting. The conflict will make me feel special and important.
20. Fighting can be an energy drain and a waste of time.
21. I can reject the other person.
21. I'll lose the chance to get close to the other person.
22. I can gossip about what a loser the other person is and get sympathy from other people.
22. People may get tired of my complaining and think of me as a whiner.
23. I can scapegoat the other person and look down on them.
23. This may create a pattern for other relationships as well.
24. I can comfort myself by overeating, drinking or using drugs.
24. The constant resentment may lead to headaches, fatigue, or high blood pressure.
25. I can focus on winning and making the other person the loser.
25. I'll lose my creativity and spontaneity.
26. I won't have to be responsible. I'll feel free to say and do whatever I want.
26. I'll constantly have to carry a heavy burden around with me.
27. I can write the other person off as a jerk and convince myself that they're hopeless and inferior.
27. As long as I tell myself that the other person is a loser, it will function as a self-fulfilling prophecy.
Chapter 15
443
If the advantages of blaming the other person strongly outweigh the disadvantages, the patient might put an 80 and a 20 in the two circles at the bottom of the CBA. If they're about equal, the patient might put a 50 in each circle. And if the costs of the blame outweigh the benefits, the patient might put a 40 in the circle on the left and a 60 in the circle on the right. If the patient decides that the advantages of blame are greater than the disadvantages, I tell them that it probably wouldn't be a good idea for us to try to work on the problem because they'd have to examine their own role in the problem and assume complete responsibility for solving it. But that wouldn't make much sense, given the fact that they're convinced it's all the other person's fault. However, I'd offer to work with them on some other problem they wanted help with. If the patient decides that the advantages and disadvantages are 50-50, I'd take the same approach. I'd explain that the pain of interpersonal therapy can be significant, and that a 50-50 weighting probably won't be sufficient for success. Finally, if the patient decides that the costs of blame outweigh the benefits, I'd congratulate them for taking this position and offer to help them with the problem, using the interpersonal techniques that we'll discuss in Chapter 25. Habits and Addictions Describe at least one source of Outcome Resistance for a habit or addiction:
Chapter 15
444
Chapter 15
445
Answer This one should be obvious. In the short-term, the habit or addiction is intensely rewarding, so the patient doesn't want to give it up. In fact, the habit or addiction may be the patient's greatest source of pleasure or satisfaction. From the patient's perspective, successful treatment might look more like a loss than a gain. For example, a patient who abuses alcohol probably loves the taste of beer and looks forward to drinking every night. His wife may be annoyed because he gets violent, blacks out and misses work, and she may have pressured him into treatment. His doctor may be concerned because his enlarged liver indicates cirrhosis. But the patient may not have a strong desire to quit drinking, and probably doesn't want to join AA, either. If you naively assume that he wants to stop drinking, and try to help him achieve this goal, your interventions may not be effective. The same considerations pertain to a bad habit like procrastination. Why do people procrastinate? It doesn't take a genius to figure that out! Procrastination is rewarding, and the thing you've been avoiding seems like a drag. It's certainly a lot more fun to watch a good sporting event or sitcom on television than to get caught up on your filing or back taxes. Process Resistance for a habit or addiction means that you want the positive outcome, but you don't want to pay for it. Think about a habit, like procrastination, or an addiction to drugs, alcohol, food, smoking, or gambling, and see if you can think of at least one source of Process Resistance. Describe
Chapter 15 your thinking here before you continue reading:
446
Chapter 15
447
Answer That one should be obvious, too. Overcoming a bad habit or addiction nearly always involves pain and deprivation. For example, a patient who's overweight may desperately want to be thin and attractive, but dieting may not be very appealing, especially if the patient loves to eat and views it as life's greatest pleasure. In addition, exercise may seem unpleasant, especially if the patient is out of shape. Let's assume that your patient, Sharon, is morbidly obese. She tells you that she desperately wants to lose weight, but for some reason, she hasn't been able to. She's tried book after book, diet after diet, and weight loss program after weight loss program, but she's never been able to stick with any of them. Why is this? Hunger is an overpowering biological force, and most of us don't have any real desire to resist something delicious. Sharon wants a slimmer figure, improved health, better stamina, and increased self-esteem, but when she feels hungry and frustrated, and she's staring at a fresh warm bagel with cream cheese, or a hot chocolate chip cookie that just came out of the oven, it's a different story. The immediate rewards of eating seem far greater than the distant rewards of prolonged dieting and exercising. In the second place, the cost of dieting and exercising is high. It takes time and effort, and it's difficult at first. You can talk until you're blue in the face about how wonderful the "runner's high" feels, but it's not something that Sharon is likely to experience initially. You can also talk about the health benefits of being
Chapter 15
448
thin, and how much sexier she'll feel when she's lost 40 pounds. She'll agree that it all makes perfect sense. But when she feels tired, frustrated, hungry, and tempted, Sharon would much prefer eating a donut to getting out and exercising, especially if it's a cold, rainy day. So the real question for Sharon is this—why should she subject herself to this kind of deprivation and discipline? After all, she can start her diet tomorrow. Tomorrow will be a better day. There may be other motivational issues as well. Sharon may use food to comfort herself when she feels upset, or may feel conflicted about sex and intimacy. It's also possible that her spouse has become preoccupied with her weight, and may constantly try to control or "help" her. She may secretly resent this and eat as a way of thwarting him. We won't know for sure until we explore these issues with her. Instead of trying to persuade Sharon to change, you can ask her this question: "Why should you change? After all, you've got a pretty good deal going here." In addition, you can ask what she'll bring to the table if you agree to help her with this problem. Patients with habits and addictions have compelling reasons not to change. They're standing at a Y in the road. At best, they feel conflicted about which road to take. The decision may not be easy. As you can see, I'm advocating a particular style of dealing with resistance. There are several basic principles: Anticipate resistance ahead of time. Be shrewd. Deal with the resistance
Chapter 15
449
the moment the patient describes the problem, during the Agenda Setting phase, before you get involved in therapeutic interventions. Remember that Outcome Resistance and Process Resistance may both be operating. Never try to persuade a reluctant patient. Once you've identified one or more compelling reasons to maintain the status quo, let the patient persuade you that they do want to change. Depressed patients may be convinced that their suffering is necessary, inevitable, or even helpful. Anxious patients may think that their anxiety protects them or their loved ones. Patients with relationship problems may enjoy the role of victim and may not want to get close to the person they're angry with. And patients with habits and addictions may not want to give up their greatest source of pleasure. Why should they? When the patient resists or expresses ambivalence, empathize. Go with the flow. Find truth in what they're saying. Convey respect, but don't try to persuade them, because you'll instantly get locked into a power struggle. Make the patient accountable. If the patient does want to change, let them know what will be required for successful treatment. If they're depressed, psychotherapy homework will be required, whether or not they feel motivated. If they're anxious, some form of exposure will be required, and it will be anxiety-provoking. If they have a relationship problem, they'll have to give up blaming the other person and examine their own role in the problem. That won't feel very good. And if they're struggling with a habit or addiction, discipline, deprivation and withdrawal will be required.
Chapter 15
450
These are not negotiable issues. They're based on what successful treatment requires. If patients seem ambivalent or express doubt about doing these things, don't try to help them or persuade them. Instead, you can offer to work on another problem or refer them to a therapist who uses an approach that's more compatible with their expectations. Paradoxically, this will often intensify the patient's desire to work with you. Of course, some patients may drop out of treatment or request a referral to another therapist or treatment program. I would consider this a constructive outcome because you've made the requirements of the treatment clear, and you've given them a clear choice. Finally, remember to integrate Agenda Setting with Empathy. If the patient gets upset or begins to resist, put all of your techniques on the shelf and switch back into empathy mode immediately. Listen and try to see the world through the patient's eyes. When the patient feels relaxed, you can try Agenda Setting again, beginning with the Invitation step. Emphasize how much you want to work with the patient and how eager you are to see them recover. Agenda Setting is a powerful technique, and a narcissistic therapist could easily use this technique to punish or get rid of a patient she or he was frustrated with. But if you use it with skill and compassion, it can be the most rewarding and empowering technique of all.
IMPORTANT: NEW and UPDATED several pages of Agenda Setting information in the Appendix starting on page 1248 of this document with flow charts, tips, and expanded help. Learn more about the Magic Button, Magic Dial, Dangling the Carrot, Gentle Ultimatum, and much more!
16*
The Defiant Veteran with PTSD
In this chapter, we're going to integrate some of the ideas you've learned about in the last two sections on Empathy and Agenda Setting. We'll do a handson exercise that will help you learn how to use these tools in real time with real patients. Imagine that you're working with a Vietnam veteran named Chuck who's participating in the PTSD treatment program at the local VA Hospital. His scores on the Brief Mood Survey confirm that he's suffering from extreme levels of depression, anxiety, and anger. His relationship satisfaction score indicates severe marital discord and almost total feelings of isolation. You've completed the intake evaluation and this is an actual treatment session. When you offer to help Chuck with his depression, he challenges you with this statement: "How are you going to help me get over my feelings of worthlessness and guilt? I intentionally killed innocent women and * Copyright
2004 by David D. Burns, M.D.
Chapter 16
452
children in Vietnam. For the past 30 years, their faces have haunted me in the middle of the night, and I wake up screaming. And you think you can show me how to feel joy and self-esteem again?" If you were Chuck's therapist, what would you say next? Put your response below. Use the Five Secrets of Effective Communication on page 242. After each sentence, indicate which techniques you used in parentheses, using the two-letter abbreviations:
Chapter 16
453
Answer Chuck has just attacked you. This may be his way of avoiding intimacy. Hopefully, you resisted the urge to defend yourself or persuade him that you can help, which will simply trigger more resistance and mistrust. Instead, you can acknowledge his feelings and try to see the world through his eyes. Find truth in what he just said. Here's one approach: "Chuck, it sounds like you've been living in a nightmare. (TE; DT) I can only imagine how worthless, guilty and overwhelmed you must feel. (TE; FE) Maybe you feel like you deserve to suffer, and think it would be impossible or even morally wrong to allow yourself to ever feel any joy or self-esteem again. (TE; FE) "I'm concerned that I might have trivialized the horrible suffering you've experienced for the past 30 years, and it seems like you might be feeling pretty angry with me. (IF; DT; FE) I'm also concerned that I might have been insensitive, especially in light of the fact that you gave everything to fight for your country when so many others ran away. (IF; DT; ST) Am I reading you right? (IN)" In this case, you're acknowledging Chuck's feelings and giving him the chance to talk. You're validating his desperation, acknowledging his anger, and avoiding his attempts to polarize the relationship. He's invited you to do battle, and you haven't accepted the invitation. Paradoxically, you're still his advocate, even though he's trying to attack you. That way, the battle will dissolve, and you'll have a chance to form a therapeutic alliance.
Chapter 16
454
Once Chuck has had the chance to vent, and you're on the same team, you can move on to Agenda Setting. What are the five steps in Agenda Setting? List them here before you continue reading: 1. 2. 3. 4. 5.
Chapter 16 Answer The five steps in Agenda Setting are: The Invitation Specificity Conceptualization Motivation Methods How will you do the Invitation step? What will you say? Put your ideas here:
455
Chapter 16
456
Answer You could say something like this: "Chuck, I respect you a lot for what you've lived through, and what you've told me here today. I can see that you're suffering intensely, and I'm wondering if there's some way we might work together to relieve your suffering. Would you be open to this possibility? "Or do you feel like it wouldn't make sense to try to change the way you're feeling, given all the horrors you've been through? You might even feel like you'd be betraying the past if you decided to let go of your suffering and move forward with your life. Where do you stand on this?" You won't become empowered as a therapist until you give Chuck the chance to take a walk and reject the therapy.* If he decides to leave, that's his choice, and he has the right to make that choice. But if he decides to work with you, he's got to sell you on the idea that he has a goal for therapy, and that he's willing to work toward it. Let's assume that Chuck says, "Oh, it's basically hopeless. There's no point in trying, doctor. Everyone knows that there's no cure for PTSD." Of course, your perspective is different. You know that there are powerful new
* Dr. David Ready, a colleague from Atlanta who works with veterans suffering from PTSD, kindly reviewed this chapter and provided much useful feedback, including this statement: "I really like the sentence, 'You won't become empowered as a therapist until you give Chuck the chance to take a walk and reject the therapy.' Many therapists seem to think that you must keep patients in treatment for as long as possible, even if no apparent progress is being made, and that time alone will get the job done. Many of the psychiatric residents I supervise seem to be pressured by their supervisors to keep patients coming in. They have a hard time with the concept that you must have motivation on the part of the patient to create change."
Chapter 16
457
techniques for treating depression and PTSD, and that the prognosis is bright if the patient is motivated. In addition, you know that the feeling of hopelessness is nearly always based on distorted thinking, such as All-or-Nothing Thinking. Still, Chuck is resisting. What will you say to him next? Put your ideas here before you continue reading:
Chapter 16
458
Answer When the patient resists, Empathy is the only thing that has any chance of working. Any attempt to persuade Chuck will be doomed to failure. You could simply respond like this: "Chuck, I know you've been through a lot, including a number of treatment programs that haven't worked out for you. (TE; DT) It sounds like you don't see any reason to pursue further treatment right now, since you're convinced that no treatment or amount of effort could possibly help. (TE; FE) I can imagine that you're probably feeling discouraged, frustrated, and hopeless. (FE) Maybe it even feels less stressful just to give up, so you won't be disappointed again. (FE) Can you tell me if I'm reading you right? (IN)" Once Chuck has had more time to vent, and begins to trust you, he may have a change of heart and decide that he does want help, or he may decide that he doesn't want any treatment at this time. Let's assume that he does want help. How are you going to help him? What will you say next? Put your ideas here:
Chapter 16
459
Answer The next step in Agenda Setting is Specificity. Chuck has to give you an example of one specific problem he wants help with. It has to be specific as to person, place, and time. You could say something like this: "Chuck, I'm glad you want to work with me. Is there a specific problem you'd like to work on first? Perhaps you could describe one moment when you were upset that you'd like my help with. It could be a time in the past week when you were feeling depressed, anxious, or angry, or it could be something that happened a long time ago. It could even be something as simple as sitting here in the office with me right now. Does anything come to mind?" The Specificity step of Agenda Setting works best when it's open-ended. We want Chuck to define the problem he wants help with. If you suggest a problem for him to work on, he'll almost definitely resist. Let's assume that he tells you about a time when he felt especially upset. Don't jump into therapy mode just yet. Don't suggest any solutions to his problem. Instead, find truth in what he's saying. How was he feeling, and what was he thinking about at that moment? What was going on? While you're listening, you'll want to do the Conceptualization step of Agenda Setting. What are the different ways you might conceptualize the problem he describes? Put your ideas here before you continue reading: 1. 2.
Chapter 16
3. 4.
460
Chapter 16
461
Answer The problem Chuck describes might be: An individual mood problem, such as depression or anxiety. For example, he may be feeling guilty, worthless, hopeless, or suffering from flashbacks and panic attacks. A personal relationship problem, such as anger or conflicts with other people. A habit or addiction, such as procrastination or substance abuse. A non-problem, such as unexpressed grief. Of course, he could have a combination of problems. For example, he could be depressed, anxious, and angry with his wife at the same time. He may also be abusing drugs or alcohol. Do you remember why the Conceptualization step is so important? There are at least two reasons. Please put your ideas here: 1.
2.
Chapter 16
462
Answer The Conceptualization step is important because each type of problem will be associated with a different type of resistance. In addition, each type of problem will respond to different types of therapeutic techniques. Once you've conceptualized the problem Chuck describes, you can do the Motivation step of Agenda Setting. Ask yourself why he might be ambivalent about solving it. Remember that for each type of problem, there can be two types of resistance: Outcome Resistance and Process Resistance. What's the definition of each type of resistance? Put your ideas here before you continue reading: What's Outcome Resistance?
What's Process Resistance?
Chapter 16
463
Answer Outcome Resistance means, "I don't want to get better." Process Resistance means, "I want to get better, but I don't want to do what I'm going to have to do to get the job done." We've already talked about Outcome Resistance for Chuck's depression. He may be reluctant to give up his suffering because he believes he deserves to suffer. He may also be reluctant to change if it means the loss of monthly disability payments for his PTSD. Chuck may also have Process Resistance. In order to improve and eventually recover from his depression, he'll have to do psychotherapy homework every day, using forms such as the Daily Mood Log, the Pleasure Predicting Sheet, and others. List five reasons why Chuck may resist doing psychotherapy homework: 1.
2.
3.
4.
5.
Chapter 16
464
Answer There are lots of reasons why depressed patients resist psychotherapy homework. Chuck may feel unmotivated or hopeless. He may think the homework will be too hard. He may buy into the cultural model of therapy, and think that he should simply be able to express his feelings and explore the past while the therapist listens attentively. He may be hooked on the medical model, and think that a pill should cure him. He may feel angry, and think that others are to blame for his problems, or he may feel the need to defeat you because he doesn't trust you. I'm sure you can add to the list! Now let's think about why Chuck may resist treatment for his anxiety. Let's say that Chuck describes panic attacks with terrifying flashbacks of killing women and children in Vietnam. At these times, he feels intense horror and rage. Describe at least one likely source of resistance. We've already talked about the moral issue, so try to focus on another barrier you may encounter. What will Chuck have to do to get over his PTSD?
Chapter 16
465
Answer Chuck may be reluctant to use Exposure Techniques because they seem too overwhelming or upsetting. These techniques can be extremely uncomfortable at first. Most patients naturally resist them, thinking there must be an easier way. Of course, avoidance is the very mechanism that prolongs the anxiety. We have many powerful tools for fighting anxiety. These include a wide variety of Cognitive Techniques, Uncovering Techniques such as the Hidden Emotion Technique, and Motivational Techniques like the Cost-Benefit Analysis. However, exposure will be a mandatory part of our treatment package. A variety of Classical, Cognitive and Interpersonal Exposure Techniques are available. For example, Cognitive Flooding and Memory Rescripting can be especially helpful for patients with PTSD. In most cases, you can't treat anxiety effectively without exposure. Computer scientists at Georgia Tech have even developed a Virtual Reality (VR) program for veterans with PTSD. I've tried this program myself. You put on Virtual Reality goggles, and the program takes you to the rice paddies in Vietnam. You see bombs exploding and snipers firing at you from the trees. You can also go up in a helicopter gunship and fly across the jungle while enemy soldiers are shooting at you. Dr. David Ready, a colleague doing research on PTSD at the Atlanta VA Hospital, has told me that although VR exposure can be powerful, very few veterans have expressed an interest in working with it. It isn't clear to me whether
Chapter 16
466
they're afraid of the intense arousal and anxiety the treatment can create, or whether they're simply afraid of losing their disability benefits if the treatment is effective. Chuck may also resist any psychological intervention because he's seen television ads proclaiming that anxiety results from a chemical imbalance in the brain, and that antidepressant drugs like Paxil or Prozac will do the trick for you. Of course, some patients with anxiety get hooked on addictive agents, such as benzodiazepines and narcotics. Chuck may be looking for prescriptions rather than effective psychotherapy. Now, let's assume that the problem Chuck describes involves anger or a relationship conflict. He may be angry with you, the VA system, or his wife. Can you think of any potential sources of Outcome Resistance or Process Resistance you may run into? Put your ideas here: 1.
2.
3.
Chapter 16
467
Answer Many people with relationship problems aren't really looking for help. Chuck may want to complain about the people he's not getting along with, but may not want to do anything to make the relationship better. He may feel like an innocent victim and think that others are to blame for his problems. If you offer to help him, he may simply get annoyed and insist that you don't understand. Alternatively, Chuck may think of himself as a dangerous monster and keep his distance from others as a way of protecting people, and himself, from his dark, violent side. Remember, he says he murdered innocent women and children in Vietnam. He may feel like he's horrible and unlovable. There's another thing to consider. In the VA system, venting anger endlessly is a treatment model that many veterans and staff seem to be stuck in. The veterans get together in groups and complain. I don't mean to be cynical or disrespectful, but am simply describing something that does happen. So Chuck may feel like his anger is more of an entitlement, or way of life, than a "problem" he needs help with. Finally, let's assume that the problem Chuck describes involves a habit or addiction. For example, he may be using drugs, drinking too much, procrastinating, overeating, or gambling. Describe at least one likely source of Outcome Resistance or Process Resistance:
Chapter 16
468
Chapter 16
469
Answer Habits and addictions feel good. If Chuck gives in to the urge to drink or use drugs, he'll be rewarded immediately. He may think of his habit as the only rewarding thing in his life. It may also be his "treatment" for the pain that's always eating away at him. From his point of view, the real question may be, "Why should I change?" Of course, we won't know the nature of Chuck's resistance until he's described the problem he wants help with and we've discussed it with him. But we already know that he's probably going to resist, since he's already bitten our hand when we reached out to help him initially. So how will you motivate Chuck and persuade him to work with you, in spite of his resistance? Put your ideas here:
Chapter 16
470
Answer Trying to persuade a reluctant patient to change will nearly always trigger more resistance. Most therapists seem to make this error most of the time. For some reason, when patients resist, we tend to take the bait. It's almost like a knee-jerk reaction. It's not your job to persuade Chuck, or any patient, to change. It's the patient's job to persuade you to work with him or her. Once you've highlighted the reasons why Chuck may feel ambivalent about change, you could ask him something like this: "Chuck, I can see that you're experiencing lots of stress and pain, but at the same time, it seems like you have some pretty good reasons not to change. Are you sure that you really do want to change? And if I agree to work with you, what will you bring to the table? What would it be worth to you? How hard would you be willing to work?" Of course, that's a general motivational question. Once we know what he wants help with, we can ask a more focused question that highlights the specific reasons for his resistance, including Outcome Resistance and Process Resistance. Some therapists are afraid to ask this type of question, fearing the patient will decide that they don't want help. In fact, Chuck may say that he's not ready or willing to work on his depression, panic attacks, relationship problem, or addiction. What would you do then? Put your ideas here:
Chapter 16
471
Chapter 16
472
Answer You have several options: You can empathize again. You may have moved into Agenda Setting prematurely, and Chuck may need more time to vent his anger and despair. After you've listened for a session or two, you can issue the Invitation again. You can accept the fact that Chuck doesn't want to work on the problem he's described, and ask if there's another problem he'd prefer to work on. You can explore why he doesn't want to change. For example, you could do a Paradoxical Cost-Benefit Analysis. Chuck could list all the advantages of the status quo, and all the disadvantages of change. Once he's completed his lists, ask him if he can see any good reason to work on the problem, given all the powerful reasons not to change. You can ask him if he wants to be in therapy, or if he's there because of some external coercion, such as pressure from his wife. If he wants help but feels that you're not the right therapist for him, you can offer to refer him to someone else. If he doesn't want to be in therapy, you can offer to terminate the treatment, but let him know that he's always welcome to return if a problem surfaces that he does want help with. There's both a philosophical and a practical basis for this approach. From a Buddhist perspective, our need to be successful causes us to fail. We sometimes chase our patients and try to force them to change because we want to feel helpful, competent and effective. But then it becomes our job to get them better. Paradoxically, this keeps them stuck.
Chapter 16
473
From a practical perspective, we're acknowledging a basic fact of human nature. You can't change people against their will. At least I can't! Without teamwork, it's practically impossible to make any kind of meaningful progress. Patients have to ask for help or we can't do a thing. But if they trust us, and are willing to work with us, we may be able to move mountains together.
17*
"Life stinks! What do you intend to do about it?"
You won't learn how to use Agenda Setting simply by reading about it. Practice will be necessary. The exercises in this chapter will show you how to develop a meaningful therapeutic agenda with challenging patients suffering from a variety of complaints, such as: Binge eating An identity crisis Codependency Chronic pain Drug addiction Self-mutilation After I describe each problem, I'll ask you what you'd say next in order to set the agenda for today's session. In each case, imagine that you've completed
* Copyright
2004 by David D. Burns, M.D.
Chapter 17
475
the history and diagnostic screening. Today, the rubber meets the road. Don't get discouraged if you feel stumped by some of the problems. Just give it your best shot. There are no right or wrong answers, and anything you write down will get your brain moving. Before you try the first exercise, let's quickly review the five steps in Agenda Setting: 1. The Invitation. Ask the patient is she or he feels ready to work on one of the problems that have been causing so much distress. 2. Specificity. If the patient accepts the invitation, ask them to describe one moment when they were feeling upset. The problem must be real, and specific as to person, place, and time. 3. Conceptualization. Is the problem an individual mood problem, like depression or anxiety, a relationship problem, a habit or addiction, or a nonproblem? Does it involve more than one category? 4. Motivation. Each type of problem may be associated with Outcome Resistance and Process Resistance. Don't try to help patients until they've convinced you that they want to change and that they're ready, willing and able to do what's going to be necessary to solve the problem. 5. Methods. There are at least 50 basic CBT methods available. Your choice of methods will depend on your conceptualization of the problem. I would suggest that you complete the problems one at a time, and read my answer before moving on to the next problem. After you've done a few of them, take a break. Don't try to do them all at one sitting. A few days later, you
Chapter 17
476
can try a few more. Your understanding and skills will increase over time.
Agenda Setting Exercises 1.
A patient who's overweight. (answer on page 489) Your patient, Marni, has had trouble trying to lose weight. Whenever she's
upset, she comforts herself with food, and often binges. She feels bad about her life and the way she looks. How will you help her? Invitation. How will you do the Invitation step of Agenda Setting? What will you say to her?
Specificity. How will you make the problem specific with regard to person, place and time? Write down what you'll say to Marni.
Conceptualization. How will you conceptualize the problem Marni has
Chapter 17
477
described? What are some possibilities?
Motivation. What will you say to assess Marni's motivation? Think about Outcome Resistance and Process Resistance.
Methods. Once Marni has described a problem, and she's convinced you that she's ready and willing to work on it, you can select the methods you're going to use. We'll discuss the selection of methods for different problems in Part VII of this book. 2.
The patient with an identity crisis. (answer on page 491) Your new patient, Alice, is an anxious high school senior. She makes
straight A's and gets along well with her parents and classmates. She's Class President and received high scores on her SATs. She's an excellent athlete, and
Chapter 17
478
is captain of the swimming team. Alice explains that she's been happy nearly every minute of her life until several weeks ago, when she suddenly became anxious. Since then, she's been struggling with overwhelming feelings of panic and anxiety every waking minute. She even wakes up with feelings of panic in the middle of the night. Her history is unremarkable. Alice has never had any episodes of depression or anxiety in the past. When you ask her if she feels ready to work on the anxiety that's been plaguing her, she seems enthusiastic. When you ask Alice what she wants to work on during today's session, she tells that she wants help with her "identity crisis." What will you say next? How will you help Alice with her "identity crisis?" Put your ideas here:
3.
A man who's suffering from chronic chest pain and fatigue. (answer on page 496) Your patient, Roger, tells you that he needs help for chronic pain and
fatigue. He's been to seven different physicians. They've done test after test but haven't been able to diagnose the problem. All the tests come back perfectly normal.
Chapter 17
479
After Roger has vented, you ask if he feels ready to roll up his sleeves and work on the problem. He says he does. How are you going to help Roger with his pain and fatigue?
4.
A patient with codependency problems. (answer on page 498) A young woman tells you she has a problem with "codependency." What's
the best way to treat this problem?
5.
A hospitalized addict who says he needs to get his life together. (answer on page 498) You ask a hospitalized, depressed addict named Robert what he'd like to
work on in today's session. After a long moment of silence, Robert says, "I guess I really need to get my life together." What will you say next to develop a
Chapter 17
480
productive agenda for the session? How will you help him get his life together?
6.
An obsessive schoolteacher who wants to have more fun in life. (answer on page 499) You're treating an attractive, 28 year-old grammar school teacher named
Eleanor who comes from a rigid, conservative religious background. She has dysthymic disorder, obsessive tendencies, and mild social anxiety. When you ask Eleanor what she wants help with during today's session, she tells you that she's bored and lonely and wants to "have more fun in life." What will you say to Eleanor so you can develop a productive, meaningful agenda for today's session?
7.
An angry, depressed, obese, pregnant physician who abuses alcohol
Chapter 17
481
and drugs. (answer on page 499) Your new patient is a severely depressed, obese physician. She's pregnant, drinks excessively and abuses drugs. She's terrified that her baby will have a birth defect because of her substance abuse, but says that she just can't control herself. She tells you she's studied virtually every weight loss book and tried all the addiction treatment programs but nothing has ever worked. She wants to know how you intend to help her when everything else has failed. What makes you such an expert? She seems defiant, and you feel anxious and defensive. What will you say next?
8.
A lonely college student who mutilates herself with razor blades. (answer on page 500) Your patient is a college student named Dina who's had several inpatient
hospitalizations for depression and self-mutilation with razor blades. She tells you that she's lonely. What will you say to her to develop a meaningful agenda for today's session?
Chapter 17
9.
482
An angry college sophomore who insists that "life stinks." (answer on page 501) An angry, depressed college sophomore named Linda was encouraged by
her parents to seek treatment. They felt like she'd been unhappy for a long time and wasn't relating very well to her classmates. When you ask Linda if there are any problems she'd like to work on, she crosses her arms, tells you that "life stinks," and wants to know what you intend to do about it. You ask Linda if she can give you an example of how life stinks. She has lots of examples. She says that friends betray her, people are two-faced, her parents are jerks, and her professors are phony and dishonest. For example, her roommate promised to spend Thanksgiving with her, but backed out at the last minute when she got a new boyfriend. The dental receptionist mixed up Linda's appointment, but got defensive when Linda accused her of being disorganized. Linda tells you that all her classmates care about is popularity, jewelry and clothing. They can't be trusted because they're superficial and out for themselves. What will you say next? How will you develop a meaningful agenda for today's session?
Chapter 17
483
10. An oppositional woman who procrastinates. (answer on page 502) Your patient is an angry, depressed woman named Margarita. She tells you that she's been procrastinating at work for years and is in danger of getting fired. All day long, she sits at her workstation, trims her nails, and reads magazines, but tries to look busy whenever her boss walks by. She explains that she's pretty good at B.S., and has been able to keep the wolves at bay, but doesn't know how much longer she can maintain the façade. Every time she tries to do some work or get caught up, she feels unbearably anxious and overwhelmed. She says she's hopelessly behind, and can't possibly do any work when she feels so upset. Whenever she thinks about work, she tells herself: I'll never get caught up. The situation is hopeless. I don't know what I'm doing, or even what I'm supposed to do. Even if I try, it will only be a drop in the bucket, and it won't make any difference in the long run. I must be a lazy person.
Chapter 17
484
I don't have what it takes to do this type of work. It would be too upsetting to do this right now. If I read this magazine, it will calm me down. Margarita tells you that her anxiety is so intense that it's literally impossible for her to do anything productive. She wants you to show her how to relax, so she can start to get caught up on things. How will you help Margarita feel more relaxed so she can get caught up at work?
11. An angry woman with diabetes and visual problems. (answer on page 503) Your patient is a 19 year-old college student named Donna who's suffering from feelings of insecurity. She has childhood-onset diabetes and has experienced episodes of blindness due to retinal hemorrhages. She has to have her eyes periodically drained to regain her vision, and even then, her vision is poor. She's been living with a young man, but their relationship isn't going very smoothly. They argue constantly. Donna tells you she was recently talking to a friend who was dating several fellows at once and playing them off against each other. When Donna's
Chapter 17
485
friend told her that she'd just gotten engaged, Donna felt angry and jealous, and had the thought, "I wonder which guy she trapped?" Donna has heard positive things about cognitive therapy, and wants you to show her how to make her anger go away, so she won't feel angry and resentful toward her superficial, manipulative friend. What will you say to her? How will you develop a meaningful agenda for today's session?
12. A lonely man who feels too shy to flirt or ask women out. (answer on page 505) Your patient is an attractive 32 year-old man named Nick who suffers from shyness. He gets intensely anxious when he interacts with attractive women. He's so afraid of looking awkward that he avoids women altogether. He's willing to do all the written psychotherapy homework assignments, like filling out the Daily Mood Log, and he's pretty good at talking back to his negative thoughts. However, he's not willing to flirt with women or ask anyone for a date. He wants you to show him how to get over his anxiety before he takes the next step. You've tried numerous CBT techniques with partial success. How will you reduce Nick's anxiety further, so he'll feel confident and relaxed enough to ask a
Chapter 17
486
woman for a date? What will you say to him?
13. A divorced man with agoraphobia. (answer on page 508) One of my psychiatric residents asked me to supervise his treatment of a divorced man named Ted who was suffering from agoraphobia and depression. Their most recent session had been particularly frustrating. The resident wanted to set the agenda properly, so he asked Ted for a specific example of how his agoraphobia was causing problems for him. Ted explained that his ex-wife had custody of their 7 year-old son. He only got to see his son twice a month, so their time together was precious. He'd promised to take his son to Atlantic City for his eighth birthday so they could walk along the boardwalk and visit the amusement park. They drove to the hotel with great expectations, but the moment they got inside, Ted's agoraphobia hit him. He became anxious and was afraid to leave the hotel. After they brought their luggage up to their room, Ted told his son that they should check out the game room. After spending some time playing video games, they returned to their hotel room. Ted's son pulled him eagerly to the window. He pointed to the roller coaster in the distance and a father walking with
Chapter 17
487
his son along the Boardwalk just below their window. Ted's son asked, "Can we go now, Daddy?" Ted felt anxious and said it wasn't time yet because they had to watch a Philadelphia Eagles football game on television first. His son looked disappointed but sat quietly as they watched the game together. The resident asked, "What happened next?" Ted hung his head and said, "Doc, I kept making excuses the whole damn weekend and we never did get out of the hotel. I feel so ashamed." The resident asked Ted if he had any negative thoughts or frightening fantasies when he thought about going out on the Boardwalk. What was he the most afraid of? What did he think might happen if he and his son went outside? Ted stared at the floor and replied, "I didn't have no thoughts, Doc. This always seems to happen!" The resident said that the rest of the session was like trying to blow air into a balloon with a hole in it. They just kept spinning their wheels. The resident said he thought he was doing it by the book, asked me if he'd made any errors. He actually made two fundamental errors. Did you spot them? Why were the resident's attempts to set the agenda so ineffective? Put your ideas here: Error 1.
Error 2.
14. A woman with an affair. (answer on page 511)
Chapter 17
488
You're treating a 42 year-old executive named Gloria who's been having an affair with a married man. He lives in another state and only sees her when he's in town for business. He typically calls her at the last minute and never contacts her between visits. Although they've never had sex, Gloria describes their relationship as special and intense. She explains that he's stuck in a bad marriage and hasn't been able to get close to his wife. But he doesn't want to leave his wife until the time is right, for fear of hurting her. Gloria has had similar relationships with married men in the past. Those relationships didn't work out, and she ended up feeling hurt. She tells you that she's perfectly content with the current relationship and just needs to talk and "sort things out." She realizes he might not leave his wife, but insists that she won't let herself fall in love with him. She imagines a course of talking therapy lasting a year or two, similar to treatments she's received in the past. What will you say to her to develop a meaningful agenda for today's session?
Chapter 17
489
Answers to the Agenda Setting Exercises 1.
A patient who's overweight. (problem on page 476) Invitation. Ask Marni if she feels ready to roll up her sleeves and work on
one of the problems she's been describing. Does she feel ready to get started? Or does she need to talk some more while you listen and provide support? Marni came to therapy because of problems losing weight, but may want help with depression, loneliness, or a relationship conflict. She's got to tell us what she wants help with today. Specificity. The problem Marni describes could be anything at all. If she wants help with overeating, ask her to describe a specific moment when she was struggling with this problem. She may describe feeling tempted that morning when she passed the bakery and caught the seductive scent of cinnamon and fresh pastries in the air. She might describe a moment right after she gave in to the urge to binge, and felt guilt and self-loathing. She might describe how she gave herself lots of excuses not to exercise once she got home. The problem could be something totally different. Marni might describe an argument with her mother or her boyfriend. If so, ask her to describe one moment when they weren't getting along. What did the other person say to her, and what did she say next? If she asks for help with depression or low self-esteem, ask her to describe a specific moment when she feeling that way. Where was she? What was going on? How was she thinking and feeling? Conceptualization. Your conceptualization will depend on the problem
Chapter 17
490
Marni describes. We could think about her weight problem as: A habit or addiction. She feels tempted to overeat. Eating provides instant gratification and comfort. A personal relationship problem. Marni may be in a power struggle with someone who's trying to persuade her to lose weight. Her overeating may be her way of declaring her independence or getting back at people she's mad at. She may fear intimacy, and being overweight may be her way of keeping people at a safe distance. An individual mood problem. Marni may binge when she's frustrated, anxious, or discouraged. Once she overeats, she may beat up on herself, thinking that the misery will make up for her transgressions and motivate her to do better next time. Motivation. What price Marni would be willing to pay if you agreed to work with her on the problem she described? For example, would she agree to record her tempting thoughts on the Daily Mood Log each time she feels the urge to binge? Would she agree to keep a Food Log, and record everything she eats each day and how many calories the food contains? She might protest and say: "Well, I'll try but I can't make any promises. Sometimes I just can't control myself. It sounds too hard to have to write down everything I eat and record the calories all day long." Marni seems to be telling you that she's not committed to change. You could tell Marni that it might be better to work on another problem instead.
Chapter 17
491
Remember, it's not your job to convince her to lose weight. You can also explore possible sources of resistance. Why doesn't she want to do what it will take to lose weight? Does she feel like you're trying to control her? Does she have mixed feelings about becoming thin and attractive? I would try to explore these ideas with kindness and respect. I'd emphasize that I liked her, and was committed to working with her, but didn't have any vested interest in pursing any specific problem or goal. If she didn't want to work on losing weight, we could work on a mood problem, a relationship problem, or anything at all that she was struggling with, as long as she was willing to work hard on the problem, both during and between sessions. 2.
The patient with an identity crisis. (problem on page 477) You can ask Alice to give you a specific example of a time when she was
struggling with her "identity crisis." What was going on when she first began to worry about her identity? Where was she? What time of day was it? Who was she with? Alice explains that her identity crisis began during a psychology class. She was reading about Erik Erickson's "Stages of Human Development." The textbook stated that you have to master certain crises at each stage of your development from birth to death. For example, you have your anal stage, your oral stage, and your Oedipal stage. The book explained that adolescents face the stage of "Identity versus Role Diffusion." In other words, you have to find out who you really are. Furthermore, the book said that if you don't find out who you are, you'll get stuck in the stage of role diffusion and can't move on to the next stage,
Chapter 17
492
which is called "Intimacy versus Isolation." Alice tells you that the moment she read about the role diffusion, she immediately felt a sense of panic because she realized she didn't know who she was. She asked the teacher if it was true that adolescents had to find out who they really were. The teacher said this was correct and asked how many students knew who they were. Every hand except for Alice's went up. She asked the teacher how you were supposed to find out who you really were, but he couldn't answer her question. Since then, she's been frantically trying to figure out who she is, but no one can tell her how to find out. Her friends tell her that they know who they are, but can't explain how they figured it out. Alice is desperate to find out who she really is. She's cooperative and the therapeutic alliance is good. She's highly motivated and willing to do lots of psychotherapy homework between sessions if you can show her how to discover her "true self." What will you say to her next so that you and she can work on this problem in a practical and helpful way in today's session? How will she figure out who she really is? Do you know who you are? How did you figure it out? Put your ideas here before you turn the page:
Chapter 17
493
Answer There's no such thing as an "identity crisis" or a "true self." These terms are meaningless. They're just buzzwords Alice is using to convey the fact that she's upset about something, although she may not be aware of this. Your job will be to find out what she's really upset about. Remember that she'll have to be specific as to person, place, and time. You might ask her if there are any problems in her life she wants help with, such as: A problem with one of her classes. A problem with college applications. An argument with a friend or sibling. A conflict with her parents or boyfriend. Concerns about her health. We need something real to work on. If you talk to her about her identity, you'll go around in circles for years, and you still won't know what the term means. But if you can pinpoint something real that's bothering her, she may be able to resolve the problem fairly quickly. Dr. Aaron Beck described this patient during one of the first cognitive therapy training seminars I attended. The vignette made a strong impact on me, and I learned a great deal from it. If I were this young woman's therapist, I might say: "Alice, I'm afraid that I'm not very good at helping people solve their identity crises. I'm not even sure what the term means. I think I cut classes the day they talked about that in medical school.
Chapter 17
494 "However, I'm sometimes pretty good at helping people with real
problems. Think back on the day you first started to feel anxious. What was going on? Did anything happen that bothered or upset you, aside from the material you read about in the book? "For example, you might have had a problem with your boyfriend, an argument with your parents, or a problem with your health. It could be anything. Does anything come to mind?" Alice explained that she'd received two upsetting letters in the mail that day. One was from Swarthmore College, and the other was from Bryn Mawr College, which was near her home. What do you think those letters said? Both letters said: "Congratulations! You've been accepted. Your qualifications were outstanding, and we're prepared to offer you a generous financial aid package." So what's the problem? Well, which college do you think Alice's mother attended? If you guessed Bryn Mawr, you're right. And what college do you think Alice really wants to attend? If you guessed Swarthmore, you're right again. Like most people who suffer from anxiety disorders, Alice is an exceptionally "nice" person who feels a tremendous need to please everyone. When she's faced with a conflict between what she wants and what she thinks someone else wants, she sweeps her feelings under the carpet. That's why she got anxious. Dr. Beck asked her to do two Cost-Benefit Analyses. First, she listed the
Chapter 17
495
advantages and disadvantages of attending Bryn Mawr. The she listed the advantages and disadvantages of attending Swarthmore. Swarthmore was the big winner. Dr. Beck suggested that Alice could discuss her dilemma with her parents, and tell them exactly how she really felt. Alice came back the next week completely "cured." After a heart-to-heart talk with her mother, she decided to go to Swarthmore and had already mailed in her acceptance letter. She was thrilled with her decision and was ready to terminate therapy. "Hold on," Dr. Beck said. "We haven't dealt with your identity crisis yet!" "Oh, I don't think I have one of those any more," she explained. She terminated treatment that day. Can you imagine what would have happened if he'd tried to help Alice find out who she "really" was? They'd still be working on this problem today! If the patient is suffering from an anxiety disorder, the Specificity step may be difficult. Patients can often give you plenty of examples of times when they felt anxious, but may have trouble pinpointing the problem that's triggering the anxiety in the first place. You can work on the patient's symptoms using CBT techniques, which will help, but the anxiety may not disappear completely until you identify the problem that's really bothering them. Your challenge will be to focus their attention on the feeling or conflict they've swept under the rug, as opposed to ruminating endlessly about their symptoms. This is called the Hidden Emotion Technique. It can complement the cognitive and behavioral techniques that have proven so effective in the
Chapter 17
496
treatment of anxiety disorders. We'll talk more about it on page 757. 3.
A man who's suffering from chronic chest pain and fatigue. (problem on page 478) The country is full of treatment programs for chronic pain. Some patients
are treated with narcotics and benzodiazepines, but these medications can cause addiction and other problems. Some therapists recommend meditation, massage, relaxation training, hypnosis, acupuncture, or other non-specific treatments. Although these approaches clearly have some value for some patients, my approach would be different. I'd find out what type of help Roger is looking for, and explain that my area of expertise is helping people solve problems in their lives. For example, Roger could be suffering from depression or anxiety, or a marital conflict. He may be angry about the shabby treatment he's received from his insurance carrier, or may feel worthless because he's no longer able to support his family. I'd explain that when people resolve these problems, the pain often improves. Of course, there's no guarantee, since everyone reacts to the treatment differently. I'd tell Roger that if he has a problem he wants to work on, I'd be eager to work with him. But if he doesn't have any emotional or interpersonal problem other than the pain, then I might not be the best therapist for him. I can't magically make his pain disappear. My clinical experience indicates that pain often results, at least in part, from emotional factors. This is true when the pain results from clearly organic causes, such as arthritis, or from purely psychogenic factors, when there is no clear-cut medical disorder.
Chapter 17
497
I've recently confirmed this hypothesis using structural equation modeling techniques to analyze the cause and effect relationships between depression and physical pain. We asked this question: Why does physical pain go hand-inhand with emotional distress? Does pain cause feelings of depression, anxiety, and anger, or does the emotional distress cause the physical pain? We examined three groups of patients at Stanford Medical School and at the University of California Medical Center in San Francisco. The parameter estimates were nearly identical in all three groups. Although there was a statistically significant causal effect of pain on depression, it was so small as to be clinically insignificant. For the most part, physical pain did not cause depression. However, there was a large causal effect in the opposite direction. Depression and anger can trigger and greatly magnify pain. In other words, if you have a broken arm, and you're extremely angry or depressed, the physical pain will be greatly magnified. And when you feel more relaxed, the physical pain will improve greatly. Roger will have to accept this notion before we can work together. If he's willing to work on his moods and personal relationships, we may be able to kill two birds with one stone. I'd also assess Roger's motivation carefully. Is he trying to get prescriptions for benzodiazepines, sedatives, or narcotics? Is he looking for support for a disability claim or lawsuit? I'd be clear that I probably won't be able to prescribe medications or support any legal claim. For example, I won't send copies of my medical records to his attorney or testify in court. If he comes to me for treatment, it will only be for psychotherapeutic treatment. This will clarify
Chapter 17
498
whether or not he wants the type of help I'm offering. 4.
A patient with codependency problems. (problem on page 479) The problem is Specificity. I would ask what time of day the codependency
occurred. What day of the week was it? Where was she? Who was she interacting with? What did the other person say? What did she say next? Once the patient describes a real problem, a variety of treatment approaches will spring to mind. But we can't do anything until we have something to hang our hats on. 5.
A hospitalized addict who says he needs to get his life together. (problem on page 479) Specificity and Motivation are the keys to this problem. Is Robert serious
about getting some help or is he just telling you what you want to hear? I might explain that "getting your life together" is too big a job for me to tackle. At most, I can only help Robert with one problem at a time, and the problem has to be specific and real. Is there something that he wants help with? What is the problem? When did it happen? Was there one moment when he felt particularly upset that he wants to work on? The Motivation step will be important because we don't yet know what his real agenda is. Is he receiving treatment because of external coercion, such as a ticket he received for driving while intoxicated, pressure from his wife, or being placed on probation at work? Once Robert describes a problem, and I'd need to find out how hard he'd be willing to work to solve it.
Chapter 17 6.
499
An obsessive schoolteacher who wants to have more fun in life. (problem on page 480) Once again, the issue is Specificity. I might ask Eleanor what her idea of
having more fun in life would be. I'd also ask her about the barriers that seem to be standing in the way. Can she describe one specific moment when she wasn't having much fun that she would like help with? Where was she? What was going on? Perhaps she was at a party, but was afraid to flirt with a young man she was attracted to. Maybe she feels guilty about sex or has negative, self-critical thoughts when she's having fun. Maybe she's compulsive and works constantly. We don't yet know what the problem is. You could also ask Eleanor when she'd like to have more fun in life. And what type of help is she looking for? Once we find out what she's talking about, we can conceptualize the type of problem it is, assess her motivation, and put a meaningful treatment plan together. 7.
An angry, depressed, obese, pregnant physician who abuses alcohol and drugs. (problem on page 480) You need to ask yourself why she's being so defiant. When patients are
upset, you can focus on the tension in a kindly way. If you try to ignore the tension, defend yourself, or attempt to set the agenda, things will quickly deteriorate. Instead, try to draw her out, using the Five Secrets of Effective
Chapter 17
500
Communication. You might say something along these lines: "Dr. Bloom, you tell me that you want help with your depression, overeating, and alcohol and drug abuse problems. I can see how much you love your baby, and how afraid you are, and I want to work with you on these problems. However, I noticed a sharp edge in your voice just now, and I almost felt like I was supposed to defend myself or prove myself to you. I'm not sure why that's going on, and I don't know if you've noticed it, but it feels like we're not quite on the same page yet. "One possibility might be that you've felt defeated each time you've tried to overcome these problems, so you don't want to get your hopes up again and risk another huge disappointment. That would be understandable. Or maybe I said something that rubbed you the wrong way. Does any of this make sense?" In this case, you're switching the focus from Agenda Setting to the failure in the therapeutic alliance. If you say this in a friendly, respectful way, Dr. Bloom will probably soften and begin to open up. Once you've formed a strong therapeutic alliance, you can return to Agenda Setting again. You can ask for a specific moment when she was feeling upset, conceptualize the nature of the problem, and think about the types of therapeutic interventions you're going to use. 8.
A lonely college student who mutilates herself with razor blades. (problem on page 481) We don’t know what Dina means when says she's lonely. Is she's having
Chapter 17
501
a conflict with a friend or roommate? Does she feel that she's not as close to her boyfriend as she'd like to be? Do they argue all the time? Does she feel shy when she's around other students because she feels insecure and doesn't know what to say? We need to find out what she's talking about. Ask her to describe one specific moment when she was feeling lonely. Then you can conceptualize the nature of the problem and assess her motivation. If she feels shy, is she willing to take chances and try new ways of relating to other people? Is she willing to do things that may be anxiety-provoking? What price would she be willing to pay to get over this problem? 9.
An angry college sophomore who insists that "life stinks." (problem on page 482) This is clearly a motivational problem. Linda can describe lots of specific
problems, but may not be motivated to work on any of them. After all, her parents sent her for treatment, and from her perspective, she's just fine. She seems to feel morally superior to her classmates, and believes that everyone else has a problem. If you want to work with Linda, you'll have to make her accountable in a way that won't turn her off. Empathy and trust will be vitally important because she's narcissistic and hypersensitive to any sign of criticism or disrespect. With this in mind, you might say: "You know, Linda, you're absolutely right when you say that life stinks. (DT; TE) I've noticed that, too. (DT) People can be extremely
Chapter 17
502
dishonest and self-serving. (DT) "You're obviously very bright, and I'd love to work with you. (ST) However, I have a problem. (IF) Obviously, we can't change the world, so we'd have to work on changing how you interact with other people, and how you think about them. But you obviously have high standards. (ST) And if the rest of the world is screwed up, I'm asking myself why you should have to change. (DT) That seems unfair. (DT) Tell me how you see it. (IN)" This statement will give you a chance to see where she stands. If you empathize skillfully, and find truth in what she's saying, she may soften. However, she may decide not to continue with therapy. If so, let her know that she's welcome to return any time in the future if she changes her mind. I would view that as an acceptable outcome because you've told her how therapy works, and what will be required. And if she does elect to work with you, you'll be empowered to work with her effectively. 10. An oppositional woman who procrastinates. (problem on page 483) This is a classic Agenda Setting problem, and we can think about Process Resistance as well as Outcome Resistance. Margarita may be asking for a solution that's unrealistic. She claims that as long as she feels anxious, she won't be able to do anything, and that she wants you to make her feel relaxed so she can get started on the many tasks she's been putting off. Unfortunately, Margarita isn't entitled to feel comfortable and confident right now. If she's way behind on everything, it seems obvious that she'll feel
Chapter 17
503
anxious when she tries to tackle those tasks. It will be upsetting at first. I don't have any magic potion that will numb this type of discomfort. I know that when I tackle some overwhelming task I've been putting off, I usually feel anxious at first as well. If Margarita is willing to get started on her work in spite of the intense anxiety she feels, the prognosis will be bright, and there are many cognitive, behavioral and interpersonal techniques we can use to further her cause. But she has to understand that she probably won't feel a whole lot better until after she starts working on the things she's been avoiding. You need to be clear that you may not be able to help her in the way she hopes, and that she'll have to agree to take action no matter how anxious or angry she feels. If this doesn't appeal to her, then you can tell her that it might be better to work on some other problem. I'd also want to listen carefully to see if I could flush out any hidden agendas. Why is Margarita clinging to a job that she seems to resent so much? Why is she acting in such a passive-aggressive manner toward her boss and colleagues? Does she even want a job in the first place? Is she hoping to go on disability for depression? Margarita appears to be on strike. What's going on behind the scenes? 11. An angry woman with diabetes and visual problems. (problem on page 484) You can ask yourself, "Is this patient asking for something realistic? Am I comfortable with what she's asking for?"
Chapter 17
504
I'm not entirely comfortable with the way Donna is setting up the problem. Although CBT can help people overcome inappropriate or excessive anger, some tension is natural in any relationship. If you learn to share your feelings in a respectful way, it can often lead to greater intimacy and friendship, even though it may be uncomfortable at the time. Donna seems to be trying to avoid any discomfort in her relationship with her friend. She blames her friend for being superficial, but she seems to want to keep the relationship on a superficial level! There are clearly some feelings of insecurity lurking underneath Donna's feelings of anger and jealousy. She may feel like she's not very sexy because of her medical problems and episodic blindness, and her relationship with her boyfriend is marginal at best. You can help her deal with her feelings of insecurity using CBT. This may reduce some of the bitterness and jealousy she feels. However, I'd be reluctant to buy her agenda wholesale. She's annoyed with her friend and she wants you to make these feelings go away. Donna's desire to stuff all her feelings and make them magically disappear with CBT sounds "off" to me. I could show Donna how to express her negative feelings to her friend in a tactful, caring way. I could also help her become a better listener, so that she can empathize if her friend feels hurt or criticized by what she has to say. But I probably can't show Donna how to make all her negative feelings go away. I've never been able to achieve that goal for myself, and I don't think it would be realistic or healthy to try. Of course, there's no single "right" or "wrong" approach with any patient.
Chapter 17
505
Psychotherapy is part art, and part science. When the patient describes the problem they want to overcome, ask yourself these questions: Is this goal ethical? Is this goal realistic? Do I have the skills and training necessary to help this patient solve this problem? Therapy involves a contract between two people. You both have to agree on the problems and the methods you're going to use to solve them. 12. A lonely man who feels too shy to flirt or ask women out. (problem on page 485) In some ways, this problem is similar to the one we just discussed. Can we really show Nick how to make his anxiety go away before he flirts with women or asks someone for a date? If I were dating, I'd feel some anxiety at first. I'd just have to start flirting in spite of the anxiety. Once I got into the swing of things, it would be easier. Nick isn't entitled to feel relaxed and confident before he asks a woman for a date. He's only entitled to feel relaxed and confident after he's enjoyed some success in the dating arena. He will be anxious at first. There's no getting around the fact that the treatment of anxiety always requires exposure. Anxious patients never want to do the exposure. But I'm not aware of any way to cure anxiety without exposure. You'll need to negotiate the agenda and find out how motivated Nick is to change. What price would he be willing to pay to solve this problem? How much
Chapter 17
506
anxiety would he be willing to endure in order to overcome this problem? CBT can be extremely helpful. Nick can pinpoint his negative thoughts, identify the distortions in them, and put the lie to them using a variety of techniques. While this may reduce his anxiety to some degree, he'll still have to bite the bullet and face his fears. Let's say that Nick protests and tells you that he just "can't" ask a woman out. He says that he's too anxious and will just make a fool of himself. How would you help him overcome this fear? Put your ideas here before you turn the page:
Chapter 17
507
Answer I wouldn't try to help him overcome this fear! In fact, that's the whole point of this exercise. Instead, I might say that if he doesn't feel ready to take the next step, it's entirely understandable. I would tell him that I'm very committed to working with him, and ask if there's some other problem he'd prefer to work on instead. Suppose he gets annoyed and says, "I came here for help with my shyness, and you're telling me to just go out and start flirting. But I already told you that I'm way too anxious to do that. You're supposed to help me!" What would you say next? ________________________________________________________________ ________________________________________________________________ ________________________________________________________________ ________________________________________________________________ ________________________________________________________________
Chapter 17
508
Answer There's just been an alliance failure, so you'll want to use the Five Secrets of Effective Communication: "Nick, you're right. (DT) You did ask for help with your shyness, and I'm convinced that you can overcome this problem. (TE; ST) However, I'm concerned that you might be feeling frustrated or annoyed with me right now, because I'm asking you to do something that feels impossible. (TE; FE) Is that how you're feeling? (IN)" This will allow Nick to vent his anger and disappointment. Once the trust has been re-established, I'd say something along these lines: "Nick, I wish I could give you exactly what you're asking for. If I had some psychological Novocaine, so that you wouldn't have to experience any anxiety when you ask women out, I'd give it to you. But I don't know how to do that. If I were dating again, I'd also feel some anxiety at first. But once you get into the dating scene, I believe that your anxiety will diminish. "I'm concerned that you may be putting the cart before the horse. You want to feel relaxed so you can ask someone out. But it works the other way around. You may have to do some flirting, and go out on a few dates before your anxiety disappears. If you're willing to bite the bullet, I have lots of methods that can help. But I need to know if you're willing to do this." 13. A divorced man with agoraphobia. (problem on page 486)
Chapter 17
509
The resident made an Empathy error and an Agenda Setting error. Whenever patients are upset, they need a listening ear. Ted hung his head and told the resident that he was feeling ashamed. He needed some time to express his feelings and receive support and understanding. But the resident was so eager to swoop in and use his CBT techniques that he ignored what Ted was saying. If you were the therapist, what might you have said when Ted lowered his head dejectedly and said, "I feel so ashamed"? Put your ideas here:
Chapter 17
510
Answer I might have said something like this: "Ted, my heart goes out to you. (ST) I can see how sad and ashamed you're feeling right now, and how much you love your son. (FE; ST) I'm a father, too, and I know how devastating it can feel when you think you've let your son or daughter down. (IF; FE; DT) I can imagine you might be feeling pretty frustrated with the agoraphobia, too. (FE; IN) Tell me what this has been like for you. (IN)" Any tender statement along those lines will be sufficient. Ted may even begin to cry. With some prompting, he may express all kinds of pent-up problems and feelings that have been bothering him. He might talk about a conflict with his ex-wife, his relationship with his son, or other problems he's experienced because of his agoraphobia. Once Ted has had a chance to get his feelings off his chest, he may feel more relaxed. Then the resident could issue the Invitation, along these lines: "Ted, you've told me about your agoraphobia, your feelings of failure as a father, and your depression. You've also mentioned how frustrating it can be when you try to talk with your ex-wife. All of those would be excellent problems for us to work on. I'm wondering if you feel ready to roll up your sleeves so we can get to work on one of these problems." This way, the resident puts Ted in the driver's seat, and Ted can let him know when he feels ready to get to work, and what he wants to work on. He may
Chapter 17
511
want to work on something other than the agoraphobia. The important thing is to make sure the patient, and not the therapist, sets the agenda for the session. 14. A woman with an affair. (problem on page 487) Some therapists might agree to talk with Gloria in a non-specific way while she "sorts things out." Of course, empathy and careful history-taking are always important, and she will need some time to talk while you listen and draw her out. But I'd be concerned that non-specific talking therapy could go on and on indefinitely without any real resolution of the problem, or any definition of what the problem was in the first place. In fact, Gloria's approach to therapy sounds very much like her approach to her relationships with men. It's vague and unfocused. I'd be tempted to use a different approach. I'd ask Gloria why she wants to sort things out, and what she hopes to accomplish as a result of treatment. She claims that her relationship with this man is wonderful, but at the same time, she seems to be seeking help. What is it that she wants help with? If we had a magic wand, and she got exactly what she wanted from the therapy, what would happen? How would her life change? Is she experiencing frustration, loneliness, depression, or disappointment? Does she want a stable, loving relationship with a man who is available? If so, why does she select married men who aren't available and avoid single men? Gloria is telling herself that she won't fall in love, and that this is just be a temporary fling. She may imagine that she's helping him by relating to him in some deep way that his wife cannot. But after a time, she may fall in love, in spite of her determination not to. She may begin to push for greater commitment, and
Chapter 17
512
ask when he plans to leave his wife. At that point, he'll probably start to feel trapped and anxious, and may back off. This will intensify her feelings of loneliness, desperation and frustration, so she'll push harder. He'll probably get resentful, since she's breaking her promise to keep things light, and may decide to stop seeing her. Then she'll end up feeling worthless, bitter, and rejected. Of course, life is unpredictable, and their relationship may evolve differently. But the pattern I've described is common. In fact, this is exactly what has happened in her previous relationships with married men. I'd discuss this scenario and ask how she feels about it. Does she see it as a problem? There are many tools we could use to help Gloria, but we need to know more about the problem she wants help with. What does she really want, and what price is she prepared to pay to achieve this result?
IMPORTANT: NEW and UPDATED several pages of Agenda Setting information in the Appendix starting on page 1248 of this document with flow charts, tips, and expanded help. Learn more about the Magic Button, Magic Dial, Dangling the Carrot, Gentle Ultimatum, and much more!
Part Six M = Methods: My Fifty Most Effective Techniques A-TEAM
Assessment
Testing Testing
Methods Methods
Empathy Empathy Agenda Agenda Setting Setting
18*
50 Ways to Untwist Your Thinking
We've talked about how to take a really good clinical history, how to empathize and develop an atmosphere of trust and understanding, and how to develop a collaborative therapeutic agenda and head off resistance at the pass. We've also talked about how you can assess clinical progress as well as the quality of the therapeutic alliance at every therapy session. This covers the first four letters of our A-TEAM acronym. Although Assessment, Testing, Empathy, and Agenda Setting are vitally important, they won't be sufficient. You'll still need to guide your patients out of the woods and show them how to overcome the feelings and problems that are bothering them. This brings us to the M of ATEAM. We'll need a variety of innovative and powerful treatment methods, and we'll need to apply them in a skillful, compassionate and creative manner. When patients feel depressed, anxious or angry, negative thoughts flow across their minds. Dr. Aaron Beck proposed that each type of negative feeling results from a specific type of negative thought. For example, if patients are * Copyright
2004 by David D. Burns, M.D.
Chapter 18
515
feeling worthless and hopeless, they may be telling themselves: I'm a loser. I'll never get better. I'm always screwing up. If they're feeling anxious, they'll usually have thoughts of danger. For example, a patient with public speaking anxiety may be thinking: Everyone will see how nervous I am. My mind will go blank. I'll make a complete fool of myself. People will look down on me. What's wrong with me? I shouldn't be so nervous. Patients who feel angry or annoyed usually believe that the other person is intentionally taking advantage of them or treating them unfairly. They may be telling themselves: All she cares about is herself. She's got no right to feel like that. He's a jerk! It's all his fault. When patients feel tempted to give in to a habit or addiction, such as overeating, they're usually having thoughts like this: Mmmm, that donut would taste so good! I'll just have a bite or two. I can skip lunch or exercise later on to make up for it.
Chapter 18
516
I've had a tough day, and I deserve it. Other people can eat whatever they want without getting fat. I have the right to enjoy myself, too. Before they know it, they've gobbled down five donuts. Now they feel intense guilt and self-loathing because they tell themselves: I'm such a fat pig. I deserve to suffer. I'll never lose weight. I just can't control myself! When patients put the lie to these thoughts, they'll feel better. But that's not easy. Most patients have lots of evidence to support their negative thoughts. Many of my patients had been depressed and anxious for years, or even decades, before we worked together. Their family, friends, and therapists had all tried to talk them out of their negative thoughts, but their efforts weren't successful. Many patients had also taken pill after pill, but the promised antidepressant effects never materialized. So when our patients tell themselves that things will never change, they feel like they're facing the truth about themselves. If we're going to help them, we'll have to use some new techniques they've never tried. By the end of the 1970s, my colleagues and I had developed a large number of powerful techniques to help patients who were suffering from depression, anxiety, relationship problems and addictions. Since that time, CBT has benefited from an enormous amount of clinical innovation and research.
Chapter 18
517
Starting on page 522, you'll find a list of 50 CBT techniques arranged by category, along with a brief description of how each technique works. I hope you'll be impressed with how many sophisticated and creative techniques are now available. Once you've mastered them, you'll have the firepower you need to help patients with almost any conceivable kind of problem. At the same time, having to learn 50 techniques may feel overwhelming at first. Many therapists are content to master a few favorite methods and let it go at that. When I was a resident, we were taught to listen and encourage our patients to express their feelings. We didn't have much more than that to offer, aside from medications. This type of treatment was called "Expressive-Emotive Therapy." It didn't work very well, but it wasn't very hard to learn. Earlier, I mentioned that CBT didn't impress me at first. I didn't believe you could really treat severe depression with mental exercises and techniques. I decided to attend Dr. Beck's weekly training seminar so I could try CBT with a few of my more difficult patients, just to satisfy myself that the methods wouldn't work. One of the first patients I treated with CBT was a Latvian woman named Helena. Helena was referred to me following discharge from the intensive care unit at the Hospital of the University of Pennsylvania after a serious suicide attempt. I didn't know quite what to do, so I asked Dr. Beck how you'd use CBT to help someone who was suicidal. He said I should ask Helena about the negative thoughts she had when she was feeling suicidal. What was she telling herself? Once I found out, he might be able to suggest some potentially helpful
Chapter 18
518
interventions. At our next therapy session, I asked Helena about her negative thoughts. She explained that just before she attempted suicide, she'd been feeling totally worthless because it seemed like her life hadn't amounted to anything, and she'd never done anything special or accomplished anything worthwhile. I explained that I was still learning CBT, and asked if I could share this information at Dr. Beck's CBT seminar later in the week. I promised to share his recommendations with her the next time we met. She was fine with that. At the seminar, I described Helena's problem and asked Dr. Beck what to do next. He explained that depressed individuals often jump to conclusions that aren't consistent with the facts, and suggested I might try a technique called Examine the Evidence. I could ask Helena to describe five things that she had accomplished during her life. That seemed logical, so I told Helena about Dr. Beck's suggestion at out next therapy session. She said that was the whole problem, and that she couldn't think of a single worthwhile thing that she'd accomplished in her entire life. I told her to give it some thought at home and jot down anything that came to mind. By the time I saw her the next week, I'd completely forgotten about the assignment and proceeded as I usually did, asking about the side effects of the medications and encouraging her to express her feelings. Halfway through the session, Helena reminded me about the homework assignment and handed me her list. She explained that she hadn't been able to think of a single thing for several days, but then a few things started to come to mind.
Chapter 18
519
The first item she listed was the fact that she'd smuggled her children out of Nazi Germany during World War II, and brought them to the United States so they didn't have to die in Hitler's concentration camps. Number two was the fact that she'd worked hard cleaning people's houses and scrubbing their floors so there'd be enough food for her children to eat. Although it had always been a struggle to make ends meet, she eventually put all her children through college, and her oldest son had just graduated from the Harvard Business School. Helena also listed the fact that she spoke five languages fluently and was a gourmet chef, along with numerous other accomplishments. I was impressed, and asked Helena how she reconciled her list with her conviction that she was a worthless human being who'd never accomplished anything. Helena said that the list didn't seem consistent with the negative thought. In fact, she said that the thought now seemed ludicrous, and she couldn't figure out how she'd ever come to that conclusion in the first place. She told me that she was starting to feel better, and asked if I had any more techniques she could try. I said, "Helena, that's the only technique I've learned so far, but if you're willing to wait for another week, I'll go back to Dr. Beck's seminar and see if I can learn some more!" She was fine with that. With a few weeks, her depression was gone. I was excited about CBT and began to use it with more and more of my patients. I tried to learn one or two new techniques every week. Most of my patients didn't seem to mind the fact that I was learning new methods while I was
Chapter 18
520
treating them, and some of them even seemed to enjoy the extra attention they were receiving. Before long, I had more than 50 techniques in my toolkit, some of which I'd learned in the seminar, and others that I'd created on my own. In the following chapters, I'll describe these techniques and provide you with exercises to help you master them. You'll probably find that you're familiar with some of them, but others will be new to you. I hope that you'll also discover some new ways of using the techniques that you're already familiar with. In most cases, I'll describe a patient who was helped by each technique. I hope these stories will bring the techniques to life for you, because you'll get to see how they work with real people. However, I don't want you to get the idea that all my patients had quick, miraculous recoveries. I almost always had to try many techniques that didn't work before I found the one that did. As a rule of thumb, you'll usually have to try 10 or 15 techniques before you find the one that works for a particular patient. So the goal of therapy becomes to fail as fast as you can. A simple calculation should convince you of this. Suppose that you're working with a chronically depressed individual who has the thought, "I'm worthless." Let's assume that the first 15 techniques you try fall flat, but the 16th technique turns out to be effective. Your patient suddenly stops believing the negative thought and feels a wave of relief. If you fail with four techniques at every session, how many sessions will it take before your patient recovers? The math is simple. Obviously, it will take approximately four sessions. That's what I mean when I say that the goal of therapy is to fail as fast as you can.
Chapter 18
521
Now, let's assume that there are just a few techniques you like to use, and you try them repeatedly with all your patients. How many sessions will it take before your patient recovers? Once again, the math is simple. Your patient may never recover, because the technique that she or he would respond to probably isn't one of the ones you typically use. Then you may wrongly conclude that the patient is resistant or exceptionally difficult to treat. Don't get carried away with any single technique, no matter how impressive it might seem. The most powerful techniques have, at best, a one in ten chance of working for any particular patient. You'll do yourself and your patients a huge favor if you keep a wide variety of techniques in your toolbox. Remember that all of these techniques are like metaphors. They're simply concepts that are designed to trigger your creativity. Don't try to use them literally, in the way that an auto mechanic might change the oil in your car in the same exact way each time. Every patient you work with will be unique, and you'll get the best results if you implement these techniques in a way that reflects your own personality and gifts.
19*
The Daily Mood Log and Recovery Circle
Let's assume that your patient wants help with depression and anxiety, and feels ready to get to work. How do you work with him or her? What do you do first? What do you do second? I nearly always start out with the Daily Mood Log (DML). You'll find a blank Daily Mood Log on pages 534 – 535. The DML may look simple, but it's far more sophisticated than it appears. There are five steps. Step 1—Upsetting Event At the top of the Daily Mood Log, the patient can briefly describe one specific moment when she or he was feeling upset. This is the same as the Specificity step of Agenda Setting. The upsetting event can be anything, but it must be specific as to person, place and time. It can be something as simple as sitting in your office during the session, feeling discouraged and worthless. It could be something that happened last week, or at any time in the patient's life. It * Copyright
2004 by David D. Burns, M.D.
Chapter 19
533
could even be something in the future, like feeling anxious about an airplane flight or a presentation the patient has to give at work next week. Good specificity questions include: What time of day were you upset? Where were you? What was going on? Some patients become evasive when you ask them to describe a specific moment when they felt upset. They may protest and insist that they're upset all the time. You can explain that Step 1 will be easy, since they can select any moment, including the current moment. If the patient refuses to zero in on one moment, you may have to go back to Empathy and Agenda Setting. CBT simply won't work on a general, abstract level. On pages 536 – 537, you can see the Daily Mood Log of a young man named Jason who was struggling with shyness. While he was standing in line at the grocery store on a Saturday afternoon, Jason noticed an attractive young woman checking groceries. He had the distinct impression that she was giving him the eye. Although he had a strong urge to flirt with her, he was gripped by feelings of anxiety and self-consciousness. When he got to the front of the line, he stared at the counter and paid the bill without looking her in the eye or saying a single word. He left the store feeling frustrated, inadequate, and humiliated. As you can see on page 536, Jason described the upsetting event as "Standing in line at the grocery store."
Chapter 19
534
Daily Mood Log* Upsetting Event: % Before
Emotions
% After
Emotions
Sad, blue, depressed, down, unhappy
Embarrassed, foolish, humiliated, self-conscious
Anxious, worried, panicky, nervous, frightened
Hopeless, discouraged, pessimistic, despairing
Guilty, remorseful, bad, ashamed
Frustrated, stuck, thwarted, defeated
Inferior, worthless, inadequate, defective, incompetent
Angry, mad, resentful, annoyed, irritated, upset, furious
Lonely, unloved, unwanted, rejected, alone, abandoned
Other (describe)
Negative Thoughts
% Before
* Copyright
% After
Distortions
1984 by David D. Burns, M.D. Revised 2003.
Positive Thoughts
% Before
% After
% Belief
Chapter 19
535
Daily Mood Log (cont'd) Negative Thoughts
% Before
% After
Distortions
Positive Thoughts
% Belief
Checklist of Cognitive Distortions* 1.
All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6.
Magnification and Minimization. You blow things out of proportion or shrink them.
2.
Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7.
Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3.
Mental Filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4.
Discounting the Positive. You insist that your positive qualities don't count.
9.
Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
Chapter 19
536
Jason's Daily Mood Log* Upsetting Event: Standing in line at the grocery store. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
50%
Embarrassed, foolish, humiliated, self-conscious
99%
Anxious, worried, panicky, nervous, frightened
99%
Hopeless, discouraged, pessimistic, despairing
90%
Guilty, remorseful, bad, ashamed
95%
Frustrated, stuck, thwarted, defeated
90%
Inferior, worthless, inadequate, defective, incompetent
95%
Angry, mad, resentful, annoyed, irritated, upset, furious
90%
Lonely, unloved, unwanted, rejected, alone, abandoned
75%
Other (describe)
Negative Thoughts
% Before
1.
I don't have anything interesting to say.
100%
2.
I never succeed with the really goodlooking girls.
100%
3.
I don't have time to deal with a relationship right now, even if I do end up having a good conversation with her.
100%
4.
I better just keep my mouth shut, since I might say something stupid and upset her.
100%
* Copyright
% After
Distortions
1984 by David D. Burns, M.D. Revised 2003.
Positive Thoughts
% After
% Belief
Chapter 19
537
Jason's Daily Mood Log (cont'd) Negative Thoughts
% Before
5.
People will think I'm a self-centered jerk if I try to flirt with her.
100%
6.
I shouldn't be so loud and obnoxious. If I'm humble and quiet, people will like me more.
100%
7.
I have no personality.
100%
8.
I must be a terrible person because I'm so concerned with superficial things like success and looks.
100%
9.
If I tried to flirt with her, I'd probably get shot down.
100%
10. That would show what a loser I am.
% After
Distortions
Positive Thoughts
% Belief
100%
Checklist of Cognitive Distortions* 1.
All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6.
Magnification and Minimization. You blow things out of proportion or shrink them.
2.
Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7.
Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3.
Mental Filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4.
Discounting the Positive. You insist that your positive qualities don't count.
9.
Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
Chapter 19
538
Step 2—Emotions You'll see nine categories of negative emotions listed near the top of the DML on page 536, with several synonyms for each category. The first category is: "Sad, blue, depressed, down, unhappy." Tell patients to circle all the words in each category that describe how they feel, and indicate how strong that type of feeling is in the "% Before" column, on a scale from 0% (not at all) to 100% (intense). Later on, when patients complete the Daily Mood Log, they can re-rate each emotion in the "% After" column. This will show whether or not they've improved, and by how much. Jason was feeling down when he left the store, and rated this feeling at 50%. He also felt anxious, guilty, inferior, rejected, embarrassed, self-conscious, discouraged, frustrated and angry when he was standing in line. These feelings were intense, so he put high ratings in the "% Before" column, as you can see on page 536. Some therapists claim they have patients who don't know how they feel. I've treated lots of patients over the years, and I can't recall ever running into this problem. I think that's because the Daily Mood Log makes it so easy for patients to identify exactly how they're feeling. Almost every type of negative emotion is listed, so patients can simply tell you which ones apply to them, and how strong each feeling is. Some therapists are unclear about the time frame. Should Jason rate how upset he felt when standing in line? Or after he left the store? Or how he feels right now, sitting in your office?
Chapter 19
539
This is up to you, and it will vary from patient to patient. You'll have to use your common sense. If the patient is depressed, they'll probably feel pretty much the same way most of the time, so the question may not come up. In contrast, anxiety fluctuates greatly, so the frame of reference will be important. I was interested in how Jason was feeling when he was in line at the grocery store, because that's when he was feeling shy, discouraged, and anxious. Identifying and rating the negative emotions will help you with the next step of the Daily Mood Log, where you ask patients to list their negative thoughts. You may recall that according to Beck's theory of cognitive specificity, specific kinds of feelings result from specific kinds of thoughts. Depression usually results from the perception that you're worthless, or that you've lost something that's important to your sense of self-esteem. Hopelessness results from the perception that things will never change and that your suffering will go on forever. Guilt results from the perception that you've done something bad, or that you've hurt someone you love. Anxiety results from the belief that something terrible is about to happen. Frustration results from the insistence that things should be different from the way they are. Anger typically results from the perception of unfairness. Once you see what kinds of feelings the patient is struggling with, it will be easier to identify their negative thoughts. Step 3—Negative Thoughts Ask patients to record the negative thoughts that flood through their minds when they're feeling upset. You could say something like this to Jason: "When you were feeling discouraged, what were you telling yourself?" He might say, "I
Chapter 19
540
was telling myself that I never succeed with the really good-looking girls." Ask him to write this down in the Negative Thoughts column. Now you might say, "And when you were feeling shy and anxious, what were you thinking? What were you telling yourself?" He might say, "If I tried to flirt with her, I'd probably get shot down." Ask him to record this thought as well. You can continue in this way until you've elicited the thoughts that are associated with each type of negative feeling that Jason recorded. Encourage him to keep the negative thoughts short, and to number them sequentially. Long, rambling discourses will be difficult to work with. Now instruct Jason to rate how strongly he believes each negative thought, on a scale from 0% (not at all) to 100% (completely). As you can see on pages 536 – 537, Jason believed all of his thoughts 100%. This is common. If patients didn't believe their negative thoughts, they wouldn't feel upset in the first place. Don't let the patient put rhetorical questions in the Negative Thoughts column, such as, "Why am I so shy? What's wrong with me?" There's really no answer to this question! But there's always a hidden claim lurking behind every rhetorical question. You can easily transform a rhetorical question into a negative thought like, "I shouldn't be so shy." This is a classic Should Statement, and it's relatively easy to challenge. Make sure that you and the patient fill out the Daily Mood Log in a step-bystep fashion, on paper. Many therapists try to work on a purely verbal level, without the help of the written exercises. I think this is a big mistake. When you
Chapter 19
541
do CBT verbally, you'll often go around and around in circles because the negative thoughts will seem so convincing and overwhelming. When the patient lists the negative thoughts on paper, it becomes far easier to identify the distortions in them and challenge them one at a time using a variety of techniques. Although the DML is a CBT treatment tool, you could also view it as a fabulous empathy tool, because you'll look inside your patient's mind and see exactly how she or he is thinking and feeling. Each patient will have a unique mix of feelings, like an emotional fingerprint. In addition, the assessment of the patient's emotions will make it clear how unrealistic the DSM-IV is. We're led to believe that our patients suffer from single "disorders," such as a Major Depressive Disorder. This type of thinking is based on the medical model. For example, a man who comes to the emergency room complaining of a cough and fever may be suffering from bronchitis, and an antibiotic may be all that he needs. But the patients we see will rarely have single problems, such as pure panic or depression. They'll nearly always have a wide variety of feelings at the same time. The DML allows you to individualize the therapy and quickly create a powerful and unique treatment program for each patient. Jason is feeling shy, but he has lots of other feelings as well, so we can't just throw some manualized shyness treatment program at him. Instead, we're going to use a variety of powerful and creative techniques to target the specific thoughts and feelings that are bothering Jason.
Chapter 19
542
Step 4—Distortions Ask Jason to identify the distortions in each negative thought, using the Checklist of Cognitive Distortions that's conveniently located on the second page of his Daily Mood Log. He can record the distortions to the right of each negative thought, using abbreviations. This will reduce the amount of writing he has to do. For example, if the thought is an example of All-or-Nothing Thinking and Emotional Reasoning, he can put AON and ER in the Distortions column. Most negative thoughts contain many distortions, and sometimes you'll find all ten. If the patient can't identify the distortions in a thought, it's probably not a negative thought, but the description of a feeling or an event. By definition, a negative thought is a judgment or interpretation. It's the distorted perception that triggers the feelings. For example, let's say Jason writes this in the Negative Thoughts column: "When I was standing in line, I was feeling frustrated and self-conscious." This is not a negative thought, because it's a description of an event (standing in line) and two feelings (frustrated and self-conscious). You can ask him to list the event at the top of the Daily Mood Log, and to list his emotions directly underneath. In the Negative Thoughts column, he can put the thought that triggered these feelings, such as, "People will think I'm a self-centered jerk if I try to flirt with her." Review the Checklist of Cognitive Distortions on page 537 and see how many distortions you can find in this thought. Check off all the distortions that apply before you read my analysis on page 544.
Chapter 19
Distortion
543
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 19
544
Answer As you can see, Jason and I found all ten distortions in his thought. Distortion
Yes
Explanation
1.
All-or-Nothing Thinking (AON)
Jason thinks that people will judge him in black-or-white terms. It's as if there were two kinds of people: the jerks and the nonjerks. Shades of gray do not exist.
2.
Overgeneralization (OG)
He generalizes from his performance to his self and assumes that everyone else will judge him in the same way.
3.
Mental Filter (MF)
Jason only thinks about all the bad things that might happen.
4.
Discounting the Positive (DP)
He discounts the fact that he's reasonably attractive and that she seemed to be giving him the eye. He also discounts the fact that if he simply smiled and said hello, it would be an accomplishment because he'd be taking the first step toward overcoming his shyness.
5.
Jumping to Conclusions Mind-Reading (MR) Fortune-Telling (FT)
He assumes that other people will be just as judgmental as he is (Mind-Reading) and predicts that he'll screw up if he tries to talk to her (Fortune-Telling).
6.
Magnification and Minimization (MAG / MIN)
Jason magnifies his importance in the eyes of other people. It's as if everyone in the grocery store is watching and waiting to see what he'll do next. He also imagines that his behavior will have an enormous impact on others.
7.
Emotional Reasoning (ER)
He feels like a "self-centered jerk," so he assumes that he really is one.
8.
Should Statements (SH)
Jason believes that he should never be self-centered and should always be humble and self-effacing.
9.
Labeling (LAB)
He labels himself as a "self-centered jerk."
10. Blame Self-Blame (SB) Other-Blame (OB)
Jason seems to blame himself for being attracted to a young lady, as if it were inherently evil. And if she doesn't respond positively, he'll blame himself and write himself off as a loser.
Jason listed these distortions next to thought #5 on his Daily Mood Log. We identified the distortions in the rest of his thoughts as well, as you can see on pages 545 – 546.
Chapter 19
545
Jason's Daily Mood Log* Upsetting Event: Standing in line at the grocery store. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
50%
Embarrassed, foolish, humiliated, self-conscious
99%
Anxious, worried, panicky, nervous, frightened
99%
Hopeless, discouraged, pessimistic, despairing
90%
Guilty, remorseful, bad, ashamed
95%
Frustrated, stuck, thwarted, defeated
90%
Inferior, worthless, inadequate, defective, incompetent
95%
Angry, mad, resentful, annoyed, irritated, upset, furious
90%
Lonely, unloved, unwanted, rejected, alone, abandoned
75%
Other (describe)
Negative Thoughts
% Before
1.
I don't have anything interesting to say.
100%
AON, MR, MIN, ER, SH
2.
I never succeed with the really goodlooking girls.
100%
OG, DP, MR, FT, SH
3.
I don't have time to deal with a relationship right now, even if I do end up having a good conversation with her.
100%
DP, FT, ER
4.
I better just keep my mouth shut, since I might say something stupid and upset her.
100%
MR, FT, MAG / MIN, ER, SH, SB
* Copyright
% After
Distortions
1984 by David D. Burns, M.D. Revised 2003.
Positive Thoughts
% After
% Belief
Chapter 19
546
Jason's Daily Mood Log (cont'd) Negative Thoughts
% Before
% After
Distortions
5.
People will think I'm a self-centered jerk if I try to flirt with her.
100%
AON, OG, MF, DP, MR, FT, MAG, ER, SH, LAB, SB
6.
I shouldn't be so loud and obnoxious. If I'm humble and quiet, people will like me more.
100%
MR, FT, MAG / MIN, ER, SH, LAB, SB
7.
I have no personality.
100%
AON, OG, MF, DP, MR, MIN, ER, SH, LAB, SB
8.
I must be a terrible person because I'm so concerned with superficial things like success and looks.
100%
AON, OG, DP, MAG, ER, SH, LAB, SB
9.
If I tried to flirt with her, I'd probably get shot down.
100%
AON, DP, MR, FT, ER
100%
AON, OG, MF, DP, MR, MAG, ER, SH, LAB, SB
10. That would show what a loser I am.
Positive Thoughts
% Belief
Chapter 19
547
You may have noticed that there's quite a bit of overlap among the ten distortions. This is intentional. Each distortion reflects a different shade of meaning for the same basic concept, but brings it to life for the patient in a slightly different way. For example, All-or-Nothing Thinking refers to the tendency to see yourself as a total loser in the here-and-now because you were rejected or failed to achieve an important goal. Overgeneralization refers to the tendency to project this sense of failure into the future, as if things could never change. Mental Filter refers to the tendency to dwell on all the negative things that have happened, while filtering out anything positive. Discounting the Positive is an even more spectacular mental error. You insist that your positive qualities or experiences don't count. This allows you to maintain a totally negative view of yourself and your life. I once did a factor analysis of the ten cognitive distortions, and came up with two basic factors called "I'm no good" and "You're no good." The "I'm no good" factor was primarily associated with feelings of depression and anxiety. Most of the distortions were strongly associated with this factor, including All-orNothing Thinking, Overgeneralization, Mental Filter, Discounting the Positive, Jumping to Conclusions, Magnification and Minimization, Emotional Reasoning, Self-Directed Should Statements, Self-Labeling, and Self-Blame. The "You're no good" factor was primarily associated with feelings of frustration and anger. Three distortions were strongly associated with this factor: Other-Directed Should Statements, Other-Labeling, and Other-Blame. This analysis suggested that depression and anxiety result from a distorted view of
Chapter 19
548
the self, while anger and frustration result from a distorted view of others. Identifying the distortions is usually easy for patients, and it gives them a sense of mastery. When they identify the distortions in a thought, they might say, "I think this one might be an example of All-or-Nothing Thinking." I immediately reinforce this idea by saying, "I agree with you. It's a classic example of All-orNothing Thinking. Can you share your thinking with me? Tell me why it's All-orNothing Thinking, and why this distortion makes people miserable." This gives patients confidence that they're on the right track, and they feel like they've discovered something important. It also cements the idea that their feelings of inadequacy result from their distorted thinking, and not from reality. This insight won't cure them, but it can be extremely helpful, and it will provide you with ideas about how to challenge each thought. This brings us to the most important principle of CBT: When you change the way you think, you can change the way you feel. Step 5—Positive Thoughts In Step 5, patients challenge their negative thoughts with thoughts that are more positive and realistic. They can record them in the Positive Thoughts column and indicate how much they believe them, from 0% – 100%. Then they can re-estimate how strongly they believe the corresponding negative thoughts. Step 5 is the most important step, because that's where the emotional change occurs. However, there's a great deal of misunderstanding about this step, and about how cognitive therapy works. To be effective, the positive thought must have two characteristics. I call them the necessary and sufficient
Chapter 19
549
conditions for emotional change: The necessary condition. The positive thought must be 100% true. Rationalizations or half-truths won't do the patient any good. The sufficient condition. The positive thought must put the lie to the negative thought. In other words, the patient's belief in the negative thought must go down drastically, and ideally all the way to 0%, or near 0%. If these two conditions are fulfilled, you'll nearly always see an immediate and dramatic change in the way the patient feels. But that's easier said than done, because most patients have believed their negative thoughts for years, and their attempts to challenge them in the past have been ineffective. Here's a common complaint I often hear from patients and therapists who are first learning about CBT: "I can see intellectually that my negative thought isn't true, but I still feel upset." When patients say this, they're actually fooling themselves. If patients really saw that their negative thoughts weren't true, their feelings would instantly change. There is no disconnection between our thoughts and feelings. Our feelings follow our thoughts just as faithfully as baby ducks follow their mother. This will be obvious if you ask the patient to record the positive thought in the right-hand column of the Daily Mood Log. Then ask how strongly she or he believes it, between 0% and 100%. In most cases, it will be a defensive statement or a rationalization, so they'll only believe it 60%, or 30%. This means that the positive thought has failed to meet the necessary condition for emotional change. If the positive thought isn't 100% true, it will have little chance of helping the patient. CBT is based on the idea that "The truth shall
Chapter 19
550
make you free." Patients never need to con or deceive themselves in order to get better. Here's an example of what I mean. Jason wanted to work on his 7th negative thought, "I have no personality." He believed this thought 100%. I reminded him that the thought contained numerous distortions, and asked if there was another way he could think about the situation. Was there another message he could give himself that would be more positive and more realistic? This is called the Straightforward Technique. You don't tell patients how they should think about the situation, but simply ask them to take their best shot and try to put the lie to the negative thought. The positive thought they come up with will nearly always be ineffective because it won't fulfill the necessary and sufficient conditions for emotional change. Jason said he could tell himself, "I have a great personality." I told him to write this down in the Positive Thoughts column and indicate how much he believed it. As you can see below, he only believed it 20%. He explained that he often saw other people his age flirting and having fun, but he always felt uncomfortable because he didn't know how to talk to girls. In this case, the positive thought failed to fulfill the necessary condition for emotional change because it wasn't 100% true. That's why he still believed the negative thought 100%, as you can see in the "% After" column. Negative Thoughts
% Before
% After
Distortions
7. I have no personality.
100%
100%
AON, OG, MF, DP, MR, MIN, ER, SH, LAB, SB
Positive Thoughts 7. I have a great personality.
% Belief 20%
Chapter 19
551
Next, I tried a technique called Examine the Evidence. I said, "Maybe it's true that you have no personality. On the other hand, this thought may not be entirely realistic. Is there any evidence that you do have a good personality?" Jason said, "Well, I can be very funny and relaxed when I'm at home, hanging out with my family." He wrote this in the Positive Thoughts column and indicated that he believed it 100%, since it was true. Then I asked him to estimate his belief in the negative thought, "I have no personality." As you can see, he still believed it 95%. This tiny reduction really amounts to condemnation through faint praise, and indicates that the positive thought wasn't effective.
Negative Thoughts
% Before
% After
7. I have no personality.
100%
100%
95%
Distortions AON, OG, MF, DP, MR, MIN, ER, SH, LAB, SB
Positive Thoughts 7. I have a great personality.
I can be very funny and relaxed when I'm at home, hanging out with my family.
% Belief 20%
100%
Jason explained that his experiences with his mother and his brother didn't count because he still felt awkward and tense when he was around girls his age. In this case, the positive thought fulfilled the necessary condition for emotional change, since it was 100% true, but failed to fulfill the sufficient condition for emotional change, because it didn't put the lie to the negative thought. Each time the patient comes up with a positive thought, ask them to write it down on their DML, rate how much they believe it, and re-rate their belief in the
Chapter 19
552
negative thought. These ratings will provide you with superb quality control. Patients often come up with positive thoughts that sound awesome, but when you ask them to re-rate their belief in the negative thought, you'll discover that they still believe it just as strongly as ever. If you weren't doing the ratings, you might be fooled into thinking that you were doing a great job, and that the patient had really put the lie to the negative thought. Now we're faced with a problem. We've used the Straightforward Technique and Examine the Evidence, but Jason is still convinced that he has no personality. He's tried to put the lie to his negative thought twice, and he's failed twice. Is that bad? Actually, it's par for the course. Every patient struggles at first. If it were easy for our patients to put the lie to their negative thoughts, they'd never come to us in the first place. Fortunately, we have more than 50 techniques available, so we can attack any negative thought from many different angles. You never know which technique is going to be effective. It's always a surprise. However, the distortions in a negative thought will often give you ideas about which techniques to try, because certain techniques are especially effective for certain kinds of distortions. Jason's thought, "I have no personality," is a hidden Should Statement because he's telling himself that he should have a bubbly, outgoing personality and say something terribly clever to the cashier. This puts him under tremendous pressure. He's also Labeling his shyness as a defect in his personality. This will make him feel defeated before he even enters the race.
Chapter 19
553
The Semantic Method is often helpful for Should Statements and Labeling. You simply encourage the patient to use kinder and gentler language. For example, instead of telling yourself that you shouldn't have screwed up, you could give yourself this type of message: "It would be great if I never screwed up, but the fact is, I'm human and I will make mistakes at times. Is there something I can learn from the situation?" Jason is telling himself that he has no personality. I pointed out that this message might feel pretty devastating, and explained that most of us feel nervous and awkward when we're just starting to date. I certainly did! You're simply not going to feel terribly funny or spontaneous at first, because you're not sure what to expect. I asked Jason if there was a less insulting message he could give himself. He came up with this positive thought: "I have a pretty good personality when I'm feeling relaxed. My problem is shyness and anxiety, not a lack of personality." I asked Jason how strongly he believed this thought. He believed it 100%, so the thought fulfilled the necessary condition for emotional change. I asked him if the positive thought reduced his belief in the negative thought. As you can see on page 554, his belief in the negative thought went down to 25%. I thought this was a terrific improvement. How far should you try to reduce the belief in the negative thought? This will depend on the type of negative thought you're working on. Sometimes, you can reduce the belief in a negative thought all the way to 0%. In this case, I thought the reduction to 25% was sufficient. If you push for a greater reduction,
Chapter 19
554
you may lose your credibility with Jason. That's because his negative thought contains some truth. He does feel awkward in social situations. In the future, that will probably change. But for now, we can give the devil his due.
Jason came up with this positive thought when we used the Straightforward Technique. It wasn't effective because he didn't believe it.
Negative Thoughts
% Before
% After
7. I have no personality.
100%
100%
Distortions AON, OG, MF, DP, MR, MIN, ER, SH, LAB, SB
Positive Thoughts 7. I have a great personality.
% Belief 20%
95%
I can be very funny and relaxed when I'm at home, hanging out with my family.
100%
25%
I have a pretty good personality when I'm feeling relaxed. My problem is shyness and anxiety, not a lack of personality.
100%
Jason came up with this positive thought when we used Examine the Evidence. Although he believed it, it didn't reduce his believe in the negative thought.
Jason came up with this positive thought when we used the Semantic Method. It was effective because he believed it, and it greatly reduced his believe in the negative thought.
Chapter 19
555
Once the patient has successfully challenged one negative thought, it's usually easier to challenge the others. Next, Jason decided to tackle negative thought #1, "I don't have anything interesting to say." This thought is another hidden Should Statement because it implies that he should say something clever. It's also an example of All-or-Nothing Thinking, because Jason is thinking about his interaction with the cashier in a black-and-white way. He thinks he'll either sweep her off her feet or make a total fool of himself. Furthermore, he's trying to leap from 0% (total loser) to 100% (Don Juan) all at once. This makes his task impossibly difficult and sets him up for almost certain disappointment and defeat. Is there a smaller, more modest goal he could aim for? After we discussed this idea, Jason came up with this positive thought: "I probably don't need to say anything terribly clever or interesting. I could just start by smiling and saying hello. That would be a good first step." As you can see on page 556, he believed this thought 100%, and his belief in the negative thought went down to 25%. Once again, I wouldn't push for more right now, because we're simply doing armchair work. Jason still needs to get out into the arena and start interacting with people. Once he experiences some success, his belief in the negative thoughts may fall all the way to zero.
Chapter 19
556
This positive thought was effective because Jason believed it, and it reduced his belief in the NT.
Negative Thoughts 1. I don't have anything interesting to say.
% Before
% After
100%
25%
Distortions AON, MR, ER, SH
Positive Thoughts
% Belief
1. I probably don't need to say anything terribly clever or interesting. I could just start by smiling and saying hello. That would be a good first step.
100%
The positive thought fulfilled the necessary and sufficient conditions for emotional change.
Jason was able to put the lie to his negative thoughts fairly easily. It's often a lot harder. You may have to try many techniques before the patient puts the lie to a negative thought. In fact, I remind myself that it will take an average of 10 – 15 techniques before I find the one that works. That means the patient and I will probably have to fail 10 or 15 times before we experience success. This brings us to an important message that we touched on earlier. The goal of therapy is to fail as fast as you can. The more you fail, the faster you'll find the technique that works for each patient. Let's assume that Jason wants to work on the thought, "People will think I'm a self-centered jerk if I try to flirt with her." I've put this thought in the center of
Chapter 19
557
the Recovery Circle on page 558. You can think of the circle as a kind of trap Jason is in, and the arrows are ways to escape from the trap. We'll need lots of techniques, because most of the techniques we try won't work. If you have lots of techniques available, that won't be a problem. Let's complete Jason's Recovery Circle. See if you can list 15 techniques that we could use to help him challenge the thought in the circle. Put one technique in each of the boxes surrounding the circle. You can review the onepage list of techniques on page 559, or the longer list that starts on page 522. Don't worry too much about how each technique would work, or picking the best techniques. If a technique sounds like it might be promising, you can list it. That's all you have to do for now. When you're done, you can read my analysis on page 560.
Chapter 19
558
Jason's Recovery Circle
16
15
1
14
2
13 12 11
3
People will think I'm a selfcentered jerk if I try to flirt with her. 100%
4 5
10 6 9
8
7
Chapter 19
559
50 Ways to Untwist Your Thinking* Basic Techniques
Exposure Techniques
Role-Playing 19. Externalization of Voices
Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques
Philosophical / Spiritual 21. Acceptance Paradox
Compassion-Based
Visual Imaging
5. Double Standard Technique
Truth-Based 6. Examine the Evidence
8. Survey Technique 9. Reattribution
39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
7. Experimental Technique
Cognitive Exposure
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Motivational Techniques
Semantic 12. Semantic Method 13. Let's Define Terms
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
14. Be Specific
Quantitative
30. Devil's Advocate Technique
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Chapter 19
560
Answer On pages 562 – 563, I've listed 25 techniques that might help Jason. I've started with the four Basic Techniques, followed by a wide variety of Cognitive Techniques and Exposure Techniques. We probably won't need all these techniques to crush the negative thought in the center of the Recovery Circle, but it's nice to know that we have so much firepower available. Therapists often ask whether they should do the Recovery Circle on their own, or with the patient. When I first developed the Recovery Circle, I thought of it as a tool for therapists. I did it on my own between sessions, or with my students when we were discussing difficult cases. One day, on impulse, I decided to try it during one of our CBT groups on the Stanford inpatient unit. We chose a negative thought that everybody could relate to, and I put it in the center of a Recovery Circle on our flip chart. I distributed the list of 50 techniques, and asked the patients to select the methods that looked the most interesting to them. They had lots of suggestions, and it turned out to be one of the most dynamic and helpful groups we'd ever had. Many patients experienced a profound improvement in their mood and outlook. I think the Recovery Circle conveyed two messages. First, I was showing them that I knew their problems would be tough, and that we'd have to try lots of methods that wouldn't work before we found the one that did. This rang true, since most of them had been struggling unsuccessfully for years to overcome their feelings of depression and anxiety. They knew that it wouldn't be easy. At the same time, the Recovery Circle conveyed a message of optimism
Chapter 19
561
and hope. Most of the patients had never heard of techniques like the Downward Arrow, the Paradoxical Cost-Benefit Analysis, the Externalization of Voices and the Acceptance Paradox, and were surprised to discover that there were so many innovative methods that could help them. Which techniques should you select for your patients? In the next section of the book, we'll talk about how to select the most effective methods for any patient with any Axis I or II Disorder. But first, I'll show you how each of the 50 CBT techniques works.
Chapter 19
562
Jason's Recovery Circle Self-Monitoring
Hidden Emotion Technique
Semantic Method
Empathy
16
15
1
14 Let's Define Terms
Identify the Distortions
3
11 Feared Fantasy
2
13 12
Acceptance Paradox
Agenda Setting
People will think I'm a selfcentered jerk if I try to flirt with her. 100%
4
Double Standard
5
10 6
Downward Arrow Technique
9
8
7
Cost-Benefit Analysis
Examine the Evidence
Reattribution
Survey Technique
Straightforward Technique
Chapter 19
563
Jason's Recovery Circle
Cognitive Flooding
32
31
Image Substitution
17
30
18
29 28
19
People will think I'm a selfcentered jerk if I try to flirt with her. 100%
27
Paradoxical Magnification
20 21
26
Shame-Attacking Exercises
Self-Disclosure
22 25
24
Smile and Hello Practice
23
Rejection Practice
Flirting Training
David Letterman Technique
20*
Basic Techniques
When I'm helping a depressed or anxious patient challenge a negative thought, I always start with the four Basic Techniques. These techniques won't necessarily result in a great deal of change in the way the patient thinks and feels, but they'll lay the foundation for excellent work and provide you with useful information about the kinds of techniques that are the most likely to be effective. If you skip these techniques, you may be in for some rough sledding, and your efforts won't be nearly as successful. You're already familiar with two of the Basic Techniques—Empathy and Agenda Setting. Now that we're working on a specific negative thought on the patient's Daily Mood Log, we're going to use these techniques in a slightly different way. 1. Empathy When we feel upset, we need someone to listen and see the world
* Copyright
2003 by David D. Burns, M.D.
Chapter 20
565
through our eyes without trying to cheer us up, change us, help us, or give us advice. It can be a tremendous relief just to know that someone's listening. We've talked about the importance of Empathy when patients resist or criticize you. If you empathize skillfully, you can often transform a hostile, mistrustful relationship into one of mutual respect and collaboration. Empathy is equally important when you're helping a patient challenge a negative thought, such as "I'm worthless," or "My problems are hopeless," or "I just know that I'll make a fool of myself when I give my talk." You have to accept patients as they are before they'll let you show them how to change. Empathy may only require a few minutes, but it's vitally important. Let's say you're treating a young woman who feels ambivalent about the man she's been dating. She's trying to decide whether or not to break up with him. She wants help with the thought, "If I break up with Tom, I might screw things up for good." You could say: "It sounds like you're feeling torn. You've told me that you sometimes feel trapped and don't know if Tom is the right guy for you. But you're also afraid that you might screw things up for good if you break up with him. Tell me how that feels." If you jump in and start challenging her negative thought without empathizing, she'll feel that you haven't listened and she may sabotage your efforts. In contrast, if you give her her day in court, she'll feel more motivated to work with you. That's why Empathy always appears in the first box on the Recovery Circle.
Chapter 20
566
2. Agenda Setting Agenda Setting is always the second technique I put on the Recovery Circle. This is sometimes confusing to therapists, because we used Agenda Setting earlier in the session when we identified the problem the patient wanted help with, conceptualized the nature of the problem, and assessed the patient's motivation. So why are we doing Agenda Setting all over again now? We're going to repeat the Motivation step of Agenda Setting because the patient might resist challenging the negative thought in the Recovery Circle. For example, let's say you're working with a depressed man named Dudley who has the negative thought, "I'm a worthless, inferior human being." Dudley tells you that he's felt inferior and worthless ever since he was a child. Ask yourself these questions: "Why does Dudley cling to this belief? Is it possible that he might resist when I start to help him challenge it?" Dudley could resist for all kinds of reasons. He may be convinced that he really is worthless and inferior to other people. He may feel that he has no unique talents and has never accomplished anything special or important. He may believe that he's telling you something valid and simply facing the truth about himself. When you encourage him to put the lie to the thought, he may think that you're being unrealistic. Obviously, he'll resist, and he'd have the right to feel frustrated and disappointed if that was all you could offer. Lots of people have already tried to talk Dudley out of this belief, but their efforts only made him feel worse. That's because they were talking at him, rather than trying to understand how worthless he feels. He may resist your efforts in
Chapter 20
567
order to protect himself from further disappointment. You won't know the exact reason for his resistance until you've explored these ideas with him. What might you say to Dudley at this point to assess his motivation? Put your ideas here:
Chapter 20
568
Answer There are lots of ways to do this. Here's one approach: "Dudley, you've told me that you feel like you really are worthless and inferior, and you've been struggling with these feelings for a long time. Is this something you'd like to work on? What would it be worth to you to overcome your feelings of worthlessness? Would you be open to this possibility if I could show you how? How hard would you be willing to work on challenging your negative thoughts?" If Dudley resists or protests that you don't understand, it means that he's probably not ready to get to work yet. You'll need to empathize again. Let him vent, and try to see the world through his eyes. After you've empathized, you can set the Agenda again, starting with the Invitation step, and ask him if there's something he wants your help with. If, on the other hand, Dudley indicates that he does want help with his feelings of worthlessness and inferiority, and that he'd be willing to work hard to overcome them, you can move on to the next technique on your Recovery Circle. 3. Identify the Distortions This technique is so basic that it's a part of the Daily Mood Log. Ask the patient to identify the distortions in the negative thought, using the Checklist of Cognitive Distortions that appears on the second page of the Daily Mood Log, and record them in the Distortions column. Dudley's thought, "I'm worthless and inferior to other people," contains nine distortions, so his Daily Mood Log might look like this:
Chapter 20
Negative Thoughts
1. I'm worthless and inferior to other people.
569 % Before
100%
% After
Distortions
AON; OG; MF; DP; MAG/MIN; ER; SH; LAB; SB
You'll notice that I've used abbreviations for the distortions. AON stands for All-or-Nothing Thinking, OG for Overgeneralization, and so forth. This saves a lot of unnecessary writing. When patients identify distortions, I use a fair amount of Stroking and Inquiry. For example, if Dudley says that the thought is an example of All-orNothing Thinking, I might say, "That's exactly right, and I like your thinking. Put AON in the Distortions column right next to the thought, and tell me why this thought is an example of All-or-Nothing Thinking." I want him to see in crystal clear terms why this distortion will create lots of unnecessary suffering. I'd ask him to spell out precisely why this is illogical and unrealistic, and how this insight might help him. What do you think? Why might it be helpful to comprehend that the thought, "I'm worthless and inferior to other people," is an example of All-or-Nothing Thinking? Put your ideas here:
Chapter 20
570
Answer Hopefully, Dudley will realize that he's thinking about people in two categories: the worthwhile, superior people, and the worthless, inferior people. Obviously, he doesn't feel like he belongs in the superior group, so he concludes that he belongs in the inferior group. Each distortion provides a different type of insight into why a negative thought is deceptive and misleading. People simply don't fall into two categories of worthwhile versus worthless, or superior versus inferior, because we're all made up of thousands of traits. For any given trait, half the human race is above average, and half the human race is below average. There is no cut-off point for a "superior" or "inferior" human being, so there's no valid way of assigning people to one class or the other. Furthermore, people who are incredibly outstanding in one or two areas will always be average or below average in many others. Einstein once got stuck in an elevator because he couldn't figure out how to operate it. I suspect that his singing voice wasn't anything to write home about, either! Happiness doesn't come from how outstanding you are, but how you think about yourself and your life. Many people who were incredibly famous and successful led miserable lives and eventually committed suicide, while billions of people who were "only average" have enjoyed tremendously fulfilling, rewarding lives. I wouldn't expect these insights to reverse Dudley's negative thinking or cause an instant flood of emotional relief. We'll need more powerful tools to bring that result about. The goal right now is simply to get him thinking about his self-
Chapter 20
571
criticisms more realistically. Each time Dudley identifies a new distortion, I'd go through the same process. For example, if he says that his negative thought contains Emotional Reasoning, I'd tell him to put ER in the Distortions column. Then I'd ask him to explain why his thought is a good example of this distortion, and why it's important to recognize it. I'd want him to see that he's reasoning from his feelings. He feels worthless, so he concludes that he really is worthless. Dudley may also realize that he's involved in a hidden Should Statement. He's telling himself that in order to be worthwhile, he should be better than he is. This is arbitrary and hurtful. No matter how much you've achieved, you can always throw cold water on your accomplishments by saying that you should have done more. Identifying the distortions in a negative thought can help you in two ways. First, patients may begin to doubt the validity of the thought. After all, how valid can a thought be if it contains nine glaring distortions? Second, different distortions tend to respond to different techniques, so you'll have more information about which techniques might help the patient challenge his thought. For example, the Semantic Method almost always works for Should Statements and Labeling, so it's one of the methods I'd definitely include on my Recovery Circle. If a thought contains All-or-Nothing Thinking, I might try Thinking in Shades of Gray, Examine the Evidence, the Double Standard Technique, the Cost-Benefit Analysis, or the Acceptance Paradox. I might also use an Uncovering Technique like the Downward Arrow. However, you don't
Chapter 20
572
need to go overboard with the idea of matching distortions to techniques, because you can never really predict which technique is going to work for a particular patient or thought. 4. Straightforward Technique The Straightforward Technique is usually the fourth technique on my Recovery Circle. Although it's rarely effective, it's always worth a try because it only takes about 30 seconds and will provide you with valuable information about why the patient has been stuck. The Straightforward Technique is very simple. All you have to do is ask the patient if she or he can challenge the negative thought with another thought that's more positive and realistic. I might say something like this to Dudley: "Dudley, we've found nine distortions in your thought, 'I'm worthless and inferior to other people.' In addition, you've said that this thought makes you feel depressed, inadequate, frustrated, ashamed, anxious and hopeless, and that you're tired of feeling that way. I'm wondering if you can think of another way to look at it. Is there another message you could give yourself that would be more positive and realistic?" The patient will nearly always come up with something that's lame and ineffective. For example, Dudley may say, "I could tell myself that I'm probably not the worst person in the world, even though I'm one of the worst." Obviously, this thought isn't going to give him dramatic emotional relief! Remember the necessary and sufficient conditions for emotional change:
Chapter 20
573
The necessary condition. The positive thought must be 100% true. The sufficient condition. The positive thought must put the lie to the negative thought. You can ask Dudley to write the new thought in the Positive Thoughts column of his Daily Mood Log and indicate how much he believes it. He'll probably give this thought a high rating, as you can see below. Then you can ask him to re-estimate his belief in the negative thought. He'll almost certainly tell you that he still believes it 100%, since the positive thought doesn't put the lie to the negative thought. In this example, he's actually validated the negative thought! Negative Thoughts 1. I'm worthless and inferior to other people.
% Before
% After
100%
100%
Distortions
Positive Thoughts
AON; OG; MF; 1. I'm probably not the DP; MAG/MIN; worst person in the ER; SH; LAB; world, even though SB I'm one of the worst.
% Belief 100%
In some cases, the patients' positive thoughts will be rationalizations that simply aren't believable. In my experience, rationalizations are never effective. The thoughts that lead to profound change are always valid. The idea behind CBT is, "The truth shall make you free." It's not surprising that the Straightforward Technique usually fails. If patients could challenge their negative thoughts this easily on their own, they wouldn't need our help in the first place. Occasionally, the Straightforward Technique is effective. In a recent CBT group on the inpatient unit of the Stanford Hospital, I was working with an attorney named Johan who'd been hospitalized for his second severe Major
Chapter 20
574
Depressive Episode. Johan recorded these negative thoughts on his Daily Mood Log: 1. I've destroyed my career and won't be able to reconstruct it. 100% 2. This time, I'm hopelessly depressed. I'll never recover from this episode of depression. 100% 3. I shouldn't be weak and have to ask colleagues for help when I'm stuck with a difficult legal problem. 100% After we identified the distortions in these thoughts, I asked Johan if he could talk back to these thoughts. With very little prompting, he was able to come up with these positive thoughts: 1. I had an episode of depression 15 years ago. After I recovered, I was able to resume my career with no problems at all. Even if I lose some clients, I'll find others, since I usually can't even keep up with the demand for my services. Furthermore, there's no evidence that I'll lose any clients, since they all seem eager to work with me. In fact, I've never lost a client. 100% 2. I recovered from my last episode of depression, and I've improved every time I've ever been in a bad mood. The evidence suggests that I'll probably recover from this episode, too, even though I'm feeling extremely discouraged right now. 100% 3. My colleagues might like me better if I asked for help at times and didn't always play the role of Superman. 100% As you can see, Johan believed all these thoughts 100%, so they fulfilled the necessary condition for emotional change. Then I asked Johan to re-rate his
Chapter 20
575
belief in the three negative thoughts. His belief in all of them fell below 20%, and he felt much better. Since we were on a roll, I decided to cement his gains with a role-playing technique called the Externalization of Voices. I asked Johan to imagine that two attorneys were arguing his case in court. I said I'd play the role of the Prosecuting Attorney and he could play the role of the Defense Attorney. I would try to convince the jury–the other patients in the group–that he was hopelessly depressed and that his career was ruined. It would be his job to challenge my arguments. Here's how it went: David (as Prosecuting Attorney): Ladies and gentlemen of the jury, I wish to point out that this is Johan's second Major Depressive Episode. This shows that he's a hopeless case. He'll never recover. Johan (as Defense Attorney): Ladies and gentlemen of the jury, I wish to point out that this argument is rubbish. Johan recovered from his previous episode of depression, and he's already feeling better. Furthermore, he's learning some useful new tools that seem to be quite helpful. The prognosis for recovery is extremely bright. David (as Prosecuting Attorney): Yes, but his colleagues and clients will find out that he was a psychiatric patient in a mental hospital. Everyone will lose respect for him, and his career will go downhill. Obviously, all his clients will leave him. Johan (as Defense Attorney): More rubbish from the Prosecuting Attorney. Don't listen to him! The fact is, Johan has so many clients right
Chapter 20
576
now, it would be a blessing if some of them left. But even when he was depressed 15 years ago, and hospitalized, he didn't lose a single client. There's simply no evidence to suggest he's going to lose clients, or that anyone is going to look down on him for being depressed. The fact is, he's a superb attorney, and he does great work. David (as Prosecuting Attorney): That may be true, but the fact is, some people will look down on him, whether or not they tell him to his face. Furthermore, he's weak. He's an emotional and intellectual weakling. Sometimes he gets stuck on difficult cases and needs help from his colleagues, even though he doesn't like to admit it. An expert shouldn't have to ask for help all the time. Johan (as Defense Attorney): You're right. Johan has all kinds of flaws and weaknesses, emotionally and intellectually. But most of his colleagues seem to like him even more when they see that he's human and doesn't know all the answers. An expert is someone who's down to earth and honest about his abilities and limitations. Only a fool knows all the answers. David (as Prosecuting Attorney): But I look down on him! He deserves to wallow in shame! Johan (as Defense Attorney): Really? How much wallowing would you recommend each day? Would five or ten minutes be enough? Or would you prefer a stiffer sentence? Johan seemed to relish shooting down my arguments. I asked him who
Chapter 20
577
had won the case, and he said it was a slam-dunk for the Defense. At this point, I asked him to rate his belief in the three negative thoughts again, and they had all fallen to 0%. I administered the Brief Mood Survey, and his scores had fallen to zero as well, indicating that his depression and anxiety had vanished. I do not mean to imply that CBT is a form of magic, or that all my patients recover as quickly as Johan. In fact, the Straightforward Technique usually isn't effective. The moment you see that it's not working, you can simply go on to the next technique on your Recovery Circle.
21*
Cognitive Techniques
Cognitions are the thoughts that flow across our minds. They include perceptions in the here-and-now as well as memories and judgments about what's happening. Right now, you're undoubtedly having thoughts about what you're reading. These thoughts create your feelings. For example, you could be thinking, "Hey, this is really interesting." If so, you're probably feeling curious and interested. Or, you could be thinking, "Ugh! This guy is way off base." If so, you're probably feeling annoyed or skeptical. Cognitive therapy is based on several simple principles: 1. You feel the way you think. Our moods do not result from what happens to us, but from how we interpret it. This principle dates back to the teachings of the Greek Stoic philosopher, Epictetus. Nearly 2,000 years ago, he wrote that people are disturbed, not by things, but by how they think about them. This simple but
* Copyright
2004 by David D. Burns, M.D.
Chapter 21
579
powerful principle is at the core of cognitive therapy. Of course, the negative thoughts and feelings feed each other in a vicious cycle. When depressed patients tell themselves, "I'm a loser. I'll never get better," they feel worthless and defeated. These feelings trigger more negative thoughts, which in turn create more negative feelings. 2. Depression is the world's oldest con. When patients feel depressed, anxious, or angry, they always think about themselves and the world in a distorted, illogical fashion. They give themselves messages that simply aren't true. If you ask them to record their negative thoughts on the Daily Mood Log, you'll see all the familiar distortions, such as Allor-Nothing Thinking, Mental Filter, Discounting the Positive, Fortune-Telling, Should Statements, and Self-Blame. However, patients don't realize that they're conning themselves, because the negative thoughts seem as real and valid as the skin on their hands. When they tell themselves, "I'm a worthless loser," they think they're just facing the awful truth about themselves. Clearly, not all negative thoughts will be distorted. There's a healthy and unhealthy version of every negative emotion. Depression is not the same as healthy sadness, and feelings of grief are appropriate when a loved one dies. Similarly, anxiety is not the same as healthy fear, and healthy anger is not the same as unhealthy, destructive anger. The thoughts that trigger healthy negative feelings will be valid, while the thoughts that trigger unhealthy negative feelings will always be distorted and illogical. Our job is not to make our patients feel happy all the time, but rather to help them get rid of unhealthy negative emotions.
Chapter 21
580
3. When you change the way you think, you can change the way you feel. When patients put the lie to the negative thoughts that trigger their depression, anxiety, or anger, they'll experience a profound and rapid improvement in the way they feel. Although the theory is simple, the implementation can be challenging, especially with individuals who've been suffering for a long time. That's why a wide variety of techniques will usually be necessary. If you look at the one-page overview of 50 CBT techniques on page 581, you'll see that they're organized into six major sections: Basic Techniques, Cognitive Techniques, Uncovering Techniques, Motivational Techniques, Exposure Techniques, and Interpersonal Techniques. In this chapter, we'll review the Cognitive Techniques. There are nine categories: Compassion-Based Techniques. Patients talk to themselves in the same way they might talk to a dear friend who had a similar problem using the Straightforward or Paradoxical Double Standard Technique. Truth-Based Techniques. Patients test the validity of their negative thoughts in much the same way that a scientist might test an interesting hypothesis or theory. This category includes Examine the Evidence, the Experimental Technique, the Survey Technique and Reattribution. Logic-Based Techniques. You expose the illogic in the patient's negative thoughts using the Socratic Method or Thinking in Shades of Gray. Semantic Techniques. Patients learn to modify the highly charged, distorted messages they give themselves using the Semantic Method, Let's Define Terms, or Be Specific.
Chapter 21
581
50 Ways to Untwist Your Thinking* Basic Techniques
Exposure Techniques
Role-Playing 19. Externalization of Voices
Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques
Philosophical / Spiritual 21. Acceptance Paradox
Compassion-Based
Visual Imaging
5. Double Standard Technique
Truth-Based 6. Examine the Evidence
8. Survey Technique 9. Reattribution
39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
7. Experimental Technique
Cognitive Exposure
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Motivational Techniques
Semantic 12. Semantic Method 13. Let's Define Terms
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
14. Be Specific
Quantitative
30. Devil's Advocate Technique
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Chapter 21
582
Quantitative Techniques. Patients can track their negative thoughts for several weeks using Self-Monitoring. They can also schedule periods of time to indulge in their negative thoughts and fantasies, instead of struggling to control them, using Negative Practice or Worry Breaks. Humor-Based Techniques. You can use Paradoxical Magnification and Shame-Attacking Exercises to expose the absurdity in the patient's fears. Role-Playing Techniques. You can transform intellectual understanding into real change at the gut level with techniques like the Externalization of Voices and the Feared Fantasy. These are the most powerful CBT techniques that have ever been developed. Philosophical / Spiritual Techniques. You modify the patient's self-critical inner dialogue and transform the patient's value system with the Acceptance Paradox. This dynamic technique helps patients develop unconditional selfesteem. Visual Imaging Techniques. Just as you can help patients modify their negative thoughts, you can also show them how to modify the upsetting mental pictures that accompany them, using techniques like Time Projection, Humorous Imaging, and Cognitive Hypnosis. Compassion-Based Techniques 5. Double Standard Technique This technique capitalizes on the fact that most of us operate on a double standard. When we feel anxious or depressed, we talk to ourselves in a critical, mean-spirited manner. We blame ourselves and rip ourselves to shreds. But if
Chapter 21
583
we were talking to a dear friend who had a similar problem, most of us would be far more supportive and encouraging. When you use the Double Standard Technique, you ask patients if they'd be willing to give up this double standard and judge all human beings—including themselves—by one set of standards based on truth and compassion. As therapists, we're vulnerable to the same kinds of insecurities that our patients experience. One of my psychology graduate students, Tracy, felt anxious about the role-playing exercises we do during class. I suggested that she might try some CBT on herself, so she recorded these negative thoughts on her Daily Mood Log:
Negative Thoughts
% Before
1. What if I screw up and don't get it right?
100%
2. Then I'll look like a fool.
100%
3. Everyone will think I don't know what I'm doing and look down on me.
100%
4. That would mean I was incompetent.
100%
5. Then I could never have a successful career as a psychologist.
100%
% After
Distortions
Chapter 21
584
Use checks ( ) to indicate all the distortions you can find in her thoughts. Feel free to review the Checklist of Cognitive Distortions on page 535.
Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 21
585
Answer I found all ten distortions in these thoughts: Distortion
Explanation
Yes
All-or-Nothing Thinking
Tracy evaluates her performance in a perfectionistic, black-andwhite manner. If she doesn't do a superb job, she feels like a complete failure.
2.
Overgeneralization
Tracy generalizes from her performance to her self. If she makes a mistake during the role-playing, she feels like she's a failure. She sees any failure as a never-ending pattern of defeat, and thinks her entire career is on the line.
3.
Mental Filter
She constantly thinks about everything she's doing wrong.
4.
Discounting the Positive
She discounts what she's doing right, as well as the tremendous amount she's learning.
5.
Jumping to Conclusions Mind-Reading Fortune-Telling
She assumes that everyone will judge her as harshly as she judges herself (Mind-Reading) and predicts that any error will mean that she's doomed to a dismal future (Fortune-Telling).
6.
Magnification and Minimization
In her mind's eye, her errors loom as large as Mt. Everest, and her strengths seem as insignificant as anthills.
7.
Emotional Reasoning
She reasons from how she feels. She feels inept and inadequate, so she thinks she really is. She feels embarrassed, so she concludes that all the other students really will look down on her if she doesn't appear smooth and polished.
8.
Should Statements
She believes that she should always be successful, and should never fail or make mistakes.
9.
Labeling
She labels herself as a "fool."
1.
10. Blame Self-Blame Other-Blame
She blames herself for her errors and mistakes, rather than viewing them as opportunities for learning and personal growth.
There are three ways we could use the Double Standard Technique to help Tracy challenge her negative thoughts. These include the Straightforward Double Standard Technique, the Paradoxical Double Standard Technique, and the Role-Playing Double Standard Technique.
Chapter 21
586
The Straightforward Double Standard Technique. I'd say something like this to Tracy: "Imagine that you're talking to your friend, Aggie, who's in your psych class. Aggie is very similar to you. In fact, she's like a clone of you, and all her strengths and weaknesses are the same as yours. She's also feeling apprehensive about the role-playing, because she knows she'll make some mistakes in front of her peers. How would you talk to Aggie? What would you say to her?" Tracy might tell you that she'd say something like this: "Aggie, we're all going to make mistakes. That's just a part of the learning process. I'm not going to look down on you, and I don't think anyone else will either. In fact, I'll respect you more, not less, for taking a chance and allowing yourself to be vulnerable in front of the group. That will make it easier for all of us, because we're all struggling with feelings of self-doubt." Ask Tracy why she'd talk to Aggie like that. Tracy will probably say that she wants to be helpful and supportive. Then you can ask if she'd be willing to talk to herself in the same way that she'd talk to Aggie. In other words, would she be willing to give up her double standard and treat all human beings, including herself, with one standard that's based on truth and compassion? If Tracy is receptive to this idea, you can ask her to put positive thoughts opposite the negative thoughts on her Daily Mood Log, and estimate how strongly she believes them. If her belief in each positive thought is 100%, or
Chapter 21
587
nearly 100%, you can ask her to re-estimate her belief in the corresponding negative thought. If her belief in her negative thoughts goes down, it means that you've made a dent in her negative thinking pattern, and she'll probably feel better. Here's an example of how this would work: As you can see, Tracy believed all of her positive thoughts 100%. In addition, there was a substantial reduction in her belief in the negative thoughts.
% Before
% After
1. What if I screw up and don't get it right?
100%
30%
1. I probably will screw up to some extent. That's just part of the learning process.
100%
2. Then I'll look like fool.
100%
15%
2. I may feel a bit foolish, but practically everyone makes mistakes during the role-playing exercises.
100%
3. Everyone will think I don't know what I'm doing and look down on me.
100%
20%
3. In fact, I don't always know what I'm doing, since I'm a beginner. We're all in the same boat. It seems unlikely that the other students will look down on me for volunteering.
100%
4. That would mean I was incompetent.
100%
10%
4. That would mean I was making mistakes and learning from them.
100%
5. Then I could never have a successful career as a psychologist.
100%
5%
5. It seems very unlikely that my entire career would be doomed if I made a mistake during a role-playing exercise!
100%
Negative Thoughts
Distortions
Positive Thoughts
% Belief
If Tracy's belief in the negative thoughts does not go down significantly, it means that this technique probably isn't going to be effective for her, and it's time
Chapter 21
588
to move on to the next technique on your Recovery Circle. The Paradoxical Double Standard Technique. Once again, tell Tracy to imagine that her dear friend, Aggie, is also feeling anxious about the role-playing during class. Remind her that all of Aggie's strengths and weaknesses are the same as hers. Ask Tracy if she'd talk to Aggie in the same way she talks to herself. Would she say, "You know, Aggie, when you do the role-playing, you'll probably screw up and look like a total fool. Everyone will look down on you and see how incompetent you are. Then your career will be ruined"? Tracy will probably insist that she'd never talk to a dear friend like that because it would be cruel and unfair. Then you might say: "But isn't honesty important? You've indicated that all your negative thoughts about yourself are 100% true, so they must be true of Aggie as well. Remember that she's just like you. So I want you to warn her that if she screws up during a role-playing exercise in class, everyone is going to look down on her and her career will go down the drain." Tracy will probably protest that she still wouldn't talk to a friend like this, because the thoughts aren't realistic. You can ask her to explain why they're not realistic, and ask what she'd say to her friend instead. If she comes up with convincing positive thoughts, she can record them on her Daily Mood Log, just as before, and rate how strongly she believes them. Then she can re-estimate her belief in the negative thoughts. Of course, some patients don't have a double standard. Tracy might say
Chapter 21
589
that she really would look down on anyone who screwed up during a role-playing exercise, even though she wouldn't tell them to their face. Once again, this would mean that the Double Standard Technique is probably not going to be effective for her. The Role-Playing Double Standard Technique. You can do either version of the Double Standard Technique in a role-playing format. This makes the technique more dynamic and interesting, because you can play the devil's advocate and hold the patient's feet to the fire.* In the following example, I'm playing the role of Tracy's friend, Aggie, and Tracy is playing herself: Aggie (played by David): Tracy, I'm feeling pretty upset, and I was wondering if I could talk to you for a couple minutes. Tracy (as herself): Sure, no problem. What's up? Aggie (played by David): Well, you know how we're supposed to volunteer for these role-playing exercises during class? I'm really worried that I'll screw up and make a fool of myself. Tracy (as herself): Gee, Aggie, we all make mistakes during the roleplaying exercises. That's why doing them in class is such great practice. It gives us a chance to make mistakes in a safe environment, so we can learn from them. In fact, there's no way to learn these techniques without making lots of mistakes. Aggie (played by David): Yes, I suppose, but won't everyone look down on me if they see me screwing up? * Much like wieners, or even marshmallows, at a picnic!
Chapter 21
590
Tracy (as herself): I sure won't. We're all in the same boat. Aggie (played by David): Yes, but let's face the facts. We're not all created equal. Everyone loves a winner, and some of the students seem to catch on a lot faster than me. Won't they look down on me if I screw up and make a fool of myself? Tracy (as herself): Well, it's certainly possible. Some people are very judgmental, but I don't think most of the students are like that. If someone in our class was extremely judgmental, it might be more of a problem for them, because compassion is crucial in our profession. You can continue to "attack" Tracy in this way, presenting her with challenging versions of her own thoughts. If she defeats you, you'll usually see an immediate change in her negative thoughts and feelings. If she gets defensive or stumbles, you can do a role-reversal and model more effective responses. The Double Standard Technique works well for people who are tenderhearted and compassionate. The idea that you can treat yourself in the same kind way you would treat someone else often makes good sense to them, and provides substantial relief. However, this technique isn't a panacea. It doesn't work well for people who are angry or bitter, because they're usually just as hard on others as they are on themselves. The Double Standard Technique may also be ineffective for perfectionists. They sometimes defend their double standard, explaining that they expect far more from themselves than from others. They may believe that if they beat up on themselves when they fail or make a mistake, it will motivate them to achieve
Chapter 21
591
something spectacular. There's usually a bit of narcissism and pride lurking behind this idea, since it implies they're so far above other people that they have to judge themselves by a loftier set of standards. You can ask if this strategy has been effective for them. Do they feel especially motivated and creative when they're beating up on themselves? If so, maybe this isn't a problem they need help with. And if it's so helpful to them, why not talk to a dear friend in the same harsh way they talk to themselves? After all, wouldn't they want a friend to feel motivated and creative as well? Truth-Based Techniques 6. Examine the Evidence The thoughts that trigger feelings of depression, anxiety, and anger are nearly always distorted and unrealistic, but patients usually don't realize this because they fool themselves with Emotional Reasoning. For example, if you feel like a hopeless loser, you may assume that you really are one and give up on life. Then nothing changes, so you conclude that things really are hopeless. When patients use Examine the Evidence, they can ask themselves, "What are the facts? What do they show?" They become like scientists who examine information that's already been published in order to evaluate the validity of a theory or hypothesis. Emily, a pastoral counselor from Atlanta had a severe flying phobia. I asked her what fantasies came to mind when she thought about flying. What was she so afraid of? She said she was afraid that the passengers would panic during the flight and that she'd be trampled to death in the aisle. She was aware that her
Chapter 21
592
fears sounded silly, but was convinced that it might really happen. I asked Emily to Examine the Evidence for this belief. How many plane tramplings had she read about in the past year? Or in the entire history of aviation? She couldn't recall a single one. Furthermore, there are millions of flights every year, so she had to admit that the likelihood of being trampled to death in a plane is vanishingly small—a fact that she'd actually never considered. I once treated a depressed, 45 year-old woman named Judy who was dying of lung cancer. Her family asked me to see her at her bedside. You might think that anyone dying of cancer would be depressed, but this is not true. Depression results from the harsh, illogical messages we give ourselves. Judy said the thing that upset her the most was being bedridden and dependent on her family. Prior to her illness, she'd been active in volunteer work, such as the local Reading for the Blind program. Now she felt useless because she had to depend on her husband and family to do everything for her, such as cooking and cleaning the house. She felt guilty, worthless, and defeated. Judy recorded four negative thoughts on her Daily Mood Log. She believed all of them 100%. They were: 1. I'm not contributing to society. 2. I'm not accomplishing any of my personal goals. 3. I'm not able to participate in active fun. 4. I'm a drain and a drag on my family.
Chapter 21
593
Use checks ( ) to indicate any distortions you find in Judy's thoughts. When you're done, you can review my analysis on page 594.
Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 21
594
Answer Judy and I found all ten distortions in her thoughts: Distortion
Yes
Explanation
1.
All-or-Nothing Thinking
Judy's thinking about her contributions to others in a black-andwhite way. She tells herself that her contributions to her family are a total zero, and that she's a complete drain on their resources.
2.
Overgeneralization
Judy can't contribute as much as before, so she tells herself that she's not contributing anything at all.
3.
Mental Filter
Judy thinks about all the things she can't do and overlooks the things she still gives to others.
4.
Discounting the Positive
She discounts the value of the many contributions she has made in the past and the contributions she's making even now.
5.
Jumping to Conclusions Mind-Reading Fortune-Telling
Judy assumes that she's a drain and a drag on her family, but she hasn't asked them how they feel.
6.
Magnification and Minimization
The situation is clearly stressful for Judy and her family, but she magnifies how burdened they feel and minimizes the value of the love and caring she provides for them.
7.
Emotional Reasoning
Judy feels guilty, so she assumes she must be guilty of doing something bad. She feels like she's a "drag," so she assumes she really is one.
8.
Should Statements
This is probably the most important distortion for Judy. She's telling herself that she should never be weak or rely on others for help. This is called a hidden Should Statement.
9.
Labeling
She labels herself as "a drain" and "a drag" on her family.
10. Blame Self-Blame Other-Blame
Judy is beating up on herself and blaming herself for not contributing more to others. But she's doing the best she can, given her circumstances.
Although Judy's cancer was real, her loss of self-esteem resulted from the illogical way in which she was thinking about the situation, and not from the cancer itself. It seemed like the Achievement Addiction might be triggering her depression. This is a common Self-Defeating Belief. Judy seemed to be telling herself:
Chapter 21
595
My worth as a human being depends on my achievements and productivity. If I'm not productive, I'm worthless and unlovable. This belief goes back to the Calvinist work ethic. It's an integral part of the fabric of our society, but it can create problems if you take it too far. If you base your entire sense of self-esteem on your productivity and achievements, you may set yourself up for a great deal of unnecessary anxiety and self-doubt. My goal was to help Judy challenge this belief. I tried many techniques that were ineffective, including Empathy, the Straightforward Technique, the Double Standard Technique, and the Cost-Benefit Analysis. Then I decided to try Examine the Evidence. Was it really true that Judy's worth as a human being depended on her productivity and contributions to others? What would the evidence show? I created a chart for her like the one on page 596. The bottom axis represents time in years, from the moment of Judy's birth to the present. The vertical axis represents Judy's worth as a human being, from 0% (worthless) to 100% (the most worthwhile), as well as her productivity, accomplishments and contributions to society, from 0% (no achievement at all) to 100% (the greatest level of achievement). I asked Judy to put a dot on the chart to indicate how worthwhile she was right after she was born. You can see that she put her dot in the upper left-hand corner of the chart. She rated herself at 90% because she thought she was a very worthwhile baby. Then I asked her to put a second mark on the chart to indicate how much she was achieving when she was born. This is the dot in the
Chapter 21
596
lower left-hand corner of the chart. Judy explained that she only rated her achievements at 5%, "because all I did was drink milk, pee and poo." I asked Judy to put marks on the chart to show how worthwhile she was, and how much she was achieving, when she was 5 years old. She said she was still 90% worthwhile but her achievements had gone up to 10% because she'd learned to walk, run, talk and read.
100
Self-Worth (%)
100 80
80
60
60
40
40
20
20
0
0
5
10
15
20
25
30
35
40
Achievement (%)
Achievement and Self-Worth
0 45
Age (years) now
birth Figure 1
You can see these new ratings in Figure 2 on page 598. Judy's ratings of self-worth are indicated by the dashed line across the top of the chart. Her estimates of her achievements are indicated by the solid line below it. I asked Judy to put additional marks on the chart at 5-year intervals to show how worthwhile she was and how much she was achieving up to the time she was 40. As you can see in Figure 3, she rated her worth at 90% each time, but her achievements continued to increase. By the time she was 25, they'd risen
Chapter 21
597
to 75% because she'd completed college, worked, gotten married and had two children. You can see that Judy estimated her achievements steadily at 75% from the age of 25 until the age of 40. Then I asked Judy to estimate them now, at age 45. As you can see in Figure 4, she said that she wasn't accomplishing much again, so she estimated her achievements at 5%, just the same as right after she was born. I told Judy to examine the two lines she had drawn and ask herself if her achievements looked like they were the same as her feelings of self-worth. She looked at the diagram for a moment, and her face lit up. She said that the two lines did not look at all similar. The dashed self-worth line was always at 90%, while the solid achievement line went up and down throughout her life. She said that it suddenly seemed perfectly clear that her worth as a human being had nothing to do with how productive she was at any time in her life. I asked Judy to estimate how worthwhile she was right now, at age 45. As you can see in Figure 5, she estimated her self-worth at 90%. Judy said she no longer felt worthless, so I gave her the Brief Mood Survey again. Her depression score had dropped into the normal range. That was the only therapy session I ever had with Judy. I don't mean to imply that it's easy to treat depression or that everyone recovers that quickly. Most of the time, it's far more challenging.
Chapter 21
598
Achievement and Self-Worth Figure 2
Figure 3
40
40
20
20 0
5
10
15
20
25
30
35
40
20
20 5
10
15
20
25
Figure 5
60
40
40
20
20 20
25
Age (years)
30
35
40
0 45
30
35
40
0 45
100
100
Self-Worth (%)
60
15
40
Figure 4
80
10
40
Age (years)
80
5
60
0
100
0
60
Age (years)
100
Self-Worth (%)
0 45
80
Achievement (%)
60
80
80
80
60
60
40
40
20
20 0
5
10
15
20
25
Age (years)
30
35
40
0 45
Achievement (%)
60
100
100
Self-Worth (%)
80
Achievement (%)
Self-Worth (%)
80
Achievement (%)
100
100
Chapter 21
599
Why did Judy respond so quickly? First, she didn't have a long history of depression, and she was eager to get better. Second, her depression was an acute reaction to an overwhelming catastrophe. These kinds of patients are usually the easiest to treat. In contrast, patients with long histories of depression, but no obvious precipitating events, are usually far more challenging. Finally, Judy and I had good rapport, and she didn't feel the need to defeat me. I received a letter from Judy two months later. She said that the session had been extremely helpful, and that her feelings of depression and worthlessness had not returned. She said that the key to her recovery was seeing that her feelings of self-esteem didn't have to depend on her achievements, or on anything at all. She said she'd grasped the concept of unconditional self-esteem, a concept she'd never really understood. She'd explained that she'd been able to use this idea to help several of her lady friends who were depressed because they were getting divorced and didn't have meaningful careers. They were all basing their self-esteem on something external. Learning how to develop unconditional self-esteem was extremely helpful to them. Judy said helping her friends in this way gave her a sense of purpose, even though she was bedridden. Unfortunately, Judy died from the complications of lung cancer six months later. However, I was grateful I could help her overcome her depression so that she didn't have to struggle with feelings of guilt and worthlessness during the last six months of her life. 7. Experimental Technique
Chapter 21
600
In the last section, you learned how Examine the Evidence helped a woman with a fear of flying. When you use the Experimental Technique, you go even further. You encourage the patient to do an experiment to test the validity of a negative thought or Self-Defeating Belief, in much the same way that a scientist would test a theory. The Experimental Technique is one of the most powerful techniques for treating anxiety disorders, but it can be useful for depression as well. A woman named Lydia often had to accompany her husband on business trips, but every flight was a terrifying, draining ordeal because she told herself: 1. Flying is incredibly dangerous. 2. The plane might tip over on turns. 3. If I don't worry, the plane will crash in a ball of flames. 4. This is awful! I'm not in control. Lydia believed all of these thoughts 100%. In fact, every time the plane banked for a turn, Lydia would lean desperately in the opposite direction in an attempt to stabilize the plane and keep it from tipping over. What kind of experiment could Lydia do to test this belief? Please put your ideas here before you turn the page:
Chapter 21
601
Answer I encouraged Lydia to sit next to the window on her next flight so she could bump up against the wall of the plane every time it banked for a turn, and see if she could force it to tip over. Lydia was extremely reluctant to do this experiment, because she believed that the plane might really tip over. She was surprised to discover that no matter how hard she bumped up against the wall, the plane remained steady as a rock. This made a huge dent in her belief in the negative thought. In fact, it fell all the way to 0%. Of course, the experiment you choose has to be a direct test of the patient's negative thought, so you'll have to be a bit creative when you use this technique. Imagine that you're treating an anxious woman named June who suffers from panic attacks. Each time she has a panic attack, she tells herself, "I'm about to lose control and go crazy." She believes this thought 100%. How could June use the Experimental Technique to test this belief? Put your ideas here before you continue reading:
Chapter 21
602
Answer June could try to drive herself crazy through willful effort in your office. I've done this with many patients with great success, although they're always afraid to try it because they think they really will go crazy. I tell them they can scream, shout, flail their arms, talk in tongues, roll around on the floor, bark like dogs, or whatever they think would happen if they actually did flip out. They're always shocked to discover that they can't drive themselves crazy, no matter how hard they try. This insight is always a tremendous relief, and in many cases has ended years of suffering. 8. Survey Technique Researchers often conduct surveys to find out how people feel about different issues. Patients can also do surveys to find out if their negative thoughts and attitudes are realistic. At the start of an inpatient group at the Stanford University Hospital, a severely depressed woman named Diane announced that she'd decided to commit suicide. She explained that this was her eighth hospitalization at Stanford for Rapidly Cycling Bipolar Disorder. She felt extremely depressed, anxious, hopeless, worthless, ashamed, angry and frustrated, and was telling herself: 1. This f___ing disease has ruined my life. 2. I'm hopeless. I'll never get better. 3. I'm a burden to my family and doctors. 4. My parents, husband and children would be better off if I were dead. You're probably aware that Rapidly Cycling Bipolar Disorder is one of the
Chapter 21
603
most severe forms of Manic-Depressive Illness, and it's considered especially difficult to treat. Patients with this disorder cycle in and out of episodes of severe depression or mania several times each year. In spite of her struggles with the disease, Diane was married and had three children. She also had a part-time consulting business designing websites. Diane said that she'd never been exposed to cognitive therapy. She'd received treatment with a wide variety of medications for more than 15 years, but none of them had ever been effective. She said she was eager to receive help, if that were possible. I asked her what thought she'd like to work on first. She selected two: I'm a burden to my family and doctors. My parents, husband and children would be better off if I were dead. We put these thoughts in the middle of a Recovery Circle, and the group selected many methods we could use to challenge them. We tried several techniques that weren't effective, including the four Basic Techniques, the Double Standard Technique, the Downward Arrow, Examine the Evidence, the CostBenefit Analysis, and Let's Define Terms. This only took about 30 minutes. Then we came to the Survey Technique. I said, "Diane, you're claiming that your family would be better off if you were dead. I know this may sound grotesque, but have you asked them if they want you to commit suicide?" Diane conceded that she'd never discussed it with them, but that it seemed true to her. I pointed out that her husband was coming in for a session
Chapter 21
604
later that day, and that it might be worth asking him, because we sometimes jump to conclusions that aren't based on the facts. I said that for the moment, she could ask the other patients in the group if they thought her parents, children and husband would be better off if she took her own life. Diane protested that the people in the group wouldn't be honest with her. I suggested that she could ask several of them, and once they answered her question, we could cross-examine them to find out if they were being honest or simply telling her what she wanted to hear. Diane turned to Martha, the young woman sitting next to her, and said, "Do you think my family would be better off if I committed suicide?" I could see tears streaming down Martha's face. She said: "You've got be crazy, Diane. You don't know what you're talking about. My younger brother committed suicide five years ago. He was in the bedroom right next to mine. I heard a gunshot, and found him with a bullet through his head." Martha sobbed when she described how devastated she and her parents felt. She said it had broken her heart, and she'd never get over it. She said she thought about her little brother many times every day. She added: "Was my little brother a burden? Yes, he was. He was always depressed and angry, and could be difficult to deal with. Sometimes, he was a royal pain. But we loved him, and we wanted him to live and recover. The burden of his depression was nothing compared to the burden of his death."
Chapter 21
605
I asked, "Diane, do you think Martha is telling you the truth, or lying through her teeth?" Diane acknowledged that Martha was clearly speaking the truth. I noticed that Erika, one of the unit nurses who was sitting in on the group, also had tears in her eyes. I said, "Diane, why don't you ask her, too?" Diane turned to Erika and said, "What do you think? Do you think I should commit suicide?" Erika wept and described the suicide of her own son 20 years earlier. She said the unbearable feelings of grief had never diminished, that she thought about her son constantly, and that she'd give anything to have him back. I was about to ask Diane if she believed what Erika was telling her, but I could see that Diane was crying. So I encouraged her to ask all the members of the group, one by one, if they thought her parents, husband, and children would be better off if she were dead. Each person told Diane how moved they were by her story. Many had friends or family members who'd made suicide attempts or died through suicide. They all described feelings of grief, shame and loss. Several thanked Diane, and said she'd made it easier for them to talk about their own feelings. I asked Diane how strongly she now believed the negative thought, "My parents, husband and children would be better off if I were dead." She said it wasn't credible at all, and her belief in it had fallen to 0%. She said she was feeling better, but was still troubled by the thoughts, "This f___ing disease has ruined my life," and "I'm a burden to my family and doctors."
Chapter 21
606
I told Diane that she and I could play the roles of the two voices that were doing battle in her head. She could play the role of her negative thoughts and attack me, using the second person, "You." I'd play the role of her positive thoughts. The dialogue went like this: Negative Thoughts (played by Diane): This f___ing disease has ruined your life! Positive Thoughts (played by David): That sounds like All-or-Nothing Thinking. There's no doubt that this disease has been a royal pain in the ass, but I've still accomplished a great deal in spite of it. For example, I've raised three wonderful children, and I've been a good mother to them. I've also been reasonably successful with my web design business. I feel proud of what I've done. Negative Thoughts (played by Diane): Well, that may be true, but let's face the facts. You've been hospitalized eight times in the past 15 years, and you're really just a burden. You're a burden to your parents, husband, children, and doctors. Positive Thoughts (played by David): You're right. I am a burden! And you know what? I accept that. So I'm just going to be the best little burden I can be! This response brought a smile to Diane's face, and she asked, "Are you saying it's okay to be a burden?" I said, "Absolutely. If that's your fate right now, accept it. It's certainly not your fault. You didn't choose to have this illness. But we're all burdens at times.
Chapter 21
607
That's just part of being human." Diane said that a light bulb suddenly lit up in her brain, and she grasped what I was saying. She'd never considered the idea that she could simply accept the fact that she had an illness, and that it was a burden at times. Paradoxically, she felt relieved. We did a role-reversal, and she was able to defeat me soundly. Then I had the entire group play the role of her negative thoughts, while she played the role of the positive thoughts. We couldn't get to her, no matter what we said. At this point, I asked Diane to complete her Daily Mood Log. She no longer believed any of her negative thoughts, and all the feelings of worthlessness and hopelessness had disappeared. I thought it was interesting that the Bipolar Illness itself was not the real cause of Diane's suffering. Although this disorder is undoubtedly biological in nature, her suffering resulted from her distorted thoughts. When she put the lie to those thoughts, her depression quickly vanished. We often get involved in false dichotomies, and think that there are two kinds of emotional problems—those that are caused by genetic and biological factors, such as a chemical imbalance in the brain, and those that result from psychological factors, such as stress, failure, or rejection. Once you've set up this artificial distinction, it's natural to conclude that the more severe "biological depressions" need to be treated with drugs, while the milder "psychological depressions" may respond to psychotherapy. Nothing could be further from the truth. In the early days of my practice,
Chapter 21
608
before I'd learned about CBT, I ran the lithium clinic at the Philadelphia VA Hospital. I treated the veterans with Bipolar Illness with the very finest psychopharmacologic techniques, but the results were disappointing. It seemed like we had a revolving door, because my patients were constantly going in and out of the hospital. Few of them seemed to be leading normal or fulfilling lives. Later on, I began to integrate CBT techniques into my treatment of bipolar patients. Of course, I continued to prescribe mood stabilizers like lithium in most instances. The CBT was extremely helpful, because nearly all of my bipolar patients had distorted negative thoughts. Most of them based their self-esteem on their achievements, and often had the idea that their achievements had to be spectacular or else they were no good at all. Showing them how to develop unconditional self-esteem made a huge difference in their moods. Although I continued to treat large numbers of patients with Bipolar Illness over the next 20 years, only one patient ever required hospitalization. I'm convinced that the CBT techniques were responsible for the superior results I observed. Keep in mind that these are powerful techniques, and you'll have to use them thoughtfully. For example, when patients think others are angry with them or looking down on them, they may be right. In this case, the Survey Technique might not be indicated. At the very least, you should prepare the patient for negative feedback first. For example, you might train the patient to respond to criticism using the Five Secrets of Effective Communication, in much the same way that I've trained you to respond to angry, critical patients.
Chapter 21
609
In Diane's case, the Survey Technique seemed like a reasonable intervention. I knew that many of the patients had had personal experiences with suicide. I also knew that Diane projected a great deal of warmth and tenderness, so it seemed likely that she'd receive helpful and uplifting feedback from the group. 9. Reattribution When patients are depressed or anxious, they often blame themselves for things they aren't entirely responsible for. This creates profound feelings of guilt, shame, and worthlessness. A Stanford inpatient named Alice used to sob non-stop during cognitive therapy groups. I asked her what she was thinking about when she was sobbing. Alice said that she was thinking about her daughter, who was feeling depressed and struggling with a painful divorce. I asked why her daughter's divorce was causing such intense pain. What was she telling herself about it? Alice had heard that depression may be caused by your genes, and concluded that she was to blame for her daughter's depression. She said she never should have gotten married or had children in the first place, and started trembling and sobbing uncontrollably again. Scientists don't yet know the cause of depression, so we could hardly argue that Alice was responsible for her daughter's depression. And even if genetic factors do play a role, we know that feelings of depression are common among people who are getting divorced, and that most people eventually recover from these feelings. You could argue that the real problem is not the fact that
Chapter 21
610
Alice is to blame, but the fact that she's blaming herself and using up all her energy feeling guilty and miserable, rather than reaching out to her daughter and providing some much-needed TLC. When you use Reattribution, you encourage patients to think about the many factors that might have contributed to the problem. They can ask themselves, "What caused this problem? What did I contribute, and what did others contribute?" They can also focus on learning from the situation and solving the problem rather than ripping themselves to shreds. You may remember Jason, the shy young man we discussed in Chapter 19, who wanted to flirt with the woman checking his groceries. Three of his negative thoughts were: People will think I'm a self-centered jerk if I try to flirt with her. If I tried to flirt with her, I'd probably get shot down. That would show what a loser I am. It's easy to understand why Jason has been stuck. He feels like he's in a can't-win situation. He thinks that if he flirts with her, the other people in line will think he's some kind of a creep. And if he gets shot down, it will prove that he's a loser. So no matter what happens, there will be a steep price to pay. Let's focus on Jason's thought, "That would show what a loser I am." This thought contains a host of distortions, such as All-or-Nothing Thinking, Overgeneralization, Mental Filter, Discounting the Positive, Magnification, Fortune-Telling, Emotional Reasoning, and Labeling. It's also a classic example of Self-Blame, because he's ready to rip himself to shreds if she doesn't respond
Chapter 21
611
positively to his attempts to flirt with her. How would you use Reattribution to help Jason with this thought? Please put your ideas here before you continue reading:
Chapter 21
612
Answer Using Reattribution, Jason could ask himself why an attractive young woman checking groceries might not respond in a friendly way to a fellow who tries to flirt with her, other than the fact that he's some kind of "loser." List some possibilities here before you turn the page:
1. 2. 3. 4. 5.
Chapter 21
613
Answer She might not respond positively to Jason's attempt to flirt with her because: She's married. She has a boyfriend she's committed to. She's gay. She's in a bad mood. Customers try to flirt with her all the time, and she finds it annoying. There's a long line of customers waiting to check their groceries. Flirting with customers is against store policy. She feels shy or insecure. Jason's not her cup of tea. For example, she may prefer guys with a certain look, or men who are older. Jason seems awkward or needy. In addition, his flirting skills may not be up to speed, since he's still inexperienced. If so, he could improve them by doing some Flirting Training, but it certainly wouldn't mean that he was a "loser." Reattribution is often misused. When patients stop blaming themselves, they sometimes start blaming someone else. This is like jumping out of the frying pan into the fire. They may feel less guilty and inadequate, but may now be consumed by feelings of resentment and superiority. The goal of Reattribution is not to rationalize failures or rejections. We do play a role in what happens to us, and our actions sometimes have a huge
Chapter 21
614
impact on others. But personal responsibility is not the same as self-blame. Once patients pinpoint the real cause of a problem, they can try to learn from it and move on, without struggling with such intense feelings of shame, inadequacy, and hopelessness. Logic-Based Techniques 10. Socratic Method You ask patients a series of questions that lead them to the inconsistency or absurdity of their negative thoughts. The goal is not to put patients down, but to free them from suffering. In Feeling Good, I described a severely depressed adolescent named Holly who I treated at my clinic in Philadelphia. She was one of my first CBT patients, and one of the most difficult I've ever seen. Holly had been diagnosed with Borderline Personality Disorder, and had made three nearly successful suicide attempts prior to our first consultation. She was also in the habit of cutting herself with razor blades and broken glass, and had spent most of her senior year of high school on the locked ward of a mental hospital in Boston. She was turbulent and impulsive, and had made little or no progress with her previous therapists. Several of her close relatives had committed suicide. Holly's father was desperate. He'd read about cognitive therapy in the Boston Globe and hoped it might help his daughter. He persuaded the hospital to release Holly for two days on a pass so he could bring her to Philadelphia for a consultation. The purpose of the consultation was to see if CBT might be
Chapter 21
615
indicated for Holly, and whether Holly would have any interest in working with me. I was just learning cognitive therapy, and Holly sounded like she was going to be quite a challenge. To make matters worse, her father was a highprofile malpractice attorney who specialized in suing doctors and mental hospitals. This put me under even more pressure! Shortly after Holly and I sat down to talk, she announced that she intended to commit suicide, and this time she'd make it stick. I asked her why she wanted to kill herself. She defiantly stated that she was a lazy human being, and that she deserved to die. I decided to use the Socratic Method to see if I could make a dent in her negative thinking. I said, "Holly, let's assume that two attorneys are arguing your case in court. You can play the role of the Prosecuting Attorney and argue that Holly deserves to die because she's so lazy. I'll play the role of the Defense Attorney and try to defend Holly. Would you be willing to give it a try?" Holly seemed curious and agreed to play along. Our conversation went like this: David (as Defense Attorney): So, you believe that Holly is guilty and deserves to die? Why is that? Holly (as Prosecuting Attorney): She's lazy. She's never accomplished anything worthwhile. David (as Defense Attorney): I see. So, are you saying that she deserves to die because she's lazy?
Chapter 21
616
Holly (as Prosecuting Attorney): Definitely! David (as Defense Attorney): I have no doubt that Holly can be very lazy at times. How many people in the United States, in your opinion, are lazy? What percentage of the population? Holly (as Prosecuting Attorney): 50%. . . . Wait, that's too high. I'd say it's more like 20%. David (as Defense Attorney): That's a good number. Probably 20% of the people in America are lazy. Since there are approximately 250 million Americans, I guess that would be roughly 50 million lazy people. Do they all deserve to die? Holly thought about it for a moment, and then continued. Holly (as Prosecuting Attorney): Well, no. That doesn't make sense. We're not going to kill off 50 million people just because they're lazy. But Holly is different. She really does deserve to die. David (as Defense Attorney): That could be. You're probably right. But could you explain why? Why does Holly deserve to die? Holly (as Prosecuting Attorney): Well, she gets bitchy and ornery and feels sorry for herself. She feels depressed all the time and makes life miserable for her father. David (as Defense Attorney): That all rings true. I'm sure that Holly can be a real pain in the ass at times. Tell me, is Holly bitchy and ornery all the time, or some of the time? Holly (as Prosecuting Attorney): Well, she's bitchy and ornery some of
Chapter 21
617
the time. Even Holly has a rare good moment. David (as Defense Attorney): That sounds right. Tell me, what percentage of the people in the United States get bitchy and ornery some of the time? Holly (as Prosecuting Attorney): Probably everybody. I'm sure that Mother Teresa gets bitchy, too, but she probably doesn't advertise the fact! David (as Defense Attorney): I agree completely. So are you saying that we all deserve die, since we all get bitchy and ornery at times? Holly reluctantly agreed that what she was saying didn't make sense. She continued to come up with reasons why Holly deserved to die, and I kept challenging her thinking using the Socratic Method. She eventually admitted that her thinking wasn't quite as logical as she'd thought, and that she'd started to feel a bit better while we were talking. I felt like we had some pretty good chemistry, so I asked Holly if she had any interest in moving to Philadelphia for a while so we could work together. She was very receptive to this idea, so her father had her transferred to a mental hospital near my office. I didn't have admitting privileges, because I was just doing outpatient work at the time, so they assigned one of their doctors to her case. However, the staff kindly allowed me to meet with Holly on the benches of the softball stadium behind the hospital for an hour at a time, several times a week. Holly was a handful! She was mistrustful and fought me every step of the
Chapter 21
618
way. But within a few weeks, she'd improved enough to be discharged from the hospital. We continued working together on an outpatient basis, and she decided to enroll in two summer school classes at the University of Pennsylvania. She predicted she'd flunk out, and insisted she was the most stupid student in either class, but ended up getting an A+ in both of them. Based on her outstanding performance, she was accepted into an Ivy League school, even though she was only able to apply in late August, long after they'd closed out their admissions. Holly insisted they'd made a gigantic mistake, and was certain that she'd flunk out. Four years later, she graduated at the top of her class and was accepted to the Harvard Medical School. She currently practices neurosurgery in Boston, and teaches at one of the medical schools there. Not bad for a lazy human being! Dr. Aaron Beck uses the Socratic Method masterfully. My student, Stirling Moorey, was also very gifted with this approach. He'd ask gentle questions that would lead patients to the point where they'd suddenly grasp the illogic behind their feelings of self-doubt. I don't actually use the Socratic Method very often because of my concern that it may sound adversarial and put the patient on the defensive. However, if you have a positive therapeutic alliance, and use the method with respect and compassion, it can be surprisingly effective. 11. Thinking in Shades of Gray Depressed and anxious individuals often view the world in an all-ornothing manner. All-or-Nothing Thinking isn't very realistic, because human beings are neither perfect nor terrible, but somewhere in-between. No one can
Chapter 21
619
be completely successful, and no one is a total failure. No one is absolutely intelligent, attractive, and loving, and no one is totally stupid, ugly, or mean. All-or-Nothing Thinking puts us under a great deal of unnecessary pressure and leads to all kinds of negative feelings, including: Feelings of worthlessness and inferiority. You see yourself as a total loser whenever you fail or make a mistake. Feelings of hopelessness. You feel totally defeated and give up every time you get upset or experience a setback. Performance anxiety. Your tell yourself that your presentation has to perfect, or else it will be no good at all and everyone will see how inept you are. Anger and rage. You may insist that you're innocent and see the person you're not getting along with as an insensitive jerk who's entirely to blame for the problems in the relationship. Thinking in Shades of Gray allows you to view the world more realistically. You ask yourself, "Is there a less extreme way to think about this situation? Was I really a complete failure, or a partial success? Was my performance 0%, 100%, or somewhere in-between?" If your performance wasn't up to par, you can pinpoint your specific shortcomings and work on them. I once gave a half-day workshop with Aaron Beck, M.D. at the Association for the Advancement of Behavior Therapy in Toronto. It was one of my first academic workshops, so I wasn't especially polished or experienced. And although Dr. Beck's contributions to the field of psychiatry have been
Chapter 21
620
considerable, I think he'd be the first to tell you that he's not the world's most charismatic speaker. Consequently, our presentation was decent, but definitely not outstanding. Afterwards, I felt dispirited because we didn't do a stellar job. Dr. Beck noticed I was feeling down, and asked what the problem was. I explained that I thought our presentation was below average. He said, "Well, Dave, we should thank our lucky stars then! Remember, by definition, average is the halfway point. That means that half of our performances have to be below average. It's a good thing we got that one out of the way. We can look forward to one that's above average next time." That was a relief! Remember that Thinking in Shades of Gray may not lead to feelings of illumination or relief. In fact, any technique you try has only a 1 in 10 or a 1 in 15 chance of being effective. If this technique falls flat, you can simply move on to the next technique on your Recovery Circle. Semantic Techniques 12. Semantic Method The Semantic Method is based on the idea that we sometimes use overly colorful language when we're upset. The words we use can have powerful effects on how we feel and behave. When you use the Semantic Method, you simply substitute language that's more objective and less emotionally loaded. If the negative thought is an overt or implied Should Statement, the Semantic Method is often the most effective technique of all.
Chapter 21
621
There are three types of Should Statements: those directed at the self, those directed at other people, and those directed at the world. Shoulds directed against the self lead to depression, guilt, and shame. An example would be, "I shouldn't have made that mistake. What's wrong with me?" Shoulds directed against other people lead to feelings of anger or annoyance. An example would be, "He shouldn't act like such a jerk!" Shoulds directed against the world lead to feelings of frustration. An example would be, "The traffic shouldn't be so darned slow when I'm in a hurry!" If you look up the word, "should," in the dictionary, you'll see that it stems from the Anglo-Saxon word, "scolde." So when we use Should Statements, we're really just scolding ourselves or other people. When you use the Semantic Method, you substitute an "It would be nice if . . ." or "It would be preferable if . . ." expression in place of the Should Statement. For example, instead of telling yourself, "I shouldn't have made that mistake," you can tell yourself, "It would be great if I hadn't made that mistake, but the fact is, I did screw up. Is there something I can learn from this situation?" The goal is not to dispute the Should Statement, but merely to soften it. After you've used the Semantic Method, you wouldn't want to ask the patient, "How much do you now believe that you shouldn't have made that mistake?" That question won't be productive because the patient may still feel like they shouldn't have made the mistake. Instead, I'd ask this type of question: "When you tell yourself it would be preferable if you hadn't made that mistake, does that soften it for you? How much is the negative thought affecting you right
Chapter 21
622
now, between 0% and 100%?" A reduction from 100% to 50% is usually sufficient to bring relief. I don't push for a reduction all the way to 0%, because we're not usually trying to deny the fact that the patient made a mistake. Instead, we're accepting the fact that an error was made and modifying the language the patient uses when thinking about it. The Semantic Method may seem humble, but it's one of the most helpful tools in the CBT arsenal. Some experts believe that Should Statements are the cause of most, if not all, emotional suffering. There's no doubt that Should Statements can trigger feelings of depression, anxiety, inferiority, and shame, as well as anger and interpersonal conflicts. For example, patients who feel depressed often tell themselves that they shouldn't feel the way they do, or that they should be smarter and better than they are. Patients who feel shy typically tell themselves that they shouldn't feel so shy. They may label their feelings as shameful, weird or abnormal. Patients who feel ticked off are usually telling themselves that the other person shouldn't be so stubborn and unreasonable. Should Statements can create emotional problems for therapists as well. If you're stuck with a difficult patient, you may feel anxious and ashamed because you're telling yourself that you should be helping the patient more than you are, and that you should know more than you do. If you feel frustrated and annoyed, you may be telling yourself that your patient shouldn't be so resistant and oppositional. You could also argue that Should Statements are an important trigger for
Chapter 21
623
war and violence. Consider the Israeli-Palestinian conflict. If you listen to statements made by the Israelis, you'll hear that the Palestinians are evil, immoral, and wrong. They'll insist that their own cause is just, and that the Palestinians shouldn't think, act, or feel the way they do. Of course, the Palestinians will say the exact same thing about the Israelis! I'm not claiming that a modest change in rhetoric would resolve that conflict, or any political conflict for that matter. I'm simply saying that the language we use can have a strong impact on how we think, feel, and behave. It's not surprising that mental health professionals have focused so much energy on trying to figure out how to help people let go of Should Statements. From a psychological perspective, the capacity to accept yourself and the world could be viewed as a sign of mental health, maturity and wisdom. From a spiritual perspective, acceptance is often viewed as an important step on the path to enlightenment. However, acceptance can be extremely difficult because Should Statements are so realistic and compelling. The negative feelings they create are addictive, so we get trapped in our misery. Dr. Karen Horney, the popular feminist psychiatrist, wrote about the "tyranny of the shoulds" in the 1950s. Around the same time, Dr. Albert Ellis began to write about the "absolutist demands" that create so much of our suffering. He irreverently calls this the "shouldy" approach to life, and also refers to this tendency as "musterbation." Dr. Ellis is skillful at exposing the grandiosity and absurdity behind our
Chapter 21
624
Should Statements. If you goof up and tell yourself, "Gee, I shouldn't have screwed up," Dr. Ellis might ask, "Where is it written that you shouldn't screw up or make mistakes? Who says? What's the evidence?" Or, if you say, "People shouldn't be such jerks," Dr. Ellis might ask, "Where is it written that people shouldn't be jerks? Why shouldn't they? Why should the world be the way you want it to be?" From a logical perspective, his approach has merit. There are really only three valid uses of the word "should" in the English language: Laws-of-the-universe shoulds. A stone should fall to the earth if you drop it because of the force of gravity. Moral shoulds. You shouldn't cheat on your spouse or murder people because it's immoral. Legal shoulds. You shouldn't drive 90 MPH because it's against the law. Most other uses of the word, "should," tend to be irrational. If you hook your golf shot into the pond, you might think, "I shouldn't have screwed up like that!" Ask yourself what kind of Should Statement this is. Is it a laws-of-theuniverse should, a moral should, or a legal should? You're certainly not violating any of the laws of physics, so it's not a "laws-of-the-universe should." Hitting a bad golf shot is not a violation of the Ten Commandments, either! And it's obviously not illegal. So this isn't a valid use of the word, "should." When you use a Should Statement in a situation like this, you create a lot of needless frustration for yourself. It's a little like insisting that it "shouldn't" rain today because you planned a picnic. Why shouldn't it?
Chapter 21
625
The potential danger with Dr. Ellis' approach is that it may sound adversarial and put the patient on the defensive. In contrast, when you use the Semantic Method, the patient is more likely to feel like you're working together. The Semantic Method is also a good technique to try when the negative thought involves Labeling or Magnification. For example, a patient who's procrastinating on studying, asking someone for a date, or exercising may tell himself, "I just can't seem to do it," or "I just can't seem to get started," or "Why am I such a procrastinator?" This makes it sound like he's paralyzed, or like there's some invisible force holding him back. It's a lot like self-hypnosis. When you hear a suggestion over and over, you'll start to believe it. Using the Semantic Method, he could tell himself that he really doesn't want to exercise, study or risk rejection because it's so anxiety-provoking. He'll still have a choice to make, but he'll no longer feel like a victim of mysterious forces beyond his control. 13. Let's Define Terms Like the Semantic Method, Let's Define Terms focuses on language and has an interesting philosophical component. It's based on the idea that there's really no such thing as a "loser," a "jerk," or a "failure." And there's no such thing as a person who's "worthless," "inferior," "unlovable," or "hopelessly depressed." But when our patients feel depressed, these labels seem absolutely true and can inflict tremendous emotional damage. When you use Let's Define Terms, ask yourself what these terms really mean. When you try to define these labels, you'll discover one of four things:
Chapter 21
626
The definition applies to all human beings. The definition applies to no human beings. The definition is meaningless. The definition doesn't apply to you. Regardless of which category your definition falls into, you won't need to be concerned about the label any more. This idea is consistent with Buddhist philosophy. The Buddhists teach us that our suffering results more from our judgments about reality than from what's really happening. Furthermore, the judgments we make about reality are illusions—pie-in-the-sky abstractions that simply aren't grounded in reality. Why is this? For one thing, it's illogical to base your entire identity on your deficiencies or problems. In fact, we're all made up of an incredible variety of thoughts, feelings, behaviors, and traits. Some of our actions and traits are positive and others are negative. Most are somewhere in-between. You do yourself a huge disservice when you label yourself because your entire sense of identity will suddenly be based on one small part of a much larger picture. Would you think of yourself as "a breather" simply because you breathe? Can you imagine what you might say if you were introducing yourself to someone at a party? You could say: You: Hi, I'm Dave. Party Guest: Glad to meet you, Dave. I'm Paul. What do you do? You: I'm a breather. How about you, Paul? What do you do? Party Guest: I'm an accountant. I've never met a breather before. What
Chapter 21
627
does a breather do, really? You: Oh, I breathe a great deal. In and out, in and out. Party Guest: Don't most people breathe? You: Yes, you hit the nail on the head, Paul. Most people are breathers, although they're not always aware of it. They typically breathe all day long, unless, of course, they're holding their breath. At those moments, you could think of them as temporary non-breathers. Party Guest: Well, Dave, that's very interesting. In fact, I'm speechless. Listen, I just spotted someone on the other side of the room I have to go talk to. Breathe on, dude! Of course, when you view Labeling like that, it's clearly ridiculous. But when our patients write themselves off as "worthless" or "hopeless," these labels don't seem ridiculous. They seem real. Patients feel certain that they've glimpsed some awful truth about themselves and suffer intensely as a result. You can ask patients to define the label they're using. For example, what's the definition of a "worthless person"? You can encourage the patient to challenge their definition and show that it doesn't make sense. Let's say the patient defines a "worthless person" as someone who's worse than everyone else. You could ask the patient to clarify this. Do they mean worse than all human beings in every way, or worse than some human beings in some ways? The patient might say, "Worse than everyone in every way." Then you can point out that according to this definition, no one's worthless, because no one is worse than all human beings in every way. There are more than six billion human
Chapter 21
628
beings on the earth, and you can always find someone who's not as good as you at something! For example, no matter how bad your spelling or singing is, you can find someone who's even worse. Once the patient sees that the definition isn't valid, you can encourage them to try again, and to define a "worthless" person in a different way. The patient might say, "Well, what I really meant is that a worthless person is someone who's worse than some people in some ways." According to this definition, we're all "worthless," because there will always be people who are way better than us at all kinds of things. In that case, being "worthless" is the same as being "human," so it's not something we'd have to worry about. No matter how the patient defines this term, the definition will always fall apart. Suppose the patient says, "When I say I'm worthless, I really mean that: "I've made mistakes." "I haven't fulfilled all my dreams in life." "I've never accomplished anything truly remarkable. I'm just average." How would you challenge these definitions? Put your ideas here:
Chapter 21
629
Answer If a "worthless" person is someone who's made mistakes, then we're all worthless, because we all make mistakes every day. Sometimes we make big mistakes, and sometimes we make little mistakes. Most of our mistakes are just average. Even the world's greatest physicists and mathematicians make mistakes. The world's top tennis players make lots of unforced errors in every match, and they all lose many matches. If you say a worthless person is someone who hasn't fulfilled all of his or her dreams in life, then we're all worthless. No one ever fulfills all their dreams in life! What child hasn't dreamed of being a star athlete, a world-famous actor, a rock star, or the President? Only a handful of people can ever achieve these kinds of dreams, and we've all had many other kinds of dreams we can never fulfill. If you say a "worthless" person is someone who's never accomplished anything "truly remarkable," then practically everybody's worthless. Only a tiny handful of people can ever win a Nobel Prize or invent a light bulb. Are the rest of us "worthless"? According to this definition, 99.99% of the human race are worthless, so how bad could it be? No matter how you define a "worthless" person, your definition won't hold water. Do you know why these definitions of a "worthless" human being always fall apart? Is this just a trick with words? It's because there is no such thing as a worthless human being. There's no such thing as a "worthwhile" human being, either. All of us are a mixture of
Chapter 21
630
good and bad. The "best" people have lots of flaws and shortcomings, and the "worst" people have many strengths and positive qualities. A Chicago industrialist named Zeke had suffered from years of depression and anxiety. In spite of extensive treatment from many different psychiatrists, he'd made very little progress. After several months of therapy with me, Zeke began to experience periods of improvement lasting as long as several weeks. These periods were typically followed by painful relapses. During each relapse, Zeke would start to feel anxious and depressed again. He'd tell himself that he was "hopelessly sick" and not getting anywhere. I asked Zeke to write down his definition of a "hopelessly sick" person. I told him to examine each definition carefully and write a brief rebuttal. Here's an excerpt from his assignment: Definition: "Hopelessly sick" means a non-changing degree of depression and anxiety. Rebuttal: Then I can't be "hopelessly sick" because my depression and anxiety constantly fluctuate. Definition: "Hopelessly sick" means that I have constant thoughts about suicide. Rebuttal: The greatest amount of time I think about self-destruction is five minutes per day, and this only occurs during my most depressed phases. So it follows that I don't "constantly" have such thoughts. When my mood improves, the suicidal thoughts always disappear.
Chapter 21
631
Definition: A "hopelessly sick" person is one who commits suicide or makes a suicide attempt. Rebuttal: I often fantasize about suicide when I'm depressed, but I've never attempted suicide, or even planned a suicide attempt. Furthermore, a suicide attempt wouldn't prove that you were "hopelessly sick." It would only show that you thought you were hopeless. Most people who make suicide attempts eventually get better. This proves that their feelings of hopelessness were illusory. Definition: "Hopelessly sick" means that I can't get better. Rebuttal: What's the definition of "getting better"? Definition: "Getting better" means feeling happier and less depressed. Rebuttal: Right now, I feel 50% anxious and depressed and only 10% happy. If at any time in the future I feel happier and less depressed, I will be feeling better. The chance of this happening is good, since it happens almost every day. In fact, right now I'm feeling slightly better than I did this morning. This shows that I've already gotten better. Definition: Then "hopeless" must be a sliding scale. The more depressed and anxious you are, the more hopeless you become. Since I'm quite depressed and anxious at times, it follows that I must be quite hopeless at those times. Rebuttal: This is more Emotional Reasoning. If I'm feeling very depressed, I'll probably feel hopeless, but it doesn't mean that I really am hopeless. Severely depressed people can and do improve. When I feel
Chapter 21
632
better, I don't feel hopeless any more. No matter how he defined "hopelessly sick," Zeke discovered that he could always come up with an effective rebuttal. Eventually, it dawned on me that Zeke's feelings of hopelessness were usually a smokescreen for some other problem he was avoiding. For example, if he was upset with his wife or a colleague, he'd typically sweep his feelings under the rug. Then he'd start ruminating that he was "hopelessly sick." When he talked things over with the person he was feeling upset with, he usually started feeling better right away. This is called the Hidden Emotion Technique. It's frequently helpful for anxiety, but it's occasionally helpful for depressed patients as well. For some patients, Let's Define Terms may seem like an irrelevant word game that doesn't touch the overwhelming desperation and worthlessness they feel inside. It may seem too argumentative or lacking in compassion, much like two attorneys arguing in court. I certainly wouldn't want any patient to feel belittled or put down. By the same token, this method is philosophically intriguing, and for some patients, it can be quite helpful. 14. Be Specific This technique is geared towards Overgeneralization. When patients are feeling depressed, anxious or angry, they often generalize from a specific failure or problem to their entire selves. They may also project the failure into the future and see it as a never-ending pattern of defeat and deprivation. When you use Be Specific, you encourage patients to focus on real problems and resist making vague generalizations about their worth as human beings.
Chapter 21
633
This technique is based on three Buddhist principles: 1. All human beings have many flaws and shortcomings. We all fail at lots of things all the time. In fact, there's probably nothing about us that couldn't be improved. 2. Specific failures and shortcomings don't cause our suffering. Instead, our suffering results from our insistence that we shouldn't have failed, and that we should be better than we are. 3. When you accept your shortcomings with a sense of inner peace and humor, your suffering will disappear, and you'll experience enlightenment. A carpenter named Francisco was depressed about a back injury he'd sustained at work. He was on disability because he couldn't even bend over. Francisco described looking out his back window and noticing that his lawn was dry and overgrown with weeds. He told himself, "I can't even fix the sprinkler system or weed my own back yard. I'm worthless." Francisco was hospitalized at Stanford following a nearly successful suicide attempt. Francisco's negative feelings resulted from his conviction that he was worthless. This is a classic example of Overgeneralization. Francisco was generalizing from his back injury to his worth as a human being. He was telling himself, "Because I can't work and support my family, it means that I'm worthless and deserve to die." Francisco's back injury didn't actually cause his feelings of worthlessness. His distorted thoughts were the real enemy. It's true that he can't pull the weeds or support himself by doing carpentry work right now. It's true that he'll have to
Chapter 21
634
rely on disability payments to support his family for a while. But how does this make him a worthless human being? The act of transforming vague, global self-criticisms into specific deficiencies can be liberating. Patients often discover that there's no self-criticism they need to fear. Another way to use Be Specific is to imagine that a critic is attacking you and saying all the worst imaginable things about you. You can respond by asking the imaginary critic to make each criticism specific. Then you can agree with the specific criticism while ignoring the Overgeneralization. I like to bring this method to life with the Zigzag Technique. Divide a piece of paper into two columns labeled "Self-Criticisms" and "Self-Defense," as illustrated on page 635. In the Self-Criticisms column, write down an imaginary, sweeping criticism of yourself. In the Self-Defense column, see if you can defeat the criticism by finding some truth in it. Then write a new criticism, followed by a new defense. The idea is to convert global, sweeping criticisms into specific problems you can either solve or accept. This is a variation of a role-playing technique, except that patients can do it on their own. Of course, you'll have to help patients with it at first, because their self-criticisms will seem so realistic and overwhelming.
Chapter 21
635
Zigzag Technique Self-Criticisms
Self-Defense
Burns, you're basically a worthless human being.
That could be true. I do have lots of shortcomings. But could you be a bit more specific?
Honestly, I'd hardly know where to begin.
Gosh, I hate to burden you, because I know how busy and important you are. Perhaps you could mention just one or two of the deficiencies you're thinking about.
Okay. Your writing is boring.
Boy, that's so true. Sometimes my writing gets awfully long-winded, boring and pompous, especially if I've been drinking too much coffee! I'd love to hear any criticisms you might have of anything I'm writing, including this chapter. Does it seem boring? Good criticism is like money in the bank, because it helps me improve my writing.
We could sit around talking about all kinds of problems with your writing, but your problems go far deeper than that. You're really a self-centered person.
I couldn't agree more. Sometimes I can be really self-centered. In fact, as I've gotten older, I think I've actually gotten even more preoccupied with my own projects and activities. Is that what you mean?
What I mean is that you're fat. You need to lose weight.
Agreed. But what happened to the self-centered part?
You're undisciplined. You tell yourself you're going to diet and exercise, but then you skip your running and eat too much.
Very true. I have to plead guilty as accused!
You think you're so great. Lots of people are way more successful than you are.
You can say that again! There are so many successful people in the world that it boggles my mind!
Chapter 21
636
Quantitative Techniques 15. Self-Monitoring Patients can keep track of a repetitious negative thought or an anxietyproducing fantasy by counting it each time it happens. An easy way to do this is to keep a 3x5 card in your wallet or pocket, and put a tick mark on the card each time you have a negative thought. At the end of the day, you can record the total for that day on your calendar. Alternatively, you can use a wrist-counter like the ones golfers wear to keep track of their scores. They look like inexpensive watches, and are available at most golf shops or online for less than $10. Each time you have a negative thought, you can simply click the counter and the number on the dial will increase by one. At the end of the day, you can record the total and reset the counter to zero. During the third week of Self-Monitoring, the upsetting thoughts may diminish or even disappear. A medical student named Sam was intensely jealous after his girlfriend broke up with him to date another student in his class. Sam had disturbing fantasies of his ex-girlfriend having sex with her new boyfriend, and often drove by her apartment to see if his car was parked outside. Sam agreed to stop driving by her apartment, no matter how anxious or jealous he felt. This is Response Prevention, one of the Classical Exposure Techniques. In addition, he agreed to count the sexual fantasies on a wrist counter for several weeks. Initially, Sam had over 100 fantasies every day. For the next two weeks, he had an average of 80 – 100 a day. During the third week,
Chapter 21
637
the thoughts about his ex-girlfriend suddenly started to fall below 50 per day. After a few more days, they disappeared completely. You can also use Self-Monitoring to help patients with anxiety disorders. An anxious ophthalmologist named Jose obsessed about "floaters" in his eyes. Each time he saw a floater, he'd panic and tell himself, "I might be going blind." Then he'd give himself an eye exam and feel temporarily relieved. But soon he'd see another floater and get the urge to check his eyes again. He was checking his vision up to 20 times a day, and it was using up all his free time! A "floater" is just something that floats across your visual field. You might have had floaters from time to time. They're perfectly normal. In rare cases, floaters might indicate retinal degeneration, particularly if someone has childhood-onset diabetes. In these cases, emergency laser surgery can be helpful. But Jose didn't have diabetes and there was no reason for him to suspect he was going blind. Jose was suffering from OCD. The thought, "What if I'm going blind?" is his obsession, and the repetitious eye-checking is his compulsive ritual. I did a Cost-Benefit Analysis (CBA) to assess Jose's motivation. I asked him to list the advantages and disadvantages of checking his vision every time he saw a floater. As you can see on page 638, Jose decided the disadvantages of checking his vision outweighed the advantages by a 60-40 margin. To be sure, I used a technique called the Acid Test. I said, "Jose, let's pretend there's a little button here on my desk. If you push that button, all of your worrying about floaters would suddenly disappear. Would you push that button?"
Chapter 21
638
Jose's Cost-Benefit Analysis* List the attitude, feeling or habit you want to change: Checking my vision each day. Advantages of Checking My Vision
Disadvantages of Checking My Vision
1. It's reassuring.
1. The odds of a real problem are low.
2. I can catch any problem early.
2. The constant checking is unnecessary.
3. I can get help if I need it.
3. The anxiety is ruining my life.
40
60
"Of course, doctor," he replied. I said, "But then, if you get a floater, and there's some problem with your eyes, you won't check your vision. Then you might go blind. Are you sure you want to push that button?" Jose insisted that he'd still push the button because the constant eye checking was a total waste of time. He said that if he really had a serious eye problem, there'd be other symptoms as well, such as blurred vision, so there was no rational reason to keep checking his eyes.
* Copyright
2004 by David D. Burns, M.D.
Chapter 21
639
Next, I used Response Prevention. I asked Jose if he'd agree to stop checking his vision for several weeks, no matter how nervous he got. Instead, every time he had the thought, "I'm going blind," he could count it on a wrist counter and carry on with his work. Jose monitored his negative thoughts about his vision every day for the next 22 days. As you can see below, Jose had over 60 thoughts the first day, and reached a plateau of around 90 thoughts per day by the third day. On day 17, his thoughts about his vision suddenly dropped below 60. The negative thoughts dropped even further on day 18, and on day 21, he had only 3 thoughts about his vision. On day 22, his thoughts about his vision disappeared entirely.
Jose's Self-Monitoring Chart
Thoughts
100 80 60 40 20 0 1
2
3
4
5
6
16 17 18 19 20 21 22
Days Self-Monitoring can also be helpful for patients suffering from depression. One of my post-doctoral psychology students was treating a carpenter named Phil who became depressed following a stroke. After the stroke, Phil experienced
Chapter 21
640
spells of uncontrollable crying and laughing that were triggered by the slightest stimuli. Glimpsing a sunset, a baby, or even a flower might evoke bouts of sobbing, and even the blandest joke evoked paroxysms of laughter. This pattern of extreme emotional instability is routinely seen after certain types of strokes, and it results from brain damage. The upsetting event on Phil's Daily Mood Log was playing poker with his buddies. Poker was one of the things he enjoyed most in life, but there was a slight problem. If he got a good hand, he'd start cackling uncontrollably, and if he got a bad hand, he'd start sobbing. This made it awfully tough for him to bluff! Phil felt ashamed, depressed, embarrassed, humiliated, discouraged, and frustrated. One of his negative thoughts was, "I just can't control myself." This is a classic example of All-or-Nothing Thinking. Phil's therapist encouraged him to buy a stopwatch and keep it in his pocket. Each time he sensed he was about to burst into tears or laughter, he could hit the start button on the stopwatch. Then when he began to laugh or cry, he could hit the button again so he could see how many seconds had elapsed. He recorded his times in a notebook. That way, he could keep track of how long he could delay each emotional outburst, in much the same way that an athlete times how fast she or he can run the 100-meter dash. Even though Phil couldn't control his emotions completely, he could probably learn to control them a little bit, and with practice and training, his self-control might improve. This plan appealed to Phil, since he'd been active in sports throughout his life. His said that the emotional problem now seemed more like an athletic
Chapter 21
641
challenge and he was excited to work on it. At first, he was only able to postpone the laughing or crying for a few seconds. However, toward the end of the first week, he found he could sometimes postpone the emotional outbursts for 15 or 20 seconds. By the end of the second week, he could postpone them for more than a minute. By the end of the third week, he could postpone them indefinitely. Phil's depression was clearly the result of brain damage from his stroke, and yet, a psychological intervention was sufficient for effective treatment. Although this may seem surprising, recent brain imaging studies have confirmed that CBT can cause striking chemical changes in the brain that are similar to the changes that occur in patients who respond to psychopharmacologic treatments. I don't know why Self-Monitoring works. It may be a little like mindfulness meditation. When people meditate, they begin to notice that thoughts constantly flow across their minds. Once they notice a thought, they can learn to let go of it instead of dwelling on it or reacting to it. Similarly, when patients use Self-Monitoring, their only job is to notice the negative thought and count it. Then they can let go of it and carry on with whatever they were doing when the thought popped into their minds. They don't need to dwell on the thought, fight with it, or obsess about it. The beauty of Self-Monitoring is that it's easy, and for certain types of problems, it can be quite effective. In the three examples I provided, we used Self-Monitoring to target specific types of negative thoughts. However, patients can also track negative thoughts in general.
Chapter 21
642
Notice that I didn't blindly attack these patients with Self-Monitoring. Like any technique, Self-Monitoring has to be applied in the context of a collaborative therapeutic relationship, and the patient has to be motivated to change. Remember that this technique won't always work. Most patients will require more sophisticated techniques. It's often worth a try, however, and it can occasionally yield big dividends. 16. Negative Practice / Worry Breaks Many patients seem to have an overwhelming urge to beat up on themselves. This tendency can be very pronounced in patients suffering from Borderline Personality Disorder, but it's not limited to that diagnosis. In fact, most depressed or anxious patients rip themselves to shreds mercilessly. Often, they justify the negative thinking. For example, patients who feel guilty or ashamed may think that they deserve to suffer. Patients who feel inferior or worthless may think that their self-abuse is justified and realistic. Anxious patients may think that the constant worrying will magically protect them or their loved ones from danger, or prevent them from failing at some important task. Sometimes, the struggle to control the negative thoughts will make them more intense. In these cases, Negative Practice or Worry Breaks may help. These are paradoxical techniques. Instead of fighting the negative thoughts, patients can give in to them in a limited, structured way. They can schedule certain periods of time each day to worry or beat up on themselves intentionally. Although these two techniques are similar, Negative Practice is geared more for depression, and Worry Breaks are primarily designed to combat compulsive
Chapter 21
643
worrying. For example, if a depressed patient believes that her feelings of guilt and shame are necessary, you could ask her how much guilt and shame would be appropriate. How many minutes of suffering each day would be optimal? Is she determined to feel miserable 100% of the time, or would a lesser sentence be acceptable? If she insists that she's determined to feel miserable 100% of the time, then you may not have a meaningful therapeutic agenda. Let's assume that she's not quite that oppositional, and agrees that the constant misery isn't doing her any good. Still, she feels the urge to beat up on herself. Ask how many minutes of misery would be enough. For example, she might be willing to schedule three five-minute Negative Practice sessions each day. During these sessions, she can beat up on herself all she wants, and make herself feel as guilty and worthless as possible, without challenging any of her self-critical thoughts. Paradoxically, this often takes the sting out of the thoughts. It changes the context, so the negative thoughts lose their power. I once treated a depressed physician named Raphael who barraged himself with negative thoughts while making rounds at the hospital. When he was examining his patients, he'd tell himself: I'm a lousy doctor. I probably didn't listen to her heart properly. What's wrong with me? Other doctors have a better bedside manner. I'm not very warm or friendly. My personal life is in shambles as well.
Chapter 21
644
While there was a grain of truth in some of Raphael's self-criticisms, they weren't very realistic. He was actually a competent and dedicated physician who was held in high esteem by his colleagues at the hospital. Furthermore, even if his medical skills weren't up to par—which was not the case—it still wouldn't be productive for him to beat up on himself relentlessly, because the feelings of guilt, anxiety and worthlessness would simply interfere with his capacity to concentrate and do effective, compassionate medical work. I suggested that Raphael could jot down his negative thoughts in a small notebook when they popped into his head during rounds. Then he could transfer them to a Daily Mood Log and try to challenge them later on. Raphael had a better idea. He purchased a tiny Dictaphone and kept it in the pocket of the white lab jacket he wore at the hospital. When he was walking from room to room during rounds, he pulled out his Dictaphone and recorded his negative thoughts in a hushed voice. Then, when he was with his next patient, he tried to focus on that person's medical problems, and reminded himself that he could indulge in the negative thoughts as soon as he'd finished examining the patient. He'd dictate comments like this: "I'm doing a lousy job with that patient. What if she has a liver problem I completely overlooked? Any other doctor could do a better job. She seemed upset about the pain in her abdomen, but I barely listened to what she was trying to tell me. What if she has peritonitis and goes into shock? What if she dies? What if I get sued and lose my license?"
Chapter 21
645
At the end of rounds, Raphael went to his office and rewound the tape. Then he forced himself to listen to all of his negative thoughts. At first, the thoughts were extremely upsetting, because they sounded valid. After several days, the thoughts began to lose credibility, and by the end of the first week, they were starting to sound ludicrous. He reminded himself that he had many grateful patients, and that his colleagues often asked him for consultations when they were perplexed about challenging diagnostic problems. Furthermore, he'd never lost a patient due to any medical error, and had never been sued for malpractice. Raphael experienced a boost in self-esteem, and his negative thoughts soon disappeared completely. A University of Pennsylvania freshman named Nate came to see me for help with his test anxiety. Nate was having difficulty studying for finals because his mind was flooded with frightening thoughts every time he tried to review his notes. He'd tell himself: I'm probably studying all the wrong things. I can't remember anything. What's wrong with me? Everyone else seems to understand this material. I'm out of my league. My mind will go blank when I see the test. I just know I'm going to blow it and flunk this course. Nate agreed to schedule a one-minute Worry Break twice every hour when he was studying. During each Worry Break, he'd put down his books and verbalize all his negative thoughts without trying to challenge them. At the end of
Chapter 21
646
the Worry Break, he'd resume studying. Nate said that this made it easier to study because he knew he could indulge in his negative thoughts at his next Worry Break. The negative thoughts quickly began to lose their hold on him. He felt more relaxed and experienced an increased capacity to concentrate. He passed his finals with flying colors two weeks later. There are no hard and fast rules about which approach will work best. Some people like to write down their thoughts, while others prefer to verbalize them out loud or dictate them into a tape recorder so they can listen to them. Patients can use any schedule that appeals to them, and can modify it as they go along. This technique may make patients feel worse at first. Make sure they understand this and accept the fact that it may take some time. I would definitely avoid using this technique with patients who feel suicidal, since it might trigger a suicide attempt. Occasionally, we all get frustrated with patients who seem determined to obsess and beat up on themselves. If you're not consciously aware of how annoyed you feel, you might act out these feelings and use these techniques in a passive-aggressive way, to show patients how ridiculous and self-defeating their behavior is. Of course, this will backfire. If you keep these potential hazards in mind, Negative Practice can be a unique and paradoxical therapeutic tool. When patients surrender to the thoughts they've been struggling so hard to control, the thoughts will often lose their
Chapter 21
647
power. Humor-Based Techniques 17. Paradoxical Magnification Paradoxical Magnification is a Humor-Based Technique. Instead of trying to dispute your negative thoughts, you exaggerate them and make them as extreme as possible. Paradoxically, this can sometimes provide objectivity and relief. Paradoxical Magnification is definitely not for everybody, and I only use it occasionally. It's most likely to be helpful when the patient is suffering from performance anxiety. Usually, the negative thoughts will contain these kinds of distortions: Fortune-Telling. You predict that things will turn out terribly. For example, if you have to give a talk in front of your colleagues, you may tell yourself that you're going to screw up and make a complete fool of yourself. Mind-Reading. You tell yourself that everyone will look down on you once they find out about your vulnerabilities and flaws. Magnification and Minimization. You exaggerate how terrible things are, or shrink the importance of your accomplishments. Self-Blame. You rip yourself to shreds because of your shortcomings. A young woman named Sonia felt intensely nervous when she was preparing for her brown belt examination in Aikido, a Japanese martial art. She was telling herself, "I'll really screw up on my test on Friday." Rationally, Sonia knew this was unlikely, since she'd been practicing diligently for many years and
Chapter 21
648
had done well on all her previous Aikido tests. Nevertheless, she couldn't stop obsessing about the test. Her worrying was doubly frustrating because, according to the underlying philosophy of Aikido, you're supposed to let go of your tension and go with the flow. So Sonia felt like she was failing on two levels. She was worrying about screwing up on the test and criticizing herself because she thought she shouldn't be worrying so much. It's always difficult to predict what method will be helpful for a particular person, and there are lots of techniques we could have tried. On a hunch, I suggested Paradoxical Magnification. Instead of struggling to relax, Sonia could do the exact opposite and spend several minutes a day telling herself things like this: "I probably will screw up on my test, but it will be far worse than just that. I'll probably be the worst person in the class, and perhaps in the entire country as well. I'll lose my coordination and flail my arms and legs in a clumsy, foolish fashion, while my face turns beet red from nervousness. Then everyone will snicker and scorn me. They'll not only see that my technique stinks, but that I'm a total emotional wreck as well. No one will want to hang out with me any more. I'll be shunned. Word will spread throughout San Francisco, and pretty soon everyone will be talking about how dreadful I am, not only at Aikido, but at life in general." Sonia thought the fantasy was funny. After practicing this technique at home, her fears began to seem absurd. She decided to set her pride aside and
Chapter 21
649
accept the fact that she'd make some mistakes, no matter how hard she prepared. She realized she could view the experience as another opportunity to practice and learn. This relieved most of the tension that was plaguing her. She later reported that the test turned out to be a lot of fun, and she passed with high marks and lots of praise from the black belts who were judging her performance. You can use this technique in many different ways. I recently did a live demonstration with a woman named Rebecca during an anxiety disorders workshop I was conducting for mental health professionals in Los Angeles. Rebecca volunteered to work with me on her public speaking anxiety so the audience could observe a live therapy session and get a feel for how CBT really worked. Rebecca felt intensely anxious and insecure at the start of the demonstration, because we were working on a stage in front of 200 people. We filled out a Daily Mood Log together so I could find out what she was telling herself. Her most upsetting negative thought was, "The people in the audience will see how nervous and insecure I feel." We put this thought in the middle of a Recovery Circle, and selected many techniques we could use to challenge it, including Empathy, Identify the Distortions, Flooding, Examine the Evidence, the Double Standard Technique, the Cost-Benefit Analysis, and the What-If Technique, to name just a few. I wanted to see what was at the bottom of Rebecca's fears, so I decided to use the What-If Technique first. I said, "Let's assume that all the people in the audience really can see how nervous and insecure you feel. What then? What
Chapter 21
650
are you the most afraid of?" She said, "Then they'll think I'm weak and neurotic." I said, "Let's assume that happened? The audience decides you're weak and neurotic. What then?" Rebecca replied, "Then they'll think I suck." She said this thought was terrifying. Rebecca was likeable and seemed to trust me, and I was fairly certain that the people in the audience felt a bond with her as well. I had the hunch that she might be willing to do something radical to face her fears. On impulse, I suggested that if was feeling really courageous, she could stand in front of the group, and ask them all to stand up and shout, "You suck!" at the top of their lungs. Of course, this is another way to do Paradoxical Magnification. Rebecca said she wanted to give it a try. She walked off the stage, stood directly in front of the audience, and asked everyone to stand up. Then she asked them to shout, "You suck!" on the count of three. The group went for it and Rebecca started giggling. The people in the audience were laughing as well, and she immediately sensed the absurdity of her fears. The worst had happened, and she'd survived. She came back up to the stage, and said she was on a tremendous high. She said it was one of the most cathartic experiences of her life, and that her anxiety had disappeared completely. Following the demonstration, there was an overwhelming outpouring of warmth and support from the group. Many people told Rebecca how much they
Chapter 21
651
admired her courage, and said she was the star of the show. Rebecca was blown away and told me the experience had been life-changing. If you want to try Paradoxical Magnification, let your patients know that the goal is not to make them feel worse, but to help them see the absurdity in their fears. Humor can be very healing, but it's tricky. It's most likely to be effective if the patient likes and trusts you, and has a sense of humor as well. Paradoxical Magnification may fail with patients who feel extremely vulnerable. They might think that you're making fun of them. You should also avoid humor when patients feel angry, since your attempts at humor will usually appear defensive or disrespectful. If this or any technique backfires, you can empathize, provide support, and apologize for being insensitive. When the patient feels better, and you've reestablished a positive therapeutic alliance, you can try the next technique on your Recovery Circle. 18. Shame-Attacking Exercises Shy individuals usually have an intense fear of looking foolish in front of other people. They struggle to control their anxiety and look normal because they're convinced that everyone will look down on them if they appear nervous or do anything that seems odd or inappropriate. Of course, the more you struggle to control your anxiety, the more anxious and insecure you become. Shame-Attacking Exercises are a potent antidote to these kinds of fears. Instead of trying to act normal, you do something foolish in public on purpose. For example, you could stand up and loudly call out the name of the street at each stop while riding on the bus or subway. Or, you could go into a crowded
Chapter 21
652
department store and loudly announce the time. For example, you could say, "The current time is 2:45 PM, Central Standard Time." When people turn to look at you, you could announce the time once again. You'll usually discover that the world doesn't come to an end after all. This can be a liberating discovery. I believe that Shame-Attacking Exercises were invented by Dr. Albert Ellis. Dr Ellis has an annual contest and gives a prize to the therapist who has done the most creative and outrageous Shame-Attacking Exercise that year. Recently, a psychologist from Portland took top honors. He went into a busy drugstore and asked the pharmacist, in a loud voice, "Can I buy four-dozen condoms, please?" The pharmacist nodded. Then the psychologist forced himself to ask, in an equally loud voice, "Do you have the little, teeny-weenie size?" Fortunately, a Shame-Attacking Exercise doesn't have to be quite that extreme to be effective! I first learned about Shame-Attacking Exercises following a workshop I presented for Dr. Ellis' Institute for Rational-Emotive Therapy in New York. After my presentation, I went to dinner at a Chinese restaurant with several of Dr. Ellis' students and colleagues. It was a popular restaurant, and we had to wait in a long line to be seated. The line actually curled around inside the restaurant, so we were standing near people who were already eating. I told one of Dr. Ellis' colleagues that I'd heard of Shame-Attacking Exercises, but didn't know exactly how they worked. He explained that you intentionally do something bizarre in public so you can get over the fear of making a fool of yourself. He said that the only way to really understand how Shame-Attacking Exercises worked was to try one yourself. Apparently, all the
Chapter 21
653
trainees at Dr. Ellis' institute had to do Shame-Attacking Exercises as part of their training. He suggested that I could do one right now, while we were waiting in line. I suddenly felt uneasy, and asked what he had in mind. He said I could ask the people at one of the tables if I could sample their food. This sounded totally bizarre, and a wave of panic gripped my heart. I kicked myself for asking about Shame-Attacking Exercises! I didn't want to do it, but felt enormous social pressure from the group I was with. They all insisted they'd done Shame-Attacking Exercises, and that I should try one, too. I reluctantly walked over to a table where six people were eating. Their table was covered with a variety of tasty-looking dishes. I commented on how good the food looked. They said it was terrific, and told me that they'd been coming to this restaurant for years. Then came the hard part! I pointed at one of the dishes and said, "I know this sounds incredibly eccentric, but I was wondering what that dish tastes like. I don't suppose you'd let me taste it, would you?" They didn't seem at all perturbed and said, "Sure! Here, have some." Much to my surprise, they offered me a fork and encouraged me to taste the dish. I said it was fabulous, and they encouraged me to taste several other dishes as well. Then the people from Ellis' institute suddenly appeared and asked if they could sample the food, too. The people at the table started giving everybody samples with great enthusiasm! Soon, we were all giggling and having a good time. It was the highlight of my trip to New York.
Chapter 21
654
This experience taught me that you don't always have to be so rigid and take yourself so seriously. Most people appreciate a little good-willed humor or eccentricity. People are bored and looking for something to spice up their day. If you act a bit goofy, in a good-natured way, most people will get a kick out of it. If you're naturally outgoing, this may seem trivial or obvious, but if you're shy, this discovery can be mind-blowing. Several weeks later, I was vacationing with my family on the north shore of Lake Tahoe, and we were staying on the 14th floor of a hotel with a casino on the ground floor. I told my two children that I wanted to teach them something important, so we left our hotel room and got on the elevator. I was wearing a cowboy hat, cowboy boots and dark glasses. As we descended, I forced myself to announce each floor out loud. It was extremely difficult at first, and my kids turned bright red. They couldn't believe what their father was doing. The people in the elevator started chuckling every time I announced a floor. The laughing got louder at each stop, and by the time we got to the lobby, the elevator was crammed with people, and everybody was laughing. When the elevator doors opened, all the people streamed out into the casino and headed toward the slot machines. I realized that they'd probably found the experience amusing, and felt happy that something mildly quirky and funny had happened in the elevator. Aside from that, my eccentric behavior didn't seem to have much importance in the bigger scheme of things. It was just an unexpected, pleasant distraction. This might seem humble and obvious, but it felt
Chapter 21
655
like a profound and liberating insight. I think it's good to do Shame-Attacking Exercises from time to time as "booster shots" so your fears don't return. This past Christmas Eve, we decided to go for a family hike. It was cold outside, and I had a mild earache, so I wanted something to cover my ears. When I looked through my dresser, I couldn't find my old stocking cap. It dawned on me that when we moved from Philadelphia to California, we'd given away most of our winter clothes. I was trying to find something else that might work, but all I could dig up was an old jock strap. I was thinking about the problem from a purely logical perspective, and noticed that the jock strap had a wide elastic band that might fit snugly around my head and cover my ears. I tried it on and it felt really good, but I realized that it might look peculiar. As a joke, I put it over my head like a hat and walked to the front door where my wife and children were waiting for me. They noticed it immediately and started laughing. Then my daughter, Signe, dared me to wear it out on our hike as a Shame-Attacking Exercise. She said that when we encountered neighbors or strangers, I could smile and say, "Top o' the mornin' to you!" My wife was shocked and pointed out that not only did the jock strap look incredibly eccentric on my head, it also looked extremely old and shabby. She said that people would think I'd just escaped from a nursing home. Regardless, I took up the challenge and wore the jock strap on my head for the next hour while we were hiking. It protected my ears nicely, and all of the people we met on the trails seemed perfectly happy when I greeted them, as if
Chapter 21
656
nothing was wrong at all. So if you come to one of my workshops or lectures and notice an old, worn out jock strap on my head, you'll understand what's going on! I've provided several personal examples of Shame-Attacking Exercises because I think it's vitally important to practice what we preach. You should never ask any patient to do anything that you'd be unwilling to do yourself. Once you've tried a few Shame-Attacking Exercises, you can start to use this powerful technique to help patients who are feeling shy. I once treated a painfully shy 31 year-old man named Trevor. Although he was exceptionally handsome, he hadn't had a date in over five years. This was surprising, because he looked like a model for Gentleman's Quarterly. My daughter was helping out in the front office of my clinic that summer, and she commented that he was drop-dead gorgeous. Trevor was intensely self-conscious because he had a tendency to sweat a great deal. He was convinced that women would be disgusted if they saw the circles of sweat on his shirt under his armpits. He was so worried about sweating that he always stayed indoors, especially during the summer months. It was especially hot and humid that summer in Philadelphia. I scheduled a double session for Trevor and told him that instead of sitting inside and talking during our session, we were going to visit several stores in the neighborhood so we could do some Shame-Attacking Exercises. I warned him that it would probably be frightening at first, but might help him get over his fears once and for all. Trevor courageously agreed to give it a try. On the way out of the hospital, I borrowed a squirt bottle from the clinical
Chapter 21
657
laboratory and filled it with water. Once we were outside in the hot sun, I told Trevor to raise both his arms so I could squirt the area under his armpits with water to make it look like he was sweating profusely. I also squirted his head and forehead liberally so it looked liked sweat was dripping from his face. To add to the effect, we jogged to a small grocery store in the neighborhood to produce some real sweat. This made him very anxious, because he was convinced that people would see how sweaty we were and be repulsed. I told Trevor to go into the store, raise one arm over his head, point to his armpit, and make the following announcement loudly enough so that everyone in the store could hear him: "Boy, it sure is hot today! Look at me! I'm sweating like a stuffed pig!" Trevor was terrified and refused to do it. He said that people would be totally grossed out. I told him that it was extremely important to confront his fears, no matter how anxious he felt. He protested again and said, "If you think it's so easy, I'd like to see you do it!" I said, "Sure, no problem!" I squirted myself liberally with water, went into the store, raised my arm above my head, pointed to my armpit and loudly declared how hot and sweaty I was. The people in the store didn't seem terribly interested in my sweaty armpits and just went about their business. In fact, I noticed that there was a man sitting on the sidewalk near the front door, quacking like a duck. Nobody seemed to be paying any attention to him, either! I told Trevor it was his turn. He swallowed hard and went for it. No one in
Chapter 21
658
the store seemed repulsed or shocked by his sweat, either. He could barely believe it. Then we jogged to another store and repeated the exercise. This time, people seemed amused and chatted with us enthusiastically about how hot it was. They seemed eager to talk. Trevor was surprised that we were getting such friendly reactions from people. I noticed an attractive young woman giving Trevor the eye. I told him to approach her, point to his sweaty armpit, and comment on how hot, sweaty and disgusting he felt. He was intensely resistant, and insisted that he simply couldn't do something that extreme. I pushed him, and told him that his fear was a sign that this was exactly what he had to do if he wanted to be totally liberated from his fears. He reluctantly approached the woman, raised his arm above his head, pointed to his armpit and shyly commented on how hot and sweaty he was. She didn't seem at all perturbed and started flirting with him. Soon they were engrossed in conversation. After a few minutes, she said that she had to go over to the medical center for a doctor's appointment, but she'd really like to have the chance to get together and talk some more. She offered him her phone number. Trevor was surprised, to say the least. He discovered that people didn't really care about his sweating. This experience put the lie to his negative thoughts, and his shyness was history. Many experts believe that exposure always works like this. It may not be the exposure, per se, that ends your fears. Instead, your anxiety will vanish at the
Chapter 21
659
exact moment when you discover that your fears are fraudulent. If you use Shame-Attacking Exercises skillfully, they can be tremendously liberating and funny, but if you use them inappropriately, they can backfire. This is true of all the CBT techniques I'm describing. They're powerful, and have to be used thoughtfully. When you're doing Shame-Attacking Exercises, keep the following guidelines in mind: Use good judgment. I knew that Trevor was attractive and charming, and that he was probably going to get good reactions from people. If he'd had poor interpersonal skills and came across in an off-putting way, other techniques would have been more appropriate. Don't do anything insensitive or offensive. The idea is simply to be a little outrageous and have fun. What Trevor and I did was harmless, and everyone enjoyed our zany behavior. Don't do anything unprofessional that could hurt your career. For example, I wouldn't dream of announcing the stops on the elevator at the Stanford University Hospital, because that would be disrespectful to the patients and staff. But it was a lot of fun at the casino in Nevada, and the people in the elevator seemed to enjoy my goofiness. Don't do anything hostile or aggressive. Have you ever seen the old Tom Green Show on the Comedy Channel? He did lots of zany things in public, which was great. However, many of his skits seemed hostile, and they were nearly always at someone else's expense. He often made people feel uncomfortable. As a result, his brand of humor, which had tremendous
Chapter 21
660
potential, seemed irritating and often fell short. In contrast, the British comic, Dom Joly, used to go about London doing zany, surrealistic things in public. His skits were televised on the British version of Trigger Happy TV. He nearly always poked fun at himself, and often played the role of a buffoon. His skits were incredibly funny, and he quickly became a celebrity in England. Role-Playing Techniques 19. Externalization of Voices I developed the Externalization of Voices in the mid-1970s because it seemed like we needed a CBT technique with real punch that could transform intellectual understanding into emotional change at the gut level. The Externalization of Voices is the most powerful of all the CBT techniques, but it has to be used with caution. I use the Externalization of Voices once patients have successfully put the lie to their negative thoughts on paper, using the Daily Mood Log. The Externalization of Voices will accomplish several things: You'll develop an amazing level of empathy for your patients, because you'll suddenly see what it feels like to be in their shoes, trying to fight off a constant barrage of devastating negative thoughts. You'll help your patients cement their gains and find out if they can crush their negative thoughts in real time. You can model effective responses to any type of negative thought and illustrate the difference between the Self-Defense Paradigm and the Acceptance Paradox.
Chapter 21
661
You can transform partial improvement into complete recovery. You can greatly reduce the likelihood that your patients will have to struggle with painful relapses in the future. In the late 1990s, I developed a daily group CBT program for the psychiatric inpatient unit at the Stanford University Hospital as part of my volunteer work for the Department of Psychiatry. Some of our groups were phenomenally effective, and we'd see dramatic changes in many of the patients' moods within a single 90-minute session. The Externalization of Voices was usually the technique that brought about these profound and rapid changes in their thoughts and feelings. Many patients encouraged me to tell all my students and colleagues that the Externalization of Voices was the most helpful technique of all. I've had similar experiences in individual therapy sessions. In fact, when I was treating patients, I spent approximately 40% of my time working with the Externalization of Voices. It blows most of the other techniques out of the water. Here's how it works. Let's say your patient has listed these negative thoughts on his Daily Mood Log: I'll never get better. What's wrong with me? My problems are hopeless. I'm such a loser. I'm always screwing up. I should be feeling better by now. I must be a weak person. What's wrong with me?
Chapter 21
662
Let's assume that he's already identified the distortions in these thoughts and has successfully put the lie to them. Now you can use the Externalization of Voices to cement his gains. One of you will play the role of his negative thoughts, and the other will play the role of his positive thoughts. The person playing the negative thoughts will attack, and the person playing the positive thoughts will fight back and try to defeat the negative thoughts. There are two ways to use the Externalization of Voices: the "I—I" method and the "You—I" method. The "I—I" method is gentle and safe, but not especially powerful. It's often a good first step when you're working with patients who are fragile or vulnerable. The "You—I" method is vastly more powerful, but can be intimidating to therapist and patient alike. When you use the "I—I" method, you and the patient will both use the first person, "I." In other words, the person playing the role of the negative thoughts will speak in the first person, "I," and the person playing the role of the positive thoughts will also speak in the first person, "I." When you use the "You—I" method, the person playing the role of the negative thoughts will speak in the second person, "You," and the person playing the role of the positive thoughts will speak in the first person, "I." So in both cases, the person who plays the role of the positive thoughts will speak in the first person. It's vitally important to remember this. If you forget, and the person playing the role of the positive thoughts uses the second person, "You," the method will fail miserably. That's because it will sound like you're trying to give the patient advice or cheer them up. This is never effective, and it's not a valid CBT
Chapter 21
663
technique. Urging depressed or anxious individuals to think more positively is irritating and nearly always makes them feel worse. Let's assume that the patient has decided to work on his negative thought: "I'm such a loser. I'm always screwing up." Using the "I—I" method, the person playing the role of the negative thoughts would say this: "I'm a total loser. I'm always screwing up." Using the "You—I" method, the person playing the role of the negative thoughts would say this: "You're a total loser. You're always screwing up." Remember that in both cases, the person playing the role of the positive thoughts will reply using the first person, "I." This person will try to refute the negative thoughts using the Self-Defense Paradigm, the Acceptance Paradox, or a combination of the two. When you use the Self-Defense Paradigm, you argue with the negative thought and point out that it's distorted and unreasonable. When you use the Acceptance Paradox, you defeat the negative thought by surrendering and finding truth in it. Here's an example of the "I—I" Method: Negative Thoughts: I'm such a loser. I'm always screwing up. Positive Thoughts: I'm a human being with strengths and weaknesses, just like everyone else. Sometimes I make mistakes, and that can be painful. But to say that I'm always screwing up, that's just patently absurd. Now, here's a brief example of the "You—I" Method: Negative Thoughts: You're such a loser. You're always screwing up. Positive Thoughts: I'm a human being with strengths and weaknesses,
Chapter 21
664
just like everyone else. Sometimes I make mistakes, and that can be painful. But to say that I'm always screwing up, that's just patently absurd. Notice that the only difference is the voice the person playing the role of the negative thoughts uses. In this example, the person playing the positive thoughts has used the Acceptance Paradox along with the Self-Defense Paradigm. If the person playing the positive thoughts does a good job, the person playing the negative thoughts should continue to attack as ruthlessly as possible, as in this continuation of the "You—I" version: Negative Thoughts: Sure, you can make excuses and rationalize all you want. But the fact is, you did screw up, and you screw up way more than other people because you're so inferior. You're a disappointment as a human being. Positive Thoughts: You're right! I did screw up. And I have lots of flaws. In fact, once you get to know me better, you'll see that the ones you're aware of are just the tip of the iceberg! This response illustrates the Acceptance Paradox. If you were playing the role of the positive thoughts, and you made this statement with a sense of humor and inner peace, you'd silence the critic. You'd win by losing, so to speak. Some therapists have asked me when they should use the Self-Defense Paradigm, and when they should use the Acceptance Paradox. I'm afraid there's no simple formula. You can only learn this with lots of practice. It's a bit like asking, "What type of shot should you hit during a tennis match?" The answer
Chapter 21
665
might be, "Use the shot that seems to work the best at that moment." However, I can provide you with some general guidelines. On average, the negative thoughts that rob the patient of self-esteem usually respond best to the Acceptance Paradox, as in the example above. In contrast, if the negative thoughts involve feelings of hopelessness, the Self-Defense Paradigm usually works much better, as in this example: Negative Thoughts: You'll never get better. You're a hopeless case! Positive Thoughts: I can't agree with that. I may feel hopeless, but that doesn't mean I really am hopeless. Whenever I've gotten anxious or depressed in the past, I've always been able to resolve the problem, and sooner or later, I felt better again. I'm sure it will happen this time, too. But even when I'm 80 years old, upsetting things will happen. I can't expect to be happy all the time! This response illustrates the Self-Defense Paradigm. I wouldn't want a depressed patient to agree with the idea that she or he is hopeless. In the first place, it's not realistic, and in the second place, it might trigger a suicide attempt. But even in this response, I'm giving the devil his due by acknowledging that there will always be times when the negative feelings come bubbling up again. You can also use the Self-Defense Paradigm when the negative thoughts involve factual errors. For example, a shy young woman named Allison decided to attend a dance at her church, even though the idea made her very anxious. An attractive younger man named Ben repeatedly asked her to dance. Although she thought he was exciting, she kept turning him down because she told herself,
Chapter 21
666
"Ben isn't really attracted to me. He's just being nice." This thought was patently absurd. Ben had called her at home several times to ask for a date. Using the Self-Defense Paradigm, Allison could attack her negative thought along these lines: "The idea that Ben isn't attracted to me is ridiculous. In fact, he's been asking me to go out with him for the past six weeks." There are a few nearly universal errors you should try to avoid when you're using the Externalization of Voices. First, remember that you should only attack patients with their own negative thoughts. Some therapists get carried away and begin to attack patients with all kinds of negative thoughts they've never had. This will sound lame and irrelevant, and will defeat the whole purpose of the technique. The best way to avoid this problem is to read the patient's negative thoughts directly from the Daily Mood Log during the role-playing, using either the first person or the second person. Second, remember that this is not assertiveness training. When you use the "You—I" version of the Externalization of Voices, the person playing the role of the negative thoughts will sound like another person who's attacking the patient. For example, the person in the negative thoughts role might sound like the patient's critical parent, boss, or spouse. If the technique degenerates in this direction, stop and remind the patient that they're doing battle with their own negative thoughts, and not with another person. This type of confusion is so common that I created two signs that read, "My Negative Thoughts" and "My Positive Thoughts." I used these signs during my Stanford inpatient groups whenever we did the Externalization of Voices.
Chapter 21
667
Patients would hold these signs in front of their chests to indicate which role they were playing. This reminded everyone that this was a dialogue between the two parts of the patient's mind. These signs appear on pages 668 – 669. Feel free to photocopy them for use with your patients. The third error is to rely too much on the Self-Defense Paradigm. From a Buddhist point of view, self-defense creates instant war. When you defend yourself, you invite further attack. So you end up at war with yourself, which is a war you can never win. In contrast, when you find truth in the criticisms, you take all the wind out of the critic's sails. If the patient stumbles when playing the positive thoughts, do a rolereversal so you can model more effective responses. Keep in mind, however, that when you're playing the role of the positive thoughts, you may also begin to feel overwhelmed. You may find that you can't effectively challenge the patient's negative thoughts because they seem so valid and intense. This is especially common when you use the more powerful "You—I" version. This used to happen to me a lot. Sometimes, neither the patient nor I could come up with effective responses by the end of the session. I'd simply acknowledge that we were both stuck. I'd say, "I'm pretty sure there's something rotten in Denmark here. We just haven't figured it out yet." Then I'd suggest that we could both think about the problem as homework. More effective responses nearly always popped into my head within a day or two, and at the next session, we continued where we'd left off.
Chapter 21
My Negative Thoughts
668
Chapter 21
My Positive Thoughts
669
Chapter 21
670
When you can't refute a negative thought, you can always go back to basics. Put the intimidating thought in the middle of the Recovery Circle and select at least 15 techniques you could use to challenge it. You can incorporate any of these techniques into the role-playing when you're doing the Externalization of Voices. When patients develop the ability to shoot down their negative thoughts in a convincing manner, there will nearly always be a sudden and profound shift in how they feel, along with a shift in their underlying values and beliefs. I strongly recommend the Externalization of Voices, but it will take a little courage at first, and lots of practice before you get really good at it. Once you've mastered this technique, you'll be head and shoulders above most other CBT therapists. 20. Feared Fantasy Sometimes our patients are afraid of things that they'll never be able to confront in reality, so the Classical Exposure Techniques won't work. The Feared Fantasy is a powerful Role-Playing Technique that can be quite effective in these situations. When you use the Feared Fantasy, you invite patients to enter an Alice-in-Wonderland nightmare world where their worst fears actually spring to life. This world differs from reality in two unusual ways. First, if you think people are looking down on you, they really are. In fact, their negative thoughts about you are even worse that what you imagined. And second, the people in this world are not at all polite. They always tell you exactly what they're thinking, no matter how cruel or brutal it might sound.
Chapter 21
671
This gives patients the chance to confront the monster they fear the most and discover that it has no teeth. Their worst fear turns out to be a kind of cosmic joke. Bob was a handsome and successful corporate executive from Atlanta who suffered from severe shyness (Social Anxiety Disorder). You'd never imagine that Bob suffered from shyness because he came across in such a polished, articulate manner. He did well in business settings because he was the man in charge, and the meetings always followed a certain predictable protocol. But he was terrified by informal social gatherings and avoided them like the plague. He even felt uncomfortable at family gatherings. He coped with his shyness primarily by avoiding all social functions, and spent most of his time alone. Bob was convinced that: His shy feelings were abnormal and showed that he was inferior, defective and unmanly. Normal people rarely or never experienced feelings of shyness and insecurity in social situations. If others knew how he really felt inside, they'd be shocked and look down on him. Bob agreed to test these beliefs using an extreme form of Self-Disclosure. He rode the Philadelphia subway continuously for several hours and forced himself to have conversations with the people he was sitting next to. In the course of these conversations, he disclosed the fact that he felt shy and anxious
Chapter 21
672
in social situations. He was surprised that nobody seemed at all shocked or put off. Most of them were remarkably warm and kind. Several people told him that they'd struggled with the same kinds of feelings. Bob said that these were some of the best conversations of his entire life, and that he felt intoxicated after his subway adventure. This intervention was helpful because Bob was able to put the lie to his negative thoughts. However, he still hadn't confronted his worst fear. He'd simply discovered that his fears weren't realistic. Using the Feared Fantasy, Bob can examine the other side of the coin. Suppose he disclosed his shyness to someone who turned out to be just as hostile and rejecting as he imagined? What then? Would that be terrible? Bob's wife had scheduled a Superbowl party at their home, and Bob was dreading the event. He said that the worst part for him would be sitting around with the guys watching the game, making small talk and trying to appear normal. He especially dreaded having to interact with his nephew, who admired him a great deal. His worst fear was that his nephew would "discover" his horrible secret and lose all respect for him. In the following Feared Fantasy dialogue, Bob will play the role of the Nephew from Hell, and I'll play Bob. We're watching the Superbowl at a party and I've decided to stop faking it and trying to hide my shyness. Instead, I'm going to disclose my shyness and let the chips fall where they may. When my nephew hears about my shyness, he'll try to rip me to shreds. He'll say all the most horrible, humiliating things he can possibly think of:
Chapter 21
673
Nephew from Hell (played by Bob): Hi, Uncle Bob, how have you been? Bob (played by David): Oh, pretty good. Everything at work is booming along. Nephew from Hell (played by Bob): You know, Uncle Bob, there's something I've been meaning to ask you. You always seem really formal and awkward when the family is hanging out together. Is something bothering you? Bob (played by David): You probably picked up on my shyness. I've never felt very comfortable around other people, but I usually try to hide it. I've decided to stop that and just be honest with people. The fact is, I'm damn shy, and always have been. Nephew from Hell (played by Bob): Gee, that seems abnormal. I always thought you were a real stud. Is there something wrong with you? I thought only girls or wimps felt shy. I mean, that's pretty weird. Bob (played by David): You know, lots of people view me as quite different from the way I really am. I wish I didn't feel so shy, but I do. It's one of my flaws. But believe me, I have lots of others as well. Nephew from Hell (played by Bob): In all honesty, I'm disappointed. You were always someone I looked up to. Now it seems like you're some kind of a nut case.* Bob (played by David): Well, I'm glad we cleared the decks, because I'd
Chapter 21
674
hate to mislead you or have you thinking I'm something that I'm not. Nephew from Hell (played by Bob): Uncle Bob, I have to be honest. I really look down on you. In fact, I don't even want to talk to you any more. Why don't you go and sit in the corner so you won't contaminate anyone with your weirdness. Bob (played by David): Wow! That's really a strong reaction! It sounds like you're ticked off. Do you look down on everybody who feels insecure, or is it because you used to look up to me, and now you feel disappointed because I have clay feet after all? Nephew from Hell (played by Bob): Ugh! I'm done with all this touchyfeely garbage. You suck! Maybe you should go and help the women make salad in the kitchen. I'm going to go chew on a Slim Jim and talk to Uncle Joe about professional wrestling and other more manly topics. Now, who's being the bigger jerk here? Is it Bob, or the Nephew from Hell? Bob could see that the Nephew from Hell was the one who sounded "off." It might be awkward to interact with someone who was so judgmental, but it clearly wouldn't be a reflection on Bob. Once the patient gets it, you can do a role-reversal, so she or he can do battle with the monster. This will convert intellectual understanding into real change at the gut level. You can also use the Feared Fantasy to help patients develop unconditional self-esteem and put the lie to their Self-Defeating Beliefs, such as * There could be various types of nuts, and cases of differing sizes, but you get the idea.
Chapter 21
675
Perfectionism, Perceived Perfectionism, the Achievement Addiction, the Love Addiction, the Approval Addiction, and others. When I'm leading CBT groups for depressed and anxious patients, I ask how many of them sometimes struggle with feelings of inferiority, worthlessness, or low self-esteem. Typically, all the hands go up. Then I ask the patients how we measure our self-esteem. What do we think we have to have or do in order to be worthwhile human beings? Patients generally come up with a long list, including things like this: Outstanding achievements, intelligence or productivity Loving other people, or being loved by others Being approved of Being happy Strong faith in God Altruism and compassion toward people who are suffering. I divide the patients into small groups, and have each group create a CostBenefit Analysis for a different SDB. For example, the Great Achievers group can list the advantages and disadvantages of basing your self-esteem on your accomplishments and productivity. The Ideal Love group can list the advantages and disadvantages of basing your self-esteem on being loved. The other groups can list the advantages and disadvantages of basing their self-esteem on other people's approval, on being happy, on having a strong faith in God, or on any other criterion they come up with. Most groups will decide that even though there are lots of tangible
Chapter 21
676
advantages to all these belief systems, the disadvantages are greater. For example, let's say you tell yourself that you're a worthwhile human being as long as you feel happy. One of the advantages is that you won't have to base your self-esteem on your accomplishments, and you won't have to feel inferior to all the people who've accomplished more than you. But on the disadvantages side, no one can feel happy all the time. We all fall into the occasional black hole of depression, anxiety or self-doubt. If you base your self-esteem on your happiness, you'll conclude that you're worthless whenever you feel unhappy. Furthermore, you'll succumb to the trap of Emotional Perfectionism, thinking that you're not allowed to have negative emotions. The CBA is a useful first step in changing an SDB. However, many patients will still feel convinced that their SDBs are valid, even though there are some disadvantages. For example, patients may cling to the belief that people who are exceptionally attractive, famous, or successful really are superior human beings, and that these "beautiful people" are living wonderful, incredibly joyous lives that the rest of us can only dream about. In fact, this type of thinking is so prevalent in our culture that it's almost impossible to escape it. The Feared Fantasy can put the lie to this line of thinking in a dramatic way. In the following example, an anxious patient named Nick has an imaginary encounter with an old classmate, Peter Perfect, at their 25th high school reunion. Peter Perfect is one of the "beautiful people" who represents all the qualities that Nick thinks a "superior" person would have. He's a brilliant, attractive, self-made billionaire. He's also a world-class intellectual who's loved and admired on every
Chapter 21
677
continent. He has boundless self-confidence and lives in a constant state of euphoria. To top it off, Peter Perfect has a gorgeous wife who adores him and three precocious children with IQs above 180. In this Feared Fantasy dialogue, I'll play Nick, and Nick will play the role of Peter Perfect: Peter Perfect (played by Nick): Hi there, Nicky. Do you remember me? Nick (played by David): You bet I do. I saw your photo on the cover of Time Magazine last week as Man of the Year. I couldn't believe that someone I went to high school with had become so famous. It blew me away. Congratulations! Peter Perfect (played by Nick): Well, I must admit, I've had my share of good luck. As you probably know, I just won the Nobel Prize in physics for my work on string theory. They think my pioneering efforts have finally paved the way for an understanding of the origin of the universe. I wouldn't argue! And of course, I've also achieved unparalleled success in business. Actually, my list of achievements goes on and on. I'm a world leader in philanthropic, charitable work. I'm about to be on the cover of Newsweek as well. They've named me the Man of the Decade. It's all a bit over the top, but what can you do? I try to be as gracious as I can. Nick (played by David): That's amazing, Peter. It sounds like you've really arrived! I can remember how you got all those awards in high school, too. You were valedictorian, captain of the football team, Student Body President, and King of the Senior Prom. What's it like being so rich and famous?
Chapter 21
678
Peter Perfect (played by Nick): Oh, it's really beyond my wildest dreams. I only hang out with the beautiful people now, like George Bush. He invited me to hang out with him on his ranch in Texas just last week because he wanted to pick my brain about international policy, but as you can imagine, I had to turn him down because my time is so valuable. After all, I have so many friends and admirers clamoring to hang out with me, like Tom Cruise, Sting, Britney Spears, Madonna, and Michael Jordan. Sometimes, it gets hard to keep up with all the demands, if you know what I mean. But then, that's what social secretaries are for! Nick (played by David): Wow! What do you do when you hang out with all those famous people? Peter Perfect (played by Nick): They mainly just like to admire me and be seen with me. Of course, that's understandable. People are usually chasing after them, so it's nice for them to be able to just relax and fade into the background for a change when they're with me. Of course, a lot of them want to have sex with me, too. Did I mention Britney? And who can blame them? I guess people just can't help but get turned on by me. Nick (played by David): Peter, I'm really impressed by your glitzy lifestyle, and I'm sure you deserve everything you get. But there's one thing I heard that confuses me, and I'm wondering if I could ask you about it. Peter Perfect (played by Nick): Sure, Nick, ask away! Nick (played by David): I heard through the grapevine that you thought
Chapter 21
679
you were better than other people because of all your achievements. I was surprised to hear that, so I thought I'd better check it out with you. Peter Perfect (played by Nick): Well, this may be hard for you to understand, given your rather modest intelligence, but let's face the facts. Everyone knows that our worth as human beings depends on our achievements and popularity. I've probably achieved far more than almost any other human being in history, and there's no one in the world as famous and popular as me, so it just logically follows that I'm superior to pretty much everybody. I've had to accept the fact that I'm, shall we say, exceptional. I don't mean to hurt your feelings, and I know that you have your own little mediocre accomplishments, like coaching the grammar school soccer team, and teaching Sunday School classes at your church. But you should know that I look down on you because I'm so vastly superior to you. That's just the way it is. Nick (played by David): It sounds like you really enjoy feeling superior and looking down on people. Do you? Peter Perfect (played by Nick): Of course! It's a lot like eating caviar all the time. I accept the fact that the world is full of peasants like you who have to settle for stale bread. Meanwhile, I'm in a state of constant euphoria. After all, I get to hang out with me all the time. What could be more wonderful? Obviously, this dialogue is ludicrous. Peter Perfect is simply the personification of Nick's value system. But even if Peter Perfect did exist, he
Chapter 21
680
doesn't seem like the most fun person to hang out with. In fact, he sounds relentlessly self-absorbed and boring. Patients who feel inferior are usually looking up at others from a one-down position. They're telling themselves, "Oh, I'm so average. I have an average career, average hobbies, an average family and an average life. There's nothing special about me. How could I ever possibly feel worthwhile or fulfilled? I really am second rate." The Feared Fantasy provides patients with a radically different perspective. They can assume the role of a "superior" human being and ask themselves, "If I had all this fame and all these fantastic achievements, would it really make me better than other people? Would I want to look down on people and think they were inferior to me?" Often, patients will be able to see how irrational it is to rate people as superior human beings based on their intelligence, achievements or fame. You can use the Feared Fantasy to challenge any criterion the patient uses as a basis for self-esteem. In the following example, Nick has decided to base his sense of self-esteem on his faith in God. He runs into his old classmate, Peter Perfect, at their high school reunion, and discovers that Peter has become a profoundly religious person. Once again, I'll play Nick and Nick will play Peter Perfect: Nick (played by David): Hi, Peter. I heard through the grapevine that you've developed a tremendous, unshakeable religious faith. Peter Perfect (played by Nick): Well, Nick, that's true. In fact, I'm about
Chapter 21
681
to be named a Saint by the Catholic Church. I guess it's not such a surprise. Most religious experts say that my faith is already deeper than that of the medieval saints. And it sure feels good to be as incredibly spiritual as I am. I'm beginning to think that I must be one of God's chosen people. If you want, you can call me Saint Peter. Nick (played by David): That's awesome, Saint. I'll be proud to say that I went to high school with an actual saint! I can remember how you used to sit and pray during gym class when the rest of us were running laps. I knew there was something unique about you even then. St. Peter (played by Nick): That was nothing. I pray constantly now. Of course, God answers all my prayers. In fact, I'm praying even as we talk. Nick (played by David): Hey, mention me to Mr. Big. I can use all the help I can get! Listen, Saint Peter, there was just one thing I heard that confused me, and I wanted to bounce it off you. St. Peter (played by Nick): Shoot. I'll pray for you while you talk. Nick (played by David): Thanks! Here's my problem. I heard that you believed that you were superior to other people because of your incredible religious faith. That didn't quite compute, so I wanted to check it out with you. St. Peter (played by Nick): I can understand your confusion, but it's true. You see, the more faith you have, the more worthwhile you are. So it dawned on me that I must be the most worthwhile person in the world because there isn't anyone with a faith like mine. Even the Pope doesn't
Chapter 21
682
have the kind of awesome faith that I do, and he sometimes struggles with moments of self-doubt. I've told him that he can call on me for guidance any time. So logically, that kind of makes me top dog. Nick (played by David): So are you saying that you really are better than other people, even the Pope? St. Peter (played by Nick): I know it may sound harsh, but honesty is the best policy. I don't know of anyone who's at my spiritual level. Therefore, I must humbly accept the fact that I am better than other people. It comes with the territory of being a Saint in your own time. Nick (played by David): Gee, I have to confess that I don't have a great deal of religious faith. In fact, I think I may be more of a heathen. St. Peter (played by Nick): That's okay, Nick. I'd look down on you even if you were a man of religious faith, since my faith would be superior to yours. But I do have compassion for you. Oh, how you must suffer! I guess some of us have it, and some of us don't. That's what they mean when they say, "God works in mysterious ways." Once again, this dialogue is absurd, but it should make it clear that any basis for self-esteem is inherently ludicrous. There's simply no way to measure how worthwhile a human being is. Of course, unconditional self-esteem is just another stepping-stone on the path to enlightenment. Once you've developed unconditional self-esteem, you'll want to get rid of it as fast as possible. Selfesteem is an empty, meaningless concept. It's just a marketing term that's used to sell books and products. When you lose your "self-esteem," you haven't really
Chapter 21
683
lost anything, because there was nothing there in the first place. But you'll gain freedom and inner peace, and an increased capacity for happiness, intimacy, and creativity. Other Role-Playing Methods Many techniques can be effective in a role-playing format, and they're often more powerful and entertaining when used in this way. For example, on page 589, you learned about the role-playing version of the Double Standard Technique. Other Role-Playing Techniques include the Acceptance Paradox, the Devil's Advocate, and many of the Interpersonal Techniques such as the David Letterman Technique, Flirting Training, the Rejection Feared Fantasy, and the Five Secrets of Effective Communication. Philosophical / Spiritual Techniques 21. Acceptance Paradox The Acceptance Paradox represents the spiritual core of CBT. It can lead to emotional enlightenment, but it's the most difficult technique for patients and therapists alike to comprehend. People often equate CBT with the Self-Defense Paradigm. They think that CBT is based on: Defending yourself from attack, especially your own self-criticisms Emphasizing your strengths instead of dwelling on your shortcomings Thinking about yourself and your life more positively. All the Truth-Based Techniques, such as Examine the Evidence, the Experimental Technique, the Survey Technique and Reattribution, are based on
Chapter 21
684
the Self-Defense Paradigm. Identify the Distortions, the Socratic Method and Let's Define Terms are based on self-defense as well. These techniques can be valuable, but for certain kinds of negative thoughts, the Acceptance Paradox will be vastly more effective. Instead of disputing your negative thoughts, you accept them with a sense of humor and inner peace, without any feelings of shame or humiliation. This causes a profound shift in the way you think and feel. You'll often experience a transformation in your personal values and beliefs as well. In fact, the Acceptance Paradox is the ultimate antidote to many of the Self-Defeating Beliefs that trigger depression and anxiety, such as Perfectionism, Perceived Perfectionism, and the Achievement, Love, and Approval Addictions. Although the Acceptance Paradox is a psychological technique, it has spiritual implications, and can help patients develop a deeper understanding of their own religious heritage. Most religions, including Judaism, Christianity, and Buddhism, seem to be based on the Acceptance Paradox. I'm not an expert in theology, but I was raised in a Christian home, and have some understanding of the Christian message. Christianity is based on the idea of original sin. This is a way of saying that we're all inherently flawed. Try as we might, we can never achieve perfection. Because we can't seem to overcome our flawed and sinful nature, Christians participate in the ritual of Holy Communion. The idea is that if we confess our sins, we'll be forgiven and can experience redemption. Furthermore, we can't earn our way to heaven through our good works, but can only be saved
Chapter 21
685
by grace. So Christianity is based on a paradox. We can only achieve true joy and enlightenment when we accept the fact that we're broken beyond repair. Christians also believe that Christ died for our sins. He paid the price for our salvation. But on the third day, he rose from the dead and ascended into heaven. What does this mean? Metaphorically speaking, it means that something inside us has to die before we can discover the real meaning of life. Similarly, when you comprehend the Acceptance Paradox, your pride and ego will die, but you'll experience a profound personal liberation. The Acceptance Paradox and the Disarming Technique are very similar. When you use the Disarming Technique, you accept the criticism of another person. When you use the Acceptance Paradox, you surrender to your own inner critic. A Catholic priest with a Ph.D. in ancient languages once attended a CBT workshop I conducted in Oklahoma. He said he was intrigued by the Disarming Technique, and explained that the Christian concept of "confession" of sins is actually based on a mistranslation of the original Aramaic text. The correct translation was not, "to confess," but rather, "to agree with." So the Disarming Technique and the Acceptance Paradox are really spiritual concepts. The Acceptance Paradox is equally compatible with Buddhism. The Buddhists say that our suffering does not result from reality, but rather from the judgments we make, and from our insistence that things should be different from the way they are. The Buddhist concept of enlightenment and freedom from suffering is based on acceptance.
Chapter 21
686
Of course, words are cheap. Integrating the Acceptance Paradox into your own value system is far more challenging. It's like the difference between seeing a post card of the Grand Canyon and seeing the real thing. It takes your breath away! Perhaps you've had this experience. The first time I saw the Grand Canyon, I was on a camping trip with a friend. We arrived late in the evening and couldn't see much because it was so dark. We camped out in sleeping bags next to our car. When I woke up in the morning, I realized that we were sleeping a few feet from the edge. The sun was just coming up. As I turned to look, I saw the Grand Canyon for the first time. Wow! I'd heard there was a big hole in the ground, but I had no idea it would be like that! By the same token, when you suddenly grasp the Acceptance Paradox for the first time, it's a mind-boggling experience. However, this type of understanding will usually only develop during one of the role-playing exercises, such as the Externalization of Voices or Feared Fantasy. When I do workshops for mental health professionals, I often ask how many of the therapists in the audience sometimes struggle with feelings of selfdoubt. Nearly all the hands go up. Then I ask them what kinds of negative thoughts they have when they're feeling that way. They volunteer thoughts like this: I don't know what I'm doing with my patients. There are so many patients I'm stuck with. I should know how to help them, but I don't.
Chapter 21
687
Other therapists are smarter than I am. I'm a fraud. I don't really know anything. I'm so inadequate. I'm always screwing up! Do any of these thoughts sound familiar? If you like, you can jot down a few of your own negative thoughts here: 1. 2. 3. 4. 5. Then I ask for several volunteers to come forward so I can illustrate the difference between the Acceptance Paradox and the Self-Defense Paradigm. I explain how the Externalization of Voices works, and tell them that I'll play the role of their negative thoughts, using the second person, "You." Their job is to defeat me, using the first person, "I." They can use the Self-Defense Paradigm, the Acceptance Paradox, or both. When I attack them with their own negative thoughts, they nearly always respond defensively. Then I ask them if their response felt strong or weak, and who won the exchange. They tell me that I won, and that their attempt to defend themselves wasn't effective. Then we do a role-reversal, so I can model a different way of responding, as in this example: Negative Thoughts (played by volunteer from audience): You're so
Chapter 21
688
inadequate! You're always screwing up! What's wrong with you? Positive Thoughts (played by David): You're right. I have many inadequacies. In fact, there's probably nothing about me that couldn't be improved. But hey, once you get to know me better, you'll see that the flaws you mentioned are only the tip of the iceberg! Negative Thoughts (played by volunteer from audience): You don't know anything. Positive Thoughts (played by David): You know, the older I've gotten, the more aware I've become of just how little I know. And sometimes, I get to thinking that there's almost nothing I'm really certain about. But that's kind of exciting, because there's so much room for research and creative work in the behavioral sciences. Most of the important discoveries are still ahead of us. Negative Thoughts (played by volunteer from audience): Okay, if you admit that you don't know anything, that proves you're a fraud. Positive Thoughts (played by David): Definitely! In fact, that's one of my better characteristics! Negative Thoughts (played by volunteer from audience): You can joke about it if you want, but this is serious. If you're a fraud, then you can't help any of your patients. Positive Thoughts (played by David): That's actually not true. Many of my patients have improved a great deal, and lots of them have told me how much they've appreciated the work we've done together.
Chapter 21
689
Negative Thoughts (played by volunteer from audience): Sure, maybe you've helped a few of the easier cases, but anyone could've helped them. The fact is, you've got many patients who aren't improving. If you were a better therapist, you could help them. Positive Thoughts (played by David): Oh, you're right about that! There are several patients I feel stuck with, and I'm sure there are plenty of therapists who would have more effective strategies for helping them. Negative Thoughts (played by volunteer from audience): Oh, so you admit that there are lots of other therapists who are smarter and better than you are? Positive Thoughts (played by David): Absolutely! I have no doubt about it. Negative Thoughts (played by volunteer from audience): Well, that's just shameful. Maybe you should leave therapy to the experts and pursue a more suitable career. Perhaps you'd make a good janitor or hairdresser. Positive Thoughts (played by David): You know, I've actually thought about that. Given all the hassles of managed care, I've wondered if I might make more money as a hairdresser. But I've also thought about the fact that most of my patients really seem to like me, even though I'm not perfect. In fact, they seem to like me more when they see that I'm human and real. And the great majority of them seem to improve in spite of my "averageness." So I think I'll just keep trucking along.
Chapter 21
690
Negative Thoughts (played by volunteer from audience): You don't seem to get what I'm saying. You stink. You constantly screw up. Positive Thoughts (played by David): I doubt that I constantly screw up, but I do make mistakes, and there's lots of room for improvement. Could you point out a few specific things I could work on? Do I need to be more empathic? Do I make too many Agenda Setting errors? Do I need to improve my skill with some of the 50 CBT techniques, such as the Acceptance Paradox? I'm eager to learn as much as I can. Negative Thoughts (played by volunteer from audience): Ugh! This is a total waste of time. I quit! Positive Thoughts (played by David): No problem. In fact, I was just having the same thought! Now ask yourself—who was the "winner" and who was the "loser"? Who looked like the bigger jerk? When you use the Acceptance Paradox, you win by losing. You achieve victory through surrender. The choice between the Acceptance Paradox and the Self-Defense Paradigm isn't black-and-white. You can blend the two. In the dialogue above, I used self-defense twice. When the negative thoughts said, "You can't help any of your patients," and "You constantly screw up," I defended myself because those criticisms were blatantly false. But I also included liberal doses of the Acceptance Paradox. In fact, we all have plenty of patients we feel stuck with, and we all make therapeutic mistakes. One of the secrets of the Acceptance Paradox is to transform vague,
Chapter 21
691
judgmental criticisms into specifics. For example, when the negative thoughts said, "Your therapeutic style stinks," I agreed that there was lots of room for improvement, and asked for some specifics. This response tends to leave the critic speechless because most of the destructive power in a negative thought results from the Overgeneralizations and hidden Should Statements. Remember that this is not a battle between two people. It's a battle between the negative and positive voices in your own mind. Make sure that the person playing the role of the positive thoughts always uses the first person, "I." If the person playing the positive thoughts uses the second person, "You," the technique will fail miserably. If the patient "sees" it right away, you've hit a home run, and the patient will experience profound relief. However, most patients won't be able to grasp the Acceptance Paradox initially. I've emphasized that when a technique doesn't work, you can simply move on to the next technique on your Recovery Circle. The Acceptance Paradox is an exception to this rule. If the patient doesn't see it, you can continue to model it, using frequent role-reversals. I've had many patients who couldn't comprehend the Acceptance Paradox until we'd worked with the Externalization of Voices for several sessions. Then it was as if somebody had turned flipped a switch in their brain, and they suddenly saw the light. The Acceptance Paradox is difficult to comprehend because our culture is steeped in the values of Western European civilization. We emphasize the importance of individualism and pride. We think we're supposed to be "winners"
Chapter 21
692
and defend ourselves from attack. The Acceptance Paradox is more compatible with Eastern philosophy. Instead of fighting, you surrender. In the process of "losing," you paradoxically "win." Patients may have trouble comprehending the Acceptance Paradox because they think that they have accepted themselves. They believe that they've discovered the horrible truth about themselves, and feel convinced that they're irreversibly flawed, worthless, and hopeless. These feelings can be so painful that many patients turn to suicide as the only escape from their suffering. These patients haven't distinguished healthy from unhealthy acceptance. As you can see on page 693, unhealthy acceptance is characterized by feelings of self-hatred and despair. In contrast, healthy acceptance is characterized by feelings of joy and involves a celebration of life. Patients may resist true self-acceptance because they think that something awful will happen if they accept themselves. They may think they'll have to settle for a life of mediocrity and unhappiness, and give up on their dreams of greatness. They may also think that if they accept their flaws, they'll never grow or change.
Chapter 21
693
Healthy Acceptance
Unhealthy Acceptance
Self-Esteem
Self-Hatred
Joy
Despair
Productivity
Paralysis
Hope
Hopelessness
Intimacy
Isolation
Growth
Atrophy
Laughter
Cynicism
These fears result from a lack of understanding of the Acceptance Paradox. The problem is not that we have deficiencies or flaws, but that we have the urge to hide them in shame. When we insist we shouldn't be like that, and struggle to be better than we are, we get stuck, so nothing really changes. In contrast, when you accept your flaws without a sense of shame, it becomes far easier to learn from them and grow. In fact, you could argue that self-acceptance is the most fundamental change that a human being can make. Paradoxically, the moment you accept yourself, you have changed. All humans are flawed. This idea is as basic as the law of gravity. So we have a choice to make. We can accept our humanness with joy or with despair. It's about as simple as that. Now let's practice. I'm sure you've had patients who suffered from feelings
Chapter 21
694
of inferiority or a lack of self-esteem. Usually, they're telling themselves that they aren't sufficiently: Intelligent Successful Charming Funny Loved Attractive Athletic Sexy Or, they may be telling themselves that: They've made too many mistakes in life. They should have done things differently. They should be better than they are. They've hurt other people or done things that are bad. They've failed to achieve their goals or fulfill their dreams. Imagine that your patient is playing the role of the negative thoughts, and you're playing the role of the positive thoughts. The patient attacks you by saying: Negative Thoughts (played by your patient): You really aren't very intelligent, are you? What will you say next? Write your response here before you turn the page:
Chapter 21
695
Chapter 21
696
Answer Of course, there's no single "correct" response, but here's one example of how the Acceptance Paradox might work: Positive Thoughts (played by you): As a matter of fact, there are lots of people who are a whole lot smarter than I am. Just think of all the millions of fabulously talented physicists, mathematicians, scientists, musicians, athletes and writers throughout the world. There are more than six billion people on the earth right now. Even if only 1% of them have IQs in the genius range, it means there are 60 million geniuses out there! Wow! Now, let's say the patient comes back at you like this: Negative Thoughts (played by your patient): Oh, so then you accept the fact that you're really just a stupid, inferior person? What will you say next? How would you use the Acceptance Paradox? Write your response here before you turn the page:
Chapter 21
697
Answer Here's one approach: Positive Thoughts (played by you): When you say that I'm a stupid, inferior person, I'm not completely sure what you mean. There's no doubt that some people are incredible geniuses, and I'm definitely not in that group. Is that what you mean? Here's how the rest of the dialogue might go. Notice that we'll continue to focus on the Acceptance Paradox: Negative Thoughts (played by your patient): Boy you sure are slow! It should be obvious. What I mean is that all those brilliant people are superior to you. You're inferior. You're just a peasant. You're cannon fodder, a common foot soldier. Positive Thoughts (played by you): Well, that's okay with me. I kind of enjoy being a foot soldier. In fact, I have many wonderful friends and colleagues who are probably also foot soldiers, so we share a lot in common! But I may be missing something here. Are you saying that there's something bad or terrible about being the way I am? You may have to spell this out for me. Remember, I'm not a genius. Negative Thoughts (played by your patient): What I'm trying to say is that you aren't entitled to feel any real joy or self-esteem because you aren't good enough. You don't measure up to the high, lofty standards I have in mind. Positive Thoughts (played by you): Oh, I realized that years ago. It
Chapter 21
698
dawned on me how many limitations and flaws I have. But one day, I decided to accept myself, and I've experienced tremendous joy ever since. Negative Thoughts (played by your patient): But you've just admitted that you're a bag of deficiencies. How can you live with yourself? You should just cash in your chips and jump off the Golden Gate Bridge! Positive Thoughts (played by you): I used to think like that, too, but once I realized how flawed I really was, I decided to lower my standards. In fact, I dropped them way down. And to tell you the truth, I've felt so relaxed and happy ever since. And another funny thing happened. I've become so much more creative and productive because I don't worry about your constant criticisms any more. Negative Thoughts (played by your patient): Well, that's shameful. Positive Thoughts (played by you): You're absolutely right. I'm a pretty shameful guy! I hope you'll try the Externalization of Voices with a friend or colleague. You'll see that the Acceptance Paradox is far more challenging than it looks. Practice will be necessary if you want to use this powerful therapeutic tool in your clinical work. In fact, you won't be able to bring this technique to life for your patients until you've brought it to life for yourself. You should expect to stumble quite a few times before you "get it," but you'll find that it's well worth the effort. The Acceptance Paradox has been life-changing for me personally, and it's one of the best gifts we can share with our patients.
Chapter 21
699
Visual Imaging Techniques Cognitive therapists don't simply focus on the kinds of negative thoughts that patients record on their Daily Mood Logs, like "I'm a loser," but on perceptions in general. Perceptions exist on many different levels, including the pictures and images that flow across our minds. Strong emotions are often embedded in these pictures. For example, when you visualize something positive, like holding your baby in your arms for the first time, you may feel a sense of joy and pride. By the same token, when you visualize something negative, like a horrifying automobile accident or an episode of sexual abuse you endured when you were young, the pictures in your mind's eye may trigger strong feelings of anxiety, depression, shame, or anger. The mental pictures aren't always memories of traumatic events that happened in the past. Sometimes, patients visualize frightening things that might happen in the future. A man with agoraphobia and panic attacks was afraid to leave home alone because he pictured himself losing control and freaking out when he was standing in line at the grocery store or sitting in a movie theater. Just as patients can use cognitive restructuring techniques to modify negative messages, like "I'm a loser" or "I'll never get better," they can learn to change the upsetting pictures in their minds. In this section, I'll describe Time Projection, Humorous Imaging, and Cognitive Hypnosis. These imaging techniques can be helpful for feelings of depression, anxiety, or anger. In the section on Cognitive Exposure Techniques on page 848, I'll describe Cognitive Flooding, Image Substitution, and Memory Rescripting. These imaging
Chapter 21
700
techniques are primarily used in the treatment of anxiety. 22. Time Projection Patients who are struggling with painful memories can close their eyes and project themselves into the past, so they can confront the memories or have dialogues with the people who abused them. This is called Past Projection. For example, a woman who was abused by her father when she was a child could imagine that she was eight years old again, and having a conversation with him. This will give her the opportunity to tell him all the things she never had the chance to say when she was growing up. She might want to tell him how hurt, rejected and terrified she felt when he abused her. She could tell him that the pain was especially devastating because she loved him so much, and desperately wanted his love and support. This procedure often leads to a cathartic outpouring of emotions that have been bottled up for years. Dr. Jaime Galindo has developed a role-playing version of this technique that he's used successfully in his "Forgiveness Workshops." The participants are typically individuals with a history of depression and childhood abuse. He has them pair off in twos. One of them plays the role of the abusing parent, and simply listens without speaking, while the one who has been abused has the chance to talk. Dr. Galindo emphasizes the importance of framing the conversation in a loving manner, along the lines I described in the last paragraph, rather than in a hateful or vengeful way. Many participants have told Dr. Galindo that they made far more progress during these one-day workshops than they'd experienced in many years of conventional therapy.
Chapter 21
701
Patients can also project themselves into the future. One of my Stanford residents, Dr. Caroline Little-Cribari, used Future Projection in her work with a mistrustful, bulimic young woman named Nancy. Nancy had been depressed for years, and the treatment seemed to be going nowhere. She refused to do any homework between sessions and wasn't making any progress on her bulimia or depression. Dr. Little-Cribari encouraged Nancy to close her eyes and imagine she was taking a trip several years into the future, so she could have a conversation with her future self who has recovered and now feels happy and joyful. Nancy crossed her arms defiantly and said the idea sounded totally stupid. She insisted that she'd never recover, and that this technique would be a total waste of time. Dr. Little-Cribari gently urged her to give it a try anyway, so Nancy reluctantly closed her eyes. Dr. Little-Cribari told her to imagine that the recovered Nancy was standing in front of her, and that she could talk to her. Nancy began to explain her how worthless and defeated she felt. Suddenly, Nancy started sobbing, displaying the vulnerability that she'd been hiding from Dr. Little-Cribari. After she'd cried for a while, Dr. Little-Cribari encouraged her to take the role of her recovered self and talk to her current, depressed self in a compassionate, encouraging way. The moment Nancy began to talk, she began crying again. At the end of the session, she thanked Dr. Little-Cribari and said that it was the best session they'd ever had. The next week, Nancy reported that she'd
Chapter 21
702
stopped purging and had done her psychotherapy homework for the first time. In this case, the visual images opened up a floodgate of emotion that Nancy had been struggling to suppress, and allowed her to form a more meaningful bond with her therapist. 23. Humorous Imaging Humorous Imaging can sometimes help patients who feel anxious or angry. A shy woman named Nadine often noticed an attractive single attorney in her apartment building, but felt so self-conscious that she was afraid to talk to him or even make eye contact. I suggested she might try flirting with him the next time she ran into him. Nadine said she'd love to do that, but felt too nervous. She was afraid she'd seem awkward or needy and turn him off. I suggested that when she was talking to him, she could look directly into his eyes and imagine that he was defending a case in court in his underpants. This might lighten her mood and make him seem less intimidating. Nadine was intrigued by this idea and decided to give it a try, even though she was still pretty anxious. The next day, she ended up alone with him in the elevator and decided to take the plunge. She gazed into his eyes and commented on what a neat tie he was wearing. At the same time, she pictured him prancing around the courtroom in his underwear. She began to giggle, and no longer felt intimidated. He asked what she was giggling about, and they had a lighthearted conversation. He seemed flattered and asked her for a date. Humorous Imaging certainly wouldn't be appropriate for every patient.
Chapter 21
703
Nadine was attractive and had a good sense of humor, so it seemed like the technique would probably be effective for her. But if it doesn't strike the patient's funny bone, it clearly won't be helpful, and the patient may even feel like you're making fun of them or trivializing their concerns. If so, other techniques will be far more effective. 24. Cognitive Hypnosis I'm always looking for innovative new techniques that will provide new windows into the psyches of our patients. Recently, my Stanford residents and I have been exploring the integration of CBT and hypnosis. Dr. Jose Maldonado, a colleague at Stanford with expertise in hypnosis, has been demonstrating some of the latest hypnotherapy methods at my Wednesday evening psychotherapy seminar. He emphasizes that if the patient is suggestible, you can administer virtually any type of psychotherapy technique under hypnosis. The only difference is that the therapy may progress more rapidly because you'll have a more direct access to the thoughts, feelings, and motivations that are submerged in the patient's subconscious mind. Of course, hypnosis itself is not therapeutic. The effectiveness of the therapy will result from the way you work with the patient, whether or not you've induced a trance. Furthermore, your effectiveness as a hypnotherapist will depend entirely on your skill as a therapist in general. If you're an outstanding psychotherapist, you'll probably be an excellent hypnotherapist. The use of hypnosis may boost your effectiveness with some patients, but hypnosis won't transform an ineffective therapist into an effective one.
Chapter 21
704
Most experts agree that at least one-third of the population can be hypnotized fairly easily. Individuals with anxiety disorders, dissociative disorders, and psychosomatic problems tend to be the most hypnotizable. However, OCD is a notable exception to the rule. Most OCD patients are difficult to hypnotize. Psychotic individuals are also difficult to hypnotize, along with individuals who are intoxicated or taking sedative agents, such as benzodiazepines. Depressed patients tend to be somewhat less hypnotizable than average, at least when they're depressed. Mistrust of the therapist, as well as performance anxiety, will reduce a patient's capacity to be hypnotized. Before you attempt hypnosis, find out if the patient has an interest in this approach. If the patient is not enthusiastic, I'd use other techniques instead. If, on the other hand, the patient is receptive to the idea, you can assess his or her suggestibility with one of the following brief tests: Pendulum Test. Ask the patient to hold a 10-inch piece of string with an object, like a key or crystal, attached at the end. Tell the patient to stare at the object without trying to move it. Suggest that the object will begin to swing back and forth, like a pendulum. Back and forth, back and forth. Tell the patient not to do anything to cause the object to swing, because it will start to swing on its own. Suggest that this will be surprising to the patient. Once the pendulum starts swinging back and forth, tell the patient that it will begin to change direction and start swinging forward and backward instead. Tell the patient not to make any conscious effort to influence the motion of the object, since it will change directions entirely on its own.
Chapter 21
705
If this suggestion is successful, tell the patient that the object will begin to change direction again. Now it will start swinging around in circles. Remind the patient not to influence the object, since it will change directions on its own. Afterwards, you can congratulate the patient for a job well done and ask him or her to describe what the experience was like. You can score up to two points for each of the three types of pendulum movement, so the total score will range from 0 (no movement at all) to 6 (strong movement following all three suggestions). I've included a scoring sheet for the Pendulum Test below. The interpretation of the score is somewhat subjective, but scores of 5 or 6 usually indicate a high level of suggestibility. Scoring the Pendulum Test Type of Pendulum Motion
No Motion (score 0)
Some Motion (score 1)
Strong Motion (score 2)
1. Left-right 2. Forward-backward 3. Circular Total Score
If the patient protests and says that the test seems foolish, you can stop and process these feelings with the patient. Remember that empathy is always the best response to any form of resistance. Find out how the patient feels, and what she or he is thinking. The patient may be trying to tell you that hypnosis is not for them. If so, drop it and use a different approach. Hypnosis is not for
Chapter 21
706
everyone, and there's never any reason to push a technique on a reluctant patient. Falling Test. Ask the patient to stand with their feet together, like a soldier standing at attention, and to stare at a spot on the ceiling about three feet in front of them. Stand behind the patient, and put your hands about an inch away from the patient's face, with your palms facing the patient's cheeks, so the patient can see your hands in their peripheral vision. Say something like this while you slowly move your hands backwards: "As you stare at the spot on the ceiling, you'll begin to notice an urge to fall backwards, and you will find yourself falling backwards. You will feel a force coming from my hands, like a magnetic force, pulling you backwards, and you will fall backwards. Don't worry, because I will catch you as you start to fall, so you are perfectly safe. You are falling backwards. A force is pulling you backwards, and I will catch you. You do not need to be afraid. A force is pulling you backwards." Most individuals will begin to teeter back and forth, and many will suddenly fall backwards. Catch the patient after they've fallen backwards about six inches. Don't let them go crashing to the floor! The patients who fall the most rapidly will be the most hypnotizable. This test assesses not only the patient's capacity for hypnosis, but also whether the patient trusts the therapist. Eye Closure Test. Ask the patient to sit in a chair and stare at a spot on the wall several feet above the level of their eyes. Tell them that you'll count backwards from five to one, and that at each number, they will close their eyes
Chapter 21
707
and slowly open them again. Then say, "Five, slowly close and open your eyes." Explain that while you're counting, their eyes will get heavier and heavier, heavier and heavier, and it will become harder and harder for them to open them. You can say things like this: "Four. Close them and open them again. Notice that they're starting to get heavy now, heavier and heavier, heavier and heavier. It is getting harder to hold them open. You will notice that they really want to close. You are starting to feel sleepy and relaxed, sleepy and relaxed. "Three, close them . . . and open them. Notice how heavy and sticky your eyelids are getting. Heavy and sticky. It's getting harder and harder to open them. Your eyelids feel like heavy lead weights. It is SO HARD to keep them open. "Two, close them … and open them. They're getting heavier and heavier, heavier and heavier. Notice how hard it's getting to open them back up. They are sticky and heavy, and really want to stay closed. When I get to zero, they'll be so heavy that you won't be able to open them at all. "One, close them and open them again. They are getting heavier and heavier. SO heavy, SO tired. "Zero. Now your eyes will close, but they will not open. You may try, but you'll find that you cannot open your eyes. Try to open them. Notice how heavy they are, and how they will not open, no matter how hard you try."
Chapter 21
708
Most patients will wrinkle their forehead muscles and try to open their eyes, but most will be unable to open them. Now you can say: "You feel so peaceful and relaxed, as you sink deeper and deeper, deeper and deeper, resting comfortably. Notice how peaceful and relaxed you feel. You eyes will not open until I count to three. "You're doing a great job. Now I'm going to count to three. On the count of three, you'll suddenly discover that your eyelids no longer feel sticky and heavy, and you'll be able to open them easily. You'll wake up feeling totally refreshed, and you can tell me what this experience was like for you. One, two, three." Now you can process the experience with the patient. Did they try hard to open their eyes? How did their eyes feel? How did the experience feel? Was it pleasant? How deeply relaxed did they feel, on a scale from 0 (not at all relaxed) to 10 (deeply relaxed). Did they feel anxious or surprised at any point? Hand Flotation Test. Ask the patient to sit in a chair with both feet on the ground and both hands resting comfortably on the arms of the chair. Tell the patient to roll their eyes back in their head, as if they were staring at the inside of their skull. Tell them to face directly ahead, so that their eyes are forced to the top of their sockets, and you can see the whites of their eyes. Some patients will make the mistake of tilting their heads back, rather than rolling their eyes. Tell them, instead, to roll their eyes up and back in their sockets without tilting the head, as if they were staring at the top of their skull. If needed, ask them to watch while you demonstrate.
Chapter 21
709
Once their eyes are rolled back in their sockets, tell the patient to take a deep breath. Now they can slowly exhale while closing their eyes. Once their eyes are closed, tell them to relax deeply and concentrate on the sound of your voice. Tell them they are going deeper and deeper, deeper and deeper, and that nothing with bother them or awaken them. Tell them that if they hear any distracting sounds, like sound from the outdoors, they can gently bring their mind back and concentrate on your voice again. Now tell them to concentrate on their left hand, and suggest that they may begin to notice involuntary movements in their fingers as well as tingling sensations in their hand and arm. Touch one of their fingers and gently stroke the back of their hand while you say this.* Now tell them to notice how light and floaty their hand feels, light and floaty, like a balloon. Tell them it will begin to feel so light that it will actually begin to float up into the air on its own, with no effort on their part, almost as if it's no longer a part of their body, but has a mind of its own. Tell them it's getting lighter and lighter, lighter and lighter, and wants to float right up into the air. If their hand fails to elevate, tell them that you are going to help them get started. Gently raise their hand, with their elbow still resting on the arm of the chair, and say, "Notice that your hand feels light and floaty, like a balloon, and you feel so peaceful and relaxed. All you will hear is the sound of my voice." Once the hand is floating, tell the patient that you are going to ask them to
Chapter 21
710
open their eyes when you count to three. They will feel completely awake and refreshed, and will describe the experience. You can say, "However, your left hand will continue to float until I touch your elbow, like this." Now, touch their left elbow, so the post-hypnotic suggestion will be clear. You can also say, "Until I touch your elbow, you will notice that your left hand will always want to keep floating in the air, on its own, because it will feel light and floaty, like there's a helium balloon attached to it. If I push it down, it will just float right back up into the air." Now count to three. When patients open their eyes, ask them to describe the experience. What was it like? How did it feel? You can ask five questions to determine their score on the Hypnotic Induction Profile (HIP) on page 712: 1. Dissociation. "Does your left hand feel like it's not as much a part of your body as the right? In what way? Does it feel like it's not connected to your wrist?" Score 2 points if the answer is a definite yes, and 1 point for maybe. 2. Post-hypnotic levitation. Now gently lower the patient's left hand to the chair and say, "You will experience something surprising now." Score 2 points if the patient's hand floats up from the arm of the chair again. If the hand does not float spontaneously, you can say, "Notice that your left hand is feeling light and floaty again, like there's a helium balloon attached to it. You will notice that it is starting to float up in the air again, even though you're not trying to raise it." If the hand floats now, score 1 point. If there's no movement in the hand or * If you're concerned about an ethics violation, or a misunderstanding of your motives by the patient, avoid touching the patient. This aspect of the procedure is controversial, and probably unnecessary.
Chapter 21
711
fingers, score 0 points. 3. Control differential. If the left hand fails to float, manually elevate it and ask the patient to voluntarily raise their right arm as well. Now ask them to make a fist with both hands. Ask if they have a greater sense of control in their right arm, and whether there's any difference in their sense of control of their two hands. Score 2 points if they report a diminished sense of control in the left hand and arm, 1 point for maybe, and 0 points if there's no difference at all. 4. Cut-off. Now tell the patient that you're going to lower both of their hands to the arms of the chair. While you do this, touch the patient's left elbow in the same way you did earlier, when you gave the post-hypnotic suggestion. Ask if the left arm and hand feel normal again, and whether they now have a full sense of control in their left hand and arm. Score 2 points if the left and right arms both feel normal again, and 1 point if there's been a change, but a difference still exists. Score 0 if the patient still has a diminished sense of control in the left hand.* You can also ask them what happened, and why their sense of control in their left arm is suddenly normal again. Some patients will not remember that you just touched their elbow, and will not realize that they just responded to a posthypnotic suggestion. Amnesia to the post-hypnotic suggestion does not formally increase the patient's score on the Hypnotic Induction Profile, but will provide you
* The psychometric properties of this test probably have not been adequately investigated. You could argue that if the patient still has a diminished sense of control in the left hand after you touch his or her elbow, this might actually indicate a high degree of suggestibility. For example, the patient may not have comprehended the post-hypnotic cut-off suggestion, so their left hand may still feel different from their right.
Chapter 21
712
with interesting information about how the patient is processing the experience. Patients who cannot recall why their sense of control returned are usually more suggestible. 5. Floating sensation. You can ask, "Did you notice any different kinds of sensations in your left hand and arm when it was floating? What were they like? Did one arm feel heavier than the other? Warmer or colder? Did you notice any tingling sensations, or feelings of numbness, in your left hand or arm? Did any of those sensations spread to the rest of your body?" Score 1 point if the patient describes different sensations in the left hand or arm, and 2 points if these sensations spread to other parts of the body. Hypnotic Induction Profile (HIP) Test
Yes (score 2)
Maybe (score 1)
No (score 0)
1. Dissociation 2. Post-hypnotic levitation 3. Control differential 4. Cut-off 5. Floating sensation Total score
The total HIP score can vary between 0 and 10. Scores of 9 or 10 indicate extremely high hypnotizability, and scores of 7 or 8 indicate reasonably high hypnotizability. However, you will have to use your own common sense when
Chapter 21
713
you interpret the HIP score. For example, if the patient has difficulties understanding what the hypnotist is saying, or isn't fluent in English, this may cause a false lowering of the HIP score. Similarly, if the hypnotist is inexperienced and administers the test in a vague or confusing manner, the patient may have trouble understanding some of the hypnotic suggestions, and the score will be misleading. If your suggestibility test indicates that the patient is a suitable candidate for hypnosis, you can induce a trance quickly using a variety of techniques that are similar to the suggestibility tests you just administered. For example, you can tell the patient to roll their eyes back in their head, take a deep breath, and let the air out while slowly closing their eyes. You can remember this as the 1, 2, 3 hypnotic induction procedure, and it works like this: Step 1. Roll your eyes back in your sockets. Step 2. Take a deep breath. Step 3. Let your eyes close while slowly exhaling. This induction procedure takes less than 60 seconds and will be sufficient to induce a trance in suggestible individuals. After you induce the trance, you can use induce a deeper trance with suggestions like this: "Notice that you're feeling deeply relaxed and peaceful now. Nothing will bother you. Your entire body feels so peaceful and relaxed. You are going deeper and deeper. Concentrate on the sound of my voice. Deeper and deeper. Notice that your breathing is getting deeper
Chapter 21
714
and slower, even though you make no effort to change the way you are breathing. Deeper . . . and deeper." Most patients will appreciate the chance to unwind and immerse themselves in a deeply relaxed and peaceful mood. This creates the expectation that the hypnotic experience will be safe and rewarding. Now tell the patient to visualize a peaceful scene where they feel happy and deeply relaxed. Ask them to signal by moving their left index finger when they have the scene in mind. It can be any real or imagined scene with positive associations in their mind. Once their finger moves, ask them to describe the scene. Where are they? What does it look like? A woman named Laura described this scene during a hypnotherapy induction at one of my Wednesday evening seminars: Laura: I'm standing on the end of a pier at a lake near where I grew up. I'm ready to jump in and swim. It's so beautiful. The sunset is gorgeous. It feels so peaceful here. Dr. Maldonado: Would you like to jump in and take a swim? Laura: Yes. Dr. Maldonado: Go ahead and jump in. Take a swim and tell me what the water feels like. Laura seemed delighted. She said that the water was cool and refreshing, and that she could feel the gentle waves under her head, just as real as if she were really swimming. While she spoke, she tilted her head backwards, and it seemed to bob, as if she really were floating in a lake.
Chapter 21
715
Laura had been under a lot of stress, due to pressures at work and tensions at home. Dr. Maldonado asked if she felt any different, floating in the lake, from the way she'd been feeling recently. She said, "This is weird. I feel so different. I feel incredibly happy and peaceful. I can see the sky and the clouds, and the water feels refreshing and cool." Then Dr. Maldonado said, "You will always feel happy and peaceful here in your special place. You can come back to this spot at any time you want, and you'll feel deeply relaxed and peaceful again. This is your secret place, and it will always be here for you." Once you've established a safe and peaceful place for the patient, you can use it throughout the hypnotherapy session in a variety of ways. For example, if the patient begins to feel overwhelmed by painful or frightening memories, you can suggest that she or he can return to the special place and feel safe and deeply relaxed again. You can deepen the trance by saying something like this: "As I count from five to zero, you will go deeper and deeper, deeper and deeper. Five. You are feeling more and more relaxed, free of all worries. Every muscle feels relaxed and limp as you allow yourself to sink deeper and deeper. "Four. You are going deeper and deeper. You will find that your head feels heavy, and your neck muscles feel limp and relaxed, so your head will nod forward until your chin rests on your chest. Even though you will make no effort to change your breathing, you will notice that you
Chapter 21
716
are breathing more and more slowly and deeply, slowly and deeply, and you will feel so peaceful and relaxed. "Three. As you focus on my voice, you will notice that nothing will bother you. Concentrate on my voice. If your mind drifts away, simply bring it gently back to the sound of my voice. You feel safe and relaxed, peaceful and happy. "Two. You are going deeper and deeper, deeper and deeper. It is so beautiful here. You can see the blue sky, the tall trees, as you lie in your hammock in the woods, and you can feel the cool breeze on your face as you go deeper and deeper, deeper and deeper. "One. You feel so peaceful and relaxed. Nothing will bother you. Every muscle feels limp and heavy. Your breathing is slow and deep. You can see the air moving in and out of your nostrils with each breath, like a white fog, as you sink deeper and deeper, deeper and deeper. "Zero. You are deeply asleep. You feel so peaceful and relaxed. Nothing will bother you. At times we will talk, and I may even ask you to open your eyes, but you will continue to feel very peaceful and relaxed, and nothing will bother you." Once you've induced the trance, you can use a wide variety of CBT techniques. Of course, you can use any of the Visual Imaging Techniques or Cognitive Exposure Techniques, since these techniques essentially are hypnotic techniques without the trappings of the hypnotic induction. You can also use Role-Playing Techniques, Uncovering Techniques, Motivational Techniques and
Chapter 21
717
others. Your choice of techniques will depend on the nature of the problem you're working on, and your skill as a therapist. One popular hypnotic technique is called the Split Screen. Tell the patient to return to the peaceful scene where they feel safe and deeply relaxed. It might be any real or imagined scene with positive associations in their mind, such as a cabin in the woods or lying in a hammock in a beautiful garden. Once they've visualized the scene, tell them that they'll discover a screen nearby, like a movie or television screen. The screen might even be a piece of the scenery, such as a large, flat rock or a portion of the sky. Tell them that they can project various kinds of images and experiences onto the screen, so they can watch them, in much the same way that they might watch a movie. For example, if they have a phobia, like the fear of flying, ask them to visualize what it would be like to be on a plane, feeling terrified. If they have a driving phobia, you can ask them to describe what they fear the most, such as losing control and causing a terrible accident while driving on a bridge or freeway. You can quickly elicit their worst fear by saying, "Tell me what you're the most afraid of. What's the worst thing that could happen? You can visualize it on the screen and tell me what you see." This is simply a version of the What-If Technique, one of our four Uncovering Techniques. Once the patient describes the fantasy, you can ask, "And then what would happen? What do you fear the most? What's the worst thing that could happen now?" Alternatively, you could ask, "What does that mean to you? Why would that be upsetting to you?" These questions will often elicit additional fears,
Chapter 21
718
and will allow the patient to explore the meaning of the event that's so painful to them. If they become overwhelmed with anxiety, tell them that they can sweep the upsetting scene—such as the image of an airplane crash or the fantasy of losing control while driving—to the left half of the screen and project a positive, reassuring scene on the right. For example, a patient with a fear of heights can visualize herself at some time in the future, when she can climb ladders and hike along mountain trails with no fear at all. Once she pictures this scene, tell her to describe it for you. What does she see? What has changed? You can also ask if she feels more relaxed, and if her fear has diminished. Then you can suggest that her subconscious mind will find a way to master the fear, and that she'll progress forward, step by step, until she's achieved her goal. You will recognize this as Image Substitution, a Cognitive Exposure Technique. The only difference is that the patient is in a trance, so the visual images will be more vivid and the effect may be more intense. You can also use Affective Dissociation. Tell the patient that they can describe the feelings of the person in the scene who feels frightened, hurt or humiliated, just as if they were watching an actor in a movie, but they won't actually feel those feelings themselves. There are several other types of safety nets you can use when patients visualize frightening fantasies or traumatic events. Ask them to tell you or signal you by moving their left index finger if they begin to feel overwhelmed. Then explain that they can simply turn the frightening movie off by flicking a switch,
Chapter 21
719
and they'll find themselves back in the idyllic scene again, feeling peaceful and relaxed. Once they visualized the scene and feel deeply relaxed, remind them that they can return to this safe place anytime they feel overwhelmed and need relief, even when they're not in a hypnotic trance. Memory Rescripting can help patients restructure their memories of painful events. A woman with PTSD who has memories of being raped or abused may want to enter the scene of the trauma and talk to herself in a comforting, reassuring way, just as a loving parent might have done. A man with a phobia can enter the frightening fantasy as a recovered, confident adult and tell the frightened self why he no longer needs to be afraid of the thing that's been bothering him. When patients describe frightening fantasies or phobias, you can use Affect Bridging to activate memories of partially forgotten traumatic experiences that may have occurred at an earlier time in their lives. Then you can explore these memories and their meaning to the patient, just as you might if you were not using hypnosis. One of my residents used Affect Bridging to help a woman with a bridge phobia. While she was in a trance, he asked her to imagine driving across a bridge. She visualized a bridge near San Francisco and suddenly became frightened. Then he asked if she could recall the first time she felt frightened when crossing a bridge. She remembered riding over a winding mountain road with her uncle when she was young. They had to cross several bridges over deep canyons, and he seemed to be driving too fast. She asked him to slow
Chapter 21
720
down, but he ignored her and kept speeding along. She panicked, and ever since then, she'd had feelings of panic and helplessness whenever she had to cross bridges. In retrospect, she could see that she was angry with her uncle because he was ignoring her requests to slow down, but she'd never expressed those feelings or even realized that she was feeling that way. Of course, every technique has its downside, including hypnosis. One danger is that you may inadvertently create false memories that the patient cannot distinguish from valid memories. For example, suppose that you regress a patient to age 8, and he tells you that he feels frightened in the hallway of his grammar school. You might ask, "Who are you afraid of?" In this case, you've given him the suggestion that there's someone there, so he may concoct a story about some frightening person in order to comply with your hypnotic suggestion. In fact, he may not have been afraid of anyone at all. A better question would be, "Can you tell me what you're afraid of? What thoughts and pictures come to mind?" Although hypnotherapy really shines with individuals suffering from anxiety, it can be helpful for depression as well. The Library Technique is a hypnotic version of the Daily Mood Log. Tell the patient that they're going to visit a special library with two kinds of books. The bookshelf on the left is filled with negative, frightening books, like "The Book of Rape" and "The Book of Worthlessness." In contrast, the bookshelf on the right is filled with positive, joyful books, like "The Book of Happiness" and "The Book of Self-Esteem." Tell them to take a book from the negative bookshelf first. When they open it, they'll be
Chapter 21
721
surprised to discover that it's all about them, and contains amazingly accurate descriptions of all their most private and hurtful negative thoughts and feelings about themselves and their lives. If you've been working with the Daily Mood Log, you'll already know what kinds of thoughts they have. For example, if they were raped or abused when they were young, they may see sentences like, "It was all my fault. I was a dirty little girl. If anyone knew what happened to you, they'd think you liked it." If they're struggling with acute or chronic depression, they may see sentences like, "I've totally screwed up my life. Things will never change. My problems are hopeless." Tell them to read out loud from the book, and to tell you how the sentences make them feel. Now tell them that they can destroy the negative book so it will no longer affect them. They can bury it, put it in a gigantic paper shredder, or throw it into a fire and watch it burn. Once they've destroyed it, you can tell them to walk to the positive bookshelf, where they'll find another book about themselves. This book contains joyful, positive messages, like, "You're a worthwhile, loveable human being. The abuse wasn't your fault. If anyone knew what happened to you, they'd give you lots of love and support." Ask them to read out loud from this book, and to tell you how they're feeling now. You may recognize this as a hypnotic version of the Straightforward Technique, because patients come up with positive thoughts that put the lie to their negative thoughts. The Straightforward Technique isn't usually very helpful, particularly with severely depressed individuals; however, when patients are in a trance, they'll have a better chance
Chapter 21
722
of coming up with effective positive thoughts. Cognitive Hypnosis can also be used as a powerful motivational tool for habit modification. Let's say that your patient, Manuel, wants to quit smoking. After you've induced a trance, ask Manuel to picture himself in a beautiful, peaceful place, as described previously. One he's deeply relaxed, you can talk to him along these lines: "Manuel, lots of people try to change bad habits by scolding themselves or by focusing on all the negative consequences of the habit they're trying to overcome. For example, you might tell yourself that you'll end up with lung cancer if you keep smoking. However, these scare tactics usually don't work very well, because you'll feel so anxious and demoralized that you'll reach for another cigarette. "The subconscious mind works differently, because all human beings tend to pursue things that they really want. So the trick is to focus, instead, on the benefits of becoming a non-smoker. I want you to describe all the benefits of becoming a non-smoker. Tell me about all the good things that will happen in your life after you quit. I'll list all the advantages you describe, and help you word them in a positive way. "For example, you wouldn't want to tell yourself, 'If I quit smoking, I won't get lung cancer,' because this statement is iffy and negative. Instead, you can tell yourself, 'When I become a non-smoker, I'll have healthy lungs and greater stamina.' This positive message will be far more relaxing and motivating, and you'll find yourself naturally moving
Chapter 21
723
toward this goal because it's something that you really want." While Manuel describes all the benefits of becoming a non-smoker, list them for him on a piece of paper. He may include benefits like these: I'll have fresh breath. I'll have better stamina. It will be easier to exercise so I can get in shape. I can save money. I can tell people that I've quit, and feel proud of myself. I'll have greater self-esteem, because I can tell myself, "I really did it!" I'll have a healthy heart and lungs. I'll be able to walk up stairs without huffing and puffing. People will be more attracted to me, and they won't be put off by the secondhand smoke. I'll live longer and enjoy my life so much more! Each time Manuel mentions a benefit, ask him to visualize it while you add it to the list. For example, when he says, "I'll be able to walk up stairs without huffing and puffing," ask him to picture himself walking up the stairs at his apartment feeling filled with energy and a sense of pride. Tell him to signal you with his right index finger when he can see himself walking up the stairs easily and briskly. Ask him how he feels when he visualizes this scene. Once you've listed all the benefits Manuel can think of, read the list to him out loud, and ask him how strongly he wants these advantages on a scale of 0 to
Chapter 21
724
10. Then ask him to indicate when he wants these benefits to begin. Tell him to signal you by moving his right index finger if he wants to become a non-smoker immediately. Alternatively, he can move his left index finger if he wants to become a non-smoker later on, and both index fingers if he feels unsure about when he wants to become a non-smoker. If he moves his right index finger, indicating that he wants to quit immediately, tell him that after you awaken him from the trance, he'll discover that his desire for cigarettes has diminished or disappeared entirely. Tell him that he'll frequently picture all the benefits of becoming a non-smoker, and that this will make him feel happy and peaceful. Tell him that before he leaves, you'll give him the list of benefits so he can put it in a visible place at home, such as on his refrigerator or desk. In addition, you can give him the post-hypnotic suggestion that every night before he goes to sleep, he will return to his safe, peaceful place and focus on all the benefits of being a non-smoker. Now tell him that you will awaken him from his trance by counting to 3, and that on the count of 3, he'll open his eyes and feel refreshed and relaxed, and describe what the hypnotic experience was like. If, in contrast, he tells you that he wants the benefits later on, or he's unsure of when he wants to quit, tell him that's fine, and that you'll awaken him on the count of 3. Suggest that when he opens his eyes, he'll feel peaceful and relaxed, and describe what the experience was like. When he's awake, you can discuss his ambivalence. Remember that when patients resist, empathy is always your best tool. In addition, the decision
Chapter 21
725
to quit smoking has to be his agenda, and not yours. Rather than viewing the hypnosis as a failure, I would say that you've discovered that Manuel still has pretty strong mixed feelings about giving up his habit, and you can process these feelings with him. I first learned about the use of hypnosis for habit modification during my psychiatric residency training. The instructor at one of our seminars induced a trance in the group, and asked all of us to focus on a bad habit we wanted to modify. I wasn't really convinced I was hypnotized, but felt relaxed and chose smoking, since I'd been smoking for a couple years and had been thinking about quitting. Following the induction, I never again had any desire to smoke a cigarette, and never had any withdrawal symptoms either. I've used the same technique with a number of patients over the years, and it's been effective about 50% of the time. For a brief, one-shot intervention, this seems like a reasonably good batting average. The integration of CBT and hypnosis is relatively new territory, and more research will be needed to shed light on basic questions such as: Which patients or problems are the best candidates for hypnotherapy? Will hypnotherapy boost the effectiveness of conventional CBT techniques? Conversely, will CBT boost the effectiveness of hypnotherapy techniques? Is hypnotherapy contraindicated for some patients? Keep in mind that this is not intended to be a comprehensive review of Cognitive Hypnosis, but simply an overview to help you get started. If you're interested in learning more about this approach, you can consult textbooks,
Chapter 21
726
attend workshops that focus on cognitive hypnotherapy, and practice with your own patients. Hypnotic techniques will not appeal to every therapist, and many patients will not be good candidates for hypnosis. The potential strengths and weaknesses of Cognitive Hypnosis are intertwined. On the one hand, it's less rational and more magical than many other CBT techniques. This will appeal to some people. After all, the mental health profession evolved from the work of shamans and spiritual healers. Perhaps we should try to re-establish those roots to some extent. On the other hand, some therapists have told me that they gave up using hypnotic techniques once they learned about CBT. They preferred CBT because it taught active coping skills and made patients responsible for solving the problems in their lives. I can see both sides of the argument, and don't feel strongly one way or the other. To me, the effectiveness of these methods is a scientific question that can only be answered by testing and measurement. If these methods help some refractory patients who haven't responded to other techniques, or work much more rapidly than other techniques, then I would say they deserve a place in our therapeutic armamentarium.
22*
Uncovering Techniques
We're not only interested in helping patients feel better in the here-andnow, but in uncovering the root causes of their problems. The goal of the Uncovering Techniques is not so much to change the way our patients feel, but to find out why they got upset in the first place. Cognitive therapists believe that Self-Defeating Beliefs (SDBs) can trigger individual mood problems, such as depression and anxiety, and interpersonal problems, such as anger and conflicts in the patient's relationships with family, friends, and colleagues. Cognitive therapists also believe that a modification of the patient's belief system can facilitate recovery and help prevent relapses following recovery. This theory is controversial, and not all investigators have been able to confirm the hypothesized causal links between SDBs and emotional problems (Burns and Spangler, 2001). Still, the theory is intuitively appealing, and it can be helpful clinically because patients will suddenly comprehend why
2003 by David D. Burns, M.D.
Chapter 22
728
they have a tendency to get depressed or anxious. SDBs also explain the precise timing of dysphoric episodes in an elegant fashion. For example, if you believe that your worth as a human being depends on your intelligence, productivity, and achievements, you'll feel good as long as you feel successful, but you may be vulnerable to feelings of depression and anxiety whenever you fail or fall short of your goals. Or, if you tell yourself that people should always be the way you want them to be, you may get excessively frustrated and angry when people don't behave in the way you expected. According to this theory, an SDB, such as "I can't feel happy and worthwhile unless I'm loved," plus a negative event (e.g. rejection), causes distorted negative thoughts, such as "I'm unlovable. It was all my fault. I'll be alone forever." These thoughts instantly trigger feelings of depression, worthlessness, and hopelessness, which lead to more negative thoughts. There are two basic categories of Self-Defeating Beliefs: Individual SDBs and Interpersonal SDBs. Individual SDBs make us vulnerable to bouts of depression and anxiety. They're usually "self-esteem equations" because they tell us what we need to have or do in order to be worthwhile human beings. The basic formula is, "I must have X in order to feel happy and fulfilled." X could be intelligence, success, productivity, perfection, love, or approval. In other words, patients may base their self-esteem on their achievements, on being perfect, on being loved, or on getting other people's approval. In contrast, Interpersonal SDBs are expectations about what will happen in intimate relationships. These beliefs shape the patient's understanding of what
Chapter 22
729
other people will be like, as well as what they have to do to win other people's love and respect. They also influence the patient's understanding of conflicts in their relationships with other people. Here are a few examples of Interpersonal SDBs: Blame. You believe that others are to blame for the problems in your relationships with them. Truth. You believe that there is one correct way to view the situation, and feel overwhelmingly convinced that you're right and the other person is wrong. Entitlement. You believe that other people should meet your expectations. When they don't, you feel angry and frustrated. Perceived Perfectionism. You believe that you must impress others with your talent or accomplishments to get them to accept you. You believe that people wouldn't love or respect you if they saw that you were flawed and vulnerable. Narcissism. You believe that people should always cater to you and make you feel special. Perceived Narcissism. You believe that the people you care about will always be demanding, self-centered and exploitative. Submissiveness. You believe that you have to meet everyone else's needs and expectations in order to be loved. You think you always have to please others, even if you make yourself miserable in the process. Love feels like a form of slavery.
Chapter 22
730
Conflict Phobia. You believe that anger is dangerous, and that people who love each other should never fight or argue. SDBs tend to be unrealistic, but patients usually don't realize this. That's because SDBs function as self-fulfilling prophecies, so they appear to be true even when they're not. For example, let's say that I believe most people are untrustworthy and will try to put me down. Now, let's imagine that a student raises a difficult question during a class I'm teaching. If I assume the student is an adversary, I'll feel upset and threatened, and I'll respond defensively. This will trigger more skeptical questions from the student, and from the rest of the class as well. Soon, I'll find myself at odds with everybody in the room, so my experience will appear to confirm my negative expectations. I'll feel like a victim because I won't realize that I triggered the very consequences that I feared the most. In reality, I was the puppeteer pulling everyone else's strings. In contrast, if I assume that the student is my ally, and that we're working together, I won't feel threatened, so I'll respond differently. I might say, "Wow, that's a really important question you asked, and I'm not sure I know the answer. Tell me what your thinking is. Maybe we can figure this out together." Then, when the student shares his thoughts, I can find some truth in what he's saying, and praise him for his efforts. This will make everyone in the class feel relaxed and enthusiastic, and suddenly I'll have a room full of allies. Once again, my assumption will function as a self-fulfilling prophecy. We create our own interpersonal reality in exactly this way all the time, but we're not aware that we're doing it. This is a Buddhist notion. The Buddhists
Chapter 22
731
teach us that the world is one, and that most suffering results from the assumption that there's a reality that's separate from us. This idea is easy to understand in the context of relationship conflicts. We suffer because we think that we're the victims of the other person's bad behavior. We don't realize that they're usually just responding to us, and to the role that we're projecting onto them. 25. Individual Downward Arrow The Individual Downward Arrow helps patients pinpoint Individual SDBs. You ask the patient to select a negative thought on his or her Daily Mood Log, and draw a downward arrow underneath it. The arrow is a form of shorthand for this type of question: "If this were true, why would it be upsetting to you? What would it mean to you?" Of course, if patients are doing the Individual Downward Arrow on their own, the questions would be slightly different: "If this were true, why would it be upsetting me? What would it mean to me?" These questions will trigger a new negative thought that the patient can record directly under the arrow. Then you repeat the questions, and the patient will come up with another negative thought. Once you've done this several times, you can review the list of negative thoughts the patient generated. It will usually be easy to identify the SDBs at the core of the patient's suffering. A life insurance agent named Roger was referred to me by a local neurologist because he was having problems with anxiety, especially when he was at work. I learned that Roger was the company's top salesman, and that he'd won numerous awards over the years. He also loved golf and tennis, and prided
Chapter 22
732
himself on his athletic abilities. However, Roger had experienced episodes of dizziness, stumbling and blurred vision on and off for several months. His symptoms were puzzling because they were pronounced at times, and then they'd mysteriously disappear, only to return again later. Roger's family physician suspected multiple sclerosis (MS) and arranged for a consultation with a neurologist, who confirmed the diagnosis. Of course, anyone who discovered they had MS would be understandably upset, but I was eager to find out exactly why Roger was feeling so anxious. What was he telling himself about his illness? The upsetting event on his Daily Mood Log was, "Feeling dizzy or stumbling at work." His negative feelings included intense anxiety, shame, embarrassment, and inferiority. One of the negative thoughts he recorded was, "My colleagues might see me stumble or fall." Roger actually had fallen at home on several occasions, but he'd been able to control his symptoms at work by being especially cautious and hiding his hands in his pockets whenever he started to tremble. He hadn't told any of his colleagues about his multiple sclerosis because he felt so ashamed. I asked Roger to draw a small downward arrow under his negative thought, and said, "Let's assume that your colleagues did see you stumble or fall. Why would this be upsetting to you? What would it mean to you?" Roger replied, "Then they'd find out that there was something wrong with me."
Chapter 22
733
I told Roger to record this new negative thought under the arrow on his Daily Mood Log, and to draw another arrow directly underneath it, as you can see on page 735. Then I said, "Let's assume that your colleagues did find out about the MS. What would that mean to you? Why would it be upsetting to you?" He replied, "They'd think I was weak or defective." I told Roger to write this thought down and to draw another arrow under it. Then I said, "Let's suppose your colleagues did conclude that you were weak and defective. What would that mean to you? Would that be upsetting?" Roger exclaimed, "Of course it would!" This sometimes happens when you use the Downward Arrow Technique. To the patient, it may seem self-evident that what they've just described would be a catastrophe, so they may not understand what you're driving at. If this happens, you can simply rephrase the Downward Arrow question. Here's what I said: "Roger, you're absolutely right. No one would want to have their colleagues thinking they were weak or defective, so that probably seemed like a stupid question. But at the same time, we're all unique, and we all view things a little differently. I'm wondering what it would mean to you if some or all of your colleagues concluded you were weak and defective. What is it about this that bothers you the most?" He replied, "Then they wouldn't respect me any more. They'd look down on me." I told him to record this thought on his Daily Mood Log and to put another arrow underneath it, and said this:
Chapter 22
734
"Of course, nobody would want their colleagues to look down on them. But let's assume that this happened, and all your colleagues lost respect for you because they saw you stumble and fall at work. Why would that be upsetting to you? What would it mean to you?" Roger replied, "That would mean I was worthless." You've usually completed the Downward Arrow chain when you encounter a thought like one of these: That would mean I was worthless. That would mean life was not worth living. Then I could never feel happy again. Review Roger's negative thoughts on page 735 and see if you can identify some of his SDBs. You can review the list of Common Self-Defeating Beliefs on page 1080 while you do this exercise. I always keep a copy of this list at my desk, and hand it to the patient at this point. Patients are usually intrigued by what we come up with. When you've listed a few of Roger's SDBs, you can turn to page 736. 1. 2. 3. 4. 5.
Chapter 22
735
Roger's Negative Thoughts 1. My colleagues might see me stumble or fall. Let's assume that your colleagues did see you stumble or fall. Why would this be upsetting to you? What would it mean to you? 2. Then they'd find out that there was something wrong with me. Let's assume that your colleagues did find out about the MS. What would that mean to you? Why would it be upsetting to you? 3. They'd think I was weak or defective. Let's suppose your colleagues did conclude that you were weak and defective. Would that be upsetting? What would that mean to you? 4. Then they wouldn't respect me any more. They'd look down on me. Let's assume that this happened, and all your colleagues lost respect for you because they saw you stumble and fall at work. Why would that be upsetting to you? What would it mean to you? 5. That would mean I was worthless.
Chapter 22
736
Answer Here are the SDBs that Roger and I identified: Achievement Addiction. Roger bases his self-esteem on his accomplishments. If he's successful and productive, he feels happy and worthwhile, and tells himself he's "a winner." Perfectionism. Roger believes that he must be outstanding in every way to be worthwhile. His perfectionism extends to his career, health and athletic performance. Perceived Perfectionism. Roger thinks his colleagues are very judgmental and will turn against him if they find out he's flawed in any way. He believes that he has to impress them with his success and athleticism to win their friendship, admiration, and respect. Approval Addiction. Roger thinks that he can't feel happy and fulfilled unless he gets everyone's approval. Superman. Roger thinks he's supposed to be bulletproof and superhuman, and never display any vulnerabilities or weaknesses. You can see that Roger's attitudes, and not the MS, were the real cause of his anxiety. He'd always based his self-esteem on being a success, and didn't know how to cope with the feelings of vulnerability and weakness. I wanted Roger to focus on two questions. First, were these beliefs realistic? Second, were they helpful to him? With regard to the first point, it's interesting that Roger may be selling his colleagues short in much the same way that he's selling himself short. Roger
Chapter 22
737
seems to think that the many years of friendship, loyalty and hard work they've shared don't count. You can imagine that he might also have some resentment and anger lurking under the surface. It would be pretty irritating to live in a world where people were as judgmental and critical as Roger imagines. Roger admitted that he did feel angry. With regard to the second point, it's important to realize that Self-Defeating Beliefs are double-edged swords. They have a healthy, positive side and an unhealthy, destructive side. Roger's hard work and need for approval have rewarded him handsomely. He's been one of the top salesmen in his company, and he's always been extremely popular with his colleagues and customers. But there may be a downside as well. Once Roger sees that he can't be a "winner" all the time, he may have no other basis for self-esteem. He may be convinced that he'll end up as a "loser" or a "failure," and that everyone will abandon him. Once you've identified an SDB, it can be helpful to do an Attitude CostBenefit Analysis (CBA). Ask the patient to weigh the advantages against the disadvantages of one of their SDBs. On page 738, you can see how Roger listed the advantages and disadvantages of basing his self-esteem on other people's approval. Note that he's not listing the advantages and disadvantages of getting everyone's approval, but rather, the advantages and disadvantages of needing everyone's approval. These are quite different! You'll need to keep this distinction clearly in mind when you do Attitude CBAs with your patients.
Chapter 22
738
Roger's Attitude Cost-Benefit Analysis "I need everyone's approval to be worthwhile."
Advantages of Needing Approval
Disadvantages of Needing Approval
1. I'll work hard to get people to approve of me.
1. Other people will control my self-esteem.
2. I'll respect other people and pay careful attention to what they say and how they feel.
2. I'll get upset when people criticize me.
3. I'll sell lots of life insurance and make lots of money. 4. I'll be a people person and have lots and lots of friends. 5. I'll feel great when people do approve of me.
30
3. I may try too hard and turn people off. 4. I may not know what I believe in or stand for. 5. My emotions will go up and down like a roller coaster, depending on whether or not people like me.
70
Chapter 22
739
Although there were several advantages, Roger said that the first disadvantage was a huge one. He didn't like the idea that he was giving other people the power to control his self-esteem. I asked him to balance the advantages against the disadvantages on a 100-point scale. Which list felt greater? Roger decided that the disadvantages of needing everyone's approval greatly outweighed the advantages, so he put a 30 in the left-hand circle and a 70 in the right-hand circle. I encouraged him to revise the belief so he could keep the advantages, while getting rid of the disadvantages. This is actually the Semantic Method. Here's his revised belief: "There's nothing wrong with wanting other people's approval and working hard to get it, but I don't need everyone's approval. Some people will like me and other people won't. When someone is critical of me, I can listen and try to understand where they're coming from, and we can probably solve the problem. But ultimately, their approval or disapproval has nothing to do with my worth as a human being or my capacity for happiness." Roger liked this new formulation. However, he was still concerned that his colleagues might look down on him if they found out about his MS. I encouraged him to test this belief by telling several colleagues about his illness. Of course, this is the Experimental Technique. He decided to try it and said he'd just have to let the chips fall where they may. He was surprised to discover that his colleagues were supportive and
Chapter 22
740
kind. Paradoxically, Roger ended up feeling closer to them because of his "flaws." He ended up winning on two levels. First, he learned that his negative thoughts had been off base, as is so often the case. He'd been involved in MindReading and Fortune-Telling, along with several other distortions. Second, he changed his value system, so that he was no longer a slave to the thoughts and opinions of others. 26. Interpersonal Downward Arrow The goal of the Interpersonal Downward Arrow is to help patients identify their Self-Defeating Beliefs about intimate relationships. When you use the Interpersonal Downward Arrow, you focus on a negative thought on the patient's Daily Mood Log, and ask these types of questions: "If this were true, what would it tell you about— "The kind of person she or he is?" "The kind of person you are?" "The kind of relationship you have with this person?" Although you'll usually use this technique to help patients understand their conflicts with other people, you can also use it to explore their negative feelings about you. In this case, you're analyzing the patient's "transference" reactions from a cognitive perspective. I once treated a young chemist named Rodney who suffered from severe depression, shyness, and panic attacks. He was referred to me by a colleague who used aggressive pharmacologic approaches. My colleague treated all his patients with large doses of antidepressant medications, but also had a kindly,
Chapter 22
741
charming demeanor and considerable expertise in psychotherapy. Whenever he referred a patient to me, I knew he'd tried a lot of things that hadn't worked, and it was likely to be a pretty challenging case. Rodney was no exception. Rodney had completed a post-doctoral fellowship in chemistry at MIT, and worked in a laboratory in Delaware doing research on membrane receptors. Rodney had suffered from mood and anxiety problems all his life, and lived with his mother, who also had emotional difficulties. Although he was attractive and successful, Rodney had a phobia about eating in public and was crippled by shyness. Whenever he was around young women he was attracted to, he felt nauseated and had the overwhelming urge to vomit on them. Needless to say, this put a bit of a crimp in his social life! At the initial evaluation, Rodney's depression and anxiety scores were off the charts, so it was clear that the antidepressant he was taking was completely ineffective. He was reluctant to stop taking it, however, because he'd heard that depression resulted from a chemical imbalance in the brain. At the same time, Rodney was very motivated and faithfully did all his written therapy homework with the Daily Mood Log. Over time, his depression and anxiety improved considerably, and I was able to taper him off the medication. Still, I couldn't get him over the hump completely, and he was unwilling to confront his fears. He carefully avoided women and always ate lunch alone in his lab. This was awkward because two attractive women from his lab would often drop by and invite him to join them for lunch. He'd thank them, but sheepishly
Chapter 22
742
make an excuse about a crucial experiment that he simply had to continue working on. Despite my best efforts, Rodney always gave me low scores on the Therapeutic Empathy scale. His scores indicated that he didn't think I was warm or supportive, and that I didn't really understand how he felt inside. Whenever I encouraged him to tell me more about these feelings, he resisted. He'd insist that the therapy was helping him, and why didn't we just let it go at that. I had a hunch that it was going to be important for him to tell me how he really felt, but he wouldn't open up. One day, I asked him what he was so afraid of. What did he think would happen if he criticized me? After a moment he said, "You might get upset if I criticized you." I told Rodney to write this down in the Negative Thoughts column of a Daily Mood Log, and to put a downward arrow under it. I said, "Let's assume that was true. Imagine that I've encouraged you to open up and criticize me, and you finally go ahead and do it. Then I get upset. What would that mean to you? Why would it be upsetting to you?" Rodney said, "Then you'd get mad and wouldn't want to work with me any more." I told him to write that down directly underneath the arrow, and to put another arrow underneath it. I said, "Rodney, let's assume that happened. You criticize me, just as I've asked you to do, and I get mad and decide that I don't want to work with you any more. What would that tell you about the kind of person I was?" He paused and then replied, "I guess that would mean that you were very
Chapter 22
743
fragile and narcissistic." I told him to write that down directly under the arrow, and to put another downward arrow under it. Then I said, "Let's assume that I was very fragile and narcissistic. What would that tell you about the kind of relationship you had with me?" Rodney replied, "That would mean I'd have to be really careful all the time–like walking on eggshells." I told him to write that down directly under the arrow, and to put another downward arrow underneath it. This time I said, "And how would you feel about working with someone like that? First, Dr. Burns pushes you to tell him how you really feel, but when you do, he gets mad and rejects you. How would you feel about Dr. Burns?" He said, "I guess I'd feel pretty angry. I wouldn't like him much at all." I told him to write that down, and said, "Rodney, it sounds like you do have some negative feelings about me, but you've been reluctant to express them because of these fears. Does that ring true?" He nodded, but didn't say a word. We're trying to understand three things about the way Rodney views his relationship with me, and perhaps with people in general: 1. How does he view me? In his mind, what role am I in? 2. How does Rodney view himself? What's his role in the relationship? 3. What's Rodney's understanding of how two people in an intimate relationship interact with each other? What are the rules? Let's see if we can answer those questions. Review Rodney's negative thoughts on page 745. What are his assumptions about me? What kind of person
Chapter 22
744
does he think I am? What's my role in the relationship? Put your ideas here:
What are Rodney's assumptions about himself? What kind of person does he think he is? What's his role in the relationship? Put your ideas here:
What are his assumptions about close relationships? Put your ideas here:
When you've written down your ideas, you can turn to page 746 and I'll share my thinking with you.
Chapter 22
745
Rodney's Negative Thoughts 1. You might get upset if I criticized you. Let's assume that was true. Imagine that I've encouraged you to open up and criticize me, and you finally go ahead and do it. Then I get upset. What would that mean to you? Why would it be upsetting to you? 2. Then you'd get mad and wouldn't want to work with me any more. Rodney, let's assume that happened. You criticize me, just as I've asked you to do, and I get mad and decide that I don't want to work with you any more. What would that tell you about the kind of person I was? 3. That would mean that you were very fragile and narcissistic. Let's assume that I was very fragile and narcissistic. What would that tell you about the kind of relationship you had with me? 4. That would mean I'd have to be really careful all the time–like walking on eggshells. And how would you feel about working with someone like that? First, Dr. Burns pushes you to tell him how you really feel, but when you do, he gets mad and rejects you. How would you feel about Dr. Burns? 5. I guess I'd feel pretty angry. I wouldn't like him much at all.
Chapter 22
746
Answer Here's what Rodney came up with: The people I care about are powerful, self-centered and dangerous. I must always please them and be on my guard. If I express my needs or feelings, I'll be punished and rejected It's no wonder that Rodney avoids intimate relationships! It's interesting that he sees me as both powerful and weak at the same time. On the one hand, I'm dangerous, and if he isn't careful, or if he offends me in any way, he thinks I'll hurt him. But at the same time, he sees me as very weak and fragile, because he believes I can't tolerate criticism. He seems to view himself with the same type of ambivalence. He sees himself as the weak, submissive member of the dyad, who always has to please the other person in order to avoid being crushed or rejected. But he also sees himself as powerful and dangerous, because he thinks that any expression of his feelings would be devastating to others. As a result, he experiences intimate relationships as superficial and dangerous. I told Rodney that I liked his analysis, and that it was suddenly clear why he'd been so reluctant to open up and tell me how he felt. I reminded him that we'd been working together for 11 months, and that I was proud of all he'd accomplished. At the same time, he was still struggling with feelings of anxiety and depression, and he was still holding back in the therapy. He also hadn't confronted his fears of dating and getting close to other people yet. I said that the next step might feel a lot like jumping off the high dive at the
Chapter 22
747
pool for the first time, and that there was no way I could make his fear go away. But if I could persuade him to jump, he'd quickly land in the water, and realize that he'd conquered his fear. I told him that I wanted him to take the plunge today. Right now, in fact. He looked puzzled and asked what I was talking about, and what he was supposed to do. I said: "Rodney, I think you know what I'm talking about. Every week, you mark me down on the Therapeutic Empathy scale. But when I ask you about it, you clam up and refuse to tell me how you feel inside. It's suddenly clear why you've been doing this. You're afraid that I'll get upset and reject you. But that's what I'm asking you to do right now. I want you to tell me how you really feel." Rodney swallowed hard and said: "Dr. Burns, this is hard to say, because you're by far the best shrink I've ever had. I feel like I'm finally making some progress, and the techniques you've taught me are invaluable. But if you want to know the truth, I don't actually like you very much. I don't like coming in for sessions, and I don't like being around you. When our sessions are over, it's always a huge relief, and then I dread having to come back again the next week. I hate to hurt your feelings, because you've done so much for me, but that's how I really feel." I said: "Rodney, to tell you the truth, I haven't really enjoyed our sessions
Chapter 22
748
as much as I'd like, either, because it never seems like we're really connecting. But now I feel like you're being honest and real, and I just discovered that I really like you! I hope you'll continue to be open with me, the way you were just now." Rodney's jaw dropped open as if he couldn't believe his ears. It was the best session we'd ever had. At the end, he gave me a perfect score on the Therapeutic Empathy scale. When he handed me his depression and anxiety tests the following week, I could see that his scores had improved dramatically. He explained that our last session had been extremely helpful, and that the next day, the two young ladies had invited him to lunch again. Only this time, he had the thought, "Why not give it a try?" So he decided to join them. He was surprised to find that he didn't get nauseated at all, but got into an animated discussion with them. One of them asked him if he enjoyed movies. He said he loved movies. Then she asked him if he ever went out on dates. He said, "Well, not real often, but it could be lots of fun." She said, "How about tonight?" Rodney replied, "I'd love to!" They went to a movie and had a ball. When he dropped her off, she asked if he wanted to come in and have a drink. They ended up making love all night long. It was actually the first time he'd ever had sex. He said he was crazy about her, and told me that they'd gone out every single night since then. The odd thing was that he attributed his success to the fact that he was
Chapter 22
749
wearing Birkenstock sandals. He made me promise to tell all my colleagues that they should tell all their lonely, shy patients to wear Birkenstock sandals, and they'd get laid right away. So I'm passing the information along to you! I felt, however, that expressing his feelings was really the crucial component of his recovery. He'd believed that his own feelings of anger and sexuality were too powerful and dangerous for other people to handle. When he finally confronted this monster, he discovered that it had no teeth. You could view the Interpersonal Downward Arrow as a bridge between CBT and the psychodynamic / psychoanalytic therapies, but it won't take years of analysis to identify the core conflicts that trigger the patient's problems. Instead, you simply ask a series of questions, and all the information comes spilling out of the patient's head, almost like magic. Of course, the insight alone won't be enough. Patients will still have to take action and confront their fears if they want to change their thinking patterns. 27. What-If Technique The What-If Technique was designed for patients with anxiety disorders. The goal is to find out what the patient is the most afraid of. What's the patient's deepest fear? What catastrophe is she or he trying to avoid? Ask the patient to draw a downward arrow underneath a negative thought on the Daily Mood Log, just as you'd do with the other Downward Arrow Techniques. In this case, the arrow is a form of shorthand for these kinds of questions: "What if that were true? What's the worst thing that could happen? What are you the most afraid of?"
Chapter 22
750
A new thought or fantasy will usually spring to mind. Tell the patient to write it down under the arrow and draw another arrow underneath it. Ask the same types of questions, and another thought or fantasy will spring to mind. If you repeat this process several times, you'll eventually uncover the fantasy that's at the root of the patient's anxiety, worrying or panic. Once you've unearthed the patient's worst fear, you have several options: You can ask, "How likely is it that this would happen?" or "Could you live with this in the unlikely event that it did happen?" You can identify the patient's SDBs, just as you would with the Individual and Interpersonal Downward Arrow Techniques. You can encourage the patient to confront his or her deepest fear using a variety of Exposure Techniques, such as Gradual Exposure, Cognitive Flooding or the Feared Fantasy Technique. You can use the Hidden Emotion Technique to identify a conflict the patient has been sweeping under the rug. The patient's deepest fear will sometimes be a symbolic expression of the problem that's bugging him or her. For example, the patient could be feeling annoyed with a friend or family member, or may feel ambivalent about his or her career. But because of the need to be nice, to please other people, or to avoid conflict, the patient hasn't yet brought the problem to conscious awareness. Kristin was a divorced woman who lived in Manhattan with her two boys, Tom and James. She was prominent in New York social circles and charitable activities, and came from old money. However, Kristin had suffered from mild
Chapter 22
751
depression and severe agoraphobia for more than ten years. As you know, patients with agoraphobia are afraid that something terrible will happen if they leave home alone. As a result, they often become housebound, and can only leave home in the presence of a trusted friend. According to conventional wisdom, they're usually afraid they'll have a panic attack when they're on the bus or waiting in line at the grocery store. But sometimes the fear is different. I used the What-If Technique to find out what Kristin was afraid of: David: Kristin, you say you're terrified to leave home alone. What's the worst thing that could happen? Suppose, for example, that you decided to walk to the grocery store near your apartment. What then? Kristin: I might drop my handkerchief on the sidewalk without noticing that I'd lost it. David: Let's suppose that happened. You drop your handkerchief on the sidewalk on your way to the grocery store. What would happen then? What are you the most afraid of? Kristin: Well, what if a terrible crime was committed on the spot where I lost my handkerchief? For example, what if someone got mugged or murdered there? David: Let's assume that this really did happen. A murder is committed right on the spot where you dropped your handkerchief. Then what would happen? Kristin: The police might find my handkerchief at the scene of the crime
Chapter 22
752
and trace it back to me. They might find my DNA on it. David: And then? Kristin: Well, they might conclude that I was the murderer and arrest me. And I'd have no alibi, since I was alone. David: It seems unlikely, but let's assume that this really did happen. What are you the most afraid of? What's the worst thing that could happen? Kristin: They might convict me, and send me to prison for the rest of my life. David: Obviously, no one would want to spend their life behind bars. But what is it about being in prison that's especially upsetting to you? What are you the most afraid of? At this point, Kristin begin to cry. I asked her what she was thinking. She blurted out, "My sons would have to grow up alone without their mother. I wouldn't be there for them." I asked her why this fantasy was so upsetting. Clearly, no mother would want to be separated from her children, but why was she so concerned about this? She explained that Tom, who was 11, was flunking several classes and had been acting out aggressively at school. Recently, the police had caught him throwing rocks at neighbors' windows, and threatened to arrest him if he didn't straighten up. Kristin was angry with Tom but afraid to lay down the law for fear of upsetting him. She was the kind of parent who tries to discipline her children with niceness and logic, which doesn't work. She was also frustrated with her ex-
Chapter 22
753
husband, because he didn't support her efforts to discipline the boys. Instead of telling him how she felt, Kristin swept her feelings under the rug. I asked Kristin if she wanted to brainstorm about how she might discipline her sons and communicate with her ex-husband more effectively. We worked on how she could be a little tougher and more assertive with her sons, and Tom's behavior and grades soon began to improve. I also taught her how to use the Revise Your Communication Style form so she could develop a better relationship with her ex-husband. However, Kristin was still afraid to leave home alone, so I suggested we try some exposure. I encouraged her to walk to Central Park one Saturday morning, which was several blocks from her apartment, and sit on a park bench. No matter how anxious she got, she had to tough it out until her anxiety went away–even if it took two or three hours. Kristin was frightened but agreed to give it a try. I told her that if she started to get overwhelmingly anxious, she could distract herself. She decided to bring a Rubik's Cube along, so if she started getting overwhelmed, she could pull it out of her purse and concentrate on solving the puzzle. I also told her to bring a notebook so she could record how anxious she was each minute on a scale from 0% – 100%, and write a brief description of the frightening thoughts and fantasies that flooded through her mind. The big day came. Kristin walked to the park and sat down on a bench, just as she'd promised. She was intensely nervous, and had fantasies of being arrested and thrown in jail for a crime she did not commit. She estimated her
Chapter 22
754
anxiety at 90%, but forced herself to sit there and endure the torture for 20 minutes. Then Kristin spotted a policeman. Horrors! Her fear suddenly jumped to 100%. She panicked, and had an almost irresistible urge to run home, but remembered my instructions and pulled the Rubik's Cube from her purse. She looked down and started concentrating on it as intensely as she could, hoping the policeman wouldn't notice her. Out of the corner of her eye, she could see the policeman slowly turn and start walking directly towards her. This was awful! He stopped directly in front of Kristin, less than a foot away. Kristin was staring at the ground, and could see his shoes. She resigned herself to getting arrested and forced herself to look up at him. But when she did, she recognized him as an old Irish police officer she'd known ever since she was a child. He smiled and said, "Top o' the mornin' to ya, Kristin! It's such a beautiful day. Great to see you up and about!" Kristin couldn't believe her ears. She was flooded with euphoria, and her fears vanished. She chatted enthusiastically with the officer for a few minutes. Then she walked through downtown Manhattan for several hours, shopping and doing all kinds of things she hadn't been able to do for more than ten years. She said she didn't have one hint of anxiety the entire time. The three Downward Arrow Techniques will quickly produce a large amount of useful information about the patient's psyche. You can often learn as much about the patient in five or ten minutes as you might learn in several years of conventional therapy. Furthermore, the information you uncover will usually be
Chapter 22
755
right on target. Patients nearly always confirm that the insights fit like a glove. The Downward Arrow Techniques are also easy to use and will usually work effectively the first time you try them. A grammar school counselor who attended one of my workshops said she'd even tried them out with children in the first to fifth grades, and they'd worked beautifully without any modification. She said the children's Self-Defeating Beliefs turned out to be nearly identical to those of adults. The children felt depressed or anxious because they weren't popular, pretty or smart enough. Some of them were beating up on themselves because they thought they had to be perfect. Once you've pinpointed the patient's Self-Defeating Beliefs, you'll have an excellent blueprint for the treatment. You won't simply focus on the complaint that brought the patient to therapy, but can address the values and beliefs that triggered the problem in the first place. For example, a student may be struggling with panic attacks in class, but when you use the Individual Downward Arrow, you may discover that Perfectionism, Perceived Perfectionism, and the Achievement Addiction are at the root of the problem. You can help the student modify these attitudes and develop unconditional self-esteem. That way, she or he will not only feel better in the here-and-now, but won't be so vulnerable to painful mood swings in the future. When you use these techniques, you won't be imposing your own preconceived ideas on the patient. All you have to say is, "If that were true, what would it mean to you?" Regardless of what the patient says next, you can say,
Chapter 22
756
"Good, write that down." The patient will determine the outcome of this process. So in a sense, these are rather pure techniques that won't be contaminated by your own training or personal bias. Most CBT techniques focus on change, but the Downward Arrow Techniques focus on understanding. Many of our patients want to know "why" they feel the way they do. You may think you have to come up with an answer, but this can be difficult because the causes of all the psychiatric disorders are unknown. The only truly honest answer would be to tell the patient that you don't have the vaguest idea why they're suffering from depression, panic attacks, or shyness, and that no credible scientist does, either. The most we could say is that these problems might result from our genes, our experiences in life, or from some combination of genetic and environmental influences. But there's something cold and unsatisfying about answering the question this way. Instead, you can ask patients to describe a specific moment when they were upset, and list their negative thoughts and feelings on a Daily Mood Log. Ask the patient to select one negative thought, and walk them through one of the Downward Arrow Techniques. Most patients enjoy these techniques and feel excited about what you come up with. Remember that there are three different Downward Arrow Techniques, each involving slightly different kinds of questions: Individual Downward Arrow. You ask, "If this were true, why would it be upsetting to you? What would it mean to you?" Interpersonal Downward Arrow. You ask, "If this were true, what would it
Chapter 22
757
tell you about your relationship with this person? What role are you playing, and what role is the other person playing?" What-If Technique. You ask, "What if this were true? What are you the most afraid of? What's the worst thing that could happen?" You don't have to be a purist about it, and you can mix and match. Sometimes, I'll start out with the What-If Technique, but switch to the Individual Downward Arrow because that's where the energy seems to be leading. When I was working with Rodney, I started out with the Individual Downward Arrow, but didn't hit pay dirt until I switched to the Interpersonal Downward Arrow. 28. Hidden Emotion Technique Early in my career, I realized that patients who suffer from anxiety have a tendency to avoid problems that they don't want to face. Many of them are exceptionally nice individuals who are preoccupied with pleasing others. When they're upset about something, like a conflict with a family member or a problem at work, they sweep the negative feelings under the rug and forget all about the problem that's bugging them. However, the feelings soon bubble to the surface again, disguised as some form of anxiety, such as a panic attack, chronic worrying, a phobia, OCD symptoms, or even hypochondriasis. When patients bring these problems to conscious awareness and express the feelings they've been trying to suppress, the anxiety will often disappear. Rodney was a classic example of this phenomenon. He was upset with me for months but didn't think he had the right to express his negative feelings. He was afraid of his positive, sexual feelings as well, so he avoided the women
Chapter 22
758
he was attracted to. When he finally told me how he really felt, and gave himself permission to explore relationships with women, his anxiety disappeared. However, it's usually hard to figure out what the underlying problem is. People who are anxious are very good at convincing themselves that everything is fine. They insist that they have no problems, other than the anxiety itself, and that they get along well with everyone. If you show me 100 anxious individuals, I'll show you 100 of the "nicest" people you ever met! Here's where the Hidden Emotion Technique comes in. First, you help the patient identify the hidden problem. This will be the tough part, because the patient will try hard to convince you that there is no problem other than the anxiety itself. This means you'll have to put on your detective cap and look for clues, and you'll have to go down a few blind alleys as well. Sooner or later, the patient will generally identify the hidden feeling. Then they'll have to do something about it. This could involve solving the problem that's bugging them, or simply expressing the feelings they've been denying. That's usually the easy part. You can use the Hidden Emotion Technique at any time during a session. I might ask a question like this: "Alicia, you've told me that you've been struggling with feelings of panic at work. You also say that you admire your boss and love your work, and yet every time your boss walks past your desk, you panic and get nauseated, and have an almost irresistible urge to vomit on him. Then you have to go home because you're feeling sick. Something about
Chapter 22
759
what you're saying doesn't seem to add up. I can't help but wonder if there might be a problem at work that you haven't told me about? You strike me as an awfully conscientious and nice person. But some people are overly nice, and then when something's bugging them, they kind of ignore the problem. For example, are you upset with your job or your boss? Is there a problem with your marriage or with anything else in your life?" That's how you initiate the Hidden Emotion Technique. You ask the patient if there's some problem they're avoiding, and they'll nearly always shoot you down. When this happens, you can simply drop the issue for the time being and use other CBT techniques. At the end of the session, you can try again. With Alicia, I might say: "I think we've done some good work here today challenging your negative thoughts, and your anxiety seems to be improving. But I'm still wondering if anything's upsetting you that you're not telling me about. Has anything come to mind?" Once again, the patient will typically shoot you down. You can continue to use the Hidden Emotion Technique twice each session, and the rest of the time, you can work with other CBT techniques. After a handful of sessions, the patient will often "remember" something important, and it will change the entire focus of the treatment. I've rarely been able to figure out what the hidden problem or feeling was. Usually, only the patient can do that. But there are a few hints that might help.
Chapter 22
760
First, the hidden problem is nearly always something in the here-and-now. It's not something that's buried in the past. Second, the problem will nearly always be something very ordinary and obvious, like feeling angry with your spouse, or hating your major in college. It's usually about as subtle as an elephant in the room. Finally, the anxiety tends to be a symbolic expression of the problem. In other words, the patient was telling you about the hidden problem all along, but speaking in a kind of symbolic code. Alicia was a patient I treated for anxiety and panic attacks during the late 1970s. Alicia had gotten married after college and gone to work for a man who was starting a business as a beverage wholesaler. After a few months, she started having panic attacks at work. Alicia wasn't aware of any problems in her marriage or at work. She insisted that she adored her husband and loved her job. She explained that her boss always praised her contributions and said that her hard work was crucial to the success of the company. But Alicia started having more and more panic attacks at work, and often felt so sick that she had to go home. It seemed like Alicia's panic attacks came from out of the blue, and weren't triggered by any problems in her life. Freud claimed that panic strikes suddenly, like lightning, without rhyme or reason. But is this really the case? See if you can guess what was bugging Alicia. Don't worry about getting it right. Most of the time, my theories about what's bugging the patient turn out to be wrong. But it's still worthwhile to make a wrong guess because when the patient says, "No, that's not it," she or he has to compare your theory with the
Chapter 22
761
real problem. This will tend to activate the part of their brain that knows what the problem is. After enough incorrect guesses on your part, the patient will usually come up with something important. Please put your ideas about what might be bugging Alicia here:
Chapter 22
762
Answer During our sixth session, Alicia asked if cognitive distortions, such as Allor-Nothing Thinking and Labeling, could apply to family dynamics. I told her that I didn't see why not, and asked her what she meant. Alicia explained that she had a twin sister named Beth, and that her parents had labeled Beth the "black sheep" of the family. When they were growing up, Beth was wild and sometimes got into trouble. In contrast, Alicia was always the "good daughter." She got straight A's, was a model of good behavior, and was elected president of her senior class in high school. But when she thought about it, Alicia said that these labels weren't entirely valid. She said that her sister clearly wasn't "all bad" and that she definitely wasn't "all good." In fact, they were more similar than different. For example, Beth was now happily married and had blossomed into a wonderful mother. In addition, Alicia emphasized that she wasn't always the "good girl" that her parents thought she was. She confessed that she actually hated being a beverage wholesaler and wished she didn't have to be so good all the time. She explained that she liked her boss, and enjoyed having the chance to help his young company prosper, but said it wasn't what she really wanted to do with her life. And yet, she felt like she had to be the "good daughter," and keep helping him out instead of pursuing her own dreams. I asked her what she'd really like to do. She told me that she'd always wanted to design women's sportswear. She didn't know if she had any talent for it, but really wanted to give it a try. She added that she'd been working and
Chapter 22
763
studying non-stop for as long as she could remember, even during the summer months when she'd worked as a waitress to help her family out financially. She'd never really had the chance to take time off and have fun. Alicia said she dreamed of taking three months off just to sit in the sun and smell the roses. Alicia's panic attacks suddenly appeared in a different light. Although she repeatedly insisted that she loved her job and admired her boss, her symptoms conveyed a very different message. They said, loud and clear, "This job makes me sick." The panic attacks allowed her to express these feelings indirectly, without appearing angry, ungrateful, or demanding. Once the patient has identified the problem that's bugging them, they've got to do something about it. I asked Alicia if she'd ever considered pursuing her dreams. Was there any reason why she couldn't simply quit and take a few months of vacation, and then look for a job designing women's clothing? She seemed shocked, and expressed the concern that her boss, husband and parents might be disappointed and think she was irresponsible for giving up a good job. I pointed out that she could use that reasoning to delay her dreams forever, but that she only had one life to live. Alicia decided to bite the bullet and talk things over with her boss that very afternoon. He was sorely disappointed, but said he realized that the job wasn't sufficiently challenging for her. She gave him a month's notice so he'd have plenty of time to find someone to fill her position. By that very evening, Alicia's anxiety had completely disappeared. She was feeling so much better that she terminated treatment at the next session. Alicia wrote to me six months later. She told me that she'd never had
Chapter 22
764
another panic attack or any anxiety at all since our last session. She said she'd enjoyed a three-month vacation and subsequently found a job as an apprentice to a woman who designed and manufactured women's sportswear. She was excited about her new life and loving every minute of her new career. The Hidden Emotion Technique can be invaluable in the treatment of any type of anxiety. It will provide you with a much deeper understanding of your patients and greatly improve the effectiveness of the treatment. I once treated a pathology resident named Corey who sought treatment for OCD. Corey became upset when a small piece of a cadaver's spinal column snapped off and lodged in his eye during an autopsy. He quickly removed it, and his eye didn't seem injured, but he started worrying that he might have contracted Creutzfeldt-Jacob Disease. This is an infectious and horrible form of rapidly fatal dementia. It's the human version of Mad Cow Disease. Rationally, Corey knew that this was impossible, since the man he was dissecting had died of a heart attack, and did not have Creutzfeldt-Jacob Disease. Still, his anxiety was overwhelming, and he developed a contamination phobia. He began to wear multiple gowns and meticulously made sure that no flesh was exposed before he started his autopsies. He even started wearing two pairs of gloves, goggles and a NASA space helmet! It took Corey more than an hour to get properly dressed before each autopsy. He also started spending longer and longer performing autopsies to "insure correctness." Before long, he'd slowed down to a snail's pace, and couldn't finish any of his dissections, even after many hours of intense effort.
Chapter 22
765
Partially dissected bodies began piling up in the morgue, and the other pathology residents started complaining that they couldn't complete their autopsies because there wasn't enough room in the morgue. When I asked Corey if anything was bothering him, he insisted that everything was fine. He said he'd always wanted to be a pathologist and got along with all the people in his program. He said that everything in his life was great, aside from his symptoms. He added that he'd struggled with OCD on and off since childhood, and simply couldn't understand the sudden and mysterious flare-up in his symptoms. Do you believe Corey when he says there are no problems in his life? Do you think these symptoms actually developed without rhyme or reason? It seems unlikely, doesn't it? Let's see if we can use the Hidden Emotion Technique. What hidden feeling or problem could Corey be struggling with? Put your best guess here before you turn the page:
Chapter 22
766
Answer Corey is the only one who can tell us for sure what's going on. We can only make educated guesses. But ask yourself these questions: 1. Does he really seem to enjoy his work? 2. Does he really seem to have positive feelings toward the other residents in his program? What's the impact of his symptoms on them? Corey and I used a variety of CBT techniques with only partial success. His feelings of anxiety improved about 50%, but he was still impaired. At every session, I asked if there were any problems that he hadn't told me about. Was anything bugging him? He always insisted that everything was fine, except for the OCD. However, at the beginning of the eighth session, Corey brought me an advertisement from a local medical newsletter. A teaching hospital down the road needed an emergency room resident beginning in July. Corey seemed excited. I said, "Corey, why are you so excited about this ad? You told me that you always wanted to be a pathologist." He replied, "No, I told you that my father always wanted me to be a pathologist. If you want to know the truth, I hate pathology. I've always wanted to be an emergency room doctor." Then he admitted something else. He was Jewish, and was working in a fundamentalist Baptist hospital. He felt there was some subtle anti-Semitism among the staff. For example, he sometimes thought he got the short end of the stick in terms of the on-call schedule and rotations, but always acted polite and agreeable so that his colleagues and supervisors wouldn't label him as a complainer.
Chapter 22
767
Suddenly, Corey's symptoms made perfect sense. His contamination phobia and obsessive slowness were his way of saying, "I can't stand dissecting dead bodies. I don't want to spend my life this way!" At the same time, he was making life miserable for all the other residents in his program. But by playing the role of an innocent victim of OCD, he could express his anger indirectly, as if his symptoms were the result of some mysterious force that was beyond his control. Of course, insight alone won't be enough. Now that Corey has uncovered the hidden problems, he'll have to express the feelings he's been hiding and solve the problems that are bugging him. Following the session, Corey drove to the hospital down the road and interviewed for the emergency room position. He had excellent credentials, and they accepted him on the spot. Later that day, he met with the Director of Residency Training at his hospital. Corey explained that he'd decided to resign at the end of June because he'd decided that pathology was not for him. He also expressed his concerns about the religious bias in a tactful way. The two of them had a good heart-to-heart talk. When I saw Corey the next week, he was jubilant and symptom-free. His fears of contamination had vanished and he'd gotten caught up on all his autopsies. In fact, he said he could do autopsies faster than any other resident in the program. He was excited about his new career plans and was ready to terminate therapy. The Hidden Emotion Technique can be very helpful for patients with
Chapter 22
768
anxiety disorders and somatoform disorders, such as chronic pain or hypochondriasis. It's rarely helpful for depression. There are two steps: 1. You help the patient identify the problem or feeling that she or he is upset about. 2. You encourage the patient to express the feelings and take steps to resolve the problem. The first step is by far the hardest, because anxious individuals are so good at convincing you that there aren't any problems in their lives. When you unearth the hidden conflict or emotion that's triggering the symptoms, you'll see exactly why the patient is suffering. You'll also see how off base Freud was when he said that panic and anxiety strike unexpectedly, without rhyme or reason. Anxiety is a human problem that emerges in a human context. That's why the Hidden Emotion Technique is a powerful treatment method in its own right, and a wonderful complement to the other CBT techniques.
23*
Motivational Techniques
So far, we've asked these kinds of questions: Are the patient's negative thoughts valid? How can we help the patient put the lie to them? What kinds of attitudes and beliefs triggered the negative feelings in the first place? In this chapter, we'll ask these questions: Does this patient want to change? What are the advantages of the way the patient is thinking, feeling, and behaving? How does this mindset reward the patient? And what costs does the patient have to pay? Motivational problems will be important in about half of the patients you treat for depression and anxiety. Although they're suffering, they may have mixed feelings about change (Outcome Resistance), or about putting out the effort that will be necessary for the change to occur (Process Resistance). In contrast, if the problem involves a relationship problem, habit, or addiction, motivational issues will dominate the clinical picture 90% – 100% of the time. Patients with these problems will have strong reasons to maintain the status quo. * Copyright
2004 by David D. Burns, M.D.
Chapter 23
770
Many mental health professionals treat relationship problems and addictions with cognitive, behavioral, or psycho-educational techniques, thinking that the patient wants or needs help. For example, if you're treating a troubled couple who constantly bicker and blame each other for the problems in their relationship, you might try some communication training techniques, thinking that better listening and self-expression skills will lead to greater intimacy and trust. But you may be in for a surprise when they sabotage these techniques and consistently "forget" to practice between sessions. Instead, they may report that they spent the entire week arguing and blaming each other for the lack of progress. When you encourage them to examine their own distorted thinking patterns, they suddenly turn on you, insisting that you just don't understand. Of course, the cognitive and behavioral marital therapy strategies look good on paper. Every time a troubled couple tries to talk about the problems, they blame each other and defend themselves. Their negative thoughts about each other—"He's such a jerk! He never listens! He shouldn't be like that!"—are loaded with all the familiar cognitive distortions, such as All-or-Nothing Thinking, Mental Filter, Mind-Reading, Should Statements, Labeling, and Blame. In spite of this, the cognitive and behavioral treatment strategies usually miss the point because people with troubled relationships feel self-righteous and empowered by their anger. They're often far more interested in revenge and vindication than in getting close to the person they're annoyed with. Furthermore, their distorted thoughts about each other are emotionally reinforcing, so they don't feel motivated to challenge them. In fact, most angry patients will defend
Chapter 23
771
their distorted perceptions and hostile, provocative comments with the ferocity of a mother lion protecting her cubs. By the same token, people don't usually develop bad habits, like compulsive eating or drinking too much, because of a lack of understanding of the negative consequences of these behaviors, or because of a lack of selfesteem, but because they like what they're doing. It's fun to get high and eat whatever you want, whenever you want. In addition, abstinence, dieting and exercising can seem like hard, unrewarding tasks. You may view the patient's addiction as a problem, but the patient may view it as more of a solution, so you end up in a power struggle. You'll do yourself and your patients a service if you back off and learn to deal with the motivational problems skillfully at the beginning of the intervention, and whenever the patient shows any signs of ambivalence. Some of the Motivational Techniques in this chapter, such as the CostBenefit Analysis (CBA), are straightforward. These techniques are suitable for reasonably cooperative patients who feel ambivalent about change. When you bring the factors that sabotage the patient to conscious awareness, it will often boost their motivation to change. In contrast, techniques like the Paradoxical CBA or Devil's Advocate Technique are suitable for patients who are oppositional and strongly committed to the status quo. These paradoxical techniques will force the patient to confront the many powerful reasons whey they really don't want to change. You won't have to get into frustrating and unproductive power struggles with them, because
Chapter 23
772
they'll have to persuade you, and not vice versa. Of course, you've already learned the most important motivational technique of all, Agenda Setting. You can use the techniques in this chapter when you're doing Agenda Setting, but you can also use them at any subsequent point in the therapy when you sense you're bumping up against some resistance. 29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA) This was one of the first Motivational Techniques I created. It's useful in both individual and group therapy, and it's easy to learn. There are five different types of CBAs. Each type can be done in a straightforward or paradoxical manner, so there are actually ten different kinds of CBAs: Cognitive CBA. Patients list the advantages and disadvantages of a negative thought, such as, "I'm such a loser," or "My problems are hopeless." Attitude CBA. Patients list the advantages and disadvantages of a SelfDefeating Belief, such as "I should always try to be perfect," or "I need other people's approval to be worthwhile." Emotion CBA. Patients list the advantages and disadvantages of a negative feeling, like depression, anger, guilt, inferiority, anxiety, or hopelessness. Relationship CBA. Patients list the advantages and disadvantages of blaming someone else, such as their spouse, for the problems in their relationship. Habit CBA. Patients list the advantages and disadvantages of a habit or addiction, such as drinking, using drugs, overeating or procrastinating. Here's how you do a Straightforward CBA. Ask the patient to write a brief
Chapter 23
773
description of the thought, feeling, behavior or habit they're trying to change at the top of the CBA on page 774. Then you can ask, "What are the advantages and disadvantages of this mindset? How will it help you, and how will it hurt you?" After they list all the advantages and disadvantages they can think of, they can balance them against each other on a 100-point scale. They can put two numbers that add up to 100 in the circles at the bottom of the CBA to show whether the advantages or disadvantages feel greater. Let's revisit Jason, the shy young man described on page 533, who wanted to flirt with the cashier at the grocery store. One of his negative thoughts was, "People will think I'm a self-centered jerk if I try to flirt with her." Put yourself in Jason's shoes. Can you think of any advantages of believing this thought? List several benefits in the left-hand column of the CBA on page 774. When you're done, see if you can think of some disadvantages. What's the downside? What price will Jason have to pay for giving himself this message? List all the disadvantages you can think of in the right-hand column of the CBA on page 774. Once you've completed your CBA, ask yourself which list seems more compelling, and put two numbers that add up to 100 in the circles at the bottom. If the advantages are slightly greater, the number in the left-hand circle will be larger. If the disadvantages are greater, the number in the right-hand circle will be larger. Please complete your CBA before you continue reading!
Chapter 23
774
Cost-Benefit Analysis List the attitude or feeling you want to change:
Advantages
Disadvantages
Chapter 23
775
You can see Jason's CBA on page 776. He completed it on his own, and I was impressed with what a great job he did. You can see that there's some narcissism fueling the system. Although Jason's shyness makes him feel intensely uncomfortable, he also feels morally superior and imagines that he's sacrificing his own needs for the good of mankind. He believes he's the center of attention and thinks his every action will have a huge effect on other people. This belief also allows him to feel sorry for himself and blame other people for his impoverished social life. The disadvantages were equally revealing. He imagines that the people in line are extremely judgmental and will be angry with him if he tries to flirt with the cashier. This makes it impossible to feel relaxed, spontaneous or carefree. Can you imagine if people really were this judgmental and preoccupied with Jason? I can picture a man coming home from the grocery store and telling his wife, "Honey, I just saw a young man struggling with the urge to flirt, but he chose to remain quiet and humble. This gladdens my heart and gives me renewed hope for the human race!" Or, "Honey, listen to this. When I was in line at the store, I saw a nervous young man trying to talk to the cashier. I had the distinct impression that he was trying to flirt with her. It was devastating to have to watch. Can you believe the impertinence? Young people today are such selfcentered jerks. What's the world coming to?" Obviously, these scenarios are absurd, but to Jason, they seem realistic and threatening.
Chapter 23
776
Jason's Cost-Benefit Analysis List the attitude or feeling you want to change: People will think I'm a selfcentered jerk if I try to flirt with her. Advantages of Believing This 1. I won't have to risk embarrassment.
Disadvantages of Believing This 1. I won't do what I want.
2. I won't get shot down. 3. I won't upset people. 4. I'll feel morally superior because I'll be sacrificing my own needs to make other people happy. 5. I can blame other people for my impoverished social life.
2. I won't grow because I'll be so afraid of rejection. 3. If I do try to talk to her, I'll get really uptight because I'll think everyone is mad at me. 4. I'll be angry and blame other people for my inhibitions. 5. I'll end up alone.
6. I can feel sorry for myself. 35
65
The two numbers in the circles at the bottom of Jason's CBA indicate that the disadvantages of the negative thought greatly outweighed the advantages in his mind. Jason told me that he was tired of feeling shy and lonely, and willing to do whatever it took to overcome these problems. A CBA can buy you some motivation and determination, but it usually won't cure the patient. Before Jason can overcome his shyness, he'll have to put the lie to the negative thoughts that flood through his mind when he's feeling shy and self-conscious. In addition, he'll have to learn to flirt and develop relationships with other people. These tasks will require hard work and courage.
Chapter 23
777
The more CBAs you do, the better you'll get at them. Over time, you'll begin to see more and more deeply into the hidden rewards of your patients' negative thoughts, feelings, and behaviors. You'll develop a more sophisticated understanding of why your patients get stuck every time they try to change. There are several common errors to be aware of when doing a CBA. Let's assume that your patient is listing the advantages of this SDB: "I must be loved to feel happy and fulfilled." The patient might get confused and list the advantages and disadvantages of being loved. This won't be very illuminating, because there are lots of advantages and few or no disadvantages! The patient has missed the point. A better question would be this: "What are the advantages and disadvantages of basing my self-esteem and capacity for happiness on being loved? How will this mindset help me, and how will it hurt me?" The answer to this question will be far more revealing. You and your patients may also overlook some of the most important and compelling advantages of the negative thought, attitude, emotion or behavior. For example, if you ask the patient to list the advantages of drinking, he may insist that there aren't any advantages. He may tell you that he just got his second DUI and that his doctor told him that there's evidence of liver damage from the alcohol. He's having blackouts, he's been put on probation at work, and his wife is threatening to divorce him. Although these disadvantages may seem overwhelming to you, the patient may simply be telling you what you want to hear, or may feel temporarily motivated because of the recent crises. But there's an equally compelling list of
Chapter 23
778
advantages that he's carefully editing out of his conversation with you. If you buy what he's telling you, and you don't focus on all the advantages of drinking, the CBA will be superficial and ineffective. In fact, drinking has been working for him. He's probably been discounting the negative consequences of his habit for years, and he'll probably discount them again before long. Ask him to describe the thoughts he has when he's feeling tempted and ends up giving in to the urge to drink. He's probably telling himself: 1. Boy, a beer would sure be nice right now. 2. One or two beers can't hurt. 3. My wife is too uptight. She shouldn't be so bossy and nag me all the time. 4. The Giants game will be more fun to watch if I get a nice buzz going. 5. My doctor is exaggerating to try to make a point. My liver will be fine. 6. I've learned my lesson about driving. It won't be a problem again. I can handle it. 7. I'm in control. I can quit any time I want. Now we've got a more realistic start on the advantages of drinking. You may think, "Well, these advantages aren't real. They're simply justifications and rationalizations." That may be true, but it won't buy you a cup of coffee in New York! The patient will buy into these arguments the next time he wants a drink, so they definitely belong in the Advantages of Drinking column on his CBA. Now let's see how an Attitude CBA would work. Let's assume that you base your self-esteem on your achievements, and often beat up on yourself when you make a mistake because you think you should always try to be perfect.
Chapter 23
779
List all the advantages of perfectionism on the CBA on page 780. Ask yourself, "How will this mindset help me? What are the rewards of this belief?" There will be lots of them. Then list the disadvantages of perfectionism. Ask yourself if there's a downside to this mindset. When you're done, balance the advantages against the disadvantages and put two numbers that add up to 100 in the two circles at the bottom. Please complete your lists before you continue reading! You can see a completed Attitude CBA on page 781. I'm sure you could add to these lists. There are lots of advantages and disadvantages of any SelfDefeating Belief, including perfectionism. In this example, the disadvantages narrowly edged out the advantages. What do you do if the advantages are greater than the disadvantages? Let's say your patient puts 60 – 40 in the two circles at the bottom, indicating that the benefits of the perfectionism outweigh the costs. What would you say next? Write out what you'd say to this patient before you continue reading:
Chapter 23
780
Attitude Cost-Benefit Analysis List the attitude or feeling you want to change: I should always try to be perfect. Advantages of Believing This
Disadvantages of Believing This
Chapter 23
781
Attitude Cost-Benefit Analysis List the attitude or feeling you want to change: I should always try to be perfect. Advantages of Believing This
Disadvantages of Believing This
1. I won't settle for mediocrity, so I'll do outstanding work.
1. Nothing I do will ever seem good enough.
2. When I achieve something great, I'll feel special.
2. I feel tense and constantly worry about things.
3. Other people will admire me because of my high standards.
3. My self-esteem always seems to be on the line.
4. My perfectionism will show that I'm a cut above other people. After all, we wouldn't expect an "average" person to be perfect.
4. When I fail or fall short of my goals, I feel devastated.
5. I'll have an easy way of measuring my self-esteem.
5. I'm afraid to take chances and risk failure. 6. I often procrastinate because I'm so worried about having to do everything perfectly. 7. Failure will be guaranteed, because nothing I do could ever be perfect. 8. I get frustrated when other people don't measure up to my standards. 9. It's hard to handle criticism because I feel so defensive. 10. I sometimes lose sight of the bigger picture because I get so obsessed with the details.
45
55
Chapter 23
782
Answer The most common therapeutic error would be to try to talk the patient out of the perfectionism. You might try to persuade him or her that this mindset is unrealistic and will trigger all kinds of frustration and disappointment. These persuasive efforts will usually trigger resistance. Instead, you can point out that the perfectionism seems to be working for the patient, and ask why the two of you are working on this problem, given the fact that there are so many advantages. You could also say something like this: "Jackie, it's clear that there are a lot of advantages of your perfectionism. I used to feel the same way. Even though my perfectionism was stressful, it seemed to be working for me. I was afraid that if I gave it up, I'd have to settle for second best. Is that how you feel?" The main idea here is to let go of your need to help the patient. Take a Buddhist approach and surrender. The patient is saying, "I'm not ready to give this up." Let her hang on to the perfectionism, and try to see the world through her eyes. Support her. Validate the advantages, because most of them are real. Paradoxically, she may begin to argue for the other side, and talk about how the perfectionism causes problems for her. If she doesn't, you can ask her if there's another problem she wants to work on instead. If the disadvantages of the perfectionism outweigh the advantages, you can ask her to revise the belief so she can get rid of the disadvantages while maintaining the benefits. Imagine, for the moment, that you're the patient. What
Chapter 23 personal value could you substitute for, "I should always try to be perfect"? Is there something you could aim for other than perfection? Put your ideas here before you continue reading:
783
Chapter 23
784
Answer There are many ways to revise any SDB, but here's one approach: "There's nothing wrong with wanting to do superb work or enjoying my accomplishments. However, no one can achieve perfection or avoid some failures and mistakes. When I make a mistake, I can view it as an opportunity to learn and grow. Great achievements can be rewarding, but they won't make me any better than other people, and failures won't make me any less worthwhile." Of course, this is an example of using the Semantic Method to modify an SDB. It's appealing to patients because they won't feel like you're challenging their basic values and beliefs. Instead, you're showing them how to give their personal value system a tune-up. The CBAs we just reviewed were straightforward. When you do a Paradoxical CBA, you'll ask the patient to list only the advantages of the negative thought, feeling, behavior or habit. Then you ask a question like this: "Given all these advantages, why should you change?" This technique can be quite effective when the patient is oppositional and firmly committed to the status quo. A Paradoxical CBA can be especially helpful if you're working with patients who are angry, as well as those who are struggling with habits or addictions. You can also do a double paradox. In this case, you'd list all the advantages of the status quo in the left-hand column, and the disadvantages of change in the right-hand column. For example, if the patient is struggling with overeating, the advantages of the status quo might include, "It's easy," and "I can
Chapter 23
785
eat whatever I want, whenever I want." The disadvantages of change might include, "Dieting sucks," and "Exercise is a pain in the butt." Once the patient completes these lists, you can ask the same type of question: "Why should you change, given all the powerful reasons not to?" Paradoxical CBAs have to be administered in a respectful way, or else they'll seem gimmicky and manipulative. In fact, a genuine paradox is not a paradox at all, because you're simply reading how the patient really feels. A valid paradox is actually a sophisticated form of empathy. I once treated an endocrinologist named Jasper who suffered from chronic depression and episodic attacks of intense anger. Although Jasper was doing reasonably well in his research and clinical work, he was always unhappy. He'd received years of treatment with antidepressant medications and psychotherapy, but nothing had ever put a dent in his feelings of depression and anger. At our first visit, Jasper explained how angry he felt after learning that a colleague he disliked had received a promotion to Associate Professor of Medicine. Jasper had been feeling frustrated and resentful about the promotion for weeks, and was taking it out on his wife, children, and colleagues. He was particularly annoyed because he felt his own research was outstanding, and yet he'd been stuck at the rank of Assistant Professor of Medicine for five years. Jasper described his colleague as a manipulative and dishonest individual who did shoddy work. The thought that was triggering his anger was, "It's unfair that a phony like that should get a promotion!" Angry individuals are nearly always convinced that they're right and the
Chapter 23
786
other person is wrong. They often feel like innocent victims and believe that their angry feelings are justified. If you try to "help" them modify the distorted thoughts and attitudes that trigger the anger, they'll insist that you just don't understand, and may even think you're siding with the person they're at odds with. Anger management programs are currently in vogue, but the concept makes me uncomfortable. The implication is that our patients are bad children, and we're going to show them how to "manage" their childish, pouty feelings, since they're not capable of managing them on their own. To my ear, this idea lacks empathy and fails to convey respect. Furthermore, it seems intrusive and controlling, and is likely to fire up the patient's resistance. Instead, I try to see the world through the patient's eyes. After all, some anger can be justified and healthy. The patient may have expressed the anger too aggressively, but there's bound to be a kernel of truth in the way they're thinking about the person they're mad at. If they feel that you understand and accept them, their defenses will come down, and you'll be able to work together far more effectively. I told Jasper that I was aware that there were some bad apples and phonies doing research, and that some of them seemed more interested in promoting their own careers and political agendas than in doing good, honest work. I added that I wasn't convinced that his anger was a bad thing, and suggested we might do a CBA together. I asked Jasper to list all the advantages of his anger in the left-hand column of a CBA. See if you can come up with at least five advantages of Jasper's anger. List them here before you continue
Chapter 23 reading: 1. 2. 3. 4. 5.
787
Chapter 23
788
Answer Jasper and I thought of many advantages of his anger. They included: I can feel self-righteous and morally superior. My anger shows that I'm a man of principle and feel strongly about integrity in academic research. I can feel powerful. I can play the role of victim and feel sorry for myself. My colleagues might take a second look at the fellow who got promoted. When I complain, my closest colleagues, friends and family usually agree that the other fellow really is a jerk. It gives me an excuse for the fact that I haven't been promoted to Associate Professor yet. I can avoid talking to the department chairman about my own promotion, which would be anxiety-provoking. After all, if the phonies are the ones who get promotions, there's no point in trying. If I tell myself that the academic system favors manipulative, dishonest individuals, it's like having a handicap, because I'm so honest. I can feel like a hero or martyr, and anything I do accomplish will seem wonderful. I can snap at people when I'm in a bad mood. This will keep them at a distance, and let them know that they have to treat me with respect. I didn't ask Jasper to list the disadvantages of his anger. Instead, I said this in an admiring tone of voice: "You know, Jasper, looking at all these advantages, it's not clear
Chapter 23
789
to me why you should give up your angry feelings. Your anger shows that you're a man of integrity with strong values and ethical principles. I'm convinced that you're morally superior to me, and I think that you might even be the most morally superior doctor in the entire United States right now!" Fortunately, this comment hit Jasper's funny bone, and he started to giggle. Then he explained all the reasons why his anger really was a problem. It alienated his family and colleagues and made him constantly unhappy. Furthermore, he was using up all his energy feeling resentful and helpless instead of doing creative research or compassionate clinical work with his patients. Then I said, "But you're telling yourself that it's unfair when a phony like that gets a promotion. To me, that sounds reasonable. It is unfair when phonies get ahead. It seems like you have every right to be angry." Jasper pointed out that he could obsess about his colleague forever, but it wouldn't do him any good. He said he was just making himself and his family miserable. Notice what happened. When I sided with Jasper's resistance, he suddenly argued for change. This reaction is almost as predictable as the law of gravity. But if I'd tried to "help" Jasper, he would have fought me. Now that we were on the same team, and Jasper had put the lie to his negative thought, I used the Externalization of Voices to cement his gains. I explained that I'd play the role of the negative voice in his brain that made him
Chapter 23
790
feel angry and resentful, and he could play the role of the positive, self-loving voice that refused to give in to the anger. Our dialogue went like this: Negative Voice (played by David): Jasper, you have every right to be angry. The phonies always get the promotions. Positive Voice (played by Jasper): That's only partially true. Phonies sometimes get rewarded, but hard, honest work gets rewarded, too. Sooner or later, he may be in for a fall. Negative Voice (played by David): That's just a rationalization. You know in your heart of hearts that he'll get tons of grants and all kinds of academic recognition because he kisses ass, and it's totally unfair! You should be angry. Your anger shows that you have high standards and won't put up with his B.S. Positive Voice (played by Jasper): Some anger may be justified, but enough is enough. Furthermore, I believe that I can compete with him successfully, but I need to swallow my pride and talk to the department chairman about my promotion. Negative Voice (played by David): Oh no, you shouldn't have to crawl and beg! That would be way too humiliating and anxiety-provoking. Besides, your department chairman should recognize your excellent research and outstanding clinical work and offer you a promotion. Positive Voice (played by Jasper): In an ideal world, everyone would admire my work and I wouldn't have to ask for a promotion. But the department chairman is probably more focused on his own duties than
Chapter 23
791
on keeping track of my research. When we've talked in the past, he's always been very supportive and interested in what I was doing, so there's no reason why I can't talk to him now and tactfully explain my feelings. Notice that I'm still siding with the Jasper who wants to be angry and resentful. As a result, he argues for change, and I don't have to struggle with his resistance. Jasper kept bursting out laughing when we were doing the Externalization of Voices. He said that the thoughts that had triggered his anger were clearly absurd. He seemed relieved, so I asked him to take the brief anger and depression tests, and his scores were both zero. He said it was the first time in years that he'd felt free of the feelings of resentment and inadequacy. Of course, a one-shot cure won't be sufficient. Jasper's angry thoughts are seductive and will definitely come back to plague him in the future. Psychotherapy homework and practice will be necessary to cement the gains he made during the session. All of that occurred in our first therapy session. One of my colleagues, Dr. Tony Bates, had done the intake interview and diagnostic screening for Jasper. Tony and I used to jog around Haverford College on Saturday mornings. While we were jogging, we'd often discuss difficult cases. The Saturday following my session with Jasper, I told Tony that Jasper had been really easy to work with and that all of his symptoms had disappeared in one session. Tony began to laugh and sarcastically exclaimed, "Sure they did!"
Chapter 23
792
I asked Tony what he meant, since we didn't seem to be on the same page. He said, "You're joking, right?" I said, "No, I'm not joking. Haven't you had patients who were really easy to treat? Jasper seems to be that kind of person." Tony looked incredulous and repeated, "You're joking, right?" I was puzzled and asked Tony why he thought I was joking. He asked if I'd looked at Jasper's diagnostic summary sheet. I explained that I hadn't gotten it yet. He said that Jasper was suffering from severe Borderline Personality Disorder (BPD). Of course, BPD is a difficult disorder, and the prognosis can be poor, even with prolonged, intensive treatment. I told Tony that he must be mistaken, and that he had to be thinking about some other patient. Tony insisted that Jasper was the exact patient he was referring to. I couldn't believe what he was telling me, so I checked the diagnostic summary sheet first thing Monday morning when I got to the clinic. Sure enough, Jasper was suffering from severe BPD. We were using the SCIDS Axis I and II structured diagnostic interview system with every new patient at the intake evaluation, and I could see that Jasper had every conceivable symptom of BPD, along with Dysthymic Disorder, Major Depression, and several other diagnoses. In spite of his severe diagnostic profile, the Paradoxical CBA and the Externalization of Voices had been incredibly helpful for Jasper. Why were they so effective? I think there were several reasons: He felt respected and accepted.
Chapter 23
793
He didn't feel that I was trying to change him. Once he verbalized all the reasons to let go of the anger, I gave him the tools he needed to transform this goal into an emotional reality. Some therapists are concerned that a Paradoxical CBA might be risky. Once you list all the advantages of the status quo, the patient might conclude that she or he really doesn't want to change. The patient might say, "I'm just here because my wife thinks I have a problem." If you were the therapist, how would you respond? Remember that empathy will nearly always be your best strategy when the patient resists. Write down exactly what you'd say to this patient. You can review the Five Secrets of Effective Communication on page 242. Put the names of the techniques you're using in parentheses after each sentence, using abbreviations:
Chapter 23
794
Answer You could say something like this: "Palmer, I'd know I'd hate to have to go to a therapist just because someone was pressuring me to go. (IF; TE) I can imagine that you're feeling pretty skeptical or even trapped. (FE) In fact, I wouldn't be surprised if you were feeling a bit ticked off at your wife. (FE) Can you tell me more about this? (IN)" After he responds, you can say something like this: "I want you to know that I don't work with people unless they have a pretty strong desire to be here. (IF) Don't get me wrong—I'd love to have the chance to work with you, or maybe even with you and your wife together, but this would have to be something you wanted. (ST) Can you tell me a bit more about the situation? (IN)" In this case, you're showing respect for your patient and letting him know that you're not going to chase after him or scapegoat him. You may discover that he doesn't have a meaningful therapeutic agenda and doesn't really want to be there. In that case, I'd tell him that I was reluctant to accept him as my patient, but if he changed his mind and wanted to consult with me at any point in the future, my door would always be open to him. The Paradoxical CBA is not just a technique, but a mindset. It represents a way of interacting with patients that may require a substantial change in your personal values and therapeutic style. Some therapists have trouble letting go of the idea that they're supposed to "help" all their patients. But if the person hasn't
Chapter 23
795
asked for help, they'll simply yes-but you, and the harder you try, the more resistant they'll become. Instead, you can raise this question: "Maybe this isn't something you want to work on right now." The wall of resistance may suddenly disappear, and your patients may tell you why they do want to change. If you listen in a warm and receptive way, you can let them persuade you that they really do want your help, and that they're ready, willing and able to do whatever it will take to change. Then you'll be in the driver's seat again. Earlier, I mentioned that a double paradox can sometimes help. You can ask the patient to list the advantages of the status quo and the disadvantages of change on a CBA. Of course, you wouldn't balance these lists against each other, because they don't represent competing options. A narcissistic Chinese woman named Eileen suffered from feelings of chronic depression, loneliness and bitterness. She consistently "forgot" to do any psychotherapy homework between sessions. A number of individuals in our clinic had interacted with Eileen, and they all had negative feelings about her because she could seem childishly demanding and completely preoccupied with herself. At every session, Eileen complained about all the snooty people who'd wronged her, and all the people who thought they were better than her. But she was reluctant to pinpoint any specific problems she wanted to work on. She liked to be the center of attention and seemed to have a never-ending appetite for therapeutic listening and support. Perhaps you've had an Eileen in your practice as well!
Chapter 23
796
One day, Eileen said, "Maybe I like feeling depressed." I told Eileen that she might be onto something and suggested we could list all the advantages of being depressed and all the disadvantages of getting better. Together, we came up with 15 advantages of being depressed, including: I get lots of attention from my husband. I don't have to cook or do any housework. He does everything for me. I don't have to go out and look for a job, which frightens me. I can play the role of victim. I can feel sorry for myself. I can complain about all the people who don't love me enough, especially my father and my sister. I can be angry all the time. I can feel special. I can frustrate Dr. Burns and show him that he can't control me or tell me what to do. I can justify drinking every night. I can take tranquilizers and get high whenever I want. We also came up with an impressive list of disadvantages of getting better. They included: I'll have to do my psychotherapy homework, which seems like being back in school again. I'll have to stop drinking and maybe even attend AA meetings. I'll have to cook and do housework.
Chapter 23
797
I might have to look for a job. There won't be any reason to meet with Dr. Burns. I won't feel special any more. I'll be ordinary, like everyone else. I'll have to develop better relationships with people. I'll have to do lots of things I've been putting off. I won't be able to complain about all the people who have wronged me. I'll lose my sense of identity. I'll no longer get to play the role of victim. I told Eileen that her depression seemed to be a good thing, and that her resistance to change made perfect sense. I said I was relieved to see that there were so many advantages of the depression, and so many disadvantages of recovering, especially since she scheduled two double sessions every week and was a full-fee patient. I told her that even though we sometimes seemed to argue or clash during sessions, she was one of my favorite people to fight with, and that I'd miss her if she recovered and we couldn't meet any more. I said I hoped she'd keep forgetting to do the homework assignments so we could work together for years to come. When Eileen returned for her session the next week, she proudly reported that she'd worked with the Daily Mood Log for half an hour every day. She'd stopped drinking and had already attended two AA meetings. She said she was feeling so much better that she thought she might be ready for termination within a few weeks. Eileen's suffering was real, but she'd resisted treatment for years. Her
Chapter 23
798
resistance was a reflection of her fears that the treatment might be effective, and that she'd have to say goodbye to her depression and bitterness–faithful friends that had served her well for many decades. 30. Devil's Advocate Technique The Devil's Advocate Technique is a role-playing version of the Paradoxical CBA. It's helpful for patients with bad habits or addictions, and I use it early in my work with them. It's easy to learn, and it's very rewarding for patient and therapist alike. You can use this technique effectively in group or individual therapy sessions. The Devil's Advocate Technique may not be sufficient to cure patients with habits or addictions, but it can be a powerful and necessary first step in your treatment program. It's similar to the Externalization of Voices, but easier to learn. Once you've mastered the Devil's Advocate Technique, you'll find the Externalization of Voices less intimidating. When you use the Externalization of Voices, the patient talks back to the negative, self-critical voice that creates feelings of depression, hopelessness, anxiety and worthlessness. In contrast, when you use the Devil's Advocate Technique, the patient talks back to the positive, tempting voice that persuades them to give in to their habit or addiction. On page 515, I described the positive thoughts that might tempt someone on a diet to give in to the urge to binge. You may recall some of those tempting thoughts: Mmmm, that donut would taste so good! I'll just have a bite or two.
Chapter 23
799
I can skip lunch or exercise later on to make up for it. I've had a tough day and I deserve it. Other people can eat whatever they want without getting fat. I have the right to enjoy myself, too. The Checklist of Cognitive Distortions on page 535 lists the 10 thinking errors that trigger feelings of depression, anxiety, and anger. Most therapists aren't aware that there's a corresponding list of positive distortions. Each positive distortion is the mirror image of one of the ten negative distortions. The positive distortions can trigger addictions, aggression and violence. For example, when the patient says, "I'll just have a bite or two," she's making an unrealistic positive prediction. This is an example of Fortune-Telling, since she never stops after just one bite. In addition, she's ignoring all the evidence that's inconsistent with her claim, so it's an example of Discounting the Negative. This is the opposite of Discounting the Positive. These positive distortions can be far more difficult to dispute than negative distortions, because they make patients feel good. If patients give in to them, they'll be instantly rewarded. Ask the patient to describe the kinds of thoughts they have when they're feeling tempted. Once you list them on paper, explain that you're going to play the role of the Devil and tempt them to give in to the urge to drink, overeat, or procrastinate. Tell the patient to resist you as forcefully as possible. The dialogue might go like this: Devil (played by you): Stacy, look at all those fresh, delicious glazed
Chapter 23
800
donuts. They just came out of the oven. Mmm, they smell so good! You really should try one. You can just take a bite or two and save the rest for later. Patient (playing self): No, I'm not going to do that, because I'll just lose control and end up gobbling down a whole bunch of donuts. Then I'll feel bloated and disgusted with myself. Devil (played by you): But even the dieting experts say that you should give yourself a treat every once in a while. Why should you have to be so pure? Those extremist approaches never work. Besides, you deserve it. You've had a tough day. Patient (playing self): Well, I also deserve to feel good about myself, and I'm not going to feel good about myself if I stuff myself with donuts. Devil (played by you): Stacy, one or two bites couldn't possibly make you feel bad about yourself. Besides, you can make up for it by exercising a little more later on, or cutting back on how much you eat for lunch. You can have a healthy green salad with no dressing, and a tall glass of grapefruit juice. The citric acid will burn off all the extra calories. Patient (playing self): I've listened to that kind of B.S. a thousand times, and it's never worked for me. I end up binging and feeling guilty, so I eat more donuts. Then I feel so bloated that I don't exercise at all. Devil (played by you): Stacy, you really shouldn't think that way. Remember that eating is a special sort of freedom, and those donuts are the best in the world. Just imagine how delicious that donut is going to
Chapter 23
801
taste when it touches your lips. Wow! It will better than sex! Go for it, Stacy. Go for it now! You deserve it! Just reach out and do the right thing, the thing you really want to do in your heart of hearts! Patient (playing self): Kiss off! I'm walking away from you right now. I refuse to listen to you any more! When you play the role of the Devil, you should try to be as seductive and persuasive as you possibly can. That's because the patient's thoughts will be at least this persuasive when they're standing at the bakery counter, struggling with temptation. Make sure you take a careful inventory of the patient's tempting thoughts before you start role-playing. That way, you'll have the proper ammunition to do a good job. If you tempt patients with seductive thoughts they don't really have, the technique will seem irrelevant and lose its punch. I do my best work when I side with the part of the patient's brain that really wants to give in and really can't see any good reason to change. If the patient has a tough time talking back to the tempting thoughts, it means that you're doing a good job. And if they can't defeat you during the role-playing, they definitely won't be able to resist the thoughts when they're alone and the temptation hits. For example, the patient may cave in and say, "You've got a good point. I think I will have a donut!" Then you can do a role-reversal and model a more effective response. Alternatively, you can say, "It sounds like that argument is going to win the day when you feel tempted. Perhaps you don't feel ready to change." If you do this with sincerity, the patient will have to convince you to treat them, and you won't have to persuade them to change.
Chapter 23
802
When I describe the Devil's Advocate Technique to patients, I tell them it's like buying your ticket to a show. You're simply not allowed into the theater until you've got your ticket. If you skip this step and try to "help" patients who aren't really motivated, the rest of your treatment program will be doomed to failure. The Devil's Advocate Technique allows patients to do battle with the powerful, seductive part of their minds that's always trying to defeat them. Once they can soundly defeat all of their tempting thoughts, the likelihood of successful treatment will be greatly enhanced. 31. Stimulus Control If patients are trying to break an addiction, such as alcoholism or overeating, they can reduce temptation rather than struggling with it. For example, they can eliminate all alcohol from their homes, avoid going to places where liquor is served, and stop purchasing alcoholic beverages at the store. Stimulus Control is not a complete treatment for any addiction, but can be a useful part of a more comprehensive program. This technique is crucial because sights, sounds and smells can trigger intense craving. Studies indicate that when heroin addicts return to their old neighborhoods after discharge from prison, they often go into withdrawal, even though they've been incarcerated and haven't used heroin or cocaine for years. The familiar sight of needles or people dealing drugs can trigger the physiologic withdrawal symptoms. Most people can only withstand so much temptation, and sooner or later, they'll give in. That's why it's so important to reduce the temptations in advance.
Chapter 23
803
Like the Devil's Advocate Technique, Stimulus Control is a good test of the patient's motivation. If patients resist this technique, they're telling you that they're not really willing to let go of their habit. 32. Decision-Making Form The Decision-Making Form is a sophisticated version of the Cost-Benefit Analysis. It helps patients make difficult decisions and reveals why they were stuck in the first place. It may seem a bit complex at first, but once you've used it with a patient, you'll see that's it actually pretty easy to use. Indecisive patients sometimes pressure us into giving them advice or telling them what to do. This may cater to our narcissism, because we get to play the role of expert. But if you give patients advice, you're asking for trouble. Your advice might not work out, and then you'll be in a pickle. The bad outcome will be your fault. The patient may lose confidence in you and drop out of therapy. Giving advice could even constitute an ethics violation. We're not there to tell patients how to lead their lives, but to give them the tools they need to make their own decisions. Patients may ask for help with all kinds of decisions, such as career decisions: "Should I stick it out in graduate school, and try to complete my Ph.D., or drop out and do something I really want to do?" Or, "Should I ask my boss for a raise or look for a new job?" Or, "Which college should I go to?" Decisions about personal relationships can also be stressful: "Should I get divorced or try marital therapy first?" Or, "Should I make a clean break with Donald, and make it clear that I'm not interested, or continue to see him as a
Chapter 23
804
friend?" Patients who struggle with habits or addictions are usually indecisive as well. They may say, "I really want to lose weight," or, "I really want to quit drinking," or, "I really want to stop procrastinating. My desk is a total mess, and I've been putting off my tax returns for months." But they don't always mean what they say. The patient who's overweight may really be saying, "I'd love to be thin and attractive, but I don't want to diet or exercise." The patient with a drinking problem may really be saying, "My wife keeps nagging me about my drinking, so I thought I'd drop in for a visit just to placate her." The patient who procrastinates may have the fantasy of how wonderful it would be to be caught up on things, but may not want to face the anxiety of doing all the odious chores that she or he's been putting off. If you take what the patient says at face value, you may run into frustration when they don't follow through. Let's face it, if patients really wanted to diet and exercise, they'd already be doing it! Very few of us want to diet and exercise. What we really want is to eat whatever we want, whenever we want, and magically be thin and attractive at the same time. The Decision-Making Form can often help patients who are ambivalent. Ask the patient to label the two competing options as Option A and Option B. Harry, the man who completed the Decision-Making Form on page 805 was trying to decide whether or not to go on a diet and start exercising. As you can see, Option A was "Continue to eat whatever I want" and Option B was "Start jogging and dieting."
Harry's Decision-Making Form Option
Describe
Total Points
A
Continue to eat whatever I want
B
Start jogging and dieting
Advantages of Option A
0 Disadvantages of Option A 1. 2. 3. 4.
1. It's great to eat whatever I want, whenever I want. 2. I love eating. Yum, yum! 3. It gives me something to look forward to. 4. It gives me a sense of freedom. 5. Nobody is telling me what to do. 6. Life is hard. I deserve some simple pleasures. 7. People should like me as I am. I shouldn't have to try to impress anybody.
5. 6. 7. 8.
1
2
50
50
9 95
5 45
1. I'll look fit and trim. 2. My clothes will fit. 3. People will have positive impressions of me. 4. I'll have more stamina. 5. I'll feel better about myself.
11
10 105
9. I don't want to take my shirt off at the beach. 10. I feel less sexy. 11. I feel inadequate.
1. I'll feel deprived of one of life's greatest pleasures. 2. Regular exercise takes a lot of discipline. I may 100 55 fail. 3. Regular exercise 4 12 seems like a pain in the ass at first. No fun. 4. Exercise is time-consuming, and I have too much to do right now. 5. I'm old and should be able to do whatever I want! Life is short! Enjoy it! 6. My friends and family will love me either way, 45 8
45 3
6. I'll have greater self-confidence. 7. I'll feel healthy. 8. Women will look at me again and then I'll feel sexier. 9. My family will feel like I'm taking care of myself.
Advantages of Option B
I look gross. My clothes don't fit. People may have poor impressions of me. I'm out of shape. I get short of breath easily, and it's hard to bend over. I have less stamina. I feel fat and have low self-esteem. My doctor says I have high blood pressure and high cholesterol. I sometimes feel defeated and discouraged.
55 7
6 55
100
-10
Disadvantages of Option B
Chapter 23
806
Encourage the patient to list all the advantages and disadvantages of these options in the appropriate quadrants. Then ask him to fold the paper in half across the middle so he can focus exclusively on Option A, while ignoring Option B. Ask him to balance the advantages against the disadvantages of Option A on a 100-point scale, just as you'd do with a CBA. As you can see, there was a dead heat—the ratings were 50 – 50. These ratings appear in circles 1 and 2. Now ask him to turn the paper over and balance the advantages against the disadvantages of Option B on a 100-point scale. As you can see, the disadvantages of jogging and dieting were slightly greater, so Harry put 45 – 55 in circles 3 and 4. At this point, you might be tempted to think that Option A is the winner, since Option B is slightly negative, but we're not done yet. Ask the patient to open the paper again, and fold it vertically in half, from top to bottom, so he can weigh the advantages of Option A against the advantages of Option B, while ignoring the disadvantages of both options. Harry can ask himself, "If there were no disadvantages of either option, which list of advantages would feel greater to me?" As you can see, the advantages of jogging and dieting won out by a rather narrow 55 – 45 margin. These numbers appear in circles 5 and 6. You might think that Harry would strongly prefer to be thin, attractive, and healthy, but those are long-term rewards. The rewards of eating are immediate and extremely appealing. In fact, hunger is a biologically determined drive, and it can be almost irresistible. That's why you have to be skeptical when patients tell you that they really want to lose weight. It may not be true.
Chapter 23
807
Finally, ask him to turn the paper over, so he can weigh the disadvantages of both options against each other, while ignoring the advantages. Now Harry can ask himself this question: "Which list of disadvantages feels greater?" Tell him to assign the larger number to the list that seems more odious. Harry put 55 – 45 in circles 7 and 8 because the disadvantages of overeating felt somewhat greater than the disadvantages of jogging and dieting. Now we can tally up the scores. The two numbers in the upper left-hand quadrant represent the advantages for Option A. These numbers—45 and 50— add up to 95. This is the total score for the advantages of Option A, and this number appears in circle 9. The two numbers in the upper right-hand quadrant—50 and 55—add up to 105. This is the total score for the disadvantages of Option A, and it appears in circle 10. The total score for Option A is simply the advantages (95) minus the disadvantages (105), or –10. Harry recorded this number at the top of the Decision-Making Form. Harry calculated the total points for Option B in the same way, and put 0 at the top of the page. How would you analyze these results? What do the cell-bycell comparisons, as well as the total points for each option, tell us? Put your ideas here. If you're unsure, you can just make an educated guess.
Chapter 23
808
Answer To my way of thinking, the two options are very similar, so I'd be tempted to say something like this to Harry: "I can see that you're struggling with this decision, but the results aren't really clear. Even though Option B came out slightly ahead, the two options aren't that far apart, and neither option is positive. I have the feeling that you're sitting on the fence. We both know that jogging and dieting will take a lot of discipline and determination, and I'm not convinced that you're ready to start working on this problem yet. Tell me more about how you're feeling." What have we gained? We've discovered that Harry is ambivalent. This doesn't mean that he's "bad" or "resistant." It simply means that he's not yet ready to change. It wouldn't be wise to forge ahead, because he'll almost definitely sabotage any weight loss program you offer, and he may feel like a failure when the treatment doesn't work. In contrast, we can acknowledge Harry's ambivalence and let him take the lead. Encourage him to express his feelings, and use your best listening skills. When he sees that you're not pushing, it may fire up his determination and he may decide that he really does want to lose weight. Or, he may decide that he's not ready, and that some other therapeutic agenda would be more appropriate. By the end of our session, Harry had decided that he definitely wasn't ready for dieting and exercising. Oddly enough, he decided to try jogging after he got home, and found it rewarding. When I saw him a week later, he'd already
Chapter 23
809
jogged five times. I advise patients that the results of the Decision-Making Form are not written in stone, and that they can redo it as many times as they want. It won't show them what the "correct" decision is, but will help them sort out their options and show where they stand right now. These feelings will probably change over time. When you use the Decision-Making Form, a number of interesting patterns can emerge, including: No Brainer. One option is strongly positive and the other option is negative or neutral. This decision will usually be easy because one of the options clearly seems superior. Can't-Lose. The scores for both options are strongly positive, so it probably won't make any difference which choice the patient makes. The patient can just flip a coin. Sometimes, patients in Can't-Lose situations feel tormented because they think they're supposed to make the "perfect" or "correct" decision. In reality, there may be no single best choice. Furthermore, any decision will have unanticipated positive and negative consequences that are impossible to predict. The secret to happiness usually has more to do with making a decision and moving ahead with your life with a creative and positive attitude, rather than waiting around until you've figured out what the "best" decision is. Can't-Win. In this pattern, the total scores for both options are strongly negative. This is the opposite of the Can't-Lose pattern. For example, if the
Chapter 23
810
total scores for Option A and B are -75 and -40, it will seem like both choices are bad, and the patient can't win no matter what they do. This result often happens when the patient is depressed and anxious, and distorting everything in a negative way. If so, cognitive therapy may be helpful. For example, a man named Paul was trying to decide whether to get divorced or stay married. Paul had a strong desire to get divorced, and listed many advantages of this option. At the same time, he was afraid that his friends and family would look down on him and reject him if he got divorced, so the disadvantages of this option were even greater than the advantages. Staying married was equally unappealing. Paul constantly fought with his wife and had no desire to try to resolve their problems. He clearly wanted out. On his Decision-Making Form, the total scores for getting divorced and staying married were both strongly negative. I suggested that Paul could test his negative thoughts about getting divorced with the Survey Technique. He told several friends that his marriage wasn't going very well and asked if they'd think less of him if he and Jennie separated. He discovered that several of them were also experiencing marital problems and that they weren't at all judgmental. Paul felt relieved and repeated the Decision-Making Form. This time, pursuing a divorce came out strongly positive, and remaining in his marriage was still strongly negative. When both options are negative, it's also possible that there are other options that the patient hasn't considered. I told Paul that he could still
Chapter 23
811
consider marital therapy or a trial separation. He compared these options with getting divorced, but decided that he really did want to leave his wife. Fence-Sitter. This was the situation that Harry found himself in. When both options hover around zero, the patient has no strong reason to choose either of them. This indicates ambivalence, and therapeutic empathy will usually be your most productive course. The Decision-Making Form is not something I use on a daily basis in my clinical work. I might use it once a month, or once a week at most. But when patients are agonizing over a difficult decision, or trying to decide whether to give up a bad habit or addiction, it often seems to be just the right tool. 33. Daily Activity Schedule Motivational paralysis is one of the cardinal symptoms of depression. Of course, when depressed patients do nothing, their demoralization intensifies. Depressed patients give up on life for many different reasons, including: Loss of interest. They may lose interest in their family, friends, and work, as well as hobbies or sports they once enjoyed. They feel convinced that these activities would no longer be rewarding, so they don't bother to try. Some depressed patients find pleasurable activities aversive because they feel so ashamed and think they deserve to suffer. Loss of self-esteem. Depressed individuals may avoid people because they feel worthless and unlovable. A depressed woman named Marilyn stopped answering her phone because she was convinced that every person who called would be the bearer of bad news. Of course, after a while, people
Chapter 23
812
stopped calling, and she took this as proof that everyone had rejected her. Hopelessness. Most depressed patients are convinced that their problems are insoluble and that their suffering will go on forever. Of course, once they give up, nothing changes, so they conclude that they really are hopeless. Love addiction. Some depressed patients believe that they can't feel truly happy or fulfilled without love. If a rejection or divorce triggered their depression, they may assume that they're bound to feel worthless and miserable as long as they're alone. Of course, this expectation also functions as a self-fulfilling prophecy, because they give up on life, avoid other people, and wallow in self-pity whenever they're alone. Almost any activity has a good chance of boosting a depressed individual's mood. In fact, Dr. Peter Lewinsohn's therapy for depression is based almost entirely on behavioral activation techniques (Lewinsohn, Munoz, & Youngren, 1986). Depressed patients are encouraged to participate in more rewarding activities, as well as activities that will help them achieve their goals. For example, if a depressed man feels lonely, his therapist might help him develop more rewarding relationships with other people. I'm not a fan of therapeutic reductionism, and it's hard to imagine that any single treatment method could ever be sufficient to treat all of our depressed patients. People are just too unique. There's no doubt that behavioral activation techniques can be helpful for some depressed patients, but if those were the only techniques I had available, my treatment options would seem way too limited. Dr. Neil Jacobson's studies with Behavioral Activation Therapy seem to
Chapter 23
813
support this view (Jacobson, Dobson, Truax, et al., 1996). By the end of a 20session treatment program, only 50% of the patients had achieved scores below 9 on the Beck Depression Inventory (BDI). Although scores below 10 indicate improvement, scores above 3 or 4 indicate that patients still feel somewhat depressed. Furthermore, half of the patients in the improved group relapsed during the two years following recovery, suggesting that they were still vulnerable to depression and may not have had sufficient training in relapse prevention. I've included several behavioral activation techniques on my list of 50 CBT techniques. They're relatively easy to learn and implement. The Daily Activity Schedule on page 814 was one of the first CBT techniques ever developed. It's simple. Patients record what they do at each hour of the day and rate each activity on a scale from 0 (not at all rewarding) to 5 (the most rewarding). This helps them grasp the connection between what they do and how they feel. Sometimes you'll discover that patients spend most of their time on passive activities, like watching TV, that are relatively unrewarding, and that activities that the patient rarely does, like jogging, turn out to be very rewarding. If patients are motivated, you can use this information to help them structure a more meaningful and rewarding schedule. 34. Pleasure Predicting Sheet The Daily Activity Schedule is rather primitive because it doesn't take the patient's thoughts or beliefs into account. You can get some mileage out of it, especially with passive, severely depressed patients who are doing very little, but it's definitely not one of the more potent CBT techniques.
Chapter 23
814
Daily Activity Schedule* Instructions: Record what you do each hour of the day. In parentheses, record how satisfying each activity was between 0 (not at all rewarding) and 5 (the most rewarding). Monday
Tuesday
Wednesday
Thursday
Morning
7:00 8:00 9:00 10:00 11:00
Afternoon
Noon 1:00 2:00 3:00 4:00 5:00 6:00 Evening
7:00 8:00 9:00 10:00 11:00
* Copyright
1992 by David D. Burns, MD.
Friday
Saturday
Sunday
Chapter 23
815
Pleasure Predicting Sheet* Activity Schedule activities with the potential for pleasure, learning, or personal growth.
Companion Who do you plan to do this with? Use "self" for things you plan to do alone.
* Copyright
Satisfaction Predicted (0% - 100%)
Actual (0% - 100%)
Record before each activity.
Record after each activity.
1980 by David D. Burns, MD.
Chapter 23
816
After using the Daily Activity Schedule for several years, I developed a more sophisticated behavioral activation technique called the Pleasure Predicting Sheet, which appears on page 815. The Pleasure Predicting Sheet takes the depressed patient's cognitions and behaviors into account simultaneously. In the Activity column, patients can schedule activities with the potential for pleasure, learning, or personal growth. If they can't think of anything that seems rewarding or worthwhile, they can schedule activities that used to be enjoyable, even if they don't think they'll be very satisfying now. They can include activities they can do by themselves, such as jogging, reading or getting caught up on paperwork, as well as activities they can do with other people, such as going to a movie with a friend. In the Companion column, they can indicate who they plan to do each activity with. I tell them not to put the word "alone" in this column. Instead, they can use the word "self" as a reminder that they're never truly alone. In the Predicted Satisfaction column, patients can predict how satisfying or rewarding each activity will be on a scale from 0% (not at all satisfying) to 100% (the most satisfying). Make sure they record these predictions before they do each activity. After they've completed each activity, they can record how satisfying it turned out to be in the Actual Satisfaction column, using the same scale. When you examine the Actual Satisfaction column with the patient, you'll see how pleasurable and rewarding the various activities turned out to be. When you compare the Predicted and Actual Satisfaction columns, you'll often discover
Chapter 23
817
that some activities turn out to be significantly less rewarding than they expected, while others turn out to be substantially more rewarding than they expected. This helps patients see how off base their negative expectations can be. For example, Marilyn, the woman on page 811 who stopped answering her phone, was convinced that no one liked her any more. To test this belief, she agreed to call a friend and invite her out to lunch. Marilyn felt certain that her friend would spurn her and predicted that the call would be 0% satisfying. Marilyn was shocked when her friend said she'd been missing her and would love to join her for lunch. Marilyn's ratings for the phone call and the luncheon were over 90%. This experience greatly boosted her mood. In fact, you could argue that the reduction in her depression was the direct result of the change in her negative thoughts. You can also use the Pleasure Predicting Sheet to test certain kinds of Self-Defeating Beliefs, such as the Love Addiction. An accountant named Mark became depressed when he discovered that his wife was having an affair with one of the senior partners at the law firm where she worked. She soon moved out and filed for divorce. Mark was crushed and convinced he'd be depressed forever. At the top of a Pleasure Predicting Sheet, I told him to write, "I could never feel happy or fulfilled without Marsha's love." He believed this 100%. I encouraged Mark to test this belief by scheduling activities he could do by himself, activities with other people, and activities with Marsha. He was convinced that the activities he did by himself or with other people would be unpleasant and unrewarding, so his predictions were all below 20%. In contrast,
Chapter 23
818
he felt like anything he did with Marsha would be wonderful. For example, Marsha had suggested they meet for lunch later in the week so they could discuss the details of their divorce. Mark predicted that this meeting would be 95% satisfying, since he'd be able to spend some time with her. He had fantasies that he could win back her love. He told me how gorgeous and brilliant she was, and said his life could never be meaningful or exciting without her. He said he felt like he was a rather dull person, and that she was one of the "beautiful people" who "had it all." Mark was surprised by the results of his experiment. The activities he did on his own turned out to be far more satisfying than he expected. For example, he'd been so depressed that he'd almost completely abandoned his accounting business, and had been moping around at home for several weeks doing almost nothing. He forced himself to go to work, and ended up spending several hours straightening up his desk, answering phone calls and getting caught up on things. This turned out to be 90% satisfying, although he'd only predicted 10%. He also went on a blind date that a friend arranged. He predicted it would only be 5% satisfying, but he had a terrific time and gave it a 95% rating. Finally, he had lunch with Marsha. It was a miserable experience because she spent the entire time talking about how wonderful her new lover was, so he gave it a 0% rating. The data were hardly consistent with Mark's belief that Marsha was the source of all happiness. This led to a dramatic shift in his mindset, and within a few weeks, his depression was gone. He terminated treatment shortly after that, and sent me a thank-you note two months later, right after the first of the year.
Chapter 23
819
He told me that he'd spent New Year's Eve alone, and although he never would have believed it, it was one of the most rewarding holidays he'd ever experienced. Many people who use the Pleasure Predicting Sheet make similar discoveries. They find that they can be just as happy when they're by themselves as when they're with other people. This can be a tremendous source of selfconfidence, and can put the lie to the belief that the only true happiness comes from loving relationships with other people. Many patients experience a real boost in self-esteem when they realize that they don't really need others to feel good about themselves. Paradoxically, this awareness often leads to better relationships, because they no longer appear so desperate or afraid of rejection. 35. Anti-Procrastination Sheet Patients who procrastinate usually give themselves messages like this when they think about the tasks they're putting off: I don't feel like it right now. I'm not in the mood. It's going to be overwhelming. It's going to be incredibly boring. It will make me too anxious. I can't even stand to think about it. I don't have enough time today. I have more important things to do. Anything I do right now would only be a drop in the bucket, so there's no
Chapter 23
820
point in trying. Tomorrow will be a better day. I shouldn't have to do this in the first place. It's unfair! I just can't get started. This always happens! What's wrong with me? I must be lazy. Check off all the distortions you can find in these thoughts. Feel free to review the Checklist of Cognitive Distortions on page 535. Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 23
821
Answer I think you can make a pretty solid case for all ten distortions. Distortion
Yes
Explanation
1.
All-or-Nothing Thinking
You tell yourself that if you can't complete the whole job today, there's no point in doing any of it.
2.
Overgeneralization
You tell yourself that you always procrastinate, but in fact, you only procrastinate on a few things that seem particularly odious to you.
3.
Mental Filter
You think about all the things you haven't done, and overlook the many things you have done.
4.
Discounting the Positive
You tell yourself that anything you do won't count because there's so much more to do.
5.
Jumping to Conclusions Mind-Reading Fortune-Telling
You predict that the task will be a terribly unpleasant experience. (Fortune-Telling).
6.
Magnification and Minimization
You exaggerate how overwhelming the task will be, so it mushrooms to the size of Mt. Everest.
7.
Emotional Reasoning
You reason from how you feel. The task feels awful, so you conclude that it really is awful.
8.
Should Statements
You tell yourself you shouldn't have to do such irritating, menial tasks. You may also tell yourself that you really should do it anyway. These messages create feelings of frustration, anxiety and guilt, so you can't even stand to think about the task, much less get started on it.
9.
Labeling
You label yourself as "lazy" and tell yourself you can't get started, but you really mean that you don't want to.
10. Blame Self-Blame Other-Blame
You blame yourself for not having done the task, or you blame fate and tell yourself it's unfair that you should have to do it.
Although these thoughts are unrealistic, they function as self-fulfilling prophecies. For example, if patients label themselves as "lazy" and tell themselves that they just "can't" get started, they'll put the job off. After all, that's what a "lazy" person does. Then they conclude, "Sure enough, I really must be
Chapter 23
822
lazy. What's wrong with me?" Patients can record these thoughts on a Daily Mood Log and attack them with a variety of CBT techniques. The Anti-Procrastination Sheet on page 823 is one method you might use. It's a modification of the Pleasure Predicting Sheet. You encourage the patient to break large, overwhelming tasks down into small steps that they can complete in just a few minutes. They can list each step in the Task column. In the next two columns, they can predict how difficult and how satisfying each step will be on a scale from 0% – 100%. After they complete each step, they can record how difficult and satisfying it actually turned out to be in the last two columns. Patients sometimes discover that the task is far less difficult and much more rewarding than they expected. This will often motivate them to do even more than they planned. They may discover that their procrastination was based on a kind of mental hoax. After we moved from Pennsylvania to California in 1995, our garage was filled with junk for eight years. There were dozens of boxes of research data, old books, and things we'd shipped to the West Coast with us. We ignored the mess because cleaning the garage seemed like such an overwhelming and unrewarding task. In addition, I was pretty sure there were rats and spiders out there, so I was afraid of what we might run into once we started rummaging around.
Chapter 23
823
The Anti-Procrastination Sheet* Task Break the task into small steps. Number each step.
Predicted Difficulty
Predicted Satisfaction
(0% – 100%)
(0% – 100%)
* Copyright
1978 by David D. Burns, MD.
Actual Difficulty (0% – 100%)
Actual Satisfaction (0% – 100%)
Chapter 23
824
And then, there was all the anxiety of making decisions. Do we need this? Do we need that? Should I throw this away? How about that? To make the first step really easy, I decided I'd simply step into the garage, turn the light on, and look around. That only took about 30 seconds, and wasn't especially difficult. I made the second step equally simple. I decided to open one box to see what was inside. It was pretty interesting. The box was stuffed with office supplies, like old staplers, pencil sharpeners, obsolete software, and computer cables. It was obvious that if I hadn't needed any of that stuff by now, I was never going to need it. So I pushed that box into a "bring to the dump" pile. My wife and son were eager to get the job done, so they pitched in as well. We spent several Saturday afternoons on it, and it wasn't bad at all. One afternoon, we listened to a Stanford basketball game on the radio while we were cleaning. Stanford came back from one of their biggest fourth quarter deficits in history and maintained their #1 national ranking. Before we knew it, we'd gotten rid of nearly everything and the garage was as clean as a whistle. Some patients have asked, "What if I don't feel rewarded or motivated after I get started? What if the task really is upsetting and difficult?" That's a possibility. Some tasks will never be fun, and patients may never enjoy doing them, even after they've gotten started. Of course, they won't know for sure until they've given it a try. You can ask the patient if they want to do the task in spite of the fact that it may be anxiety-provoking. If they'd decide to avoid the task, that's not a problem. You can simply suggest another agenda for the session.
Chapter 23
825
Other Anti-Procrastination Techniques Procrastination is a slippery problem to treat. Over the years, I began to view it as more of an addiction than a problem patients really wanted or needed help with. It dawned on me that some patients were looking for magical solutions that required no effort, while others were asking for help out of a sense of guilt, because someone else—like a parent, spouse or employer—was pressuring them to get their act together. If you try to "help" these patients, you can get locked into a power struggle with the rebellious part of their personality. Their procrastination suddenly becomes your problem, as if you're supposed to solve it for them. This enables them to keep procrastinating without guilt. The Socratic Method can help you avoid this trap. You ask a series of questions about the type of help the patient is looking for. This process often leads to the absurdity behind the idea that they can't do the thing they're procrastinating on. I once treated a physician named Perry who had trouble getting up in the morning. Perry suffered from chronic mild depression and feelings of inadequacy. Instead of getting up and going to the hospital to make rounds each morning, he'd sleep in. Then he'd get up late and start rounds after lunch. This was stressful because he was constantly behind and scrambling to get caught up on his work. Perry explained that he'd tried everything, including the use of several alarm clocks at the same time. He'd place each one a little further from his bed, and set them to go off at intervals. But it was totally useless, because he'd simply
Chapter 23
826
get up when the first one rang and turn them all off. Then he'd crawl happily back into bed and drift into a deep, satisfying sleep. Perry had been locked into the same pattern for years. He said he just couldn't get up in the morning and really needed my help. I told him I'd be more than happy to help him, but said I wanted to be clear on the type of help he was looking for. What, exactly, was the problem he needed my help with? He said he thought he'd already made that clear. He needed help getting out of bed in the morning. I said I'd be pleased to help him get out of bed, and suggested that we could break the job down into its tiniest parts. What would he have to do first? What would he have to do second? We came up with the following steps: 1. Open my eyes. 2. Move my right leg to the edge of the bed. 3. Swing my left leg over to the edge of the bed. 4. Sit up on the edge of the bed. 5. Stand up next to the bed. 6. Walk into the bathroom. Then I said, "Let's look at the first step. Is that something you need my help with? For example, do your eyelids feel heavy and sticky? Do you forcefully try to open them, only to discover that they're frozen shut?" Perry seemed perplexed and said he'd never had any problems opening his eyes. I said, "Okay, then maybe you need help with the second and third
Chapter 23
827
steps, moving your legs over to the edge of the bed. Do they feel especially stiff or heavy? Perhaps we could practice this part here in the office. Try swinging your left leg back and forth now, so I can watch and see what happens." Perry seemed annoyed and said he could obviously move his legs over to the edge of the bed. Then I said, "Perry, I apologize if my questions seem foolish. I really do want to help you, but it still isn't clear to me exactly what you need my help with. Can you clarify that for me?" This is the essence of the Socratic Method. You shift the responsibility back to the patient by asking questions about the type of help they think they need. We're not trying to punish the patient. Instead, we're projecting a therapeutic message. Patients will say, "I just can't seem to get started," but what they really mean is, "I don't want to!" Suppose that Perry said, "You just don't understand. I need help with motivation. I don't feel like getting out of bed in the morning. That's why I sleep in." If you were his therapist, what would you say or do next? Put your ideas here before you continue reading:
Chapter 23
828
Answer Perry is putting the cart before the horse. Like so many people who procrastinate, he thinks he's entitled to feel motivated before he tackles the problem he's avoiding. To me, this isn't realistic. We're not entitled to feel motivated to do the things we've been putting off. Highly productive people know that action comes first, and motivation follows. If you wait until you "feel" like doing some unpleasant task, you'll be waiting forever! Personally, I feel anxious when I start doing tasks I've been putting off. I don't feel motivated until I'm well into the task. Sometimes I don't feel motivated until the task is nearly completed. Of course, patients are entitled to avoid discomfort, but if they don't want to confront their fears, than I can't agree to help them with their anxiety. This is a basic principle of Agenda Setting—you have to ask yourself if the type of help the patient wants makes sense. After all, we're not obligated to rush in and do the patient's bidding! Other strategies you could pursue with Perry might include the Paradoxical CBA. Ask him to list all the good reasons for staying in bed, and all the justifications that flow through his mind when he decides to sleep in. Then ask him why he'd want to give them up, since they all seem compelling. You could also use the Devil's Advocate Technique. You'd play the role of the part of his mind that tempts him to stay in bed, and see if he can defeat you. I often use the Problem-Solution Method with procrastinators as well. Let's say the patient wants help with some task she or he has been putting off, such as
Chapter 23
829
straightening up their desk. I ask the patient what day she or he would like to get started on it. If they say, "tomorrow," I tell them I can only help them with the problem today, because putting things off until tomorrow is the very essence of the problem. If they agree to work on it today, I ask them what time they want to work on it. Let's say they agree to work on their desk at 3 PM. Then I ask them if they'd be willing to work on it for a very limited amount of time, such as five or ten minutes. If they protest and say it isn't worth it because it would only be a drop in the bucket, I remind them of the Buddhist saying that the longest journeys start with a single step. If they're not willing to take that step, I won't be able to help them. Five minutes of an odious task is manageable. If they try to take on too much, they'll probably feel overwhelmed and avoid the task forever. If they agree to work on it for five minutes, I ask them to list every conceivable type of problem that might distract them and prevent them from following through at 3 PM. They can record all the potential obstacles in the lefthand column of the Problem-Solution list below. I ask them to put the solution to each problem in the right-hand column. If they ask for help, I encourage them to come up with the answer on their own, because the answers are nearly always obvious. If they still can't figure out the solutions, then they're probably not trying. If you give in and try to help them, they'll start yes-butting you, and the problem will become your responsibility again.
Chapter 23
830
Problem
Solution
1. Someone may call and I'll tell myself that I really need to talk to them. 2. I'll tell myself that I need to watch the news, to make sure that nothing important is happening. 3. One of the kids might need my help with something. 4. I'll tell myself that I'm not in the mood, and that tomorrow will be a better day. 5. I may get hungry and decide that I have to have a snack first, so I'll have enough energy. 6. I may decide that I have to lie down and rest for a while, so I don't get all tired out. 7. I may tell myself that I'd be better off if I went out and did some jogging first. 8. I may decide that it's not really as important as I thought. Once the patient has come up with solutions for all the problems they can think of, I give them one last assignment. Let's assume that they've agreed to work on straightening up their desk between 3:00 and 3:05 PM. I ask them if they'd be willing to call and leave one of two messages on my answering machine at 3:05. They can either say, "Mission accomplished," or "I stubbornly refused." Most patients will agree to make the call, but some refuse. Over the years,
Chapter 23
831
every patient who agreed to call my office actually completed the assignment. In contrast, every patient who refused failed to complete the assignment. Therefore, this is one last test of the patient's motivation. If patients say they don't want to call, for any reason, I tell them it would probably be better not to follow through on the assignment, because they still seem to have mixed feelings. Notice that this Problem-Solution strategy leads to the same result as the Socratic Method. There really is no invisible barrier holding the patient back, and they won't need a lot of fancy footwork to solve the problem.
24*
Exposure Techniques
Exposure is one of the most extensively researched psychotherapy techniques ever developed. Many experts are convinced that you cannot treat anxiety effectively without it. In this chapter, you'll learn about several Classical Exposure Techniques, such as Flooding, Gradual Exposure, and Response Prevention, as well as many innovative Cognitive and Interpersonal Exposure Techniques. When I give my Scared Stiff workshop, I ask how many of the therapists in the audience routinely use Exposure Techniques in their work with anxious patients. Usually, about half of the hands go up. This boggles my mind. I'm surprised that so many therapists seem to be disregarding a massive body of scientific literature that validates exposure. In fact, I'm not even sure what it would mean to treat someone with an anxiety disorder without exposure. For example, how could you possibly treat a phobia, like the fear of heights, if the patient refused to confront this fear? What would successful treatment even look * Copyright
2003 by David D. Burns, M.D.
Chapter 24
833
like? This concept makes no sense to me. At the same time, I wouldn't want to oversell any technique, including exposure. Exposure is nearly always useful for anxiety, but it may not be curative, and if I had to limit myself to just one type of technique, my effectiveness would be severely limited. That why I use a wide variety of techniques in my work with every anxious patient I treat, including Basic Techniques, Cognitive Techniques, Uncovering Techniques, Motivational Techniques, and Exposure Techniques. Classical Exposure Techniques 36. Gradual Exposure and Flooding During my sophomore year of high school, I wanted to be on the stage crew for the school's production of Brigadoon. The drama teacher, Mr. Cranston, told me that people on the stage crew had to climb tall ladders and crawl around on the scaffolding near the ceiling so they could adjust the lights. I told him that this might be a problem for me, since I was afraid of heights. Mr. Cranston said that I couldn't be a member of the stage crew unless I was willing to get over this fear. I asked how I could do that. He said it was simple. He set up a 20-foot ladder at the center of the stage and told me to climb up and stand on the top rung. I was fairly trusting and followed his advice. But when I got to the top, it dawned on me that there was nothing to hang on to up there, and I was terrified! I asked him what I was supposed to do next. He said I didn't have to do anything except stay there for a while. He waited for me at the bottom of the ladder and encouraged me to stick it out.
Chapter 24
834
I was absolutely petrified for about 15 minutes. Then my fear suddenly started to diminish. A minute or two later, it disappeared completely. I excitedly announced, "Mr. Cranston, I think I'm cured now. I'm not afraid of heights any more." He said, "That's great, David! Welcome to the stage crew!" I was proud to be a member of the stage crew and found that I loved crawling around on the scaffolding near the ceiling and adjusting the lights. It was surprising that something I'd feared so intensely had become so thrilling. Obviously, Mr. Cranston wasn't a therapist, but he'd treated me with a Classical Exposure Technique called Flooding. I exposed myself to my worst fear and didn't fight or struggle with the anxiety. Instead, I surrendered and allowed myself to be flooded with fear. Flooding is more terrifying, but often works rapidly. In my case, a single treatment was curative. Alternatively, a patient with the fear of heights could go up a ladder one step at a time, and pause at each step until the anxiety diminished or disappeared. This would be an example of Gradual Exposure. Gradual Exposure is less traumatic but takes longer. Both approaches have been successful in the treatment of nearly all forms of anxiety. I once treated a young woman named Dolly who was suffering from agoraphobia. She was dependent on her husband and couldn't leave home without him or some other person she trusted. I proposed an innovative form of Gradual Exposure I'd heard about during a presentation by Dr. Stanley Rachman at a meeting of the Association for the
Chapter 24
835
Advancement of Behavior Therapy (AABT). You encourage agoraphobic patients to confront their fear of being outdoors alone, but there's a slight twist. The patient always moves toward a trusted friend, rather than simply enduring the unknown alone. Dolly was motivated and agreed to give it a try. I set up a double session so we'd have plenty of time to try the new technique. Dr. Steve Ristvedt was working at my co-therapist at the time as part of his psychology training at the University of Pennsylvania. He wanted to join us so he could learn how to use this technique with his own patients. Dolly was fine with this. The three of us left my office together. Dolly trusted us, and wasn't afraid as long as she was with us. We asked her to wait alone on a street corner while we walked ahead one block. We explained that we'd wait for her at the next corner while she walked toward us. She was frightened, but somewhat reassured to know that she'd be with us again in a couple minutes. Walking one block alone was a small but important victory for her. Then we increased the distance to two blocks, and waited for her again. Each time Dolly reached us, we increased the distance by another block. Eventually, we increased the distance to a half-mile. Although she was terrified when she was walking alone, she knew that we'd be waiting for her. This gave her the courage to continue. She was surprised that she actually made it, and seemed pleased with herself. I asked Dolly if she'd be up to trying a full mile. She was anxious, because this meant she'd be alone outdoors for at least 20 minutes, but said she'd try.
Chapter 24
836
I explained that Steve and I would walk to the Girard Bank building on the corner of 36th and Market, right across the street from the University of Pennsylvania campus, and wait for her there. I instructed her to give us a tenminute head start, and then she could begin walking towards us. While Steve and I were walking, he asked for a consultation about an anxious businessman he was treating. The man had collapsed at work six months earlier because of a heart attack. After his discharge from the hospital, he developed an intense fear of fainting. I asked Steve what his patient was so afraid of. Why did it seem so terrible to faint? Steve explained that the fellow wasn't afraid of death, but was petrified of fainting in public because he thought he'd look weak or foolish. In addition, if he was on the ground, people would literally be looking down on him. This idea made him anxious. I suggested that Steve might try a Shame-Attacking Exercise for his patient. Specifically, I proposed that the man could go to downtown Philadelphia at noon, when the streets were crowded with people going to lunch. Then he could lie down on the sidewalk for several minutes. That way, he could get over his fear of lying on the ground in public while people looked down on him. Steve got excited and said it was a splendid idea. He said he'd definitely recommend this as a homework assignment for his patient at their next session. By this time, Steve and I had arrived at the corner of 36th and Market. There were lots of food trucks parked there. It was noon, and dozens of people
Chapter 24
837
were lining up to buy lunch. I said, "You know, Steve, I believe there's an ethics rule that says you should never ask a patient to do anything that you wouldn't be willing to do yourself. Does that sound reasonable?" Steve said he was familiar with this concept and agreed with it. I said, "Well, Steve, this is your chance. There are lots of people here. Why don't you lie down on the sidewalk right now? You can do a ShameAttacking Exercise." Steve seemed intensely embarrassed and insisted he couldn't possibly do that! He pointed out that the psychology building was right across the street and was concerned that his professors might see him and think he'd lost it. I pointed out that he was whining and resisting, and asked how he could expect his patient to try this if he wasn't willing to do it himself. Steve said, "Okay, if you think it's so easy, I'd like to see you do it!" I said, "Sure, Steve, no problem!" I lay down on the sidewalk and propped my head on my hands. It was surprisingly comfortable. People were stepping over me to get to the food trucks, but no one seemed to care that I was lying there. They seemed far more interested in getting their cheese steaks and fries. I said, "See, Steve, it's easy. It's really nice down here, too. It's kind of like being on the beach in Miami. Why don't you lie down here next to me? We can talk some more about therapeutic strategies while we wait for Dolly." Steve decided to go for it, so he lay down on the sidewalk next to me. The whole thing seemed perfectly natural, and we had a great time discussing cases.
Chapter 24
838
While we were lying there talking, I realized there was a disheveled, bearded man sitting on a brick wall ten feet from us, talking in tongues, waving his hands in the air, and shouting at the sky. No one was paying any attention to him, either! Ten minutes later, Dolly arrived and found us lying on the sidewalk. I explained that we'd been doing a Shame-Attacking Exercise while we were waiting. She hardly seemed to notice what I was saying but said she felt absolutely exhilarated that she'd made the entire distance alone. We all walked back to the hospital feeling elated about our achievements that afternoon. Should you use Gradual Exposure or Flooding? It's mainly a matter of personal preference. Both methods can be effective. By way of analogy, let's say you're going swimming in Lake Tahoe in California. The water is cold, even in the summer! You can go in slowly, inch by inch, or you can jump in all at once. For me, the gradual approach is like slow torture. It seems easier to jump in and get it over with. But if Flooding seems too overwhelming or threatening to your patient, you can use Gradual Exposure. You can get the job done either way. If you're using Gradual Exposure, you can help the patient prepare a Fear Hierarchy like the one on page 841. This will help them break the exposure into small, increasingly challenging steps. They can work their way up the hierarchy one step at a time. I once treated a young businessman named Andre who suffered from panic attacks. During each panic attack, his chest would get tight and he'd tell himself that he was on the verge of a massive heart attack. He was so convinced
Chapter 24
839
he was about to die that he'd sit motionless, desperately hoping that his heart wouldn't fail, until the attack passed. Andre had been to numerous doctors who all told him that there was nothing wrong with his heart, but their reassurances didn't seem to last more than a few days, until the next panic attack. I encouraged Andre to use the Experimental Technique. The next time he had a panic attack at home, he could do some strenuous exercise. For example, he could run up and down the stairs in his apartment. That way, he could to test his belief that he was about to die. Obviously, if he really was on the verge of cardiac arrest, strenuous exercise would be impossible. Andre was shocked. He insisted that the experiment I proposed was totally irresponsible and dangerous, and refused to do it. I suggested that he could start by doing something really mild instead. For example, the next time he had a panic attack, he could slowly raise one arm above his head while he sat in his chair. Then, if his heart was still beating, he could raise both arms above his head. If that went okay, he could slowly stand up. Then, if he still felt okay, he could take one small step forward. If he didn't keel over and die, he could take several slow steps forward. This idea appealed to Andre. We developed a list of increasingly strenuous activities to help him test his belief that he was about to have a heart attack. This was his Fear Hierarchy: 1.
Raise my arms above my head.
2.
Stand up slowly and take one small step forward.
3.
Take several slow steps forward.
Chapter 24 4.
Take several steps more rapidly.
5.
Walk all the way to the stairs.
6.
Walk up one step slowly.
7.
Walk up several steps slowly.
8.
Walk up several steps rapidly.
9.
Walk all the way up and down the stairs.
840
10. Run up and down the stairs at high speed. Andre agreed to do at least the first few steps, because they seemed reasonably safe, but wouldn't promise that he'd do much more than that. Several days later, Andre had a panic attack. He remembered his Fear Hierarchy, and cautiously raised one arm above his head. He was surprised when nothing happened. Then he raised both arms, and found that he was still alive. He stood up very slowly and took one step forward, but still didn't keel over. Andre felt encouraged and continued working his way up his hierarchy. Soon, he was zooming up and down the stairs in his apartment at full speed. When there were no adverse consequences, it dawned on him that he couldn't possibly be having a heart attack, and his panic vanished completely. Some therapists like to use a modified version of Gradual Exposure called Systematic Desensitization. You induce a state of deep relaxation in the patient, using hypnosis or a relaxation technique. When the patient feels deeply relaxed, you can ask him or her to imagine proceeding slowly up their Fear Hierarchy, level by level. They don't proceed to the next level until they've achieved deep relaxation at the level they're at.
Chapter 24
841
My Fear Hierarchy Instructions. Develop a hierarchy of feared situations. List the least frightening situation first, and the most frightening situation last. Describe your phobia: Rating 1
2
3
4
5
6
7
8
9
10
What I Fear
Chapter 24
842
There are many ways to induce a state of relaxation. You can ask the patient to sit in a comfortable position and close their eyes. Then they can imagine a peaceful scene, like lying on a quiet beach or sitting on the porch of a cabin in the woods. Any scene that appeals to the patient will do. While the patient pictures the peaceful scene, you can say: "Imagine that all your problems have been solved and all your fears have vanished. The bills have been paid, and any conflicts or problems with other people have been resolved. You feel happy, peaceful, and close to everyone. "It's beautiful here on the beach. You can hear the waves breaking, and you can see the blue sky and white clouds. You can feel the warm sand under your back. "Concentrate on your breathing. Breathe slowly and deeply. Picture the air going in and out of your nose as a white mist. If your mind wanders, bring it gently back and concentrate on your breathing, and on what I'm saying to you." You may want to use direct hypnotic suggestions, and say things like this: "You're falling into a deep, deep sleep. You're slipping deeper and deeper, deeper and deeper. You're feeling relaxed and peaceful. Nothing will bother you or disturb you. Concentrate on the sound of my voice." You can also ask the patient to concentrate on a single word, such as "Om." Tell them to close their eyes and try to picture the word floating in front of them. They may discover that their mind wanders. Tell them that this is perfectly
Chapter 24
843
okay, and when they notice it happening, they can simply focus on the word, "Om," again. Alternatively, you can try relaxation exercises. Have the patient close their eyes and squeeze their right hand into a tight fist. Tell them to imagine that they're squeezing all the tension and worry out of their body. After ten or fifteen seconds, they can relax their hand. As it goes limp, tell them to imagine it's like butter melting in the sun, and that all the tension in their body is draining out of that hand. Then you can repeat the exercise with their left hand. Tell them to tighten it into a fist, and let it go limp as the tension slowly drains away. You can repeat this with the right foot, the left foot, the right arm, the left arm, the stomach, and the chest. Finally, tell them to scrunch up their face into a tense, angry grimace, and then let their facial muscles relax as the tension drains away. Tell them that their mouth may open slightly as their neck and jaw relaxes. If your patients like the relaxation exercises, they can practice them at home between sessions and modify them in any way that makes sense to them. For example, they may want to start the relaxation exercise at the top of their heads and work their way down to their toes, tightening and then relaxing every muscle group as they proceed. Patients can also purchase relaxation tapes at health food stores, music stores or bookstores. Someone with a soothing voice will guide them through a relaxation procedure as they hear peaceful music or the sound of ocean waves in the background.
Chapter 24
844
You can use relaxation procedures in several ways. As noted above, you can combine relaxation with real or imagined exposure in an attempt to make the exposure less stressful for the patient. Patients can also practice relaxation before doing something that makes them anxious, such as giving a talk at work. And of course, many people like to meditate for a certain period each day as a general practice, so they can cope with stress more effectively and develop a more spiritual perspective on life. Relaxation techniques can be very helpful for some people, but they don't appeal to everybody. I used them frequently early in my practice, but drifted away from them when I began to learn about CBT, which seemed more powerful and interesting. To be honest, I got tired of talking at my patients while they sat there relaxing with their eyes closed. It seemed like I was doing all the work, and it was rather boring! Recently, I've had a change of heart. I now believe we might be able to use relaxation, meditation and hypnosis to good advantage in our work with at least some patients. If you like these techniques, and they work for you, you should certainly include them in your toolbox. 37. Response Prevention As you know, many anxious patients become addicted to superstitious rituals to ward off danger. For example, a man with a contamination phobia may compulsively wash his hands 50 times a day in spite of his rational understanding that his hands are not really contaminated, and that the frequent washing is unnecessary and even damaging to his skin. Or, he may get out of bed several
Chapter 24
845
times to check the burners on the kitchen stove before he goes to sleep, even though he's rationally aware that they were off the last time he checked them, and that they rarely turn on by themselves! A life insurance salesman named Howard had the urge to shout, "Dark! Dark! Dark!" every night when he parked his car in the garage after work. Although he knew this was nonsensical, he couldn't resist the urge and had the superstitious belief that this practice would somehow keep his family safe. One day, Howard invited a colleague over for dinner following a successful business meeting, and they drove to his house together. When he pulled into the garage, Howard nervously realized that he'd have to suppress his urge to shout, or else he'd look like a total nut. While they were having a drink in the living room before dinner, Howard became anxious about the fact that he hadn't done his shouting yet. It started eating away at him, and he had trouble concentrating on the conversation. Finally, he said that he'd left his appointment book in the car and had to go out and get it. Once he was in the garage, he did his shouting and felt relieved. What Howard didn't realize was that his wife and colleague could clearly hear him shouting "Dark! Dark! Dark!" When Howard went back inside, his wife took him aside and explained that his guest had heard him. Howard felt profoundly embarrassed and made up a lame excuse that they'd been having problems with rats, and that he had to scare them away by shouting in the
Chapter 24
846
garage every night!* Response Prevention is a simple intervention that's based on common sense, and it's probably been around for hundreds, if not thousands, of years. You simply tell the patient to stop performing the ritual, no matter how anxious they get. For example, if the patient has a powerful compulsion to keep checking the locks on the doors every day before driving to work, you can tell her to force herself to stop doing this. She's allowed to check the doors once when she leaves the house, but no more. Explain that her anxiety will temporarily get worse, but if she refuses to give in, her urges to perform this ritual will probably diminish greatly within a few days. Response Prevention can be effective for any type of compulsive ritual, and in most cases, the rituals quickly disappear. Unfortunately, Response Prevention is less effective for the anxiety itself. Even when patients lose the urge to perform their rituals, they'll usually still be plagued by fears and obsessions. That's why it's important to include a wide variety of techniques in the treatment of all the anxiety disorders. 38. Distraction This is a simple technique that can be combined with Exposure and Response Prevention. Essentially, patients distract themselves from their upsetting thoughts or fantasies by concentrating on something else or getting involved in a strenuous physical or mental activity. Admittedly, I've never thought of Distraction as a very powerful or useful technique. The main problem, as I see * Several of the examples in this section were adapted, with permission, from my book,
Chapter 24
847
it, is that patients may get into a struggle with their negative thoughts when they try to ignore them. The struggle energizes the system, so the thoughts may increase in intensity. That's why I prefer other CBT techniques. However, Distraction can sometimes be effective. You may recall Kristin, the woman who was afraid to leave home alone because she had fantasies of being arrested and thrown in jail. When she sat on a bench in New York's Central Park, she was flooded with fear, so she concentrated on her Rubik's Cube. The Distraction helped her endure the intense anxiety she felt when a police officer approached the bench she was sitting on. In Chapter 6, we discussed some of the controversies surrounding EMDR and TFT. There's no doubt that the practitioners of these new approaches experience success with many patients, but it's not clear whether the techniques they use—for example, tapping on a particular body part such as the eyebrow or clavicle—are effective, or whether these techniques simply represent forms of Distraction. In addition, it's unclear whether the eye movement of EMDR or the finger tapping of TFT actually enhance the effectiveness of the Exposure Techniques they're always paired with. Finally, these techniques may simply represent forms of hypnosis. For example, during EMDR, the patient stares at the therapist's moving finger while the therapist makes a variety of suggestions and modifies the frightening images in the patient's mind. The dialogue surrounding EMDR and TFT is heated. An ideal scientific test of their efficacy might be to compare "pseudo EMDR" or "pseudo TFT" with the real thing. But in order to perform a definitive study such as this, the Worried Sick.
Chapter 24
848
proponents of these treatment methods would have to be willing to define the difference between "true EMDR" and "pseudo EMDR," or between "true TFT" and "pseudo TFT." This research strategy intrigues me because of an article on biofeedback that I reviewed for one of the behavioral science journals. The authors compared "pseudo biofeedback" with real biofeedback in the treatment of anxiety. The pseudo biofeedback consisted of random feedback that was not related to any changes in the subjects' muscle tone or brain wave activity. As it turned out, both groups of patients learned to relax, but there was no statistically significant difference in the degree of improvement in the patients who received "pseudo biofeedback" and the patients who received true biofeedback. The study indicated that biofeedback had no specific anti-anxiety effects, above and beyond its placebo effects. It was a well-designed and executed study, and I recommended publication. If we were all willing to hold our methods up to that kind of high-level scrutiny, I think our field would move forward more rapidly. There's certainly no harm in Distraction, TFT, or EMDR. If you like these procedures and find that they help your patients endure the intense anxiety that occurs during exposure, I can't see any reason not to use them. But it would probably be premature to jump to conclusions about their efficacy or mechanism of action at this time. Further studies will be needed to address these questions. Cognitive Exposure Techniques We know that anxious patients can't always confront their fears in reality.
Chapter 24
849
For example, patients with PTSD may be haunted by terrifying memories of traumatic experiences that happened many years ago. If a patient has a fear of being struck by lightning, dying in an airplane crash, or losing control and shouting obscenities during church services, it's hard to see how the Classical Exposure Techniques, like Gradual Exposure or Flooding, would work! Fortunately, patients can confront these kinds of fears in imagination using techniques like Cognitive Flooding, Image Substitution, and Memory Rescripting. 39. Cognitive Flooding When patients use Cognitive Flooding, they intentionally flood themselves with the painful memories or frightening fantasies they've been trying to avoid. They can try to make themselves as anxious and upset as possible, and simply endure the anxiety without fighting it. After a period of time, the anxiety will usually burn itself out and the images will lose their power to upset the patient. Sometimes this happens rapidly. You may recall reading about a therapist named Melinda who told me about her fear of flying during one of my workshops. Melinda was upset because she and her fiancé planned to get married at his parents' home in France, which meant that she'd have to endure a long airplane flight across the ocean. I asked Melinda to close her eyes and visualize what she was the most afraid of. She imagined the airplane shaking violently in bad weather and crashing toward the earth while all the passengers screamed in terror. Her anxiety instantly shot up to 100%. After just a few minutes of Cognitive Flooding, it disappeared.
Chapter 24
850
Sometimes, the desensitization to the fantasies can take longer. In my book, Worried Sick, I described a new mother named Theresa who developed an anxiety-producing obsession shortly after her son was born. She began to worry that her baby might have been switched with another baby at the hospital, and that she'd ended up with the wrong one. Rationally, she realized that this was extremely unlikely, but couldn't seem to shake the obsession from her mind. Theresa's son had been born via Caesarian section. While she was in the recovery room, the doctor explained that he'd accidentally nicked the baby's heel with his scalpel during the delivery. He reassured her that the cut wasn't serious and would heal up nicely. Aside from that, everything had gone smoothly. When Theresa held her son for the first time, she immediately examined his foot. Sure enough, he had a small cut on his heel in the exact spot the doctor had described. Theresa was flooded with feelings of joy and relief. But soon, she began to wonder if the cut was in the right location on his heel. If not, it would mean she had another baby with a cut on his foot, and not her own child. Although she realized that this idea was totally absurd, she couldn't shake the obsession from her mind. She began checking her baby's foot 20 – 30 times a day in an attempt to reassure herself that she had the right baby. By now, Theresa had developed full-blown Obsessive-Compulsive Disorder. Her obsessive thought was, "I might have the wrong baby," and her compulsion was the overwhelming urge to keep checking his foot. I tried more than 30 techniques to help her overcome this fear, but none of them helped her at all. I wondered if she had mixed feelings about being a
Chapter 24
851
mother that she hadn't owned up to, since I knew that she'd had a successful career as a corporate executive at the time she became pregnant. I explored this possibility with her, but the idea didn't seem to be on target. One day, I used the What-If Technique to see if I could find out why Theresa was so worried. Suppose she did have the wrong baby—what then? What frightening fantasy was at the root of her fears? Our dialogue went like this: David: Theresa, we know rationally that this is your baby. But suppose it turned out that he wasn't your baby, but someone else's. Obviously, no one would want the wrong baby, but I'm wondering what this would mean to you. What if you did have someone else's baby? Why would that be upsetting to you? Theresa: It would mean that someone else has my baby. David: Okay. Let's assume that someone else does have your baby. Why would that be upsetting to you? What are you the most afraid of? Theresa: Well, maybe the people with my baby are kidnappers, or bad people who abuse children. David: That sounds truly awful. But let's suppose that happened. What are you the most afraid of? What do you picture in your mind's eye? Theresa reluctantly described a horrible scenario. In her fantasy, sadistic kidnappers have taken her little boy to a cabin in the desert south of the Mexican border. She told me that she could see one of the kidnappers holding her baby by his foot and swinging him through the air, smashing his head against the wall. Then they throw him down the stairs and kick him around, like a basketball.
Chapter 24
852
Finally, they lock his broken and bleeding body in a dark closet. Theresa sobbed as she described the fantasy. On a scale from 0% – 100%, she said she felt 100% anxious and upset, the absolute worst. I was concerned that I was hurting her, since even I felt uneasy, and wondered if I should back off. At the same time, it seemed like we'd finally gotten to the bottom of her fears. I reminded myself that patients have to confront the monster they fear the most if they want to recover completely. If they turn away, the problem intensifies. I encouraged Theresa to stick with the fantasy and endure the anxiety for as long as possible. Her anxiety stayed at 100% and didn't decrease at all. I told Theresa that I felt badly about making her so miserable, and reminded her about the rationale for Cognitive Flooding. I told her I hoped she'd continue using this technique, but reassured her that we could use some other method if it seemed too overwhelming. Theresa bravely said that she'd try, and agreed to practice at home for 15 minutes each day. I told her not to do anything to try to make her anxiety go away, and explained that if she felt extremely anxious, it meant that we were probably on the right track. At the next session, Theresa explained that she hadn't done any Cognitive Flooding on her own because it seemed too upsetting. However, she was willing to try it again in the office with my support. We spent the entire session with the same horrible fantasies, but once again, Theresa's anxiety did not diminish. I reemphasized the importance of practice at home, since it can take time
Chapter 24
853
to get over these fears. Theresa made a firm commitment to practice for at least 15 minutes every day, no matter how upsetting it was. The next week, Theresa reported that the first few times she'd tried it, she'd gotten intensely upset, but on her fourth try, the fantasies began to seem unrealistic and her anxiety diminished. The fifth time she tried it, the fantasies seemed totally absurd, and her anxiety disappeared completely. Theresa said she had no more doubts at all that this was her son, and no more urges to check his foot. Her anxiety had vanished, and she finally felt excited to be mother. She terminated therapy the following week. You might be thinking that the treatment was just too gruesome, and that there had to be a better way. That was exactly my thinking as well. But I'd already tried many techniques that hadn't been helpful. I'm convinced the results were worth the discomfort we both had to endure. Some therapists are concerned that Cognitive Flooding might retraumatize a patient who's endured a terrible ordeal in the past, and victimize them once again. One of my greatest problems as a teacher is that therapists sometimes think about applying techniques in a vacuum, without looking at the larger therapeutic context. You'll need a strong therapeutic alliance and a motivated patient before you can use any technique. If you try to impose a technique on a reluctant patient, you'll be asking for trouble. The patient will resist and may act out in order to punish you. Then you might conclude that the technique was ineffective or inappropriate, when the real cause of the failure was a lack of trust and collaboration.
Chapter 24
854
Theresa and I had a positive therapeutic alliance, and I'd routinely received perfect scores from her on the Therapeutic Empathy scale. In addition, she was highly motivated and determined to beat the problem that was plaguing her. 40. Image Substitution When you use Image Substitution, you substitute a more positive or peaceful image for the frightening one, in much the same way that a movie director modifies a scene in a film. For example, a patient with the fear of flying can fantasize landing safely and greeting her family or relaxing on the beach in the warm sun every time a frightening fantasy of a plane crash pops into her mind. Suppose you feel nervous about a talk you have to give. You may imagine standing nervously in front of the crowd, trembling and stumbling over your words. In your fantasy, your mind goes blank and you can't remember what you were supposed to say. The audience begins to chuckle. Everyone looks bored and people begin to sneak out. By the end of your talk, three-quarters of the audience have disappeared and the few who remain are snoring and drooling. You feel totally humiliated as you slink off the stage. Each time this fantasy pops into your mind, you'll feel panicky and inadequate. It's almost as if you're giving yourself post-hypnotic suggestions: "I'm going to fail. I'm going to screw up. I'm going to blow it." By the time you give your talk, you'll have worked yourself into such an anxious state that you may mumble and read your presentation nervously instead of speaking directly to the
Chapter 24
855
audience in an enthusiastic and spontaneous manner. Of course, the people in the audience will sense your tension and feel just as bored as you feared. You'll feel like a victim, and won't realize that you choreographed the entire scenario. Instead, you can practice Image Substitution each night just before you go to sleep. You can start with the negative fantasy, and then switch to a more positive fantasy at the height of your anxiety. For example, you could visualize the people in the audience smiling and looking interested as you explain your ideas. Instead of reading from a written text, you can picture yourself talking to the people in the audience in the same friendly way that you might talk to a good friend who was interested in your work. At the end, you can imagine people telling you how much they enjoyed your talk and congratulating you on a job well done. Although these positive fantasies may not seem realistic at first, they have a way of reprogramming your expectations and feelings, and will often function as self-fulfilling prophecies. Patients can also do Image Substitution spontaneously throughout the day. Every time they notice an upsetting fantasy, they can substitute a more positive image. They can also combine Image Substitution with Self-Monitoring, and count the negative thoughts and fantasies on a wrist counter throughout the day. Although Image Substitution is most often used for anxiety disorders, it can be helpful for patients who are depressed and angry as well. An attractive marketing executive named Edna had been having a passionate love affair with a cute, semi-professional baseball player named Matt. Although she promised
Chapter 24
856
herself that she wouldn't take the relationship seriously, Edna soon realized she was falling in love with Matt, and asked him if he was ready for a long-term commitment. Matt became evasive and tried to change the subject. Edna's anxiety increased, so she pushed a bit harder. Matt told her he needed some space, and their relationship was soon ancient history. Edna had gone through the exact same pattern over and over again. As long as things were light and fun, her relationships with men were glorious. But the moment she tried to get serious, the man she was dating suddenly ran in the opposite direction. Edna felt doomed to spending her life alone. Edna had two goals in therapy. First, she wanted help overcoming her feelings of loss and longing for Matt. Second, she wanted to know how to develop a healthy, enduring relationship with a man she loved and respected. Edna's suffering resulted from her negative thoughts about the relationship with Matt, as well as the fantasies that flowed across her mind. She was telling herself things like this: I'll never find another man like Matt. He was so wonderful. I'll end up a lonely old maid. At the same time, Edna tortured herself with memories of the best moments she and Matt had enjoyed together. In her mind's eye, she'd picture the two of them making love or having fun at a party. These images made her intensely sad and triggered feelings of hopelessness, frustration, and inadequacy. When Edna wasn't thinking about Matt, she felt much better and
Chapter 24
857
was able to carry on with her life. But each time a positive memory of Matt popped into her mind, she crashed. Our mental images can be just as distorted as our thoughts. Edna's fantasies were filled with positive distortions. She only thought about the most idyllic moments she'd shared with Matt, and filtered out his many shortcomings. I asked Edna if she had any negative memories about Matt. She said that although he was good looking and a great party animal, he seemed shallow. He rarely opened up or talked about his feelings, so she often felt lonely, even when they were together. He was preoccupied with himself, and didn't show much interest in other people. Whenever she tried to talk about anything meaningful, Matt changed the subject or talked about baseball. And when she expressed her feelings, Matt tuned out or put her down. In addition, Matt was always giving other women the eye. I suggested that every time Edna had a positive, romantic memory about Matt, she could substitute one of these negative memories. We practiced this during the session. I asked Edna to close her eyes, relax, and visualize something positive about Matt. She pictured the first time they made love, and was flooded with feelings of sadness. Then I asked her to switch to a negative memory. She pictured a time when she discovered Matt groping a sexy woman in the kitchen when they were at a party together. Her sadness instantly disappeared, and she felt angry. Although this was a simple intervention, it combated Edna's tendency to idealize him. We also worked on Edna's cognitions. When she told herself that she'd
Chapter 24
858
lost the perfect man, she was involved in All-or-Nothing Thinking, Overgeneralization, Mental Filter, Fortune-Telling, Emotional Reasoning, Magnification, and Self-Blame. Although Matt was sexy and cute, he was also superficial, narcissistic, insensitive, and untrustworthy. Furthermore, he wasn't interested in a meaningful relationship. I pointed out that it might actually be a good thing if she didn't have to waste her time with another guy like Matt in the future. After working with these thoughts on the Daily Mood Log, we used the Externalization of Voices. In this example, Edna is playing the role of her negative thoughts, and I'm playing the role of her positive thoughts: Negative Thoughts (played by Edna): You know, Matt was the ideal man, and you lost him. Positive Thoughts (played by David): It's true that I lost him, and he was definitely sexy and charming, but he was far from my ideal man. He didn't know how to share his feelings and he wasn't at all loyal. He was great eye candy, and he was good for a quick roll in the hay, but he wasn't good for a whole lot more than that. Negative Thoughts (played by Edna): That may be true, but the fact is, you'll never find another man like him. Positive Thoughts (played by David): All human beings are unique, so it's true that I'll never find someone else who's just like Matt. To be honest with you, that's a relief. If I did find someone exactly like Matt, I'd have to go through that whole dreadful experience again. No thanks! I'm
Chapter 24
859
looking for someone who's different from Matt. I'd like a man I can really connect with, someone who will be a lover and a friend. Negative Thoughts (played by Edna): Then you're out of luck. You'll never find anyone like that. All the good men are taken. You're destined to be an old maid. Positive Thoughts (played by David): That's a lot of horseshit. I've dated tons of guys in the past, and there have always been lots of men who were attracted to me. But I probably need to change my approach, and I definitely need to stop chasing superficial men who don't have any real interest in a meaningful relationship. Negative Thoughts (played by Edna): That's just the problem. You know in your heart of hearts that you're never going to learn. You've been trapped in this pattern for years, and you'll be trapped in it for the rest of your life. Positive Thoughts (played by David): There's no evidence for that. It's just more of your horseshit. I actually learn pretty quickly when I put my mind to it. In fact, I've already made a big step in the right direction, and I've learned to stop listening to your bull! In Edna's case, Image Substitution and the Externalization of Voices dovetailed. Image Substitution provided her with a convenient tool to zap the painful memories as they occurred throughout the day. The Externalization of Voices helped her put the lie to her negative thoughts about Matt at the gut level. 41. Memory Rescripting
Chapter 24
860
Individuals with PTSD are often plagued by painful, intrusive, horrifying memories of traumatic events, such as rape or violence. A Vietnam veteran with PTSD described discovering the dead bodies of his buddies near the edge of a river. They'd been horrendously mutilated and murdered, with gaping wounds and their ears cut off. Decades later, these images still created feelings of rage and horror. Because these kinds of memories trigger such intense feelings of panic and helplessness, patients nearly always struggle to control them or shut them out of their minds. Of course, avoidance always makes anxiety worse, so the memories become more and more intense. A depressed and anxious patient named Jeremy described his childhood experiences as a Boy Scout. Jeremy's father insisted that he faithfully attend all the scout meetings and go on every camping trip so he'd learn to be trustworthy, obedient, and brave, and develop the qualities of citizenship, service, and leadership. Jeremy's scouting experiences were not exactly what his father imagined. Jeremy told me how the scoutmaster and some of the older scouts would drag him out into the woods late at night, when all the other scouts were sleeping, so they could sexually abuse him. He felt so ashamed that he never told his father about what was happening. The vivid memories still aroused powerful feelings of helplessness, fear, worthlessness, and humiliation. Memory Rescripting is a combination of Cognitive Flooding and Image Substitution that was designed for people suffering from PTSD. There are two steps. First, the patient visualizes the traumatic event and surrenders to the
Chapter 24
861
feelings of horror, shame, and fear. This is Cognitive Flooding. Cognitive Flooding alone might be sufficient for most patients with PTSD. However, with Memory Rescripting, you can do more. At the height of the patient's distress, they can modify the painful memories so the outcome is different. This is Image Substitution. For example, Jeremy might want to appear in the woods as a powerful adult and punish the scoutmaster and older boys who abused him. He could also comfort the little boy, tell him that he loves him and reassure him that it's not his fault. When the traumatic event occurred, patients were usually helpless. For example, when Jeremy was abused in the woods, there was little or nothing he could do to stop it. Jeremy didn't realize that he was now victimizing himself every time he pictured the horrible scene in exactly the same way it happened originally. Memory Rescripting can empower patients, because it puts them in control and takes them out of the role of victim. However, the patient, and not the therapist, must create the new scenario, and this is where you may run into problems. Some patients get in touch with feelings of intense anger and rage that have been buried for years. The sadistic revenge fantasies they sometimes create can be disturbing and may create an ethical and practical dilemma for you. Should you allow them to indulge in these violent fantasies, or encourage them to go in a different direction? The answer isn't straightforward. If you try to control angry feelings or fantasies, they will paradoxically increase in intensity because they'll suddenly be forbidden. On the other hand, you may be concerned that if you allow patients to
Chapter 24
862
indulge in their most violent fantasies, your "therapeutic" intervention might backfire and trigger a violent act with catastrophic consequences. This isn't a trivial concern, because many of the people who are most in need of Memory Rescripting are severely disturbed individuals who occasionally do act out and threaten suicide or aggressive acts. If you've treated patients with Axis II problems, such as Borderline Personality Disorder, you're already aware of this. And if you treat Vietnam veterans with PTSD, you know that some of them have murdered innocent people, so it's not out of the realm of possibility. Whenever you're in doubt, screen the patient carefully and obtain a consultation from a colleague first. Be sure to document your consultation in the chart. Because this technique often activates intense, frightening feelings, I only use it with patients who like and trust me. In addition, I only use this technique with patients who can distinguish fantasy from reality. I avoid this technique with paranoid or delusional patients, as well as those with a history of violence or suicide attempts. Of course, you should always clearly explain any procedure to the patient, and obtain informed consent before implementing it. You might conclude that Memory Rescripting is too dangerous and not worth the risk. By the same token, we sometimes need more aggressive procedures to help difficult, refractory patients. Coronary artery bypass surgery was also considered very risky in the early days, and many patients died on the operating table. And yet, the surgery frequently saved lives and relieved the excruciating pain of intractable angina, so it was definitely worth the risk. Memory Rescripting is not a panacea. In many cases, it won't be effective.
Chapter 24
863
If you use it in a thoughtful and sensitive way, it can be very helpful for selected patients, but I'd never impose any technique on a patient based on his or her diagnosis. Nevertheless, there are many new PTSD treatment programs for veterans and other trauma victims that are based almost exclusively on Cognitive Exposure Techniques. Can you think of any potential problems with this approach? The problem is that the therapists in these programs set the agenda for the patients. They decide ahead of time what kinds of problems will be addressed and which tools they'll use to treat them. Of course, this is the prototypic therapeutic error. While some patients will be motivated and will respond positively, others will resist. Then the therapists find themselves in the position of trying to persuade skeptical patients that the techniques really will work. Most of the time, persuasive strategies simply trigger more resistance. When you read about Cognitive Flooding or Memory Rescripting, you may be tempted to think, "Oh, now I know how to treat patients with PTSD!" This type of thinking may be intellectually appealing, because it means that you'll only have to learn one or two techniques for PTSD, or for any disorder you treat. It's also emotionally appealing because you get to play the role of expert. You'll think you know what's wrong with your patients and how to save them. Although this dynamic may fuel our narcissism, it frequently leads to frustration and failure. Many patients will resist because you're setting the agenda. Then you may jump to the conclusion that they're being stubborn or just don't want to get better. In the final analysis, Agenda Setting will always be the
Chapter 24
864
key to effective clinical work, no matter what diagnosis the patient has. Other Cognitive Exposure Techniques You can do any of the Cognitive Exposure Techniques, such as Cognitive Flooding, Image Substitution, and Memory Rescripting, under hypnosis. You could also think of Worry Breaks (page 642), the Feared Fantasy (page 670), and the Acceptance Paradox (page 683) as Cognitive Exposure Techniques. These techniques can be helpful for patients suffering from shyness, performance anxiety, perfectionism, or fears of disapproval. Interpersonal Exposure Techniques The techniques in this section are geared toward patients who struggle with shyness, although a few of them have other applications as well. These techniques may seem interesting or even fun from your perspective, but most shy patients will find them intensely frightening and will be reluctant to use them. As you already know, the best time to deal with resistance is at the Agenda Setting step. If patients want help with their shyness, but don't feel "ready" for techniques like these, I tell them that I'd love to work with them, but can't agree to treat their shyness yet, given their reluctance to confront their fears. If they have some other problem they want help with, we can work on it together. If they change their mind about Interpersonal Exposure later on, we can tackle their shyness as well. This type of paradoxical intervention protects you from having to drag reluctant patients along by their heels. It's crucial not to impose these or any techniques on patients simply because they're struggling with loneliness, social anxiety, or any other problem.
Chapter 24
865
Instead, empathize and set the therapeutic agenda at every therapy session. If a patient wants help with shyness, ask them to describe a specific moment when they felt shy and anxious. Where were they? What was going on? What were they thinking and feeling? If the patient is motivated and willing to try Interpersonal Exposure, you can generate a Daily Mood Log and ask the patient to choose one negative thought they'd like to work on first. Then select at least 15 techniques you could use to challenge the thought, including several Interpersonal Exposure Techniques and a variety of other techniques as well. This will allow you to create an individualized treatment plan specifically designed for each patient. In my book, Intimate Connections, I include descriptions of all the Interpersonal Exposure Techniques, along with many other useful treatment techniques for shy and lonely individuals. That book greatly expands on the techniques described here and may be a useful resource for patients who are having a difficult time in the dating arena. 42. Smile and Hello Practice This is a simple technique that can be quite challenging for shy patients. Instruct them to smile and say hello to at least 10 strangers every day. They can put tick marks on a 3x5 card to track how many people respond to them in a positive, neutral or negative way. If you ask them to predict how people will respond, you can compare their expectations with what actually happens after they start interacting with other people. Keep in mind that the results will vary in different parts of the country. A
Chapter 24
866
colleague and I once smiled and said hello to more than 50 strangers in under 20 minutes while walking around Rockefeller Center in New York City. Very few people smiled back or even acknowledged our greeting. But when I've done the same thing in smaller cities, most people have smiled in a friendly way and returned my greeting. 43. David Letterman Technique Shy patients often suffer from two Self-Defeating Beliefs called the Spotlight Fallacy and the Brushfire Fallacy. When they interact with people, they feel like a performer onstage under a spotlight, and think they have to impress the other person in order to be liked and accepted. Of course, they're afraid that the other person won't be impressed with their performance. They imagine that the word will spread like brushfire, and pretty soon, nearly everyone will be looking down on them and thinking they're weird. These beliefs aren't especially valid. Most of the people we meet in social settings aren't terribly interested in us. They're far more interested in themselves. They want to hear about how great they are and how interesting they are, and not how interesting we are. When you try to impress people and talk about yourself, other people usually get bored or turned off pretty quickly. Shy individuals can overcome this trap by learning the same communication techniques used by successful talk show hosts, like David Letterman and Jay Leno, who can instantly generate fascinating conversations with practically anybody. In fact, they're so good at it that millions of people watch them every night on television. How do they do it? They actually use the Five
Chapter 24
867
Secrets of Effective Communication that we discussed in Chapter 9. The basic idea is that you focus the spotlight on the other person in a friendly and admiring way, rather than struggling to impress them by talking about yourself. Here's a quick review: The Disarming Technique. Find truth in what the other person is saying, even if it sounds boring or off base. Thought and Feeling Empathy. Paraphrase what the other person just said, using their own words, and acknowledge how they're probably feeling, based on what they said. Inquiry. Ask the other person to tell you more about their ideas and feelings. "I Feel" Statements. This technique is overrated and often won't be necessary. You don't usually need to talk a great deal about yourself when you're getting to know someone. Instead, you can keep the other person in the spotlight, and make them feel special and important. Stroking. Imagine that the other person has a sign tattooed on their forehead that reads, "I want to feel important!" Find genuine ways to compliment them for their ideas and interests. After you explain these techniques and the underlying philosophy to your patient, you can practice with role-playing. You can ask the patient if there's a particular kind of person she or he would find especially threatening or difficult to interact with. In the example below, the patient is playing the role of an unbelievably boring fellow named Jarvis who I've just met at a cocktail party. My job will be to entice him into a fascinating conversation. I'll indicate which
Chapter 24
868
techniques I'm using in parentheses following each sentence: David: I'm glad to meet you, Jarvis. (ST) What do you do? (IN) Patient (as Jarvis): I study dust for a living. David: You study dust? (TE; IN) That sounds intriguing. (ST) I've never met anyone who studied dust before, but I'll bet it's fascinating. (ST) In fact, I recently learned on TV that there are regions in the universe where there are incredible dust showers consisting entirely of diamonds. (DT) What kind of dust do you study? (IN) Patient (as Jarvis): I study mummy dust. I'm an archeologist. David: Really? (IN) Mummy dust? (TE; IN) That's cool! (ST) I'll bet you can learn all kinds of fascinating things from mummy dust. (DT; ST) Tell me more about it. (IN) No matter what the other person says, you can always find a way to make it interesting if you use the Disarming Technique, Thought Empathy, Inquiry, and Stroking. Once the patient sees how easy it is to set the other person at ease and trigger an animated discussion, you can do a role-reversal so the patient will get the hang of it as well. The patient's fears may be different. Many shy individuals aren't particularly afraid of having to interact with someone who's boring. Instead, they're afraid of having to talk to someone who's extremely successful and narcissistic. In the next example, the patient will play the role of an incredibly attractive, successful CEO named Dirk who constantly talks about all his accomplishments:
Chapter 24
869
David: Hi, Dirk, glad to meet you. (ST) What do you do? (IN) Patient (as Dirk): I buy and sell large corporations. I'm the CEO of Big Bucks. David: Oh, I've heard all about Big Bucks. (ST) I read a really neat article about you in the San Francisco Chronicle last Sunday. (ST) Patient (as Dirk): Well, I try to do my share of interviews. Of course, as you might imagine, I can only respond to a few of the many requests I get. I thought that one might inspire people because they traced my success all the way back to my successful lemonade franchise when I was only seven. Since then, pretty much everything I've touched has turned to gold. David: That's awesome. (ST) What's the secret of your success? (ST; IN) Do you attribute it to creativity, hard work, courage, or something else? (ST; IN) In this conversation, you probably wouldn't have to do much more than ask flattering questions. Narcissistic individuals crave admiration, so it's easy to get them eating out of your hand. All you have to do is prime the pump, and the rest takes care of itself. The patient may complain that this way of responding would be phony. It is a bit phony, but sometimes you have to blow a little smoke in the other person's face to get things moving. Social conversation is a kind of dance you do in order to develop relationships with other people. Once you get to know the person, you can be more open about your own ideas and feelings. Initially, it's a
Chapter 24
870
lot easier, and far more effective, to focus the conversation on them. The Five Secrets of Effective Communication will provide the structure for creating animated, rewarding conversations with virtually anyone. Once your patients get good at these techniques in your office, they can start to initiate conversations with strangers as homework. When they report back to you about their experiences, you can help them with any interactions that didn't go as well as they hoped. Although this is a communication technique, it's also an Exposure Technique, and it will be intensely anxiety-provoking at first. By the same token, once the patient begins to engage in friendly conversations with people, they'll probably experience a significant reduction in their feelings of shyness and insecurity, along with a marked increase in their interpersonal success. 44. Self-Disclosure Instead of hiding their feelings of shyness or nervousness, patients can disclose them openly. This technique is based on the notion that shyness is not the real problem. The real problem is the shame that surrounds the shyness. Without the shame, shyness can actually be an asset. In The Feeling Good Handbook, I described a computer programmer named Paul who was extremely shy. He always tried to hide his shyness because he was convinced that women would look down on him if they knew how awkward and insecure he felt in social situations. Paul had been an attractive child, and his parents had often said, "Oh, you're so handsome! All the girls are going to adore you when you get older." This message put Paul under a
Chapter 24
871
great deal of pressure, because he felt like he was supposed to be a ladies' man and have lots of girlfriends. This belief intensified the feelings of selfconsciousness and inadequacy he experienced when he was around attractive women. I suggested that he might try disclosing his shyness instead of always trying to hide his feelings and act cool. Although he found the idea frightening, he agreed to give it a try. On his way to work a few days later, Paul found himself sitting next to an attractive single woman on the train. He felt anxious, but forced himself to talk to her. She seemed receptive, and soon they were engrossed in conversation. Paul remembered his assignment, and confessed that he'd always felt shy around attractive women. He apologized and explained that he was feeling a bit shy right then. She seemed surprised, and said that men were always trying to put the moves on her and impress her by acting macho. She said that it turned her off, and explained that she'd been hoping to meet a really sensitive guy like Paul. Paul couldn't believe his ears. They ended up exchanging phone numbers, and had their first date several days later. This technique is challenging for most shy patients because they're so ashamed of their anxiety. They think of themselves as defective, and feel certain that others will view them in the same way. That's why they try so hard to act "normal" in social situations. Of course, this puts them under tremendous pressure and they appear stiff and awkward, the very consequences they're
Chapter 24
872
desperately trying to avoid. Self-Disclosure can be extremely helpful, but it requires a decent sense of self-esteem. Make sure you practice with the patient, so you can make sure they're using Self-Disclosure in a tasteful, low-key way that will maximize the likelihood of success. 45. Flirting Training Many shy and lonely patients have never learned how to flirt, and seem overly serious when they're trying to get to know someone they're interested in. In contrast, other people seem to have the gift of gab. They can connect with almost anyone in a lighthearted, affectionate way that sets others at ease. Researchers don't know for sure whether some people are born with this talent, or whether they learn it when they're growing up. By the same token, it's unclear whether some people are born with the tendency to be shy, or whether shyness develops as a reaction to traumatic experiences when we're growing up. There are animal models that support both possibilities. You may have heard about the fact that some Pointer dogs seem to have a "shyness" gene that makes them terrified of humans from the very moment they're born. When puppies with the shyness gene see a human being for the first time, they run and hide, shaking and trembling in terror. Puppies without this gene are naturally friendly and outgoing. The first time they see a human being, they eagerly run up to the person, wagging their tails excitedly and hoping to be petted. If it works the same way in humans, you could argue that shyness is probably inherited. On the other hand, you're probably familiar with the problem
Chapter 24
873
of feral cats that were raised in the wild, without human contact. Unless they're adopted as kittens, they develop a deep distrust of people. Even if they're later adopted into loving homes, they may never outgrow their fear of humans or become completely affectionate and trusting. I know from experience, because we have a feral cat, as well as two we adopted when they were six weeks old, and the differences are profound. So you could make an equally strong case that shyness is learned. Regardless of what causes shyness, I'm convinced that good interpersonal skills can be learned, and that we can do a great deal to help our patients who are having problems getting their social lives in gear. What is effective flirting? It's hard to give a precise definition, but here are a few approximations: You make people feel special and admired. You praise them for what they've done, and how wonderful they are, but you do it in a lighthearted way. You get them to talk about themselves without focusing attention on yourself. As a result, they will often conclude that you're special. You tease the other person in an affectionate way, in much the same way that an older sibling might tease a younger sibling that she or he is proud of. You create an atmosphere of fantasy and fun that makes the other person curious and intrigued. You use positive body language, including low-intensity, non-intrusive touching, such as placing your hand on someone's arm in an affectionate way while talking in an animated way.
Chapter 24
874
Of course, these techniques have to be used skillfully and thoughtfully. In some situations, it would clearly be inappropriate to touch the other person, and touching could seem intrusive in any situation if it's done in a clumsy or aggressive manner. When patients begin their Flirting Training, they can select people who aren't particularly threatening. In fact, they can even begin with animals. I do this all the time, and it works like a charm. For example, if you see a dog on the sidewalk, you can pet it and say the most outrageous things, like, "Oh, you're such a handsome fellow. I've never seen a dog with such an intelligent and friendly face!" Dogs love the attention, and they're remarkably uncritical. Next, the patient could try flirting with people who aren't objects of romantic interest. Most people are looking for a little sunlight to brighten their day. Patients can practice making friendly, admiring comments to people who are almost guaranteed to respond positively—like the bellman at the hotel, an elderly man or woman who's waiting for a bus, or people who are out walking their dogs. I learned the value of these techniques when I was a medical student. We were all afraid of a secretary named Clarisse in the Department of Medicine who was a bit caustic. She constantly complained and seemed critical of everyone. Her boss was the department chairman, so we all tried to steer clear of her, because if you got on her bad side, she could make life miserable for you. One day I had to ask her a question about one my clinical rotations. She seemed especially irritable, and I sensed I was on the verge of an attack, so I blurted out something like this: "You know, Clarisse, I really admire the way you
Chapter 24
875
run this department. You're incredibly organized and efficient. I'm always singing your praises, and I really wish I had that kind of skill." I can tell you that she melted in my hands like butter! She seemed delighted, and always treated me like a prince after that. She probably felt frustrated with her life, and may not have heard a kind word in a long time. Once patients feel comfortable with this technique, they can start to flirt with people they'd like to date. You can emphasize that the goal of this technique is not to get a date, but simply to learn to engage people in friendly, lighthearted exchanges. This mindset will take some of the pressure off, and the patient may actually end up getting a date. 46. Rejection Practice Shy individuals dread rejection and yearn for approval. But more often than not, the desperate need for approval turns people off. When they use Rejection Practice, patients can seek out rejection and view it as a success rather than a failure. We all have to endure a certain amount of rejection, and if patients are willing to do that, sooner or later, they'll usually find many people that they are compatible with. In his workshops, Dr. Albert Ellis often describes a unique experience he had when he was young. To get over his fears of rejection, he forced himself to approach 200 women on the streets of Manhattan during a two-week period and ask them for a date. All but one turned him down, and she failed to show up! Although he didn't get any dates this way, he did overcome his fears of rejection and ultimately developed a robust social life. He even ended up writing
Chapter 24
876
a sex and love advice column for a prominent men's magazine. Although I'd never heard of Dr. Ellis when I was a medical student, my friend, Spyder, and I stumbled across the same technique. Spyder lived in the garage behind the house I was renting with friends. He was a drummer looking for a band to hook up with, and he was very good-looking. However, he was painfully shy, a problem I shared as well. In an attempt to conquer our fears, we'd walk around the streets of Palo Alto and San Francisco for hours at a time, taking turns approaching attractive young ladies and trying to get to know them. If it was Spyder's turn, I'd spot a good-looking young lady, and he'd have to approach her and try to get a date. If it was my turn, he'd select someone and I'd have to do the same thing. Our experience was similar to that of Dr. Ellis. We got shot down every single time! I think it was because we were both overly serious and sincere, and still a bit on the nerdy side. But we did overcome our fears of rejection, and eventually developed exciting social lives. I was reminded about this a few years ago when I attended an art exhibit called Bad Company at the SkyDeck Gallery on the top floor of the Embarcadero Center in San Francisco. The exhibit featured the early work of the famed Bay Area photographer, Larry Keenan, and included photos of beat & counterculture icons like Bob Dylan, Lawrence Ferlinghetti and Neal Cassady, along with many colorful hippies from the late 1960s. Although I'd completely lost track of Spyder for the previous 30 years, I suddenly found myself standing in front of a huge photograph of him kissing a beautiful, half-naked young lady in a field of flowers.
Chapter 24
877
My mind was flooded with memories of the day the photo was taken. It was a "happening" we created one Saturday afternoon in Los Altos Hills. It was clear that our Rejection Practice had finally paid off! Other Interpersonal Exposure Techniques Although Shame-Attacking Exercises are listed as Humor-Based Techniques, you can also view them as a form of Interpersonal Exposure. You can review Shame-Attacking Exercises on page 651. The Feared Fantasy (page 670) can also be used as an Interpersonal Exposure Technique. Shy patients can confront the social disapproval they fear so intensely in a role-playing exercise where they'll meet a horribly critical stranger who tries to rip them to shreds. If they respond with the Acceptance Paradox, they can usually handle anything the critical stranger throws at them. In my workshops, I sometimes demonstrate the Rejection Feared Fantasy with a volunteer from the audience. In the following dialogue, I'll play the role of a shy man who just got badly shot down by a woman I was trying to flirt with. The volunteer from the audience will play the role of a hostile stranger who saw what happened, and is going to try to humiliate me in the worst imaginable way: Hostile Stranger (played by audience volunteer): Hey, I saw you trying to talk to that woman just now. Were you trying to flirt with her or pick her up or something? Shy Man (played by David): Yes I was. I thought she was interesting. Hostile Stranger (played by audience volunteer): You really got shot down, didn't you!
Chapter 24
878
Shy Man (played by David): Yup. She really blew me off! Hostile Stranger (played by audience volunteer): You can say that again! You looked like a fool. I've never seen anyone as lame as you. Shy Man (played by David): Well, to be honest, I felt like a bit of a fool. But I was really glad I tried. I'm just getting the hang of this flirting thing, and I definitely need a lot of practice. Hostile Stranger (played by volunteer from audience): Just getting the hang of it? Your technique stinks! Shy Man (played by David): I'll have to agree with you. I know there's lots of room for improvement. It sounds like you might be really good at it. Perhaps you can give me some tips. Hostile Stranger (played by volunteer from audience): Forget it, man! You're so bad that I'd have no idea where to begin. Shy Man (played by David): Well, I don't mean to put you out, but I'm really eager to learn. Perhaps you could tell me just one or two things I was doing wrong, or what you might have said to her instead. Either the Hostile Stranger will back down and begin to communicate more sensibly, or he'll end up looking cruel and foolish. Either way, the patient wins. The goal of the Rejection Feared Fantasy is to show patients that even if their worst fears came true, they'd survive. If they find this technique helpful, they'll have to back it up by flirting and connecting with real people in social situations. Sooner or later, the rubber has to meet the road. Otherwise, it will just
Chapter 24
879
be a therapeutic exercise. The Interpersonal Exposure Techniques are powerful, but they can be frightening at first. If you want to use them, you'll need a trusting therapeutic alliance and a strong therapeutic agenda with your patient. You'll also have to use these techniques selectively and thoughtfully, so you don't set your patients up for negative experiences they're not prepared to handle.
25*
Interpersonal Techniques
We can't just specialize in the treatment of one type of problem, such as depression or anxiety, because the people who come to us for treatment are usually suffering in many different ways. For example, a man who asks for help with depression may also be troubled by feelings marital discord, conflicts with friends or colleagues, and feelings of loneliness. In fact, interpersonal therapists believe that problems in intimate relationships are an important cause of depression (Burns, Sayers, & Moras, 1994). Investigators have consistently reported significant correlations between measures of depression and marital discord. My colleagues and I used structural equation modeling techniques to investigate the causal links between these variables. Our studies indicated that marital discord is not a strong cause of depression, and that depression is not a strong cause of relationship problems (Burns, Sayers, & Moras, 1994). Still, there's no doubt that depression and anxiety often occur in the context of interpersonal difficulties, and you'll often * Copyright
2004 by David D. Burns, M.D.
Chapter 25
881
have to address both types of problems during the treatment. Some experts have promoted the use of CBT in the treatment of relationship problems, but I've found that these methods usually aren't effective and that a different approach is needed. Why does CBT work so well for depression, and so poorly for anger or marital discord? If you're treating a patient who feels depressed and worthless, all the distorted thoughts will be directed against the self. The patient will be telling himself that he's a worthless loser, that he should be better than he is, and that things will never change. These distorted thoughts create enormous suffering. When he discovers that these negative thoughts aren't valid, he'll feel a wave of relief. In fact, this discovery can be exhilarating. In contrast, when people are angry, the cognitive distortions, such as Allor-Nothing Thinking, Should Statements, and Blame, are directed at someone else. Angry individuals who are enmeshed in conflict rarely feel motivated to give up these distortions because they're so empowering. For example, let's say that you're treating a woman named Mary who's angry with her husband, Sam. She records these negative thoughts on her DML: He's a jerk. 100% All he cares about is himself. 100% He'll never change. 100% He never listens. 100% Our problems are all his fault. 100% Use checks ( ) to indicate all the distortions you can find in these
Chapter 25
882
thoughts before you turn the page. Feel free to review the Checklist of Cognitive Distortions on page 535. Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 25
883
Answer I found all ten distortions, and I bet you did, too! Mary thinks their problems are all her husband's fault (Blame) and views him as "a jerk" (Labeling) with no redeeming qualities (All-or-Nothing Thinking; Mental Filter; Discounting the Positive). She tells herself that he should be a better listener (hidden Should Statement) and that all he cares about is himself (Mind-Reading; Overgeneralization). She exaggerates all his flaws (Magnification) and believes that he'll never change (Fortune-Telling). She also reasons from how she feels (Emotional Reasoning). She feels like he's a loser, so she assumes he really is one. She feels like he's to blame, so she concludes that he really is. So far, Mary has all the same distortions you'd see if you were treating a woman who felt worthless and depressed. But what will happen if you jump in and use your CBT techniques to show her that all her thoughts about her husband are distorted, and that she's wrong, wrong, wrong about him? It doesn't take a genius to answer that question! Her anger will intensify. Now she'll have two enemies—her husband and her therapist! She may even drop out of therapy. That's what I mean when I say that treating relationship problems with CBT makes about as much sense as trying to put out a fire by throwing gasoline on it. In this chapter, I'm going to illustrate interpersonal treatment techniques that are radically different from the CBT techniques you'd use to treat depression and anxiety. For the most part, I'll make the assumption that you're treating the patient individually. This may represent a departure from conventional wisdom,
Chapter 25
884
which states that you can't effectively treat a troubled relationship unless both partners participate in the therapy. This rule hasn't been consistent with my clinical experience. I've treated many patients with troubled relationships individually, with excellent results. In fact, I think that the prognosis may actually be better when you're only treating one member of the dyad. That's because it will be clear who's going to have to do the changing. Furthermore, interpersonal therapy can be humiliating, because patients will have to examine their own role in the conflict. If the patient likes and trusts you, the therapeutic alliance can reduce the patient's defensiveness and soften the blow of self-examination. In addition, it isn't always practical or possible to treat both parties in a troubled relationship. If a woman is having problems getting along with her boss, she'll have to learn to solve that problem unilaterally. We can't invite her boss to participate in the treatment! There will also be times when the patient's spouse cannot or will not attend sessions, or isn't suitable for couple's therapy. In most cases, you can make significant progress with the techniques in this chapter, even though you're only treating one of the two partners. When patients first describe problems in their relationships, I empathize and try to see the world through their eyes. I don't challenge them or try to help them. Instead, I provide support and find truth in what they're saying, even if it seems exaggerated and self-serving. Once the patient feels understood, I move to the Invitation step of Agenda Setting. I ask if they want help with the problem they've been describing, or if they simply want me to listen and understand how they feel.
Chapter 25
885
If the problem involves a conflict with another person, I point out that they have three options: 1. They can settle for the status quo. 2. They can decide to leave the relationship. 3. They can work to make the relationship better. I call this process Interpersonal Decision-Making. Most patients will be able to answer this question right away. The first option is the most common choice. Most people who complain about an irritating neighbor, colleague, sibling, spouse, or ex aren't looking for help, and definitely don't want to develop a better relationship with the other person. They simply want you to agree that the person they're mad at is a jerk, and that they shouldn't be that way. In this case, interpersonal therapy is not indicated. This is sometimes hard for therapists to accept because we naturally want to help our patients. One of my residents was treating a divorced graduate student from San Jose State who often complained about what a jerk her ex was. She described an argument they had when she picked him up at the San Jose airport. She seemed to be overlooking the defensive, antagonistic way she communicated with him, and it was clear that she was triggering the adversarial interactions she was complaining about. My resident asked if she wanted to work on her communication skills so she could develop a more harmonious relationship with him. She snapped and said that she'd never had any problem communicating with men and that her interpersonal skills were just fine! What was the resident's error? Why did she snap at him? Put your ideas
Chapter 25 here before you turn the page:
886
Chapter 25
887
Answer Like so many of us, the resident was offering to help her with a problem that she hadn't asked for help with. She didn't see the conflict with her ex as a problem, and got a lot of emotional gratification from scapegoating him. If you were her therapist, you'd have to use the Five Secrets of Communication to heal the rupture in the therapeutic alliance. You can acknowledge that your statement insulted her, and agree that her ex is undoubtedly very difficult at times. You can encourage her to tell you more about how she's feeling, and ask if there were other times when you said things that annoyed her. You can also ask her to tell you more about how she feels when she interacts with her ex. Once she trusts you again, you can move to the Invitation step of Agenda Setting. Ask if there's a problem that she'd like to work on during the session. I try to think of my patient as my boss. I have some helpful tools, but the patient has to tell me what problem she or he wants help with. If a patient wants to maintain a dysfunctional, hostile relationship, I empathize and remind myself that there are some people I don't particularly respect and don't want to feel close to, either! Now let's examine option #2. If the patient wants to leave the relationship, you can ask if they need some help from you. For example, they might have fears about being alone, or concerns that friends or family would look down on them if they were separated or divorced. They may have doubts about how to support themselves, or feel anxious about developing a social life and starting to
Chapter 25
888
date again. Once they've defined a problem, you can conceptualize it, assess their motivation, and select the most appropriate treatment tools. Some patients will choose option #3. They want to make the relationship better. If they're willing to examine their own role in the conflict, and focus on changing themselves instead of blaming the other person, they're good candidates for interpersonal therapy. Some patients aren't sure what they want. They're stuck on the horns of a dilemma. Should I get divorced or start marital therapy? Should I look for a new job or try to improve my relationship with my boss? For some patients, these kinds of decisions can be agonizing. The Decision-Making Form can help them sort out their options. An attractive young woman named Jewell was trying to decide whether or not to get engaged to her boyfriend, Rasheed. They'd been dating for three years, and Rasheed was putting pressure on her to commit. She loved him, but wasn't totally convinced he was "the one" for her. She felt intensely ambivalent and couldn't decide whether to get engaged or break up. On page 889, you'll find Jewell's Decision-Making Form. I asked her to label her two choices as Option A and Option B, and to list them at the top of the page. As you can see, Option A was getting engaged to Rasheed and Option B was breaking up.
Jewel's Decision-Making Form Option
Describe
A
Get engaged to Rasheed
+20
B
Break up with Rasheed
+30
3e Advantages of Option A 1. 2. 3. 4.
I can let go of my ambivalence. I can move on to the next stage of my life. I care very deeply about Rasheed. Rasheed would be a great person to marry and have kids with. 5. He has a nice home in Arizona. 6. I know Rasheed, so most of the surprises are out of the closet after 3 years. 7. I don't have to start over with someone else. 8. This is an easier decision that requires little or no deviation from my current path. 9. I can start a family and stop the "tick tick" fear. 1 9 10. Spend more time with friends who have kids. 95 60 11. Have kids while my friends' kids are still the same age. 12. Give my Mom grandkids. 5 35
1. 2. 3.
4. 5. 6. 7. 8.
Total Points
6 65 I get to fall in love again. I can explore other men I've been interested in, one in particular. 130 65 Life becomes full of 11 3 unknowns again. This seems exciting. I can take a shot at finding someone I feel more compatible with. I can live wherever I want. More excitement. I won't be settling for what doesn't feel right. I can try to find Mr. Right.
Advantages of Option B
Disadvantages of Option A 1.
I'll know exactly where my life is going, and it's not too exciting. I have to fit into Rasheed's life in Arizona. I was once okay with this, but now I'm not so sure. I'm not sure he's "the one." I might miss out on dating the perfect guy. I'm not convinced we can make it work long-term. I feel 70% sure we'd end up divorced…yikes! I'm not excited about getting engaged. I can't seem to squelch my desire to date someone else.
2. 3. 4. 5. 6. 7. 2
40
10 75
35 7
65 8
1. I may regret my decision. 2. I might get depressed. 3. I may hurt Rasheed deeply. 100 4. I'll lose my best friend. 35 12 5. I'll lose the house in Arizona. 4 6. It will be hard to break up. 7. I've spent a good deal of time getting to know Rasheed. To a certain extent, this was a waste. 8. I'll have to get to know someone all over again. 9. This means delaying a family for at least two or three years, and my biological clock is ticking. 10. I'm not sure I'm making the right decision. Will I regret it big time in three months? 11. Dealing with the feeling, "Did I make a mistake here?" 12. Ambiguity. Life becomes full of unknowns again, which can be scary.
Disadvantages of Option B
Chapter 25
890
I asked Jewell to list all the advantages and disadvantages of Option A, getting engaged, on the top half of the page. As you can see, there were many advantages. For example, she could resolve her feelings of ambivalence and move on to the next stage of her life. She also cared very deeply about Rasheed, and felt like he'd be a good person to have a family with. She was very aware that her biological clock was ticking, and felt some pressure to get her family started when she was still relatively young. However, there were a number of disadvantages as well. She felt like this option was unexciting, since Rasheed was very predictable and somewhat dogmatic. She had mixed feelings about living in Arizona, but he had roots there and didn't want to move. Furthermore, she wasn't convinced he was "the one," and didn't feel very excited about getting engaged. Next, I asked her to list all the advantages and disadvantages of Option B, breaking up, on the bottom half of the page. There were many advantages. She could explore a relationship with a man she'd recently met and fall in love again. Life would feel exciting, and she wouldn't have to settle for less than what she wanted simply because she thought it was time to start a family. At the same time, there were many disadvantages to Option B. She was afraid she might hurt Rasheed and regret her decision later on. In addition, she'd have to delay starting a family while she got to know someone new. Once Jewell listed the advantages and disadvantages of both options, I asked her to fold the paper in half across the middle so she could weigh the advantages of Option A against the disadvantages of Option A, while ignoring
Chapter 25
891
Option B. Did the advantages outweigh the disadvantages, or vice versa? On a 100 point scale, was it 50-50? 70-30? 10-90? Jewell was apprehensive that she might not get it "right," so I reminded her that this was just a trial run, for practice, and that her ratings weren't set in stone. She could always add more advantages or disadvantages, and change her ratings later on if she wanted to. Jewell said that Option A felt moderately positive, so she put a 60 in circle 1 and a 40 in circle 2, indicating that the advantages seemed a bit greater than the disadvantages. Still, she felt ambivalent and confused, and was tempted to break up with Rasheed, or at least take some time off from the relationship. Why? Let's examine Option B. I asked Jewell to turn the paper over so she could rate the advantages and disadvantages of breaking up with Rasheed, while ignoring Option A. You can see that her ratings in circles 3 and 4 are 65-35, indicating that this option also seemed very positive. Now Jewell's dilemma falls into a different perspective. She seems to have two positive options. Perhaps that explains her confusion. But what will happen if Jewell compares the advantages of Options A with the advantages of Option B? This is where things get interesting. I asked her to fold the paper down the middle, from top to bottom, so she could compare the advantages of the two options. I told her to imagine that there were no disadvantages, and to ask herself which list of advantages felt more desirable to her.
Chapter 25
892
You can see that the ratings in circles 5 and 6 are 35-65. This means that the advantages of Option B clearly outweighed the advantages of Option A. In other words, breaking up and dating other men seemed much more appealing to Jewell than getting engaged. Now let's see what happens when Jewell compares the disadvantages of each option. I asked her to turn the page over so she could compare the disadvantages of each option, while ignoring the advantages. Which list of disadvantages felt more negative? You can see that Jewell put a 35 in circle 7 and 65 in circle 8. These numbers indicate that the disadvantages of breaking up with Rasheed felt substantially greater than the disadvantages of getting engaged. Jewell was reluctant to break up because she was afraid she'd lose her best friend and get depressed. In fact, she'd experienced an episode of severe depression after breaking up with her previous boyfriend. In addition, the excitement of a new relationship was counterbalanced by the fear of the unknown. Once the patient has compared all the quadrants, you can calculate the overall ratings for each option. Take a look at the upper left-hand quadrant. The two numbers in circles 1 and 5 (60 and 35) add up to 95, the total points for the Advantages of Option A. This number appears in circle 9. Now look at the upper right-hand quadrant. The two numbers in circles 2 and 7 (40 and 35) add up to 75, the total points for the Disadvantages of Option A. This number appears in circle 10. We can subtract 75 from 95 to get the total points for Option A. This
Chapter 25
893
number, +20, appears at the top of the page as the total score for Option A. Similarly, you can calculate the total score for Option B, which is +30. If you compare the total points for Option A and Option B at the top of the page, you'll see that both numbers are positive. You might think about this as a Can't-Lose situation, because both options are positive. However, the overall ratings disguise an important fact that's only apparent when you examine the individual quadrant ratings. Option A is a low-energy option, and Option B is a high-energy option. In other words, the advantages of breaking up greatly outweigh the advantages of getting engaged, but the disadvantages of breaking up are also far greater than the disadvantages of getting engaged. So even though the total points for both options are similar, the implications and dynamics of each choice are radically different. If it weren't for the fact that the disadvantages of Option B were so great, Jewell's decision might be obvious. In addition, we can see that many of the disadvantages of Option B are influenced by her concerns about anxiety and depression. There may be some distortions in the way she's is thinking about this option, and we could use a wide variety of CBT techniques to help her deal with her negative thoughts and feelings about breaking up with Rasheed. For example, we could use the Double Standard Technique, and ask Jewell what she'd say to a dear friend who wanted to break up with a man she'd been dating. She might say, "Well, it probably will hurt his feelings, but he'll survive. Breaking up is a part of life. You can't protect him from that forever, and the sooner you make the break, the sooner he can get on with his life and find
Chapter 25
894
someone new." We might also use the Hidden Emotion Technique. Does Jewell avoid conflicts in intimate relationships, and then run off with someone else who seems more attractive so she won't have to get too close or deal with angry feelings? Jewell confessed that every time she felt upset with Rasheed, she swept her feelings under the rug and had the thought, "I just know I'm going to break up with this guy. This will never last." Jewell decided that she did want to break up with Rasheed, at least for a couple of months. She felt relieved, as if she finally had some room to breathe. In Jewell's case, interpersonal therapy clearly wasn't indicated. She would have resisted any attempt to improve her relationship with Rasheed because she felt trapped and wanted out. Interpersonal Decision-Making will help you screen out patients who aren't really looking for help. If, on the other hand, they do want to develop better relationships with the people they're at odds with, we'll need to assess their motivation on a deeper level. 46. Relationship Cost-Benefit Analysis (CBA) I believe that blame is the greatest barrier to intimacy. People embroiled in relationship conflicts are nearly always convinced that they're innocent and the other person is completely to blame for the problems in their relationship. As long as they maintain this mindset, effective therapy is difficult, if not impossible. Think about someone you don't like or get along with. It could be a difficult patient or an irritating family member, friend, or colleague. What do they do that
Chapter 25
895
irritates you? Perhaps they: Pout and slam doors, and insist they're not angry Refuse to open up or tell you how they feeling Whine endlessly, but ignore all your helpful suggestions Complain that you just don't understand Constantly argue and always have to be right Won't listen to how you feel Criticize you relentlessly Blame you for all their problems and refuse to look at themselves Make constant demands, but insist that nothing you do is ever good enough. Does any of this sound familiar? Now, I'd like you to think about one moment in your relationship with that person that you didn't handle very well. Think of a conflict that didn't turn out right. Try to picture the other person in your mind's eye. Write down one thing that she or he said during the argument. This exercise will work best if you limit yourself to a few sentences:
Now write down exactly what you said next. Once again, try to be brief. A few sentences will give us plenty to work with:
Chapter 25
896
If you haven't yet written anything down, please stop reading and do so now. If you're having trouble remembering exactly what the other person said, just make something up. Write down the type of thing the other person usually says, and what you generally say next. A therapist named Alyson attended a psychotherapy workshop I conducted on interpersonal conflict. She described a conflict with her exhusband, Don, like this: "Don and I are basically good friends, but he can be loud and controlling. He always gives me advice that I haven't asked for and tells me what to do. I find it irritating. We had exactly the same problem when we were married. I enjoy spending time with him, but I don't like it when he gives me advice. We met for coffee the other day and I told him I was way behind on things and felt overwhelmed, and then he started in on me." I asked Alyson to give me an example of what Don said to her. He told her: "You just need to take care of things. Go home. Get things done! Make those calls!" Then I asked Alyson to tell me exactly what she said next. She told Don: "I'm doing the best I can. I can't do any more. I feel like I'm already under too much pressure." That single exchange is all we'll need to analyze the cause of the problem and turn it around. Now think about the person you're not getting along with. What happens when you fight? Do they pout? Shout? Argue? Refuse to talk? Now I have a question for you. Who, in your opinion, is more to blame for this problem? Is it you? Or the other person? Who do you think is the bigger jerk?
Chapter 25
897
Please answer this question from your heart of hearts. I'm far more interested in how you actually feel than in hearing the politically "correct" answer. Put your answer here:
1.
In all honesty, I feel that the other person is primarily to blame for the problem.
2.
I feel that the conflict is primarily my fault.
When I do this exercise in workshops for the general public or for mental health professionals, I say, "How many of you are convinced that the conflict is the other person's fault?" Without fail, ninety percent of the people in the audience raise their hands, and there's quite a bit of giggling. Then I ask, "How many of you believe that the problem is primarily your fault?" Only a few hands go up. Then I say, "It's interesting to me how it's always the innocent ones who come to my workshops. For some reason, the guilty parties never seem to show up!" Of course, our patients will feel exactly the same way. They may say they want a better relationship with their spouse, sibling, or boss, but what they really mean is, "The other person will have to do the changing, because the problems are really his fault." As long as they maintain this mindset, effective therapy will be difficult, if not impossible, so we'll need to address this issue first. The Relationship Cost-Benefit Analysis allows you to assess the patient's motivation and make him or her accountable. Let's do it together now. Ask yourself this question: "How will blaming the person I'm not getting along with
Chapter 25
898
help me? What are some of the rewards and benefits of this mindset?" List all the advantages of blame in the left-hand column of the Relationship Cost-Benefit Analysis (CBA) on page 899. You can probably think of quite a few, including: You can feel morally superior. You won't have to change. You won't have to examine your role in the problem. You'll feel convinced that truth is on your side. You can do nasty things and get back at the other person without having to feel guilty. You can get friends and colleagues to side with you and agree that the other person really is a self-centered loser. You can feel righteous and powerful. You won't have to swallow your pride. As you can see, there are many powerful and real benefits of blaming the other person. It's an addictive mindset. We all get caught up in it. Now think about the disadvantages of blame, and list them in the righthand column of the Relationship CBA on page 899. Ask yourself if there's a downside. Do you pay a price for this mindset?
Chapter 25
899
Relationship Cost-Benefit Analysis* Instructions. List all the advantages and disadvantages of blaming the other person for the problems in your relationship. Then balance the list of advantages against the list of disadvantages on a 100-point scale. Put two numbers that reflect your ratings in the circles at the bottom. Advantages of Blame
* Copyright
Disadvantages of Blame
2004 by David D. Burns, M.D.
Chapter 25
900
Here are a few potential disadvantages: You won't be able to resolve the problem or get close to the other person. The other person will insist that you're wrong and that it's all your fault. The conflict will go on and on. You'll feel frustrated, angry and resentful. These feelings may drain your creative energy and reduce your capacity for joy and optimism. Friends may think of you as a whiner and a complainer. There will be no room for personal or spiritual growth. Once you've written down all the advantages and disadvantages you can think of, you can balance the lists against each other on a 100-point scale. Ask yourself whether the advantages or disadvantages feel greater. You don't need to get too obsessive about the ratings. Sometimes, one strong advantage will outweigh numerous disadvantages, or vice versa. Put two numbers that reflect your ratings in the circles at the bottom. Make sure the numbers add up to 100. For example, if the advantages feel considerably greater than the disadvantages, you could put a 75 in the circle on the left, and a 25 in circle on the right. If it's a draw, you can put 50 – 50 in the two circles. If the disadvantages of blame feel somewhat greater, you might put 40 – 60 in the circles. If the advantages of blame outweigh the disadvantages, I tell the patient that I probably don't have any tools that are powerful enough to help them. I explain that as long as they blame the other person, the prognosis for developing
Chapter 25
901
a close, trusting relationship is close to zero. I reassure them that I want to work with them, and ask if there's some other problem they might want to focus on instead. This is a paradoxical intervention. We're telling the patient, "As long as you set the problem up like that, I can't help you." I've found that this approach is difficult for some therapists to grasp or incorporate into their therapeutic work. Many of us get anxious and succumb to the knee-jerk reaction of trying to "help" our patients. For example, you may emphasize that it takes two to tango and attempt to show the patient that they do play a role in the conflict. Or, you may try to sell the patient on the value of developing a better relationship with the person they're annoyed with, even if they're convinced that the other person really is to blame. The problem with these persuasive efforts is that it suddenly becomes your responsibility to show the patient how to make the relationship better. This empowers the patient to sit back and resist while you do all the work. Persuasive strategies are rarely effective. In fact, trying to persuade reluctant, resistant patients to change is the cause of nearly all therapeutic failure. Alternatively, some therapists go to the opposite extreme and collude with the patient. You may view the patient as the innocent victim and agree that their spouse or boss really is an insensitive jerk. In this case, you may be reinforcing the patient's distorted perceptions and self-defeating behavior patterns. You might think that no competent therapist would fall into this trap, but I've found that it's extremely common. Scapegoating is a widespread phenomenon. When the patient tells you that the other person is an exploitative,
Chapter 25
902
tyrannical jerk, you may be tempted to take the bait. The pressure to buy into this mode of thinking can be intense. The approach I'm describing is different. You simply back off and let the patient know that change will not be possible as long as she or he blames the other person. This is a powerful but potentially upsetting message that must be delivered with compassion and respect for your patient. You could say something along these lines: "Larry, you've told me that Mimi is to entirely blame for the problems in your relationship. You say she's too emotional and that she should be more willing to listen to you, especially since your point of view is valid. I'm concerned that I might not have the tools to help you, given the way you're thinking about this. As long as you're convinced that everything is Mimi's fault, I'm afraid we're not going to be able to get the job done. But I do want to work with you, and I'm wondering if there are any other problems you need help with?" If Larry insists that the problems are all his wife's fault, you may need to offer him a referral to a different therapist. By the same token, he may simply need more time to vent his angry feelings while you listen and provide support. You may have jumped into problem-solving mode prematurely. After you've empathized, you can attempt to set the agenda again. You'll usually have to empathize and renegotiate the therapeutic agenda frequently when you're doing interpersonal therapy. Even highly motivated patients may begin to resist and yes-but you from time to time. They'll suddenly
Chapter 25
903
insist that they shouldn't have to change. Whenever this happens, put your technical tools on the shelf, empathize, and renegotiate the agenda. You can also respond paradoxically, as in this example: Larry: Why should I have to change? After all, Mimi's been acting like a jerk for the past ten years! She never listens to me. Therapist: You're right, Larry. You don't have to change, and I have no doubt that Mimi can be difficult at times. Are you saying that you'd prefer not to change? Larry: Well, it seems unfair that I should have to do all the work. Therapist: You're right about that, too. It does seem unfair. Should we work on some other problem instead? Notice that this therapist is not engaging in a power struggle, but is surrendering to Larry's resistance. At the same time, the therapist is conveying a number of powerful messages: You're the boss and I'm working for you. I won't try to change you against your will. I don't have a hidden agenda to show you how to develop a more satisfying relationship with Mimi, or with anyone for that matter. I do want to work with you, but if you want help with your marriage, you're going to have to examine your own role in the problem. If this is not acceptable to you, I probably can't help you with this problem. There's a chance that Larry will change his mind and decide that he really does want to work on the conflict with Mimi, especially when he realizes that
Chapter 25
904
you're not pushing. But if he's determined to remain in the role of victim, then at least you'll avoid the frustration of fighting with his resistance. 47. Revise Your Communication Style Let's say that you and your patient have completed the Relationship CBA. If the patient decides that the costs of blame outweigh the benefits, you can show them how to develop greater intimacy. In Chapter 12, we used the Revise Your Communication Style form to analyze therapeutic logjams with critical, mistrustful patients. Now we'll use the same approach to help our patients solve personal relationship problems. Let's think about Alyson and Don again. Don said: "You just need to take care of things. Go home. Get things done! Make those calls!" Then Alyson replied: "I'm doing the best I can. I can't do any more. I feel like I'm already under too much pressure." I've recorded this exchange as Steps 1 and 2 of the Revise Your Communication Style form on page 906. Of course, this is really the Specificity step of Agenda Setting. It's based on the idea that the entire conflict is embedded in any brief interaction between you and the other person. Once you understand why you and the other person were locking horns at that particular moment, you'll discover the cause of all the problems in your relationship. In fact, you'll probably understand the cause of all the problems in your relationships with everybody. Furthermore, when you learn how to resolve the conflict you were experiencing at that one moment, you'll see how to resolve any conflict in your relationship with that person, or with any person. So even though our focus is extremely narrow, our goals are ambitious.
Chapter 25
905
Let's do Step 3 together. Was Alyson's response in Step 2 an example of good or bad communication? Of course, we can't answer this question until we've defined what we mean by "good communication" and "bad communication." You may recall the definition I proposed that's based on the EAR acronym. Good communication involves: E = Empathy. You acknowledge the other person's feelings and find some truth in his or her point of view. A = Assertiveness. You express your feelings openly and directly, using "I Feel" Statements. R = Respect. You convey an attitude of respect and caring, even in the heat of battle. Bad communication has the three opposite characteristics: E = Empathy. You fail to acknowledge the other person's feelings, and imply that she or he is "wrong." A = Assertiveness. You don't share your own feelings openly and directly. Instead, you argue defensively or act out aggressively. R = Respect. You fail to convey respect. Instead, you project an air of condescension, superiority or competition. To make Step 3 simple for patients, I photocopy the "Good vs. Bad Communication Checklist" as well as the "Bad Communication Checklist" on page 907 on the back of the Revise Your Communication Style form. That way, patients can simply turn the form over and check the appropriate boxes when they do this step.
Chapter 25
906
Revise Your Communication Style* Step 1 – Don said: You just need to take care of things. Go home. Get things done! Make those calls! Step 2 – I said: I'm doing the best I can. I can't do any more. I feel like I'm already under too much pressure. Step 3 – Good vs. Bad Communication. Was your response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist or the Bad Communication Checklist on page 907 to analyze what you wrote down in Step 2.
Step 4 – Consequences. Did your response in Step 2 make the problem better or worse? Why?
Step 5 – Revised Response. Revise what you wrote down in Step 2. Use the "Five Secrets of Effective Communication." If the revised response is still ineffective, try again.
* Copyright
1991 by David D. Burns, MD. Revised, 1992.
Chapter 25
907
Good vs. Bad Communication Checklist* Instructions. Review what you wrote down in Step 2. Was your statement an example of Good Communication or Bad Communication?
Good Communication
Bad Communication
Empathy
1.
You acknowledge the other person's feelings.
1.
You ignore the other person's feelings.
Assertiveness
2.
You express your feelings openly and directly.
2.
You fail to express your feelings openly.
Respect
3.
Your attitude is respectful and caring.
3.
Your attitude is not respectful or caring.
Bad Communication Checklist Instructions. Review what you wrote down in Step 2. How many of the following communication errors you can find in it?
Communication Error
( )
Communication Error
1.
Truth – You insist that you're "right" and the other person is "wrong."
10. Diversion – You change the subject or list past grievances.
2.
Blame – You imply the problem is the other person's fault.
11. Self-Blame – You act as if you're awful and terrible.
3`. Defensiveness – You argue and refuse to admit any imperfection.
12. Hopelessness – You claim you've tried everything and nothing works.
4.
Martyrdom – You imply that you're an innocent victim.
13. Demandingness – You complain when people aren't as you expect.
5.
Put-Down – You imply that the other person is a loser.
14. Denial – You imply that you don't feel angry, sad or upset when you do.
6.
Labeling – You call the other person "a jerk," "a loser," or worse.
15. Helping – Instead of listening, you give advice or "help."
7.
Sarcasm – Your tone of voice is belittling or patronizing.
16. Problem-Solving – You ignore the feelings and try to solve the problem.
8.
Counterattack – You respond to criticism with criticism.
17. Mind-Reading – You expect others to know how you feel without telling them.
9.
Scapegoating – You imply the other person is defective or has a problem.
18. Passive-Aggression – You say nothing, pout or slam doors.
( )
Chapter 25
908
In light of these criteria, would you say that Alyson's response to Don was an example of good or bad communication? How many communication errors did she make? Here's how Alyson analyzed her response: "This was bad communication. I failed on all three counts. Don was probably feeling frustrated because I was complaining, but I didn't acknowledge his feelings. In addition, I didn't express my own feelings. I was anxious and frustrated because I felt like he was trying to control me and I just wanted him to listen. Instead of telling him how uncomfortable I felt, I got defensive. He was trying to be helpful but I insisted that I couldn't possibly follow his advice. I didn't convey any respect or warmth, and he probably felt annoyed." Alyson was surprised to see that she'd failed on all three counts. This is not unusual, even for a mental health professional. Of course, nearly all patients will also discover that they're not listening, sharing their feelings openly, or conveying respect. Instead, they're arguing, blaming and counterattacking. This realization can be unnerving, since the patient suddenly has to face the fact that they're fueling the fire by making every conceivable type of communication error. Some patients will be intrigued by this analysis, while others will get defensive and insist that you just don't understand. They'll remind you that the other person really is a jerk. How will you respond? Put your ideas here:
* Copyright
1991 by David D. Burns, MD. Revised 2001.
Chapter 25
909
Answer I hope the answer is obvious by now! When patients resist, empathy is the only thing that works. You'll also have to renegotiate the therapeutic agenda. You'll discover that many patients don't really want to get close to the person they're at odds with and are still heavily committed to the idea that it's the other person's fault. In this case, I suggest that we might do better to focus on some other problem that they want help with. If patients negotiate Step 3 successfully, and accurately pinpoint their own communication errors, you can go on to Step 4. Ask them to examine the consequences of the statement they wrote down in Step 2. Will it make the situation better or worse? How will the other person feel? What will she or he conclude? What will the other person say or do next? Here's what Alyson wrote for Step 4: "When I sound overwhelmed and helpless, it inspires Don to give me advice. Then I make lame excuses and argue with him. This frustrates him, because I'm not listening. He gets louder and keeps pushing his ideas and giving me more advice. In other words, I'm encouraging him to be controlling. It's like putting a line of fresh cocaine under an addict's nose, and then acting surprised when he snorts it!" This step is intellectually exciting. Hopefully, patients will see that they've been triggering the exact behavior that they've been complaining about, and that they're not helpless victims after all. Instead, they're the puppeteers who've been pulling the strings all along.
Chapter 25
910
This step is based on the Buddhist notion of oneness, or circular causality. In other words, we get back exactly what we put out. We create our own interpersonal reality at every minute of every day. This insight is potentially enlightening, but may feel extremely painful because it shatters our conviction that someone else is to blame. I recently presented a half-day personal relationship workshop for the general public in Anaheim. I asked the people in the audience who the difficult person in their life was. I also asked them to write down one thing that person said to them, and exactly what they said next. A woman named Sybil said the difficult person in her life was her husband, Charles. She said that Charles was relentlessly critical, and that she'd had to put up with his criticisms for more than 25 years. She wanted to know why men were like that. I told Sybil that scientists still didn't know a great deal about the causes of marital conflict, but that if we examined one of her interactions with Charles, we might get a feel for what was going on. She said that she had a perfect example for me. Just that morning, Charles had said, "You never listen!" I wrote this down on the flip chart so everyone in the audience could follow along with us. Then I asked her to tell me exactly what she said next. She replied, "Oh, I just ignored him and said nothing!" The people in the audience began to laugh because they could instantly see what Sybil couldn't—that she was causing the problem she was complaining
Chapter 25
911
about. Sybil obviously didn't acknowledge how Charles was feeling, and she certainly didn't find any truth in what he said. In addition, she didn't express her own feelings and she didn't convey respect or caring. Instead, she said nothing and froze him out. She acted out her angry feelings in a passive-aggressive manner. What are the consequences of Sybil's response? How will Charles feel when she ignores him? He'll probably feel frustrated, hurt, ignored, and resentful. He might feel lonely and shut out as well. What will he conclude? He'll conclude that his criticism was absolutely valid. Once again, Sybil didn't listen. What will happen next? He'll either give up and withdraw from Sybil, or keep criticizing her because she still hasn't listened or gotten the point. This type of analysis probably wasn't what Sybil had in mind when she came to the workshop. She was troubled by the lack of intimacy in her marriage and wanted to know why her husband was so relentlessly critical. Now she's gotten the answer to her question. Charles is distant and critical because she forces him to be like that. And she's probably been doing the same thing to him for the past 25 years. It won't make any difference what interaction we analyze. The pattern will almost definitely be the same every time. This insight can be humiliating. Sybil may not want to examine her role in the conflict. It can be extremely shocking to realize that we've been causing the problems that we've been complaining about for so many years. But at the same
Chapter 25
912
time, this insight can be liberating, because it means we have far more power than we think to change troubled relationships. Before we go on to Step 5, let's revisit the conflict you described earlier. On page 895, you wrote down one thing that the other person said to you, and what you said next. Copy that exchange as Steps 1 and 2 on the blank Revise Your Communication Style form on page 915. If you didn't do the writing earlier, I'd encourage you to do it now. Think about any person you're not getting along with, and complete Steps 1 and 2. If you're still drawing a blank, just make something up. All you really have to do is write down anything that someone might say to you during an argument or conflict, and what you'd typically say next.
Stop! Don't continue reading until you've completed Steps 1 and 2.
Do this exercise now.
If you still haven't done it, you can appreciate why many of your patients may resist this written exercise as well. There's something unappealing about having to roll up our sleeves and get to work on something real and specific, as opposed to complaining about things in a general way and wallowing in self-pity and resentment. Now do Step 3. Was your response in Step 2 an example of good or bad communication? Did you: Acknowledge the other person's feelings and find truth in what she or he was
Chapter 25
913
trying to tell you? Share your own feelings openly and directly, using "I Feel" Statements? Convey an attitude of caring or respect? After you've completed Step 3, try Step 4. Look at what you wrote down in Step 2 and ask yourself these questions: What are the consequences of my response? What's likely to happen next? How will the other person feel? What will she or he conclude? What's the other person likely to say? Will my statement make the situation better or worse? If you were honest with yourself, you probably just discovered that your response was an example of bad communication, and that you were contributing to the problem in a big way. In fact, you may have discovered that you were actually forcing the person to treat you shabbily. This can be disheartening, especially when you were convinced that you were the victim. This type of analysis takes a lot of courage, even if you're a mental health professional. If you're feeling defensive, annoyed, embarrassed, or ashamed, you can imagine that many of your patients will find it disturbing as well. The good news is that once you've completed the painful part, you're ready for the reward. 48. Five Secrets of Effective Communication After patients complete Steps 1 – 4 of the Revise Your Communication Style form, you can show them how to develop more satisfying relationships with
Chapter 25
914
other people. In Step 5, you can help them write out a more effective response to the person they're not getting along with, using the Five Secrets of Effective Communication on page 242. They include the Disarming Technique, Thought and Feeling Empathy, Inquiry, "I Feel" Statements, and Stroking. Make sure patients indicate which techniques they used in parentheses after each sentence they write down in Step 5. That way, they'll learn how to use the five communication techniques, rather than simply memorizing a few formulaic statements they can use during conflicts and arguments. For example, if the sentence is an example of Thought Empathy and the Disarming Technique, the patient can put (TE; DT) at the end of the sentence. You probably recall doing this earlier in the book when you analyzed conflicts with difficult patients. You'll recall that Don said this to Alyson: "You just need to take care of things. Go home. Get things done! Make those calls!" Here's what Alyson wrote down for Step 5: "You make a good point, Don. (DT; ST) I've noticed that when I tackle these things head on, I usually feel a lot better. (DT)" This response will probably end the discussion. Don will relax and lose his urge to keep giving Alyson helpful advice. Alyson really liked this response because it was radically different from her normal style, and she could see that it would probably be effective. This Revised Response is based on the assumption that Alyson may not especially want Don's advice. If she simply says something flattering, they won't get trapped in a power struggle and can talk about something more rewarding.
Chapter 25
915
Revise Your Communication Style* Step 1. S/he said. Write down exactly what your patient said. Be brief:
Step 2. I said. Write down exactly what you said next. Be brief:
Step 3. Good vs. Bad Communication. Was your response an example of good or bad communication? Why? Use the Good vs. Bad Communication Checklist and the Bad Communication Checklist to analyze what you wrote down in Step 2.
Step 4. Consequences. Did your response in Step 2 make the problem better or worse? Why? What will your patient think and feel?
Step 5. Revised Response. Revise what you wrote down in Step 2. Use the Five Secrets of Effective Communication. After each sentence, indicate which techniques you used in parentheses, using abbreviations. If your revised response still seems ineffective, try again.
* Copyright
1991 by David D. Burns, M.D. Revised 2002.
Chapter 25
916
Some people see the wisdom in this approach, while others find it objectionable. They choke on it and insist that it sounds manipulative. I agree with this criticism to some extent, but I don't think we're morally obligated to be totally sincere with everybody all the time. Of course, if Alyson hadn't like the Revised Response, we could have come up with a different response that was more to her liking. For example, she could say something like this: "Don, you've always got a lot of helpful suggestions, but I sometimes feel like you play the role of the parent, and I end up in the role of the child who needs to be told what to do. Then I feel resentful and frustrated because I'm not really asking for any help or advice. Sometimes I just want you to listen, so I get defensive when you try to help me. "Have you also noticed how we fall into this pattern from time to time? I don't want to sound overly critical or unappreciative, because I think I set you up when I complain that I'm so far behind on everything. Furthermore, I value your friendship a lot, and you're still very important to me." This response will probably lead to a lengthier and more meaningful discussion about their relationship. If it's conveyed with respect, humility and affection, and not with an attitude of blame, this message could be very effective. It will be the more challenging approach, but they may end up feeling a lot closer. Alyson can decide on the response that makes the most sense to her. You can see her completed Revised Your Communication Style form on page 918.
Chapter 25
917
Learning these communication techniques takes time and practice. Your patients will need lots of help and encouragement because they'll make lots of mistakes at first. In fact, these techniques are even difficult for therapists to learn and master, so they're definitely going to be challenging for our patients. This would be a good time for you to complete Step 5 of your Revise Your Communication Style form on page 906. Remember to put the names of the techniques you're using in parentheses after each sentence. Keep in mind that you may have to revise your Step 5 response several times before you come up with something effective. We sometimes have the fantasy that we're supposed to be experts in communication and conflict because we're mental health professionals, but that hasn't been my experience, so be patient with yourself when you're learning how to use them. You'll run into several predictable problems when you try to teach patients how to use these techniques. Many people tend to think concretely. When you suggest a more effective response, a patient might say, "Oh, that sounds great! That's the type of thing I want to be able to say." Then they'll try to mimic what you said, thinking it's some kind of magic formula. Life isn't that easy! Mouthing rehearsed phrases, such as "Thank you for sharing" or "I can see how you might feel that way," always sounds phony. The other person will instantly pick up on the fact that you don't sound natural or real. Although the Five Secrets may sound simple, they're extremely sophisticated. Learning to use them effectively takes time and effort. There are no free lunches!
Chapter 25
918
Revise Your Communication Style* Step 1 – Don said: "You just need to take care of things. Go home. Get things done! Make those calls!" Step 2 – I said: "I'm doing the best I can. I can't do any more. I feel like I'm already under too much pressure." Step 3 – Good vs. Bad Communication. This was bad communication. I failed on all three counts. E = Empathy. Don was probably feeling frustrated because I was complaining, but I didn't acknowledge his feelings. A = Assertiveness. I didn't express my own feelings. I was anxious and frustrated because I felt like he was trying to control me and I just wanted him to listen. Instead of telling him how uncomfortable I felt, I got defensive. R = Respect. He was trying to be helpful but I insisted that I couldn't possibly follow his advice. I didn't convey any respect or warmth, and he probably felt annoyed. Step 4 – Consequences. When I sound helpless and overwhelmed, it inspires Don to give me more advice. Then I make lame excuses and argue with him. This frustrates him, because I'm not listening, so he gets louder and keeps pushing his ideas. I actually encourage him to be controlling. It's like putting fresh cocaine under an addict's nose, and then acting surprised when he snorts it! Step 5 – Revised Response. "You make a good point, Don. (DT; ST) I've noticed that when I tackle these things head on, I usually feel a lot better. (DT)"
* Copyright
2004 by David D. Burns, MD.
Chapter 25
919
Many patients will have trouble distinguishing effective responses from dysfunctional responses. For example, if a patient usually responds in an argumentative, defensive manner, and you model an outstanding response that includes the Disarming Technique and Stroking, the patient may think the response is overly self-effacing and conveys weakness. Some people view any conflict as a competition or battle. They think that one person has to win, and one person has to lose. Since the response you model will not lead to winning in any conventional sense, patients may resist because of their fear that they'll lose if they convey respect or acknowledge any truth in what the other person is saying. In addition, when patients try these techniques on their own, they'll often miss the mark entirely and come up with statements that sound defensive or provocative. Then the conflict will escalate and they'll conclude that the techniques aren't effective. A woman named Mildred insisted that she'd tried the Disarming Technique when her husband criticized her, but it hadn't worked. I asked Mildred what her husband said to her, and exactly what she said next, so I could try to understand why the technique had backfired. She explained that she'd decided to prepare her husband's favorite meal to surprise him when he came home from work. She told me that she'd slaved in the kitchen all day long and had even put candles on the dinner table. When he walked through the door and saw all the elaborate dinner preparations, he seemed a bit befuddled. As they sat down and started to eat, Mildred asked, "How do you like the meal?"
Chapter 25
920
He seemed pleased and said that the meal was great. Then she asked, "Is everything okay? Are you enjoying the food?" He said he loved it, and the only little thing was that the pork was just a tad on the dry side. Mildred felt devastated and flew off the handle. She said, "Well then, you can just take the f___ing pork and stick it up your ass!" I told Mildred I could see why the Disarming Technique hadn't been quite as effective as she'd hoped! Like so many patients, she simply hadn't grasped what the Disarming Technique was. She thought that it meant being nice to the person you were mad at. Of course, there's nothing wrong with being thoughtful or expressing warmth and affection during a conflict. But the Disarming Technique is quite different! Although this is an extreme and somewhat humorous example, this kind of thing happens all the time. Patients will make gross mistakes when they think they're using the Five Secrets of Effective Communication. You'll need to be alert to this, so you don't set your patients up for failure. When you and the patient are writing out Revised Responses in Step 5, you may discover that your first efforts aren't very effective, either. Your statements may sound artificial or stilted, and you may fail to include crucial techniques. This doesn't have to be a problem, as long as you realize that you'll probably have to revise your Step 5 statements several times before you and the patient come up with a response that sounds natural and effective. Remember that we all come from different walks of life, and that different situations require different approaches. The way a clergyman talks to a
Chapter 25
921
parishioner will be very different from the way a gang member might talk to his buddy. Similarly, you wouldn't talk to a police officer who's giving you a ticket in the same way that you'd talk to your spouse during a spat. Can you imagine saying: "Oh, officer, you're so right. (DT) I was speeding. (TE; DT) I can only imagine how hurt and angry you must feel! (FE) Can you tell me more about how you're feeling? (IN) Even though we may be at odds right now, I want you to know that I like you! (ST)" But at the same time, the underlying principles will always be the same. The Five Secrets of Effective Communication are powerful, and can be effective in virtually any type of conflict or setting. Still, many patients will resist these techniques intensely. They'll have strong excuses about why they shouldn't have to listen, express their feelings openly, or treat the other person with respect. For example, a patient may complain, "I shouldn't have to treat Jermaine with respect. He's a total jerk and he treats me like crap. I can't think of anything good to say about him." Notice what's happened. Presumably, this patient indicated a desire to develop a better relationship with Jermaine or we wouldn't have gotten this far in the first place. We assessed his motivation when he first described his conflict with Jermaine, and checked it out again when we did the Relationship CBA. But now he's insisting on treating Jermaine in a shabby manner. You may feel tempted to use logic or persuasion to show this patient how illogical and self-defeating this is. Does he really think he can develop a better
Chapter 25
922
relationship with Jermaine if he continues to treat him in a shabby way? Unfortunately, logic and reason sound good on paper, but they're rarely effective in reality. You'll simply polarize the patient and trigger more complaining and resistance. How would you respond? What would you say to this patient? Put your ideas here before you continue reading:
Chapter 25
923
Answer I'd probably respond paradoxically. I might say: "You're right. I'm sure that Jermaine can be a pain, and you aren't obligated to treat him with respect. It sounds like you might have changed your mind about him. Have you decided that you don't want to develop a better relationship with him after all?" Many patients think about love and anger in a dichotomous way. They don't know how to integrate anger with affection and respect. They either love or hate someone. They also think about other people in a dichotomous way. If they love someone, they think that person is wonderful and they won't ever fight or argue. In contrast, if they're angry, they think the other person is a loser who deserves punishment. Unfortunately, pointing out the illogic of All-or-Nothing Thinking won't help angry patients who have their heels dug in. When patients resist, empathy will be the only thing that works. I've listed 12 good reasons not to listen, not to express your feelings, and not to treat the other person with respect on pages 924 – 926. I keep these lists at my desk. When a patient says, "I shouldn't have to listen to Adrianna because she's wrong," I sometimes say, "You're absolutely right. You don't have to listen to her. In fact, I have a list of good reasons not to listen right here. Why don't we review it together now?"
Chapter 25
924
12 GOOD Reasons NOT to Listen* 1. Truth
I'm right and you're wrong.
2. Blame
It's all your fault.
3. Defensiveness
I have every right to defend myself. You're full of B.S.
4. Mistrust
If I listen to you, you'll take advantage of me.
5. Denial
I'm the victim here. This problem isn't my fault.
6. Entitlement
You should be the way I expect you to be.
7. Control
I want to keep you in a one-down position.
8. Power
I enjoy intimidating you. I like to keep you under my thumb.
9. Competition
One of us must win and one of us must lose.
10. Revenge
I have the right to punish you. You deserve to suffer.
11. Problem-Solving
If we have a problem, we should try to solve it.
12. Hidden Agendas
I don't really want to get close to you.
* Copyright
1989 by David D. Burns, MD. Revised, 2004.
Chapter 25
925
12 GOOD Reasons NOT to Express Your Feelings* 1. Conflict Phobia
People with good relationships should never fight or argue. Conflict is dangerous.
2. Disclosure Phobia
I can't let you see how I feel inside.
3. Emotional Perfectionism
I shouldn't feel the way I do. I should always feel happy and in control of my emotions.
4. Submissiveness
I should always please you, even if I make myself miserable in the process.
5. Approval Addiction
I can't risk criticism. I need your approval to feel happy and fulfilled.
6. Love Addiction
I can't risk rejection. I need your love to feel happy and fulfilled.
7. Perceived Narcissism
You're fragile. If I tell you how I feel, our relationship will fall apart.
8. Hopelessness
I've tried everything and nothing works. You'll never change, so there's no point in trying.
9. Pride
I'm above feeling angry. I don't want to lower myself and let you see how upset I feel.
10. Helping
I must help you if you're upset.
11. PassiveAggression
I'll punish you with silence. I'll get back at you indirectly and maintain a façade of innocence.
12. Mind-Reading
If you really loved me, you'd know what I want and how I feel without my having to tell you.
* Copyright
1989 by David D. Burns, MD. Revised, 2004.
Chapter 25
926
12 GOOD Reasons NOT to Treat the Other Person with Respect* 1. Disdain
You don't deserve my respect.
2. Condescension
I can't think of anything positive to say about you. There's nothing good about you.
3. Hostility
I'm too angry to treat you with respect.
4. Entitlement
You shouldn't be the way you are. I intend to punish you until you change.
5. Blame
You're entirely to blame for our problems.
6. Fear of Vulnerability
I don't want to look weak.
7. Lack of Desire
I don't want to treat you with respect. I don't want to be close to you.
8. Truth
How could I possibly treat you with respect? After all, I have to be honest!
9. Genuineness
It would sound phony.
10. Justice
I have the right to get back at you.
11. Revenge
You've treated me poorly. I have every right to get back at you.
12. Hopelessness
It won't do any good. You'll never change.
* Copyright
1989 by David D. Burns, MD. Revised, 2004.
Chapter 25
927
To put it in a nutshell, when you do Step 5 of the Revise Your Communication Style form, you should anticipate strong resistance. Patients may resist because: The techniques you're modeling sound artificial and phony. This would be an example of valid resistance that results from the therapist's error. They don't really want to get close to the other person. They're still hooked on revenge and blame, and refuse to relinquish the role of victim. Intimacy has a bitter taste. They don't want to examine their own role and experience the humiliation of seeing that they're not nearly as innocent as they thought. They haven't yet "seen" how the techniques really work. When patients protest, don't argue! Instead, surrender and respond paradoxically. Let's try this exercise now. At Step 5, your patient says, "Why should I have to do all the work? When is Harold going to listen and treat me with respect?" What will you say next? Put your ideas here:
Chapter 25
928
Answer Here's one approach: "You know, Cassandra, I agree with you. You shouldn't have to do all the work. Are you saying that you'd prefer not to?" Don't take the bait and argue with this patient. If she's in a defiant mood, go with the flow. Empathize and listen. Find truth in what she's saying, and offer her support. Then you can set the agenda again. Ask if there's a problem that she does want help with and would be willing to work on. Many patients really like the Five Secrets of Effective Communication. Encourage them to work with the Revise Your Communication Style form for at least ten to fifteen minutes every day at home, in much the same way that they'd work with the Daily Mood Log if you were treating their depression. Review their homework during sessions. They will often need your help with Steps 3, 4, and 5. Over time, their skill will increase. Once they've gotten good at generating effective responses on paper, you can use role-playing so they can learn to use these techniques in the heat of battle. Explain that you'll play the role of the person the patient is having trouble getting along with, and you'll make a provocative statement. Ask the patient to respond, using the Five Secrets of Effective Communication. Now you can critique the patient's response. Tell the patient whether their response was an A, B, C, or D. Tell them what worked and what didn't, and why. Give them specific feedback about how they used each of the Five Secrets of Effective Communication. For example, the patient may have a done a good job with Thought Empathy, but you felt frustrated because she or he didn't use the
Chapter 25
929
Disarming Technique or acknowledge the truth in your comment. Perhaps they didn't acknowledge your angry feelings, or express their own feelings of embarrassment, so they ended up sounding phony. Then you can do a role-reversal. You'll play the role of the patient and the patient will play the role of the other person. When the patient attacks you, respond as effectively as you can, using the Five Secrets of Effective Communication. Then ask the patient to critique your response. Try to keep your ego out of the picture, because your response may not be effective, either. Work on the problem together with the patient. Try not to assume the role of expert, because you'll set yourself up for a fall. Continue using role-reversals until you and your patient can both respond skillfully to any statement that the patient might actually encounter when interacting with the other person. At this point, you can encourage the patient to try the techniques with the person they're not getting along with. Warn the patient that there will be times when their efforts won't be effective, especially at first. They may get flustered and revert to old habits, or think they're using the Five Secrets when they're actually being subtly defensive or evasive. When this happens, they can analyze these failures on the Revise Your Communication Style form. They can write down exactly what the other person said to them, and what they said next that didn't work. Then they can complete Steps 3 – 5, and bring the completed form to you at the next session. When you review the form with the patient, it will be easy to see why their initial effort
Chapter 25
930
backfired. You can work together to generate a more effective response. When you do the role-playing exercises, you'll notice that most of your patients have one obvious blind spot, and that they keep making the same type of error over and over again. Here are a few of the most common errors you'll see: Disarming Technique. Many patients won't be able to grasp the truth in the other person's criticisms, or they won't even try. They'll give the other person's statement lip service. Thought Empathy. Many patients will get so anxious that they'll forget to summarize what the other person said. Their response often won't even be in the right ballpark. They'll respond to something the other person didn't even say. Feeling Empathy. Most patients will completely ignore the other person's anger. Then the anger will escalate. Or, they may acknowledge the anger in a way that puts the other person on the defensive. For example, they may say this in a "gotcha" tone of voice: "I can see that you're really angry, aren't you?" Then the other person will angrily deny the anger in order to save face. Alternatively, they may say something fake sounding when they try to acknowledge anger. For example, if their partner says, "Screw you!" the patient may reply, "I just heard you say, 'Screw you.' (TE) I take it you're feeling a bit angry. (FE) Thank you for being so honest with me. (ST)" Of course, this type of formulaic response will infuriate the other person. Inquiry. Patients may apologize or offer to solve the problem, rather than
Chapter 25
931
encouraging the other person to talk about his or her feelings. "I Feel" Statements. Patients will often fail to express their feelings. Or, they may express their feelings in an overly self-effacing way in a subtle attempt to get pity and prevent the other person from expressing anger. Stroking. Patients may sound insincere, sarcastic or passive-aggressive when they try to express respect or caring. This is often because they're repressing their own negative feelings, so the anger comes bubbling out indirectly and contaminates the expression of genuine affection or respect. You can easily create role-playing exercises to help patients get past their blind spots. For example, if a man compulsively "helps" his wife, rather than acknowledging her feelings, you can play the role of the wife, and repeatedly express negative feelings. His job will be to respond with Feeling Empathy. I've had patients who missed it more than ten times in a row. They couldn't resist the knee-jerk reaction of giving advice or offering to solve the problem. Then, they suddenly got it, and were able to use Feeling Empathy for the first time. 49. One-Minute Drill When you're working with two people at the same time, such as a husband and wife with a troubled marriage, techniques like the Relationship CBA and Revise Your Communication Style form won't be effective. These techniques are far too complex and revealing for couple's work. For example, if you ask one partner to analyze his or her communication errors on the Revise Your Communication Style form, the other partner will sit back and say, "I told you so!" Now you're into a triangulated situation of blame and counterattack, and you end
Chapter 25
932
up triggering the problematic dynamic you're trying to modify. A comprehensive approach to the treatment of troubled couples is beyond the scope of this book, but I'll describe one useful technique you can hang your hat on when you're working with two people at the same time. I want to caution you that you can't just jump in and use this technique with every troubled couple you see. People who are in an angry, blaming mindset can sabotage any technique you might try. First, you'll have to do a comprehensive evaluation of the couple. I'd suggest meeting with both partners together, as well as with each of them separately, so you can assess their goals and motivation. You'll have to explain that it's unethical for you to keep secrets from either of them. If they decide to tell you a secret, like the fact that they're having an affair, they'll have to share this information with their partner. If they're reluctant to share the information with their partner, they'll have to give up on the idea of receiving couple's therapy from you. In fact, you won't be able to offer even one additional session to their partner, single or conjoint. That being said, tell each of them that you want to know where they stand. Do they each have a firm commitment to this relationship, or are they struggling with urges to separate? Are they strongly motivated to make the relationship better, or do they simply want to pay lip service to couple's therapy as one last step before separation or divorce? It will be far easier for them to answer these questions honestly if they are meeting with you alone. It can sometimes be helpful to do the Relationship CBA with each partner
Chapter 25
933
separately, as described on page 894. If either of them clings the belief that the other partner is to blame, I would not accept that individual into couple's therapy. My clinical experience has shown me over and over that I can't treat anyone who doesn't have a strong desire to change. If the patient is only there to help me straighten out their partner, I'd let them know that I probably can't accept them into treatment because they don't have a suitable therapeutic agenda. Finally, I'd ask both partners if they were willing to do daily psychotherapy homework, such as communication exercises, throughout the treatment. If either of them has the slightest reservation about this, I would not accept that person into treatment. If they both seem suitable for couple's therapy, the One-Minute Drill can be a good technique to use early in the treatment. It's especially helpful for turbulent couples who can't resist the urge to criticize and counterattack each other. It quickly breaks the pattern of accusation and arguing, and shifts the dialogue to a level of greater vulnerability, intimacy, and trust. Both partners learn effective self-expression skills and highly accurate listening skills that are radically different from the way they typically communicate when they're upset. However, there's a downside to this technique. It's somewhat artificial and doesn't lend itself to natural conversation. I would view it as a stepping-stone to more sophisticated techniques. Here's how the One-Minute Drill works. Explain that one partner will be the Talker and the other will be the Listener. Either partner can be the Talker first. The Talker will spend 30 seconds expressing his or her feelings about the
Chapter 25
934
relationship. The Talker can say anything that she or he wants. The Listener's job is to listen attentively without speaking, and to try to tune in to what the Talker is saying. The Listener does not have to agree or disagree with the Talker, but should try to see the world through the Talker's eyes. The Listener should be like a court reporter, and try to comprehend every idea the Talker expresses. The Listener should also try to understand how the Talker is likely to be feeling, given what she or he is saying. Tell the Listener to use receptive body language. This involves looking directly at the Talker without shaking the head, folding the arms, frowning or sighing. When the Talker has finished, the Listener will summarize what she or he said as accurately as possible. The Listener can paraphrase exactly what the Talker said and acknowledge how the Talker was probably feeling inside. This is actually a form of Thought Empathy (TE) and Feeling Empathy (FE). Here's a brief example of what the Listener might say: "Jake, you said that I never support you when you come home from work. (TE) Instead, I nag you and put more demands on you. (TE) You also said that I don't seem to appreciate all your hard work, and what you do to support our family. (TE) I can imagine you're probably feeling frustrated and angry with me. (FE)" Then the Talker can give the Listener a grade for accuracy, between 0% and 100%. If the grade is below 95%, the Talker can explain what the Listener missed. For example, Jake might say:
Chapter 25
935 "Paige, I'll give you an 85%. You got most of it right, but you
missed one thing. I do feel frustrated and angry, but I also feel lonely and rejected because I'd like more support, too. I wish we felt closer to each other. I often feel shut out and picked on." Now Paige can summarize this part: "Okay. It's not just that you feel angry and frustrated, but you also feel lonely and shut out, and wish we felt closer to each other. (FE) You sometimes feel picked on, and want more support from me. (FE; TE)" Now Jake will probably say, "Now you got it. That's 100%." Once the Listener's grade is 95% or higher, they're ready for a rolereversal. Now the Listener will be the Talker, and vice versa. If the exercise seems to be going well, I ask the couple how they felt during the exercise. Usually, they both say it was a great relief, and a lot different from what usually happens when they try to communicate. I ask them why it was different, and why it felt so good to them. I point out that what they were doing was rather simple. Instead of arguing defensively and insisting on their own agenda, they were focusing on how the other person was thinking and feeling, and finding some truth in it. They were also learning to express their feelings in a more open and direct way, without so much defensiveness and counterattack. That's because they knew that their partner was listening, and would summarize what they'd just said. Of course, the two partners are learning to use the Five Secrets of Effective Communication, but we're teaching these techniques in a more
Chapter 25
936
structured way because we're working with two people at the same time. The Talker primarily uses "I Feel" Statements, and the Listener primarily uses Thought Empathy, Feeling Empathy, and Inquiry. Once they've practiced the One-Minute Drill a few times in your office, the Listener will usually be able to get 95% accuracy ratings the first time she or he summarizes what the Talker says. Then the speed will pick up considerably. One partner will talk, the other will summarize, and they can reverse roles immediately. You can increase the pace by reducing the amount of time the Listener talks to approximately 15 seconds. Eventually, the exchanges will approach the pace of normal conversation. If they like the One-Minute Drill, and do a reasonably good job with it in your office, you can assign the exercise as homework. The way you set it up will be crucial. First, I ask if they'd be willing to practice together for fifteen minutes, five times a week, between sessions. If either of them expresses any reluctance, you might have to reassess that individual's motivation. Sometimes, you'll have to meet with that person separately to find out what's going on. When you meet with the reluctant partner, you can explain that you're concerned that they might have developed mixed feelings about the couple's therapy, since they seem to have changed their mind about doing the homework. If they express ambivalence, I wouldn't try to persuade them to remain in treatment. Instead, I'd explore their feelings and assess their motivation. They may have a hidden agenda they didn't previously disclose. They may also be
Chapter 25
937
committed to the idea that the problems are all their partner's fault. I'd ask if they wanted to continue with couple's therapy, and what they'd be willing to do if I agreed to continue working with them. In contrast, if both partners are willing to do homework, I'd ask them what times would work well for both of them, and where they intend to do it. Let's assume that they agree to practice from 8:00 – 8:15 PM in the den every evening, Monday through Friday. I'd say this: "Okay, I'd like you both to sit in the den with the door closed in two chairs facing each other. You're not allowed to have any distractions, like children in the room. Keep the TV and radio off. No snacking, and you both have to be sober. Make sure you each get at least one chance to be the Talker and one chance to be the Listener. If you want to do more, that's fine, but you have to do at least that much." If they both agree to this arrangement, I turn to one of them and say something like this: David: Paige, I take it that you agree to practice in the den every evening from 8:00 to 8:15, Monday through Friday? Paige: Yes, that sounds okay. David: I want to make sure there's no misunderstanding about this at all, and I want to be very clear that this agreement will be between you and me. Do you agree to sit in the den for fifteen minutes every night, whether or not Jake shows up to do his part? Paige: That doesn't make any sense. Why should I have to sit there if
Chapter 25
938
Jake doesn't show up? David: Because you've made an agreement with me to do it. That will prove to me that you're committed to this relationship, and you won't let Jake sabotage your determination. I need your absolute, irreversible commitment to sit in that chair for fifteen minutes every night, Monday through Friday, no matter what. Paige: What am I supposed to do if he doesn't show up? David: Anything you want. You can bring a book and read if you want. But you must sit in that chair for fifteen minutes. Do we have a deal? Paige: Well, what about Jake? Why is it all on me? David: I'm going to make arrangements with Jake in just a moment. But right now, I want to find out if you and I have a deal. Once she agrees, I'll make a similar arrangement with Jake. I set the homework up as a contract between each partner and me. That way, it will be abundantly clear what's happening if one of them doesn't follow through. Otherwise, they'll blame each other. They'll say, "Oh, I didn't come because John didn't show up the day before. It's his fault. He's just showing his true colors." As you can see, the homework functions on two levels. First, the practice will help the couple assimilate the tools they're learning during sessions. Second, the homework will function as a behavioral test of motivation. If either partner fails to show up for the homework exercises, it will indicate a lack of commitment to the treatment, and you may need to reassess whether ongoing couple's therapy is indicated.
Part Seven How to Create a Cutting-Edge Treatment Program for Any Patient with Any Axis I or II Disorder
26*
Selecting the Most Effective Techniques for Your Patients
Let's assume that you've done a sound initial assessment and you're testing your patient at every session. You're receiving excellent empathy scores and you've developed a solid therapeutic agenda. There are 50 CBT techniques to choose from. Which ones should you try? Although you can't predict which techniques will work for any patient or problem, there are several guidelines that can be helpful, as long as you don't take them too seriously or apply them too literally. You can select techniques based on: The distortions in the patient's thought. The type of problem the patient wants help with. The patient's interpersonal style.
* Copyright
2004 by David D. Burns, M.D.
All
* Copyright 2004 by David D. Burns, M.D. Depression and Anxiety Disorders All Habits and Addictions Anxiety Disorders
Page 941
One-Minute Drill
The Five Secrets
Revise Your Communication Style
Interpersonal
Cognitive
Exposure
Relationship CBA
Rejection Practice
Flirting Training
Self-Disclosure
David Letterman Technique
Smile and Hello Practice
Memory Rescripting
Classical
Motivational
Image Substitution
Cognitive Flooding
Distraction
Response Prevention
Gradual Exposure and Flooding
Anti-Procrastination Sheet
Pleasure Predicting Sheet
Daily Activity Schedule
Decision-Making Form
Uncovering
Stimulus Control
Devil's Advocate Technique
Cost-Benefit Analysis (CBA)
Hidden Emotion Technique
What-If Technique
Interpersonal Downward Arrow
Visual Imaging
Spiritual
Role-Playing
Humor-Based
Quantitative
Semantic
Cognitive
Individual Downward Arrow
Cognitive Hypnosis
Humorous Imaging
Time Projection
Acceptance Paradox
Feared Fantasy
Externalization of Voices
Shame-Attacking Exercises
Paradoxical Magnification
Negative Practice / Worry Breaks
Self-Monitoring
Be Specific
Logic-Based
Truth-Based
Compassionate
Basic
Let's Define Terms
Semantic Method
Thinking in Shades of Gray
Socratic Method
Reattribution
Survey Technique
Experimental Technique
Examine the Evidence
Double Standard Technique
Straightforward Technique
Agenda Setting
Empathy
How to Select Techniques for Each Distortion* Interpersonal
All-or-Nothing Thinking Overgeneralization
Mental Filter
Discounting the Positive Jumping to Conclusions Mind-Reading Fortune-Telling Magnification & Minimization Emotional Reasoning Should Statements
Labeling Blame Self-Blame Other-Blame Relationship Problems
All
* Copyright 2004 by David D. Burns, M.D. Depression and Anxiety Disorders All Habits and Addictions Anxiety Disorders
Page 942
One-Minute Drill
The Five Secrets
Revise Your Communication Style
Interpersonal
Cognitive
Exposure
Relationship CBA
Rejection Practice
Flirting Training
Self-Disclosure
David Letterman Technique
Smile and Hello Practice
Memory Rescripting
Classical
Motivational
Image Substitution
Cognitive Flooding
Distraction
Response Prevention
Gradual Exposure and Flooding
Anti-Procrastination Sheet
Pleasure Predicting Sheet
Daily Activity Schedule
Decision-Making Form
Uncovering
Stimulus Control
Devil's Advocate Technique
Cost-Benefit Analysis (CBA)
Hidden Emotion Technique
What-If Technique
Interpersonal Downward Arrow
Visual Imaging
Spiritual
Role-Playing
Humor-Based
Quantitative
Semantic
Cognitive
Individual Downward Arrow
Cognitive Hypnosis
Humorous Imaging
Time Projection
Acceptance Paradox
Feared Fantasy
Externalization of Voices
Shame-Attacking Exercises
Paradoxical Magnification
Negative Practice / Worry Breaks
Self-Monitoring
Be Specific
Logic-Based
Truth-Based
Compassionate-Based
Basic
Let's Define Terms
Semantic Method
Thinking in Shades of Gray
Socratic Method
Reattribution
Survey Technique
Experimental Technique
Examine the Evidence
Double Standard Technique
Straightforward Technique
Identify the Distortions
Agenda Setting
Empathy
How to Select Techniques for Each Disorder* Interpersonal
Depression
Anxiety Disorders
Relationship Problems
Addictions
Procrastination
Non-Problems Relationship Problems
Chapter 26
943
If you review the table on page 941, you'll see that the ten cognitive distortions are listed along the left, and the techniques appear across the top, grouped by category. Identify the Distortions is not included with the Basic Techniques because it would be redundant. The checkmarks indicate techniques that might be useful for each distortion. If a checkmark is highlighted,
, it means that the technique is likely to
be a particularly good choice. You'll notice that I've highlighted Empathy and Agenda Setting for every distortion because these techniques will always get you off to a great start. Let's say that your patient is struggling with public speaking anxiety, and he's recorded this negative thought on his Daily Mood Log: "I shouldn't be so nervous! Other people don't feel this way." This is an obvious Should Statement. On page 941, you'll see that the Semantic Method is an excellent choice for Should Statements, so I'd definitely include it on my Recovery Circle. The Externalization of Voices and Acceptance Paradox are also highlighted for this distortion, so I'd include them as well. The negative thought also contains Self-Blame, Mind-Reading, the Mental Filter, Magnification and Minimization, and Emotional Reasoning. You can see that the Cost-Benefit Analysis and the Double Standard Technique are often good choices for Self-Blame. The Survey Technique, Self-Disclosure, and Feared Fantasy can be especially effective for Mind-Reading. Other useful techniques for these distortions might include Gradual Exposure, Cognitive Flooding, and Image Substitution. In addition, any of the Uncovering Techniques,
Chapter 26
944
like the Individual Downward Arrow, the What-If Technique, or the Hidden Emotion Technique, could be very revealing. Don't just blindly select all the highlighted techniques for your Recovery Circle. Instead, try to keep the context in mind and see if you can picture how each technique might work before you include it. Of course, you can choose techniques that aren't checked as well, because they'll often be a good fit for the problem you're working on. I start every Recovery Circle with the four Basic Techniques. We’ve already selected 14 additional techniques, and we’re just getting started. So you can see that it’s easy to list many techniques for the thought in the middle of the Recovery Circle. Once you’ve practiced a few times, you’ll be able to select 20 – 25 potentially helpful techniques for practically any negative thought. You can also select techniques based on the type of problem the patient wants help with. If you look at the table on page 942, you'll see that Empathy and Agenda Setting will be needed for any disorder. You simply can't treat patients without a strong therapeutic alliance and a collaborative agenda. After that, however, the selection of techniques will vary considerably for different kinds of problems. You may recall from the Conceptualization step of Agenda Setting that there are four basic types of problems to consider. In the following pages, we'll talk about how to select the most effective techniques for: Individual mood problems, such as depression and anxiety (page 945) Relationship problems, such as a marital conflict or a problem with a friend or
Chapter 26
945
colleague (page 962) Habits and addictions, such as procrastination, an eating disorder, or drug or alcohol abuse (page 964) Non-problems, like healthy grief (page 968) Individual Mood Problems: Depression There's some overlap, as well as some important differences, in the treatment of depression and anxiety. If the patient is depressed, Motivational, Cognitive, and Uncovering Techniques will be invaluable. For example, the Daily Activity Schedule and Pleasure Predicting Sheet can help patients break the vicious cycle of do-nothingism and get productively involved in more pleasurable and rewarding activities. A Cost-Benefit Analysis (CBA) can help you identify hidden agendas and rewards that keep the patient trapped in feelings of self-pity, inferiority and hopelessness. Cognitive Techniques, like the Double Standard Technique, Examine the Evidence, the Socratic Method and the Semantic Method, will help the patient put the lie to the distorted thoughts that create the feelings of worthlessness and hopelessness. An Uncovering Technique, like the Individual Downward Arrow, will help you identify the patient's Self-Defeating Beliefs, such as Perfectionism, the Achievement Addiction, and the Love Addiction. The Acceptance Paradox and Externalization of Voices will help the patient develop unconditional selfesteem and a more meaningful personal value system. Individual Mood Problems: Anxiety Disorders Most therapists use only one favorite type of intervention for anxiety. For
Chapter 26
946
example, if a patient is struggling with OCD, many therapists will choose Exposure and Response Prevention. Exposure and Response Prevention will often be helpful, but they're rarely curative. You'll do far better if you include a wide variety of Cognitive, Uncovering, and Motivational Techniques on your Recovery Circle. The Hidden Emotion Technique plays a unique role in the treatment of anxiety and should always be included. As many as three-quarters of the patients who suffer from anxiety disorders will have hidden problems or feelings, such as anger, that they've been sweeping under the rug because of their need to be "nice." When they bring the hidden feelings to the surface and solve the problems that are bugging them, the feelings of anxiety will often disappear. Certain CBT techniques can be particularly helpful for specific types of anxiety. However, you should always stick to the basics! Don't just attack the patient with your favorite techniques just because she or he is suffering from a particular anxiety disorder. Instead, you and the patient can generate a Daily Mood Log, pick one negative thought, and select a wide variety of techniques for your Recovery Circle. With that in mind, here are some suggestions for treating GAD, OCD, PTSD, phobias, panic attacks, shyness, and performance anxiety, as well as Somatoform Disorders such as hypochondriasis and chronic pain. Generalized Anxiety Disorder (GAD). If the problem involves chronic worrying, you'll want to include the Cost-Benefit Analysis and Hidden Emotion Technique on your Recovery Circle. The CBA will address the magical thinking. For example, an anxious woman may believe that her worrying is an expression
Chapter 26
947
of love that will protect her family from danger. The Hidden Emotion Technique will help you pinpoint any feelings or conflicts that may be lurking behind the constant worrying. This technique can be challenging because anxious patients are so good at ignoring the problem that's really bugging them. It may be easier for you to identify the suppressed feeling if you ask yourself this question: is there some feeling that the patient is trying to cover up with the worrying? For example, an overly nice patient who constantly worries that her loved ones may contract fatal illnesses may be harboring feelings of resentment toward them that she's been sweeping under the rug. You can propose these possibilities, but your guesses will nearly always be incorrect. In my experience, the patient is the only one who can come up with the hidden problem. However, your guesses will prime the pump and make it a bit easier for the patient to bring the problem to conscious awareness. In selected cases, Cognitive Hypnosis may be a useful uncovering and treatment tool for GAD as well, especially if the hidden feelings are buried in the past. Obsessive-Compulsive Disorder (OCD). Exposure and Response Prevention are probably the most important keys to the treatment of OCD. However, the Cognitive Techniques can be extremely helpful as well, such as the Double Standard Technique, Examine the Evidence, the Experimental Technique, the Socratic Method, the What-If Technique, and Self-Monitoring. Motivational Techniques like the Paradoxical CBA will often play an important role in the treatment of OCD. Although the obsessions and compulsions are inconvenient and sometimes even crippling, there will usually be
Chapter 26
948
lots of obvious and hidden advantages in maintaining them. For one thing, patients won't have to confront the intense discomfort that invariably accompanies Exposure and Response Prevention. In addition, if they do recover, they may have to face problems in their lives and begin to do things they've been avoiding because they've been so consumed by their OCD rituals. Cognitive, Motivational and Exposure Techniques will usually lead to partial but incomplete recovery. The Hidden Emotion Technique will often bring the patient the rest of the way home, and will give you a far more meaningful understanding of the suppressed feelings that may have triggered the obsessions and compulsions in the first place. A woman named Sharon had many different kinds of obsessions and compulsions, including an intense fear of the number three. She spent a great deal of time every day making sure that none of the objects in her home were arranged in groups of three. This included groups of chairs, decorations, and magazines on the coffee table. I asked Sharon what she was so afraid of. What would happen if things were arranged in groups of three? She began to cry and confessed that she had a fear of having an extramarital affair. She claimed she loved her husband very deeply, but feared she'd give in to an irrational impulse to sleep with someone else if she slipped up. She wasn't actually interested in anyone specific—she was simply afraid of losing control sexually and becoming a "wild woman." I noticed that Sharon had a low score on the Relationship Satisfaction Scale. A bit of exploration revealed that although she loved her husband, she
Chapter 26
949
was deeply disappointed in their marriage and thought that he was far too dependent on his intrusive, controlling mother. She felt like she was in constant competition with her mother-in-law for her husband's loyalty and attention, and resented the fact that he always defended his mother during their many arguments. In spite of the tension they both felt, they seemed committed to each other and responded positively to a brief course of couple's therapy. If I hadn't used the Hidden Emotion Technique, I never would have discovered the real cause of her OCD symptoms, and the treatment probably would have been considerably less effective. Posttraumatic Stress Disorder (PTSD). Memory Rescripting was designed specifically for PTSD. Cognitive Hypnosis can also be effective and may enhance the effects of any Cognitive Exposure Techniques you use. However, I've seen many PTSD patients respond extremely well to other kinds of CBT Techniques, such as Reattribution, Examine the Evidence, the Double Standard Technique, and the Cost-Benefit Analysis (CBA). You may remember reading about Sam, the young man who was robbed by armed gunmen and left to die in a walk-in freezer at the fast food restaurant where he worked. Months later, Sam was still flooded with constant anxiety and anger. In spite of his intense discomfort, Sam was ambivalent about change. On the one hand, he wanted relief, but at the same time, he believed that his anxiety would protect him from a similar catastrophe in the future. He also believed that his anger proved that he was strong and determined to get revenge on the men who abused him.
Chapter 26
950
When we did a CBA, Sam had a change of heart because he could see that the disadvantages of his PTSD symptoms greatly outweighed the advantages. For one thing, there was no evidence that his constant worrying was really keeping him safe. In addition, it dawned on him that the men who robbed him had no idea how angry he was, so he was the only one who was really suffering. Over the next few weeks, Sam and I used a variety of additional CBT techniques, and his symptoms disappeared completely. Phobias, including Agoraphobia. Gradual Exposure or Flooding will be the key to the treatment of any phobia. However, you shouldn't ignore the Cognitive Techniques. For example, the Experimental Technique may be extremely effective because it involves exposure along with an innovative cognitive component. At the end of the first day of my Scared Stiff workshop at a hotel in Salt Lake City, a woman named Sheryl approached me while I was packing up my overheads. Sheryl explained that she'd been struggling with a number of phobias for many years, including the fear of elevators, hallways, tunnels, flying and driving. These fears were fouling up her life. Although she'd been talking about her problems in depth with a therapist for nearly ten years, she still hadn't gotten over any of her phobias. She wanted to know if I thought there was any hope for someone with problems as bad as hers. I said, "Oh, definitely! There's always lots of hope." She asked, "How long do you think it would take to get over my phobias?" I said, "It's hard to predict, but it might not take long at all. In fact, we could
Chapter 26
951
work on your elevator phobia right now if you wanted to." She looked surprised and asked, "What would I have to do?" I said, "There's an elevator just around the corner in the lobby. It only goes up five floors, but that would probably be good enough. All you have to do is get on the elevator and stay there until you're cured. I have to finish packing up my overheads, so I'll wait here for you." She protested, "But shouldn't we talk about the traumas in my life first?" I said, "It sounds like you've been talking about them for a long time already. But I'd be happy to chat with you after you get over your elevator phobia if you still want to." Sheryl seemed shocked and said she was way too scared to ride the elevator alone. She wanted me to go with her. I said, "No, you've got to face your fears alone. If it's not frightening, it won't work. If I come with you, you won't be afraid, so it won't do you any good." Sheryl insisted that even if I were with her in the elevator, she'd still be terrified, so I agreed to go with her. When we got on the elevator, Sheryl estimated her anxiety at 100%. I pressed the button for the fifth floor and asked what thoughts were going through her mind. She had two negative thoughts: 1. The walls will start closing in and we'll be crushed. 2. We'll use up all the oxygen and suffocate. She said she believed these thoughts 100%. I told her that we could do some experiments to test them. I asked her to touch the walls, so she could find out if they were closing in on us. She felt the walls, and admitted that they didn't
Chapter 26
952
seem to be moving or closing in on us at all. I said, "Well, keep checking them from time to time. We could be crushed at any moment." Then I asked her to take a deep breath to see if the oxygen had disappeared yet. She was surprised that there seemed to be plenty of air. I asked Sheryl how anxious she was feeling now. She said she was still frightened, but her anxiety had fallen to 90%. I asked if she could push it back up to 100%. I said I wanted her to freak out completely. She looked upset and said, "Why do you want me to freak out? That's the exact opposite of what my therapist has been telling me. She's been teaching me relaxation techniques so I can learn to control my anxiety. Shouldn't I try to control it?" I said, "My approach is just the opposite. When you try to control your anxiety, it often gets worse, because you end up struggling with the monster. Instead, I want you to confront the monster and surrender to it. Let the anxiety come. Your problem is that you're not nearly anxious enough. I want you to push it up higher. Make it as bad as you can!" By this time, we were up to the third floor, and I asked how anxious she was feeling. She apologized and said her anxiety had fallen to 70%. I said, "Sheryl, that's no good! Try to make yourself more anxious. I want to see a fullfledged panic attack!" At this point, the elevator stopped on the fourth floor, and several people
Chapter 26
953
got in. I turned to them and said, "Don't get upset if we seem to be behaving strangely. I'm a shrink, and I'm treating this woman's elevator phobia. She's probably going to freak out at any moment." Everyone started giggling, including Sheryl. When the elevator doors closed, I asked how anxious she was. She said she was only 20% anxious now. A moment later, we arrived on the fifth floor and the other people got out. Sheryl said her anxiety was gone. We rode the elevator down to the first floor and back up to the fifth floor, but she couldn't conjure up any more anxiety. I got off and told her to ride it alone for a while. I explained that she'd probably freak out, and reminded her to make herself as anxious as possible. When she returned from her solo flight a minute later, she was giggling. She said, "I can't believe it. I have no idea how you did it, but I don't have one ounce of anxiety at all! I'm totally relaxed!" Sheryl was thrilled, but reminded me that she also had a fear of tunnels and hallways. I pointed out that we were at the end of a long, narrow hallway on the fifth floor of the hotel. She said it looked terrifying. I instructed her to walk slowly to the far end of the hallway while I waited for her next to the elevator. I encouraged her to make herself as anxious as possible on the way. As she began walking down the hall, I made creepy sounds in a warbling voice. I said, "Oohhh, oohhh," like in a ghost movie. She started giggling. I said, "Don't giggle. I want you to freak out." When she got to the end of the hall, she turned around and said, "For some reason, I'm not scared."
Chapter 26
954
I said, "Okay, imagine you're in an Alfred Hitchcock horror movie, and run toward me screaming at the top of your lungs. That might help." She started screaming and waving her arms wildly while she ran down the hall. When she reached me, I asked her how anxious she was feeling. She said, "It's zero. I don't have any anxiety at all! I'm not afraid of halls or tunnels any more." "That's great," I replied. "Now we can go back and delve into your past while I pack up my overheads." Sheryl smiled and said, "I don't think I'll need to do that any more!"* Why was this brief intervention so effective? Sheryl had been struggling with her phobias for more than ten years. When we rode the elevator, I encouraged her to do experiments to test the distorted thoughts that caused the fear. When she touched the walls, she discovered that they weren't really closing in, as she'd imagined. And when she took a deep breath, she realized there was plenty of air. In addition, she took the battle to the enemy. She finally said, "Take your best shot. I'm not running away any more." The moment she surrendered and faced her fears, the spell was broken. This requires tremendous courage, but the payoff can be enormous. Although the Experimental Technique was curative for Sheryl's phobia, this won't always be the case. Sometimes, a hidden problem or feeling will be hiding behind a phobia. If so, bringing it to conscious awareness with the Hidden * It was a funny, silly little grin, so I gave her a funny, silly little grin back.
Chapter 26
955
Emotion Technique can have impressive anti-anxiety effects as well. Panic Disorder. During panic attacks, patients will nearly always have thoughts like these: I'm about to pass out. I'm about to have a heart attack. I'm about to die. I can't breathe deeply enough. I'm going to suffocate. I'm about to lose control and go crazy. According to the cognitive model, panic attacks result from the misinterpretation of benign bodily sensations. Patients who are prone to panic attacks may hyperventilate when they're upset, which causes sensations of dizziness, tightness in the chest, and tingling fingers. If you hyperventilate for a few minutes right now, you'll see what I mean. The patient misinterprets these symptoms as signs of imminent physical or psychological collapse. These distorted cognitions trigger feelings of intense fear. Then Emotional Reasoning kicks in. The patient thinks, "I feel terrified, so I must be in danger. Something awful is about to happen." So the negative thoughts and feelings feed each other and rapidly escalate into a vicious cycle of sheer panic. Any of the Cognitive Techniques can be useful, but Examine the Evidence and the Experimental Technique will usually play a key role in the treatment of panic attacks. These are Truth-Based Techniques. You can instruct the patient to use these techniques during naturally occurring panic attacks, or you can use
Chapter 26
956
them after you induce a panic attack in your office. If you want to try this, you'll need a trusting relationship with the patient and a solid therapeutic agenda, because the panic induction can be frightening. You can induce a full-blown panic attack (Flooding) or a partial panic attack (Gradual Exposure). We'll look at Gradual Exposure first. Let's assume that your patient typically gets dizzy during her panic attacks and believes that she's about to go crazy. You could ask her to sit in an office chair, and explain that you're going to spin her around in order to create feelings of dizziness. Ask her how much dizziness and panic she can endure, on a scale from 0% – 100%. Let's say she agrees to 50%. Tell her to raise her hand to let you know when she's at 50%. When she raises her hand, ask how panicky she feels and how strongly she believes she's about to go crazy. If she's strongly convinced she's on the verge of going crazy, you can use Examine the Evidence and ask, "How many times in the past have you felt convinced that you were about to go crazy?" She'll probably tell you that she's had this fear dozens of times. Then you can ask, "How many times have you actually gone crazy when you had this fear?" She'll almost definitely say never. Then you can say, "So it sounds like even though you've thought you were going crazy on many occasions, you've never actually gone crazy. Are you saying that there's no real evidence that you're on the verge of going crazy?" She'll probably insist that even though it hasn't happened yet, it could still happen at any moment because she feels like she really is on the verge of
Chapter 26
957
losing control and having a nervous breakdown. You can point out that feelings aren't the same as facts, and that we often have strong feelings that aren't valid. For example, when you buy a lottery ticket, you may have the strong feeling that you're going to win the $100 million jackpot, but it probably isn't going to happen. You can ask her once again if there's any convincing evidence that she really is going crazy. For example, is she hearing voices coming from outside her head? Is she having visual hallucinations? You can also use the Experimental Technique and encourage her to do simple experiments to test her belief that she's going crazy. For example, can she count backwards from 100 by 7s out loud? Can she read a sentence from the newspaper and tell you what it means? Can she call information and ask for someone's phone number? She'll discover that she can do all of these things. Then you can ask how strongly she now believes that she's going crazy. If she's receptive to this approach, you can encourage her to practice at home. She can spin herself around in a chair, or stand and spin until she experiences a certain level of dizziness and panic. Then she can test her belief that she's going crazy by doing the same kinds of experiments she did in your office. Each time she practices, she can increase the level of dizziness and panic that she's able to endure. Research studies indicate that this approach can be very effective for panic in either individual or group therapy, with most patients experiencing a complete elimination of symptoms within five to ten sessions. Alternatively, if the patient trusts you and is open to it, you can use Flooding. You may remember reading about June, the woman who had the fear
Chapter 26
958
of losing control and going crazy. I encouraged her to try to drive herself crazy in my office. When she discovered that she couldn't go crazy, no matter how hard she tried, she suddenly recovered from more than 50 years of panic and agoraphobia. Shyness. Ask the patient to describe one social situation that made them feel shy and self-conscious at the top of a Daily Mood Log, and to indicate what they were thinking and feeling. Each patient's thoughts and feelings will be unique. For example, you may remember Jason, the young man who was afraid to flirt with the cashier at the grocery store. One of his negative thoughts was, "People will think I'm a self-centered jerk if I try to flirt with her." After you've identified the negative thought the patient wants to work on first, put it in the middle of a Recovery Circle, and select a variety of techniques that will help the patient put the lie to it. You can include Cognitive Techniques like the Double Standard Technique, Examine the Evidence, the Survey Technique, Let's Define Terms, Thinking in Shades of Gray, the Semantic Method and the Externalization of Voices. Uncovering Techniques like the Downward Arrow will help you pinpoint the patient's Self-Defeating Beliefs, such as Perceived Perfectionism, the Approval Addiction, the Love Addiction, the Spotlight Fallacy and the Brushfire Fallacy. The Rejection Feared Fantasy and the Acceptance Paradox can help the patient overcome the fears of rejection or disapproval. Motivational Techniques will help you identify factors that keep the patient stuck. For example, the patient could list the advantages and disadvantages of
Chapter 26
959
this negative thought: "If I try to talk to her, I know I'll get shot down, so there's no point in trying." Ultimately, shy patients will have to move beyond armchair CBT work in your office and confront their fears in the real world using Interpersonal Exposure Techniques, such as Smile and Hello Practice, the David Letterman Technique, Self-Disclosure, Flirting Training, and Rejection Practice. Shame-Attacking Exercises can also be extremely helpful, although they require tremendous courage. If you have enough patients to run shyness groups, you can do many of these exercises, such as Smile and Hello Practice and Shame-Attacking Exercises, as group projects. This makes them seem slightly less threatening. When I do intensive workshops for small groups of therapists, we often go out to dinner together. On the way to the restaurant, we do group ShameAttacking Exercises, such as lying down on the sidewalk outside the entrance to the hotel we're staying in, or jumping up and shouting out the names of the stops on the bus. Try to select exercises that will be fun and funny. Avoid activities that might seem offensive, hostile or in poor taste. Of course, this will differ radically in different settings, so use good judgment. Performance Anxiety. Public speaking anxiety is one of the most common types of performance anxiety. Nearly all of us get a bit nervous before we have to talk in front of a group. Patients with public speaking anxiety will have thoughts like this: "My mind will go blank. Everyone will see how nervous I am and look down on me. I just know I'm going to make a fool of myself. What's wrong with me? I shouldn't be
Chapter 26
960
so inept!" Any of the Uncovering Techniques, such as the Individual Downward Arrow, the Interpersonal Downward Arrow, and the What-If Technique, will help you pinpoint the SDBs underneath these thoughts. They typically include Perfectionism, Perceived Perfectionism, the Achievement Addiction, the Approval Addiction, the Spotlight Fallacy, the Brushfire Fallacy, Superman/Superwoman, and others. Often, a hidden emotion is lurking behind the public speaking anxiety, specifically anger, because the patient imagines a world that's filled with people who are extremely judgmental and rejecting. Patients can confront and defeat the imaginary critics they fear so intensely using the Feared Fantasy and the Acceptance Paradox. Almost any of the Cognitive Techniques can be useful, such as the Double Standard Technique, Thinking in Shades of Gray, Examine the Evidence, and the Survey Technique. Visual Imaging Techniques, like Cognitive Hypnosis, and Cognitive Exposure Techniques, like Cognitive Flooding and Image Substitution, can help the patient restructure the frightening mental images that often accompany the anxiety. Motivational Techniques may also be useful. For example, patients can list the advantages and disadvantages of telling themselves, "I shouldn't be so anxious." How will this message help them, and how will it hurt them? They can also list the advantages and disadvantages of one of the SDBs, like basing their self-esteem on other people's approval, or believing that other people are intensely critical and judgmental. The Classical Exposure Techniques play an especially important role in
Chapter 26
961
the treatment of public speaking anxiety. Patients can give talks to groups of people in order to polish their public speaking skills and overcome their fears in the real world. They can enroll in a public speaking course at their local community college or join a group like Toastmasters, where they'll give frequent presentations and get tips about how to improve their delivery. Interpersonal Exposure Techniques, such as Self-Disclosure, may also play a key role in the treatment. Techniques for handling interpersonal conflict, such as the Five Secrets of Effective Communication, can be invaluable. Most individuals with public speaking anxiety are afraid that someone in the audience will ask a difficult or hostile question. It can be a great relief to discover how to quickly turn an adversary into an ally by using the Disarming Technique, Stroking and Inquiry. Hypochondriasis and Chronic Pain. The cognitive model of hypochondriasis is similar to the cognitive model of panic attacks. Patients catastrophize about some benign physical sensation, such as fatigue, a belly pain, a bruise, tightness in the chest, or dizziness, thinking that they're on the verge of death. For example, they may conclude that their headache results from a brain tumor, or that the tightness in their throat indicates throat cancer. Then they go from doctor to doctor in search of a medical diagnosis and treatment, but no doctor can identify any illness that could explain their symptoms. Response Prevention will be important because the patient will have to agree to stop going to doctors for every little ache or pain. The Hidden Emotion Technique will often be crucial as well. People with unexplained aches and pains
Chapter 26
962
are frequently avoiding personal problems or painful feelings, such as a marital conflict, a problem at work, or unexpressed grief. Once you've exposed the hidden problem to the light of day, and the patient deals with it, the somatic complaints will often disappear. Agenda Setting will be especially important. What's the patient looking for? Some patients will insist on a medical diagnosis and treatment, and reject any type of psychotherapy. If patients are looking for a magical treatment directed at the pain itself, and are unwilling to focus on the problems in their lives, then any psychological approach will meet with stiff resistance. Similarly, if patients are simply trying to get narcotic medications or support for disability claims or lawsuits, then all bets are off. In this case, I don't accept the patient for treatment, since that would create a conflict of interest. Relationship Problems Relationship problems are more difficult to treat than individual mood problems like depression or anxiety. That's because so many people who are embroiled in conflict have an overpowering urge to hang on to their anger. They may feel morally superior and totally convinced that they're the innocent victims of the other person's badness. They're often more interested in retaliation or "justice" than in intimacy or reconciliation. That's why I always start out with Interpersonal Decision-Making and the Relationship Cost-Benefit Analysis. If the patient doesn't really want a better relationship with the other person, or feels reluctant to give up the idea that it's the other person's fault, then I wouldn't proceed with any type of interpersonal
Chapter 26
963
therapy. In this case, my unwillingness to try to "help" them is the therapeutic intervention. If you're struggling to treat someone with a troubled relationship, and you sense that you may be stuck, ask yourself these questions: Does the patient really want to improve this relationship? You may want to help the patient develop a more rewarding relationship, but the patient may have a different agenda. He may complain about his wife, brother, or boss, but may not be looking for help. He may simply want you to agree that the other person really is a loser. Are you trying to help a patient who insists that the other person is to blame? To my way of thinking, this is like trying to make a stone float! Before you can embark on any type of interpersonal intervention, patients will have to agree to stop blaming the other person and concentrate on changing themselves. If patients are willing to examine their own role in the conflict, the Revise Your Communication Style form and the Five Secrets of Effective Communication can help them develop far more satisfying relationships. These techniques may be too complex and threatening for most troubled couples you're treating in conjoint therapy, but the One-Minute Drill can be very useful if both partners are highly motivated and committed to developing a more loving relationship. The Cognitive Techniques have only limited use in the treatment of anger and interpersonal conflict, but can help patients who find disapproval very threatening. It may be practically impossible for them to use the Five Secrets of
Chapter 26
964
Effective Communication because they bombard themselves with distracting, self-blaming messages every time their partner criticizes them. These thoughts create such strong feelings of worthlessness and shame that some patients can't even grasp what the other person said to them. Then they get defensive or respond inappropriately, and the conflict escalates. Cognitive Techniques can help these patients develop greater self-esteem, so they can tolerate the pain that's inevitably involved in getting close to others. The Interpersonal Downward Arrow Technique can help you identify the Self-Defeating Beliefs that trigger the patient's relationship problems. This will help the patient see why they fall into certain kinds of interpersonal traps over and over again, and how they've been inadvertently triggering the very problems they've been complaining about. For example, overly submissive patients may feel the need to please everyone and avoid conflict at any cost. They may automatically blame themselves for all the problems in their relationships with other people. Of course, this behavior triggers the very criticism and rejection they fear the most. In contrast, angry individuals who have strong entitlement beliefs are demanding and blame everyone else for their problems. This provokes hostility and resistance, which reinforces their conviction that the problem is the other person's fault. Once again, they feel like victims and don't realize that they're really pulling the strings. Habits and Addictions This category includes bad habits like procrastination and overeating, as
Chapter 26
965
well as addictions such as drug and alcohol abuse. Agenda Setting and other Motivational Techniques will be the keys to effective treatment. Many patients with habits and addictions will also be struggling with depression, anxiety, and troubled relationships, so the Cognitive and Interpersonal Techniques can be useful as well. However, these techniques will usually play a more secondary role in the treatment of the addictive behavior itself. Many therapists fall into the trap of pushing help at someone who hasn't asked for it. This urge sometimes results from therapeutic naiveté or narcissism, but it can be hard to resist. The most common therapeutic error is to try to help a patient with a "problem" that feels more like a solution to the patient. For example, the alcohol abuse or procrastination may be working for the patient. Another common error is treating addictions with psycho-educational methods. When I was a psychiatric resident, I treated many depressed veterans who abused alcohol. I was instructed to advise them not to work as bartenders and to avoid hanging out in bars with their friends, because sooner or later, they'd be tempted to drink. These kinds of tips make logical sense, and might conceivably have some modest value, but for the most part, they're not effective. You can educate alcoholic or drug addicted patients all you want, but they'll still go out and get high. Psychoeducational methods won't cure addictions any more than reading a book on nutrition will cure someone who's struggling with the temptation to eat a tasty, freshly baked donut. When you're working with a habit or addiction, ask yourself:
Chapter 26
966
What, if anything, does this patient really want help with? Is the patient motivated to solve the problem? The Decision-Making Form will help the patient compare the advantages and disadvantages of the habit they're struggling with, such as drinking, along with the advantages and disadvantages of complete abstinence. Have I done a Paradoxical Cost-Benefit Analysis? Let's assume your patient asks for help with procrastination. You could do a double paradox. Ask him to list all the advantages of procrastination in the left-hand column of a CBA, and all the disadvantages of tackling the task in the right-hand column. You should easily be able to come up with tons of reasons to keep procrastinating, and many disadvantages of tackling the task. Then you could say, "Given these lists, I'm not sure why you'd want to change. The procrastination seems to be working well for you." Of course, you'll have to get inside his head and identify all the reasons why he really doesn't want to do the things he's been putting off. Otherwise it will just be a thinly disguised attempt to persuade him to change. Am I using the Devil's Advocate Technique? You could ask a patient struggling with a weight problem to list all the tempting thoughts she has when she passes her favorite bakery each morning on the way to work, such as, "Oh, a donut would taste so good! And I deserve it! One little bite couldn't hurt. Perhaps I could just walk inside and take a look at what they've got this morning." Then you can play the role of the Devil and verbalize all these thoughts to her, using the second person. You could say, "Why don't
Chapter 26
967
you just walk into the bakery and take a look? That certainly can't hurt. Mmmm. It smells so good!" She'll have to resist the temptations and try to defeat you. For example, she might say, "Those donuts do smell great, but I know that if I go inside, I'll end up pigging out on them. So I think I'll just keep walking instead. Tomorrow, I'll take a different route to work so I won't be tempted." Then you can try to tempt her again. You might say, "Oh, but a donut would taste so good right now. Just imagine sinking your teeth into it. Mmmm! It's even better than making love!" Once again, she'll have to fight back and defeat you in a convincing way. If she fails, do a role-reversal so you can model more effective responses. Continue in this way until she can quickly and convincingly defeat all of the tempting thoughts you throw at her. Once you’ve dealt with the problem of motivation, you can begin to use other techniques, starting with Agenda Setting. For example, if the patient wants to continue working on her urges to binge, you can encourage her to stop and fill out the DML whenever she feels tempted, before she gives in. After she describes the tempting situation and records her feelings, she can list all the tempting thoughts and identify the positive distortions in them. For example, when she tells herself, "I'll just have one little bite," she's denying a great deal of evidence to the contrary. How many times has she really taken just one little bite of a fresh, delicious donut and stopped at that? Then she can challenge her tempting thoughts in the right-hand column of the DML. If she still feels like giving
Chapter 26
968
in to the temptation to overeat, she's free to do so, but she has to complete the DML first. You can also use the Daily Mood Log to help patients overcome the feelings of guilt and self-loathing after they've slipped up. For example, when patients overeat, they may call themselves "fat pigs" and tell themselves that they'll never lose weight. However, there will be an important motivational issue to consider. The Agenda Setting question would be: "If I could show you how to reduce the guilt you feel after you binge, so you could stop beating up on yourself, would you be willing to do it?" Patients may balk because they think they deserve to suffer. They may also believe that the self-abuse will prevent future binging. You can ask how well this strategy has worked for them. Most of the time, the self-abuse and feelings of guilt and hopelessness simply trigger additional binging. After all, if the patient really is a "fat pig" who will "never" lose weight, then additional binging seems inevitable. In other words, these negative thoughts represent a form of selfhypnosis that will make change appear impossible. Non-Problems The term, "Non-Problem," may be misleading. What I really mean is, "nonpsychiatric problem," such as healthy grief. Obviously, if a patient has just experienced a tragic event, such as the loss of a loved one, you wouldn't want to tell them that they have a "non-problem!" Under these circumstances, feelings of grief are normal. Most people can cope with healthy feelings of sadness and loss on their own, but sometimes, these feelings get all bottled up.
Chapter 26
969
I once treated a woman named Beryl who'd been depressed for six weeks, ever since her oldest daughter had gone away to college. The feelings of depression surprised her, because she'd always been an “up” person and had never felt depressed about anything. She emphasized what a wonderful relationship she had with both of her daughters. They'd always been very loving, and she'd never had any problems with either of them. She proudly told me that when they were growing up, she'd coached several of their athletic teams. Beryl said that her relationship with her daughters was much like her mother’s relationship with her and her sister. She said her mother was a very positive, loving person, and had also coached their teams when they were growing up. Beryl became quiet when she mentioned her mother, so I asked her to tell me a bit more. What thoughts and memories came to mind? She said she was thinking about a swim meet when she was 13. She could remember standing at the edge of the pool with the other girls, ready to dive into the water. She really wanted to win and make her mother proud. Her mother was standing at the far end of the pool, monitoring the event. When the gun sounded, Beryl dove in and starting swimming with all her might. Suddenly, they stopped the race and told all the girls to get out of the pool. As she pulled herself out of the water, she saw people crowded around the spot where her mother had been standing. She could see her mother lying on the ground, and rushed toward her, but they pulled her away. Her mother gasped, “Somebody call for a Priest!” Beryl hung her head and softly said, “That’s the last thing I ever heard my
Chapter 26
970
mother say.” Apparently, her mother had an undiagnosed abdominal aneurysm that suddenly burst, and she bled to death internally at the edge of the pool. Beryl looked devastated, and I told her that I could understand how she might still be feeling sad and vulnerable about the sudden loss of someone she'd loved so much, and this might even explain why she'd reacted so strongly to the separation from her daughter. I said that her grief at losing her mother must have been enormous. She said that she actually hadn't grieved her mother's death at all, or even cried at the funeral. She explained that her father was a loving but highly disciplined man, and told Beryl and her sister that they should try to be strong. He said, "Your mother wouldn't want you to cry." So up to this very day, she still hadn't cried about her mother's death, or even talked to anyone about it, including her husband and daughters. She seemed to be hanging on and trying not to cry, so I encouraged her to let the feelings out. She broke down and sobbed for several minutes. Then I told her that she'd just done something very positive, and that it was healthy and necessary to grieve. I said that she could allow herself to cry at home as well, and might even want to visit her mother’s grave so she could talk to her and say goodbye. Beryl returned for her second session two weeks later. She explained that she'd gone home and cried about her mother for several hours following our session. That evening, she told her husband and daughters about what had happened, and even cried herself to sleep that night. She said that when she
Chapter 26
971
woke up the next morning, she realized that her depression about her daughter had lifted, and she was suddenly back to her normal, happy self again. She said that she'd felt good ever since and thought she was ready to terminate therapy. Beryl's grief and sadness were healthy. She wasn't clinically depressed, and she didn’t need any medications or fancy therapy to make her negative feelings go away. All she needed was a little encouragement, and the chance to express the feelings of grief. We don't need to treat healthy negative emotions. Sadness without distortion is actually a positive thing, because it shows that we love and that we're actively involved in life and committed to other people. Sadness and grieving can be a spiritual experience. In a case like Beryl's, the real problem was not the grief, but the failure to grieve. However, it's not always quite so straightforward. In some cases, feelings of depression, guilt, anxiety or anger contaminate healthy grief and prevent the patient from working through the loss and letting go. You've seen several examples of this already. You may recall Eva, the woman with ovarian cancer who felt guilty and worthless because she thought she was letting her family down, and Judy, the woman with terminal lung cancer who felt worthless because she believed she was no longer contributing to her family or society. If you help the patient fill out a Daily Mood Log, you'll usually see all the familiar distortions in their negative thoughts, such as All-or-Nothing Thinking, Emotional Reasoning, hidden Should Statements, and Self-Blame. Most of the time, people who are facing catastrophes can challenge their distorted thoughts
Chapter 26
972
quickly because they don't have long psychiatric histories and they're not motivated to be depressed or excessively angry about the situation they're confronting. Any of the CBT techniques, like the Straightforward Technique, the Double Standard Technique, or the Cost-Benefit Analysis, can be remarkably helpful. In many cases, a session or two of skillful CBT will be sufficient. The goal is not to make all the negative feelings disappear, but to help patients modify the distorted perceptions and Self-Defeating Beliefs that rob them of hope and self-esteem. Paradoxically, patients with problems that seem the most overwhelming will often provide you with some of your most rewarding and meaningful therapeutic experiences. Some experts claim that there are certain "stages" of grief that everyone must work through sequentially. For example, in her 1969 book, On Death and Dying, Elisabeth Kubler-Ross, M.D. described the five stages of grief: denial, anger, bargaining, depression, and acceptance. While there may be some truth in this theory, I'm not in favor of such formulaic descriptions of human experience, since we all react to things so differently. Our thoughts and feelings about any event will be unique. I recently spoke with a Clinical Social Worker who works with dying patients and their families in a hospice setting. He said he'd never once seen a patient who'd gone through Kubler-Ross' five stages of grief! But if the patient is suffering and asking for help, you can offer a great deal if you simply stick to the basics. So far, we've focused on how to select methods based on the distortions
Chapter 26
973
in the patient's negative thoughts or the type of problem the patient wants help with. You can also select methods based on the patient's personality or interpersonal style. Cooperative, motivated patients will usually respond to straightforward approaches, but angry, oppositional individuals will require a much greater emphasis on motivational and paradoxical techniques. Whenever you sense opposition or resistance, respond with Empathy. Then think about techniques like Agenda Setting, the Paradoxical CBA, or the Devil's Advocate Technique. At the start of an inpatient CBT group in Philadelphia, a man named Ricky defiantly announced that the nurses had sent him to my group for some "anger management." Ricky explained that he was a loan officer at a bank, and often had to cater to obnoxious customers who demanded special treatment and didn't listen to him. He said he was tired of always having to be Mr. Nice Guy and had decided that he wasn't going to take it any more. That morning, he'd reached the end of his rope. He picked up one of his most irritating customers and slammed him against the wall. The security guards pinned Ricky down after a scuffle and called the police. The police put him in handcuffs and brought him to our emergency room, where he was hospitalized on the locked unit with a working diagnosis of Manic-Depressive Disorder in the manic phase. I realized that Ricky was still in an angry, defiant mood, and knew that if I tried to help him "manage" his anger, I'd run into a wall of resistance. Instead, I pointed out that anger was sometimes justified, and asked how many of the
Chapter 26
974
group members got ticked off at people from time to time. Every hand went up. I said that perhaps we should examine the advantages and disadvantages of Ricky's anger instead of trying to control it. I drew a line down the middle of my flip chart and labeled the two columns "Advantages" and "Disadvantages." I asked Ricky if he could think of any advantages of his angry outburst. He said, "I showed that I wasn't going to put up with any more bullshit." I said that that this sounded like a strong advantage, and wrote, "No more putting up with bullshit," in the advantages column. I said that I sometimes had to put up with whiney bullshit, too, and often had the fantasy of throwing someone against the wall instead of having to act polite. I added that it must have been incredibly gratifying. Ricky enthusiastically agreed that it was tremendously satisfying. The group began to suggest lots of additional advantages, such as: I can feel morally superior. I can feel powerful. Truth is on my side. My anger shows that I'm real, and that I refuse to act like a phony. I shouldn't have to be so nice all the time. People will know that they can't push me around any more. The customer got what he deserved. Then I turned to Ricky and said, "You know, we have to end the group shortly, and we haven't even gotten to the disadvantages yet. However, there seem to be an awful lot of advantages, and they're all pretty compelling. It isn't at
Chapter 26
975
all clear to me why you'd want to give up your anger, or why we should try to 'manage' it." Ricky said that it was a huge relief that someone finally understood where he was coming from. Since it was time to end the group, I asked the patients to fill out the Brief Mood Survey again. I was surprised to see that Ricky's anger score had fallen from 20 at the start of the group, indicating the most intense anger, to 0, indicating no anger at all. I told him that I was puzzled, since we'd just agreed that he should hang on to his anger. He said he was also confused, and didn't know why his anger had suddenly disappeared. What happened? At the start of the group, Ricky probably felt frustrated, embarrassed and scapegoated. He may have felt somewhat ashamed as well. He was ready to fight and defend his territory. When I acknowledged that he had good reasons to be angry, he didn't feel the need to defend his anger any more. He suddenly felt accepted and connected to other people. In contrast, if I'd tried to show him how to "manage" his anger, he would have gotten even more ticked off and put up a wall. Obviously, Ricky will need much more than a single group therapy session, but we did accomplish something important. Ricky began to see me as his ally. This allowed him to ask for help without losing face, so we could work together collaboratively without having to do battle. I'm hopeful that the tables on pages 941 and 942 will be helpful in your clinical work, and perhaps in research as well. If we can learn more about the techniques that are effective for different kinds of problems, our field can
Chapter 26
976
advance more rapidly. However, I hope you won't view these guidelines as a set of rules you should follow religiously. Good clinical work is far more spontaneous and intuitive than merely picking methods off a table. You have to follow where the patient leads you, and that will always be somewhat unpredictable. Remember to stick to the basics! Don't rush in with techniques the minute you spot a distortion in the patient's negative thoughts, or after the patient describes a problem, such as a marital conflict. Instead, start with empathy and work from there. Without empathy and a strong therapeutic agenda, no technique is likely to be effective. I recently saw a television documentary about a man named Davie who was a hoarder. He said that he simply couldn't resist combing through trash bins looking for "treasures," like defunct vacuum cleaners, cracked plastic ice trays, and old backpacks with broken straps. Any time he drove past a garbage dump or noticed junk that people had left on the sidewalk for the trash collectors to pick up, he'd stop and collect more "prizes." He was driving his wife up the wall, because their house was littered with junk and their garage was filled all the way to the ceiling. Davie was spending thousands of dollars a year renting space to store all the junk he'd accumulated. Even their yard was littered with his many prizes, and the landlord had issued an ultimatum—get rid of it or you'll be evicted. Everyone was trying to "help" Davie, including his wife, his therapist, the television host, and the guest expert who commented on his problem. The television host would say, "Davie, why don't you just throw all these things away and be done with it?" Davie would smile politely and reply, "I just can't!"
Chapter 26
977
Davie's therapist encouraged him to slow down, focus on each item he was pulling from the trash, and ask himself questions like, "Do I really need this? When will I need it? What will I use it for? Does it really work? Is it broken beyond repair?" These questions were supposed to help him give up his compulsive hoarding, little by little. You could think of this technique as a combination of the Socratic Method and Response Prevention. Both the therapist and the guest expert touted it as a powerful new method for treating OCD. In one key scene, Davie spots an enticing pile of trash on the sidewalk. He's been instructed to drive past the pile without stopping so he can get used to tolerating his hoarding urges without giving in to them. But instead, he parks and starts stuffing things into his station wagon with great gusto. Meanwhile, his therapist is traipsing around after him, trying to persuade him to stop and encouraging him to ask himself questions about whether each item has any real value to him. The questions seem to be rolling off Davie like water off a duck's back. As Davie is loading a broken chair into his station wagon, the TV host asks him how he's feeling. Davie smiles and says he's feeling absolutely euphoric, since he's starting to "get into the zone." As you might imagine, at the follow-up several months later, the therapy still hadn't taken hold. In fact, Davie's wife had moved out and filed for divorce, but he was still hoarding with great enthusiasm. What went wrong? To my way of thinking, all the experts were making the same error—they didn't have a therapeutic agenda with Davie. In fact, Davie clearly loved his habit, and had no intention of giving it up. When people
Chapter 26
978
encouraged him to stop, he'd say, "I can't," but what he really meant was, "I don't want to." He wasn't the victim of mysterious forces beyond his control. His compulsive hoarding was his greatest source of pleasure and excitement in life. From his perspective, there was no problem! This is the exact error I cautioned you about a moment ago. Davie had OCD, so his therapist jumped in with the latest techniques to try to fix him—a strategy that's nearly always doomed to failure. Now that you have a feeling for how to choose methods, we'll look at some real-life cases, and I'll put you in the role of the therapist so you can see how the treatment might work for patients suffering from a variety of problems.
27*
Comorbid Depression and Anxiety—The Student Who Was Afraid of Being Average
Dr. Anthony Mascola, one of the psychiatric residents I supervise at Stanford, recently treated a physics graduate student named Noah who was suffering from anxiety and depression. Although Noah was doing stellar work and was ranked near the top of his class at the University of California at Berkeley, he woke up every morning in a state of despair because he told himself: I can't figure out anything! I'm so dumb and incapable. Without my achievements, I'd just be average. There's really nothing special about me. Pretty soon, everybody will find out that I'm defective. Noah's constant self-criticisms were robbing him of any real pleasure or satisfaction in life. No matter how much he accomplished, he told himself that it wasn't good enough and that he should be doing better. During a session I * Copyright
2004 by David D. Burns, M.D.
Chapter 27
980
supervised, Noah described his problems like this: "During my first year of graduate work, I struggled academically and wasn't all that happy. Now I'm doing really well, but I'm still unhappy. I wake up every morning with a sense of doom. I tell myself that I won't ever accomplish anything worthwhile. I feel like I must be an awful, terrible person. Sometimes I think I should just pack it in. By evening, I usually feel better, but in the morning, it seems like my whole world is about to fall apart. I get so anxious that I feel short of breath. "I've always based my self-esteem on my achievements, and I've gotten lots of praise for my academic work. But I've never felt like I had any intrinsic sense of self-worth. Even when things go really well, I can't seem to give myself any credit." For example, Noah had recently submitted a paper to the top journal in his field, and it was accepted for publication. Instead of feeling excited, he felt panicky. He was certain that everyone who read the paper would see all the loopholes in his thinking and realize what a fraud he was. Noah told us that he'd struggled with feelings of insecurity for as long as he could remember. When he was a boy, his parents had gotten divorced. Noah shut down emotionally and his personality changed. He became so preoccupied with his studies that he lost interest in his friends and stopped playing with the other children in the neighborhood. His mother was concerned that he was trying to bring his father back by doing really well in school, so she sent him to a counselor so he could try to work through his feelings of loss and anger. Over the years, he did extremely well in school, but continued to struggle with intense
Chapter 27
981
feelings of anxiety and self-doubt. In Chapter 19, you learned about the five steps of the Daily Mood Log: Step 1. Upsetting Event. At the top of the Daily Mood Log on page 982, Noah described the Upsetting Event like this: "Getting out of bed this morning." Step 2. Emotions. Noah was feeling depressed, anxious, ashamed, inadequate, lonely, humiliated, discouraged, frustrated and angry. The high ratings indicate that all of these feelings were strong. Step 3. Negative Thoughts. Noah recorded four negative thoughts on his DML. He believed them all 100%. Step 4. Distortions. Noah's negative thoughts contained many distortions, including All-or-Nothing Thinking, Discounting the Positive, Mind-Reading, Fortune-Telling, and Emotional Reasoning, to name just a few. Step 5. Positive Thoughts. Before he can feel better, Noah will need to put the lie to the thoughts that are making him feel so miserable. Obviously, Step 5 is the most important, but the positive thoughts won't be effective unless they fulfill the necessary and sufficient conditions for emotional change. Do you remember what they are? Describe them here before you continue reading: The necessary condition:
The sufficient condition:
Chapter 27
982
Noah's Daily Mood Log* Upsetting Event: Getting out of bed this morning. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
90%
Embarrassed, foolish, humiliated, self-conscious
50%
Anxious, worried, panicky, nervous, frightened
90%
Hopeless, discouraged, pessimistic, despairing
90%
Guilty, remorseful, bad, ashamed
100%
Frustrated, stuck, thwarted, defeated
100%
Inferior, worthless, inadequate, defective, incompetent
75%
Angry, mad, resentful, annoyed, irritated, upset, furious
80%
Lonely, unloved, unwanted, rejected, alone, abandoned
85%
Other (describe)
Negative Thoughts
% Before
1.
I can't figure out anything!
100%
2.
I'm so dumb and incapable.
100%
3.
Without my achievements, I'd just be average. There's really nothing special about me.
100%
Pretty soon, everybody will find out that I'm defective.
100%
4.
* Copyright
% After
Distortions
1984 by David D. Burns, M.D. Revised 2003.
Positive Thoughts
% After
% Belief
Chapter 27
983 Noah's Daily Mood Log (cont'd)
Negative Thoughts
% Before
% After
Distortions
Positive Thoughts
% Belief
Checklist of Cognitive Distortions* 1. All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6. Magnification and Minimization. You blow things out of proportion or shrink them.
2. Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7. Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3. Mental Filter. You dwell on the negatives and ignore the positives.
8. Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4. Discounting the Positive. You insist that your positive qualities don't count.
9. Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5. Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
Chapter 27
984
Answer The positive thought must be 100% true—that's the necessary condition. In addition, it must put the lie to the negative thought—that's the sufficient condition. Noah said he wanted to work on his fourth negative thought, "Pretty soon, everybody will find out that I'm defective." How will we help him put the lie to this thought? I've put the thought in the middle of the Recovery Circle on page 985. Imagine that you're working with Noah. Select at least 15 techniques you could use to help him challenge it. You can review the one-page list of techniques on page 986 or the longer list with brief definitions on page 522. If a technique looks promising, simply write the name of that technique in one of the boxes surrounding the circle. Right now, you don't need to write an explanation of how each technique would work. All you need to do is make sure you have lots of different techniques on your Recovery Circle. When you're done, turn to page 989, and I'll share my thinking with you.
Chapter 27
985
Noah's Recovery Circle
16
15
1
14
2
13
3
12
Pretty soon, everybody will find out that I'm defective. 100%
11
4 5
10 6 9
8
7
Chapter 27
986
50 Ways to Untwist Your Thinking* Basic Techniques
Exposure Techniques
Role-Playing 19. Externalization of Voices
Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques
Philosophical / Spiritual 21. Acceptance Paradox
Compassion-Based
Visual Imaging
5. Double Standard Technique
Truth-Based 6. Examine the Evidence
8. Survey Technique 9. Reattribution
39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
7. Experimental Technique
Cognitive Exposure
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Motivational Techniques
Semantic 12. Semantic Method 13. Let's Define Terms
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
14. Be Specific
Quantitative
30. Devil's Advocate Technique
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Chapter 27
987
Noah's Recovery Circle Worry Breaks
Self-Monitoring
Survey Technique
Empathy
16
15
Agenda Setting
1
14 Self-Disclosure
Identify the Distortions
3
12
Thinking in Shades of Gray
2
13 Pretty soon, everybody will find out that I'm defective. 100%
11 Semantic Method
Straightforward Technique
4 5
10
Cost-Benefit Analysis
6 Let's Define Terms
9
8
7
Double Standard Technique
Individual Downward Arrow
Be Specific
Examine the Evidence
Chapter 27
988
Noah's Recovery Circle (cont'd)
Hidden Emotion Technique
32
31
17
30
Shame-Attacking Exercises
18
29
Pleasure Predicting Sheet
19
28
Pretty soon, everybody will find out that I'm defective. 100%
27
Acceptance Paradox
20 21
26
Externalization of Voices
22 25
24
Memory Rescripting
Feared Fantasy
23 Five Secrets
Cognitive Flooding
Chapter 27
989
Answer You can see my Recovery Circle on pages 987 – 988. I always list the four Basic Techniques first. After that, the techniques you select are up to you. Let's review how the techniques on Noah's Recovery Circle might work. Empathy When Noah tries to tell his family or fiancé how inadequate and anxious he feels, they try to cheer him up and encourage him to think about himself more positively. That never works. Noah ends up feeling frustrated and lonely, because it seems like no one ever listens or allows him to be human. Before Noah will let us show him how to change, he'll need the chance to express his feelings and feel accepted, without any attempt on our part to straighten him out or "help" him. The moment he feels accepted, he'll be far more open to the possibility of change. Agenda Setting Would Noah be willing to give up his depression, anxiety and constant self-criticisms if we could show him how? See if you can list a few reasons why Noah may be reluctant to give up his negative thoughts and feelings: 1.
2.
3.
Chapter 27
4.
5.
990
Chapter 27
991
Answer Here are some possibilities: Although Noah is miserable, he may believe that his constant worrying keeps him sharp and accounts for his tremendous academic success. This is a romantic notion, since so many famous artists and musicians were tortured souls who struggled with depression. But Noah has never considered the possibility that he's accomplished as much as he has in spite of his selfabuse, and not because of it. He may believe that his constant worrying protects him and keeps him safe. Noah admitted that he was afraid he might be "blindsided" by life if he let down his guard and relaxed. He may criticize himself as a way of keeping his expectations low and protecting himself from disappointment. He may believe that people who achieve a great deal really are superior human beings, and that without his accomplishments, he'd be a nothing. His scrupulousness and constant worrying may feel like an important part of his identity. There's a kind of moral integrity in Noah's self-criticisms because he constantly searches for the flaws in his work. At the same time, there's a kind of grandiosity in his suffering, because he thinks he's supposed to achieve perfection—something no scientist could ever do. Noah agreed that some of these ideas rang true. To be sure we were on the same page, I asked him this question: "Noah, imagine that there was a magic
Chapter 27
992
button on the table, and if you pushed it, all your anxiety and depression would vanish. You'd suddenly be on cloud nine. Would you push the button?" Noah said that he wouldn't push the button because it sounded irresponsible, and he was afraid he'd lose all his motivation. If you were his therapist, what would you say next? Please put your answer below:
Chapter 27
993
Answer There's no one correct answer, but empathy would be indicated. Encourage him to express his misgivings, and find truth in what he's saying. Then you can renegotiate the therapeutic agenda. Is there a way the two of you could work together in spite of his fears? Noah feels 90% anxious. But how much anxiety and self-doubt does he need in order to do outstanding work? Would 50% be enough? Or 10%? Once you agree on a reasonable figure, you could work together to reduce his feelings of anxiety and depression to that level. Of course, once he starts to improve, his perceptions may change as well, and he might decide it would be okay to reduce his anxiety all the way to 0%. I told Noah that when I was a young man, I also agonized and worried constantly that my research wasn't good enough, and I worked my fingers to the bone. I even felt like a martyr, and was proud of my perfectionistic tendencies. Later on, I discovered that I nearly always did my most creative work when I was feeling happy and relaxed, and not trying so hard. Identify the Distortions Review the Checklist of Cognitive Distortions at the bottom of the DML on page 983 and see how many distortions you can find in Noah's negative thought, "Pretty soon, everybody will find out that I'm defective."
Chapter 27
994
When you've checked off all the distortions that apply, you can review my analysis on the next page. Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 27
995
Answer Noah and I found all ten distortions in his thoughts. This is common. Distortion
Yes
Explanation
1. All-or-Nothing Thinking
Noah thinks about his achievements in a black-and-white way. If his work is not utterly spectacular, he thinks it's no good at all.
2. Overgeneralization
He generalizes from his performance to his self. If he fails at any task, he feels like he's a failure.
3. Mental Filter
Noah ruminates about all his shortcomings, and ignores his many good qualities.
4. Discounting the Positive
He discounts his accomplishments and believes that he should be smarter and better than he is.
5. Jumping to Conclusions
He assumes that other people will be just as judgmental and perfectionistic as he is (Mind-Reading), and predicts that he'll be criticized and embarrassed when his paper is published (FortuneTelling).
Mind-Reading Fortune-Telling 6. Magnification and Minimization
Noah magnifies all his flaws and shrinks the importance of his accomplishments.
7. Emotional Reasoning
He feels defective, so he assumes that he really is.
8. Should Statements
Noah believes that he should always strive for perfection and should never fail or make mistakes.
9. Labeling
He labels himself as "defective."
10. Blame Self-Blame Other-Blame
Noah constantly criticizes himself and rips himself to shreds.
A thought that's so distorted could hardly be 100% true! This insight might not provide Noah with emotional relief, but it may help him begin to challenge the validity of the negative thought on an intellectual level. Other techniques will be necessary to create real emotional change. Straightforward Technique
Chapter 27
996
You may recall that this technique is rarely curative, but it will show you why the patient is stuck. I asked Noah if he could think of a way to talk back to his negative thought. He came up with this: "I could tell myself that people will think my work is actually pretty good." I told Noah to write this in the Positive Thoughts column and indicate how strongly he believed it. He only believed it 75%. Then I asked him to estimate how strongly he now believed the negative thought. He said he believed it about 90%. This modest reduction is not terribly meaningful. Do you know why the positive thought didn't work? It's because it failed to fulfill the necessary and sufficient conditions for emotional change. Noah is telling himself that people are going to think that his work is "pretty good," but he doesn't believe this. He's really afraid that his colleagues will be judgmental and rejecting when they read his paper. In addition, he's not aiming for "pretty good" work. Noah believes he has to accomplish something phenomenal in order to land the kind of prestigious academic position he's been dreaming about. Cost-Benefit Analysis (CBA) Instead of focusing on whether or not the negative thought is true, Noah can list all the advantages and disadvantages of believing it. How will this thought help him, and how will it hurt him? What are the costs, and what are the benefits, of thinking this way? After Noah lists all the advantages and disadvantages on a CBA form, he can weigh them against each other on a 100-point scale, and put two numbers that reflect his ratings in the circles at the bottom. If Noah decides that the
Chapter 27
997
advantages outweigh the disadvantages, we can respond paradoxically and ask why he'd want to change this thought, given the fact that it seems to be helping him. But if he decides that the thought is damaging him more than it's helping him, it may soften his resistance to giving it up. You can see Noah's completed CBA on page 999. His ratings indicate that the disadvantages of the negative thought slightly outweigh the advantages. Of course, we'll have to go further. He'll have to put the lie to the negative thought before he experiences any emotional relief. Double Standard Technique You could ask Noah to imagine that he was talking to a dear friend who was exactly like him. His friend is also studying physics at a top university, is ranked high in his class, and has recently had a paper accepted for publication in a prestigious journal. What would he say to his friend? Would he say, "Oh, you're so dumb. When your paper's published, everyone will see how incompetent you really are. You'll never get a decent job"? Why or why not? How would he talk to his friend? Would he be willing to talk to himself in the same compassionate way? Individual Downward Arrow Technique Ask Noah to draw a downward arrow under negative thought #4 on his Daily Mood Log. Then you can say something like this: "Let's assume that everyone does find out that you're defective. Why would that be upsetting to you? What would that mean to you?" A new negative thought will pop into his mind. Ask him to write it down
Chapter 27
998
under the arrow and draw a new arrow underneath it. If you repeat this process several times, you'll generate a chain of negative thoughts, as you can see in the example below. The bottom of the barrel will usually be a thought like, "Then life would not be worth living," or "Then I'd be worthless." When you and Noah review the chain of negative thoughts you generated, along with the list of Common Self-Defeating Beliefs (SDBs) on page 1080, you can pinpoint his SDBs, such as Perfectionism, Perceived Perfectionism, the Achievement Addiction, the Approval Addiction, the Brushfire Fallacy, Magical Thinking, and others.
4.
Pretty soon, everybody will find out that I'm defective.
5.
Then I'll never get a top academic job, and I'll have to settle for a position at a 3rd or 4th rate school.
6.
That would mean I was a failure.
7.
Then life would be meaningless, and I'd be miserable forever.
"Why would that be upsetting to you? What would that mean to you?"
Chapter 27
999
Noah's Cost-Benefit Analysis* List the thought or feeling you want to change: "Pretty soon, everybody will find out that I'm defective." Advantages of Believing This
Disadvantages of Believing This
1. This thought keeps me on my toes.
1. This thought makes me miserable.
2. It motivates me to do the very best work I can.
2. It's hard to relate to people, especially people who might judge my work, because I'm constantly afraid of being "found out."
3. It makes me seem special, as if I'm the center of attention. 4. It keeps me from being disappointed. 5. I feel like I'm being honest with myself. 6. I can feel sorry for myself and indulge in self-pity. 7. It gives me an excuse to avoid other people.
3. I secretly feel angry and resentful because people seem so judgmental. 4. It's hard to handle criticism, because I feel so threatened. My self-esteem is always on the line. 5. Nothing I do ever seems good enough. 6. It makes me feel like a fraud. 7. I often feel lonely, inadequate, inferior and ashamed. 8. I have no real self-esteem. I always have to earn it by doing something fantastic or impressing people. But that doesn't even work, because I never really feel worthwhile. 9. I don't ever get to enjoy the fruits of my labor. 10. The thought may not be valid.
40
* Copyright
60
1984 by David D. Burns, M.D.
Chapter 27
1000
Identifying Noah's SDBs will provide you with a deeper understanding of the problem and a blueprint for the therapy. When Noah modifies these beliefs and develops a more robust value system, he'll not only feel better in the hereand-now, but he'll be far less vulnerable to bouts of depression and anxiety in the future. Examine the Evidence This is a Truth-Based Technique. You could ask Noah how he came to the conclusion that he's dumb and incapable, or that people are going to look down on him because he isn't smart enough, or because there are flaws in his thinking. You can ask these kinds of questions: What's the evidence for these beliefs? Are they valid? Who, exactly, will be looking down on you? What's happened when you've presented your work to colleagues in the past? Did they seem cordial and make helpful suggestions, or were they brutal and judgmental? If your work is so flawed, why was your paper accepted for publication in a prestigious journal that rejects more than 90% of the papers that are submitted? What kind of feedback have you received from the editor and reviewers? What do your supervisors say about the quality of your research and chances of landing an academic position following graduation? How have the students from your program done in previous years? Noah is a scientist, and he's used to thinking about ideas critically, so this
Chapter 27
1001
technique may appeal to him. Although on occasion we all run into people who are narcissistic and hypercritical, most of Noah's colleagues will probably treat him with respect and admiration, especially if he presents his work with humility, openness and enthusiasm. Be Specific We're all a mixture of strengths and weaknesses. Our suffering does not result from our flaws, but from the judgments we make about ourselves, and from the way we overgeneralize when we think about our shortcomings. When you examine the facts, things have a way of falling into a different perspective. You could say something like this to Noah: "Let's be specific. You claim that people will discover that you're defective. What, exactly, is so awful about you? What defects are you referring to?" Suppose he says, "My research could be improved." You could say, "I have no doubt about that. Can you spell out some ways your research could be improved? Do you need better measurements? A larger database? What, really, are we talking about?" Of course, scientists aren't perfect, and Noah's research undoubtedly has many flaws, but those flaws are not the cause of his suffering. Any real deficiencies in his research can easily be corrected. Noah's suffering results from the vague, absolutist judgments he's making. He's telling himself that he's no good, that he's defective, and that he should be better than he is. Better in what way? What specific defects are we talking about? Let's Define Terms
Chapter 27
1002
This technique may also help Noah with his tendency to overgeneralize and label himself. It's similar to Be Specific, but you approach the negative thoughts from a slightly different angle. You could say, "Noah, you tell yourself that you're 'defective,' 'dumb,' and 'incapable,' but I must admit that I don't know what you mean. What's your definition of someone who's defective? Is it someone who's defective in every way, or someone who has defects?" If he says "defective in every way," you could point out that this definition doesn't apply to anyone. The very notion of someone who's defective in every way is absurd. If he says, "someone who has defects," you could point out that this is true of everyone. We all have many defects. Michael Jordan is widely considered to be the greatest basketball player in history, and even he missed half of all his shots. You could use the same approach with any of the labels Noah uses. No matter how he defines a "defective person," his definition will always fall apart. Semantic Method Noah uses harsh, emotionally charged language when he thinks about himself. When you use the Semantic Method, you simply use kinder and gentler language when you think about your flaws and shortcomings. For example, instead of telling himself that people will find out that he's "defective," he could tell himself that people will discover that he's human. Instead of telling himself that he should be some kind of super-genius, like Einstein, he could tell himself that while it would be great to be that smart, he's quite creative and has his own gifts to share.
Chapter 27
1003
Thinking in Shades of Gray Noah looks at things in black-and-white categories. Either he's 100% successful or he's a complete loser. All-or-Nothing Thinking creates intense performance anxiety, and it's also incredibly unrealistic. There are very few things in the universe that can be accurately categorized in an all-or-nothing way. No one is perfectly beautiful or totally ugly. No one is absolutely brilliant or completely stupid. We're all somewhere in-between. When you use Thinking in Shades of Gray, you rate your characteristics on a sliding scale. None of Noah's characteristics could be rated at 100% or at 0%. He may be extremely bright in some areas, such as math and science, but below average in others. He could rate himself in a thousand different ways on a 0% – 100% scale. Then he could ask himself two questions: 1. How high would these ratings have to be for me to be a "worthwhile" human being? 2. How high would these ratings have to be for me to feel happy and fulfilled? Hopefully, he'll see that there is no answer to these questions, because they're inherently meaningless. The way we feel has nothing to do with how "great" or "average" we are on any rating scale, but from how we think about ourselves and our lives. I'm reminded about the story of the ancient Pharaoh who was the wealthiest human being who ever lived. He owned kingdoms. When he died, there was a great deal of excitement about his will. Who would inherit all the unimaginable riches he'd accumulated? The will consisted of tens of thousands
Chapter 27
1004
of papyrus pages. But when his heirs opened it, they were shocked to discover that every page was empty, except for a single sentence scrawled on the first page: "In all my life, I had only seven happy days." I'm also reminded about a story Dr. Aaron Beck once told during a CBT supervision group. One evening, he and his wife were listening to some live music at a café in Philadelphia. He noticed that the man sitting alone at the table next to them seemed to be in a state of elation. He applauded enthusiastically after every song and was enjoying himself greatly. During one of the breaks, Dr. Beck asked the man why he was feeling so happy. The man said he'd just received an incredible promotion at work, and he was beside himself with joy. Dr. Beck asked what kind of work he did, and what the promotion was. The man explained that he'd been working in a bakery. For the past 15 years, his job had been to bring the donuts from the kitchen to the front counter and arrange them on the shelves. But now, he was going to have the chance to wait on customers, and actually sell the donuts, an opportunity he'd always dreamed about. He said he felt like the luckiest man in Philadelphia. It dawned on Dr. Beck that the man was developmentally disabled, but he was loving every minute of his life. Self-Disclosure / Survey Technique Noah sometimes feels lonely, anxious and ashamed, but hides these feelings and tries to appear cool and collected. Instead, he could disclose these feelings to a few classmates or friends he trusts. He'll probably discover that
Chapter 27
1005
most of them struggle with feelings of insecurity at times. This may provide him with an emotional bridge to other people. Self-Monitoring Noah takes his negative thoughts very seriously and tends to get obsessed with them. Instead, he could simply count his negative thoughts on a wrist counter every day for several weeks. At the end of each day, he could record the total and reset the counter to zero. The negative thoughts often diminish or disappear during the third or fourth week of Self-Monitoring. Self-Monitoring may allow you to change your relationship with your thoughts. You learn to observe them, much like you might during meditation, so you can let go of them and focus on your life. Worry Breaks If Noah thinks his negative thoughts and compulsive worrying are helping him, he could schedule certain times each day to give in to them. During each Worry Break, he could dictate his negative thoughts into a tape recorder and try to make himself as anxious and miserable as possible. Then he could rewind the tape and listen to it. He might want to schedule one or more five-minute Worry Breaks each day. It might be a good idea for Noah to schedule one of his Worry Breaks first thing in the morning, since that's when his symptoms are the most intense. This would be a paradoxical intervention, since he'd surrender to the negative thoughts instead of struggling with them. Hidden Emotion Technique
Chapter 27
1006
Anxiety is often a smokescreen for another feeling or problem the patient is denying. Is something bugging Noah that he's sweeping under the rug? Is he upset about a problem at school or a conflict in his personal life? We could also ask whether Noah is as committed to his career path as he claims. He keeps insisting that he'll never make it as an academic when his record indicates he has loads of talent. Why is he so obsessed with failure? It could be a simple case of insecurity, but he may also be discovering that an academic career can be a stressful rat race. During my sophomore year at Amherst College, I roomed with a brilliant Iranian student named Farzam Arbab. Followed graduation, Farzam completed his Ph.D. in physics at the University of California at Berkeley. He did some impressive research on the angular distribution of pi particles at the Lawrence Radiation Laboratory, but eventually decided that a career in physics was not his thing. I was curious to find out what Farzam had done with his life, so I recently searched for his name online. I found more than 100 links to websites about him and his work. I discovered that he'd become a prominent leader in the Bahá'í Faith and had founded a "University for the Poor" in Colombia, South America. Later that very day, I mentioned his name to an officer at our bank who was also from Iran. She exclaimed, "Do you really know Farzam Arbab? He's world famous!" Clearly, in spite of his sophisticated training, Farzam was not committed to a research career. When he followed his heart, he found new avenues for his
Chapter 27
1007
enormous talent, creativity and commitment to people in need. Noah may feel exactly the same way, but it may be hard for him to admit it. His anxiety and constant preoccupation with failure could simply be his way of telling the world, "I'm not sure that an academic career is what I really want." Of course, this is just a hypothesis we can explore. Only Noah can tell us whether it rings true. Shame-Attacking Exercises Noah would probably be the first to agree that he's a bit stiff and obsessed with his work. He seems to have forgotten how to be playful and have fun. Although it might be a bit of a stretch, some Shame-Attacking Exercises might help him loosen up and break his emotional logjam. You will recall that when you do a Shame-Attacking Exercise, you intentionally do something foolish in public to get over your fears of looking foolish. If this idea appeals to Noah, the two of you could cook something up. For example, if he's got a terrible singing voice, he could walk around Berkeley dressed like a wandering minstrel and offer to entertain people with song. After each song, he could smile and hold out his hat for any contributions that might come his way. He may discover that the world doesn't come to an end, and may even find the experience liberating. He may also discover that other people like him even better when he allows himself to be a bit goofy. Because this technique may seem extreme or frightening to patients, I often describe a number of Shame-Attacking Exercises that I've done, and explain the rationale behind them. It's absolutely crucial that:
Chapter 27
1008
The patient doesn't think you're making fun of him or her. You're not encouraging the patient to do something inappropriate that will get him or her into trouble. The Shame-Attacking Exercise is reasonably tasteful and in good humor. The Shame-Attacking Exercise is not likely to backfire and trigger criticism or hostility from other people. Given these limitations, there's still plenty of room for good-natured, wacky behavior in this world. If the Shame-Attacking Exercise I've described seems too extreme, you can propose something simpler, like walking down the street singing hymns quietly. Once Noah is comfortable with that, he can begin to sing more enthusiastically, occasionally shouting, "Hallelujah!" Pleasure Predicting Sheet Noah has become so preoccupied with his work that he's like a horse with blinders on. He seems to have lost touch with the simple pleasures that most of us enjoy, and he thinks that he'll be doomed to a mediocre and meaningless existence unless he achieves an incredible level of success. But is this really true? To find out, he could schedule a series of activities with the potential for learning, personal growth, or pleasure in the first column of the Pleasure Predicting Sheet on page 1009. He can select a mixture of activities he can do by himself, like jogging, and activities he can do with other people, like going to a movie with a friend. Then he can predict how satisfying each activity will be on a scale from 0% – 100%.
Chapter 27
1009
Pleasure Predicting Sheet* Activity Schedule activities with the potential for pleasure, learning, or personal growth.
Companion Who do you plan to do this with? Schedule activities with friends and by yourself.
* Copyright
Satisfaction Predicted (0% – 100%) Record before you do each activity.
1980 by David D. Burns, MD.
Actual (0% – 100%) Record after you complete each activity.
Chapter 27
1010
After Noah completes each activity, he can record how satisfying it turned out to be. He may discover that some of life's most rewarding moments have nothing to do with achievement, but come from activities that might seem rather ordinary. Acceptance Paradox This is one of the most challenging but liberating of all the CBT techniques. Patients learn to accept their humanness, warts and all, with a sense of humor and inner peace. The Acceptance Paradox is the ultimate antidote to perfectionism and feelings of inadequacy. It's nearly always paired with a roleplaying technique, such as the Externalization of Voices or Feared Fantasy. Externalization of Voices Once Noah has put the lie to his negative thoughts, we can hold his feet to the fire to see if he's really gotten it at the gut level. You could play the role of his negative thoughts, and attack him in the same way that he attacks himself, using the second-person, "You." He will have to respond to these attacks using the first-person, "I." He can use the Acceptance Paradox or the Self-Defense Paradigm. His goal will be to blow the negative thoughts out of the water. If he can't effectively refute the thoughts, you can do a role-reversal and model more effective responses. Remind him that even though it may seem like two people involved in a battle, the two of you are actually playing the negative and positive voices inside his own mind. Feared Fantasy Noah is afraid that other people will find out that he's "average" or
Chapter 27
1011
"defective" and reject him, but he's never had the chance to face these fears. The Feared Fantasy Technique will allow Noah to enter an imaginary, Alice-inWonderland nightmare world where his worst fears will come true. He'll meet a hostile stranger who will rip him to shreds and verbalize all the criticisms he fears the most. In this example, Noah will play the role of the Hostile Critic, and I'll play the role of Noah: Hostile Critic (played by Noah): Hi, Noah. I don't mean to hurt your feelings, but I've heard that you're a rather average fellow. Noah (played by David): You heard right. In fact, I have lots of traits that are way below average. But it's exciting to be average at a school like Berkeley because I get the chance to work with so many awesome people. Hostile Critic (played by Noah): It's great that you managed to get into such an outstanding graduate school, but I can't help but wonder if they were short on candidates the year you got in. Isn't it a shame that there's nothing special about you? Noah (played by David): To be honest, I haven't really thought about it. Does it seem shameful or shocking to you? Hostile Critic (played by Noah): Of course it's shameful! You'd be a total nothing without your meager academic accomplishments. Noah (played by David): If this is what it's like to be a "nothing," then I don't mind because I'm having such a great time here. It's almost like being in a kind of academic Disneyland. In fact, I think I'm happier than
Chapter 27
1012
I've ever been before. Hostile Critic (played by Noah): You sound delusional. Everyone knows that if you're only average, you're worthless. Maybe it's time to cash it in. Noah (played by David): I'm having way too much fun for that. But when you say I'm worthless, I'm not exactly sure what you mean. Remember, I'm only average, so you may have to spell it out for me. Hostile Critic (played by Noah): Boy, you sure are slow. It should be obvious, but I'll make it simple for you. If you're only average, you're not special. And when people find out that you're not special, no one will love or admire you. Then you'll be doomed to a life of mediocrity and desperation. How can you even carry on from day to day? Noah (played by David): Actually, I just decided to lower my standards, and that seemed to do the trick. Now I'm thrilled with my life, and almost everything seems special and exciting. I'm doing great in my studies, I'm second in my class, and I just got an article published in a superb journal. I think it's all pretty amazing. Hostile Critic (played by Noah): Amazing? You must be easily impressed. Get real. You'll never get a top academic position, because you're just not good enough. You're surrounded by geniuses who are vastly superior to you. You'll probably have to settle for teaching high school science to average students who couldn't care less. Noah (played by David): I'm hoping for a good university position, but it
Chapter 27
1013
could actually be fun to teach high school science. My high school science teacher made a tremendous impression on me, and was one of the most important figures in my life. In fact, that's why I decided to go into physics in the first place. I always remind myself that there are no dead ends in life if you have the right attitude. Even Einstein couldn't get a job in physics after he graduated. He had to work for years as a clerk in the patent office, because no physicist in Europe would hire him, even for free. But he didn't let that hold him back. He just kept believing in himself. Hostile Critic (played by Noah): You disgust me. You're obviously no Einstein! I'm going to tell everyone about what an average little nothing you are. Then everyone will despise you and you'll never get a job. Noah (played by David): To be honest, I don't think anybody really cares about how "special" or "average" you think I am. I've discovered that we're basically all in the same boat, and it was such a relief when I discovered that I didn't have to be special any more. I believe that I have a contribution to make, and I'm confident that I will get a good job. Of course, anything is possible so we'll have to wait and see. You know, I've got to get back to the lab now. I'm in the middle of a really neat experiment, and I can't wait to find out how it comes out! Catch you later. Of course, this Hostile Critic is none other than Noah himself. I'm showing him how he can use the Acceptance Paradox to defeat the relentless critic inside
Chapter 27
1014
his own brain that keeps saying, "You're not good enough, not good enough, not good enough! Soon people will find out about you, and you'll be doomed!" Once he sees that he can't get my goat, no matter what he says, we'll do a rolereversal so he can learn how to defeat the Hostile Critic as well. Five Secrets of Effective Communication Most graduate students would be thrilled to have a paper accepted by a prestigious journal. Getting published is your ticket into the world of academics, and it will be a boon when it comes time to interview for jobs. But Noah's anxiety and depression seemed to intensify when his paper was accepted. He's telling himself that he'll never get a top position because the experts will discover that his work is flawed. This would be a terrific problem to work on using the Five Secrets of Effective Communication. In the following example, Noah will play the role of a brilliant physicist who's read his paper and raises a number of questions about it. This will be a bit like the Feared Fantasy, but with one important difference. This time, the critic represents a real person, and not just a figment of Noah's imagination. I'll play Noah, and I'll respond to each criticism using the Disarming Technique, Thought and Feeling Empathy, Inquiry, "I Feel" Statements, and Stroking. I'll indicate which technique I'm using in parentheses following each sentence: Critical Physicist (played by Noah): Noah, I read your paper in the May issue of The Journal of Theoretical Physics. Noah (played by David): I'm thrilled to hear that, since I've been a great
Chapter 27
1015
admirer of your work for a long time. (IF; ST) In fact, we've often discussed your theories in our classes at Berkeley. (ST) What did you think of my paper? (IN) Critical Physicist (played by Noah): In all honesty, I thought there were some fatal flaws in your thinking, and I had some problems with your methodology as well. Noah (played by David): As a matter of fact, I've had the same concerns. (DT) I also thought there were some flaws in the theory, and I've suspected that the methods we're using in our lab aren't nearly as precise as they could be. (TE; DT) I'd love to hear more about your thinking. (IN; ST) What were the problems that you noticed in the theory, and what kinds of research instruments would you recommend? (IN; ST) This kind of response has an excellent chance of making the critical physicist feel admired and respected, and will probably open up a productive dialogue. In fact, he may even decide that Noah is just the young colleague he's been looking for to fill that vacancy on his research team. Of course, Noah will have to use these techniques skillfully, and his response will have to come from the heart. If the critic doesn't believe what Noah is saying, or if Noah fails to project genuine respect, the critic will label him as a phony. Noah's real enemy is not his flaws, but his belief that others will reject him if he's not perfect. The Buddhists say that our worst enemies are actually our greatest allies in disguise. If Noah likes this approach, and develops skill when role-playing with you
Chapter 27
1016
during sessions, I'd ask him to try it in real-life. He could solicit criticism from his supervisor, colleagues and professors, and practice responding with the Five Secrets of Effective Communication, especially the Disarming Technique and Stroking. This will allow him to develop a completely different style of relating to other people that has the potential to be far more collaborative and rewarding. This concept has been extremely helpful in my own work as well. At the start of all my two-day workshops, I tell the audience that there's an evaluation form at the back of their handout, and ask them to complete it and turn it in to me at the end of day one. I explain that they'll have the chance to rate the workshop and describe what they liked best and least about my presentation. I say that they'll probably find all kinds of loopholes in my thinking, and that I want them to share this feedback with me. I promise that the next morning, I'll read out loud the five worst things that people said about me, as well as the five things they liked the best about the program. The next day, I summarize the overall ratings and read their comments, starting with the five worst criticisms. I try to find truth in every criticism and express positive regard for the person who wrote it. Sometimes this is a bit embarrassing, because the negative comments are always valid! For some reason, everyone seems to giggle when I read the most horrible criticisms. This breaks the tension and creates an atmosphere of acceptance. Fortunately, there are always many heartwarming comments as well. I can't tell you how terrific this experience is. I can feel the group getting high when I read their comments, and it often sets the stage for a truly
Chapter 27
1017
remarkable second day of the workshop. This has been one of the most liberating discoveries of my life. Cognitive Flooding / Memory Rescripting We know that Noah's preoccupation with his studies intensified after his parents got divorced, and that he saw a counselor for a period of time. We might wonder whether he ever had the chance to express his feelings of loss, confusion and anger, or if he simply converted them into an obsession about his schoolwork so he wouldn't have to deal with the pain he was feeling. If so, those feelings may still be festering under the surface. Strong emotions sometimes bubble to the surface when patients intentionally focus on the painful memories they've been avoiding. You could ask Noah to close his eyes, relax, and let his mind wander back to the time of his parents' divorce. Tell him to describe the images and feelings that drift into his mind. If he becomes sad and tearful, you can encourage him to surrender to the feelings. You could ask if there were things he wanted to say to his father or mother that he never got the chance to say. Perhaps he wants to tell them how hurt, disappointed and lonely he felt when they got divorced, and how they let him down. He could even imagine that you were his father or mother, and he could say all the things that he never got the chance to say to them. He might tell his father that he needed more love and support, and felt abandoned when he moved away. He could also describe the things his father did that meant the
Chapter 27
1018
most to him, and what he needed more of. This approach works most effectively when the patient expresses the negative feelings in a loving way, rather than in a hostile manner. This technique might strike you as too touchy-feely, and it may not be effective for Noah. However, it does represent an entirely different approach that might allow him to release the feelings that have been buried and eating away at him for so many years. Once you start working with Noah, your understanding will evolve and you may begin to view his problems from a different perspective. This will lead to other techniques you didn't think of initially. Like most of the people we work with, Noah may be stuck for a while, and you may keep bumping up against a wall. But if you persist, he'll eventually experience a shift in his thoughts and feelings. Therapists at my workshops often ask how recovery usually occurs. Does one technique suddenly work when all the rest have failed? Or do the patient's beliefs change gradually when you come in from different angles? And if you'd tried the technique that eventually worked when you first started treating the patient, would it have worked right away, without having to try all the other techniques first? I've had many patients who didn't respond to more than 20 or 30 techniques. Their depression, anxiety and anger scores were almost identical from week to week. Then, we suddenly stumbled across a technique that worked, and they immediately experienced a dramatic change in the way they were thinking and feeling. This is a heady and gratifying experience, but you
Chapter 27
1019
have to keep the faith while you're waiting for it to happen. Sometimes, the negative thoughts change more gradually. Some of the techniques may help somewhat, but the patient can't completely let go of the thought or belief that's causing so much distress. You may feel like you're on the verge of a breakthrough, but you can't quite get across the River Jordan. Then you suddenly stumble across a technique that works and brings the patient the rest of the way home. When Noah finally puts the lie to his negative thoughts, you'll observe a profound change in the way he thinks and feels. He'll finally see how off base his thoughts were. Many patients have told me that they can't understand how they could have believed the negative thoughts that seemed so realistic and intimidating when they were feeling depressed just a few days earlier. Noah will probably discover that the truth is the exact opposite of what he's believed for so many years. He's been convinced that his perfectionism is the price he has to pay for superb work, and that something terrible will happen if he stops beating up on himself. But in fact, his constant misery and worrying have been holding him back and robbing him of energy, motivation, creativity and joy. Of course, Noah will have to do outstanding work if he wants to pursue a career in physics, but his compulsive perfectionism is a far cry from the healthy pursuit of excellence. There's no such thing as a perfect theory, experiment, or paper, and there never will be. In fact, science moves ahead the most rapidly when we disprove our theories. That's what leads to the really big discoveries in
Chapter 27
1020
any field. Noah has also believed that his colleagues expect him to be perfect and will reject him if he's not. This simply isn't true. In the long run, his interpersonal skills will be at least as important as his intellect. Obviously, he's got talent, but he'll experience the greatest success in his career if he learns how to listen and make other people feel important, rather than trying to impress them with his own accomplishments. I think about treatment as trying to find your way into a mansion. There are lots of doors and windows, but none of them are open. You knock on the front door, but no one answers. You try the side door, with the same result. You try to open a window, but it's locked shut. Eventually, you notice a door we hadn't seen at first. It opens wide and someone says, "Come on in! I've been expecting you."
28*
Borderline Personality Disorder—The Woman Who Thought She Deserved To Suffer Forever
Most therapists dread having to treat patients with Borderline Personality Disorder (BPD) because they can be so resistant, turbulent, and manipulative. They may fire up intense countertransference reactions in us. Over the years, I've treated many patients with this diagnosis. Approximately 15% of the patients we saw at my clinic in Philadelphia had possible or definite BPD at intake, along with many other Axis I and II diagnoses. Our research indicated that most of these patients recovered about as rapidly as patients without BPD (Burns & Nolen-Hoeksema, 1991; 1992). We treated these patients with same A-TEAM approach you're learning about in this book. Empathy and Agenda Setting will be especially important with these patients. I'm going to put you in the therapist role and guide your treatment of a 26 year-old married woman named Janice. Your intake evaluation indicates that * Copyright
2003 by David D. Burns, M.D.
Chapter 28
1022
Janice has probable Borderline Personality Disorder along with a major depressive episode. She's been struggling with feelings of guilt and self-loathing for seven years, ever since having an abortion when she was 19. In spite of her emotional problems, she's the loving mother of two children and is doing well in her career as an assistant marketing director for a pharmaceutical firm. When Janice was nine years old, an uncle molested her on several occasions. She feels tremendous anger and mistrust when she thinks about this experience, and feels bitter that her parents never discovered what was happening or helped her. In spite of this, Janice was able to overcome the shame and worthlessness she felt at that time by developing what she describes as an "aura" that protected her from danger. She felt reasonably happy until the time of her abortion, but has felt miserably depressed ever since, and has lost her "aura." Janice's Daily Mood Log appears on page 1024. As you can see, the Upsetting Event is simply, "Thinking about my abortion." She feels intensely depressed, anxious, guilty, ashamed, worthless, lonely, humiliated, hopeless, frustrated, and angry. One of her negative thoughts is, "I deserve to suffer forever because I killed my child." Janice believes this thought 100%, and it's been plaguing her ever since her abortion. She won't be able to overcome the intense shame and self-loathing she feels until she puts the lie to this thought. Clearly, that won't be easy. All her efforts to combat the thought have been ineffective. Her husband, parents and closest friends have tried to persuade her that she doesn't deserve to suffer, but their efforts have been
Chapter 28
1023
unsuccessful. In fact, every time they try to cheer her up, she feels worse. We'll have to come up with some new ways to help Janice find her way out of the emotional trap she's in. I've put Janice's negative thought in the middle of the Recovery Circle on page 1026. Review the list of 50 CBT techniques on page 1027 and put the name of one technique that might help Janice in each box around the circle. If you aren't sure about how a technique would work, you can refer to the table on page 522. When you're done, you can turn to page 1028.
Chapter 28
1024
Janice's Daily Mood Log* Upsetting Event: Thinking about my abortion. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
100%
Embarrassed, foolish, humiliated, self-conscious
100%
Anxious, worried, panicky, nervous, frightened
80%
Hopeless, discouraged, pessimistic, despairing
100%
Guilty, remorseful, bad, ashamed
100%
Frustrated, stuck, thwarted, defeated
80%
Inferior, worthless, inadequate, defective, incompetent
100%
Angry, mad, resentful, annoyed, irritated, upset, furious
100%
Lonely, unloved, unwanted, rejected, alone, abandoned
100%
Other
Negative Thoughts 1. I deserve to suffer forever because I killed my child.
% Before
% After
Distortions
100%
2. I shouldn't have had an abortion. 100%
3. I'm a worthless human being.
100%
4. I'll be depressed forever. 100%
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
Positive Thoughts
% After
% Belief
Chapter 28
1025
Janice's Daily Mood Log (cont'd) Negative Thoughts
% Before
% After
Distortions
Positive Thoughts
% Belief
Checklist of Cognitive Distortions* 1. All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6. Magnification and Minimization. You blow things out of proportion or shrink them.
2. Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7. Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3. Mental Filter. You dwell on the negatives and ignore the positives.
8. Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4. Discounting the Positive. You insist that your positive qualities don't count.
9. Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5. Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
Chapter 28
1026
Janice's Recovery Circle*
16
15
1
14
2
13
3
12
I deserve to suffer forever because I killed my child. 100%
11
4 5
10 6 9
* Copyright © 2004 by David D. Burns, M.D.
8
7
Chapter 28
1027
50 Ways to Untwist Your Thinking* Basic Techniques
Exposure Techniques
Role-Playing 19. Externalization of Voices
Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques
Philosophical / Spiritual 21. Acceptance Paradox
Compassion-Based
Visual Imaging
5. Double Standard Technique
Truth-Based 6. Examine the Evidence
8. Survey Technique 9. Reattribution
39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
7. Experimental Technique
Cognitive Exposure
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Motivational Techniques
Semantic 12. Semantic Method 13. Let's Define Terms
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
14. Be Specific
Quantitative
30. Devil's Advocate Technique
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Chapter 28
1028
Answer Have you completed the exercise? If you haven't, give it a try now, before you continue reading. It should only take about ten minutes. My Recovery Circles appear on pages 1029 – 1030. You'll see that I've listed the four basic techniques first: Empathy, Agenda Setting, Identify the Distortions, and the Straightforward Technique. These four techniques will be important in your work with every patient. Let's review how all the techniques on Janice's Recovery Circles might work. Empathy Imagine that Janice has just said, "I feel like I deserve to suffer forever because of the abortion. I feel like I murdered my baby." What would you say next? Put your response below, using the Five Secrets of Effective Communication. Put the names of the techniques you're using in parentheses after each sentence. You can use the following abbreviations: DT = Disarming Technique
IN = Inquiry
TE = Thought Empathy
IF = "I Feel" Statements
FE = Feeling Empathy
ST = Stroking
Please don't continue reading until you've written down your response to Janice:
Chapter 28
1029
Janice's Recovery Circle Survey Technique Let's Define Terms Semantic Method
Empathy
16
15
1
14 Socratic Method Externalization of Voices
Agenda Setting
2
13
3
12
I deserve to suffer forever because I killed my child. 100%
11 Acceptance Paradox
Identify the Distortions Straightforward Technique
4
Thinking in Shades of Gray
5
10 6 Negative Practice
9
8
7
Cost-Benefit Analysis
Double Standard Technique
Self-Monitoring
Time Projection
Chapter 28
1030
Janice's Recovery Circle (cont'd)
Reattribution
Examine the Evidence
17 18
Cognitive Flooding
19 I deserve to suffer forever because I killed my child. 100%
Memory Rescripting
20 21
Pleasure Predicting Sheet
22 Hidden Emotion
23 One-Minute Drill
Chapter 28
1031
Answer Many therapists would respond in a kindly way, along these lines: "Janice, I can see how much you're blaming yourself for the abortion, but I believe we can work together to help you overcome those feelings." Can you spot any errors in this response? First, there's no Feeling Empathy. Janice has been overwhelmed with feelings of intense self-loathing, guilt, and hopelessness ever since her abortion. She may also have unexpressed feelings of grief or anger about losing her baby. If you jump in and reassure her that you can "help" her, without acknowledging these feelings, Janice may feel like you're trivializing her suffering. In fact, this is the same error that her family and friends have been making when they try to reassure her. I've done this exercise in many psychotherapy workshops and in training seminars. Almost every therapist has failed to acknowledge any of Janice's feelings. Look at the response you wrote down. Did you acknowledge her feelings of guilt, worthless, and hopelessness? Most therapists fail to use Thought Empathy as well, and you can see this clearly in the response above. This therapist has not reflected Janice's words back to her. Janice has just said that she feels like she killed her baby. This harsh message is the key to her suffering. Yet, most therapists carefully edit these words out of their response. It's as if they're afraid of going into the dark with her. Perhaps her words sound too horrible, so we feel compelled to try to save her from herself.
Chapter 28
1032
The Disarming Technique is also missing. There's no acknowledgement of the fact that Janice feels like she really has killed her child, and believes that her suffering is justified. If you rush in and reassure her that you're going to help her, she may feel the need to resist because you haven't acknowledged her "truth." Notice that there's no Inquiry in the response above, either. Instead of inviting Janice to talk about her struggle and her feelings of despair, this therapist has given her the message that it's time to move on to the problem-solving mode. That way, he can keep her at a distance and maintain the familiar role of the "expert" who's helping the "patient." Instead, you could ask about her feelings. What's it like to be drowning in so much remorse and self-hatred? What are her thoughts about the abortion? How do those thoughts make her feel? There's also no "I Feel" Statement in this therapist's response. Most of us would feel shocked or saddened by what Janice has said. But most therapists do not acknowledge their own feelings. Instead, they try to come across as polished, helpful professionals. When you try to hide your feelings, you may end up sounding condescending or fake. In contrast, if you disclose your feelings skillfully and respectfully, you'll appear human. This can strengthen the therapeutic alliance. Finally, there's no Stroking. This therapist hasn't conveyed any genuine respect or concern for Janice. He could tell Janice that he feels sad about all the suffering she's been through and point out that her suffering shows that she won't take what happened lightly or let herself off the hook too easily.
Chapter 28
1033
Why do most therapists have so much trouble with this exercise? Why do we jump in and "help" when our patients need us to listen and support them? Are we more afraid of negative emotions than we realize? Here's one way you could respond to Janice: "Janice, I feel sad to hear how much you've been suffering. (IF; FE) You say that you feel like you murdered your child and that you deserve to suffer forever. (TE) I can imagine how devastated, hopeless and guilty you must feel. (FE) Can you tell me more about what this has been like for you? (IN)" This response gives Janice the opportunity to talk about an overwhelming experience that's casting a dark shadow on her life. We're opening the door instead of closing it. It's hard to know how long Janice will need to talk. Fifteen minutes of listening may be sufficient, or she may need a whole session or two. If you try to shortcut this process, you may slow the therapy down. She won't be able to let go and move forward until someone has accepted her as she is. Agenda Setting Agenda Setting is the second technique on my Recovery Circle. Of course, we used Agenda Setting earlier in the session, right before we filled out the Daily Mood Log. Now, we'll focus on motivation once again. Is Janice ready and willing to change, or is she going to resist our efforts to help her? Let's think about Outcome Resistance. Why might Janice be reluctant to recover? Put your ideas here. Try to come up with at least three potential
Chapter 28
1034
sources of resistance. Don't read ahead until you've written something down: 1.
2.
3.
Chapter 28
1035
Answer Many factors could be keeping Janice stuck, including: She may be convinced that her suffering is morally justified and necessary because she sees herself as a murderer. She may resist change because she believes that it would be morally wrong to experience joy and happiness again. This will probably be the most important source of resistance. Janice's depression keeps her baby alive and protects her from having to grieve her baby's death. She thinks about the baby every day. If she lets go of her depression, she may finally have to grieve and say goodbye to the child she lost. Her depression may protect her from having to face a problem that she's been avoiding. Maybe she's angry with her husband or parents. As long as she's depressed, she doesn't have to deal with the conflict. Her depression may give her an excuse to avoid sex and intimacy. The self-loathing may be painful but familiar. Janice may be afraid of what life would be like without her identity as a "bad person" or a "murderer." The problem makes Janice special. She may be caught up in a kind of addictive, narcissistic self-pity, because she's constantly focusing on how bad she is. She may relate to people through her depression. Friends and family constantly reassure her because she's so miserable, so she's always the center of attention. Janice judges herself with harsh, unreasonable standards, but she may
Chapter 28
1036
believe that her perfectionism and self-abuse will protect her from some future tragedy or mistake. Once you've explored all the reasons why Janice might not want to change, you can ask if she'd be willing to get better, given all the compelling reasons to maintain the status quo. In other words, we want Janice to persuade us to work with her, and not vice versa. Let's say that Janice tells you that she feels like she really does deserve to suffer. How will you deal with her resistance? What, specifically, will you say to her? Put your ideas here. When you're done, you can read my response on page 1037:
Chapter 28
1037
Answer You could say something along these lines: "Janice, I can understand the intense feelings of shame and worthlessness that you've struggled with since your abortion, and my heart goes out to you. I have many powerful tools that might help, and I'm eager to share them with you. But I'm reluctant to use them until I get the green light from you, and you feel ready to change. In other words, I want to know if you'd be willing to feel joy again, if I could show you how?" If she says she feels ready to change, you'll want to ask several additional questions along these lines: What will she bring to the table if you agree to work with her on this problem? Will she do self-help assignments between sessions? How hard would she be willing to work? Is she willing to go to battle with the harsh voice inside her head? What's the spiritual justification for letting go of her suffering and moving ahead with her life? Does she feel that she's suffered enough? If her answers to these questions are convincing, you can use the additional techniques on your Recovery Circle. But if she continues to express ambivalence, you'll need to empathize and do the Invitation step of Agenda Setting again. Is there something she wants help with? I would do this dance respectfully but firmly. Don't move forward until Janice is ready to move forward with you. Identify the Distortions
Chapter 28
1038
How many distortions you can spot in Janice's thought, "I deserve to suffer forever because I killed my child"? Use checks ( ) to indicate your answers below. Feel free to refer to the definitions of the distortions on page 1025.
Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 28
1039
Answer Janice and I found all ten distortions in her negative thought. Distortion
Yes
Explanation
1. All-or-Nothing Thinking
Janice equates her abortion with premeditated murder and feels totally worthless.
2. Overgeneralization
Janice generalizes from one experience—the abortion—to her entire self, and sees herself as a despicable human being.
3. Mental Filter
Janice ignores all her positive qualities and focuses on the abortion. In fact, she's a devoted wife and mother, and does outstanding work.
4. Discounting the Positive
Janice thinks that her good qualities don't count.
5. Jumping to Conclusions Mind-Reading Fortune-Telling
Janice may assume that others look down on her (MindReading) and predicts that she'll be depressed forever (Fortune-Telling).
6. Magnification and Minimization
Janice magnifies her culpability. She could hardly be any harder on herself if she were a serial killer!
7. Emotional Reasoning
Janice feels bad, so she assumes she is bad.
8. Should Statements
Janice tells herself that she should not have had the abortion, and should never allow herself to feel happy again.
9. Labeling
Janice labels herself as a murderer and tells herself that she killed her child.
10. Blame Self-Blame Other-Blame
Janice constantly rips herself to shreds instead of living in the here-and-now.
Chapter 28
1040
Straightforward Technique Once Janice has seen how distorted the negative thought is, you might say something like this: "Janice, I can see that your suffering is intense. You've also told me that you can see that your suffering results from your thoughts. In other words, every time you tell yourself that you deserve to suffer, you feel guilty and worthless. And even though the thought seems overwhelmingly valid, we've discovered that it contains all ten cognitive distortions. So it may not be quite as true as it seems. "Can you think of a more positive and realistic way to think about the problem? What could you tell yourself instead of, 'I deserve to suffer forever because I killed my child?'" Janice might say, "I could tell myself that I had no choice and simply did what I had to do." Ask her to write this in the Positive Thoughts column of her Daily Mood Log, directly opposite the negative thought, and rate how strongly she believes it. She'll probably tell you that she only believes it about 20% because it's a rationalization. She may say, "The fact is, I did have a choice. I chose to have an abortion for selfish reasons." Remember the necessary and sufficient conditions for emotional change: The necessary condition. The positive thought must be 100% true. The sufficient condition. The positive thought must put the lie to the negative thought. In this case, her positive thought has failed on both counts.
Chapter 28
1041
Suppose she comes up with this positive thought: "Lots of women have abortions every day." She'll probably believe this thought 100%, since it's factually correct. So this thought fulfills the necessary condition for change. But it still won't help, because it won't put the lie to the negative thought. In other words, she'll still believe that she deserves to suffer. The fact that other women have abortions will probably be irrelevant to her. So this thought doesn't fulfill the sufficient condition for emotional change. Although there's only a small chance that the Straightforward Technique will change the way Janice is thinking and feeling, it will show you why she's been trapped in her suffering for so long. You'll see the kinds of errors she makes when she tries to talk back to her negative thoughts on her own. Thinking in Shades of Gray This technique can be helpful for All-or-Nothing Thinking. Instead of looking at things in black-and-white extremes, you evaluate them in shades of gray. We could remind Janice that there's a healthy and unhealthy version of every kind of negative feeling. Healthy sadness is not the same as clinical depression. Healthy remorse is not the same as neurotic guilt. And healthy fear is not the same as a neurotic anxiety. If this idea makes sense to Janice, we could ask whether her negative feelings seem healthy or excessive. We could agree that feelings of grief and remorse about the loss of her baby are appropriate. But does she need to feel 100% miserable, every minute of every day, for the rest of her life? To put it differently, is there a level of remorse and sadness that would
Chapter 28
1042
seem more appropriate? For example, would it be acceptable to lower the intensity of some of her negative feelings from 100% to 50%, or even 25%? If she agrees, she might find it easier to talk back to the negative thoughts on her Daily Mood Log. Cost-Benefit Analysis Janice can list all the advantages and disadvantages of believing that she deserves to suffer forever. Ask her how the thought will help her, and how it will hurt her. Remember that we're not asking Janice to list the advantages and disadvantages of being a rotten human being who murdered her child. Instead, we're asking her to list the advantages and disadvantages of believing that she deserves to suffer forever because of her abortion. Janice can weigh her list of advantages against the disadvantages and put two numbers that add up to 100 in the circles at the bottom of the CBA. As you can see on page 1043, there were an equal number of advantages and disadvantages on Janice's CBA, but the disadvantages outweighed the advantages by a margin of 65 to 35. Now ask Janice what she could tell herself that would be more positive and realistic. If she can come up with a compassionate and convincing thought, ask her to write it down in the Positive Thoughts column of her DML and indicate how much she believes it, between 0% and 100%. Then ask her to re-rate how strongly she believes the negative thought. Unfortunately, even though the disadvantages outweighed the advantages, the CBA was not effective because Janice was still convinced that she deserved to suffer.
Chapter 28
1043
Janice's Cost-Benefit Analysis* Describe the thought or feeling you want to change: "I deserve to suffer forever because I killed my child." Advantages of Believing This
Disadvantages of Believing This
1. This thought seems true, so the truth is on my side.
1. This thought creates tremendous feelings of misery.
2. It shows that I'm not just going to ignore what happened.
2. It robs me of feelings of joy and love.
3. I feel like I'm doing the morally correct thing.
3. The depression sometimes holds me back in my career. I'm less creative and enthusiastic.
4. I can feel sorry for myself.
4. It's frustrating to other people, because I never accept their reassurance.
5. When I criticize myself, my parents and husband reassure me.
5. I don't feel as close to my husband or children as I'd like.
6. This is a way of keeping my baby alive.
6. Maybe I've suffered enough already.
35
* Copyright
65
2003 by David D. Burns, M.D.
Chapter 28
1044
Sometimes the advantages of a negative thought or feeling will be greater than the disadvantages. In this case, you can ask why the patient would want to change the thought, given all the advantages of believing it. Now the patient has to convince you that she or he wants to change. If the patient tells you that they don't want to change, you can simply ask if there's another problem they'd prefer to work on instead. Double Standard Technique You can ask Janice what she'd say to someone else with the same type of problem. Here's how I might set it up: "Janice, let's imagine that you have a dear friend named Sarah who's almost a clone of you. All the facts of her life are similar to yours. She's the same age as you, went to the same college, is married for the second time, and has two children. All her strengths are the same as yours, and her flaws are similar as well. "Sarah tells you that she feels guilty and ashamed about an abortion she had when she was 19. She feels like she deserves to suffer forever because she killed her child. What would you say to her?" Janice might say, "I'd tell her that I understand exactly where she's coming from." Then I'd ask, "Would you tell her that she deserves to suffer?" Janice might say, "Well, I wouldn't say that to her, but I'd be thinking it." In this case, you'd know that Janice does not have a double standard, and that this technique probably isn't going to help. Some patients are just as hard on others
Chapter 28
1045
as they are on themselves. In contrast, Janice may say that she'd talk to Sarah in a more compassionate and realistic way. If so, I might continue like this: David: Why would you talk to Sarah in a more compassionate and loving way? Why not tell her that she deserves to suffer forever because she murdered her baby? Janice: Because it would be cruel to say something like that to someone I cared about. David: Are you saying that you'd treat a friend who was suffering in a kindly, helpful way instead of ripping her to shreds? Janice: Absolutely. David: But don't you think it's important to be honest with people? Janice: Yes, of course. David: Well, if you're going to be honest with her, shouldn't you tell her that she deserves to suffer because she killed her child? After all, you've said that this thought is 100% true. And since Sarah is identical to you, wouldn't it be true for her as well? Janice: It still doesn't sound right. It doesn't seem like she deserves to suffer forever. David: I agree with you, but I want you to spell it out for me. Why is it that Sarah doesn't deserve to suffer forever? What are you driving at? As you can see, I want Janice to explain why Sarah doesn't deserve to suffer. If she can do this in a convincing manner, I'd ask her if she'd be willing to
Chapter 28
1046
talk to herself in the same way she'd talk to Sarah. Of course, there's no guarantee that the Double Standard Technique will be effective. She might say, "I wouldn't talk to myself the same way I'd talk to a friend because I have higher standards for myself." In this case, you could ask Janice if her high standards have been helpful to her. You could also ask, "Why not have equally high standards for a dear friend? If these standards have been so helpful for you, shouldn't they be just as helpful for a friend who's just like you?" Time Projection Ask Janice to close her eyes and relax, and imagine that she can travel into the future and meet the new Janice who's recovered from her depression. The new Janice has learned to forgive herself and feels tremendous joy and selfesteem. Janice can tell her future self about all the feelings of hopelessness and self-hatred that are now overwhelming her. Then she can switch to the role of the happy, recovered Janice, and talk to her current self in a loving, encouraging way. She can provide guidance about how to work her way out of the trap she's in, and explain why she deserves to recover. Alternatively, Janice could travel into the past, to the time when she had the abortion or the time when she was sexually molested, and have a conversation with the young Janice who's suffering and confused. When she plays the role of the young Janice, she can describe what's happening to her, and how she's thinking and feeling. Then she can play the role of her adult self and counsel the young Janice, in much the same way that a loving parent or
Chapter 28
1047
friend might provide comfort and support to a child who's been hurt. Time Projection allows patients to act out the negative and positive voices in their minds, in much the same way that Gestalt therapists have sometimes used the "two-chair technique." These techniques can be effective because of the strong outpouring of emotion, as well as the cognitive restructuring that can occur. Self-Monitoring Janice can track her negative thoughts on a wrist counter and record how many she has at the end of each day. All she has to do is count each negative thought. Then she can let go of the thought and continue with what she was doing when it popped into her mind. After a few weeks of Self-Monitoring, the negative thoughts may begin to decrease in frequency and intensity, or even disappear completely. Negative Practice Janice believes that she deserves to suffer because of her abortion. However, she may agree that the intensity and duration of her suffering have become excessive. For example, we generally wouldn't condemn a murderer to constant, intense suffering for the rest of his or her life. We'd want that person to learn and grow, and move forward with their life in a positive way. If Janice agrees with this line of reasoning, you could ask her how much suffering would be appropriate. How many minutes a day of shame, guilt and self-loathing would seem helpful, or morally correct? Would an hour a day be sufficient? Would ten minutes a day be enough?
Chapter 28
1048
If she's open to the idea, she may be willing to schedule periods of time each day when she can sit and quietly allow the negative thoughts to flow across her mind. She may even want to beat up on herself intentionally during these Negative Practice sessions, and surrender to the feelings of sadness, guilt, hopelessness, worthlessness, or anger. She shouldn't try to fight with the negative thoughts or avoid the painful feelings. At the end of each Negative Practice session, she can give herself permission to focus on living her life in a more positive, productive manner. If she begins to beat up on herself again, she can remind herself to postpone the negative thoughts and feelings until the next Negative Practice session. This is a paradoxical intervention. Sometimes, the struggle to change causes us to get stuck. It's like quicksand. The harder you try to escape, the more you sink. In contrast, when you stop struggling, the suffering sometimes loses its power over you. Acceptance Paradox and Externalization of Voices The Acceptance Paradox also involves surrender rather than struggle, but the acceptance is on a much deeper level. Instead of arguing with the negative thoughts, Janice could learn to acknowledge the truth in them with a sense of inner peace and self-esteem. In the following example, Janice will play the role of the negative, self-critical voice in her mind, and I'll play the role of the positive, self-loving voice. She'll try to rip me to shreds in the same way she rips herself to shreds. At times, I'll respond with the Self-Defense Paradigm and argue with the negative thoughts. At other times, I'll use the Acceptance Paradox, and defeat
Chapter 28
1049
the negative thoughts by finding truth in them. When you use this technique, remind patients that you're not playing the role of two people arguing with each other. Instead, you represent the negative and positive voices inside their minds. Here's how the dialogue might go: Negative Thoughts (played by Janice): Janice, you deserve to suffer forever because you killed your own child. Positive Thoughts (played by David): You know, my abortion was a tremendously painful experience. As I look back on it, I do feel a lot of grief and remorse. Sometimes, I wish with all my heart that I could turn back the clock and do things differently. But I can't. So I've decided to accept what happened and move forward with my life. I owe it to my family and friends. I owe it to myself as well. Negative Thoughts (played by Janice): I'm sorry, but I simply can't permit that. You're a murderer, so you must suffer forever. I won't allow you to feel any happiness, love, joy or creativity ever again. Positive Thoughts (played by David): You know, I've felt a great deal of sadness and shame for several years. I've suffered enough. It's time to let go of all that. Negative Thoughts (played by Janice): Oh, no you don't! You haven't suffered nearly enough yet! I won't let you off the hook so easily. You're a rotten, selfish human being. Positive Thoughts (played by David): Well, there's definitely some truth in what you're saying. I have many flaws, and I can be very selfish
Chapter 28
1050
at times. I'm probably even more flawed than you realize. Negative Thoughts (played by Janice): Oh, so you admit it? Positive Thoughts (played by David): Definitely. I do admit it. Sometimes I can be nasty and irritable. I can be critical and difficult to live with. But I've decided to go ahead and live a happy life in spite of all my flaws. Negative Thoughts (played by Janice): How can you do that? That's outrageous! Positive Thoughts (played by David): It's actually pretty easy. I just decided to lower my standards and stop listening to you. Once I did that, everything kind of fell into place. If Janice feels that my responses are effective, I'd ask her to explain why. How did I defeat the negative thoughts? What, exactly, worked? Once she understands how the Acceptance Paradox works, we'd do a role-reversal so she could try to defeat the negative thoughts as well. This will allow her to incorporate the insight at the gut level. If she flounders, I'd suggest another role-reversal so I could model effective responses again. We'd continue doing role-reversals until she could convincingly defeat the negative thoughts. Socratic Method You can ask Janice a series of questions that will lead her to the illogic of what she's telling herself. For example, you might say: David: Janice, you're telling yourself that you deserve to suffer forever because you had an abortion. Is this correct?
Chapter 28
1051
Janice: Yes, exactly. David: We know that abortions aren't rare. I wonder how many women in the United States have abortions each year? Do you have any idea? I know that you probably don't know the exact number, but give me your best guess. Janice: Maybe 50,000 women. David: Are you saying that all 50,000 women deserve to suffer forever? Janice: No. It doesn't make sense when you put it that way. David: I agree with you, but I'm wondering if you can spell it out for me. Why is it that they don't they deserve to suffer forever? Janice: I guess it doesn't seem fair. David: I agree with you. It wouldn't be fair to say that those 50,000 women deserve to suffer forever because they had abortions. Would it also be fair to say that you don't deserve to suffer forever because of your abortion? This Logic-Based Technique definitely won't be helpful for everyone. In addition, if you're frustrated with the patient, you may sound adversarial. Then patients will feel like they have to defend themselves, so you'll just fire up more resistance. But if you use the Socratic Method in a collaborative, respectful way, you can sometimes achieve outstanding results. Semantic Method This method is especially helpful for Should Statements and Labeling. The patient simply replaces the harsh, pejorative language in their negative thoughts
Chapter 28
1052
with softer, kinder expressions. For example, instead of telling herself that she shouldn't have had the abortion, Janice could tell herself, "I wish with all my heart that I hadn't needed to have an abortion." Instead of telling herself that she's a murderer who deserves to suffer forever, she could tell herself that she's endured a terrible loss and deserves support. Let's Define Terms Janice sees herself as a murderer. You could ask her if she thinks there's a difference between having an abortion and committing murder. Why do we have different words for them? Janice also tells herself that she's a bad, worthless human being. You could ask her what she means by this. What's the definition of a "bad, worthless human being"? She might say that a bad, worthless human being is someone who does bad things. You could ask her to clarify what she means. Does a bad, worthless human being do bad things all of the time, or some of the time? If she says "some of the time," you can point out that according to this definition, we're all bad, worthless human beings, since we all do bad things some of the time. If, in contrast, she says that a bad, worthless human being is someone who does bad things all of the time, you can point out that according to this definition, no human being is bad or worthless, since no one does bad things all the time. Furthermore, we know that Janice does many positive, loving things every day. So this definition doesn't hold water, either. No matter how she defines "a bad, worthless human being," you can easily show that the definition applies to all human beings, or to no human
Chapter 28
1053
beings. The purpose of this technique is to show Janice that there is no such thing as a "good" or "bad" human being. We're all a mixture of good and bad traits, feelings, thoughts, and actions. This may seem obvious, but it can be quite a revelation when you're trapped in All-or-Nothing Thinking and you suddenly "see" it for the first time. Let's Define Terms can help patients let go of the hurtful, restrictive labels at the core of their suffering, so they can develop a broader and more realistic view of themselves as human beings. However, it may seem overly philosophical or legalistic and leave the patient in the dust, or fire up the patient's resistance. If so, you can drop it and move on to another method. Survey Technique Janice feels lonely and isolated. She believes that her problems are unusual and shameful, so she avoids people. The isolation reinforces the idea that she's worthless and different from other people. When Janice does try to connect with other people, it doesn't work very well because she's involved in a kind of narcissistic self-absorption. She complains about how worthless she is, and then everyone tries to cheer her up. They sound patronizing and condescending because they're not really listening, so Janice gets frustrated and keeps complaining. They get frustrated with her as well, but rarely express their feelings because Janice seems so fragile. She senses their annoyance and ends up feeling even more inadequate. Instead, Janice might find it useful to ask several close friends if they've ever made any mistakes they regret, or done anything that seemed bad or
Chapter 28
1054
hurtful. If so, how did they feel? Did they have any feelings of shame or worthlessness at the time? Do they have any lingering feelings of guilt or embarrassment? She may discover that people are more human than she imagines, and that she can connect with them in a new way, without having to play the role of victim all the time. If she's reluctant to open up to friends, she could attend a support group where she'd have the opportunity to interact with other people who have suffered. For example, at AA meetings, people sometimes stand and make powerful personal disclosures, like: "I'm an alcoholic. I can't tell you how many times I've gotten drunk, stolen things, and beaten people up. When I was 23, I killed my best friend in a fight over drugs, and spent seven years in prison. If it weren't for AA, I'd probably be out getting drunk and doing the same kinds of things tonight. But I've been clean and sober for 17 years because of AA. God bless AA!" This type of radical self-acceptance can sometimes have a significant healing effect on others. Of course, AA wouldn't be a good fit for Janice if she doesn't have an alcohol or drug problem, but support groups like Recovery, Inc. or Emotions Anonymous might provide similar opportunities. Reattribution Janice is consumed by self-blame and tells herself that she's a bad, worthless human being. But was her "badness" the real reason for her abortion? Using Reattribution, Janice could identify all the factors that actually contributed
Chapter 28
1055
to her decision to have an abortion. Had she been raped? Was she using drugs at the time? Did she feel pressured by her boyfriend or family to have the abortion? Did she feel torn? What was she thinking and feeling? What was going on? The goal of Reattribution is not to make excuses or rationalize what happened, but simply to think about it more realistically. She could also ask herself what she can learn from the experience. If she had to confront a similar dilemma today, would she make a different decision? Why or why not? Would she approach the problem differently? In what way? What can she take from the experience that will help her learn and grow? Examine the Evidence Depression and anxiety result from a mental hoax. People who feel depressed and anxious nearly always tell themselves things that aren't true. Emotional Reasoning often fuels the deception. Janice feels totally rotten and despicable, so she concludes that she must be totally rotten and despicable. She feels completely hopeless, so she thinks that she is completely hopeless. She feels unlovable, so she believes that she is unlovable. You could ask Janice if there's any evidence that supports what she's telling herself. The dialogue might go like this: David: Janice, you're telling yourself that you're a worthless human being and that you'll never recover from your depression. I know that those feelings are incredibly painful for you. But sometimes, we feel things very strongly that turn out not to be true. I'm wondering if there's any evidence that you really are worthless?
Chapter 28
1056
Janice: Well, I've felt totally worthless ever since my abortion. It's hard for me to let go of the idea that I killed my baby. David: I know that was a devastating experience, and you seem to be writing yourself off completely because of it. But I'm wondering if we might look at it from another perspective. For example, is there any evidence that you're not worthless? Do you have any positive qualities we should consider? Janice: People tell me that I'm a good Mom, and I have two wonderful children who love me very much. I'm completely devoted to them, and I'd do anything for them. I've received several awards at work as well. Our new cancer drug is helping so many people already. David: So you're a loving mother and you're doing outstanding work for your company. Does that sound like the description of a totally worthless human being? Janice: Perhaps not, but what if these feelings never change? I feel tainted. David: Maybe that's the worst part of it for you—the idea that things will never change. But once again, feelings aren't always the same as facts. Did you ever feel hopeless in the past? Janice: Oh, yes, I felt contaminated when my uncle abused me. I felt so ashamed and dirty, and I thought those feelings would never go away. David: What happened? Did those feelings go on forever, or did you feel better after a period of time?
Chapter 28
1057
Janice: I've told you about the aura that I developed. It was like a glow that surrounded my body, and it seemed to protect me. I even felt happy and worthwhile for a long time. But after the abortion, I lost my aura, and I've felt worthless and guilty ever since. David: So you felt hopeless and worthless after you were abused, but you found a way to cope, and you actually began to feel happy again. Those good feelings lasted for many years, right up until the time of your abortion. Did I get that right? Janice: Yes. David: So does the evidence suggest that you can never recover from traumatic events, or that you do have the power to recover? Maybe the real question is not so much whether you really are worthless and hopeless, but whether you feel ready to let go of the suffering and move ahead again. When you use Examine the Evidence, you're trying to show patients that they're deceiving themselves about something very basic and important. However, you'll need to use this technique in a kind, collaborative way, so you don't fire up the patient's resistance. Remember that the goal is not to put Janice down, but rather, to show her how to escape from her emotional prison so she can experience joy and self-esteem again. Cognitive Flooding and Memory Rescripting Janice seems to be suffering from the aftermath of two traumatic experiences: the sexual abuse she endured as a child, and her abortion many
Chapter 28
1058
years later. Cognitive Flooding and Memory Rescripting will provide you with the chance to intervene at the source of her suffering, rather than simply dealing with her negative thoughts and feelings in the here and now. You could ask Janice to close her eyes and visualize how she was feeling around the time of the abortion. Ask her to describe the scene, and tell you what she's thinking and feeling. Was she feeling sad? Frightened? Confused? Overwhelmed? Once she's flooded with these feelings, she can edit or change the scene. For example, she might want to bring her baby back to life and comfort it. She could tell the baby much she loves and misses it. This might open up a floodgate of emotion and allow her to do the grieving that she's been avoiding for the past six years. Alternatively, Janice may want to confront the sexual abuse she endured as a child, because she may still be harboring strong feelings of humiliation and rage. First, she could close her eyes and vividly picture the abuse. Once again, you can ask her to describe exactly what's happening, and what she's thinking and feeling. Once the feelings of anger, shame, anxiety, and worthlessness are at maximum intensity, she can edit the pictures in her mind. She might want to enter the scene as a powerful adult and punish her uncle. She might want to tell him how damaged, exploited and hurt she felt. She might want to tell her parents how enraged and victimized she felt and ask why they didn't protect her from his abuse. Or, she might want to comfort the little girl and tell her that she loves her, and that she didn't deserve what happened.
Chapter 28
1059
There's no formula on how to rescript the scenes, and every patient will come up with something unique and unpredictable. I usually try to go where the patient leads, without too much editing or suggestion. Pleasure Predicting Sheet Janice believes that she's doomed to endless suffering. She can test this belief with the Pleasure Predicting Sheet. She can schedule a series of activities with the potential for pleasure, learning, or personal growth, and predict how satisfying each activity will be on a scale from 0% (not at all satisfying) to 100% (extremely satisfying). After she completes each activity, she can record how satisfying it turned out to be. This technique could help Janice in three different ways. First, research studies indicate that pleasurable activities can have significant antidepressant effects. Second, Janice would be treating herself in a more loving and compassionate way. And finally, she'd be testing her belief that she's hopeless. She may discover that many activities are considerably more rewarding than she anticipated, and that she's not, in fact, doomed to endless suffering. This discovery may motivate her to do even more. Hidden Emotion and One-Minute Drill None of the CBT techniques I've described so far were helpful for Janice. I actually used many more techniques than the ones I've discussed here, but her depression score remained the same week after week. I couldn't seem to put a dent in her belief that she was a murderer who deserved to suffer forever. This is not unusual. Even mildly depressed patients can be challenging, and I've usually
Chapter 28
1060
had to keep the faith in the face of repeated therapeutic failures. At the time Janice and I were working together, I was developing my brief Anger and Relationship Satisfaction Tests. One week, I asked Janice if she'd be willing to fill them out and tell me if they seemed useful. Her anger score was extremely high, and her Relationship Satisfaction score was low, indicating marital conflict. When I asked Janice about this, she became tearful and revealed something she'd been hiding the entire time we were working together. She suspected that her husband, Charlie, was having an affair with his secretary. She felt so hurt and ashamed that she hadn't had the courage to bring it up during our sessions. I asked if she might want to invite Charlie to join us for a session or two, so we could try to assess what was going on. She agreed to invite him, but didn't know if he'd be willing to join us. They came to the next session together. Charlie seemed completely devoted to Janice, and didn't strike me like the type of fellow who was having an affair. When she confronted him with her suspicions, tears came to his eyes. He said that he loved her greatly, and had no interest whatsoever in his secretary or any other woman. He said that he'd been feeling incredibly lonely and frustrated, and would to do anything to improve their relationship, including coming to all her therapy sessions if she wanted him to. Janice welcomed this idea, and we decided to do some couple's communication training, using the One-Minute Drill. They were strongly motivated to improve their relationship, and practiced at home every day
Chapter 28
1061
between sessions. Janice's marital satisfaction quickly increased, and her mood began to lift at the same time. Although she still felt some healthy sadness and remorse about her abortion, these feelings were no longer a problem for her. You can see her completed Daily Mood Log on page 1062. Janice was one of the most challenging individuals I've ever worked with. I tried dozens of techniques that didn't work before I found the one that did. She was often critical of me during sessions and gave me low empathy scores. I had to repair these alliances failures with my best empathy skills. It wasn't always easy because her criticisms often felt quite biting. I couldn't have predicted that the Hidden Emotion Technique and the OneMinute Drill would be effective, but in retrospect, it makes perfect sense. Janice was convinced that she was a worthless human being, and it's not surprising that she believed her husband didn't really love her. When she discovered that he was completely devoted to her, and they learned to communicate more openly, her depression finally disappeared.
Chapter 28
1062
Janice's Daily Mood Log* Upsetting Event: Thinking about my abortion. % Before
% After
% Before
% After
Sad, blue, depressed, down, unhappy
100%
25%
Embarrassed, foolish, humiliated, self-conscious
100%
0%
Anxious, worried, panicky, nervous, frightened
80%
0%
Hopeless, discouraged, pessimistic, despairing
100%
0%
Guilty, remorseful, bad, ashamed
100%
25%
Frustrated, stuck, thwarted, defeated
80%
0%
Inferior, worthless, inadequate, defective, incompetent
100%
0%
Angry, mad, resentful, annoyed, irritated, upset, furious
100%
0%
Lonely, unloved, unwanted, rejected, alone, abandoned
100%
0%
Other
Emotions
% Before
% After
1. I deserve to suffer forever because I killed my child.
100%
2. I shouldn't have had an abortion.
Negative Thoughts
Emotions
% Belief
Distortions
Positive Thoughts
0%
AON; OG; MF; DP; FT; MAG; ER; SH; LAB; SB
1. This is unreasonable. I've suffered enough. I owe it to my family, my friends, and myself to let go of this pain and self-abuse.
100%
100%
50%
ER; SH; SB
2. I wish I hadn't needed to have an abortion, because I lost a baby I loved. It was a very confusing time, and I wasn't sure what I should do.
100%
3. I'm a worthless human being.
100%
0%
AON; OG; MF; DP; MAG; ER; SH; LAB; SB
3. I'm a human being with strengths and flaws, just like everyone else.
100%
4. I'll be depressed forever.
100%
10%
AON; DP; FT; ER
4. That's not true. Whenever I've felt upset, I've gotten better eventually. In fact, I'm already feeling better, so I can't possibly be hopeless!
100%
* Copyright
1984 by David D. Burns, M.D. Revised 2004.
29*
Public Speaking Anxiety— The Woman Who Was Afraid to Faint
I once treated a woman named Georgia who was in an executive training program at a Fortune 500 company, and was often called on to make presentations to her colleagues. Although she was doing well in the program, she'd always struggled with public speaking anxiety and had "frozen up" in front of audiences a few times. In fact, she'd even fainted once while giving a presentation to the management team at a previous job. She said that the Vice President of Operations caught her as she was wobbling at the podium just before she blacked out. Georgia felt extremely embarrassed about fainting. She said, "The rumors that flew after that were incredible. According to one rumor, I was pregnant. According to another rumor, I was anorexic." She was relieved that anxiety was not one of the explanations people were considering, and told me it was probably
* Copyright
2004 by David D. Burns, M.D.
Chapter 29
Page 1064
because she'd given many successful presentations in the past. Fainting is common in people with blood or needle phobias, but it's not nearly as common with other forms of anxiety. Fainting occurs when there's a sudden fall in blood pressure, along with a slowing of the heart. As a result, the heart temporarily can't pump enough blood up to the brain, so you get dizzy and pass out. Once you're lying down, your heart can pump blood to your head more easily because it doesn't have to pump the blood uphill, against gravity. This allows you to regain consciousness. Fainting is a defense mechanism that guarantees that your brain will always have an adequate supply of oxygen. Certain psychiatric medications, including some antidepressants, can cause lightheadedness. The drugs cause the blood vessels to relax, so when you stand up, blood temporarily pools in your legs. As a result, your heart can't pump enough blood up to the brain, and you experience dizziness or even a brief blackout. Patients can combat this by standing up more gradually. They can also walk in place for a few seconds when they stand up. If they lift their knees high with each step, their leg muscles will squeeze the pooled blood back up to the heart. The Valsalva maneuver may also help. You forcefully try to exhale while keeping your mouth and nose closed. This causes a brief increase in your blood pressure, so your heart pumps out more blood. Alternatively, you can tighten your face, arm and chest muscles. Then you can relax them and tighten them up again, much like someone pumping iron. This also gets your heart pumping more
Chapter 29
Page 1065
efficiently and may relieve the dizziness. Although these techniques usually prevent fainting, Georgia will still feel anxious and vulnerable when she has to give a talk at work because she's telling herself: What if my mind goes blank and I forget what I'm speaking about? What if someone in the audience knows more than me and asks a hard question? What if I bore my audience? What if they see how nervous I am? What if they think I'm an idiot? What if I faint? These thoughts are all rhetorical questions of the "what if" variety. I encouraged Georgia to convert them into statements when she filled out the Negative Thoughts column on her Daily Mood Log. That's because you can't put the lie to a rhetorical question, but you can challenge the claim behind it. Georgia's Daily Mood Log appears on page 1066. The upsetting event was, "Having to give a talk in front of my colleagues at work." As you can see, she felt anxious, ashamed, embarrassed, discouraged, frustrated and inadequate. The high ratings in the "% Before" column indicate that all of these feelings were strong. Georgia strongly believed the negative thoughts as well, because they all seemed realistic to her.
Chapter 29
Page 1066
Georgia's Daily Mood Log* Upsetting Event: Having to give a talk in front of my colleagues at work. Emotions
% Before
Anxious
Emotions
% Before
100%
Discouraged
60%
Ashamed
75%
Frustrated
75%
Embarrassed
100%
Inadequate
90%
Negative Thoughts 1. My mind might go blank. I
% Before
% After
% After
Distortions
100%
might forget what I'm speaking about. 2. Someone might know more
90%
than me and ask a really hard question. 3. People might get bored.
90%
4. They'll see how nervous I
100%
am. 5. My colleagues will think I'm
80%
an idiot. 6. I might faint when I give my
100%
presentation.
* Copyright
2004 by David D. Burns, M.D.
Positive Thoughts
% After
% Belief
Chapter 29
Page 1067
The thought that was bugging Georgia the most was, "I might faint when I give my presentation." I've put that thought in the middle of the Recovery Circle on page 1068. Which techniques can we use to help Georgia put the lie to this thought? Review the list on page 1069, and see if you can come up with at least 15 techniques that might be helpful to Georgia. Put the names of the techniques you select in the boxes around the Recovery Circle. When you're done, you can turn to page 1070 and I'll describe a few of the techniques that were the most helpful for her.
Chapter 29
Page 1068
Georgia's Recovery Circle*
16
15
1
14
2
13
3
12
I might faint when I give my presentation. 100%
4
11 5
10 6 9
* Copyright © 2004 by David D. Burns, MD
8
7
Chapter 29
Page 1069
50 Ways to Untwist Your Thinking* Basic Techniques
Exposure Techniques
Role-Playing 19. Externalization of Voices
Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques
Philosophical / Spiritual 21. Acceptance Paradox
Compassion-Based
Visual Imaging
5. Double Standard Technique
Truth-Based 6. Examine the Evidence
8. Survey Technique 9. Reattribution
39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
7. Experimental Technique
Cognitive Exposure
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Motivational Techniques
Semantic 12. Semantic Method 13. Let's Define Terms
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
14. Be Specific
Quantitative
30. Devil's Advocate Technique
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Chapter 29
Page 1070
Empathy You can see my Recovery Circle on page 1071. As usual, I've listed the four Basic Techniques first, starting with Empathy. Georgia is afraid she'll faint when she gets up to give her talk. How would you empathize with her? What would you say? Use the Five Secrets of Effective Communication, and put the names of the techniques you're using in parentheses after each sentence you write below. You can include the Disarming Technique (DT), Thought and Feeling Empathy (TE and FE), Inquiry (IN), "I Feel" Statements (IF), and Stroking (ST). You'll find the definitions of these techniques on page 242 in case you'd like to review them.
Chapter 29
Page 1071
Georgia's Recovery Circle* Five Secrets SelfMonitoring Image Substitution
Empathy
16
15
1
14 Cognitive Flooding
Agenda Setting
2
13
3
12
Cost-Benefit Analysis
I might faint when I give my presentation. 100%
Straightforward Technique
4
11 Hidden Emotion Technique
Identify the Distortions
5
10
Downward Arrow
6 Survey Technique
9
8
Self-Disclosure / Survey Technique Feared Fantasy
Examine the Evidence * Copyright © 2004 by David D. Burns, MD
7
Acceptance Paradox
Chapter 29
Page 1072
Answer Here's one approach: "Georgia, it sounds like you're feeling intensely anxious about giving talks in front of your colleagues at work. (FE) You're afraid that you might faint, and that everyone will look think you're an idiot. (TE) That must feel humiliating and intimidating. (FE) It's almost as if you're always working under a cloud, hoping that lightning won't hit you. (FE) Can you tell me what that's been like for you? (IN)" The goal is simply to give Georgia another chance to vent, so she'll know that you're listening and that you've "gotten it," before you jump in and begin to challenge the negative thought. Agenda Setting Are there any motivational issues we should explore at this juncture? Why might someone with public speaking anxiety resist treatment? Think about Outcome Resistance and Process Resistance. Put your ideas here:
Chapter 29
Page 1073
Answer Georgia might resist treatment because she'll have to confront the monster she fears the most. We know that she's willing to give talks because she's already doing it. However, there are some potentially helpful Exposure Techniques that she might resist. For example, if we asked her to use SelfDisclosure, and tell one or two colleagues about her public speaking anxiety and her fainting, would she do it? Georgia was extremely courageous and eager to get help with her public speaking anxiety. She reassured me that she'd do written homework regularly and take any risks that would be necessary to conquer her fears and put them behind her once and for all. Identify the Distortions Identify the Distortions is the third technique on the Recovery Circle. Usually, the patient and I identify the distortions in the negative thoughts one at a time, but for the purposes of this exercise, I'd like you to consider all of Georgia's negative thoughts. Use checks ( ) to indicate all the distortions you can find in them. When you're done, you can review my analysis on the next page. Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 29
Page 1074
Answer Georgia and I found all 10 distortions in her negative thoughts. Distortion
Yes
Explanation
1. All-or-Nothing Thinking
Georgia thinks about her public speaking ability in black-and-white terms. Either she's a star, or she's no good at all.
2. Overgeneralization
She thinks that if one person feels bored, everyone will. She also thinks that fainting or freezing up in front of a group will become a never-ending pattern of defeat and humiliation. Finally, she generalizes from her performance when she gives a talk to her entire sense of self-esteem.
3. Mental Filter
She worries about the one time that she did faint, and overlooks the many times that she's done well and hasn't fainted.
4. Discounting the Positive
She thinks that her accomplishments and good relationships with people at work don't count.
5. Jumping to Conclusions
She tells herself that she'll probably faint when she gives her next speech (Fortune-Telling). She also assumes that even if she doesn't faint, her colleagues will be bored, ask hostile questions, and lose respect for her (Mind-Reading).
Mind-Reading Fortune-Telling 6. Magnification and Minimization
She magnifies the likelihood of fainting. She feels like her entire career is on the line every time she gives a talk.
7. Emotional Reasoning
She feels like she's going to blow it and look like an idiot, so she assumes she really will.
8. Should Statements
Georgia thinks she shouldn't be so nervous and that she shouldn't faint. She also thinks she should know more about her topic than every person in the audience.
9. Labeling
She labels herself as "an idiot."
10. Blame
She blames herself for fainting, as if it were a moral flaw.
Self-Blame Other-Blame
If you review the table on page 941, you'll find numerous techniques you could try, based on these distortions. For example, Georgia is involved in MindReading, so we might want to include the Survey Technique on the Recovery
Chapter 29
Page 1075
Circle. She's also trapped by many hidden Should Statements, so we could include the Semantic Method, the Externalization of Voices and the Acceptance Paradox as well. Any time you run out of methods to try, you can review the distortions in the thought you're working on and consult the table on page 941. Straightforward Technique As you know, this is always the fourth technique on my Recovery Circle. Although it isn't usually effective, it worked very well for Georgia. She was able to put the lie to her first five negative thoughts in a convincing fashion using the Straightforward Technique. You can see the positive thoughts she generated on pages 1076 – 1077. However, she continued to draw a blank on her sixth thought, "I might faint when I give my presentation." Downward Arrow Technique It was hard for her to challenge this thought because she had fainted once, and there was a possibility that she could faint again in the future. I wanted to find out why Georgia was so afraid of fainting. I told her to draw a downward arrow under the sixth negative thought on her Daily Mood Log. Remember that the downward arrow is a form of shorthand for these types of questions: "If that were true, what would it mean to you? Why would it be upsetting to you?" You could also use the What-If Technique and ask these types of questions: "What are you the most afraid of? What's the worst thing that could happen?" A new thought will pop into Georgia's mind. Tell her to write it down and draw a new arrow underneath it. Repeat this process until you get to the bottom of the barrel, as illustrated on page 1078.
Chapter 29
Page 1076
Georgia's Daily Mood Log* Upsetting Event: Having to give a talk in front of my colleagues at work. Emotions
% Before
100%
Discouraged
60%
Ashamed
75%
Frustrated
75%
Embarrassed
100%
Inadequate
90%
Emotions
% Before
Anxious
Negative Thoughts 1. My mind might go blank. I
% Before
% After
100%
20%
might forget what I'm speaking about. 2. Someone might know more
90%
10%
than me and ask a really hard question.
3. People might get bored.
90%
30%
* Copyright
% After
Distortions
Positive Thoughts
AON; DP; FT; MAG; ER; SH
1. I've never once forgotten what I was
DP; MR; FT; MAG; ER; SH
2. This is my area of expertise, and I'll
AON; OG; DP; MR; FT; ER; SH
% After
% Belief 100%
talking about during a presentation. But if I do get lost, I can just glance at my outline, which will be right in front of me. 100%
definitely know more than most of the people in the audience. If someone asks a difficult question, I can simply say that I don't know the answer. No one expects me to know all the answers. 3. I've gotten good feedback about nearly all
my presentations so far. But there's always room for improvement.
2003 by David D. Burns, M.D.
100%
Chapter 29
Page 1077 Georgia's Daily Mood Log (cont'd)
Negative Thoughts 4. They'll see how nervous I
% Before
% After
100%
10%
am. 5. My colleagues will think I'm
80%
an idiot.
6. I might faint when I give my
presentation.
100%
0%
Distortions AON; OG; DP; MR; FT; ER; SH; SB AON; OG; DP; MR; FT; ER; SH; LAB; SB
MF; DP; FT; MAG; ER; SH
Positive Thoughts 4. No one has ever said that I looked
% Belief 100%
nervous before, but even if they did, would it be the end of the world? 5. I don't believe that any of my colleagues
100%
think I'm an idiot. I've always received lots of positive feedback from them. Even if I do give a mediocre presentation from time to time, they'll probably just assume I'm human. 6. ???
Kathryn (editor), notice that we are using two different styles for the Emotions table at the top of the DMLs in the book. One has all the emotions listed in each row, with certain feelings circled. This one shows how I do it in real life. The version in this chapter as well as several others is simplified, only showing one emotion on each row. This looks cleaner, but is less clear to the reader where those particular emotion words came from. Let us know which you prefer. I think the one with the circled emotions may be preferable.
100%
Chapter 29
Page 1078
Here's how Georgia's Downward Arrow went: I might faint when I give my presentation. Let's assume that you do faint. What would that mean to you? Why would it be upsetting? What are you the most afraid of? Then I'll look like a fool in front of all my colleagues. Let's assume that happened. What would it mean to you? Why would it be upsetting to you? My colleagues will find out that I'm not as confident as I seem. Let's assume that also happened. What would that mean to you? Why would it be upsetting to you? Then they'll lose respect for me and won't want to work with me any more. And what then? It will hurt my career, and I'll get passed up for promotions. And then? That would mean I was a failure. Let's suppose you were a failure. What would that mean to you? That would mean I was worthless. Review this list of negative thoughts. What do they tell us about: Georgia's personal values? The way she measures her self-esteem? The assumptions she makes about other people? Her expectations about how people will judge her? Review the list of common SDBs on page 1080, and see if you can pinpoint a few of Georgia's SDBs. Put your ideas here:
Chapter 29
1. 2. 3. 4. 5. When you're done, you can turn to page 1081.
Page 1079
Chapter 29
Page 1080
Common Self-Defeating Beliefs* Achievement
Depression
1. Perfectionism. I must never fail or make a mistake. 2. Perceived Perfectionism. People will not love and accept me as a flawed and vulnerable human being. 3. Achievement Addiction. My worth as a human being depends on my achievements, intelligence, talent, status, income, or looks.
Love
13. Hopelessness. My problems could never be solved. I could never feel truly happy or fulfilled. 14. Worthlessness / Inferiority. I'm basically worthless, defective, and inferior to others.
Anxiety 15. Emotional Perfectionism. I should always feel happy, confident, and in control.
4. Approval Addiction. I need everyone's approval to be worthwhile.
16. Anger Phobia. Anger is dangerous and should be avoided at all costs.
5. Love Addiction. I can't feel happy and fulfilled without being loved. If I'm not loved, then life is not worth living.
17. Emotophobia. I should never feel sad, anxious, inadequate, jealous or vulnerable. I should sweep my feelings under the rug and not upset anyone.
6. Fear of Rejection. If you reject me, it proves that there's something wrong with me. If I'm alone, I'm bound to feel miserable and worthless.
Submissiveness 7. Pleasing Others. I should always try to please others, even if I make myself miserable in the process. 8. Conflict Phobia. People who love each other should never fight or argue. 9. Self-Blame. The problems in my relationships are bound to be my fault.
Demandingness
11. Entitlement. You should always treat me in the way I expect.
* Copyright
19. Brushfire Fallacy. People are clones who all think alike. If one person looks down on me, the word will spread like brushfire and soon everyone will look down on me. 20. Spotlight Fallacy. Talking to people feels like performing under a spotlight on a stage. If I don't impress people by being sophisticated, witty, or interesting, they won't like me. 21. Magical Thinking. If I worry enough, everything will turn out okay.
Other
10. Other-Blame. The problems in my relationships are the other person's fault.
12. Truth. I'm right and you're wrong.
18. Perceived Narcissism. The people I care about are demanding, manipulative, and powerful.
22. Low Frustration Tolerance. I should never have to feel frustrated. Things should be the way I expect them to be. 23. Superman / Superwoman. I should always be strong and never be weak.
2001 by David D. Burns, M.D.
Chapter 29
Page 1081
Answer Georgia and I identified many SDBs, including: Perfectionism. She believes she must never make a mistake. Perceived Perfectionism. She thinks that her colleagues will judge her as harshly as she judges herself, and will reject her if she has any flaws or imperfections. Achievement Addiction. She seems to base her sense of self-esteem on her accomplishments. Approval Addiction. She thinks she needs everyone's approval or else she's no good. Brushfire Fallacy. She thinks that disapproval will spread like brushfire, so if even one person looks down on her, everyone will. This makes disapproval seem extremely dangerous. Spotlight Fallacy. She feels like she's constantly being judged and has to impress people to get them to like her. Superwoman. Georgia thinks she's never supposed to show any signs of weakness or vulnerability. Now we can see that the fainting is not the real problem. The real problem is the way Georgia thinks about it. She believes that her colleagues are extremely judgmental and will turn against her if they discover that she's not perfect. This mindset puts her under a great deal of pressure because it seems like her entire career and feelings of self-esteem are on the line whenever she stands up to speak.
Chapter 29
Page 1082
Self-Disclosure / Survey Technique I suggested that Georgia could tell one or more colleagues about the time she fainted at work and ask if they'd ever experienced public speaking anxiety or done something foolish or embarrassing. This would be a way of testing her belief that people will turn against her if they discover that she's vulnerable. She may discover that people are far less judgmental than she thinks. She could even say something like this at the start of one of her talks: "It's great to be here today. I've been looking forward to this presentation. However, I want to warn you that I occasionally pass out due to my intense public speaking anxiety, so if I keel over before your very eyes, you'll know what happened. Just throw a pitcher of ice water on me or slap me a few times and I'll be fine. And if I don't keel over today, we'll be in glorious shape!" That may bring a laugh and put everyone at ease. Of course, the tone of the delivery will have a huge impact on whether or not this approach is effective. If Georgia sounds nervous or self-effacing, the technique could fall flat and backfire. To drive the point home, I told Georgia a story about Dr. Albert Ellis. He's over 90 years old, and has suffered from diabetes for years. He has to take insulin shots and eat sandwiches throughout the day to keep his blood sugar steady. In spite of this, he still works 60 or 70 hours a week seeing patients at his Institute in New York and giving presentations all around the country. There are rumors that he'll never stop working, and will probably die while giving a
Chapter 29
Page 1083
workshop or treating a patient. My colleague, Dave Lima, sponsored a workshop for Dr. Ellis a few years ago in Chicago. At the start of the workshop, Dr. Ellis passed out on stage and everyone thought he was dead. Dave rushed to his side to try to revive him. When Dr. Ellis opened his eyes, Dave gave him some orange juice to boost his blood sugar. Before long, Dr. Ellis stumbled to his feet and loudly announced, "Diabetes is an f___ing pain in the ass. But it's not terrible! So let's get going." He proceeded to give a brilliant and highly appreciated workshop. Because he wasn't ashamed, his fainting was actually an asset. It allowed him to form a human bond with the group. Dr. Ellis has always emphasized that our feelings result from our thoughts, and not from what happens to us. Clearly, he practices what he preaches! Georgia said that this story really hit home, and that what she was learning in therapy dovetailed with what she was learning in her executive training program. She said that the person in charge of the program was keen on molding them into strong leaders, and constantly stressed humility and not being afraid to admit your mistakes or what you don't know. Coincidentally, Georgia was coaching a colleague who had to give a presentation for the meeting she was MC'ing later that week. He wasn't comfortable with public speaking either. After our session, Georgia decided to take a chance and tell him that she'd actually fainted once at the start of a presentation. She was surprised that he didn't say anything negative or even look shocked, and they ended up giggling about it. Then he confessed that he was so
Chapter 29
Page 1084
nervous about his own presentation that he'd made an excuse to his manager about why he couldn't attend the meeting. His manager didn't buy it and told him he had no choice. He said that Georgia's disclosure made him feel a whole lot better. After their coaching session, Georgia said she felt so relieved that her anxiety practically disappeared, and she actually started looking forward to her next presentation. As it turned out, she did a tremendous job and received overwhelming praise from her colleagues. Feared Fantasy / Acceptance Paradox Dr. Ellis emphasizes the difference between a "low-level solution" and a "high-level solution." So far, Georgia has achieved a low-level solution. She feels better because she's realized that her fears were unfounded. But if she continues to base her self-esteem on other people's approval, she may still be vulnerable to anxiety in the future. A "high-level solution" is more powerful. It involves a profound change in the patient's value system. You take the next step and ask this question: "If people really were incredibly judgmental and rejecting, would I need to be concerned? Would it be as terrible as I fear?" I suggested that Georgia could confront the monster she feared the most with the Feared Fantasy Technique. In the following dialogue, Georgia will play the role of a Hostile Critic who saw her faint while she was giving a presentation at work. He will say all kinds of mean things that a real person would never say. I will play Georgia's role and try to defeat the Hostile Critic using the Acceptance
Chapter 29
Page 1085
Paradox: Hostile Critic (played by Georgia): Hi Georgia, I saw your presentation at work last week. Georgia (played by David): Oh, you did? I'm afraid it wasn't one of my more stellar performances! Hostile Critic (played by Georgia): You can say that again. You passed out! You really looked like a fool. Georgia (played by David): You got that one right! I felt pretty foolish, too. Hostile Critic (played by Georgia): Well, there must be something wrong with you. I've never seen anyone faint at work before. Georgia (played by David): You know, I used to worry that there might be something medically wrong with me, but my doctor explained that it was just anxiety. Apparently, some people faint when they get anxious. My heart slows down and my blood pressure drops, so I keel over. But it's actually a good thing, because my heart can pump blood up to my brain more easily. Then I come to again. Hostile Critic (played by Georgia): That sounds awfully weak and neurotic. I wouldn't advertise the fact if I were you. Georgia (played by David): I'm not sure I catch your drift. Are you thinking I should keep my anxiety a secret? Hostile Critic (played by Georgia): Definitely. I think you should feel ashamed of yourself. Fainting at work is disgraceful.
Chapter 29
Page 1086
Georgia (played by David): Listen, I've done things far more disgraceful than that! I'm actually a rather shameless lady. Hostile Critic (played by Georgia): You can joke about it if you want, but I think this is serious business. To be honest, I've lost all respect for you. I used to think you had it all together. Now I can see that you're just a basket case. Georgia (played by David): I've wondered if I sometimes appear more confident than the way I feel inside. You may have overestimated me. Hostile Critic (played by Georgia): So you admit that you're weak and neurotic? Georgia (played by David): Oh, definitely! I'll have to plead guilty as charged. In fact, I have tons of flaws. Hostile Critic (played by Georgia): Well, I'm shocked! I'm going to tell everyone at work about you. Georgia (played by David): Oh, please do. That would be great, because then I wouldn't have to tell them myself. You might even want to distribute a memo. I can see it now: "Executive trainee faints due to public speaking anxiety. Admits to numerous other flaws as well. Employees shocked. Corporate stock plummets." Now, ask yourself, who's being the bigger jerk here? Is it Georgia, or the Hostile Critic? Georgia found the Feared Fantasy and Acceptance Paradox extremely helpful. At this point, she was ready to challenge her sixth negative thought.
Chapter 29
Page 1087
Here's what she came up with: "I could faint, since I did faint once, but it's not likely, since I've given so many presentations without fainting. Furthermore, I have some new tools to prevent fainting, like walking in place when I stand up. Even if I did faint, it wouldn't be the end of the world. If that's the worst thing I ever have to worry about, I'll be in good shape!" Georgia believed this thought 100%, and her belief in the negative thought fell to 10%. You can see her completed DML, along with the changes in her negative emotions, on pages 1089 – 1090. Georgia completed therapy the next week. She'd just given another tremendously successful presentation at work and was on cloud nine. The treatment only required a few sessions, and most of the techniques on the Recovery Circle weren't necessary. Occasionally, you'll have highly motivated patients like Georgia who work hard in therapy. The good news is that these patients are rewarding to work with, and will often recover quickly. The bad news is that when they recover, they have no need for further treatment, and so you lose them just about the time you're getting to know and like them. I received a warm and enthusiastic thank you note from Georgia several months later. She wanted me to know she was still on a high. She'd completed her executive-training program, and had accepted an attractive job offer from her company. Apparently, she'd become such a charismatic public speaker that she'd been asked to head up the public speaking training program for all the executives and trainees employed by her company around the United States.
Chapter 29
Page 1088
This type of outcome is not unusual. When patients conquer fears that have intimidated them for many years, the thing they feared often becomes a source of deep satisfaction or even exhilaration.
Chapter 29
1089
Georgia's Daily Mood Log* Upsetting Event: Having to give a talk in front of my colleagues at work. Emotions
% Before
% After
Emotions
% Before
% After
Anxious
100%
10%
Discouraged
60%
0%
Ashamed
75%
0%
Frustrated
75%
0%
Embarrassed
100%
10%
Inadequate
90%
0%
% Before
% After
1. My mind might go blank. I might forget what I'm speaking about.
100%
2. Someone might know more than me and ask a really hard question.
3. People might get bored.
Negative Thoughts
% Belief
Distortions
Positive Thoughts
20%
AON; DP; FT; MAG; ER; SH
1. I've never once forgotten what I was talking about during a presentation. But if I do get lost, I can just glance at my outline, which will be right in front of me.
100%
90%
10%
DP; MR; FT; MAG; ER; SH
2. This is my area of expertise, and I'll definitely know more than most of the people in the audience. If someone asks a difficult question, I can simply say that I don't know the answer. No one expects me to know all the answers.
100%
90%
30%
AON; OG; DP; MR; FT; ER; SH
3. I've gotten good feedback about nearly all my presentations so far. But there's always room for improvement.
100%
* Copyright
2004 by David D. Burns, M.D.
Chapter 29
1090 Georgia's Daily Mood Log (cont'd)
Negative Thoughts
% Before
% After
4. They'll see how nervous I am.
100%
10%
AON; OG; DP; MR; FT; ER; SH; SB
5. My colleagues will think I'm an idiot.
80%
0%
6. I might faint when I give my presentation.
100%
10%
Distortions
Positive Thoughts
% Belief
4. No one has ever said that I looked nervous before, but even if they did, would it be the end of the world?
100%
AON; OG; DP; MR; FT; ER; SH; LAB; SB
5. I don't believe that any of my colleagues think I'm an idiot. I've always received lots of positive feedback from them. Even if I do give a mediocre presentation from time to time, they'll probably just assume I'm human.
100%
MF; DP; FT; MAG; ER; SH
6. I could faint, since I did faint once, but it's not likely, since I've given so many presentations without fainting. Furthermore, I have some new tools to prevent fainting, like walking in place when I stand up. Even if I did faint, it wouldn't be the end of the world. If that's the worst thing I ever have to worry about, I'll be in good shape!
100%
30*
Driving Phobia— The Woman with Rubbery Legs
A psychologist named Kim approached me during a break at one of my Scared Stiff workshops and asked if I could give her some tips on how to overcome her driving phobia. She told me she was the most anxious when she had to drive across bridges. This was particularly inconvenient because there were lots of bridges near her home in Berkeley, California. Kim had been working on a Daily Mood Log during the workshop. As you can see on pages 1093 – 1094, the upsetting event was simply, "Thinking about driving over a bridge." She felt unhappy, anxious, panicky, ashamed, defective, foolish, discouraged, stuck, annoyed and trapped, and had six negative thoughts: 1. My hands are too wet and weak to hold the steering wheel. 2. My legs feel like jelly. They're so rubbery that I won't be able to use the brakes or gas pedal.
* Copyright
2004 by David D. Burns, M.D.
Chapter 30
Page 1092
3. I'm too dizzy to focus and concentrate. 4. I'll harm innocent people. 5. The bridge is even more unstable than I am and will probably collapse. 6. What's wrong with me? I should be over this by now! There are really two parts to her problem: the anxiety itself, and the shame she feels about the phobia. The anxiety results from the first five negative thoughts, and the shame results from the sixth thought. If you were treating Kim, you'd need to do two Recovery Circles, one for the anxiety, and one for the shame. We'll focus on the anxiety here. I've put Kim's first negative thought in the middle of the Recovery Circle on page 1095. Select a variety of techniques that might help her put the lie to this thought, and write their names in the boxes around the circle. You can consult the list of techniques on page 1069. When you're done, you can turn to page 1096 to review the techniques I selected.
Chapter 30
1093
Kim's Daily Mood Log* Upsetting Event: Thinking about driving over a bridge. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
35%
Embarrassed, foolish, humiliated, self-conscious
95%
Anxious, worried, panicky, nervous, frightened
85%
Hopeless, discouraged, pessimistic, despairing
80%
Guilty, remorseful, bad, ashamed
50%
Frustrated, stuck, thwarted, defeated
100%
Inferior, worthless, inadequate, defective, incompetent
65%
Angry, mad, resentful, annoyed, irritated, upset, furious
50%
Lonely, unloved, unwanted, rejected, alone, abandoned
—
Other (describe) Trapped
90%
Negative Thoughts
% Before
1.
My hands are too wet and weak to hold the steering wheel.
100%
2.
My legs feel like jelly. They're so rubbery that I won't be able to use the brakes or gas pedal.
100%
3.
I'm too dizzy to focus and concentrate.
100%
% After
* Copyright
Distortions
2004 by David D. Burns, M.D.
Positive Thoughts
% After
% Belief
Chapter 30
1094 Kim's Daily Mood Log (cont'd)
Negative Thoughts
% Before
4.
I'll harm innocent people.
100%
5.
The bridge is even more unstable than I am and will probably collapse.
100%
6.
What's wrong with me? I should be over this by now!
100%
% After
Distortions
Positive Thoughts
% Belief
Checklist of Cognitive Distortions* 1.
All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6.
Magnification and Minimization. You blow things out of proportion or shrink them.
2.
Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7.
Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3.
Mental Filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4.
Discounting the Positive. You insist that your positive qualities don't count.
9.
Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
Chapter 30
1095
Kim's Recovery Circle*
16
15
1
14
2
13 12 11
3
My hands are too wet and weak to hold the steering wheel. 100%
4 5
10 6 9
* Copyright © 2004 by David D. Burns, M.D.
8
7
Chapter 30
Page 1096
Empathy My Recovery Circle appears on page 1097. Once again, I started with Empathy. It will be important to acknowledge the intensity of Kim's fear, as well as the shame she feels, before you try to help her. I've had to overcome a few phobias of my own over the years, including public speaking anxiety and shyness, as well as the fear of heights, blood, bees, and dogs, so I may be able to normalize her feelings by sharing my own experiences. Therapeutic selfdisclosure can be helpful if it's done skillfully. Patients like to hear that you've been there yourself because it makes you seem human and gives you credibility. At the same time, they want to know that you've conquered the problem and can guide them out of the woods as well. Empathy will be important because you're going to ask Kim to confront her fears using Exposure Techniques. She'll have to trust you in order to endure the intense anxiety that will be involved. If she senses a lack of warmth or acceptance, she may dig in her heels and resist your efforts. Agenda Setting What will Kim bring to the table if you agree to help her with her phobia? Does she just want to talk about her fears, or does she want to overcome them? Talking about her fears or exploring the past probably won't get the job done, and we can't make her anxiety go away by magic. Would she be willing to work with the DML between sessions, and confront her fears as well?
Chapter 30
1097
Kim's Recovery Circle* Hidden Emotion
Flooding
Gradual Exposure
Empathy
16
15
Agenda Setting 1
14 Image Substitution
12
Cognitive Flooding
2
13
11 What-If Technique
Identify the Distortions 3
My hands are too wet and weak to hold the steering wheel. 100%
Straightforward Technique
4 5
10
Cost-Benefit Analysis
6 Experimental Technique
9
8
Externalization of Voices * Copyright © 2004 by David D. Burns, M.D.
7
Double Standard Technique Examine the Evidence
Socratic Method
Chapter 30
Page 1098
Identify the Distortions The negative thought in Kim's Recovery Circle is a classic example of Fortune-Telling, Magnification, and Emotional Reasoning. These three distortions are associated with practically every form of anxiety. She's also involved in the Mental Filter and Discounting the Positive, because she focuses on the fact that her hands are sweaty, and overlooks the fact that she's never actually had an accident or lost control of her car. Identifying the distortions will help Kim see how illogical her thoughts are. When she feels anxious, the thoughts swirl through her mind so fast that she never has the chance to put them in perspective. Once you've pinpointed the distortions in her thoughts, you'll get lots of ideas about techniques you could use to help her challenge them. Straightforward Technique You can say, "Kim, you're telling yourself that you'll lose control of the car on the bridge because your hands will be so slippery and your legs will be too weak to press the pedals. We know that these thoughts create intense anxiety and contain lots of distortions as well. Can you think of a way to talk back to these thoughts? Is there another message you could give yourself that would be more positive and realistic?" Kim might say, "Well, I could tell myself that I might make it across the bridge, since other people seem to get across safely." This thought probably won't be effective because it won't put the lie to her belief that she's going to lose control and crash. The fact that other people can get across safely will probably be irrelevant to her.
Chapter 30
Page 1099
Cost-Benefit Analysis (CBA) On page 1100, Kim listed all the advantages and disadvantages of believing that she wouldn't be able to hold the steering wheel or control the car if she drove across a bridge. She decided that the disadvantages slightly outweighed the advantages of this belief, so she put a 55 and a 45 in the two circles at the bottom. It was a close call because she still believed that she might lose control of the car if she tried to drive across a bridge. At the same time, her ratings indicated that she was motivated to overcome her phobia. What would you have done if the advantages of her belief had outweighed the disadvantages? Think about it for a moment before you read my answer. I hope the answer to that question was easy for you. Empathy is always your best bet when a patient expresses doubt. Listen and encourage Kim to express all her feelings of anxiety and fear. Provide support. Find some truth in what she's saying. Then you can paradox her. Why should she work hard to put the lie to this thought, given all the advantages of maintaining it? Double Standard Technique What would Kim say to a friend or patient with a driving phobia? Would she say, "You know, you might get so anxious that you'll lose control and drive right off the bridge? Perhaps it would make more sense not to try"? Why or why not? Would she be willing to talk to herself in the same way she'd talk to someone else with this problem?
Chapter 30
Page 1100
Kim's Cost-Benefit Analysis* Describe the thought or feeling you want to change: My hands are too wet and weak to hold the steering wheel. Advantages of Believing This 1. I won't have to confront my fear of driving across bridges. 2. If I don't drive across a bridge, I won't risk hurting anyone. 3. If I do drive, I won't get too relaxed or distracted and cause an accident. 4. If I stop worrying, something awful might happen. 5. My husband drives me everywhere, just like a chauffeur. 6. My family worries about me and gives me lots of attention. 7. If I get over my fear of driving across bridges, I might have to take on more responsibilities.
Disadvantages of Believing This 1. I feel trapped because I can't drive to lots of places I want to go to on my own. I always have to get my husband or a friend to drive me. 2. This makes me feel inadequate, like a child. 3. My husband and friends may feel that I'm a burden. 4. I feel ashamed and frustrated. 5. I'll feel terrified if I try to drive across a bridge. 6. I won't do what it takes to overcome my driving phobia because it seems too dangerous. 7. I'm not even convinced that this thought is true. 8. I lose out on opportunities to do new things and have fun.
45
* Copyright
55
1984 by David D. Burns, M.D.
Chapter 30
Page 1101
Examine the Evidence Kim reasons from how she feels. She feels like she won't be able to hold the steering wheel, so she thinks she really can't. But what do the facts show? Does water pour off her hands like Niagara Falls when she's anxious? Does she often drop things, like glasses, because her hands get so slippery? Kim also tells herself that the bridge is on the verge of collapse. But how many bridge collapses has she read about in her community in the past year? How about in the entire United States in the past 100 years?* And how many cars go across bridges every day? Has she lost friends who died while driving across bridges that suddenly collapsed? This type of analysis will help Kim see that she's been magnifying the danger. Although it's possible that a bridge could collapse, the probability is vanishingly small. Socratic Method You could ask a series of questions that will make Kim aware of the illogic in her fears. This therapeutic style can be powerful, but you'll have to be gentle and collaborative. Otherwise the patient might feel like you're arguing or putting them down. You might ask questions like these: Kim, it sounds like you're concerned about your hands sweating and getting slippery when you drive. Has that been your experience? Do your hands sweat a great deal? Have they ever gotten so wet and slippery when you were driving that you couldn't turn the steering wheel, no matter how hard
Chapter 30
Page 1102
you tried? If you stuck your hands in a tub of water just before you got in the car to drive, so they were soaking wet, do you believe that you wouldn't be able to hold on to the steering wheel or turn the car properly? What's the steering wheel made of? Is it something really slippery, like plastic? Have you ever lost control of a car and driven off a bridge because you couldn't turn the steering wheel or use the brakes? Do your legs get so rubbery that you collapse when you try to walk? Have you ever been unable to apply the brakes or the accelerator, no matter how hard you pushed? Obviously, there's some humor in this approach. Humor can provide relief if the patient is laughing with you, and feels like you're on the same team. However, if the patient feels that you're laughing at them or belittling them, it will definitely backfire. Externalization of Voices You can play the role of Kim's negative thoughts and attack her in the same way that she attacks herself, by saying things like this, "Boy, you'd better not drive over that bridge. Your hands will get so sweaty that you won't even be able to hold the steering wheel." Kim can play the role of the positive thoughts and say things like, "That's just emotional reasoning. I will get nervous at first, and my hands may even sweat, but I'll still be able to hold the steering wheel and * Many people are familiar with the dramatic footage of the famous Tacoma Narrows Bridge Disaster of November 7, 1940. It shook apart due to wind-induced harmonic vibrations and
Chapter 30
Page 1103
drive the car properly. Your criticism is just a lot of malarkey." If she isn't able to come up with convincing responses, you can do a role-reversal and model more effective responses. For Kim's driving phobia thoughts, the Self-Defense Paradigm will probably be far more effective than the Acceptance Paradox. In other words, when you're playing the role of her positive thoughts, you wouldn't want to say, "It's true that I won't be able to hold the steering wheel, and I probably will drive off the bridge and kill a bunch of people, but hey, I can accept death!" Experimental Technique Kim could do small experiments while driving to test the validity of the messages she's giving herself. For example, she could keep a paper towel in the car, and grab it from time to time to see how much water it absorbs from her hands. She could test her belief that she can't control the car by looking in the rearview mirror, signaling, and changing lanes. She could test the belief that her legs are too rubbery to use the pedals by speeding up and slowing down. This is a cognitive intervention as well as a form of exposure, because she'll be confronting her fears and putting the lie to her negative thoughts at the same time. Kim could test her belief that the bridge is in danger of collapsing by walking on it, jumping up and down, and stomping her feet as hard as she can. She can also shake the girders and pound on them with her fists to see if she can topple the bridge. What-If Technique
poor design. However, bridge collapses are exceedingly rare.
Chapter 30
Page 1104
Ask Kim to draw a downward arrow under one of the negative thoughts on her Daily Mood Log, such as, "My legs feel like jelly. They're so rubbery that I won't be able to use the brakes or gas pedal." Then you can ask a question along these lines: "Kim, what if that were true? Imagine that you were driving over a bridge and your legs got so weak and rubbery that you actually couldn't use the brakes. What are you the most afraid of? What's the worst thing that could happen?" A frightening thought or fantasy will pop into her mind. For example, she may fear smashing into other cars and plunging into the river. Ask her to write this down and put another downward arrow underneath it. Then ask a similar question. If you repeat this process several times, it will lead to the most frightening fantasy at the root of her fears. Cognitive Flooding Kim obviously can't drive off the bridge and plunge into the river in order to confront her fears! However, she can confront her most terrifying fantasy in her mind's eye using Cognitive Flooding. For example, if she's afraid of plunging into the river and drowning, she can picture this and try to make herself as anxious as possible. If her anxiety levels skyrocket, it means that you're probably on the right track. If Kim sticks with the fantasy, the odds are high that her anxiety will eventually disappear. This sometimes happens quickly, but it may require several hours of exposure. Image Substitution At the height of her anxiety, Kim can substitute a more positive fantasy, such as arriving safely on the other side of the bridge and feeling a deep sense of pride and accomplishment. She could also substitute a happy memory from
Chapter 30
Page 1105
her past. She can practice Image Substitution every night before she goes to sleep. First, she can flood herself with frightening fantasies, and then she can switch to a positive, peaceful image. Over time, the frightening fantasies will probably lose their power to intimidate her. Gradual Exposure Kim could develop a Fear Hierarchy, like the one on page 1106. Level 1 involves getting into the car, starting it, and getting familiar with the steering wheel and controls, without any actual driving. Once she's comfortable with Level 1, she can progress to the next level on her hierarchy. She can continue to work on each level at her own pace until she reaches Level 10, driving across a long bridge alone during rush hour traffic. Kim could keep track of her progress on the Exposure Log on page 1107. There are many ways you and Kim could set up her Fear Hierarchy. For example, Level 1 could be watching a movie that involves cars driving across bridges. Once it no longer frightens her, she can move up her hierarchy. Level 2 might involve watching the film of the famous Tacoma Narrows Bridge collapse of 1940, which she can easily find online. Once this footage no longer frightens her, she can move up to Level 3, which might involve standing on a bridge, or even walking across a bridge. Kim can put anything on her Fear Hierarchy that makes sense to her. The important thing is to start with something that feels relatively safe, and then slowly move up to more and more challenging activities.
Chapter 30
Page 1106
Kim's Fear Hierarchy Instructions. Develop a hierarchy of feared situations. List the least frightening situation first, and the most frightening situation last. Describe your phobia: Driving, especially over bridges. Level
Description
1
Sit in the driver's seat of the car, turn the engine on and off, practice turning the steering wheel and pressing on the accelerator and brake pedals.
2
Drive down the driveway.
3
Drive around the empty parking lot next to our home on the weekend.
4
Drive around the block with my husband in the car.
5
Drive around the block without my husband in the car.
6
Drive to the supermarket on my own.
7
Drive across a short bridge with my husband in the car.
8
Drive across a long bridge, like the Bay Bridge, when there isn't much traffic, with my husband in the car.
9
Drive across a long bridge, like the Bay Bridge, when there isn't much traffic, without my husband in the car.
10
Drive across the Bay Bridge on my own during rush hour.
Chapter 30
Page 1107
Exposure Log Instructions. Rate your anxiety at the beginning and end of each exposure session on a scale from 0% (no anxiety) to 100% (sheer terror or panic). Describe any frightening thoughts or fantasies you have. Date
Hierarchy Level
Time Spent
Anxiety at Start (0%–100%)
Anxiety at End (0%–100%)
Frightening Thoughts and Fantasies
Chapter 30
Page 1108
Flooding Instead of progressing slowly up her Fear Hierarchy, Kim would start out at Level 9 or 10. This would be a more frightening approach, but would probably work much more quickly. You can present her with both options and pursue the method she feels more comfortable with. Hidden Emotion Is there a hidden problem or feeling that Kim hasn't acknowledged? For example, what would happen if she got over her phobia and could easily drive across bridges? Is there something on the other side of the bridge that she's trying to avoid? Would she get to spend less time with her husband because he'd no longer be chauffeuring her around? If she can bring the hidden problem to conscious awareness and deal with it, you may see a dramatic reduction in her driving phobia. When I was a research fellow, I worked with a brilliant young scientist named Fred. Fred was one of the most down-to-earth, enthusiastic, happy people I've ever known. He was a good friend and a superb researcher, and we did some exciting work together. One day, while we were walking to the computer center, I noticed that Fred seemed upset. I could see that there were tears in his eyes, and I asked if everything was okay. He said that he thought he might be depressed and wondered if he could schedule a few sessions to talk with me as a psychiatrist. This was a surprise, because it seemed like everything was going great for him, and he seemed like the last person in the world who'd ever get depressed. I told
Chapter 30
Page 1109
Fred that I couldn't ethically treat a friend, but if we talked a little bit about the problem, I might be able to refer him to a colleague I respected. We sat down on the grass in front of the computer building and Fred explained that'd he'd received a disturbing letter that morning. He handed it to me. The letter contained a phenomenal job offer to become the director of research at a prestigious laboratory in San Francisco. I told Fred that I was puzzled, since most people would be thrilled to receive such an offer at the beginning of their career. Fred stared at the grass and said he had something to confess that he was very embarrassed about. He said he had a bridge phobia, and the moment he read the letter, he felt overwhelmed. He said that living in San Francisco sounded like a nightmare, because of all the bridges there. He was absolutely terrified by the idea of having to cross the Golden Gate Bridge, the Bay Bridge, and the San Mateo Bridge. If you were Fred's therapist, how would you use the Hidden Emotion Technique to help him with his bridge phobia? Put on your detective cap and ask yourself if there's some feeling or problem that's bugging him. What is he trying to tell us? Put your ideas here before you turn the page:
Chapter 30
Page 1110
Answer I told Fred that he didn't sound excited about the job, even though it was clearly a fantastic offer, and asked if he really wanted to move to San Francisco. He explained that he and his wife were both fifth generation Philadelphians, and he'd always assumed that he'd raise his family in Philadelphia. He said that he'd never had any interest in moving to the West Coast, but felt obligated to accept the offer. I asked him why he felt that way. He said that if he turned it down, his family, friends and colleagues would think he was nuts to let such a tremendous opportunity slip through his fingers. He was worried that I'd be disappointed in him as well. In addition, this was his first job offer, and he was concerned that he might not get any others. I told Fred that if he decided to stay in Philadelphia, I'd be thrilled because we could keep working together. I pointed out that life was short, and ultimately, he had to please himself. I suggested that he might also be involved in some mind-reading, and making assumptions about how other people thought and felt about him. Finally, I asked Fred why he thought that he wouldn’t get any other good job offers. I reminded him that he was one of the most highly regarded young scientists in the country, and had recently published several important articles in prestigious journals. I told him that I thought he'd get lots of great offers, and could probably afford to pick and choose something that really appealed to him. Fred said he felt immediately relieved. Later that day, he talked things
Chapter 30
Page 1111
over with his wife and decided to decline the offer. He felt exhilarated, and said the funniest thing was that his bridge phobia mysteriously disappeared, and that he'd driven across the Ben Franklin Bridge with no problems at all. Fred eventually accepted a prestigious position with an excellent research laboratory near his home. Why didn't Fred just admit that he didn't want to move to San Francisco? Why did his bridge phobia flare up instead? Fred was busy telling himself that he should accept the offer. He felt like he didn't have the right to say, "I'm sorry, but I've decided not to relocate to the West Coast." His anxiety did the talking for him. When he brought the hidden feelings to conscious awareness and acted on them, his phobia suddenly disappeared. Does this mean that a hidden problem or feeling is always lurking underneath a phobia? Sometimes, a phobia is just a phobia, and nothing more. But when there is a hidden feeling, then your attempts to overcome the problem with straightforward CBT techniques may fall short, because the patient needs the phobia. And when you tune in to the message that the patient is trying to convey, the problem will suddenly fall into a radically different perspective.
31*
Performance Anxiety—The Therapist Who Thought She Was a Fraud
Imagine that you're treating a young man named Barry who suffers from paranoid schizophrenia. You've already completed the intake evaluation. At the start of today's session, Barry tells you that your receptionist is eavesdropping on the conversation. He's convinced that she can hear all his thoughts and insists that she's trying to control his mind with a secret electronic device. He seems mistrustful, anxious, frustrated, and angry. How will you help him? Recent studies suggest that CBT can be very useful in the treatment of schizophrenia. But we have 50 techniques available. Which ones will you use? Review the list on page 1120 and put your ideas here:
* Copyright
2003 by David D. Burns, M.D.
Chapter 31
Page 1113
Answer If you decided to start with Empathy and Agenda Setting, you get an A+! These are the only techniques that will have any value at this point, because Barry hasn't yet asked for help. We don't know what, if anything, he wants help with. If you try to challenge his delusions, he'll see you as another enemy and resist your efforts. I could have asked you this question instead: "How would you treat a patient with OCD?" Or, "What techniques would you select for a patient with PTSD," or for any disorder, but the answer will always be the same. You'll need to develop a trusting therapeutic alliance and a collaborative agenda with every patient or you won't get anywhere. Barry has to feel that you support him and can see the world through his eyes. Your best listening skills will be crucial, especially the Disarming Technique. But how in the world can you find any truth in his bizarre statements? Let's give it a try. Barry says, "I know that your secretary, Margarita, is spying on us. She's taking notes on everything we're saying right now. She's an undercover agent for the FBI." What will you say next? Use the Five Secrets of Effective Communication. Make sure that you include the Disarming Technique in your response. Remember that the Disarming Technique means that you find real truth in what Barry is saying, and you don't simply give his statement lip service. You have to agree that he really is right about something. Put your response to Barry below, and record the names of the techniques you're using in parentheses following each sentence you write.
Chapter 31
Page 1114
Chapter 31
Page 1115
Answer You could say something like this: Barry, that sounds disturbing. (FE) I'm concerned that Margarita and I haven't done a very good job of making you feel safe or protected. (DT; FE) You're absolutely right, too. (DT) I've sensed some tension in the air as well. (IF; DT) If you feel like you can't trust me, it will be awfully hard to open up. (FE) What you're saying is important. (ST; DT) Can you tell me a bit more about how you're feeling? (IN) Did Margarita or I say or do something that seemed unprofessional or turned you off? (IN) If you say this with warmth and humility, the odds are high that Barry will relax and open up. Now review your response. Did you find real truth in what Barry said? Or did you say something patronizing like, "I can see how you might feel that way"? I don't mean to cast stones, but rather to emphasize that it takes lots of practice to learn to use the Disarming Technique skillfully. If you don't hit the mark and find genuine truth in Barry's complaints, he'll see through you. Then he'll feel annoyed and become even more mistrustful. Barry may feel lonely. He sounds crazy, and rarely has meaningful conversations with anybody. Most people write him off because they find him threatening and can't hear the truth behind his wildly delusional statements. If you disarm him skillfully, you'll greatly enhance your chances of working with him successfully. After you've empathized, you can ask Barry if there's something specific he wants help with. This is the Invitation step of Agenda Setting. He may want help with depression, dating, or procrastinating on his schoolwork. It could be
Chapter 31
Page 1116
anything. He probably won't ask for help with his delusions, but that's not important. What is important is that you can form a therapeutic alliance and work together on something that makes sense to him. In most cases, the intensity of the schizophrenia fluctuates with the patient's mood. Once you help Barry develop better self-esteem, and you start to see reductions in his depression, anxiety and anger levels on the Brief Mood Survey, you'll see a significant reduction in the symptoms of schizophrenia as well. But this will only happen if you have a trusting relationship and a meaningful therapeutic agenda. Now I'll describe ten patients with a variety of Axis I and II disorders. I'll tell you exactly how each patient was thinking and feeling. When you review each case, ask yourself how you'd treat that patient. What techniques would you try from the list of 50 Ways to Untwist Your Thinking? We'll do the first case together. Case #1. Performance Anxiety with Feelings of Inferiority In Chapter 21, you read about Tracy, a psychology graduate student who felt insecure about her skills as a therapist. Her negative feelings became quite intense during the role-playing exercises in class. Perhaps you've also felt this way from time to time. I know I have! Working through these experiences can make you a far more caring and effective therapist, because you'll see similar thinking patterns in your patients practically every day. A psychology graduate student named Gwen also felt anxious and insecure during the class role-playing exercises. She was telling herself: 1. I'm not as smart as I should be.
Chapter 31
Page 1117
2. I should be able to help more of my patients. 3. Everyone else seems to be catching on more quickly. 4. I have the same kinds of problems as my patients! I should have it all together by now. 5. Pretty soon, my patients and colleagues will see that I'm a fraud. You can see Gwen's Daily Mood Log on page 1118. I've put her first negative thought in the center of the Recovery Circle on page 1119. Select a variety of techniques that might help her put the lie to this thought, and put one technique in each of the boxes around the Recovery Circle. You can review the brief list of techniques on page 1120 or the longer list that starts on page 522. When you're done, you can turn to my analysis on page 1121.
Chapter 31
1118
Gwen's Daily Mood Log* Upsetting Event: Role-playing how to respond to an angry patient during group supervision. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
35%
Embarrassed, foolish, humiliated, self-conscious
65%
Anxious, worried, panicky, nervous, frightened
85%
Hopeless, discouraged, pessimistic, despairing
75%
Guilty, remorseful, bad, ashamed
50%
Frustrated, stuck, thwarted, defeated
90%
Inferior, worthless, inadequate, defective, incompetent
65%
Angry, mad, resentful, annoyed, irritated, upset, furious
30%
Lonely, unloved, unwanted, rejected, alone, abandoned
35%
Other (describe)
Negative Thoughts
% Before
1.
I'm not as smart as I should be.
100%
2.
I should be able to help more of my patients.
100%
3.
Everyone else seems to be catching on more quickly.
100%
4.
I have the same kinds of problems as my patients! I should have it all together by now.
100%
5.
Pretty soon, my patients and colleagues will see that I'm a fraud.
100%
* Copyright
% After
Distortions
1984 by David D. Burns, M.D. Revised 2003.
Positive Thoughts
% After
% Belief
Chapter 31
1119
Gwen's Recovery Circle
16
15
1
14
2
13
3
12 11
I'm not as smart as I should be. 100%
4 5
10 6 9
8
7
Chapter 31
Page 1120
50 Ways to Untwist Your Thinking* Basic Techniques
Exposure Techniques
Role-Playing 19. Externalization of Voices
Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques
Philosophical / Spiritual 21. Acceptance Paradox
Compassion-Based
Visual Imaging
5. Double Standard Technique
Truth-Based 6. Examine the Evidence
8. Survey Technique 9. Reattribution
39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
7. Experimental Technique
Cognitive Exposure
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Motivational Techniques
Semantic 12. Semantic Method 13. Let's Define Terms
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
14. Be Specific
Quantitative
30. Devil's Advocate Technique
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Chapter 31
Page 1121
Answer Gwen's Recovery Circle appears on page 1124. Empathy will be crucial, because Gwen feels ashamed and alone. Your support will be a great help to her. Agenda Setting will also be important. The Agenda Setting question would be this: "Gwen, if we could make all of your feelings of inadequacy and self-doubt disappear, and you could walk out of today's session feeling joyful and confident, would you want that result?" Although "yes" might seem like the obvious answer, I wouldn't be so quick to jump to that conclusion. Gwen may be reluctant to let go of her negative thoughts and feelings for many reasons, including: She may think that her constant self-criticisms will motivate her to stay on her toes and do her best work. She may think that if she lets up on herself, something terrible will happen, or she'll have to settle for mediocrity. She may think that her negative thoughts are realistic, and that she deserves to feel inadequate because she really is inadequate. She may think that if she criticizes herself, other people won't. In fact, they may reward her with praise and reassurance. She may think that she isn't entitled to feel happy and confident until she's doing outstanding work with all her patients. She may think of self-esteem and peace of mind as rewards that she must earn, rather than gifts she can give herself unconditionally. These would all be examples of Outcome Resistance. Gwen might have
Chapter 31
Page 1122
some Process Resistance as well. In other words, even if she wants to get better, she may feel some reluctance about doing the things she'll have to do in order to overcome her fears. In this case, the Agenda Setting question might be, "Gwen, what would you be willing to bring to the table if I agreed to work with you on this problem? Would you be willing to do homework between sessions, like working with the Daily Mood Log? Would you also be willing to do some things that might seem risky or anxiety-provoking?" The answers to these questions will show you whether or not Gwen is motivated to work on solving this problem. Identify the Distortions is the third technique on Gwen's Recovery Circle. The thought, "I'm not as smart as I should be," is a classic Should Statement. It's also an example of All-or-Nothing Thinking, Overgeneralization, Mental Filter, Discounting the Positive, Jumping to Conclusions, Emotional Reasoning, and Self-Blame. Once you've identified the distortions in a thought, you can consult the table on 941 to get some good ideas on how to attack it. The Semantic Method is a great choice for Should Statements, so I've included it early on my Recovery Circle. Be Specific can be helpful for Overgeneralizations, and Examine the Evidence can be useful for Jumping to Conclusions, so I've included these techniques as well. The Straightforward Technique appears fourth on Gwen's Recovery Circle. We know that it's not usually effective, but it's always worth a try. Even if Gwen can't come up with an effective positive thought, we'll see why she gets stuck when she tries to wrestle with the feelings of inadequacy on her own. In the table on pages 1125 – 1126, I've included brief descriptions of how
Chapter 31
Page 1123
the rest of the techniques on Gwen's Recovery Circle would work. Don't worry if your own selection of techniques differs from mine. There's no single solution or correct way to approach any patient or problem. The most important thing is to use a wide variety of techniques, because there's no way of knowing in advance which technique will work for any patient. The techniques I've listed are merely a way of getting the therapy off to a good start. There will probably be some unexpected discoveries and twists and turns in the road along the way, and you may suddenly find yourself heading off in another direction. Good therapy involves a skillful integration of spontaneity and structure. If you stick too closely to the script in your mind, you may miss your best opportunity to connect with the patient in a deep and meaningful way.
Chapter 31
1124
Gwen's Recovery Circle Five Secrets
Empathy
Hidden Emotion
Thinking in Shades of Gray
16
15
Agenda Setting 1
14
11 Acceptance Paradox / Feared Fantasy
Identify the Distortions 3
12
Self-Disclosure / Survey Technique
2
13
Be Specific
I'm not as smart as I should be. 100%
Straightforward Technique
4
Cost-Benefit Analysis
5
10 6
Externalization of Voices
9
8
7
Semantic Method
Double Standard Technique
Downward Arrow Technique Examine the Evidence
Chapter 31
1125 Techniques on Gwen's Recovery Circle
Cost-Benefit Analysis
Gwen can list the advantages and disadvantages of believing the thought, "I'm not as smart as I should be." How will it help her, and how will it hurt her? A Straightforward or Paradoxical CBA will help you assess Gwen's motivation.
Semantic Method
Gwen can modify the harsh language she uses when she thinks about her shortcomings. She could tell herself, "It would be great to be so incredibly smart that I learned everything quickly and without effort, but I'm human. Intelligence is important, but compassion, hard work and creativity are also crucial to good clinical work." This message is more realistic and will take the sting out of the negative thought.
Double Standard Technique
What would Gwen say to a classmate who was struggling with feelings of insecurity? Would she be as hard on her as she is on herself? Why or why not? Would she be willing to talk to herself in the same compassionate way she'd talk to a friend who was feeling anxious?
Examine the Evidence
Gwen is reasoning from how she feels. She feels inadequate, so she thinks she really is inadequate. But what do the facts show? How is she doing in her classes? How do her patients rate her on the Therapeutic Empathy and Helpfulness scales? Do their session-by-session scores on the Brief Mood Survey indicate that some of them are making progress?
Downward Arrow Technique
Any of the Downward Arrow Techniques could be useful, including the Individual Downward Arrow, the Interpersonal Downward Arrow, and the What-If Technique. These techniques will lead to the Self-Defeating Beliefs that trigger Gwen's feelings of insecurity, such as Perfectionism, Perceived Perfectionism, the Achievement Addiction, the Approval Addiction, and the Brushfire Fallacy, among others.
Externalization of Voices
This technique, more than any other, transforms intellectual understanding into real emotional change at the gut level. You can play the role of Gwen's negative thoughts and attack her in the same way that she attacks herself, using the first person, "I," or the second person, "You." She can play the role of her negative thoughts and defend against your attack, using the first person, "I." If she gets defensive, falters, or responds in an ineffective way, you can do a role-reversal so you can model a more effective response. When you're in the positive thoughts role, you can use the Self-Defense Paradigm, the Acceptance Paradox, or a combination of the two. The kinds of thoughts that plague Gwen almost always respond far better to the Acceptance Paradox. For example, Gwen tells herself that she should be able to help more of her patients. Instead, she could remind herself that she's still a beginner, that she's learning all the time, and that there will always be lots more to learn, even when she's a seasoned veteran.
Chapter 31
1126 Techniques on Gwen's Recovery Circle (cont'd)
Acceptance Paradox / Feared Fantasy
Instead of struggling with feelings of inadequacy, Gwen could simply accept the fact that there are always going to be lots of people who are smarter and more talented than she is. This message can lead to a sense of inner peace. The Acceptance Paradox only comes to life during a role-playing technique like the Externalization of Voices or the Feared Fantasy. In the Feared Fantasy, Gwen would enter an Alice-in-Wonderland nightmare world where her worst fear comes true. She meets a Classmate from Hell who is far smarter and more talented than she is. The Classmate from Hell berates Gwen and threatens to tell everyone what a hopeless loser she is. If Gwen responds with the Acceptance Paradox, she can easily make a monkey out of the Classmate from Hell. This will show her that the social ostracism and disapproval she's always feared aren't really threats at all.
Self-Disclosure / Survey Technique
Gwen could tell one or two classmates that she feels anxious during the role-playing exercises in class, and ask if they've ever felt this way.
Be Specific
This technique can be useful for Overgeneralization and All-or-Nothing Thinking. Gwen writes herself off in a global way because she thinks her therapy skills aren't up to speed. She thinks she's either smart or dumb, skillful or clumsy, a success or a failure. But what are her specific strengths and weaknesses? Does she need to develop more refined listening skills or Agenda Setting skills? Once she focuses on a real and specific deficiency, it becomes far less threatening and much easier to deal with.
Thinking in Shades of Gray
Once Gwen begins to focus on improving specific therapy skills, such as empathy, she could rate herself on a sliding scale, between 0% and 100%, rather than thinking about herself in an All-or-Nothing way.
Hidden Emotion
Is Gwen upset about something that she's not telling us? For example, is she frustrated with an oppositional patient or annoyed with a classmate? Does she have mixed feelings about going into psychology? Does she feel upset about spending so little time with her husband because of all the pressures of school? Bringing these problems out into the open can often put the anxiety into a radically different perspective and lead to rapid relief.
Five Secrets of Effective Communication
Gwen believes that she has to impress her patients, classmates and professors with a superb performance in order to get them to like and respect her. This is going to put her under extreme pressure. An alternative strategy would be to solicit negative and positive feedback from other people, and to respond with the Disarming Technique, Thought and Feeling Empathy, Inquiry, "I Feel" Statements, and Stroking. This will give her some real data about her strengths and weaknesses so she can learn and grow. It will also allow her to develop far more vibrant and meaningful relationships with other people.
Chapter 31
Page 1127
On the following pages, you'll find nine additional cases covering a variety of Axis I and II problems. Choose a problem that interests you, and put one of the patient's negative thoughts in the middle of the Recovery Circle on page 1133. Select a variety of techniques that might help the patient, and put one technique in each of the boxes around the circle. If you come up with more than 16 techniques, that's great. It means that you'll have even more firepower available. You can put the additional techniques on the second Recovery Circle on page 1134. Feel free to make extra copies of the Recovery Circle if you need them. I like to photocopy the one-page overview of the 50 CBT techniques on the back of the Recovery Circle so I can simply turn the page over and review the list. This makes it easy to select a variety of helpful techniques. If you're ever in doubt about how a technique might work, you can consult the detailed list of techniques that starts on page 522. If you're teaching psychotherapy techniques and using this book in your class, you can have the students break into groups of two or three to do this exercise. Each group can select the case they want to work on. After 20 minutes, a spokesperson from each group can report back on the problem their group selected, and you can discuss how the techniques would work. You can also use role-playing to illustrate how you'd use techniques like Empathy, Agenda Setting, the Double Standard Technique, and the Externalization of Voices. In my work with the psychology students and psychiatric residents at Stanford, this has been one of the most useful and
Chapter 31
Page 1128
entertaining teaching methods. In fact, you could easily base many productive and highly educational classes on the vignettes in this chapter. Keep in mind that there are no single "correct" solutions to these problems. The goal of the exercise is to think about how you'd approach each case, and how you'd bring a wide variety of techniques to life for that patient. Don't feel like you have to work on all these cases at once. Try one or two, and give yourself time to digest what you've learned. Then try a few additional cases later on. Of course, you can begin to use the Recovery Circle with your own patients as well. With practice, your skills will increase dramatically. Case #2. Antisocial Personality Disorder Bennie was a violent, oppositional, severely depressed heroin dealer who was hospitalized for suicidal urges. During one of our inpatient CBT groups in Philadelphia, Bennie defiantly challenged me to show him how to put the lie to this thought: I'm a hopeless case, and there's nothin' you can do about it! 100% Case #3. Depression, Anxiety and Anger A physician named Rick was involved in a malpractice suit that had dragged on for years. He felt resentful because he was convinced the suit was without merit. However, he was advised to settle it because of the unfavorable climate for malpractice cases in Illinois. The cost of Rick's malpractice insurance had recently increased to $60,000 per physician, per year. Rick was the head of a clinic with eight doctors, and was outraged that they now had to generate nearly half a million dollars annually just to pay for their liability insurance.
Chapter 31
Page 1129
Rick had recently hired a new graduate from Stanford's internal medicine residency program. Rick became upset following a conversation with her because he noticed how high-powered she was. He felt inadequate, washed up, panicky, frustrated, angry, discouraged, and sad, and estimated all these feelings in the range of 70% – 100%. He had these negative thoughts: I don't know enough about my field. I'm over the hill. 90% My life is out of kilter. I have too many management responsibilities, and I've sacrificed all of my own time and personal interests for my career. 80% I didn't do anything wrong, so the lawsuit is unfair. 100% The plaintiff's attorneys are painting me as a terrible, callous person who didn't give my patient the proper care while he was in the hospital. 100% I'm trapped because all I know is medicine, and I can't get away from it now. 100% Case #4. Test Anxiety A young man named Aldo was studying to be a pilot and was anxious about his upcoming FAA examination. He felt nervous, inadequate, embarrassed, pessimistic, and frustrated, and was telling himself: I might fail the test and look bad in front of my peers. 90% Everything I've lived and worked for will go down the drain. 90% That would mean I'd wasted all my time and money. 80% Aldo's thoughts seemed unfounded, since he was at the top of his class. Case #5. Depression with Terminal Cancer A 44 year-old medical school administrator named Eva became
Chapter 31
Page 1130
depressed after she learned she had ovarian cancer and had only three years to live. Eva had never married, and was caring for three relatives with disabilities who lived with her. She was very active at the medical school and often went out of her way to help medical students and residents with their research projects. Eva felt guilty, worthless, hopeless, and anxious. Her negative thoughts included: I'm letting my family down. 100% They can't exist without me. 100% It's my fault I got cancer. 100% Case #6. Shyness and Inferiority Chuck was a single accountant who sought treatment for feelings of loneliness, inferiority and shyness. He was especially anxious because he had a congenital chest abnormality called "pectus excavatum." People with this problem have a breastbone with a sunken, concave appearance. Aside from this flaw, Chuck was tall, athletic, and reasonably good-looking. Chuck lived in Miami and wanted to be able to go to the beach and take his shirt off, but said he felt too embarrassed. His negative thoughts included: I'm inferior to all the other men who have such terrific physiques. 100% If I take off my shirt, everyone will stare at me and think I'm abnormal. 100% Case #7. Depression and Shame A documentary filmmaker named Abby had a history of chronic, recurrent depressions. Her depression lifted several weeks after I prescribed imipramine, an antidepressant that had helped her many years earlier. Abby felt ashamed about the improvement in her mood because she told herself:
Chapter 31
Page 1131
There must be something wrong with my brain. 100% This proves that I'm defective. 100% Case #8. OCD with a Handwashing Compulsion A woman named Gail had fairly severe OCD with a contamination phobia and a handwashing compulsion. She had the following thought over and over throughout the day: If I don't wash my hands, my children will die of leukemia. 100% Case #9. Depression Following Romantic Rejection A gay man named Thomas was rejected by the man he'd lived with for eight years. He was so ashamed that a month after the breakup, he still hadn't told his parents about it. When his ex-lover left town to celebrate his birthday with another man, Thomas felt depressed, guilty, worthless, lonely, humiliated, discouraged, defeated and resentful. He estimated all these feelings at 80% – 100%. He was telling himself: I'll never be in a loving relationship. 95% I must be impossible to live with and impossible to be in a relationship with. 95% There must be something wrong with me. 100% I've totally screwed up my life and flushed it down the toilet. 100% I'll end up an old, ugly, fat, gray-haired, lonely gay man. 100% Case #10. Binge Eating Disorder A woman named Cindy was diagnosed with Binge Eating Disorder. She felt agitated when a colleague threw a stale box of chocolates in the trash. The
Chapter 31
Page 1132
box was left over from the office New Year's Eve party a year earlier. Cindy felt tempted because she told herself: Mmmm, those chocolates would taste so good! 100% I'll go check it out. That couldn't hurt. 100% I could just eat one or two of them. 100% I can always skip lunch if I eat too much chocolate. 100% She also felt resentful because she told herself: She's got no right to throw away good food! 100% It's unfair! Other people can eat whatever they want and still be thin. 100% When no one was looking, Cindy snuck the box out of the trash and hid it in her desk. She started nibbling at the chocolates, and had soon devoured the entire box. Then she felt worthless, upset, frustrated, angry, and humiliated because she told herself: I just can't control myself. 100% I'm a fat pig! 100% I should be punished. 100% I shouldn't have given in. 100% I'll never lose weight. 100% If you're working with this problem, you can do three separate Recovery Circles: one for the tempting thoughts, one for the resentful thoughts, and one for the self-loathing thoughts. Each Recovery Circle will be quite different.
Chapter 31
1133
Recovery Circle
16
15
1
14
2
13
3
12
4
11 5
10 6 9
8
7
Chapter 31
1134
Recovery Circle (cont'd)
32
31
17
30
18
29
19
28
20
27
21
26 25
22 24
23
32*
Feeling Better vs. Getting Better— Relapse Prevention Training
Earlier in this book, I asked you to accept a basic fact about human nature: most human beings are inherently ambivalent about change. Once you really understand this idea, you'll be able to deal with therapeutic resistance much more easily. Now I'm going to ask you to accept another basic fact. All patients will relapse following their initial recovery. This will be true regardless of whether their initial problem involved depression, anxiety, anger, a habit or an addiction. There are no exceptions. No one can be happy all the time. Sooner or later, the same problem will return to plague the patient again. The relapse itself is not the problem. The real problem is the lack of acceptance and preparation. If patients accept the inevitability of relapses, and learn how to deal with them ahead of time, then they will lose their sting.
* Copyright
2004 by David D. Burns, M.D.
Chapter 32
Page 1136
When I was living in Philadelphia, I had a colleague named George Collette who was a practicing Buddhist. From time to time, George would mention Buddhist teachings, because he knew I was interested in the connections between Buddhist philosophy and cognitive therapy. The things he said rarely made sense to me at first. Then, after a few days, it would suddenly dawn on me what he might have meant. At least, I'd discover a meaning in what he'd said, based on my personal experience or the experiences of my patients. One evening, while George and I were out sharing a beer after a lecture,* he said that the Buddha taught that we constantly drift in and out of enlightenment. This sounded intriguing, but I didn't know exactly what he was talking about. What's enlightenment? Is it some kind of fantastic, mystical experience? How do we know when we're enlightened? And why do we drift in and out of it? A few days later, one possible meaning of what he'd said suddenly came to me, and I got excited. Have you ever noticed how you sometimes feel very confident, loving and relaxed? At these times, you feel like you don't have any ego or territory to defend. It's easy to relate to other people, and you feel at peace with the world. When I get into this mind-set, it feels wonderful. I feel at one with other people. If someone is critical or annoyed with me, I don't feel threatened or upset. I can see the world through their eyes, and can quickly turn any tense or hostile interaction into a warm and trusting one. It dawns on me that I don't really need * Two beers, actually. He had one and I had one as well.
Chapter 32
Page 1137
"self-esteem," or even a "self," and that these are simply empty concepts. Experts in Buddhism might have fancier versions of enlightenment, but on a humble, practical level, you could think of the experience I've described as a kind of emotional enlightenment. It's pretty fantastic, and it seems like it will go on forever. Unfortunately, these feelings of enlightenment never do last. All of a sudden, it's a few days later, and you've drifted out of enlightenment again. You start to feel vulnerable or anxious, and little things threaten you. You may feel like you're not good enough, or not as good as you think you should be. You may worry about things. You may easily get annoyed, frustrated, defensive, or angry, and your ego seems to be on the line. If you're criticized, you may feel like you have to defend your territory, or prove something. Of course, that never works, so the conflict escalates. Do you know what I'm talking about? Our patients will experience the same kinds of ups and downs. When they first recover from depression and anxiety, or overcome conflicts in their relationships with others, they may experience a kind of enlightenment. Many have told me that they feel like they've been born again. Some have said that it's the happiest they've ever felt in their entire lives. They often comprehend their own spiritual beliefs in a much deeper way as well. Recovery can be much more than just an improvement in your mood and outlook. Sometimes, it's like a profound personal transformation. This "enlightenment" seems so vivid and easy that most patients think that it will go on forever. But it never does. Before long, they'll drift back out of
Chapter 32
Page 1138
enlightenment again, just as we all do. Suddenly, they'll be struggling with feelings of self-doubt, defensiveness, anxiety, despair, or anger again. This is as certain as the law of gravity. What goes up must come down. It's hard to predict when the first relapse will occur. It could happen within a few days, a few weeks, or a few months. When patients relapse, they typically feel shocked and intensely demoralized. The depression may feel worse than any depression they've ever felt before, because of the sharp contrast with the incredible feelings of joy they were experiencing just a few days earlier. It's like having the rug pulled out from under you. If you don't prepare your patients for relapses ahead of time, you'll be in for lots of heartache. Many patients will become angry, discouraged and uncooperative because they've lost trust in you and in the therapeutic process. They may feel like they've been conned or misled. If they give up and conclude that things are hopeless, it will function as a self-fulfilling prophecy. Nothing will change, so they'll conclude they really are hopeless. In contrast, if you prepare patients for relapses, the prognosis is bright. Most of us can tolerate almost any emotional or interpersonal difficulty if we know that our suffering will be short-lived, and that we'll soon be feeling good again. If we have hope, we can weather the storm. The best time to prepare the patient is when they first recover. If you've been monitoring the patient's symptoms at every session with the Brief Mood Survey, you'll be looking for scores in the range of 0 – 1 on the depression, anxiety, and anger tests. In addition, patients should look and behave like they're
Chapter 32
Page 1139
feeling happy and symptom-free. If the score is higher than this, the patient has not yet completely recovered. For example, if the depression score has gone from 16 (severe) to 4 (borderline) on the Brief Mood Survey, there's been a tremendous amount of improvement. You and your patient should be proud of the extraordinary work you've done together. However, you shouldn't get too complacent, because the patient is still feeling somewhat discouraged, worthless, and unhappy, and probably still doesn't completely enjoy activities that would normally be pleasurable. I would continue working with the patient, using CBT techniques, until the score is lower. You may need to use powerful techniques like the Externalization of Voices and the Acceptance Paradox. Once the patient can truly put the lie to any remaining negative thoughts, you'll generally see the score on the depression scale drop all the way to zero, or nearly zero. This is the time to do Relapse Prevention Training. It only takes one session, and there are several steps: Step 1. Predict and Reframe Relapse Step 2. Recovery Circle Revisited Step 3. Daily Mood Log with Externalization of Voices Step 1. Predict and Reframe Relapse When patients have recovered, I often tell them something like this: "Joseph, I can see from your scores on the Brief Mood Survey, and from the way you're talking, that you're feeling terrific. That's good
Chapter 32
Page 1140
news. The even better news is that we can predict with 100% certainty that you're going to have a horrible relapse. It may occur within a few days, or a few weeks, but sooner or later, it's going to happen. One morning in the near future, you're going to wake up with the worst depression of your entire life. Do you know why this is a great thing?" The patient generally doesn't have the slightest notion what I'm talking about, and doesn't understand how there could be anything good about a horrible relapse. Then I explain the difference between feeling better and getting better. The first time patients recover, they feel terrific, but usually don't know why or how the recovery came about, or attribute it to the wrong things. They may think, "Oh, I'm feeling better now because I got a promotion," or "because I got a date with Jeannie." The problem with these formulations is that they make patients victims, because they think their moods depend on external forces that are beyond their control. When they experience a problem at work, or when Jeannie gives them the cold shoulder, they may fall into a black hole again. The second time patients recover, they begin to see the direct cause and effect relationship between the tools they've learned in therapy and the changes in their mood. Being depressed for an hour, a day, or a week is perfectly acceptable. If patients use the same tools that helped them the first time, and they begin to feel better, they'll know that they can use those same tools to break out of bad moods for the rest of their lives. I tell patients that I want them to relapse as soon as possible, while we're still working together. That way, I can guide them through it. But even if the
Chapter 32
Page 1141
relapse occurs after we've terminated, they can still come back for a tune-up later on. Predicting and reframing the relapse ahead of time softens the blow when the relapse actually occurs. Patients may feel totally miserable, but they'll remember that you predicted this would happen. This gives them confidence and prevents disillusionment. In addition, they'll remember that they've got to roll up their sleeves and get to work again, using the tools that were so helpful to them the first time they recovered. This provides hope and gives them a specific plan so they won't just give up and wallow in the feelings of hopelessness. Step 2. Recovery Circle Revisited Whenever you treat a patient for the first time, you'll have to try many different techniques before you find a way to put the lie to the patient's negative thoughts. A depressed patient with Borderline Personality Disorder might have the thought, "I'm defective at the core." A patient with public speaking anxiety might think, "Everyone will see how nervous I am and look down on me. What's wrong with me? I shouldn't be so insecure and inept!" A patient with panic attacks may believe, "I'm about to pass out," or "I'm on the verge of cracking up." While the initial treatment can be very challenging, the good news is that relapses are far easier to treat. That's because patients will have the same kinds of negative thoughts and feelings as when they first came to you for treatment. In addition, the technique that worked the first time will probably work again when the patient relapses, so you can use that technique right away. When I discover the technique that works for a patient during the initial
Chapter 32
Page 1142
treatment, I circle it in the chart. If the patient calls months or even years later with a relapse, I grab the chart and look to see what technique worked for that patient. I tell the patient I'll see them at my first available slot, which is generally within a couple days. I also tell them to fill out a Daily Mood Log in the meantime, and to use the technique that was so effective for them when we first worked together. This approach has worked well. I once treated a mildly depressed and anxious New York options trader named Wilson who suffered from mild chronic depression and panic attacks. During these attacks, he noticed his heart beating rapidly and thought he was on the verge of death. He would rush to the emergency room, but after a brief exam, they'd send him home with the reassurance that everything was okay. To make matters a bit more complicated, Wilson was receiving treatment from a cardiologist for a cardiac disturbance, but it wasn't a life-threatening condition. Wilson constantly obsessed about the fact that he wasn't good enough. Although he was doing well and lived in an attractive home in a fancy neighborhood, his boss and several of his colleagues had made tens of millions of dollars trading stock options, and he always compared himself to them. He felt inferior, and believed that there was some kind of intense, wonderful feeling that only the "beautiful" people with loads of money and success could experience. This belief is not uncommon in our culture. Wilson could see that he based his feelings of self-worth on his achievements, productivity, and success. He was intrigued by CBT, and loved all the techniques we were using. He also loved to philosophize and traced his low
Chapter 32
Page 1143
self-esteem to his relationship with his father. He felt like he'd always had to earn his father's love, and hoped that these discussions about his childhood would eventually lead to greater self-esteem. Unfortunately, Wilson's feelings of depression and anxiety did not improve. Still, he always gave me the highest possible marks on the Evaluation of Therapy Session, and I think he would have been perfectly content to come in for sessions indefinitely. I also looked forward to our sessions, because we seemed to have tremendously meaningful conversations. But I was concerned about the fact that he did not seem to be recovering. One day, Wilson told me about a confidential meeting he'd just had with his boss. His boss had informed him that their company was facing a financial crunch because of the recession. He told Wilson that he was pretty sure he could save the company, but they'd all have to lower their expectations for a period of time. He said he needed to ask Wilson and all his colleagues to take a 20% pay cut so the company could get back in the black. He promised that when the company was doing better, he'd increase Wilson's salary again. Wilson admired his boss and wanted to help the company, so he graciously agreed to the salary reduction. Six weeks later, he reported a sudden increase in his feelings of depression and inadequacy. He'd had several panic attacks and was obsessing about his heart again. I asked Wilson if anything upsetting or stressful had happened. He explained that he'd gone out for a beer with a colleague Friday after work. Wilson asked his colleague how he felt about the 20% pay cut. His colleague said that
Chapter 32
Page 1144
he'd flat-out refused to take any pay cut. He said that as far as he knew, everyone else had objected as well. It suddenly dawned on Wilson that he was the only person in the company who'd agreed to a pay cut. At that exact moment, he started to feel anxious and depressed again. I suddenly began to see Wilson's problems in a completely different light. Although his feelings of depression and anxiety were accompanied by all kinds of distorted negative thoughts about not being good enough, it seemed like his excessive niceness and lack of assertiveness might be the real cause of his symptoms. It dawned on me that his symptoms nearly always intensified right after he'd had a conflict with someone—his wife, a friend, or a colleague. But Wilson always acted nice and polite, and swept his feelings under the rug, even if he was upset about what was going on. Then he'd get anxious and go off to the emergency room to have his heart checked out. I asked Wilson if there might be a relationship between his feelings about the pay cut and the sudden increase in his symptoms. He said he'd never considered that possibility. I also asked him if he was planning to talk the problem over with his boss, so he could tell his boss that he felt taken advantage of. The very suggestion caused an instant spike in his anxiety, and he had a dozen excuses about why it wouldn't be helpful or appropriate. He explained that it might not be a good idea to rock the boat, that he admired his boss, that his boss was just doing his best, that he didn't have as much seniority as several of his colleagues, and that the financial crisis would soon be over anyway. I told Wilson that he was bullshitting and making a lot of excuses. I
Chapter 32
Page 1145
explained that he was ultimately in charge, and would have to do whatever he thought was right, but it seemed clear that he was conflict phobic. I was concerned that he might not be able to overcome his chronic feelings of depression, inadequacy and anxiety until he started sticking up for himself and telling people how he really felt. Wilson reluctantly agreed to talk things over with his boss. His boss was embarrassed, and told Wilson how much he valued his contribution to the company. He agreed to refund all the salary that he'd withheld. Wilson experienced a sudden surge of self-confidence, and his scores on the depression and anxiety tests fell to 0 for the first time. The Hidden Emotion Technique turned out to be the solution to Wilson's problems. This will probably be the only technique he'll ever need to deal with anxiety and depression for the rest of his life. Every time he starts feeling anxious and inadequate, it will probably be because he's upset with someone, but hasn't expressed his feelings. The moment he addresses the problem he's been avoiding, his negative feelings will probably disappear again. Wilson was disappointed to discover that the solution to his problems was so simple and obvious. He loved talking about his childhood and exploring deep, philosophical issues during our sessions. Those dialogues were fun but never led to any improvement, much less a cure. In contrast, when we used the Hidden Emotion Technique, Wilson's symptoms disappeared completely within 24 hours. Step 3. Daily Mood Log with Externalization of Voices This step in the Relapse Prevention Training program is absolutely crucial.
Chapter 32
Page 1146
Tell the patient to imagine that it's three weeks from today and they've just woken up with the worst depression they've ever experienced. The sharp contrast from the feelings of joy and self-esteem they've been feeling since their initial recovery just a few weeks earlier is practically unbearable. Explain that you're going to prepare for that moment today, so they'll know exactly how to nip the relapse in the bud when it does happen. Help them fill out a Daily Mood Log, based on how they imagine they're going to be thinking and feeling when they suddenly relapse. At the top, they can write something like, "I'm suddenly feeling severely depressed again." Or, they could describe the type of event that would usually be upsetting, such as a fight with their spouse or a problem at work. Ask them to record the negative feelings they're going to have during the relapse, and to rate them on a scale from 0 – 100%. Most patients will feel intensely depressed, anxious, worthless, ashamed, frustrated, angry and hopeless. Now ask them to record the negative thoughts they think they might have during the relapse, and to indicate how strongly they think they're going to believe them. The thoughts and feelings on pages 1147 – 1148 are typical.
Chapter 32
1147
Daily Mood Log Upsetting Event: Having a depression relapse. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
100%
Embarrassed, foolish, humiliated, self-conscious
100%
Anxious, worried, panicky, nervous, frightened
100%
Hopeless, discouraged, pessimistic, despairing
100%
Guilty, remorseful, bad, ashamed
100%
Frustrated, stuck, thwarted, defeated
100%
Inferior, worthless, inadequate, defective, incompetent
100%
Angry, mad, resentful, annoyed, irritated, upset, furious
100%
Lonely, unloved, unwanted, rejected, alone, abandoned
100%
Other (describe)
Negative Thoughts
% Before
1.
I'll never get better. This shows that the therapy didn't really work.
100%
2.
My improvement wasn't real. I was never really better. I just thought I was, but underneath, I was depressed the whole time.
100%
3.
Cognitive therapy can't work for me. My problems are too deep.
100%
% After
Distortions
Positive Thoughts
% After
% Belief
Chapter 32
1148
Daily Mood Log (cont'd) Negative Thoughts
% Before
4.
I'm really worthless after all.
100%
5.
What good are a few weeks of improvement? Now I'll be depressed for years and years again.
100%
6.
My improvement was just a fluke.
100%
7.
This is unfair. Other people don't have to work so hard to be happy.
100%
8.
There must be something wrong with me.
100%
% After
Distortions
Positive Thoughts
% Belief
Chapter 32
Page 1149
After they identify the distortions in these thoughts, they can try to challenge them with thoughts that are more positive and realistic. Most patients find this easy because they're feeling happy today and can quickly see through their negative thoughts. However, if you wait until they relapse, it will be a different story. They'll be totally convinced that the thoughts are valid. That's why it's vitally important to do the Relapse Prevention Training ahead of time, when the patient feels happy and optimistic. See how many distortions you can find in the first two negative thoughts about relapse: 1.
I'll never get better. This shows that the therapy didn't really work.
2.
My improvement wasn't real. I was never really better. I just thought I was, but underneath, I was depressed the whole time.
When you're done, turn the page and I'll share my analysis with you. Distortion
( )
Distortion
1. All-or-Nothing Thinking
6.
Magnification and Minimization
2. Overgeneralization
7.
Emotional Reasoning
3. Mental Filter
8.
Should Statements
4. Discounting the Positive
9.
Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 32
Page 1150
Answer I found nine distortions in the first two negative thoughts. Distortion
Yes
Explanation
1. All-or-Nothing Thinking
The patient is telling himself that the therapy was worthless because it didn't work perfectly. He sees his progress as a complete zero, with no room for improvement.
2. Overgeneralization
He sees his current relapse as a never-ending pattern of defeat and suffering.
3. Mental Filter
He sees his entire life in terms of the negative feelings he's having right now.
4. Discounting the Positive
He insists that his improvement wasn't real, and that he was just fooling himself when he recovered.
5. Jumping to Conclusions
When he tells himself that he'll never get better, he's involved in Fortune-Telling. In fact, he's already experienced substantial improvement, even though he's feeling down in the dumps right now.
Mind-Reading Fortune-Telling 6. Magnification and Minimization
He's blowing the importance of the relapse out of proportion.
7. Emotional Reasoning
He feels hopeless, so he thinks he really is.
8. Should Statements
He seems to be telling himself that he should be happy all the time, and that he should never get upset. He's also telling himself that the therapy should work perfectly.
9. Labeling
Although this distortion is not present in the first two negative thoughts, he's labeling himself as "worthless" in the fourth negative thought. In the sixth negative thought, he's labeling his improvement as "a fluke." In the seventh negative thought, he's labeling his relapse as "unfair."
10. Blame Self-Blame Other-Blame
He seems to be blaming himself for feeling depressed again. He may also be blaming the therapist, or the therapy, for the relapse.
Chapter 32
Page 1151
How could this patient talk back to these thoughts? Remember that it's usually much easier to talk back to one thought at a time. Let's focus on the second thought, "My improvement wasn't real. I was never really better. I just thought I was, but underneath, I was depressed the whole time." This is a particularly challenging relapse thought. What could he tell himself instead? Put your ideas here before you continue reading:
Chapter 32
Page 1152
Answer There are lots of ways to talk back to any negative thought. Here's one approach: "My improvement was real. I was feeling better. In fact, I felt terrific for the past few weeks. But everyone gets upset at times, and I'm no different. No one can feel happy all the time. Right now, I need to work with the tools that were so helpful to me three weeks ago." Ask the patient to record how much he believes the positive thought. If his belief is 100%, ask him to re-rate his belief in the negative thought. Often, it will be 0%. Keep in mind that you're doing this exercise when the patient feels happy and confident, so the patient can usually put the lie to the negative thoughts pretty convincingly. You can see an example of a completed relapse Daily Mood Log on pages 1153 – 1155. Once the patient has refuted all the relapse thoughts on paper, it's time for the Externalization of Voices. You can play the role of the patient's negative thoughts, using the second person, "You." Ask the patient to play the role of the positive thoughts, using the first person, "I." The patient can try to demolish your attacks. This is the more aggressive "You" – "I" version of the Externalization of Voices. If you think the patient may still be somewhat fragile, you can start out with the gentler "I" – "I" version of the technique, and then move up to the "You" – "I" version once the patient has gotten used to the technique.
Chapter 32
Page 1153
Daily Mood Log Upsetting Event: Having a depression relapse. % Before
% After
% Before
% After
Sad, blue, depressed, down, unhappy
100%
50%
Embarrassed, foolish, humiliated, self-conscious
100%
10%
Anxious, worried, panicky, nervous, frightened
100%
25%
Hopeless, discouraged, pessimistic, despairing
100%
25%
Guilty, remorseful, bad, ashamed
100%
15%
Frustrated, stuck, thwarted, defeated
100%
35%
Inferior, worthless, inadequate, defective, incompetent
100%
15%
Angry, mad, resentful, annoyed, irritated, upset, furious
100%
35%
Lonely, unloved, unwanted, rejected, alone, abandoned
100%
10%
Other (describe)
Emotions
Negative Thoughts
1.
I'll never get better. This shows that the therapy didn't really work.
% Before
% After
100%
25%
10%
Emotions
Distortions AON; OG; MF; DP; FT; MAG; ER; SH; OB
Positive Thoughts
1. It's not true that I'll never get better,
% Belief 100%
because I've already improved. In fact, every time I've been depressed, I've gotten better sooner or later. The therapy did work, even though it didn't work perfectly. I simply need to roll up my sleeves and use the same techniques that helped me the first time.
100%
Chapter 32
Page 1154
Daily Mood Log (cont'd) Negative Thoughts
% Before
% After
Distortions
100%
10%
AON; DP; ER
Positive Thoughts
% Belief
2. That's nuts. My improvement was
100%
3. The cognitive therapy was quite
100%
2.
My improvement wasn't real. I was never really better. I just thought I was, but underneath, I was depressed the whole time.
3.
Cognitive therapy can't work for me. My problems are too deep.
100%
4.
I'm really worthless after all.
100%
35%
AON; OG; MF; DP; 4. MAG; ER; SH; LAB; SB
5.
What good are a few weeks of improvement? Now I'll be depressed for years and years again.
100%
25%
DP; FT; MAG/MIN; ER; SH
quite real. I did feel better. But now I feel depressed again and need to get back to work. This happens to everybody.
20%
AON; OG; DP; FT; MAG; ER
helpful to me, even though I've had a relapse. Relapses are common— everyone has them. There I go labeling myself again. I'm depressed, not worthless!
5. A few weeks of improvement are great! It was a terrific breakthrough for me, and a relief. My next improvement could last even longer. Let's take it one step at a time.
100%
100%
Chapter 32
Page 1155
Daily Mood Log (cont'd)
6.
Negative Thoughts
% Before
% After
Distortions
My improvement was just a fluke.
100%
0%
DP; MIN; ER; LAB
Positive Thoughts
6. That's also a nutty claim. My
% Belief 100%
improvement wasn't a "fluke." It was the result of the tools I was learning to use.
7.
8.
This is unfair. Other people don't have to work so hard to be happy.
100%
There must be something wrong with me.
100%
50%
MR; ER; SH; LAB; OB
7. Now I'm feeling sorry for myself again.
100%
I have the right to do that, but do I really want to? It's unfortunate that I have a tendency to become depressed, but it's not "unfair." 25%
AON; OG; MF; DP; 8. MAG; ER; SH; LAB; SB
Hey, there's a lot that's wrong with me. However, just about everyone else seems to have a lot of defects, too, so I'll have lots of people to hang out with!
100%
Chapter 32
Page 1156
Remind the patient that it may sound like two different people who are in a battle with each other, but in reality, you're just playing the two parts of the patient's brain. You will be the playing the role of the negative, self-critical, pessimistic voice in the patient's head, and the patient will play the role of the positive, self-loving voice. The dialogue might go like this: Negative Thoughts (played by therapist): Face it. This relapse shows that you're a hopeless case. You'll never get better. Positive Thoughts (played by patient): That's ridiculous. Everyone gets upset from time to time. My therapist warned me that this would happen, and explained that it happens to everybody. Negative Thoughts (played by therapist): That's a nice fantasy, but let's be serious. He only told you that you were going to relapse because he knew you were a hopeless case. Positive Thoughts (played by patient): No, he told me that I'd relapse so that I'd be prepared when it happened. This is actually a great opportunity to practice using the tools that were so helpful to me three weeks ago. Negative Thoughts (played by therapist): Let's face the facts. You didn't really get better three weeks ago. You might have thought that you were feeling happy, but you were just fooling yourself. Underneath, you were still depressed the entire time. You'll always be depressed, because you're a hopeless, worthless human being. Positive Thoughts (played by patient): Hey, you've been giving me
Chapter 32
Page 1157
that kind of bullshit for years! But the fact is, I really was feeling better for a few weeks. In fact, I felt terrific. Of course, I'll always have the tendency to get upset about things at times. All human beings do. It's normal. And when this happens, I'll just have to pick up these tools and use them again. When you do the Externalization of Voices, you should be as tough on the patient as you possibly can. Patients will be at least that tough on themselves when the actual relapses occur, so you won't do them any favors by being "nice." This practice will be invaluable, but it has to work at the gut level. It has to be real. Continue until the patient can easily blow you out of the water, no matter what you attack him with. If the patient has trouble, gets upset, or responds ineffectively, do a rolereversal. Tell the patient to play the role of the Negative Thoughts, while you play the role of the Positive Thoughts. This will give you the chance to model effective responses. Once the patient gets the idea, do another role-reversal. This exercise is challenging, and it's possible that neither you nor the patient will be able to come up with convincing positive thoughts initially. If so, acknowledge this, and suggest trying again at the next session. You'll usually do better after some time has passed and you've had a chance to think about the negative thoughts that you and the patient had trouble smashing. Let's say your patient has this negative thought: "This relapse shows that I'm hopeless after all." How would you respond? Please write down a positive thought, using the first person, "I," before you continue reading:
Chapter 32
Page 1158
Chapter 32
Page 1159
Answer Here's one way to challenge this thought: "I couldn't be hopeless because I did improve and enjoy three weeks of happiness. That was a terrific first step. But there will always be problems that I'll have to deal with. Last night I had an argument with my wife. That's the type of thing that usually triggers my dark moods, so it's not surprising that I'm upset this morning. I need to talk things over with her so we can get back on track." Look at the response you wrote down. How did you do? When your patients relapse, their negative thoughts will seem completely realistic and overwhelming. That's why so many patients commit suicide during relapses. If you prepare them ahead of time, it will be much easier for them to talk back to the thoughts when the relapse hits. This exercise has saved many patients' lives, and may be one of the most important things you do for your patients. Other Relapse Prevention Techniques I've prepared a treatment termination form that patients can fill out prior to completing therapy.* The form asks patients to evaluate the quality of the therapy by rating items like this: The therapy was helpful to me. I was able to talk about my problems and get my feelings off my chest. The therapy helped me understand more about myself.
* The termination form appears in my Therapist's Toolkit, along with a wide variety of useful treatment and assessment tools. Toolkit purchase includes license for unlimited reproduction in your clinical practice. For more information, send an email to [email protected].
Chapter 32
Page 1160
The therapy helped me change some of my negative thoughts and selfdefeating attitudes. I learned to communicate more effectively and improve my relationships with people. I learned techniques to improve my productivity and function more effectively in my daily activities. I learned to solve problems in my career and personal life. Response options include "not at all," "somewhat," "moderately," "a lot," or "does not apply." Patients can also write out their answers to a variety of questions, such as: Did you have any problems that you weren't able to discuss in therapy? Were there issues or feelings that your therapist didn't understand? Was there anything that your therapist did or said that irritated you or rubbed you the wrong way? What did you like the least about your therapist? What was the most helpful and useful part of the therapy for you? What did you like the best about your therapist? What were the most helpful ideas or techniques that you learned about? How will you use these skills to cope with personal difficulties in the future? Why are you terminating treatment at this time? Have you successfully completed therapy? Are you dropping out because of personal pressures, a lack of progress, or other factors? lack of progress, or other factors? What were your goals when you first came to therapy?
Chapter 32
Page 1161
How much progress did you make on these goals? Did you have some goals that were not met? Have you discussed the possibility of relapse with your therapist? Have you practiced relapse prevention techniques with your therapist? Would you be willing to return for additional treatment if you needed help? If so, would you like to work with the same therapist, or a different one? These questions will help you and your patient evaluate what the two of you accomplished during the therapy. You'll also pinpoint any problems that haven't been addressed, in case further treatment is needed. If the patient ever returns for help with a relapse, this information will be invaluable. Many psychiatrists tell patients with depression and anxiety disorders that they have chronic, relapsing illnesses, like diabetes. Patients are also told that they'll probably need treatment with antidepressant medications for the rest of their lives to correct the "chemical imbalance" in their brains. In fact, this has become the official position of the American Psychiatric Association, and it's strongly endorsed by the pharmaceutical industry. I find this message distressing for two reasons. First, I believe that it can act as a self-fulfilling prophecy. If an "expert" tells a patient that she or he is essentially hopeless, the patient will probably believe it! I've also wondered whether feelings of hopelessness may sometimes result from the ineffective treatment that patients have received. Second, my own clinical experience has been completely inconsistent with this notion. Over the course of my career, I've had over 35,000 therapy sessions
Chapter 32
Page 1162
with individuals who were suffering from depression, anxiety disorders, relationship problems and personality disorders. I treated 60% of them without medications, and 40% with a combination of CBT plus antidepressant medications. Aside from patients with schizophrenia or type I bipolar illness, nearly all the patients who received antidepressants tapered off of them successfully following recovery. Only a few of my patients ever returned to therapy because of relapses, and the great majority of those who did return only required one or two sessions to turn the problem around. I attributed the good long-term results I observed to the fact that I did careful Relapse Prevention Training with every patient prior to discharge, using the techniques I've described in this chapter. In addition, I required all my patients to do homework throughout the treatment, so they developed a high degree of skill with tools such as the Daily Mood Log and the Revise Your Communication Style form. They became very clear about the types of problems and thinking patterns that triggered their mood problems in the first place, and the types of techniques that were the most helpful to them. During the time we worked together, they really learned to be their own therapists. That's probably why they didn't need to rely on medications for the rest of their lives. Certainly, my clinical experience is not the same as scientific data, because I was involved in private practice, and there was no control group. Still, my experiences with so many severely disturbed patients were extremely encouraging.
Part Eight Healing Yourself
33*
"I Don't Like You Either!" Countertransference from a CBT Perspective
I'm not a huge fan of psychoanalysis, but I think the psychoanalysts had a good idea when they decided to require all their trainees to undergo their own psychoanalysis as part of their training. With the proliferation of so many new schools of psychotherapy, we've gotten away from this tradition. But no matter what your therapeutic orientation might be, I think some experience in the patient's shoes can be invaluable. After all, therapists are human, too, and our humanness doesn't disappear the moment we receive our licenses. From time to time, most of us experience the same feelings of self-doubt, insecurity, frustration, anxiety or discouragement that our patients experience. These feelings may surface when we're treating patients, and can interfere with therapy. There are two ways that therapists typically react when challenged by
* Copyright
2003 by David D. Burns, M.D.
Chapter 33
Page 1165
critical or resistant patients. There's the "You're no good" reaction and the "I'm no good" reaction. In the "You're no good" mindset, we get annoyed or resentful and subtly blame the patient for the conflict or lack of progress. We tell ourselves that the patient "shouldn't" be so irrational, ungrateful, critical, or oppositional. We may also tell ourselves that she or he "should" be more enthusiastic and motivated because we're working so hard to try to help them. You may remember the therapist in Chapter 12 who got upset when his angry adolescent patient, Jimmy, said, "You're a dickhead! This therapy sucks!" The therapist exclaimed, "This session is over!" and kicked Jimmy out of his office. In the "I'm no good" mindset, we feel ashamed, inadequate, or anxious because we blame ourselves for the conflict or lack of progress. At my recent intensive workshop in Napa, California, a therapist described how a college student she'd treated had hanged himself in his dormitory room several hours after their therapy session at the student counseling center. She felt profoundly guilty and devastated because she told herself, "It was my fault. I should have known that he was suicidal that day, and I should have prevented his death." Fortunately, she was able to express these feelings during the workshop and resolve the grief and pain that she'd been sweeping under the rug since his death two years earlier. We all have our own unique ways of thinking about conflicts and failures in our relationships, including our relationships with our patients. The kinds of problems that trigger your insecurities will probably be quite different from the kinds of problems that make me feel anxious. Cognitive therapy tools like the
Chapter 33
Page 1166
Daily Mood Log provide us with a unique opportunity to examine our own reactions to clinical difficulties. You'll see exactly why you react the way you do. You can also use cognitive therapy techniques to change the way you think and feel about your work. There are several potential benefits: If you practice what you preach, and learn to deal with your own negative feelings successfully, you'll have much more credibility and integrity when treating your patients. You'll have greater empathy, because you'll know what if feels like to be in the patient's shoes. You'll enjoy your clinical work more, because you won't go home at night feeling so anxious, guilty, frustrated, or burned out. You'll be a far more effective therapist, because you'll learn how to turn therapeutic failures into breakthroughs. It's awfully hard to fake it when you're feeling annoyed, anxious, defensive or inadequate. No matter how hard you try to disguise your feelings, your tone and body language will convey the fact that you're upset. You and your patient will both be aware of the tension in the air. If you try to hide your feelings and act "professional," the problem may get worse. In contrast, if you learn to feel reasonably relaxed and confident when you're working with patients who are hostile and mistrustful, you can often do superb clinical work. During one of my Wednesday evening supervision groups at Stanford, a psychiatric resident named Danielle asked what you're supposed to do if you don't like one of your patients. Danielle was treating a mildly depressed young
Chapter 33
Page 1167
woman named Suni who was attending the law school in San Francisco. Suni felt ambivalent about her career and was having difficulties at school because of procrastination. She was also having problems with her academic supervisor, who was urging her to take some time off. Danielle had been tracking Suni's progress at every session with the Brief Mood Survey and the Evaluation of Therapy Session form. Although Suni was making modest progress, she consistently gave Danielle low marks on the Therapeutic Empathy scale. Danielle encouraged Suni to express her negative feelings about the therapy, but Suni became annoyed and said she'd prefer to use the time to work on her own problems, rather than analyzing her relationship with her psychiatrist. Danielle continued to use the CBT techniques that Suni liked, but encouraged Suni to talk about her negative feelings at the start of each session. After resisting this invitation for several weeks, Suni finally agreed to tell Danielle what she didn't like about the therapy. The moment Suni opened up, Danielle began to feel defensive and annoyed. She said, "I wasn't feeling particularly irritated until Suni gave me the negative feedback I'd been asking for! Then my sudden anger and frustration about what she was saying made it hard for me to respond to her effectively." Our thoughts and expectations often act as self-fulfilling prophecies. Suni was afraid to criticize Danielle because she was convinced it would be too upsetting. Then, when she finally opened up, her prediction came true. Danielle got upset and the tension escalated.
Chapter 33
Page 1168
It's interesting how we often play the role that our patients expect us to play, even though we struggle not to. If a patient is afraid that we'll be cold and rejecting, we may suddenly feel like we really do want to reject them. If the patient expects us to be judgmental, we may suddenly discover that we do feel judgmental. The harder we try to resist the trap, the quicker we fall into it. It's almost as if our patients hypnotize us, and we can't seem to resist falling under their spell. Danielle's negative feelings about Suni provided us with a terrific opportunity to focus on countertransference from two different perspectives. First, how was Danielle feeling, and what was she telling herself when Suni criticized her? Second, what were Suni's specific criticisms, and how might Danielle respond more skillfully? Here's what Suni said to Danielle: "You're clumsy and awkward during sessions. Sometimes, it seems like you don't know what you're doing." "You talk about yourself too much. I come to therapy to discuss my issues, not to hear your stories!" "Nobody could ever understand me. How can you pretend to know how I feel, since you can't get inside my head and know my thoughts and feelings?" "You don't listen to what I'm saying. If I said, 'My brother just died,' you'd probably say, 'Let's get back to work on your Daily Mood Log.'" Danielle's Daily Mood Log appears on pages 1170 – 1171. The upsetting
Chapter 33
Page 1169
event was simply, "Being criticized by Suni." You can see that Danielle felt unhappy, self-conscious, discouraged, anxious, ashamed, and inferior. She also felt frustrated and angry because she was telling herself: 1. Screw you! I don't like you either! 2. Suni's criticisms aren't true. 3. She's ungrateful. 4. She's not being fair. 5. Maybe she's right and I am a bad therapist. 6. She's a horrible person. Danielle's belief in these six thoughts ranged from 70% to 100%. She wanted to work on negative thought #6 first. I've put this thought in the middle of the Recovery Circle on page 1172. Put yourself in Danielle's shoes, and review the list of 50 Ways to Untwist Your Thinking on page 1173. Select a variety of techniques you could use to put the lie to the thought, "She's a horrible person," and put the name of one technique in each box. When you're done, you can review my Recovery Circle on page 1174.
Chapter 33
Page 1170
Danielle's Daily Mood Log* Situation or Event: Being criticized by Suni. % Before
Emotions
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
50%
Embarrassed, foolish, humiliated, self-conscious
60%
Anxious, worried, panicky, nervous, frightened
30%
Hopeless, discouraged, pessimistic, despairing
50%
Guilty, remorseful, bad, ashamed
20%
Frustrated, stuck, thwarted, defeated
90%
Inferior, worthless, inadequate, defective, incompetent
20%
Angry, mad, resentful, annoyed, irritated, upset, furious
80%
Lonely, unloved, unwanted, rejected, alone, abandoned
—
Negative Thoughts
% Before
1. Screw you! I don't like you either!
100%
2. Suni's criticisms aren't true.
70%
3. She's ungrateful.
100%
* Copyright
% After
Other (describe)
% After
Distortions
1984 by David D. Burns, M.D. Revised 2003.
Positive Thoughts
% Belief
Chapter 33
Page 1171
Danielle's Daily Mood Log (cont'd) Negative Thoughts
% Before
4. She's not being fair.
100%
5. Maybe she's right and I am a bad therapist.
70%
6. She's a horrible person.
70%
% After
Distortions
Positive Thoughts
% Belief
Checklist of Cognitive Distortions* 1.
All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6.
Magnification and Minimization. You blow things out of proportion or shrink them.
2.
Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7.
Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3.
Mental Filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4.
Discounting the Positive. You insist that your positive qualities don't count.
9.
Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
* Copyright
10
2004 by David D. Burns, M.D.
11
12
13
14
9
16
8
She's a horrible person. 100%
15
7
1
6
5
2
Danielle's Recovery Circle*
4
3
Page 1172
Chapter 33
Page 1173
50 Ways to Untwist Your Thinking* Basic Techniques
Exposure Techniques
Role-Playing 19. Externalization of Voices
Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques
Philosophical / Spiritual 21. Acceptance Paradox
Compassion-Based
Visual Imaging
5. Double Standard Technique
Truth-Based 6. Examine the Evidence
8. Survey Technique 9. Reattribution
39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
7. Experimental Technique
Cognitive Exposure
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Motivational Techniques
Semantic 12. Semantic Method 13. Let's Define Terms
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA)
14. Be Specific
Quantitative
30. Devil's Advocate Technique
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Danielle's Recovery Circle* Examine the Evidence
Be Specific
Thinking in Shades of Gray
Empathy
16
15
1
14 Survey Technique
2
13 She's a horrible person. 100%
Semantic Method
4
11 Let's Define Terms
Identify the Distortions
3
12
Straightforward Technique
Agenda Setting
5
10
Downward Arrow
6 Acceptance Paradox
9
8
Cost-Benefit Analysis
7
Externalization of Voices Five Secrets
Double Standard
* Copyright
2004 by David D. Burns, M.D.
Page 1174
Chapter 33
Page 1175
I won't review all the techniques on the Recovery Circle on page 1174, but I'll highlight a few that were helpful for Danielle. After you've read this chapter, ask yourself how some of the other techniques would work. For example, how would you use the Cost-Benefit Analysis, the Double Standard Technique, Examine the Evidence, Be Specific, or the Acceptance Paradox? Empathy Imagine that Danielle has just described how she felt when Suni criticized her. How would you empathize with Danielle? What would you say next? Record your response below. After each sentence you write, indicate the names of the techniques you used in parentheses, using these abbreviations: DT = Disarming Technique; TE = Thought Empathy; FE = Feeling Empathy; IN = Inquiry; IF = "I Feel" Statement; and ST = Stroking.
Chapter 33
Page 1176
Answer All you really need is a brief empathic statement along these lines: "Danielle, it sounds like you're feeling really frustrated with Suni. (TE; FE) Can you tell me more about what it's been like to work with her? (IN)" The following response might also be good: "You're right, Danielle. (DT) Some patients can be extremely irritating, especially if they have narcissistic or borderline tendencies. (FE; DT) I've felt frustrated and annoyed plenty of times during sessions. (IF; FE) Tell me more about how you feel when you're working with Suni. (IN)" The goal is simply to listen and normalize Danielle's feelings so she feels understood and accepted. Agenda Setting You know by now that the most common therapeutic error is to try to help our patients before they've asked for help. Your patient describes the problem, and you jump in with your favorite therapy technique. Then the patient yes-buts you, and you end up feeling frustrated and annoyed with each other. It would be easy to make the same error with Danielle. Even though it's therapeutic supervision, Agenda Setting will still be important. What is Danielle looking for? Does she just want to let off some steam while you listen and support her? Or is she looking for help so she can learn to work with Suni more effectively? You can assess her motivation by saying something along these lines: "Danielle, you've told us how difficult Suni can be, and I have no doubt that you're right. Suni knows how to push your buttons, and she
Chapter 33
Page 1177
may do that to other people as well. She puts up a wall and pushes people away, and then feels bitter about the fact that she feels so lonely and alone. In fact, she's told you as much. When you asked Suni about the low ratings she gave you on the Therapeutic Empathy scale, she said that no one could possibly understand the way she feels inside. "You've described a fascinating problem. Where would you like to go with it? Some therapists might not want to continue working with her. They may be afraid that their strong feelings of dislike for her might sabotage the therapeutic process. Other therapists might view the conflict as a terrific opportunity for learning. "Where do you stand? Are you saying that you don't think you can work with Suni? Or would you like some get some guidance so you can learn to work with her more effectively?" Here's a brief version of the same kind of statement: "Danielle, I can see that Suni is difficult to work with. Some patients can be very challenging because they have a way of pushing our buttons and making us feel defensive and frustrated. Are you looking for some help in your work with her?" If Danielle says yes, then you could ask: "What type of help are you looking for?" Give her the chance to tell you what she wants from the supervision so you'll be working together on the same team. Danielle said she wanted to feel less frustrated in her work with Suni, and she wanted to learn how she might respond to Suni more effectively. This was
Chapter 33
Page 1178
the answer I was hoping for. Identify the Distortions Review the list of cognitive distortions at the bottom of page 1171 and see how many you can find in Danielle's thought, "She's a horrible person." Check the distortions below: Distortion
( )
Distortion
1. All-or-Nothing Thinking
6. Magnification and Minimization
2. Overgeneralization
7. Emotional Reasoning
3. Mental Filter
8. Should Statements
4. Discounting the Positive
9. Labeling
5. Jumping to Conclusions Mind-Reading Fortune-Telling
10. Blame Self-Blame Other-Blame
( )
Chapter 33
Page 1179
Answer You could make a good case that Danielle's thought, "She's a horrible person," contains at least nine distortions, and possibly all ten. Distortion
Yes
Explanation
1. All-or-Nothing Thinking
Danielle is thinking about her patient in black-and-white terms.
2. Overgeneralization
Danielle is generalizing from this conflict to Suni's worth as a human being.
3. Mental Filter
Danielle focuses on the things she doesn't like about Suni.
4. Discounting the Positive
Danielle overlooks Suni's many strengths and discounts the fact that when Suni criticized her, she was doing something that was hard for her.
5. Jumping to Conclusions Mind-Reading Fortune-Telling
?
This is not entirely clear. Danielle may assume that the relationship is doomed (Fortune-Telling), and may not believe that positive, friendly feelings can develop once you resolve a conflict with someone you're annoyed with. Danielle may also assume that Suni doesn't respect her (Mind-Reading). In fact, Suni probably has positive and negative feelings toward Danielle.
6. Magnification and Minimization
Danielle is magnifying how horrible Suni is and exaggerating the "awfulness" of her criticisms.
7. Emotional Reasoning
Danielle feels angry and annoyed, so she concludes that Suni really is a horrible person.
8. Should Statements
Danielle is telling herself that Suni shouldn't be so critical and that she should be more appreciative and enthusiastic.
9. Labeling
Danielle labels Suni as "a horrible person."
10. Blame Self-Blame
Danielle seems to be blaming Suni for the problems in their relationship.
Other-Blame
Chapter 33
Page 1180
Semantic Method Nearly all of Danielle's negative thoughts contain hidden Should Statements. Self-directed shoulds create feelings of guilt, shame, and inadequacy, and other-directed shoulds create feelings of frustration and anger. Danielle is telling herself that Suni shouldn't be so critical and annoying, and that she should be more reasonable and grateful. The Semantic Method is one of the most effective techniques for combating Should Statements. Danielle could use a phrase like, "It would be preferable if" in place of the Should Statements. For example, she could tell herself that it would be great if Suni were likeable, reasonable, and grateful, but our patients won't always live up to these standards. This subtle shift in semantics can take the sting out of a Should Statement. The Semantic Method is also extremely helpful when the negative thought involves Labeling. Danielle's negative thought, "She's a horrible person," is a classic example of Labeling. Instead, Danielle could tell herself that Suni can be annoying, or that she seems to have a hard time dealing with conflicts in her relationships with other people. Danielle could remind herself that Suni tends to be prickly, and that she puts up walls so that she doesn't have to get close to people. Danielle could also tell herself that Suni is suffering and having a hard time. Any of these thoughts might allow Danielle to be honest about the fact that Suni is difficult and challenging to work with, without having to label her as a "horrible person." Downward Arrow Technique
Chapter 33
Page 1181
The purpose of the Downward Arrow Technique is to pinpoint the SelfDefeating Beliefs (SDBs) that trigger feelings of depression, anxiety or anger. You can also use this technique to generate additional negative thoughts so you can get a better perspective on how your patient is thinking and feeling. I asked Danielle to draw a downward arrow under negative thought #6 on her Daily Mood Log, and asked: "If that were true, what would it mean to you? Why would it be upsetting to you?" This process stimulated several additional negative thoughts, as you can see on page 1182. Review them now and see if you can identify a few of Danielle's SDBs. If you want, you can consult the list of Common SDBs on page 1183, but remember that it's not comprehensive. Put your ideas here: 1. 2. 3. 4. 5. When you're done, you can turn to page 1184 and see what Danielle and I came up with.
Chapter 33
Page 1182
Danielle's Negative Thoughts 6. She's a horrible person. If that were true, what would it mean to you? Why would it be upsetting to you? 7. I'll have to spend an hour a week with someone I don't like. If that were true, what would it mean to you? Why would it be upsetting to you? 8. Life is too short to have to hang out with people I don't like. If that were true, what would it mean to you? Why would it be upsetting to you? 9. It's unfair that I have so many things to keep up with in this residency program. Everything should go smoothly. If that were true, what would it mean to you? Why would it be upsetting to you? 10. What the hell am I doing this for? I could be traveling around the world and doing things that I really enjoy. If that were true, what would it mean to you? Why would it be upsetting to you? 11. I have no control over my life or my schedule. It's overwhelming.
Chapter 33
Page 1183
Common Self-Defeating Beliefs* Achievement
Depression
1. Perfectionism. I must never fail or make a mistake. 2. Perceived Perfectionism. People will not love and accept me as a flawed and vulnerable human being. 3. Achievement Addiction. My worth as a human being depends on my achievements, intelligence, talent, status, income, or looks.
Love
13. Hopelessness. My problems could never be solved. I could never feel truly happy or fulfilled. 14. Worthlessness / Inferiority. I'm basically worthless, defective, and inferior to others.
Anxiety 15. Emotional Perfectionism. I should always feel happy, confident, and in control.
4. Approval Addiction. I need everyone's approval to be worthwhile.
16. Anger Phobia. Anger is dangerous and should be avoided at all costs.
5. Love Addiction. I can't feel happy and fulfilled without being loved. If I'm not loved, then life is not worth living.
17. Emotophobia. I should never feel sad, anxious, inadequate, jealous or vulnerable. I should sweep my feelings under the rug and not upset anyone.
6. Fear of Rejection. If you reject me, it proves that there's something wrong with me. If I'm alone, I'm bound to feel miserable and worthless.
Submissiveness 7. Pleasing Others. I should always try to please others, even if I make myself miserable in the process. 8. Conflict Phobia. People who love each other should never fight or argue. 9. Self-Blame. The problems in my relationships are bound to be my fault.
Demandingness
19. Brushfire Fallacy. People are clones who all think alike. If one person looks down on me, the word will spread like brushfire and soon everyone will look down on me. 20. Spotlight Fallacy. Talking to people feels like performing under a spotlight on a stage. If I don't impress people by being sophisticated, witty, or interesting, they won't like me. 21. Magical Thinking. If I worry enough, everything will turn out okay.
Other
10. Other-Blame. The problems in my relationships are the other person's fault. 11. Entitlement. You should always treat me in the way I expect. 12. Truth. I'm right and you're wrong.
* Copyright
18. Perceived Narcissism. The people I care about are demanding, manipulative, and powerful.
22. Low Frustration Tolerance. I should never be frustrated. Life should be easy. 23. Superman / Superwoman. I should always be strong and never be weak.
2001 by David D. Burns, M.D.
Chapter 33
Page 1184
Answer Danielle and I found several SDBs in her thoughts: Other-Blame. The problems in my relationship with Suni are her fault. She shouldn't be so ungrateful or critical of my efforts, especially when her criticisms are so unfair and irrational. Entitlement. I'm entitled to patients who respect me and appreciate my efforts to help them. Low Frustration Tolerance. Things should always go smoothly. If things don't go the way I like, then I'm bound to feel upset. Conflict Phobia. People with good relationships shouldn't fight or argue. If two people aren't getting along, they should end their relationship. Emotional Perfectionism. I should try to be happy all the time. Happiness is the point of life. There seemed to be some narcissism operating as well. Although we all like to imagine that we're incredibly humble and caring, it's easy to let our egos get in the way. I can think of lots of times when I also felt annoyed or resentful because a patient didn't seem to appreciate my efforts on his or her behalf. Empathy and Agenda Setting are two techniques you have to be ready to use at any moment during a therapy session, and they're every bit as important when you're teaching. In fact, Empathy has to be seamlessly integrated into everything we do, and it will be especially important whenever the other person is upset. Similarly, you should be poised to do Agenda Setting at any moment when you suspect a motivational issue has surfaced.
Chapter 33
Page 1185
When we did the Downward Arrow Technique, it seemed like Danielle was struggling with some ambivalence about her residency training. She said that the demands of the program were overwhelming and that she frequently had to work with people she didn't like. She also felt like she had to please many attending psychiatrists with conflicting orientations. And most important, she said that she could be doing something far more appealing and rewarding, like traveling around the world. Imagine that you're working with Danielle. What would you say to her in order to set the agenda at this point during the session? Put your ideas here:
When you're done, you can turn the page.
Chapter 33
Page 1186
Answer There are lots of ways you could assess Danielle's motivation. Here's one approach: "Danielle, perhaps you really could be traveling around the world and doing lots of exciting things. Are you saying you might prefer that? The fact is, psychiatry can be frustrating, and we often have to deal with ungrateful, irritating patients. In fact, if there weren't so many difficult patients seeking help, we'd be out of business. "Furthermore, the residency experience definitely has all the hassles you described. I believe you have a lot of talent, and a terrific aptitude for psychiatry, but there's no rule that says you have to pursue this career. What are your feelings about this?" The important thing is to convey respect and to explore this issue with Danielle collaboratively. If she senses that you're trying to persuade her to stay in the residency program, she may feel the need to resist, and you may end up on opposite teams. It may be more productive to ask Danielle why she should stay in the residency program, given all the other appealing options that are tugging at her. Danielle indicated that she was committed to sticking with the residency program, in spite of the frustrations, and didn't have any plans to leave. However, she emphasized her desire to try to change the way she was thinking and feeling about her work with Suni. I decided to try a very challenging technique and see if Danielle could hit the ball out of the park.
Chapter 33
Page 1187
Externalization of Voices You probably recall that the Externalization of Voices is the most powerful CBT technique of all because it transforms intellectual understanding into real emotional change. I proposed that the other residents in the supervision group could play the role of Danielle's negative thoughts, and attack her by saying the same things she was saying to herself, using the second person, "You." I asked Danielle to play the role of the positive, self-loving part of her brain, using the first person, "I." Her job was to defeat the negative thoughts using the Self-Defense Paradigm, the Acceptance Paradox, or both. The dialogue went like this: Danielle's Negative Thoughts (played by group): Life is too short to spend an hour of your week with someone you don't like. Danielle's Positive Thoughts (played by Danielle): It's true that life is short, but I don't think an hour a week is too long to spend with Suni. It's great to have happy, easy experiences, but life might get a little boring if everything were easy. These challenges feel awkward sometimes, but they provide me with opportunities to learn and grow. Danielle's Negative Thoughts (played by group): Yes, but you know very well that life should be easy. The point of life is to be happy all the time. You shouldn't have to put up with so many annoying patients. Danielle's Positive Thoughts (played by Danielle): That's an appealing fantasy, but I've found that when life is too easy, and I don't have any obligations or responsibilities, I actually feel less happy. Challenging experiences add richness to life. During my internship, when
Chapter 33
Page 1188
I only had one weekend a month off, I really looked forward to those weekends, and I relished my time off, even if I didn't have anything special planned. Even something as simple as going shopping or going to bed after a night on call would feel really wonderful. Danielle's Negative Thoughts (played by group): That may be true, but you know that psychiatry residency isn't worth it. You have no control over your schedule and you have too many masters to please. You deserve to be doing something fun, like traveling around the world. Danielle's Positive Thoughts (played by Danielle): There are definitely many challenging aspects of residency, such as not having the control I'd like over my schedule and having to figure out how to work with all the different attending psychiatrists. However, it's something I want to do to get to my desired goal of being a psychiatrist. I really enjoy psychiatry because it's intellectually fascinating to me and because there are so many facets to our profession. What could be more interesting than thinking about how the mind works? Plus, it appeals to my nosy side. I get to hear all the intimate details of people's lives. And it feels great to help someone feel better. There are actually many parts of residency that I enjoy, so it's really not so bad. As you can see, Danielle was winning every exchange. She agreed, and said that the negative thoughts no longer upset her. Several themes had emerged: I have free choice. This is a path that I've chosen. Becoming a psychiatrist is
Chapter 33
Page 1189
something I want to do. The friction and frustration are an inherent part of the growing and learning process. If everything were smooth and easy, the experience would be boring and there'd be no growth. Perfect patients might not be that much fun to work with. Psychiatry is multi-faceted, with so many areas to explore, and I get the chance to look into the human mind and spirit and share people's deepest secrets. This is an opportunity that most people never get. Danielle's completed Daily Mood Log appears on pages 1190 – 1191. As you can see, her belief in all the negative thoughts went down considerably, and her negative feelings went down all the way to 0%. Danielle responded much more rapidly than the average patient because she was highly motivated and already familiar with the techniques. But what if she still believed one or more of her negative thoughts, and was still feeling upset? For example, she might still believe this thought: "Maybe she's right and I am a bad therapist." You can put this thought in the middle of a Recovery Circle and select a variety of techniques to attack it. Then try them out, one by one, until Danielle no longer believes the thought. When you're done, remember to use the Externalization of Voices to make certain that she can put the lie to all her negative thoughts in a convincing fashion.
Chapter 33
Page 1190
Danielle's Daily Mood Log* Situation or Event: Being criticized by Suni. % Before
% After
% Before
% After
Sad, blue, depressed, down, unhappy
50%
0%
Embarrassed, foolish, humiliated, self-conscious
60%
0%
Anxious, worried, panicky, nervous, frightened
30%
0%
Hopeless, discouraged, pessimistic, despairing
50%
0%
Guilty, remorseful, bad, ashamed
20%
0%
Frustrated, stuck, thwarted, defeated
90%
0%
Inferior, worthless, inadequate, defective, incompetent
20%
0%
Angry, mad, resentful, annoyed, irritated, upset, furious
80%
0%
Lonely, unloved, unwanted, rejected, alone, abandoned
—
—
Other (describe)
Emotions
Negative Thoughts
% Before
% After
Emotions
—
Distortions
Positive Thoughts
% Belief
1.
Screw you! I don't like you either!
100%
5%
AON; OG; MF; DP; MAG; ER; SH; LAB; OB
1. Suni can be critical and difficult. This is challenging, but also exciting, because her difficulty getting along with people is one of the reasons why she's in therapy.
100%
2.
Suni's criticisms aren't true.
70%
0%
AON; OG; MF; DP; MAG; SH; LAB; OB
2. There's definitely an element of truth in her criticisms. But more importantly, this is a chance for us to form a more meaningful relationship and work together more effectively.
90%
* Copyright
1984 by David D. Burns, M.D. Revised 2003.
Chapter 33
Page 1191
Danielle's Daily Mood Log (cont'd) % Before
% After
3. She's ungrateful.
100%
4. She's not being fair.
Negative Thoughts
% Belief
Distortions
Positive Thoughts
5%
AON; OG; MF; DP; MAG; ER; SH; LAB; OB
3. It would be wonderful if all my patients were grateful, but that's not very realistic. Once we've begun to work together more effectively, she'll probably feel more positive about our work.
100%
100%
0%
AON; OG; MF; DP; MAG; ER; SH; LAB; OB
4. The fact is, I urged her to criticize me. Now I can't complain that she's being unfair, just because her criticisms sting!
100%
5. Maybe she's right and I am a bad therapist.
70%
2%
AON; OG; MF; DP; MR; MAG; ER; SH; LAB; SB
5. She does have a point with some of her criticisms, but this doesn't mean I'm a "bad therapist." This conflict is a great opportunity for both of us. Discussing my patients' negative feelings about me is a sign of good therapy.
100%
6. She's a horrible person.
70%
0%
AON; OG; MF; DP; MAG; ER; SH; LAB; OB
6. She's a human being, with strengths and weaknesses, just like everyone else.
100%
Chapter 33
1192
Because Danielle was feeling better, we began to work on how she could respond to Suni's criticisms. Suni's criticisms sting, so people usually pull away and reject her. Without the judgment that this "should not" be happening, it becomes a fascinating clinical challenge, especially if Danielle can explore these feelings with Suni in a way that feels safe and collaborative. Imagine that you were Suni's therapist, and indicate how you'd respond to each of her criticisms, using the Five Secrets of Effective Communication. Write your responses below. Indicate the techniques you used in parentheses after each sentence you write. You can use the following abbreviations: DT = Disarming Technique; TE = Thought Empathy; FE = Feeling Empathy; IN = Inquiry; IF = "I Feel" Statement; and ST = Stroking. I would recommend that you review the answer to each problem after you've written your response. That way, your understanding and skills will evolve progressively. For your convenience, I've listed the page number where the answer appears after each problem. Communication Exercises 1. "You're clumsy and awkward during sessions. Sometimes it seems like you don't know what you're doing."
My answer appears on page 1194.
Chapter 33
1193
2. "You talk about yourself too much. I come to therapy to discuss my issues, not to hear your stories!"
My answer appears on page 1195. 3. "Nobody could ever understand me. How can you pretend to know how I feel, since you can't get inside my head and know my thoughts and feelings?"
My answer appears on page 1196. 4. "You don't listen to what I'm saying. For example, if I said, 'My brother died,' you'd probably say, 'Let's get back to work on your Daily Mood Log.'"
My answer appears on page 1197.
Chapter 33
1194
Answers to Communication Exercises When you read my analyses below, you may notice that there's some overlap in the recommended therapist responses to Suni's criticisms. Of course, you shouldn't say the same things over and over in a real-life interaction with your patient, because you'll sound like a parrot! When you respond to the patient's first criticism skillfully, a natural conversation will evolve. Please take this into account as you review this material. 1. "You're clumsy and awkward during sessions. Sometimes it seems like you don't know what you're doing." Comment: There's definitely some truth in Suni's criticisms. Danielle feels awkward during her sessions with Suni, so she tries hard to act professional. This has the opposite effect and she appears forced and unnatural. Danielle and Suni don't flow because Danielle feels, quite correctly, like she's constantly being judged, but Suni seems reluctant to discuss her negative feelings. According to the Law of Opposites, when you defend yourself against the patient's criticisms, the patient will conclude that she or he was right about you. In contrast, when you find truth in the criticism, you put the lie to it. But how can Danielle gracefully agree that she's awkward and clumsy? Residents have told me that the criticism they're most afraid of hearing from patients is, "Aren't you just a trainee? I thought I was going to see a staff psychiatrist." Any statement from patients that hints at a lack of skill or experience seems very threatening to residents, who feel understandably vulnerable and unsure about their abilities.
Chapter 33
1195
Here's one approach: "You know, Suni, you're absolutely right, and I'm glad you brought that up. (DT; IF) Sometimes I have felt a bit awkward during our sessions, and I've been trying to figure out why. (DT; IF) I've wondered if I might be trying a bit too hard, because I don't want you to be disappointed in the work we're doing. (ST) I can imagine that you might be feeling frustrated with me as well. (IN; FE) Tell me what it's been like from your perspective. (IN)" 2. "You talk about yourself too much. I come to therapy to discuss my issues, not to hear your stories!" Comment: Most patients seem to like it when the therapist tastefully shares a personal experience that has a good teaching point. It makes the therapist seem more human and accessible, and can be quite inspiring to the patient. However, some patients are quite narcissistic and want all the attention to be focused on them. The key here is to tune in to Suni's feelings. She may feel hurt or lonely, but expresses these feelings aggressively. The anger may be her defense against the hurt feelings. One key to responding to a critical, narcissistic patient is to try to acknowledge the thinly disguised feelings of sadness, rejection, loneliness or disappointment when the patient lashes out angrily. Danielle might be the first person she's had a chance to explore these feelings with, since other people will probably find Suni's aggression too distasteful, and will simply avoid her. With this in mind, Danielle could say:
Chapter 33
1196 "Suni, you're absolutely right. (DT) This time is for you. (DT) I can
imagine you might be feeling annoyed with me when I talk about myself instead of listening to you. (TE; FE) Can you tell me a bit more about how you're feeling? (IN)" This is the Law of Opposites again. When Danielle agrees that she hasn't been listening, she is listening. Instead of getting defensive, Danielle is giving Suni the chance to express her negative feelings directly. If Suni opens up, Danielle can ask about any feeling of disappointment or loneliness that may be hiding underneath the anger. Danielle's response is an invitation to intimacy. She's showing Suni that the door is wide open. Suni will have to decide whether or not she wants to accept the invitation and step inside. 3. "Nobody could ever understand me. How can you pretend to know how I feel, since you can't get inside my head and know my thoughts and feelings?" Comment: This one is easy. All Danielle has to do is agree with Suni, and encourage her to talk some more about the problem, along these lines: "Suni, you're right. (DT) Other people can never completely understand how we're thinking and feeling. (TE; DT) Furthermore, I don't think I've done a very good job of tuning in to how you're thinking and feeling, and I can imagine you might be a bit annoyed with me. (TE; FE) I'm wondering, too, if you might be feeling lonely and alone, since you say that nobody could ever understand you. (IN; FE; TE) What you're
Chapter 33
1197
saying is incredibly important. (ST) What are some of the feelings that have been especially difficult to get across? (IN)" If Danielle doesn't take the bait and get defensive, Suni's criticism will provide a perfect opportunity for them to connect in a more meaningful way. Paradoxically, the moment Danielle agrees that she hasn't understood Suni, she's proving that she does understand, because she's accepting Suni's thoughts and feelings. In other words, at the precise moment that Danielle agrees that she's failed, the failure suddenly disappears and she achieves success. Of course, Danielle's tone will be vitally important or the technique could backfire. She'll have to convey these messages with genuine curiosity, selfesteem, and respect for Suni. Because Suni is quite narcissistic, Stroking will be especially important. If Danielle does this skillfully, Suni will probably lower her defenses and open up. 4. "You don't listen to what I'm saying. For example, if I said, 'My brother died,' you'd probably say, 'Let's get back to work on your Daily Mood Log.'" Comment: Suni is sending a message on two different levels. On the surface, she's complaining that Danielle isn't paying attention to her. Once again, there may be some wounded narcissism. Suni wants to be the center of attention and she may be involved in a power struggle with her therapist. At the same time, Suni is hinting about some tender feelings that Danielle may not have acknowledged. Suni may be feeling sad and lonely, but protects herself from these vulnerable feelings by lashing out angrily. With this in mind, Danielle could say:
Chapter 33
1198 "Suni, I can see how that would be hurtful and unprofessional.
(FE) I've also felt like I haven't done a very good job of listening to how you feel. (TE; DT) I can imagine that you might be feeling ticked off at me for missing the boat so badly. (FE) I think this is exactly what we need to talk about right now. (ST) Can you tell me more about ways that I've let you down? (IN)" Therapeutic failures are difficult, if not impossible, to avoid. They happen all the time. Sometimes we feel ashamed because we have the fantasy that other therapists are far more skillful and effective. In reality, most of us fail to live up to the lofty standards we imagine, and react to challenging patients in ways that are pretty human. The good news is that those moments when the therapeutic relationship seems to be falling apart nearly always provide us with our best opportunities for personal and therapeutic breakthroughs.
Part Nine A-Team Revisited
34*
The Therapist's Report Card
Frequent failure is a necessary and important part of therapy. Once you've pinpointed the precise reason for the impasse, you can often transform your worst clinical failure into your greatest therapeutic success. Therapeutic failure nearly always results from a therapist error in one or more of the following five dimensions: A = Assessment. Did you complete a comprehensive Axis I and Axis II diagnostic survey at the initial evaluation? Did you make the patient accountable and flush out any hidden agendas that could sabotage the treatment later on? T = Testing. Are you monitoring progress in several dimensions at every therapy session using brief, accurate self-assessment tests? E = Empathy. Do you have a warm, vibrant, trusting therapeutic alliance with
* Copyright
2003 by David D. Burns, M.D.
Chapter 34
Page 1201
this patient? Does she or he feel supported, accepted, and understood? Are you monitoring the quality of the therapeutic alliance and helpfulness of the therapy at every session using the Empathy and Helpfulness scales on the Evaluation of Therapy Session,* or some comparable instrument? A = Agenda Setting. Have you developed a meaningful, collaborative therapeutic agenda with this patient? Does the patient want to change, or simply talk about how bad his or her life is? Have you identified a specific problem the patient wants help with? Have you correctly conceptualized the problem? Have you anticipated and negotiated the patient's resistance before jumping in and using a variety of techniques aimed at helping the patient? Is the patient working hard and consistently doing psychotherapy homework between sessions? M = Methods. Are you using methods that are appropriate for the patient's problem? For example, if the patient is depressed or anxious, have you filled out the Daily Mood Log in a step-by-step manner? Have you selected at least 15 techniques from the list of 50 Ways to Untwist Your Thinking that will help the patient put the lie to his or her negative thoughts? If the patient is struggling with a relationship problem, have you done Interpersonal DecisionMaking and completed the Relationship CBA? Are you using the Revise Your Communication Style form? If the patient is struggling with an addiction or
*
You can review this instruments on page 203. If you are interested in using this instrument in your clinical practice, send an email to [email protected]. Therapist's Toolkit purchase includes license for unlimited reproduction of an extensive variety of assessment and treatment tools.
Chapter 34
Page 1202
habit, are you using Motivational Techniques such as Agenda Setting, the Paradoxical CBA, and the Devil's Advocate Technique? A multidimensional assessment of therapeutic failure is important because different kinds of therapeutic failure will respond to different kinds of corrective interventions. For example, if the patient keeps yes-butting you and complaining that the therapy isn't helping, you've probably made empathy and Agenda Setting errors. Although it may be tempting to keep trying more and more CBT techniques, it won't help. You simply can't correct empathy problems or Agenda Setting failures this way. If the patient doesn't feel understood, or isn't committed to change, the best therapy techniques in the world won't work. You and your patient will have to work hard together, with a spirit of understanding and mutual respect, in order to be successful. Therapeutic empathy won't usually solve an Agenda Setting problem, either. You may be a terrific listener, and your patient may appreciate your understanding, warmth and compassion, but if she or he has mixed feelings about recovery, all the listening in the world won't lead to change. By the same token, if there's been a failure of empathy, you won't be able to solve the problem with Agenda Setting, or by using more treatment techniques, because the patient will feel the urge to resist anything you suggest. I don’t mean to be pessimistic. It's actually pretty easy to diagnose and correct these errors. For example, if there's an alliance failure, you'll see it right away because your score on the Therapeutic Empathy scale will be less than 20. In addition, you may sense that you don’t feel very close to the patient, either.
Chapter 34
Page 1203
This can be a great opportunity, because you can use the Five Secrets of Effective Communication to explore and repair the problem. Additional practice with the exercises in Part IV of this book can get you up to speed. As we review the five components of the A-TEAM model in more detail, I'd like you to think about one patient you feel stuck with. After you've read each section, fill out the corresponding section of the Therapist's Report Card on page 1227. You can also use the Therapist's Report Card when you discuss challenging patients in case conferences and supervision sessions. This will help you think about your patients far more systematically and sharpen your therapeutic skills. If you get a bad grade on the Therapist's Report Card at first, don't get discouraged! This is actually a good thing. You can think of it as the first step toward success with a patient you've been stuck with.
A = Assessment Therapists typically make four types of errors during the initial evaluation, including diagnostic errors, conflict of interest errors, motivational errors, and errors of conceptualization: Diagnostic Errors Did you do a structured, systematic Axis I and Axis II diagnostic screening using DSM-IV criteria? Most therapists do not do comprehensive diagnostic screening interviews at intake because they're so cumbersome and timeconsuming. However, nearly all patients will have many problems in addition to
Chapter 34
Page 1204
the problem they're seeking help for. If you use the Easy Diagnostic System described in Chapter 4, you'll develop a reasonably accurate understanding of every patient's Axis I and Axis II problems, and it will only require about 10 minutes of your time. It will be much easier to identify any hidden problems, such as substance abuse, a marital conflict, or Borderline Personality Disorder, that may come back to sting you later on if they aren't identified and addressed. Conflicts of Interest Have you asked about any competing motives that might create a conflict of interest? Is the patient pursuing a lawsuit or disability claim? Does she or he expect you to support this claim? Remember that patients who use psychotherapy to get money rarely recover. Treating patients under these conditions is naïve at best, and in some cases could be considered an ethics violation, because you're involved in a rather glaring conflict of interest. I ask patients if they're involved in any disability claims, lawsuits, or other forensic problems at the intake evaluation. If the answer is yes, I tell them that I don't do forensic work. For example, I don't sign disability papers for patients I'm treating, and I don't testify for patients in court. However, I can refer them to a forensic expert who can handle these issues for them. A few patients have become indignant and refused to work with me when they learned that I couldn't treat them and certify them for disability at the same time. Most prospective patients have understood the wisdom behind this policy and have continued to work with me, with the understanding that I wouldn't provide any information,
Chapter 34
Page 1205
positive or negative, to any expert who represented them legally. If they remain depressed, I won't testify to this fact, and if they recover, I won't tell anybody. This clears the decks and allows you to unearth any financial motives that could lead to therapeutic failure later on. The rationale for this policy should be obvious. As human beings, we're easily tempted. If the patient plans to use therapy to get money or win a legal battle, then you're not really involved in therapy, and your attempts to help that patient are not likely to be effective. Motivational Errors Why is the patient seeking therapy at this particular time? What are the patient's goals for therapy? Is someone else pressuring the patient to seek therapy? Is the presenting problem something that the patient really wants help with? How hard is the patient willing to work if you agree to work with him or her? Are there any problems the patient hasn't disclosed, perhaps because of feelings of shame? In Chapter 15, you learned about the eight types of therapeutic resistance, including Outcome Resistance and Process Resistance for depression, anxiety, relationship problems, and addictions. Although you'll negotiate therapeutic resistance at the Agenda Setting step in subsequent therapy sessions, you can also address it at the intake evaluation. There are two basic questions: First, does the patient really want to get better? Second, is the patient ready, willing and able to do what it's going to take to get better? For example, if your patient just received a DUI and was ordered by the
Chapter 34
Page 1206
court to seek help, he may not be motivated to stop drinking because he loves to drink. In addition, he may not have the slightest interest in joining AA or doing the hard work of therapy. He may just be paying you a visit to pacify the judge. If you naïvely try to "help" him without assessing his motivation and making him accountable, your therapeutic efforts will probably be doomed to failure. Errors of Conceptualization Do you really know what makes this patient tick? Have you conceptualized where this patient is coming from and what kinds of problems she or he wants help with? You can't simply apply therapeutic interventions without understanding your patient in depth, as a human being. What's going on in this person's life? What attitudes or beliefs are triggering the symptoms? What are the patient's negative thinking patterns? What problems and feelings is the patient struggling with? Is there something important that the patient hasn't disclosed, such as drug use, violent or suicidal urges, or an unusual sexual fantasy, because of feelings of shame or embarrassment? I once treated a severely depressed nurse named Virginia who'd suffered from decades of horrific depression. Although she was highly motivated, hardworking, and intelligent, she simply couldn't put the lie to any of her self-critical thoughts. She could see that her negative thoughts were irrational and distorted, but she still ripped herself to shreds relentlessly all day long. After we'd worked together for about six weeks, Virginia confessed that she'd been sexually abused by a babysitter from the time she was 5 years old
Chapter 34
Page 1207
until she was 10. It was one of the most horrific stories of sexual abuse that I'd ever heard. The babysitter threatened to kill her baby sister if she ever told on him, so she simply endured the suffering in silence for five years. When Virginia was 10, the babysitter was shot and killed in a barroom brawl. She was relieved, and was never sexually abused again. But even though the babysitter couldn't hurt her any more, she felt so ashamed that she never told anyone about the abuse. In fact, I was the first person she'd ever told. She'd been hanging on to her dreadful secret for nearly four decades. This information put Virginia's depression into an entirely different perspective, and I could understand the source of the self-hatred she was struggling with. We were able to work together far more effectively, and within a month, she'd recovered from the overwhelming depression and self-loathing that had plagued her since childhood. Errors of conceptualization are particularly common when treating patients with anxiety disorders because they nearly always have hidden problems they've been sweeping under the rug. If you focus exclusively on their symptoms, without bringing the hidden problems to conscious awareness, the treatment may only be partially effective. Sometimes we misperceive the nature of the patient's problem, even when the patient has it right. A woman named Trina complained that her husband didn't love her any more. She was convinced that he was having an affair and was going to leave her. Trina's therapist was just learning cognitive therapy and encouraged her to identify the distortions in her thoughts, like All-or-Nothing
Chapter 34
Page 1208
Thinking, Mind-Reading, Fortune-Telling and Emotional Reasoning. Trina began to yes-but her therapist and insisted that he just didn't understand. She seemed oppositional, and they were soon locked in a power struggle. In fact, Trina wasn't being resistant. Her perceptions about her husband were correct. He was having an affair and he didn't love her any more. But the young therapist was so eager that he swooped in with his CBT interventions before he'd empathized and assessed what was really going on. Please turn to page 1227 and complete the Assessment section (item 1) of the Therapist's Report Card now.
T = Testing Our perceptions about how our patients feel will often be very different from the way they actually do feel. For example, you may believe patients are improving when they're not. Or, you may believe that patients aren't making any progress when they've improved a great deal. If you ask patients to complete the Brief Mood Survey between therapy sessions and report their scores at the beginning of each subsequent session, you'll be able to track therapeutic progress—or the lack of progress—accurately. You'll get immediate feedback about what's working and what's not. If the testing reveals that your interventions are not effective, you can change your strategy and try a different approach. But if you don't know that you're failing, you'll be stuck indefinitely. If the testing indicates that the patient is making progress, you're probably
Chapter 34
Page 1209
on the right track. In this case, I'd ask the patient which technique, activity or idea seems to be helping the most so I can do more of the same. I may learn that the patient felt excited about the Acceptance Paradox during an Externalization of Voices role-play. Alternatively, the Pleasure Predicting Sheet, Cost-Benefit Analysis, or Hidden Emotion Technique may have been helpful. Once patients begin to improve, I encourage them to pour on the coals and push hard, because complete recovery may be only a few weeks away. Please turn to page 1227 and complete the Testing section (item 2) of the Therapist's Report Card now.
E = Empathy You can't get anywhere without empathy. The patient has to like you and feel accepted and understood, or all bets are off. Does the patient: Feel that you're warm and caring? Trust you? Believe that you understand how she or he feels inside? Feel accepted? Think that you're genuine and down-to-earth? Alternatively, does the patient feel: Anxious during sessions? Intimidated? Judged? Misunderstood?
Chapter 34
Page 1210
Frustrated? Annoyed with you? Research indicates that therapeutic warmth and understanding have moderately strong positive effects on recovery. On average, patients who rate their therapists as warm and caring improve the most rapidly. However, most of us cannot accurately judge how empathic we are, or how our patients see us. Your perceptions of your own warmth and understanding will often be very different from the way your patients view you. When you think you're coming across in a warm, professional manner, the patient may feel turned off, or vice versa. Furthermore, your patients' perceptions of your empathy will be valid, but your own perceptions will not be. Research studies indicate that patients' assessments of therapist empathy accurately predict the degree of recovery, but therapists' self-assessments of their own empathy do not. Your patients' verbal reports of your empathy may not be accurate, either. If you ask patients how they feel about the therapy, they will nearly always say you're doing "fine," even when you're not. The only way to get accurate information is to ask your patients to rate you after each session using an assessment instrument like the Therapeutic Empathy scale on page 203. Anything less than a perfect score on this scale indicates a significant alliance failure that needs to be explored. Even a score of 19 out of 20 on this test indicates a failure in the therapeutic alliance. Most therapists are surprised to discover that they receive unsatisfactory empathy ratings from 50% – 100% of
Chapter 34
Page 1211
their patients when they first use this instrument. This can be a shock to the system. The good news is that if you use this scale routinely with all your patients, and you learn to respond to their criticisms non-defensively using the Five Secrets of Effective Communication, you can rapidly develop vastly improved empathy skills. Many therapists have told me that they began to receive perfect empathy scores from 80% – 90% of their patients after they practiced these techniques and used the Therapeutic Empathy scale consistently for several weeks. Please turn to page 1227 and complete the Empathy section (item 3) of the Therapist's Report Card now.
A = Agenda Setting One of the unique features of CBT is that the patient is the boss. Unlike some forms of therapy, where the therapist plays the role of expert, CBT is highly collaborative. We have numerous tools to offer our patients, but they have to tell us what they want to accomplish. Therapy probably won't be effective unless you and your patient are both working hard on a problem that the patient desperately wants help with. This means that the patient is working hard both during and between sessions. If you and the patient just talk about things in a general way during sessions, without rolling up your sleeves and focusing on something specific, you probably won't get anywhere. Nearly all therapeutic failure results from Agenda Setting errors, or from
Chapter 34
Page 1212
the therapist's failure to set the agenda in the first place. If the patient resists or argues with you during sessions, or if you feel like you're doing all the work while the patient sits back and "yes-buts" you, then you have an Agenda Setting problem. Agenda Setting may seem obvious and overly basic at first, but it's the most difficult topic in psychotherapy. The basic idea behind Agenda Setting is that our patients must be accountable for their own recovery. It's not our job to persuade them to change. Instead, it's their job to persuade us to work with them. These ideas may represent a profound paradigm shift for many therapists, and can be difficult to comprehend at first. You may recall that there are five steps in Agenda Setting: The Invitation Specificity Conceptualization Motivation Methods You'll have to complete all five steps at every therapy session. In some cases, it will be easy and automatic. Some patients come to sessions prepared. They've done their homework and they know exactly what they want help with. They set the agenda for you. But at least half of your patients will not have clear agendas, and they'll be ambivalent about change. You won't be able to help these patients until you master the art of Agenda Setting. If your answer to any of the following questions is yes, you probably have
Chapter 34
Page 1213
an Agenda Setting problem: Do you feel like you're working harder than your patient? Does the patient yes-but you? Does the patient tend to talk on and on, jumping from complaint to complaint, without focusing on any specific problem? Does the patient blame others and insist that he or she shouldn't have to change? Do you feel frustrated, anxious or annoyed when you think about the patient? Do you dread your sessions with this patient? Do you feel like the patient isn't making any real progress? You may also have an Agenda Setting problem if your answer to any of these questions is no: Are you and your patient working hard together on a problem that the patient strongly wants help with? Does the patient agree with your assessment of the problem and feel that your therapeutic interventions are helpful? Is the patient satisfied with the therapy? Does the patient consistently do psychotherapy homework between sessions? Your patients' perceptions of the helpfulness of the therapy will often be very different from your own. You may feel that the therapy is going superbly, but the patient may feel that you're not making any progress at all. Or, you may feel
Chapter 34
Page 1214
like you're spinning your wheels when the patient thinks the sessions are quite helpful. The Helpfulness scale on the Evaluation of Therapy Session form will show how your patients feel about the quality of your therapeutic interventions. They can fill it out, along with the Therapeutic Empathy scale, in the waiting room before they leave, or at home between sessions. You can discuss the patient's responses at the beginning of the next session. Agenda Setting errors are extremely common and hard to avoid. Even the most sophisticated therapists seem to stumble. Here are a few tips that will help you navigate each step successfully: The Invitation Some therapists jump into a helping mode before they've asked their patients if they feel ready to roll up their sleeves and get to work. In this era of managed care, many of us feel pressured to treat patients quickly. You may feel like you don't have enough time to listen and form a solid relationship with the patient. However, premature attempts to rush into problem-solving mode will nearly always slow the therapy down. If you don't listen, patients will feel frustrated and invalidated, and will resist your efforts to help them. Some therapists make the opposite mistake. They allow the patient to talk on and on indefinitely, without ever focusing on solving any specific problems. The therapy may drag on for years without any tangible, measurable progress. Agenda Setting is a powerful technique that may intimidate the patient. We're really asking the patient these kinds of questions:
Chapter 34
Page 1215
"Is there a problem you want help with?" "Can you give me a specific example of the problem you want help with? What time of day was it? Where were you? What was going on?" "If I agreed to help you with this problem, how hard would you be willing to work, during and between sessions?" Some patients—especially those with Borderline Personality Disorder (BPD) or Narcissistic Personality Disorder (NPD)—may become defensive or angry in response to these kinds of questions. They may not want to assume any responsibility for working hard to change their lives. They may want you to change them via magic while they sit back, complain and resist your efforts! If the patient becomes irate and lashes out at you when you're trying to set the agenda, what are you going to say or do next? Put your ideas here before you turn the page:
Chapter 34
Page 1216
Answer Any time your patient gets upset or resists, empathy will be the only effective response. Even though empathy and Agenda Setting are inherently different processes, they need to be seamlessly integrated. If the patient gets upset or resists when you try to set the agenda, put all your techniques on the shelf and try to see the world through the patient's eyes. Listen and validate what the patient is saying. Surrender and go where the patient leads you. When the patient feels accepted, and trust has been reestablished, you can try the Invitation step again, with a question along these lines: "Mel, you've done an excellent job describing the problems you're struggling with, and I can only imagine how angry, overwhelmed and defeated you must feel. I'm wondering if you want some help with the problems you're describing, and if this would be a good time for us to work on one of them. Alternatively, you may feel like you need more time to get your feelings off your chest. I want to make sure I understand exactly how you're feeling, and I don't want to rush to the next level until you feel ready." Specificity The Specificity step is based on two powerful ideas. First, all the patient's problems will be embedded in any one moment when she or he was feeling upset. When you understand how the patient was thinking, feeling, and behaving at that moment, you'll understand the cause of all his or her problems. Second, when patients learn how to change the way they were feeling at that moment,
Chapter 34
Page 1217
they'll suddenly understand the solution to all their problems. Many patients and therapists indulge in lengthy, general discussions about all the problems in the patient's life. CBT can only be effective if the patient is willing to focus on one specific problem or moment when she or he felt upset. The problem can be anything, but it has to be real and specific as to person, place, and time. For example, the patient may have felt: Discouraged and frustrated following a meeting with her boss yesterday. Upset during an argument with his wife on Tuesday. Terrified during a panic attack earlier in the week. Guilty after an eating or drinking binge last night. Worthless and panicky when getting out of bed this morning. Ask yourself these questions: Has the patient identified a real problem that she or he wants help with? What day of the week was it? What time of day was it? Where was the patient? What was going on? Does the patient really want help with this problem, or does she or he simply want to talk about it? Is the patient willing to work exclusively on this problem for a number of sessions, and work hard on solving it between sessions? Are you comfortable with the patient's agenda? Are the patient's goals realistic? Some patients will ask for things that aren't consistent with your understanding of how effective therapy works. For example, a shy man may
Chapter 34
Page 1218
want you to make his anxiety go away before he tries flirting and interacting with people in social situations. This involves putting the cart before the horse. Or, a patient who procrastinates may want you to boost his motivation so he'll feel like doing the task he's been putting off. Or, a depressed, alcoholic woman with a troubled marriage may want help overcoming her mood problems, without having to address her alcoholism or marital problems. Are you comfortable with the patient's agenda from an ethical perspective? A radiologist named Ralph felt guilty and inadequate because he made so many errors reading x-rays. He was embarrassed and ashamed because his diagnostic errors were frequently exposed during case conferences at his hospital. Then he'd beat up on himself and tell himself, "I shouldn't have made that mistake. Even a medical student would have gotten it right. What's wrong with me? One of these days, I'm going to goof up and kill somebody." You could probably use CBT techniques to help Ralph overcome the constant feelings of shame and inferiority that were plaguing him, but it might not be ethical because his medical skills really weren't up to speed. In fact, his diagnoses were frequently incorrect. However, radiologists were in short supply in his community, so he wasn't in any immediate danger of getting fired. I pointed out that Ralph was involved in Should Statements. When he told himself, "I shouldn't have made that mistake," he was fooling himself, because it made him sound far more competent than he really was. Ralph began to think about his errors like this: "Actually, I should have made that mistake because
Chapter 34
Page 1219
my medical skills aren't up to speed. If I don't get more training, I probably will kill somebody." Paradoxically, he felt relieved when he finally accepted his shortcomings. He courageously decided to give up a lucrative position at his hospital so he could pursue two additional years of residency training. He said that the emotional relief and surge in self-esteem far outweighed any financial sacrifices he'd have to make. Conceptualization Once the patient describes a specific moment when she or he was upset, ask yourself what the type of problem it is. Is it: An individual mood problem, such as depression, guilt, anxiety, or panic? A personal relationship problem, such as a conflict with a family member, friend, or colleague? A habit or addiction, like procrastination, alcohol or drug abuse, smoking, or overeating? A "non-problem," like healthy grief, that simply requires empathic listening? A combination of several types of problems? Motivation The Conceptualization step is important because different types of problems will respond to different types of interventions. The techniques I'd use to treat a patient with panic attacks are radically different from the methods I'd use to help someone with a troubled marriage. In addition, each type of problem will present a unique type of resistance.
Chapter 34
Page 1220
The resistance of a depressed patient will be different from the resistance of an anxious patient. The resistance of a patient with a marital problem will be different from the resistance of a patient with a habit like procrastination. Before we swoop in with treatment methods, we'll have to head the resistance off at the pass. You'll have to consider the two different types of resistance for each problem: Outcome Resistance and Process Resistance. For example, a man who abuses alcohol may enjoy drinking and may not see any compelling reason to quit. This would be an example of Outcome Resistance because if he recovers, he'll have to give up his goodies. In contrast, a patient with an anxiety disorder may desperately want to recover, but may not want to endure the intense discomfort of confronting his worst fears. This would be an example of Process Resistance. Change may involve loss. A chronically depressed, angry woman with Borderline Personality Disorder may derive her sense of identity as well as feelings of moral superiority from her role as victim. The self-pity may be painful but addictive. She may also fear a loss of support from her family and friends if she recovers, and may be reluctant to assume the responsibilities that will come with being a happy, fully functioning adult. Sometimes, the status quo subtly rewards the patient. A man with a troubled marriage may not want to develop a more loving relationship with his wife because he enjoys having affairs and secretly wants to get divorced. Or, he may enjoy intimidating his wife with verbal or physical abuse. If you're not aware
Chapter 34
Page 1221
of his hidden motives, you may get frustrated when he sabotages your attempts to show him how to develop a more loving relationship with his wife. Why is it so hard for therapists to see these kinds of motives? I think it's because we're so eager to see our patients in a positive way that we sometimes overlook the dark side of their personalities. When you feel stuck with a patient, ask yourself these questions: Have you accurately pinpointed the reasons why this patient might be reluctant to change? Has the patient convinced you that she or he really wants help with this problem? Has the patient convinced you that she or he is willing to do what's necessary to solve the problem? Is the patient willing to do psychotherapy homework consistently between sessions? Psychotherapy homework can include a wide variety of activities you might assign, such as the Daily Mood Log, Pleasure Predicting Sheet, or Revise Your Communication Style form, as well as any self-help activities that patients initiate on their own. If you aren't getting anywhere with a patient, the odds are high that the patient isn't doing psychotherapy homework between sessions. Recent research suggests that psychotherapy homework plays a vital role in the treatment of depression, anxiety, relationship problems, and addictions. It's not just an optional frill. My clinical experience has been consistent with this research. The patients who work hard to solve their problems between sessions
Chapter 34
Page 1222
seem to improve the most. In contrast, patients who consistently refuse or "forget" to do their homework usually do not improve. In some cases, they may even get worse. Psychotherapy homework functions on two levels. First, it's a powerful behavioral test of the patient's motivation. Patients may give lip service to wanting to change, but the psychotherapy homework is where the rubber meets the road. Second, homework speeds recovery and helps prevent relapses following recovery. CBT is an extremely active form of therapy. We're trying to give our patients the tools for developing greater self-esteem and more rewarding relationships with others, so they won't need to rely on us for the rest of their lives. The best time to deal with the issue of psychotherapy homework is at the initial evaluation, because the patient is not yet legally in your care. After I review the patient's responses to the Concept of Self-Help memo,* I tell them that recovery from emotional or interpersonal problems is no different from learning tennis. It requires hard work and practice. If patients are strongly committed to a form of treatment that does not involve psychotherapy homework, I offer to provide them with a list of fine therapists in the community who do not require their patients to do homework. I make it clear that although I'd love to have the chance to work with them, I probably can't accept them as my patient, because all my patients have to do homework, with no exceptions. Paradoxically, this
* You can read more about the Concept of Self-Help memo on pages 109 and 145.
Chapter 34
Page 1223
nearly always causes a shift in the patient's attitude. Most of them suddenly discover that they do want to stay and are, in fact, committed to working hard between sessions. The key to this intervention is not the educational component, but the motivational component. Remember the Burns Rule: people only want what they can't get, and never want what they can get. If you pursue the reluctant patient, and try to convince them to work with you, they'll lose respect for you and the probability of success will be zero! In contrast, when you project the message that you like the patient, and would love to work with them, but will not pursue them or try to persuade them to do the homework, the power suddenly shifts. Now they have to pursue you, because you're what they can't get. Of all the techniques I've tried to boost homework compliance, this is the only one that's been effective! Please turn to page 1227 and complete the Agenda Setting section (item 4) of the Therapist's Report Card now.
M = Methods This is the fifth step of Agenda Setting and the last letter of the A-TEAM acronym. Your conceptualization of the patient's problem will guide you in the selection of techniques. The CBT techniques that are so effective for depression will not be effective for a patient with a marital problem. The techniques that are the most appropriate for a patient with a marital problem will be quite different from the techniques that would help a patient with a habit or addiction.
Chapter 34
Page 1224
The following questions will help you avoid common errors in the selection of methods for various kinds of problems: General Questions Have you negotiated a meaningful therapeutic agenda before swooping in with CBT techniques? Is the patient strongly committed to solving this problem? Do you use the same general approach with all your patients, or do you use a variety of techniques that have been empirically validated for the specific problem the patient wants help with? Do you feel qualified to treat the problem the patient is asking for help with? Do you have the tools you need to help this patient? Depression and Anxiety Questions Have you and the patient filled out the Daily Mood Log in a systematic, stepby-step manner? Has the patient selected one negative thought she or he wants to work on first and written it down in the middle of the Recovery Circle? Have you selected at least 15 techniques to help the patient put the lie to this negative thought? Are you failing as fast as you can, moving from method to method until you find the one that works for this patient? If the patient is anxious, are you using the Hidden Emotion Technique along with a variety of Cognitive Techniques, Uncovering Techniques, Motivational
Chapter 34
Page 1225
Techniques, and Exposure Techniques? Relationship Problems Does the patient want to develop a more satisfying and loving relationship, or simply want you to listen and agree that the other person is a jerk? Have you used Interpersonal Decision-Making? Does the patient want to leave the other person, settle for the status quo, or work to make the relationship better? Have you done a Relationship Cost-Benefit Analysis? Is the patient willing to stop blaming the other person and assume responsibility for solving the problem? Are you using the Revise Your Communication Style form? Have you pinpointed one specific moment in the relationship that the patient wants help with? What did the other person say, and what did the patient say next? Habits and Addictions Has the patient persuaded you that she or he really wants to give up the habit or addiction? From the patient's perspective, is the addiction really a problem, or more of a solution? Is the habit or addiction working for the patient? Have you explored reasons why he or she might want to maintain the status quo? Is the patient strongly motivated to solve this problem? Or are you trying to persuade the patient to change? Are you using Motivational Techniques, like the Decision-Making Form, the
Chapter 34
Page 1226
Paradoxical Cost-Benefit Analysis, and the Devil's Advocate Technique? Are you using the Daily Mood Log to pinpoint the patient's tempting thoughts, as well as the negative thoughts that create the feelings of guilt, shame, and frustration? Please turn to page 1227 and complete the Methods section (item 5) of the Therapist's Report Card now.
1. Initial Diagnostic Assessment. Did you complete a comprehensive Axis I and Axis II diagnostic survey at the initial evaluation? 2. Clinical History. Did you flush out hidden agendas or conflicts of interest that could sabotage the treatment? Did you assess the patient's motivation and make him or her accountable? Did you ask about disability evaluations or legal entanglements, such as lawsuits, that could bias this patient's response to the treatment? Have you conceptualized the problem properly? 3. Psychotherapy Homework. Did the patient fill out the "Concept of SelfHelp Memo," along with the Self-Help Contract? Is the patient willing to do psychotherapy homework consistently between sessions? 4. Session-by-Session Testing. Do you track changes in symptoms at every therapy session, using instruments that accurately measure depression, suicidal urges, anxiety, anger, and relationship satisfaction? 5. Therapeutic Empathy. Do you have a vibrant, trusting therapeutic alliance? Does the patient feel accepted and cared about? Does the patient rate you on the Therapeutic Empathy scale after every session to indicate how warm, respectful and understanding you were? Are you getting scores of 20? 6. Therapeutic Helpfulness. Does the patient rate you on the Therapeutic Helpfulness scale after every therapy session? Does the patient feel that your interventions are relevant and helpful? 7. Agenda Setting. Invitation: Have you asked if the patient wants something more than listening and support? Specificity: Have you pinpointed one specific moment the patient wants help with? Conceptualization: Have you conceptualized the problem as an individual mood problem, relationship problem, or habit / addiction? Motivation: Have you explored Outcome and Process Resistance? Is the patient ready to change and willing to work hard, if you agree to help him or her with this problem? 8. Methods. Are you using a variety of techniques that specifically target this patient's problem? If it's an individual mood problem, are you using the Daily Mood Log and Recovery Circle, and "failing as fast as you can"? If it's a relationship problem, are you using interpersonal techniques, such as the Revise Your Communication Style form? Total
* Copyright © 2003 by David D. Burns, M.D.
2—Yes
Therapist's Report Card * Instructions. Therapeutic failure usually results from the therapist errors listed below. Think of a patient you're stuck with and use checks ( ) to indicate how well you're doing in each category.
1—Unsure
1227
0—No
Chapter 34
Chapter 34
1228 Scoring Key: Therapist's Report Card
Score
Grade
Interpretation
16
A+
Awesome! Few therapists do this well.
14 – 15
A
Very good. There's only a little bit of room for improvement.
11 – 13
B
Decent, but there are some problem areas to work on.
8 – 10
C
Not so good. There are lots of areas that need work.
4–7
D
Hmmm. What a can I say? Well, the good news is that the reasons for the therapeutic failure should be obvious, and there's lots of room for improvement!
0–3
F
Heck, we've all got to start somewhere. Furthermore, you've done an honest job of pinpointing the reasons for the therapeutic failure. There's nowhere to go but up!
How did you do? Were you honestly able to give yourself a "Yes" in every category? If so, you deserve an A+! If you're like most therapists, you probably had a number of "No" or "Unsure" answers. This will give you some clues about why the therapy is failing and what you can do to get things back on track. The table on the next page will serve as a brief review of the ideas behind the Therapist's Report Card.
Chapter 34
1229
Relative Importance of Each Type of Therapeutic Error Category
Relative Importance
Initial Diagnostic Assessment
Moderately Important
Clinical History
Very Important
Psychotherapy Homework (HW)
Extremely Important
Session by Session Testing
Exceedingly Important
Therapeutic Empathy
Very Important
Therapeutic Helpfulness
Moderately Important
Agenda Setting
Exceedingly Important
Methods
Exceedingly Important
Explanation Most therapists don't do an adequate initial assessment. You can sometimes get away with this; however, you may overlook an important problem, such as Borderline Personality Disorder or Substance Abuse. If the patient has a hidden agenda or conflict of interest you haven't addressed, the likelihood of therapeutic success will be low. Patients who refuse to do psychotherapy homework assignments between sessions generally won't improve, and often deteriorate during the treatment. At my clinical this is mandatory, not optional. Patients who are unwilling to do HW are referred elsewhere for treatment at the initial evaluation. Surprisingly, very few will elect to leave once they know where you stand. We need accurate information to do meaningful therapy, but cannot accurately perceive how our patients feel. Without session-bysession testing, it's difficult to do effective psychotherapy or sound psychopharmacologic treatment. The information on the Suicidal Urges scale can be life saving. Without a warm, trusting therapeutic alliance, the probability of success is low. You cannot accurately assess the alliance without the Therapeutic Empathy scale is sensitive to the smallest failures in the alliance and will show you where you stand in the patient's eyes. You'll see how relevant and helpful your interventions are at the end of every therapy session. Most therapeutic failure results from Agenda Setting errors, or from the failure to set the agenda in the first place. Few patients can overcome challenging emotional or behavioral problems simply by coming to sessions and venting for an hour a week. Agenda Setting allows you to target the most important problem and head off the patient's resistance at the pass. Most therapists rely on a few methods they strongly believe in. This is a serious problem, because there's no single method that will work for everybody. Patients are unique and it's usually impossible to predict which approach will work for a particular individual or problem. If you want to provide effective therapy, you'll need to use lots of techniques and fail as fast as you can.
Appendix
References
1231
References Ackerson, J., Scogin, F., Lyman, R.D., & Smith, N. (1998). Cognitive bibliotherapy for mild and moderate adolescent depressive symptomatology. Journal of Consulting and Clinical Psychology, 66, 685-690. Antonuccio, D.O., Burns, D., Danton, W.G., & O'Donohue, W. (2000). The Rumble in Reno: The psychosocial perspective on depression. Psychiatric Times, 17, 10-13. You can read this article online: http://www.mhsource.com/pt/p000824.html Antonuccio, D.O., Burns, D., & Danton, W.G. (2002). Antidepressants: A triumph of marketing over science? Prevention and Treatment, 5, Article 25. You can read this article online: http://journals.apa.org/prevention/volume5/toc-jul15-02.htm Antonuccio, D.O., Danton, W.G., & DeNelsky, G.Y. (1995). Psychotherapy versus medication for depression: Challenging the conventional wisdom with data. Professional Psychology: Research and Practice, 26, 574-585. Antonuccio, D.O., Danton, W.G., DeNelsky, G.Y., Greenberg, R., & Gordon, J.S. (1999). Raising questions about antidepressants. Psychotherapy and Psychosomatics, 68, 3-14. Arbuckle, J., & Wothke, W. (1999). Amos 4.0 for Windows: User's Guide. Chicago: SmallWaters Corporation (in press). Barlow, D.H., Hayes, S.C., & Nelson, R.O. (1984). The Scientist-Practitioner: Research and Accountability in Clinical and Educational Settings. New York: Pergamon.
References
1232
Barlow, D.H. (Ed.). (2001). Clinical Handbook of Psychological Disorders: A Step-By-Step Treatment Manual (3rd ed.). New York: Guilford Press. Baxter, L.R., Schwartz, J.M., Bergman, J.M., Szuba, M.P., Guze, B.H., Mazziotta, J.C., Alazraki, A, Selin, C.E., Ferng, H, Munford, P., & Phelps M.E. (1992). Caudate glucose metabolic rate changes with both drug and behavioral therapy for obsessive-compulsive disorders. Archives of General Psychiatry, 49, 681-689. Beck, A.T. (1976). Cognitive Therapy and the Emotional Disorders. New York: International Universities Press. Beck, A.T. (1996). Beyond belief: A theory of modes, personality and psychopathology. In P. M. Salkovskis (Ed.), Frontiers of Cognitive Therapy (pp. 1-25). New York: Guilford. Beck, A T., Rush, A.J., Shaw, B.F., & Emery, G. (1979). Cognitive Therapy of Depression. New York: Guilford. Beck, A.T., Steer, R.A., & Garbin, M.G. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8, 77-100. Beck, A.T., Ward, C.H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561571. Beck, J.S. (1995). Cognitive therapy: Basics and beyond. New York: Guilford. Beutler, L. (1998). Prozac and placebo: There's a pony in there somewhere. Prevention and Treatment, 1, Article 0003c. You can read this article online:
References
1233
http://journals.apa.org/prevention/volume1/pre0010003c.html Blackburn, I. M., Eunson, K.M., & Bishop, S. (1986). A two-year naturalistic follow-up of depressed patients treated with cognitive therapy, pharmacotherapy and a combination of both. Journal of Affective Disorders, 10, 67–75. Bollen, K.A. (1989). Structural Equations with Latent Variables. New York: John Wiley, & Sons. Burns, D.D. (1980). Feeling Good: The New Mood Therapy (preface by Aaron T. Beck). New York: Wm. Morrow and Co (hardbound); New American Library, 1981 (paperback). Revised (Avon), 1999. Burns, D.D. (1984). Intimate Connections. New York: William Morrow and Co., (hardbound); New American Library, 1985 (paperback). Burns, D.D. (1989). The Feeling Good Handbook. New York: William Morrow and Company. Revised, 1999. Burns, D.D. (1993a). Ten Days to Self-Esteem. New York: Quill. Burns, D.D. (1993b). Ten Days to Self-Esteem: The Leader's Manual. New York: Quill. Burns, D.D. (1995). Anger and interpersonal conflict: New approaches to an ancient problem. Professional Workshop Series. Mentor: David R. Lima, Inc. Burns, D.D. (1995). Therapist's Toolkit. Philadelphia: Author. Burns, D.D. (1997; 2004). Toolkit Upgrade. Includes the Speedy Screening for Axis I and II Disorders and the Therapist's Diagnostic Guidebook. Los Altos: Author.
References
1234
Burns, D.D. (1998). Strategies for Therapeutic Success: My Twenty Most Effective Techniques. Professional Workshop Series. Mentor: David R. Lima, Inc. Burns, D.D., Adams, R.L., & Anastopoulos, A.D. (1985). The role of self-help assignments in the treatment of depression. In E.E. Beckham, & W.R. Leber (Eds.), Handbook of Depression Treatment, Assessment, and Research (pp. 634-668). Homewood: Dorsey Press. Burns, D.D., & Auerbach, A.H. (1992). Do self-help assignments enhance recovery from depression? Psychiatric Annals, 22(9), 464-469. Burns, D.D., & Auerbach, A. (1996). Therapeutic empathy in cognitive-behavioral therapy: Does it really make a difference? Chapter 7 in Frontiers of Cognitive Therapy (P. Salkovskis, Ed.) New York: Guilford Press, pp. 135-164. Burns, D.D., & Eidelson, R.J. (1998). Why are depression and anxiety correlated? A test of the tripartite theory. Journal of Consulting and Clinical Psychology, 66(3): 461 - 473. Burns, D.D., London, J., Brunswick, D., Pring, M., Mendels, J., Garfinkel, D. & Rabinowitz, J.L. (1976). A kinetic analysis of 5-hydroxyindoleacetic acid excretion from rat brain and CSF. Biological Psychiatry, 11(2), 125-147. Burns, D.D., Neilands T., & Spangler, D. (2002). Was Epictetus right? Do negative thoughts cause negative emotions? A microanalytic case study using structural equation modeling. Manuscript under review. Burns, D.D., & Nolen-Hoeksema, S. (1991). Coping styles, homework assignments and the effectiveness of cognitive-behavioral therapy. Journal of
References
1235
Consulting and Clinical Psychology, 59, 305-311. Burns, D.D., & Nolen-Hoeksema, S. (1992). Therapeutic empathy and recovery from depression in cognitive-behavioral therapy: A structural equation model. Journal of Consulting and Clinical Psychology, 60(3), 441-449. Burns, D.D., Sayers, S.S., & Moras, K. (1994). Intimate relationships and depression: Is there a causal connection? Journal of Consulting and Clinical Psychology 62(5), 1033-1042. Burns, D.D., Shaw, B.F., & Crocker, W. (1987). Thinking styles and coping strategies of depressed women: An empirical investigation. Behavior Research and Therapy, 25(3), 223-225. Burns, D.D., & Mendels, J. (1979). Serotonin and affective disorders. Chapter 3 in Current Developments in Psychopharmacology, Vol. 5 (Essman, W. B. and Valzelli, L., Eds.), New York: Spectrum Publications, Inc., pp. 293-360. Burns, D.D., & Spangler, D. (2000). Does psychotherapy homework lead to improvements in depression in cognitive behavioral therapy? Or does improvement lead to increased homework compliance? Journal of Consulting and Clinical Psychology, 68(1), 46-59. Burns, D.D., & Spangler, D. (2001). Do changes in dysfunctional attitudes mediate changes in depression and anxiety in cognitive behavioral therapy? Behavior Therapy, 32, 337-369. Castonguay, L.G., Schut, A.J., Aikins, D., Constantino, M.J, Laurenceau, J.P., Bologh, L., & Burns, D.D. (2002). Integrative cognitive therapy: A preliminary investigation. Journal of Psychotherapy Integration (in press).
References
1236
Carroll, K.M., Rounsaville, B.J., & Nich, C. (1994). Blind man's bluff: Effectiveness and significance of psychotherapy and pharmacotherapy blinding procedures in a clinical trial. Journal of Consulting and Clinical Psychology, 62, 276-280. Cohen, P., & Cohen, J. (1983). Nominal or Quantitative Scales. Chapter 5 in Applied Multiple Regression / Correlation Analysis for the Behavioral Sciences, second edition. Hillsdale: Lawrence Erlbaum Associates. Cohen, P., & Cohen, J. (1984). The clinician's illusion. Archives of General Psychiatry, 41, 1178-1182. Craske, M.G., Barlow, D.H., & Meadows, E.A. (2000). Mastery of Your Anxiety and Panic (Map-3): Therapist Guide for Anxiety, Panic, and Agoraphobia, 3rd edition. San Antonio: Graywind Publications / The Psychological Corp. Cuijpers, P. (1997). Bibliotherapy in unipolar depression: A meta-analysis. Journal of Behavior Therapy and Experimental Psychiatry, 28(2), 139-147. Detweiler, J.B., & Whisman, M.A. (1999). The role of homework assignments in cognitive therapy for depression: Potential methods for enhancing adherence. Clinical Psychology: Science and Practice, 6(3), 267- 282. Devilly, G.J. (2001a). The successful treatment of PTSD through overt cognitive behavioral therapy in non-responders to EMDR. Behavioural and Cognitive Psychotherapy, 29, 57-70. Devilly, G.J. (2001b). The roles of popularised distraction during exposure and researcher allegiance during outcome trials. The Behavior Therapist, 24, 1821.
References
1237
Dobson, K.S. (1989). A meta-analysis of the efficacy of cognitive therapy for depression. Journal of Consulting and Clinical Psychology, 57(3), 414-419. Dunlap, K.L. (1936). Elements of Psychology. St. Louis, MO: C. V. Mosby. Dunner, D.L., & Dunbar, G.C. (1992). Optimal dose regimen for paroxetine. Journal of Clinical Psychiatry, 53, Supplement 2, 21-26. Ellis, A. (1977). Reason and Emotion in Psychotherapy. Seacaucus, NJ: The Citadel Press. Epstein, N.B., & Baucom, D. (2002). Enhanced Cognitive-Behavioral Therapy for Couples: A Contextual Approach. Washington, DC: American Psychological Association. Evans, M.D., Hollon, S.D., DeRubeis, R.J., Piasecki, J.M., Grove, W.M., Garvey, M. J., & Tuason, V. B. (1992). Differential relapse following cognitive therapy and pharmacotherapy for depression. Archives of General Psychiatry, 49, 802–808. Fabre, L.F., Abuzzahab, F.S., Amin, M., Claghorn, J.L., Mendels, J., Petrie, W.M., Dube, S., & Small, J.G. (1995). Sertraline safety and efficacy in major depression: A double-blind fixed dose comparison with placebo. Biological Psychiatry, 38, 592-602. First, M.B., Spitzer, R. L., Gibbon, M. & Williams, J. B. W. (1997). Structured Clinical Interview for DSM-IV® Axis I Disorders (SCID-I), Clinician Version. Arlington, VA: American Psychiatric Publishing, Inc. http://www.appi.org/group.cfm?groupid=SCID-I Fisher, S., & Greenberg, R.P. (1993). How sound is the double-blind design for
References
1238
evaluating psychotropic drugs? Journal of Nervous and Mental Disease, 181, 345-350. Frank, J.D. (1961). Persuasion and Healing. Baltimore, MD: Johns Hopkins University Press. Frank, J.D. (1982). Therapeutic components shared by all psychotherapies. In J. H. Harvey, & M. M Parks (Eds.), Psychotherapy Research and Behavior Change (pp. 5 – 37). Washington, DC: American Psychological Association. Garland, E. J. (2004). Facing the evidence: antidepressant treatment in children and adolescents. Canadian Medical Association Journal, 170, 489-491. Gortner, E.T., Gollan, J.K., Dobson, K.S., & Jacobson, N.S. (1998). Cognitivebehavioral treatment for depression: relapse prevention. Journal of Consulting and Clinical Psychology, 66, 2, 377-384. Greenberg, R.P., & Fisher, S. (1989). Examining antidepressant effectiveness: Findings, ambiguities, and some vexing puzzles. In S. Fisher & R.P. Greenberg (Eds.), The Limits of Biological Treatments for Psychological Distress: Comparisons with Psychotherapy and Placebo (pp. 1 – 37). Hillsdale, NJ: Erlbaum. Greenberg R.P., & Fisher S. (1997). Mood-mending medicines: Probing drug, psychotherapy, and placebo solutions. In Fisher S., Greenberg R.P. (Eds.), From Placebo to Panacea: Putting Psychiatric Drugs to the Test. New York, John Wiley & Sons, Inc., pp 115-172. Grossman, D.S., Cohen, T.J., Goldner, B., & Jadonath, R. (1994). Pseudorecurrence of paroxysmal supraventricular tachycardia after
References
1239
radiofrequency catheter ablation. American Heart Journal, 128, 516-519. Haaga, D.F., Dyck, M.J., & Ernst, D. (1991). Empirical status of cognitive theory of depression. Psychological Bulletin, 110, 215-236. Haislip, G.R. (1996). ADD/ADHD Statement of Drug Enforcement Administration. San Antonio. You can read this article online: http://www.add-adhd.org/ritalin.html Hatcher, R.L., Barends, A., Hansell, J., & Gutfreund, M.J. (1995). Patients' and therapists' shared and unique views of the therapeutic alliance: An investigation using confirmatory factor analysis in a nested design. Journal of Consulting and Clinical Psychology, 63(4), 636-643. Healy, D. (2003). Lines of evidence on the risk of suicide with selective serotonin reuptake inhibitors. Psychotherapy and Psychosomatics. 72, 71-79. Herzberg, A. (1941). Short-term treatment of neurosis by graduate tasks. British Journal of Medical Psychology, 29, 36-51. Heyman, R.E., Sayers, S.S., & Bellack, A.S. (1994). Global marital satisfaction vs. marital adjustment: an empirical comparison of three measures. Journal of Family Psychology, 8, 432-446. Hollon, S.D., & Beck, A.T. (1994). Cognitive and cognitive behavioral therapies. Chapter 10 in A. E. Bergin, & S. L. Garfield (Eds.), Handbook of Psychotherapy and Behavioral Change (pp. 428-466). New York: John Wiley, & Sons, Inc. Hollon, S.D., & Najavits, L. (1988). Review of empirical studies of cognitive therapy. In A. J. Frances & R. E. Hales (Eds.), American Psychiatric Press
References
1240
Review of Psychiatry (Vol. 7, pp. 643–666). Washington, DC: American Psychiatric Press. Horney, K. (1937). The Neurotic Personality of Our Time. New York: W.W. Norton Company. Horney, K. (1939). New Ways in Psychoanalysis. New York: W.W. Norton Company. Horney, K. (1950). Neurosis and Human Growth. New York: W.W. Norton Company. Horvath, A.O., & Luborsky, L. (1993). The role of the therapeutic alliance in psychotherapy. Journal of Consulting and Clinical Psychology, 61(4), 561573. Hypericum depression trial study group. (2002). Effect of Hypericum perforatum (St. John's wort) in major depressive disorder: A randomized, controlled trial. Journal of the American Medical Association, 287, 1807-14. You can read a summary online at: www.nih.gov/news/pr/apr2002/nccam-09.htm Ilardi, S.S., & Craighead, W.E. (1994). The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice, 1(2), 138-156. Imber, S.D., Pilkonis, P.A., Sotsky, S.M., Elkin, I., Watkins, J.T., Collings, J.F., Shea, M.T., Leber, W.R., & Glass, D.R. (1991). Mode-specific effects among three treatment programs. Journal of Consulting and Clinical Psychology, 58(3), 352-359. Jacobson, N.S., Dobson, K.S., Truax, P.A., Addis, M.E., Koerner, K., Gollan, J.
References
1241
K., Gortner, E., & Prince, S.E. (1996). A component analysis of cognitivebehavioral treatment for depression. Journal of Consulting and Clinical Psychology, 64, 295-304. The following citation is an online reprint of this study. Jacobson, N.S., Dobson, K.S., Truax, P.A., Addis, M.E., Koerner, K., Gollan, J.K., Gortner, E., & Prince, S.E. (2000). A component analysis of cognitivebehavioral treatment for depression. Prevention, & Treatment, Volume 3, Article 23, 1 – 17. You can read this article online at: http://journals.apa.org/prevention/volume3/pre0030023a.html Jamison, C., & Scogin, F. (1995). Outcome of cognitive bibliotherapy with depressed adults. Journal of Consulting and Clinical Psychology, 63, 644650. Jureidini, N., Doecke, C.J., Mansfield, P.R., Haby, M.M., Menkes, D.B., & Tonkin, A.L. (2004) Efficacy and safety of antidepressants in children and adolescents, British Medical Journal, 328, 879-883. Kassler, D.M., & Neimeyer, D.M. (1997). Homework compliance and skill acquisition as predictors of outcome in cognitive-behavioral group therapy for depression. (Unpublished manuscript.) Kirsch, I., Moore, T.J., Scoboria, A., & Nicholls, S.S. (2002). The emperor's new drugs: An analysis of antidepressant medication data submitted to the U.S. Food and Drug Administration. Prevention and Treatment, 5, Article 23. You can read this article online: http://journals.apa.org/prevention/volume5/pre0050023a.html
References
1242
Kirsch, I., & Sapirstein, G. (1998). Listening to Prozac but hearing placebo: A Meta-Analysis of Antidepressant Medication. Prevention and Treatment, 1, Article 0002a. You can read this article online: http://journals.apa.org/prevention/volume1/pre0010002a.html Krupnick, J.L., Sotsky, S.M., Simmens, S., Moyer, J., Elkin, I., Watkins, J., & Pilkonis, P. (1993). The role of the therapeutic alliance in psychotherapy and psychotherapy outcome: Findings in the NIMH treatment of depression collaborative research program. Journal of Consulting and Clinical Psychology, 64(3), 636-643. Lambert, M.J., Hatch, D.R., Kingston, M.D., & Edwards, B.C. (1986). Zung, Beck, and Hamilton rating scales as measures of treatment outcome: A metaanalytic comparison. Journal of Consulting and Clinical Psychology, 54, 5459. Lewinsohn, P., Munoz, R.F., & Youngren, M.A. (1986). Control Your Depression. Englewood Cliffs: Prentice-Hall. Mehra, N. (1995). From demons to drugs: A brief history of epilepsy. In Epilepsy Matters: The Newsletter of the Canadian Epilepsy Alliance. Volume 6(3). Epilepsy: Across Time and Place. You can read this article online at: www.epilepsytoronto.org/people/eaupdate Mendels, J., Stinnett, J.L., Burns, D.D. & Frazer, A. (1975). Amine precursors and depression. Archives of General Psychiatry, 32, 22-30. Moncrieff J, Wessely S, Hardy R. Meta-analysis of trials comparing antidepressants with active placebos. British Journal of Psychiatry 1998;172:
References
1243
227-231. Moncrieff J & Double DB (2003) Double blind random bluff. Mental Health Today Nov: 24-6. Web link: http://www.critpsynet.freeuk.com/CPNpublish.htm Neimeyer, R.A., & Feixas, G. (1990). The role of homework and skill acquisition in the outcome of group cognitive therapy for depression. Behavior Therapy, 21, 281-292. Neimeyer, R.A., Twentyman, C.T., & Prezant, D. (1985). Cognitive and interpersonal group therapies for depression: A progress report. The Cognitive Behaviorist, 7, 1-22. NIH (April 9, 2002). NIH News Release. http://www.nih.gov/news/pr/apr2002/nccam-09.htm Norcross, J.C., Santrock, J.W., Campbell, L.F., Smith, T.P., Sommer, R., & Zuckerman, E.L. (2003). Authoritative Guide to Self-Help Resources in Mental Health, Revised Edition. New York: Guilford Press. Orlinsky, D.E., Grawe, K., & Parks, B.K. (1995). Process and outcome in psychotherapy--Noch einmal. Chapter 8 in A. E. Bergin, & S. L. Garfield (Eds.), Handbook of Psychotherapy and Behavioral Change (pp. 270-376). New York: John Wiley, & Sons, Inc. Pekarik, G. (1987). Outpatient clinic therapist attitudes and beliefs relevant to client dropout. Community Mental Health Journal, 23(2), 120-130. Persons, J.B., & Burns, D.D. (1985). Mechanism of action of cognitive therapy: Relative contribution of technical and interpersonal intervention. Cognitive Therapy and Research, 9(5), 539-551.
References
1244
Persons, J.B., & Miranda, J. (1992). Cognitive theories of vulnerability to depression: Reconciling negative evidence. Cognitive Therapy and Research, 16, 485-502. Persons, J.B., Burns, D.D., & Perloff, J.M. (1988). Predictors of dropout and outcome in cognitive therapy for depression in a private practice setting. Cognitive Therapy and Research, 12, 557-575. Persons, J.B., Burns, D.D., Perloff, J.M., & Miranda, J. (1993). Relationships between symptoms of depression and anxiety and dysfunctional beliefs about achievement and attachment. Journal of Abnormal Psychology, 101(4), 518-524. Pitman, R., Orr, S., Altman, B., Longpre, R., Poire, R., & Macklin, M. (1996, NovDec). Emotional processing during eye movement desensitization and reprocessing therapy of Vietnam veterans with chronic posttraumatic stress disorder. Comprehensive Psychiatry, 37(6), 419-429. Preskorn, S.H. (1997). Clinically relevant pharmacology of selective serotonin reuptake inhibitors: an overview with emphasis on pharmacokinetics and effects on oxidative drug metabolism. Clinical Pharmacokinetics, 32, Supplement 1, 1-21. Robins, C.J., & Luten, A.G. (1991). Sociotropy and autonomy: Differential patterns of clinical presentation in unipolar depression. Journal of Abnormal Psychology, 100, 74-77. Robinson, L.A., Berman, J.S., & Neimeyer, R.A. (1990). Psychotherapy for the treatment of depression: A comprehensive review of controlled outcome
References
1245
research. Psychological Bulletin, 108, 30-49. Rogers, C.R. (1957). The necessary and sufficient conditions of therapeutic change. Journal of Consulting and Clinical Psychology, 21, 205-214. Salisbury, D. F. (2002). Cognitive therapy effective as drugs in long-term treatment of severe depression. Exploration: The online research journal of Vanderbilt University. July 3, 2002. You can read this article online at: http://exploration.vanderbilt.edu/news/news_hollon.htm Salpom, P., Schrodt, R., & Wright, J. (1989). Temporal gradient of anxiety in a stressful performance context. Medical Problems of Performing Artists, 4, 7780. Santrock, J.W., Minnett, A.M., & Campbell, B.D. (1994). The Authoritative Guide to Self-Help Books. New York: Guilford Press. Schatzberg, A. F., Cole, J.O., & DeBattista, C. (1997). Manual of Clinical Psychopharmacology, Third Edition. Washington, DC: American Psychiatric Press. Scogin, F., Hamblin, D., & Beutler, L. (1987). Bibliotherapy for depressed older adults: A self-help alternative. The Gerontologist, 27, 383-387. Scogin, F., Jamison, C., & Davis, N. (1990). A two-year follow-up of the effects of bibliotherapy for depressed older adults. Journal of Consulting and Clinical Psychology, 58, 665-667. Scogin, F., Jamison, C., Floyd, M., & Chaplin, W. (1998). Measuring learning in depression treatment: A cognitive bibliotherapy test. Cognitive Therapy and Research, 22, 475-482.
References
1246
Scogin, F., Jamison, C., & Gochneaut, K. (1989). The comparative efficacy of cognitive and behavioral bibliotherapy for mildly and moderately depressed older adults. Journal of Consulting and Clinical Psychology, 57, 403-407. Shea, M.T., Elkin, I., Imber, S.D., Sotsky, S.M., Watkins, J., Collins, J.F., Pilkonis, P.A., Leber, W.R., Krupnick, J., Dolan, R.T., & Parloff, M.B. (1990). Course of depressive symptoms over follow-up: Findings from the National Institute of Mental Health treatment of depression collaborative research program. Archives of General Psychiatry, 49, 782–787. Shea, M.T., Elkin, I., Imber, S.D., Sotsky, S.M., Watkins, J., Collins, J.F., Pilkonis, P.A., Beckham, E., Glass, D., Dolan, R.T., & Parloff, M.B. (1992). Course of depressive symptoms over follow-up. Archives of General Psychiatry, 49, 782-787. Sheehan, D. V., Lecrubier Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry; 59 Supplement 20: 22-33; quiz 34-57. Simons, A.D., Garfield, S.L., & Murphy, G.E. (1984). The process of change in cognitive therapy and pharmacotherapy for depression. Archives of General Psychiatry, 41, 45-51. Simons, A.D., Murphy, G.E., Levine, J.E., & Wetzel, R.D. (1986). Cognitive therapy and pharmacotherapy for depression: Sustained improvement over one year. Archives of General Psychiatry, 43, 43–49.
References
1247
Smith, N.M., Floyd, M.R., Jamison, C., & Scogin, F. (1997). Three-year follow-up of bibliotherapy for depression. Journal of Consulting and Clinical Psychology, 65(2), 324-327. Talbott, J. A., Hales, R. E., & Yudofsky, S. C. (1988). Comprehensive Textbook of Psychiatry. Washington, D.C.: American Psychiatric Press. Teasdale, J.D. (1983). Negative thinking in depression: Cause, effect, or reciprocal relationship? Advances in Behavioral Research and Therapy, 5, 325. Wernicke, J.F., Dunlop, S.R., Dornseif, B.E., Bosomworth, J.C., & Humbert, M. (1988). Low-dose fluoxetine therapy for depression. Psychopharmacology Bulletin, 24, 183-188. Wernicke, J.F., Dunlop, S.R., Dornseif, B.E., & Zerbe, R.L. (1987). Fixed-dose fluoxetine therapy for depression. Psychopharmacology Bulletin, 23, 164168. Westra, H.A., & Stewart, S.H. (1998). Cognitive behavioral therapy and pharmacotherapy: Complementary or contradictory approaches to the treatment of anxiety? Clinical Psychology Review, 18 (3), 307-340. Whittington, C.J., Kendall, T., Fonagy, P., Cottrell, D, Cotgrove, A, & Boddington, E. (2004). Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. The Lancet, 363, 1341-1345. Young, J.E., Beck, A.T., & Weinberger, A. (1993). Depression. In D. H. Barlow (Ed.), Handbook of Psychological Disorders (pp. 240-277). New York:
2020 NEW Materials Section Flow Sheets & Outlines T.E.A.M. Therapy Session Flow Sheet
1250
T.E.A.M. Session Flow Sheet PAS Expanded
1251
Depression Recovery Flow Map
1252
Anxiety Recovery Flow Map
1253
Anger/Relationships Recovery Flow Map
1254
Habit/Addiction Recovery Flow Map
1255
51+ More Methods 51 Additional Methods Descriptions
1257
Comparing Role-Playing Techniques
1275
Strategies for Defeating Dysfunctional NT or PT
1276
Complete list of 100+ methods with book page numbers
1277
Complete list of 100+ methods in alphabetical order
1285
Advanced Empathy Techniques Overview
1294
Changing the Focus
1295
Assessment of Resistance (Paradoxical Agenda Setting) 5 Steps - handout from the latest workshops
1303
Why Our Patients Resist
1304
Basic Concepts
1306
Positive Reframing in detail
1322
Positive Reframing Ideas
1324
Tips on Agenda Setting
1327
What to Say at Each Step
1336
Agenda Setting Flowchart
1351
Positive Reframing for Relationships
1353
Habit & Addictions including help for procrastination and difficult decisions Handout on Treading Habit & Addictions
1358
Positive & Negative Distortions
1359
Agenda Setting for Complex Cases
1365
Habit & Addictions Feeling Great “Additional Chapters”
1371
Making Difficult Decisions Feeling Great “Additional Chapters”
1386
NEW – Flowcharts & Outlines for T.E.A.M. Therapy Sessions
T.E.A.M. Therapy Session Flow Sheet*
T = Testing
Tools Tick () Before Session Brief Mood Survey Depression Suicide Anxiety Anger Relationship Satisfaction Positive Feelings
Comment
Time Required
Patient completes the “Before Session” tests in the waiting room prior to the start of the session. Therapist reviews scores at start of session, along with end-of-session scores from previous session.
Typically 1 minute, but may require more time to process problems from previous session
Empathy is needed at the start of the session and throughout the session. The goal is to understand and accept how the patient thinks, feels and behaves without trying to help or give advice or make interpretations.
Varies
5 Secrets of Effective Communication Disarming Technique E = Empathy
Thought / Feeling Empathy Inquiry “I Feel” Statements Stroking Invitation Step Specificity Step
A = (Paradoxical) Agenda Setting
Conceptualization Step
Motivation Step
M = Methods
T = Testing
Daily Mood Log Recovery Circle 50 Ways to Untwist Your Thinking Interpersonal DecisionMaking Relationship Cost-Benefit Analysis Relationship Journal 5 Secrets of Effective Communication Intimacy Exercise / 1 Minute Drill Decision-Making Form Habit / Addition Lot Devil’s Advocate Technique End-of-Session Brief Mood Survey Evaluation of Therapy Session
*
Straightforward or Paradoxical Invitation Patient selects the problem and describes one moment when that problem was upsetting him / her. Individual Mood Problem? (depression and anxiety) Relationship Problem? Habit / Addiction? “Non-Problem”?
1 minute 2 - 3 minutes This may only take 1 minute but is an ongoing process as well
The therapist melts away Outcome and Process Resistance.
10 – 15 minutes or more
For Depression and Anxiety
May require several sessions
For Relationship Problems
May require several sessions
For Habits and Addictions
May require several sessions
Patient completes this in the waiting room after the session and leaves the form for the therapist to review when the session is fresh in mind.
2 to 3 minutes, on average
Copyright © 2013 by David D. Burns, M.D.
Disarming
Testing
Thought/Feeling Empathy
Empathy
I Feel
Sample TEAM Session Flow and PAS for Mood Problems
Stroking
Miracle Cure
Inquiry
TEAM Stages
Magic Button
Invitation
Agenda Setting
(Specificity)
(Acid test)
Outcome resistance Positive Reframing
(Conceptualization)
Paradoxical inquiry
Motivation
Magic Dial Dangling the Carrot
Methods Process resistance
Daniele V. Levy, PhD, 2016
Gentle Ultimatum Fall Back position/Sitting with open hands
Depression Recovery Map*
Depression
Empathy
Agenda Setting
Daily Mood Log
Recovery Circle
Cognitive Techniques
Motivational Techniques
Uncovering Techniques
Role-Playing Techniques
Relapse Prevention
* Copyright © 2006 by David D. Burns, M.D.
Behavioral Activation Techniques
Interpersonal Techniques
Anxiety Recovery Map*
Anxiety
Empathy
Agenda Setting
Daily Mood Log
Recovery Circle
Cognitive Techniques
Motivational Techniques
Uncovering Techniques
Hidden Emotion Technique
Relapse Prevention
* Copyright © 2006 by David D. Burns, M.D.
Exposure Techniques
Interpersonal Techniques
Anger / Relationship Recovery Map*
Relationship Problem
Empathy
Interpersonal DecisionMaking
Cognitive Techniques
Agenda Setting
Blame CostBenefit Analysis
Daily Mood Log
Revise Your Communication Style
Motivational Techniques
Uncovering Techniques
Role-Playing Techniques
Relapse Prevention
* Copyright © 2006 by David D. Burns, M.D.
Five Secrets of Effective Communication
Interpersonal Role-Playing
Habit / Addiction Recovery Map*
Habit or Addiction
Empathy
Agenda Setting
Devil's Advocate Technique
Decision-Making Form
Daily Addiction Log
Cognitive Techniques
Motivational Techniques
Uncovering Techniques
AntiProcrastination Techniques
Relapse Prevention
* Copyright © 2006 by David D. Burns, M.D.
Role-Playing Techniques
NEW – More Methods! 51+ more methods descriptions 100+ List with Book numbers
Additiona
a s to
nt ist
our
in in
a e
51 Additional Ways to Untwist Your Thinking* The Advanced Toolkit—for Therapists (and Super Curious Patients) Only! By David D. Burns, M.D. The first techniques listed here are tools therapists can use during the T = Testing, E = Empathy, and A = (Paradoxical) Agenda Setting phases of a therapy session, but you might find them of interest even if you’re not a therapist. The techniques listed in the M = Methods section may be of interest to therapists and the general public alike.
estin 1. Easy Diagnostic Survey This is a diagnostic survey you can ask your patients to complete on their own between therapy sessions. They bring you the completed survey, and this makes it easy to diagnose approximately 50 of the most common DSM5 / ICD10 diagnoses. This will only take you about 5 to 10 minutes. It’s a quick and easy way of assigning psychiatric diagnoses, and it comes with helpful tools for you as well. Most patients will have many definite or probably diagnoses according the DSM criteria. Although I am not a strong advocate for DSM, this does allow you to pinpoint many problematic areas for each patient with investing lots of time in diagnostic interviewing. For more information, go to this link. (David, include link to order form.)
2. Brief Mood Survey (BMS) This is a vitally important assessment test that patients can complete in the waiting room immediately before and after every therapy session. In TEAM therapy, we require this of every patient at every session with no exceptions. The BMS assesses the severity of depression, suicidal urges, anxiety and anger, as well as happiness and relationship satisfaction. It also asks how much psychotherapy homework patients have done since the last session. By comparing the before-and-end of session scores, therapists you can see, for the first time, exactly how effective or ineffective every session was. It’s a great learning tool that can revolutionize the way you do therapy and vastly boost your therapeutic effectiveness.
3. Specialized Brief Mood Survey (BMS) There are quite a few varieties of the BMS designed for patients with specific kinds of problems. For example, one version assesses violent tendencies, another includes a scale for self-mutilation tendencies, and another includes the Craving and Urges scale for individuals struggling with habits and addictions..
4. Evaluation of Therapy Session Patients complete this form in the waiting room after the session. They rate the therapist on
Additiona
a s to
nt ist
our
in in
a e
Empathy, Helpfulness, Satisfaction with the Session, Commitment to doing psychotherapy homework, Negative Feelings not expressed during the session, and honesty in filling out the scales. They also write down what they specifically liked and disliked about the session. The results are often surprising and shocking to therapists, as falling grades are common.
5. Daily Mood Journal Although the Daily Mood Journal is an invaluable tool for identifying and modifying Negative Thoughts, it is also a superb internal measuring tool, because you assess how the patient feels “right now,” on a scale from 0 (not at all) to 100 (extreme) at the beginning of the session, when you are starting to work with the DMJ, and again at the end of the session, when you have completed your work with the DMJ, in nine different dimensions, including depression, anxiety, guilty, inadequacy, loneliness, embarrassment, hopelessness, frustration, and anger.
E
E pat
6. What s My Grade? TEAM-CBT emphasizes the importance of getting an “A” on Empathy before moving on to the Agenda Setting phase of the session. But how can you know if you’re getting an A on Empathy? After all, the patient won’t fill out the Empathy Scale on the Patient’s Evaluation of Therapy Session until the session is over. Here’s how you can find out how you’re doing on Empathy in real time: you can ask! Once you feel you’ve done a good job of listening, and you’re think the patient might be ready for the Invitation Step of Paradoxical Agenda Setting, you can ask, “How am I doing so far in empathy, in terms of understanding how you think and feel, and providing warmth and support? Would you give me an A? A B? A C? Or a D?” You might think patients would not be honest, or would think this type of question is goofy, but it works well. Patients will usually give you honest feedback. Sometimes, out of politeness, the patient might give you an A- or a B+. This means you’ve missed something important. If you ask what part you missed, the patient will tell you, and if you summarize what you missed in a kindly and accurate way, the patient will nearly always boost your grade to A or an A+! Very few therapists are aware of this technique, but it’s invaluable!
7. The Disarming Technique You find truth in the patient’s criticism of you, even if you feel convinced that it isn’t true. You can also use this technique to enhance empathy with patients as well as colleagues, family and friends who are upset but not mad at you.
8. Thought Empathy You summarize the other person’s words.
Additiona
a s to
nt ist
our
in in
a e
9. Feeling Empathy You acknowledge how the other person might be feeling, based on his or her words.
10. Inquiry You use gentle probing questions to learn more about what the other person is thinking and feeling, as well as to find out if you got it right.
11. I Feel Statements You share your own feelings in a respectful, professional way, us “I Feel” Statements.
12. Stroking You convey liking, warmth, or admiration even in the heat of battle.
13. Changing the Focus You bring the tension in the room to conscious awareness in a respectful way that invites productive dialogue.
14. Multiple Choice Empathy You suggest a number of feelings that the other person might be having, based on what she or he has said.
15. Interpersonal Positive Reframing You cast a heated or conflicted exchange with a patient, colleague or family member in a positive light, emphasizing that while the dialogue may feel awkward, it can lead to improvements in the therapeutic relationship, or even breakthroughs.
16. Humor Initially, I could only think of 49 additional techniques and was wracking my brain to think of one more, and then it came to me in the middle of the night last night, so I got up excitedly to add it—humor. Because I’ve been recording sessions and hearing myself, I realized that I use a tremendous amount of humor in therapy, and it definitely has powerful antidepressant effects. It can also be thought of as an affectionate way of deepening the therapeutic alliance, so I’m included as an Empathy technique. I rarely teach humor, since it is somewhat non-specific and difficult to treat. But I decided to try to figure out how I create humor, since it’s never been totally clear to me. But one device I use is to suddenly blurt out some kind of totally outrageous comment. For example, when I’m asking patients or colleagues about their negative thoughts when filling out a Daily Mood Journal, they may say that they’re telling themselves something like “I’m a bad mother,” or father, or therapist, etc., or “I feel like I’m just a totally worthless human being.” Then I might say, “No, I’m just looking for a distorted thought!” This nearly always gets the patient laughing. Or, sometimes I will blurt out something that is totally politically incorrect, or just simply bizarre. This can be helpful for several reasons. First, it sends an implied meta-message that the Negative Thought probably isn’t true, or couldn’t be true, and that the patient is being awfully hard on himself / herself. Second, it sends a friendly message that I, the therapist, like you, and that we can be human and joke about things together.
Additiona
a s to
nt ist
our
in in
a e
The Buddhists sometimes call this “laughing enlightenment.” Laughter really can be a form of enlightenment, almost a kind of instant healing. In a high percentage of cases, my patients begin laughing uncontrollably at the moment of recovery, when the suddenly see that the thoughts that have been plaguing them throughout their lives are just a con, and that their suffering has been the result of a kind of gigantic cosmic hoax. On two occasions, I’ve had patients laughing so hard that they fell out of their chairs and had trouble getting back up! If you want to hear the integration of humor into therapy, I would recommend the live podcasts on the treatment of Marilyn, who had just been diagnosed with stage 4 lung cancer by her doctor. She was in a panic, and was intensely depressed and enraged, because she’s never been a smoker, and the diagnosis caught her entirely by surprise. Surprisingly, we laughed a great deal during the session. Of course, there were many tears as well. You can read about Marilyn in Chapter 24 of this book, and listen to her life starting with Podcast #49 entitled, “Live therapy with Marilyn, Part 1—the Dark Night of the Soul” (link). She described the session as mind-blowing. Like all techniques, humor has its limits. First, not all therapists have a convenient sense of humor they can easily access during sessions, so this technique will not be suitable for everyone. Second, it’s generally not good to use humor when the patient is angry with you, or mistrustful. The use of humor in these situations is a defense and may feel belittling to the patient. The skillful use of the Five Secrets of Effective Communication will be far more effective.
A
aradoxica
A enda
ettin
Note. Several additional Agenda Setting techniques were included in the beginner’s list, including the Magic Dial, Positive Reframing, and Straightforward CBA. Several additional like Paradoxical Inquiry and Devil’s Advocate are listed below.
17. Straightforward Invitation Once you’ve received an A in empathy, you ask if this is a good time to get to work on one of the problems the patient has been describing, or if the patient needs more time to vent, since that’s also important and you don’t want to jump in before he or she is ready. This invitation is usually reserved for cooperative patients who are asking for help for depression or anxiety. The question you are asking, essentially, is do you want to get to work “now or later?” Your working assumption is that the patient does want help.
18. Paradoxical Invitation This invitation is usually reserved for uncooperative or oppositional patients who are asking for help with relationship problems or habits / addictions. Once you’ve received an A in empathy, you tell the patient that you have some terrific tools to help him or her with problem X (X might be a problem with his wife, colleague or family member), and that you’d love tow work with him on it, but that it isn’t clear to you that he’s actually asking for help or wants to work on the problem with X. Then you ask him if you’re reading him right. The question you are asking, essentially, is do you want to get to work “now or never?” Your working assumption is that the patient does not want help.
Additiona
a s to
nt ist
our
in in
a e
19. The Specificity Step If the patient wants help, you ask which problem, of the many he described during the E = Empathy phase of the session, that he or she wants to focus on. That’s Level 1 Specificity. Once the patient describes the problem (like low self-esteem, panic attacks, or a marital conflict) you ask him or her to describe a specific moment when she or he was having that problem. That’s Level 2 Specificity. Specificity is one of the most important keys to TEAM-CBT. There are several assumptions: 1. You can only help a person with one specific problem at one specific moment on one specific day. 2. All the patient’s problems will be encapsulated in that one brief moment. This is the concept of a psychological “fractal.” When you understand the nature of the problem at that moment, you will understand everything of importance in the patient’s struggles and suffering. In addition, that complete understand is easy to achieve. 3. When the patient changes at that one moment, all his or her problems will usually fall apart like a house of cards. So, although the focus of the treatment is tremendously narrow, the yield is incredibly broad. This is another paradox of TEAM-CBT. It is embedded in Buddhism and based on fractal geometry.
20. Conceptualization Once the patient has described a specific moment when s/he wants help, you ask yourself what type of problem it is. Here are the choices: 1. Individual mood problem, such as depression or anxiety. 2. Relationship problem or conflict. 3. Habit or addiction. 4. Nonproblem (e.g. uncomplicated grief not requiring aggressive treatment or medications. 5. Another potential category is somatic complaint, such as chronic pain, insomnia, tics, stuttering, and so forth.
21. Miracle Cure Question If a miracle happened in today’s session, and you left feeling like something fantastic had happened, what miracle would you be hoping for?
22. Magic Button Imagine there’s a Magic Button in front of you, and if you pressed it, all your negative thoughts and feelings would instantly disappear, with no effort on you part, and you’d feeling tremendous joy and self-confidence, and all of your depression, anxiety, shame, and anger would be gone. Would you press the Magic Button?
23. Acid Test Once you’ve generate a list of positives using Positives Reframing (there will typically be 20 or more), you can ask: Given all these positives, why would you want to press that Magic Button? After all, once your Negative Thoughts and feelings disappear, all these positives will disappear as well.” You can also do the Acid Test following a Paradoxical Cost-Benefit Analysis for a Negative Thought, feeling, belief, or habit. For example, after listing all the many advantages of feeling defective, anxious or angry, you can ask the patient, “Given all the many advantages of this feeling, it’s not clear to me why you’d want to get rid of it.”
Additiona
a s to
nt ist
our
in in
a e
24. Externalization of Resistance The patient and therapist are the same person, with the same name, exactly as in the Externalization of Voices. The therapist plays the role of the “Resistant Self,” and verbalizes all the good reasons NOT to change and NOT to do psychotherapy homework, etc. The patient plays the role of the motivated self that DOES want to change. The motivated self tries to defeat the “Resistant Self.” If the patient cannot defeat the Resistant Self, the therapist can say something along these lines: “It sounds like maybe this is not something you’d want to change. Am I reading you right?”
25. Dangling the Carrot The therapist indicates that the prognosis is positive and that three are many powerful tools to help the patient—IF she or he wants help.
26. Gentle Ultimatum This is a Process Resistance tool. You will recall that the four forms of process resistance involve • • • •
psychotherapy homework (depression) exposure (anxiety) giving up blaming and working to pinpoint your own role in the problem (relationship conflicts) discipline and deprivation (habits and addictions.)
The therapist indicates that the homework (or exposure, etc.) is a requirement of the therapy that is not negotiable. Assuming the patient wants treatment for depression, the statement you make to him or her might be along these lines: “Sherry, I’d really love to help you with your depression, and I have some tremendous tools that I think will be helpful to you (Dangling the Carrot), and it would be a joy to work with you, but I just wouldn’t know how to help you with the homework. Sadly, my skills and tools won’t be effective without the homework, so I couldn’t agree to treat your depression if you feel strongly that you want a type of therapy that doesn’t require homework. I’m hoping that you WILL decide to work with me, but I want to be very clear that consistent therapy homework will be required, even on the days when you just don’t feel like it.”
27. Sitting with Open Hands If the patient does not agree to do homework, exposure, or whatever is required for successful treatment, you might say: “Sadly, I won’t be able to be helpful to you if you feel strongly that you don’t want to do psychotherapy homework (or exposure, etc.) If you change your mind at some future time and want to work with me, my door will always be open to you.” That’s just one specific example of the Open Hands mindset that’s at the core of TEAMCBT. Sitting with Open Hands means that the therapist has given up the need to help, rescue, or save the patient. Instead, you, the therapist, become the voice of the patient’s resistance and you invite the patient to try to convince you to work with him or her. This is very difficult for many therapists to learn because of an addiction to helping,
Additiona
a s to
nt ist
our
in in
a e
rescuing, and playing the role of “expert.” Often, something within the therapist must change before the therapist can help the patient change. Learning to do this in actual therapy sessions requires quite a lot of group training and or individual supervision and consultation for therapists.
28. Fallback Position If the patient does not want to do homework, or use exposure, or do whatever will be required for effective treatment, you will need a Fallback Position, and there are many possibilities: •
•
You can suggest that the patient seek treatment with a therapist who offers the type of therapy they are looking for. For example, you can remind the patient that most therapists in the community do talk therapy and do not believe in the value of psychotherapy homework and remind the patient that if it does not work out, and he or she wants to return, you’re door is always open. This is best done at the initial evaluation, before you’ve accepted the patient into treatment, so as to avoid abandonment issues later on. You can offer to work with the patient on some other problem. However, the process resistance issue may surface again.
29. Double Paradox If a patient wants help with a habit or addiction, like binge eating, you can ask them to list the advantages of binge eating and the disadvantages of diet and exercise in a two-column format. Make sure you list LOTS of advantages and disadvantages. Then you can ask, “Given all those tremendous advantages of eating all that delicious food, and all the tremendous hassles of diet and exercise, why in the world would you want to change?”
30. Triple Paradox You add a third column, listing what the habit or addiction shows about you that’s positive and awesome, then finish with the same paradoxical question listed for the Double Paradox.
et ods 31. Worst, Best, Average This technique is described on page Error! Bookmark not defined., Ut can be helpful for Overgeneralization and Labeling. Let’s say you have a negative thought like “I’m a bad father” or “therapist,” or whatever. You can list five or ten specific skills or characteristics of a “good father” or “therapist” or whatever. Then rate yourself in each specific area, using a scale from 0 to 100, when you’re at your worst, your best, and on average. Then you can select a specific area where you’d like to improve, such as “good listening skills,” and make a plan to improve in that area.
32. Habit / Addiction Log The patient records the kinds of tempting thoughts he or she has when tempted, such as: • •
Oh, that glazed donut looks SO GOOD. I’ll just have one little bite. That can’t hurt!
Additiona
• •
a s to
nt ist
our
in in
a e
I deserve it, I’ve had a hard day. I can have a light dinner to make up for it.
Then the patient can identify the Positive Distortions in the tempting thoughts, and practice challenging them with the Devil’s Advocate Technique (see below).
33. Checklist of Positive Distortions This is a list of ten positive distortions that are the mirror images of the ten negative distortions. For example, in Positive Emotional Reasoning, you jump to conclusions that might not be warranted because you feel so good. The positive distortions trigger mania, narcissism, gambling, addictions, relationship problems, and violence. Positive Distortions are far more difficult the challenge because they make the patient feel so good, and they are rewarding. For example, “that donut looks SO GOOD! (Magnification) I’ll just have one little bite. (Discounting the Negative) That can’t hurt! I’ll have a really small dinner tonight anyway. (Fortune Telling)””
Additiona Ro e
a in
ec ni ues
Note. Some of these were listed in the beginner’s list of 50 Methods, like Externalization of Voices and Feared Fantasy. Some, like the Externalization of Resistance, are listed with the section on Paradoxical Agenda Setting. You will find comparison and strategy tables for all of the role-playing techniques on pages 19 - 20.
34. Devil s Advocate Technique Once the patient has listed all of us or her tempting thoughts, you do a role-play. You, the therapist, ask the patient to imagine being in the tempting situation (walking past the bakery and smelling the donuts), and explain that you will be the Devil who tempts them. The patient must try to defeat you. As the Devil, try your hardest to persuade the patient to give in to the temptation. If she or he cannot defeat you, DO NOT try to help. Instead, say something like this: “It seems like you can’t convincingly defeat your tempting thoughts. Perhaps this is not something you really want to change.”
35. Paradoxical Double Standard Technique You ask the patient to list all the advantages of a Negative Thought (I’m worthless), feeling, (anger anxiety), Self-Defeating Belief (I should always try to be perfect), relationship problem (blaming your spouse for the problems in your marriage) or habit (drinking,, overeating, internet porn, etc.) in the left-hand column of a Cost-Benefit Analysis, but you ignore the Disadvantages column. Then you ask an Acid-Test Question, like, “Given all those advantages, why would you want to give this up?” if you do this with genuine curiosity and respect for you patient, it will be effective. If you do this to manipulate your patient, it will backfire.
36. High School Reunion This is a Feared Fantasy technique to help patients with Self-Defeating Beliefs, such as the Achievement Addiction. Some patients may realize that it is not to their advantage to link their feelings of self-esteem with their achievements, but they may still cling to the notion
Additiona
a s to
nt ist
our
in in
a e
that people who achieve a great deal, like Bill Gates or Albert Einstein, really are “superior” or “more worthwhile” human beings. To illustrate why this is not true, you invite the patient to a bizarre, Alice-in-Wonderland nightmare world. In this case, it is their high school reunion. You explain that one of you will play the role of the patient (named Aziz, for this example) and one of you will play the role of a high school classmate at the reunion (named Rajesh for this example) who has achieved a tremendous amount—in fact, Rajesh was just named “Man of the Year” by Time Magazine., and comes to the reunion in a limousine with body guards and handlers. Patient and therapist can do role-reversals. In this example, the therapist starts out as Rajesh. Rajesh (played by therapist). Oh, hi Aziz. Great to see you at the reunion! You probably saw my picture on the cover of Time Magazine. Aziz (who is the patient). Oh yes, very impressive. Rajesh (played by therapist). I guess I’ve been pretty lucky. Everything I’ve touched has turned to gold. I’ve made billions. They say I’m now the most successful person in the world! Aziz (who is the patient. That is fantastic. Rajesh (played by therapist). I agree, I really am pretty fantastic! Do you recall our value system? Remember, you and I both agree that our worthwhileness as human beings depends on our accomplishments? I know you’ve believed that for a long time! And have you noticed how my accomplishments are vastly superior to your own rather average accomplishments in life? Aziz (who is the patient. I guess so. Rajesh (played by therapist): And so, I don’t mean to hurt your feelings, but I guess I have to be totally honest, and it kind of follows, doesn’t it, that I’m superior to you now, and to be honest, I’m kind of looking down on you! Aziz (who is the patient. You sound like a total jerk! It’s crucial to do a role-reversal as well, to make sure the patient really “sees” it. In this example, the therapist starts out as Aziz. Aziz (played by the therapist). Hi Rajesh, great to see you at the reunion. It’s impressive. I saw your picture on the cover of Time Magazine, and it blew me away. I’m so proud of all the things you’ve accomplished. Gosh, you’re here with handlers and body guards. Its’ really mind-boggling! Rajesh (played by the patient): Well, I guess I have accomplished quite a bit. Aziz (played by therapist). Listen, there’s something I heard through the grapevine that bothered me a little bit, and I wanted to bounce it off of you because I can’t believe it’s true. Rajesh (played by the patient): What is it you wanted to ask me? Aziz (played by therapist). Well, this is a bit awkward, but I heard that you think you’re better than other people, now that you’ve accomplished so much. I could hardly believe ti. Do you really feel like that? Rajesh (played by the patient, who must agree that he’s superior): Yes, in all honesty, I think that does follow, because our worthwhileness as humans is determined by our accomplishments. And I’ve accomplished more than just about anyone! Aziz (played by therapist). So, are you looking down on me right now, for example?
Additiona
a s to
nt ist
our
in in
a e
Rajesh (played by the patient): Oh, absolutely! Aziz (played by therapist). Well, enjoy your reunion, big guy! I’ll have to be running along because I have to meet some friends in low places! In most cases, the patient will suddenly see the absurdity of basing your self-esteem on your accomplishments, or on anything at all. The fantasy can be modified for other beliefs, like basing your self-esteem on being loved, or popular, or on your belief in God, and so forth. The point is subtle but massively important: You can be better at something specific thing, like tennis, or math, or business. Does that make you a more worthwhile human being? More worthwhile than who?
37. Anti-Brushfire Technique People with social anxiety or the fear of disapproval sometimes believe that disapproval is extremely dangerous and will spread like wildfire. That’s one reason they are inhibited and avoid taking risks in relationships. The fear is at least partially misguided, since it rests on the erroneous belief that all humans are like clones who think about things in the same way. The fear of disapproval is also based on the erroneous notion that people will be incredibly interested in whatever social goofy thing they said or did and will be eager to tell as many people as possible about it. In this role-play, I tell patient X that I will play the role of someone they know name Robert, and they can play the role of someone trying to gossip to me about patient X. The dialogue might go like this: Patient X (playing the role of the gossiper): Did you hear about X? David (playing the role of Robert): No, I don’t think I did. Patient X (playing the role of the gossiper): Oh, apparently X was giving a talk at work and her mind went blank. I guess she made a fool our of herself! David (playing the role of Robert): That’s too bad! I’ve actually had that happen to me once when I was speaking to a group of several hundred women, but it worked out okay. I’ve made a fool of myself pretty often, actually. Patient X (playing the role of the gossiper): Well, don’t you think that X is kind of a loser? I mean, that was really stupid, what she did! David (playing the role of Robert): No, I don’t actually think public speaking anxiety is unusual. In fact, most of the people I know have public speaking anxiety. Are you thinking that maybe you don’t like X because she has public speaking anxiety? The idea is simply to illustrate that in most instances, the world won’t come to an end if you goof up at something, and people try to gossip about you. I most cases, they’ll simply make themselves look bad.
38. Man (or Woman) from Mars This is similar to the Downward Arrow Technique. Let’s say a patient has a belief that causes pain, like “I’m inferior,” or “defective” or “worthless” and so forth. You explain that you’re a man (or woman) from mars, and you don’t quite understand how things work on the earth, and is it okay if you ask some questions. Then you can ask questions like these: Therapist (as Man from Mars). You say that you’re defective. We don’t have the concept
Additiona
a s to
nt ist
our
in in
a e
on Mars. Is it good or bad to be defective? Patient. It’s bad. Therapist (as Man from Mars). Oh, I see. And can you explain that to me? Why is it bad. For example, will they refuse to sell you coffee at Starbuck’s? What happens if you are defective? Patient. They’ll sell you coffee, but no one will love you. Therapist (as Man from Mars). Oh, I see. So if you’re dating, for example, do you have to demonstrate that you’re not defective? Are defective people not allowed to date? Patient. They’re allowed to date, but no one will date them. Therapist (as Man from Mars). That is so cool and so interesting. We just don’t have that idea on Mars. How do you find out if someone is defective? And what does it mean, really, to be defective? Patient. You can just tell when someone is defective? Therapist (as Man from Mars). Very cool! How do you tell? Do they have a mark of some type? Patient. You can just tell? Therapist (as Man from Mars). I still don’t get it, and need your help. I think I’m a slow learner. I saw on TV that many death row inmates get tons of letters from women who want to date and even marry them. Does this mean that they’re not defective? The idea is to lead the patient to the absurdity of their belief, or the label, they are using.
Anti
rocrastination e a iora Acti ation ec ni ues
39. Little Steps for Big Feats The patient breaks a complex task into tiny steps that can each be completed in just-minute or so.
40. Problem-Solution Method Schedule a time when you can do five minutes of the task you've been avoiding. Let's say you decide to start organizing the mess on your desk at 3:00 PM. Draw a line down the center of a piece of paper and list all the problems that will get in your way and all the excuses you'll give yourself for not getting started at 3:00 in the left-hand column. You might put, "A friend may call and need to talk," or "It may seem too anxiety-provoking," or "I may decide that I need to rest for a while first." You can put solutions to each problem in the right-hand column.
41. Mission Accomplished / I Stubbornly Refused Technique The patient agrees to do only five minutes’ worth of work on some problem he or she has been putting off. Let’s say the patient agrees to do five minutes’ worth of filing at 6 PM today. Then the patient must agree to call the therapist at 6:05 and leave one of two
Additiona
a s to
nt ist
our
in in
a e
messages—“Mission Accomplished” or “I Stubbornly Refused.” If the patient will not agree to do this, the therapist withdraws the assignment, since the patient is really saying that he or she isn’t going to do the assignment!
nterpersona
ec ni ues
42. Interpersonal Decision-Making When you're at odds with someone, you have three choices: you can settle for the status quo, work to make the relationship better, or leave the person you're not getting along with. Most of time, people know what they want, but sometimes it's confusing. You may ask yourself: "Should I get engaged or break up and look for someone more exciting?" Or, "Should I get divorced or try to make my marriage better?"
43. Relationship Journal The Relationship Journal can help you improve your relationships with family members, friends and colleagues. However, the main goal of the RJ is Interpersonal Enlightenment— this is the liberating but shocking discovery that you are creating your own interpersonal reality—for better or worse—at every moment of every day. There are five steps: Step 1. Write down one thing the other person said to you. Step 2. Write down exactly what you said next. Step 3. Analyze what you wrote down in Step 2. Was it an example of good or bad communication? Check it out using the EAR Checklist. Step 4. Think about the consequences of what you wrote down in Step 2. How will the other person think and feel? What will she or he say next? Will your response make the situation better or worse? Can you see how you’ve been forcing the other person to treat you in the exact way you’ve been complaining about? Step 5. Generate a more effective response using the Five Secrets of Effective Communication.
44. Intimacy Exercise After the patient has created an outstanding response, with the help of the therapist, in Step 5 of the Relationship Journal (RJ), the therapists and patient can role-play the problem. The therapist can be the person the patient is having trouble with, and can say what the patient wrote down in Step 1 of the RJ. Then the patient will respond, using the Five Secrets of Communication. The therapist will then give three kinds of feedback: 1. The letter grade (was it an A, a B, a C, or a D?) 2. What worked and what didn’t work. 3. How to improve, using the Five Secrets more effectively. Then the therapist and patient can do a role-reversal, and the therapist (now in the role of the patient) will be graded by the patient (who is now playing the role of the person he or she is at odds with.) Therapist and patient will continue doing role-reversals until the patient can get an “A” grade consistently. At that point, the patient can try using the Five Secrets between sessions with the person he or she is not getting along with.
Additiona
a s to
nt ist
our
in in
a e
The patient must agree to use the Relationship Journal for any interaction that does not go well, and must be advised that some failures will be inevitable while learning.
45. Paradoxical Inquiry When you’re training a patient in how to use the Five Secrets of Effective Communication to resolve a conflict with a loved one or friend, he or she may suddenly resist and say, “Why should I have to listen to him when he never listens to me?” You can reply along these lines? “Actually, you don’t have to listen, or empathize, or find the truth in what he’s saying. Are you saying you don’t want to?” Then if the patient sticks to his guns and insists he doesn’t want to use the listening techniques, you can say, “I’m glad you told me that. Sadly, I don’t know how to resolve conflicts without the listening skills. Perhaps I can help you with something else.” You can use a similar strategy for patient who insist they shouldn’t have to share their feelings openly, as well as those who resist Stroking (treating the other person with the spirit of admiration or respect.) This response also conveys the spirit of “Sitting with Open Hands,” rather than trying to persuade an oppositional or angry patient who is resisting treatment.
46. 12 GOOD Reasons NOT to Listen, Share Your Feelings, or Treat the Other Person with Respect You can give this document to clients who resist the Five Secrets of Effective Communication. It lists good reasons not to use the listening skills, not to use “I Feel” Statements, not to convey warm or respect to the person you’re in conflict with. The idea here is to “Sit with Open Hands” instead of trying to convince the oppositional, angry patient.
47. Relationship Probe I must warn you that this technique requires a meaningful agenda with both partners. They must both have a strong desire to develop a more loving relationship. If either of them has the secret agenda to get our of the relationship or to keep blaming the other person, this technique, and any technique, is certain to fail. This technique was developed by Dr. Don Baucom from the University of North Caroling. It can help with the initial evaluation of a couple in therapy. You ask the couple to talk for a couple minutes as they generally do when they are not getting along. Tell them that you will not interfere, and they can just ignore you. Explain that you will take notes and then make an interpretation for each of them when they are done. While they talk and argue, I take notes, writing down what they are saying, and try to figure out what the pattern is. There are not too many patterns, so you can usually figure it out pretty quickly. One common pattern is that each one criticizes the other, who then responds defensively or makes a counter criticism. Then I speak to each of them, asking if I am right in my understanding. I tell the other partner not to say anything or interfere when I’m talking to his or her partner. With each one, I follow this type of sequence. David: Jenet, I notice that one of the things you were try to tell Bill is that he doesn’t listen and doesn’t seem to want to spend much quality time with you. But every time you try to tell him this, he defends himself and criticizes you back, so you never really get heard. So you may end up feeling frustrated, hurt, angry, and lonely. Is that correct? Am I reading you
Additiona
a s to
nt ist
our
in in
a e
right? Jenet: That’s exactly right doctor. You nailed it! He puts up a wall and argues every single time. David: I’m sure that’s really painful for you. So I think you are saying that you really want him to listen and understand what you’re saying, so you can feel closer to him. Is that correct? Jenet: That’s exactly right. We haven’t felt close for months, may be for the past year or more. It’s just argue argue argue. David: So I think, Jenet, you’re saing you’d reall like to feel closer to Bill, and to have more of a loving, supportive relationship. is that correct? Jenet. Absolutely! David: Can you tell me why? Why do you want to be closer to Bill? I’m sure when you were dating, you had the pick of many men. What was it about Bill that particularly attracted you? What were some of the cool and exciting things about him, and what were the things you used to do together that you really loved and enjoyed? Now Jenet will tell you about Bill’s positive side and what she really loved about him, and what they used to do together that she cherished. This will include a long list of adjectives, like caring, good sense of humor, handsome, exciting, and on and on. Then I finish with this kind of interpretation. David: So I think what you’re saying Jenet, is that your grieving the loss of Bill, that handsome, sexy, caring, exciting fellow you fell in love with. And that every time you reach out to try to get close, you run into a wall of resistance. So you feel lost, hurt and kind of defeated and discouraged, and really lonely, because you miss Bill tremendously. You miss that fellow you love so deeply. Is that about it? Jenet will nearly always say, “That’s exactly right, doctor.” What we’ve done now is a radical Positive Reframe of the conflict from Jenet’s perspective. Then I turn to Bill, and ask how he was feeling just now, when he heard Jenet saying all those really beautiful things about him. In nearly all cases, he will have melted and say he was feeling really open to her, and surprised in a good way at what he’d just heard. That’s because troubled couples usually get into a rut of never-ending criticisms, so they no longer hear anything positive and loving. Then I turn to Jenet and say something like this: “Jenet, did you notice the sudden change in Bill? Instead of arguing and putting up a wall, he seems really warm, open, and receptive.” Jenet will confirm this. Then I ask, “How did you do that so quickly, Jenet. You seemed to transform him from an angry, defensive, enemy into a warm puppy dog in about one minute. How in the world did you make that happen?” Then I guide her to the insight that she was using “I Feel’ Statements and Stroking rather than arguing, criticizing, attacking or lashing out in frustration. I tell her that we might weant to remember Jenet’s hidden source of power later on, when we’re doing some couples’ communication training.(See the next technique.) Then I repeat the exact same sequence with Bill. This fairly simple and effective procedure helps you pinpoint and identify the dysfunctional pattern for each couple and gives you some gentle but powerful tools to quickly change it and give the couple greater feelings of closeness at the first session.
Additiona
a s to
nt ist
our
in in
a e
48. Don Baucom Technique (aka Machine Gun Therapy) This is an energetic way of doing communication training for couples. It is a form of behavior therapy, since you constantly shape and reshape the way both partners communicate, using positive and negative feedback. The goal is to reshape their compulsive dysfunctional pattern of arguing and bickering. In this exercise, you tell the partners to go ahead and talk about how things have been going, but advise them that you will interrupt the process over and over to provide each of them with guidance and suggestions. To continue with the example just illustrated, let’s say that Jenet is telling Bill that he didn’t do X, Y or Z during the week, or that she’s ticked of because he failed to keep his promise to do A, B or C, and that her tone is off-putting, sarcastic, or hostile and almost certain to trigger a defensive response in Bill. Before Bill can respond, you, the therapist, can intervene with a “compliment sandwich.” You start with a compliment, then suggest and model a modification in her statement, then end with another compliment, and an invitation for her to try again. Here’s what you might say as the therapist: Therapist: Jenet, I thought there was a whole lot of merit in what you just said. For one thing, you were very open with your feelings and told Bill exactly what he did and didn’t do that turned you off. Lots of people are kind of passive-aggressive and hide their feelings, but you are very direct and open, which is great. The only thing that might not work for you is that he might very well feel hurt and respond by arguing or criticizing something you did or didn’t do, and then you’ll be right back in that lonely, frustrating zone of frustration and loneliness. Let’s try again and remember your two secret tools—“I Feel” Statements and Stroking. So you might say something like this, “Bill this week when you did K, it meant so much to me, and reminded me of how much I love you and how lucky I am to have you as my husband and best friend. But when you do L it really hurt my feelings, and I felt sad and ignored. I wouldn’t feel that way if I didn’t love you so much.” Jenet: You deserve a loving and vulnerable response from Bill, so why don’t you try again, using the tools I just modeled, but putting things in your own words.” Then, if she does a reasonably improved job, you, the therapist, can compliment and reward her, so as to reinforce the more effective response. Then, when Bill responds, you can go through the exact type of pattern if his response is hostile or off-putting. This technique requires tremendous concentration and energy on the part of the therapist but provides an extremely rich therapeutic experience with multipole opportunities for learning for both partners at every therapy session. It is crucial that you express your feedback to both partners in a way that is respectful. Never force either partner to lose face in front of the other. Finally, as noted earlier, this technique, and all techniques, will fail if one or the other partner is not committed to developing a more loving relationship, and if either of the partners is unwilling to give up blame and continues to try to change the other person, rather than learning to change himself / herself. If either partner sabotages this process, and keeps arguing and lashing out, I temporarily terminate the couples therapy and meet with that person individually to re-establish his or her therapeutic agenda and find out if, in fact, he or she will be suitable for couples therapy.
Additiona
a s to
nt ist
our
in in
a e
Ideally, that type of agenda setting would have been done with each partner individually prior to accepting them into couples therapy. The ten vital questions I ask include these: • • • • • • • • • •
How committed are you to developing a more loving relationship? What would it be worth to you if I agreed to treat you and show you how to improve your marriage? Do you sometimes have thoughts or urges to separate or get out of your marriage? What kinds of changes would you like to see? What, in your opinion, is the cause of the problems in your marriage? Who, in your opinion, is more to blame for the problems in your marriage? Would it be upsetting to you if you discovered that you actually play a big role in the problems you’re having, and that it’s not all your partner’s fault? Who, in your opinion, needs to do most of the changing? If I agree to work with you, would you be willing to focus 100% of your energy on changing yourself, instead of blaming, criticizing, and trying to change your partner? Would you be willing to do psychotherapy homework between sessions, even if your partner refuses to do the homework?
If I don’t get a satisfactory answer to all of these questions, I usually will not accept the individual into couples’ therapy. I would still work with one or the other if either if she or he wanted individual therapy instead. In this case, it would not be appropriate to treat the other individually as well, since that would likely create a conflict of interest and confront you with an ethics violation.
49. Forced Empathy This technique is described on page Error! Bookmark not defined.. The patient plays the role of someone s/he is angry with or not getting along with. The therapist plays the role of a friend of that person. You tell the patient that the person s/he is not getting along with has taken truth serum, and must agree to tell the truth, the whole truth, and nothing but the truth. Then the therapist interviews that person, using the Five Secrets of Effective Communication., developing some empathy for the way that person is thinking and feeling. To be successful, the patient must have a strong desire to develop a more loving and satisfying relationship with the other person.
50. 25 Qualities I m Looking for in an Ideal Mate People who’ve been rejected typically idealize the person who rejected them, thinking that he or she was the most wonderful catch in the entire world. As an antidote, you can ask the patient to list 25 qualities he or she is looking for in an ideal mate, including: 1. 2. 3. 4. 5. 6. 7.
Available (this should usually be listed first) Right age range Preferred ethnicity Attractive appearance Honest Trustworthy Faithful
Additiona
8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25.
a s to
nt ist
our
in in
a e
Loyal Reliable Sexy Intelligent Sense of humor Shared values and beliefs Similar interests Solid career Gets along with my friends Adventuresome Good communicator Kind and caring Fun to be with Independent, not needy or clingy Charismatic, exciting, interesting Genuine, not phony Good listener Warm and compassionate
Of course, the characteristics and ordering will vary from person to person. Then you ask the patient to rate the person who rejected him / her in each category on a scale from 0 (not at all) to 4 (totally) and add up the total score (0 to 100). The patient can also rate other people s/he is dating on the same scale. The results are nearly always surprising and eye-opening from multiple perspectives. Sometimes, that “awesome person” who rejected the patient won’t score terribly high, and others will score higher than expected. You can also help the patient develop a scoring key. For example, if the score is • • • •
below 60, do not date 60 - 65: date at least once 70-75: date several times. > 75: marry immediately!
Of course, this scale is subjective and can be individualized for each patient.
t er 51. Relapse Prevention Training When a patient has completely recovered from depression and anxiety, let the patient know that relapse is inevitable but does not need to be a severe problem if she or he is prepared. Preparation involves several steps and takes about 30 minutes. 1. The patient must know that the method that worked for them will always work for them in the future. For example, she or he may have been helped by the Hidden Emotion Technique, Positive Reframing, Examine the Evidence, Experimental Technique, or Acceptance Paradox. Whatever it was, try it again when the same
Additiona
a s to
nt ist
our
in in
a e
kinds of negative thoughts and feelings return, and it will usually be effective once again. 2. Fill out a Relapse Daily Mood Journal with the patient, indicating how they’ll be thinking and feeling when they relapse. The will have Negative Thoughts like these: • This relapse proves the therapy didn’t work. • I’m hopeless after all. • The therapy was just a band aid. • My improvement was just a fluke. • I just thought I was feeling better, but I was fooling myself. • Now I can see the truth, that I really am worthless. 3. Encourage the patient to identify the distortions in these thoughts. 4. Role play how to crush these thoughts using the Externalization of Voices. Do not discharge the patient until s/he can knock all the Negative Thoughts out of the park. 5. You can also use Externalization of Voices with the Negative Thoughts that were causing the depression and anxiety in the first place. 6. Encourage the patient to record this relapse prevention Training on his or her cell phone and listen to it when the Negative Thoughts return. 7. Tell the patient he or she can come back anytime for a tune-up if needed.
a s
a e
Comparing the Role-Playing Techniques* Technique
Patient’s Name
Therapist’s Name
RoleReversals?
Paradoxical Double Standard
His or her real name
The name of an imaginary dear friend of the same gender as the patient, but not someone the patient knows.
Externalization of Voices
His or her real name
Same name as the patient
Externalization of Resistance
His or her real name
Same name as the patient
His or her real name
You play the role of some judgmental or critical person the patient is afraid of.
A former high school classmate the patient runs into at a high school reunion. This classmate is now incredibly successful, famous and wealthy.
The patient’s name
His or her real name
You play the role of a seductive Devil who tempts the patient to give in to a seductive, positive thought that tempts the patient to give in to a habit of addiction.
No!
Some person the patient is not getting along with.
A trusted friend of person the patient is not getting along with.
No
His or her real name.
A curious person from Mars who does not understand how things work on earth.
No
Some person who the patient believe would judge him / her.
A friend of the person who is gossiping about the patient.
His or her real name.
Some person who the patient the patient is not getting along with, like his or her spouse, family member, or friend..
Feared Fantasy
High School Reunion
Devil’s Advocate Technique Forced Empathy Man (or Woman) from Mars Anti-Brushfire Technique Intimacy Exercise
No Yes Yes Yes
Yes
No Yes
a s
a e
Strategies for Defeating Dysfunctional Negative or Positive Thoughts* Strategy
General Concept
Negative Thought
Example of How to Defeat the NT
Self-Defense Paradigm
Victory. You defeat or crush the NT by arguing with it and insisting that it’s not true.
A patient who suddenly relapses several weeks after recovery will often have this thought, “This shows that the therapy didn’t work and that I really am a hopeless case.”
“That’s ridiculous. I had a fight with my wife last night, so it’s not surprising that I’d be feeling upset. The therapy was very effective, and this would be a good time to pull out the tools I learned and get to work.”
Acceptance Paradox
Surrender. You defeat the NT by buying into it and insisting that it is true, but you do this with a sense of humor or inner peace.
During a moment of insecurity, a therapist may have the thought, “I’m not as good as I should be.”
“As a matter of fact, I still have tons of flaws and a great deal to learn. Even when I’m 85 years old, there will still be tons of room for learning and improving, and that’s kind of exciting.”
Be Specific
Reality. You defeat Overgeneralization or Labeling by asking for specific flaws; then you can use Thinking in Shades of Gray as well as the Acceptance Paradox.
“I’m a loser” or “I’m a failure as a father” or I’m a bad mom,” etc.
You ask, “What are some specific things I’ve failed at, or errors that I’ve made?” Or, “What are the things I do as a father (or mother) that aren’t so good?”
Positive Reframing
Seduction. You show what’s positive about a negative thought or feeling: the advantages of thinking or feeling that way, and what it shows about you that’s positive and awesome.
“I’m a loser,” or “I’m defective.”
This thought shows that you
• • • •
have high standards. are realistic, since you do have many flaws. are accountable, since you’re not blaming everyone else. humble.
In addition, your high standards may motivate you to work hard and not settle for mediocrity.
Methods with Book Page Numbers
Burns' tools Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Therapist e-book
Feeling Good
01. Empathy (also see 5 secrets, zero technique)
Basic
233-359, 564-565
02. Agenda Setting
Basic
383-512, 566-568
03. Identify the Distortions
Basic
31-43, 238537, 542, 239, 402581 403
04. Straightforward Technique
Basic
572-575
05. Double Standard
Compassion
582-591
06. Examine the Evidence
Truth
591-599
185-191, 304-306
The Feeling Good Handbook
10 Days to SelfEsteem
When Panic Attacks
638-656
115-127
656-677
8-11, 98-99
62-65
49-51
137-138
133-143
327-341
100-101, 164-165
92, 97, 105-106
144-146, 379-380
123-124
102-104, 139-140, 226-229
92, 97, 250-252
146-163
Truth
599-602
08. Survey Technique
Truth
602-609
107-108, 118
92, 97
163-167
09. Reattribution
Truth
609-614
111-112
99
167-170
10. Socratic Method
Logic
614-618
11. Thinking in Shades of Gray
Logic
618-620
104-107, 142-143
98, 157, 266-267
171-176
Semantic
620-625
109-111, 150-151
98-99, 130, 157
179-182
12. Semantic Method
Semantic
625-632
108-109
14. Be Specific
Semantic
632-635
15. Self-Monitoring (Counting what counts or counting the positive)
Quantitative
636-642
16. Negative Practice / Worry Breaks Quantitative
642-646
Humor Based
205-206
230-231
Role Playing
659-670
16-26
191-198
70-72, 202205, 383384
19. Externalization of Voices
06/12/2020
121-123
647-651
651-659
6-7
185-190
198-200
Humor Based
458-461
182-185
349, 358
18. Shame-Attacking Exercises
Intimate Connections
97 101-102, 164-165
372-373
Feeling Great
38 77, 174, 193-194, 287, 429
07. Experimental Technique
17. Paradoxical Magnification
Feeling Good Together
122, 127129
209-214
63-64
1
Burns' tools Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
20. Feared Fantasy
Category
Role Playing
Therapist e-book
The Feeling Good Handbook
Feeling Good
130-136, 173-174, 244-247, 356-357
670-683, 877-879
38, 67, 243248
10 Days to SelfEsteem
When Panic Attacks
59-60
99, 122140, 268
214-220, 358-359, 384-386
176-180
683-699
22. Time Projection
Visual Imaging
700-702
23. Humorous Imaging
Visual Imaging
702-703
24. Cognitive Hypnosis
Visual Imaging
703-731
25. Individual Downward Arrow (Vertical Arrow)
Uncovering
731-740
263-271 122-126, 135
26. Interpersonal Downward Arrow (rules vs roles)
Uncovering
740-749
287-288, 291
27. What-If Technique
Uncovering
749-757
287-288
127-132
28. Hidden Emotion Technique (getting in touch)
Uncovering
757-768
248-251
10-11, 2530, 313-336
113-116, 166, 296123-127, 298, 355 140, 146-147
308-313 plus 66-67, 221several 229, 380more 381, 430
206-208
29. Straightforward and Paradoxical CBA
Motivational
772-798
30. Devil's Advocate Technique
Motivational
798-802
31. Stimulus Control
Motivational
802-803
32. Decision-Making Form
Motivational
803-811
33. Daily Activity Schedule
Motivational
811-813
34. Pleasure Predicting Sheet
Motivational
813-819
104-107, 318-322
35. Anti-Procrastination Sheet
Motivational
819-825
99
36. Gradual Exposure and Flooding (see also Fear Hierarchy)
Exposure
833-844
06/12/2020
844-846
Intimate Connections
279-284, 384-386
Philosophical / Spiritual
Exposure
Feeling Great
134, 173176
21. Acceptance Paradox
37. Response Prevention
Feeling Good Together
101-107, 186-187 222-227
61, 63, 97, 298-306, 169, 113
228-230
230-234
275-278
129-131, 147-149
183-184, 314-136
235-238, 435
35-40
695
233-234
242-243, 436
233, 252 360-362
141, 147149, 161
251-267 264-267, 372-373
2
Burns' tools Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Therapist e-book
Feeling Good 377-378
The Feeling Good Handbook
10 Days to SelfEsteem
When Panic Attacks
Feeling Good Together
Exposure
846-849
39. Cognitive Flooding
Exposure
849-854
40. Image Substitution
Exposure
854-859
41. Memory Rescripting
Exposure
859-864
275-279
42. Smile and Hello Practice
Exposure
865-865
288-292
43. David Letterman Technique
Exposure
865-870
288, 303309
44. Self-Disclosure
Exposure
870-872
45. Flirting Training
Exposure
872-875
292-299
46. Rejection Practice
Exposure
875-877
299-300
47. CBA Blame
Interpersonal
894-904
51-55 (All book) 150-153
242-243
253-255, 268-284 377-378
372
240-241
272-275
274-279
48. Revise Your Communication
Interpersonal
904-913
412-419
49. Five Secrets of Effective Communication
Interpersonal
913-931
see below
Interpersonal
Intimate Connections
131-132, 267
38. Distraction
50. One-Minute Drill
Feeling Great
290-303
931-938
303-309
150-151, 177-185
324-325
186-190, 218-219, 264-265
125
51. EASY Diagnostic Survey 52. BMS
Testing
32-39, 416
3-5, 456
72-102, 417-421
169-187
53. Specialized BMS (see happiness, intimacy, etc.) 54. Evaluation of Therapy 55. Daily Mood Log (triple column technique)
Testing
56. What's My Grade
Testing, Empathy & Basic
57. Disarming
Interpersonal
117-119, 376-385, 137 406-407, 419
303-306, 309, 363
100-114, 194-195
58. Thought Empathy
Interpersonal
385-386, 407, 419
303-306
118-120, 195-197
06/12/2020
545-570
63, 66
74-96
59, 79-80
255-256
3
Burns' tools Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Therapist e-book
Feeling Good
The Feeling Good Handbook
10 Days to SelfEsteem
When Panic Attacks
Feeling Good Together
59. Feeling Empathy
Interpersonal
386, 407, 419
303-306
120-122, 195-197
60. Inquiry
Interpersonal
390-395, 407-408,419
304-306
128-133, 197
Interpersonal
389, 408409, 412, 419
78-79, 134139, 197304-306 201
62. Stroking
Interpersonal
311-312, 400-402, 409, 419
304-306
63. Change the focus
Interpersonal
424-427, 649
64. Multiple Choice Empathy
Interpersonal
61. I Feel...
Feeling Great
Intimate Connections
140-149, 201-202 237-242 251-255
65. Interpersonal Postitive Reframing 66. Humor 67. Invitation straightforward 68. Invitation paradoxical
Basic
383-385
69. Specificity Step
Basic
385-390
70. Conceptualization
Basic
390-397
71. Miracle Cure
Basic
524
181
72. Magic Button
Basic
n/a
28, 39
73. The Acid Test
Basic
n/a
163
74. Externalization of Resistance (voicing the resistance) 75. Dangling the Carrot
Advanced
76. Gentle Ultimatum
Advanced
77. Sitting with Open hands
Advanced
78. Fallback Position
Advanced
79. Double Paradox 80. Triple Paradox
Motivational
81. Worst, Best, Ave
Logic
82. Habit/Addiction Log
Testing
Bonus Chapter
83. Checklist of Positive Distortions
06/12/2020
4
Burns' tools Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Therapist e-book
Feeling Good
The Feeling Good Handbook
10 Days to SelfEsteem
When Panic Attacks
Feeling Good Together
Feeling Great
Intimate Connections
84. Devils Advocate (yes, listed twice) 85. Paradoxical Double Standard 86. High School Reunion
Exposure
87. Anti-Brushfire Technique 88. Person from Mars 89. Little Steps for Big Feats
Motivational
90. Problem Solution
Motivational
231-233, 236 825-831
310-311, 348
238-241 244-247
91. Mission Accomplished / Stubbornly Refused Technique 92. Interpersonal Decision-Making 93. Relationship Journal
Testing
68, 260
286-288, 398-399
94. Intimacy Exercise 95. Paradoxical Inquiry
Advanced
96. Barriers to Listening (Good Reasons NOT to...)
Interpersonal
924-926
443-446
24-30, 56, 73
97. Relationship Probe 98. Machine Gun/ Don Baucom Tech. Interpersonal 99. Forced Empathy
Interpersonal
a100. Twenty-five Qualities I’m Looking for in an Ideal Mate a101. Relapse Prevention Training Alternative Interpretations Method
54
Antiheckler technique
Interpersonal
Antiperfectionism Sheet
Quantitative
Antiwhiner technique
Interpersonal
But Rebuttal Technique
Motivational
107-109
Can't Lose System
Logic
124-126
06/12/2020
145
See disarming
356-359 222
See empathy
5
Burns' tools Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch CAT - The Counter Attack
Category
Therapist e-book
Feeling Good
10 Days to SelfEsteem
When Panic Attacks
Feeling Good Together
Feeling Great
345-347 Semantic
167-169
Desert Island Fantasy Exposure Log Fear Hierarchy & Gradual Exposure
Intimate Connections
Philosophical / Spiritual
Compartmental Technique Cooling Hot Thoughts
The Feeling Good Handbook
41-42 Exposure
432
Exposure
254-258, 431
Forgetful Twin/Clone Give Yourself Credit
Motivational/ Compassion
201-202
Grieving Method (type of self monitoring)
Quantitative
308-309
Happiness Test
Testing
Intimacy Inventory
Testing
10-17
Lonliness Scale
Testing
4-5
Magic Dial
Basic
9-10
n/a
30, 198-199
Make a Plan
235-236
Mirror Method
129-131
Moorey Moaner
Interpersonal
223-225
Paradoxical Approach for sexual issues
243-244
Phobia Log
Exposure
Pivot Question
Basic
n/a
30, 162
Positive Reframing (Examples Table) Basic
n/a
26-30, 3558, 182-198
Positive reframing interpersonal version
Interpersonal
Process vs Outcome
243-250 366-367
Recovery Circle
Basic
Relationship Satisfaction Scale
Testing
Self Defeating Beliefs
Uncovering
06/12/2020
433
176-179 423
205 41-46
6-7
98, 146158
6
Burns' tools Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Self-Defense or Self-Endorsing
Compassion
Stick Man or Stick Figure
Uncovering
Tempations Test
Testing
Tempting thoughts vs Loving Thoughts
Motivational
TIC/TOC Technique
Motivational
Twelve Motives that Compete with Love
Interpersonal
Zigzag technique
Semantic
06/12/2020
Therapist e-book
Feeling Good
The Feeling Good Handbook
10 Days to SelfEsteem 122, 131137, 268
109-110 82-90
When Panic Attacks
Feeling Good Together
Feeling Great
Intimate Connections
214-215
44-55 8
110-113
196-200, 205-206
230-233 23-30
634-635
7
Methods with Book Page Numbers in Alphabetical Order
Alphabetical Version Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Therapist e-book
Acceptance Paradox
Philosophical / Spiritual
Acid Test
Basic
n/a
Basic
383-512, 566-568
Agenda Setting
The Feeling Good Handbook
Feeling Good
38, 67, 243248
683-699
10 Days to SelfEsteem 99, 122140, 268
When Panic Attacks
Feeling Good Together
Feeling Great
Intimate Connections
214-220, 358-359, 384-386
176-180 163
656-677
38
Alternative Interpretations Method
54
Anti-Brushfire Technique Anti-Procrastination Sheet Antiheckler technique Antiperfectionism Sheet Antiwhiner technique
Motivational
819-825
Interpersonal
695
See disarming See empathy
222
Barriers to Listening (Good Reasons NOT to...) Interpersonal
924-926
Be Specific
632-635
24-30, 56, 73
443-446 185-190
BMS (wt or wto Eval. of Therapy Session) Testing
32-39, 416
But Rebuttal Technique
Motivational
107-109
Can't Lose System
Logic
124-126
CAT - The Counter Attack
Philosophical / Spiritual
CBA Blame
Interpersonal
894-904
CBA Straightforward and Paradoxical Change the focus
242-243, 436
356-359
Interpersonal
Motivational
233-234
145
Quantitative
Semantic
99
772-798
Interpersonal
3-5, 456
51-55 113-116, 166, 296123-127, 298, 355 140, 146-147
308-313 plus 66-67, 221several 229, 380more 381, 430
424-427, 649
55, 61, 63, 97, 298-306, 169, 113 237-242
Checklist of Positive Distortions Cognitive Flooding Cognitive Hypnosis Compartmental Technique
06/12/2020
Exposure
849-854
Visual Imaging
703-731
253-255, 268-284
345-347
1
Alphabetical Version Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Therapist e-book
Conceptualization
Basic
Cooling Hot Thoughts
Semantic
Daily Activity Schedule
Motivational
811-813
Testing
545-570
Daily Mood Log (triple column technique) Dangling the Carrot David Letterman Technique Decision-Making Form
Feeling Good
The Feeling Good Handbook
10 Days to SelfEsteem
When Panic Attacks
Feeling Good Together
Feeling Great
390-397 167-169
63, 66
74-96
59, 79-80
72-102, 417-421
169-187
Distraction
255-256
Advanced Exposure
865-870
Motivational
803-811
288, 303309
Desert Island Fantasy Devil's Advocate Technique
Intimate Connections
41-42 Motivational
798-802
Exposure
846-849
Compassion
582-591
228-230 377-378
230-234
275-278
131-132, 267
242-243
Double Paradox Double Standard
101-102, 164-165
137-138
133-143
53-54
EASY Diagnostic Survey Empathy (see 5 secrets, zero technique)
Basic
233-359, 564-565
185-191, 304-306
638-656
Truth
591-599
327-341
100-101, 164-165
92, 97, 105-106
144-146, 379-380
54
123-124
102-104, 139-140, 226-229
92, 97, 250-252
146-163
56
115-127
458-461
Evaluation of Therapy see BMS Examine the Evidence Experimental Technique Truth Exposure Log Externalization of Voices Fallback Position Fear Hierarchy & Gradual Exposure
Exposure Role Playing
432 122, 127129
659-670
209-214
63-64
316
Advanced 254-258, 431
Exposure
Feared Fantasy Role Playing
06/12/2020
599-602
670-683, 877-879
130-136, 173-174, 244-247, 356-357
134, 173176
279-284, 384-386
59-60, 93-94, 174-175
2
Alphabetical Version Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch Five Secrets - Disarming Five Secrets - Feeling Empathy
Category
Therapist e-book
Feeling Good
Five Secrets of Effective Communication
When Panic Attacks
Feeling Good Together
117-119, 376-385, 137 406-407, 419
303-306, 309, 363
100-114, 194-195
Interpersonal
386, 407, 419
303-306
120-122, 195-197
Interpersonal
389, 408409, 412, 419
Interpersonal
390-395, 407-408,419
304-306
128-133, 197
Interpersonal
311-312, 400-402, 409, 419
304-306
140-149, 201-202
Interpersonal
385-386, 407, 419
303-306
118-120, 195-197
see below
303-309
150-151, 177-185
Five Secrets - Stroking Five Secrets - Thought Empathy
10 Days to SelfEsteem
Interpersonal
Five Secrets - I Feel... Five Secrets - Inquiry
The Feeling Good Handbook
Interpersonal
913-931
Flirting Training
Exposure
872-875
Forced Empathy
Interpersonal
Feeling Great
Intimate Connections
78-79, 134139, 197304-306 201 54-55
292-299
Forgetful Twin/Clone Gentle Ultimatum
Advanced
Give Yourself Credit
Motivational/ Compassion
Gradual Exposure and Flooding (see also Fear Hierarchy)
Exposure
Grieving Method (type of self monitoring)
Quantitative
Habit/Addiction Log Happiness Test
201-202 833-844
233, 252
251-267
308-309 Bonus Chapter
Testing Testing
Hidden Emotion Technique (getting in touch)
Uncovering
High School Reunion
Exposure (Feared Fantesy)
9-10 757-768
248-251
10-11, 2530, 313-336
Humor Humorous Imaging
06/12/2020
Visual Imaging
702-703
206-208
3
Alphabetical Version Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Identify the Distortions Basic
Therapist e-book
Feeling Good
The Feeling Good Handbook
537, 542, 581
31-43, 238239, 402403
8-11, 98-99 240-241
Image Substitution
Exposure
854-859
377-378
Individual Downward Arrow (Vertical Arrow)
Uncovering
731-740
263-271 122-126, 135
Uncovering
740-749
287-288, 291
10 Days to SelfEsteem
49-51
When Panic Attacks 77, 174, 193-194, 287, 429
Feeling Good Together
6-7
Feeling Great
Intimate Connections
16-26
50-51
272-275 141, 147149, 161
101-107, 186-187
Interpersonal Decision-Making Interpersonal Downward Arrow (rules vs roles)
222-227
Interpersonal Positive Reframing Intimacy Exercise Intimacy Inventory
Testing, Empathy & Basic
10-17
Invitation straightforward Let's Define Terms Little Steps for Big Feats
Semantic
625-632
108-109
182-185 231-233, 236
Motivational
238-241
Lonliness Scale
4-5
Machine Gun/ Don Baucom Tech.
Interpersonal
Magic Button
Basic
n/a
28, 39
Magic Dial
Basic
n/a
30, 198-199
Make a Plan
235-236
Memory Rescripting
Exposure
Miracle Cure
Basic
859-864
275-279
524
181
Mirror Method
129-131
Mission Accomplished / Stubbornly Refused Technique Moment in Time (DML, relationship journal, habit log, etc.) Moorey Moaner
Interpersonal
Multiple Choice Empathy
Interpersonal
Negative Practice / Worry Breaks
Quantitative
06/12/2020
223-225 251-255 642-646
349, 358
198-200
4
Alphabetical Version Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch
Category
Therapist e-book
Feeling Good
The Feeling Good Handbook
10 Days to SelfEsteem
When Panic Attacks
One-Minute Drill Paradoxial Invitation
Interpersonal
931-938
Basic
383-385
324-325
Feeling Good Together
Feeling Great
Intimate Connections
186-190, 218-219, 264-265
Paradoxical Approach for sexual issues
243-244
Paradoxical Double Standard Paradoxical Inquiry
Advanced
Paradoxical Magnification
Humor Based
647-651
205-206
Person from Mars Phobia Log
Exposure
Pivot Question
Basic
Pleasure Predicting Sheet Positive Reframing (Examples Table)
Motivational Basic
Positive reframing interpersonal version
Interpersonal
Problem Solution
Motivational
433 n/a 813-819
30, 162 104-107, 318-322
129-131, 147-149
183-184, 314-136
235-238, 435
35-40 26-30, 3558, 182-198
n/a 243-250 825-831
Process vs Outcome
310-311, 348
244-247
366-367
176-179
Qualities I’m Looking for in an Ideal Mate
171
Reattribution
Truth
Recovery Circle
Basic
Rejection Practice
Exposure
609-614
111-112
99
167-170 423
875-877
205
299-300
Relapse Prevention Training Relationship Journal
Testing
68, 260
286-288, 398-399
Testing
41-46
6-7
Relationship Probe Relationship Satisfaction Scale Response Prevention Revise Your Communication Self Defeating Beliefs
06/12/2020
Exposure
844-846
Interpersonal
904-913
Uncovering
264-267, 372-373
360-362
(All book) 150-153
412-419
125, 306-310
98, 146158
5
Alphabetical Version Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch Self-Defense or Self-Endorsing
Category
Therapist e-book
Compassion
Feeling Good
Exposure
870-872
372
Self-Monitoring (Counting what counts or counting the positive)
Quantitative
636-642
121-123
Semantic
Shame-Attacking Exercises
Humor Based
Sitting with Open hands
Advanced
Smile and Hello Practice
Exposure
865-865
Socratic Method
Logic
614-618
Specificity Step
Basic
385-390
Stick Man or Stick Figure
Uncovering
Stimulus Control
Motivational
802-803
Straightforward Technique
Basic
572-575
Survey Technique
Truth
602-609
Tempations Test
Testing
Tempting thoughts vs Loving Thoughts
Motivational
274-279
651-659
When Panic Attacks
Feeling Good Together
Feeling Great
Intimate Connections
214-215 290-303 191-198
109-111, 150-151
620-625
10 Days to SelfEsteem 122, 131137, 268
109-110
Self-Disclosure
Semantic Method
The Feeling Good Handbook
98-99, 130, 157
179-182
56
70-72, 202205, 383384
230-231
288-292
86-89
Specialized BMS see happiness, etc.
Thinking in Shades of Gray TIC/TOC Technique
Logic
Time Projection Triple Paradox
Motivational
Twelve Motives that Compete with Love
Interpersonal
What-If Technique
Uncovering
What's My Grade
Testing, Empathy & Basic
Worst, Best, Ave
Logic
62-65
44-55 97
107-108, 118
92, 97
163-167 8
618-620
Motivational Visual Imaging
06/12/2020
82-90
372-373
104-107, 142-143
98, 157, 266-267
110-113
196-200, 205-206
230-233
171-176
700-702 23-30 749-757
287-288
127-132
56
6
Alphabetical Version Copyright (Various dates) © by David D. Burns, M.D. List compiled by Angela Poch Zigzag technique
06/12/2020
Category Semantic
Therapist e-book
Feeling Good
The Feeling Good Handbook
10 Days to SelfEsteem
When Panic Attacks
Feeling Good Together
Feeling Great
Intimate Connections
634-635
7
NEW – Advanced Empathy
Ad anced E pat a id
ec ni ues urns
an in t e
ocus
You focus on the process rather than the content of the argument. In other words, you might gently point out that the two of you are arguing and not working together as a team. You bring the conflict to conscious awareness in a kindly way, so you can both talk about your feelings, rather than trying to figure out who's right and who's wrong. In a sense, there's an elephant in the room, but everyone's ignoring the tension pretending it isn't there. When you change the focus, you point to the elephant and say, "Do you see what I see?" u tip e
oice E
pat
When you have no idea where someone is coming from, and they're reluctant to tell you, you can suggest several possibilities and ask if any of them ring a bell. It's like priming the pump. You might say, “I can imagine you might be feeling X, Y, or Z. Do any of those words ring a bell?” X, Y and Z could be words from the Feeling Words chart. Multiple-Choice Empathy can be especially helpful when the other person refuses to open up and tell you how they're feeling. You'll have to be disarming rather than blaming when you list the possible reasons why the other person doesn’t want to talk to you. You'll also have to do this in a way that sounds caring, respectful, and concerned, and not demanding or condescending. ositi e Re ra
in
You put a positive spin on the situation. For example, you can reframe an angry conflict as a golden opportunity to develop a better relationship with the person you’re at odds with, rather than viewing the problem as a prelude to Armageddon. You can also reframe the other person's motives or behavior in a positive way. For example, if someone seems stubborn, dogmatic, and argumentative, you could think of them as having intense conviction and desperately wanting you to understand them. You can also consider the almost possibility that you haven’t been disarming them in a genuine way, and that’s the precise reason they keep arguing. Or, if a loved one is acting nasty, you could reframe their behavior as an expression of the hurt, loneliness, or frustration she or he is feeling.
* Copyright © 2007 by David D. Burns, MD. Revised 2014.
Change the Focus
Page 1
Change the Focus Collection from Dr. David Burns & the Tuesday Group. Special thanks to Jill Levitt for the “how to” list.
Definition: You focus on the process rather than the content of the argument. In other words, you might gently point out that the two of you are arguing and not working together as a team. You bring the conflict to conscious awareness in a kindly way, so you can both talk about your feelings, rather than trying to figure out who's right and who's wrong. In a sense, there's an elephant in the room, but everyone's ignoring the tension pretending it isn't there. When you change the focus, you point to the elephant and say, "Do you see what I see?"
Resources: Podcast # 158: Changing the Focus, one of the Advanced Secrets https://feelinggood.com/2019/09/16/158-changing-the-focus-one-of-theadvanced-secrets-of-effective-communication/ Feeling Good Together: Chapter 28 - Changing the Focus: Is there an elephant in the room?
When to Use it: How do you know when you need to use CTF in a session? One huge tip is when you feel uncomfortable—frustrated, anxious, annoyed, defensive, or unsupported. That’s a good time to ask yourself what’s going on in your interaction with this patient. Here are some scenarios where CTF would be indicated: ·
Where the patient is talk, talk, talking (and sometimes in the tone of constant complaining) and does not seem to listen to you, and does not seem interested in getting to work on anything.
·
Patient ignores the therapist’s attempts to set the agenda and get down to work.
·
Patient who accepts the invitation to get to work on something, but then when you ask what s/he would like to work on today, s/he kind of ignores you and jumps to yet another complaint.
Change the Focus
Page 2
·
Patient ignores what you just said.
·
You and the patient are arguing / debating about some conceptual idea or theory.
·
You and the patient are just schmoozing without doing any real work using Methods.
·
You are feeling bored during the session and find yourself daydreaming.
·
You wish you didn’t have to see this patient today.
·
You find yourself feeling annoyed with the patient, or not liking the patient.
·
The patient comes late to sessions.
·
The patient keeps “forgetting” to do psychotherapy homework.
·
A patient who continually says “I’ll try” to do the homework, but never really does any homework.
·
Where you are trying to “help” and the patient is “yes-butting” you.
·
Another common one would be where you see less than stellar scores on the Evaluation of Therapy Session, but when you ask about it, the patient kind of “saves you” or changes the subject or denies any negative feelings about you or the previous session. For example, he or she might say “Oh, I never give perfect grades,” or some such evasive comment.
·
Another clinical example would be when you are trying to do E = Empathy with a patient, but you are kind of feeling some dislike for the patient, or you are feeling a lack of genuine warmth and connection, or it feels “yucky” and not comfortable. This actually happened to me recently during a session with a co-therapist colleague, and I had to use Changing the Focus. Also, my brain was flooded with self-critical negative thoughts at the time—this is why Changing the Focus can be very challenging!
·
A common personal / clinical situation is where you are trying to interact with someone who is reluctant to talk, or who completely refuses to talk.
·
A personal situation would be where you are feeling socially anxious during an awkward silence with a friend, family member, or even someone you are dating.
·
Another personal example would be where a friend or family member is treating you in a kind of brusque or mildly hurtful way, but avoiding you to some extent and brushing you off when you try to engage him / her in some dialogue.
Change the Focus
Page 3
When would Five Secrets empathy vs CTF be indicated during a session? When there is no elephant in the room (some dynamic/tension/problem, etc.) being ignored. When you need to bring something to conscious awareness.
How to do Change the Focus : There are six parts to the changing the focus method (order can be varied): 1) Notice the tension Ask permission — Label it & Invite client to a new conversation --"I just wanted to stop us for a minute--I just noticed that...." OR “Could we talk a bit about something I noticed coming up?” 2) I feel — Embarrassed, a little bit frustrated, a little bit awkward, stuck, etc. 3) Feeling empathy — And I wonder if you might be feeling ---annoyed with me, frustrated, rushed by me, etc. 4) Stroking — I really enjoy working with you, I care about you, you have been so persistent, I would love to be able to help you with your anxiety, etc. TIP: this can go before I feel especially if the topic is controversial or inflaming. 5) The positive reframe — Even though this is a little bit awkward to bring up, or even though this is uncomfortable to notice, I am really hopeful that we can talk about this and I am thinking that this might actually be an opportunity in disguise. (e.g., it might be a chance for us to get back on the same page, or for me to understand you better, or for us to improve our work together, or this reminds me of the discomfort you feel with other people, and I am hopeful that if we can think about and better understand what is happening between the two of us that it might help you in your other relationships as well!) 6) Inquiry — Have you noticed this too? How were you feeling just now? or This seems important I wonder if you can tell me what this has been like for you? TIP: Inquiry about the process NOT the content.
Troubleshooting: When you are working with challenging or aggressive or critical patients, it is easy to get upset, and then to get distracting by our own negative feelings. This can interfere with the effective use of the Five Secrets as well as CTF. It can be helpful to pinpoint your own negative thoughts so you can find the distortions in them and challenge them effectively.
Change the Focus
Page 4
Ask yourself: What is the content of the interaction / dialogue / dispute? Careful NOT to get caught up in this! What is process that’s going on between the patient and therapist? Here is where you want to focus. If you cannot answer these questions in a crisp, totally clear manner, reach out to the group, via the emailing list, and ask for help. Bring your written answers to the group.
What prevents you from using CTF: ·
Therapist’s Conflict Phobia - The therapist does not want to acknowledge or deal with the conflict. Afraid of addressing it.
·
Therapist’s Anger Phobia - The therapist does not want to acknowledge or deal with anger. Either their own or the clients.
·
Therapist’s “Niceness.” - They feel they are 100% to blame and struggle with feelings of discomfort toward a client. They think they are not allowed to or shouldn’t have negative feelings toward their client.
·
Therapist’s determination to “save” or “rescue” the patient - The therapist gets stuck trying to help the client. Their desire to help is at odds with sitting with open hands and the client’s free will.
Other tips: What are two or three potential benefits from using CTF? ·
First, it requires self-awareness which is a useful skill to the therapist in preventing bias from disrupting therapy.
·
Secondly, it can be a tool that creates even more therapeutic regard or alliance between the client and the therapist.
·
Thirdly, it can be the breakthrough the client needs to move forward. Since we are cyclic creatures the behaviour patterns within the therapeutic relationship are likely patterns in the clients other relationships.
Change the Focus
Page 5
CHANGING THE FOCUS PRACTICE SHEET Created by: Daniele Levy, Jill Levitt, David Burns
A)
Frame the problem (therapist only):
What is happening between you and the client that is counter-productive to the therapy? (e.g., evading invitation to work, yes-butting, intellectual power struggle, endless venting, lack of specificity, etc.)
How did you notice that? If a neutral third party came into the room, what would they see that is a clue to this problem?
What is your role in this dynamic?
What you doing or failing to do that may be contributing to it?
How are you feeling about the dynamic?
How do you think the patient is feeling about the dynamic?
B)
Frame the delivery (therapist to patient): 1.
Stop the process: "I just wanted to stop us for a minute…”
2. Get buy in from patient for changing the focus: “I wanted to talk for a few minutes about something that I am noticing…is that ok?”
Change the Focus
Page 6
3. Be sure to use the DISARMING TECHNIQUE, so you can “take the blame” for the problem. This helps the patient save face and minimizes the likelihood that he or she will feel blamed or defensive. For example: “I notice that when I asked you if you wanted to get to work, you didn’t respond to my question, but continued to talk about your problems with X. I have a hunch you’re trying to let me know that I’m rushing you too much, and that you need more time to talk and vent and get some support.”
4.
Use other 5 Secrets to share your point, namely: a. I FEEL b. STROKING c. FEELING EMPATHY
5. Insert POSITIVE REFRAME, if helpful acknowledge awkwardness of the conversation, but highlight expected positive outcome: “Even though this is a bit uncomfortable to bring up, I am really hopeful that if we talk about it, it would be a great chance for us to get back on the same page and move forward towards the goals we set for your therapy…”
6. Close with specific INQUIRY: “Have you…sensed this tension too?....noticed this cycle of back and forth?...found that we are caught up in this hidden power struggle?...” Am I reading you correctly- and did you notice that just happened?”
NEW – Assessment of Resistance Expanded Information, Tips, and Flowcharts (Paradoxical Agenda Setting)
2016 Workshop Handout aradoxida A enda ettin a id
urns
Dr. Burns' email: david feelinggood.com Website: www.feelinggood.com Table of Contents A = Assessment of Resistance or Paradoxical Agenda Setting = PAS The Five Steps in Agenda Setting
2
Why Our Patients Resist
3
Paradoxical Agenda Setting (PAS)—Basic Concepts and Techniques
5
• Definition of Outcome Resistance
6
• Definition of Process Resistance
8
• Basic PAS Techniques
9
• Techniques that Target Outcome Resistance
12
• Techniques that Target Process Resistance
19
Overview of Positive Reframing
21
Positive Reframing Table
23
Paradoxical Agenda Setting
Page 2
The Five Steps in Agenda Setting* By David D. Burns, M.D. 1.
The Invitation. At the beginning of each session, patients need the chance to tell you how they've been feeling. After you've listened for a while, you can ask if they're ready to roll up their sleeves and get to work on the problems that are bothering them, or if they need you to listen for a while longer. This conveys the idea that listening alone won't be sufficient, and that active effort will be required if they really want to change their lives.
2.
Specificity. If the patient accepts the invitation, ask them what problem they'd like to work on first. They may want help with depression, anxiety, a marital conflict, or a bad habit. Then ask them to describe one specific moment when they were struggling with that problem. For example, can they tell you about a time when they were feeling depressed, anxious, or angry with their spouse? It could be anything, but the problem must be specific as to: •
Person. Who were they with? What was going on?
•
Place. Where were they?
•
Time. What time of day was it?
Vague complaints, like "I need better self-esteem," "Life stinks," or "I think I'm codependent," won't work. The problem must be real, and it must be something that the patient wants help with. 3.
Conceptualization. Once the patient describes the problem, ask yourself what type of problem it is. Is it: • • • •
An individual mood problem, such as anxiety or depression? A relationship problem, such as anger or a conflict with a family member, friend, or colleague? A habit or addiction, such as an eating disorder, drug or alcohol abuse, smoking, or procrastination? A non-problem, such as healthy sadness or grief, where no therapeutic techniques other than empathic listening are required? Some problems will fall into more than one category. For example, a woman may be depressed because of a problem in her marriage. Or, a man may be struggling with shyness and substance abuse. 4.
Motivation. Does the patient really want to get better, or does he simply want to talk about the problem while you listen? How hard will he work to solve the problem, if you agree to help him with it? How many sessions is he willing to spend on it? Will he do homework assignments between sessions? Your conceptualization of the problem will help you predict the most likely forms of resistance you're likely to run into. Depression, anxiety, anger and addictions are all associated with unique forms of Process Resistance and Outcome Resistance. Together, you and the patient can think about all the reasons why he may not want to change (Outcome Resistance) or why he may not want to do what it's going to take to get better (Process Resistance). Then you can let him try to persuade that he really does want to change, even though there are many good reasons to maintain the status quo.
5.
Methods. Depression, anxiety, anger and addictions all respond to different kinds of techniques. The techniques you use will depend on the way you conceptualize the problem.
*
Copyright © 2005 by David D. Burns, M.D. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
Page 3
Why Our Patients Resist* By David D. Burns, M.D.
Outcome Resistance— Why Patients Cling to the Status Quo
Process Resistance— Why Patients Resist Working Hard To Change
Depression
Depression
Worthlessness. I don't deserve to feel good because I really am inferior or defective. Guilt. I don't deserve any happiness or self-esteem because I'm bad and I deserve to suffer. Realism of Depression. Life really is awful. People who feel happy are stupid and naïve. Perfectionism. If I beat up on myself relentlessly whenever I fall short, it will motivate me to achieve great things. Achievement Addiction. I couldn't possibly feel happy or fulfilled until I've accomplished something outstanding. But I've never done anything special, so I could never feel any real joy or self-esteem. Love Addiction. I couldn't possibly feel happy or fulfilled without a loving relationship. Self-Pity. I like being a victim and feeling sorry for myself.
Anxiety
Magical Thinking. My fears protect me or my loved ones. If I stop worrying, something terrible may happen. No Pain, No Gain. My constant worrying is the price I have to pay to do superb work. If I stop worrying, I'll get complacent and fail. Conflict / Anger Phobia. I don't want to face the problem that's triggering my anxiety in the first place.
Hopelessness. Nothing will ever change, so why try? If I don't get my hopes up, I won't be disappointed. Motivational Paralysis. I don't feel like doing any self-help assignments between sessions. I'll wait until I'm in the mood. Overwhelmed. The psychotherapy homework assignments are just too much work. I'm drowning in commitments and don't have time to do more. Entitlement. I shouldn't have to work so hard to recover. Medical Model. My doctor said that I have a chemical imbalance in my brain, so a pill should cure me. Traditional Psychiatric Model. I thought that all I had to do was come to sessions, talk about all the problems in my life, and explore the past.
Anxiety
Avoidance. Facing my worst fears will be dangerous and uncomfortable. I shouldn't have to do that. There has to be an easier way. Medical Model. The ad I saw on TV said that my shyness results from a chemical imbalance in my brain, and that an antidepressant will solve the problem.
* Copyright © 2005 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
Page 4
Why Our Patients Resist (cont'd)*
Outcome Resistance— Why Patients Cling to the Status Quo
Process Resistance— Why Patients Resist Working Hard To Change
Anger / Relationship Problems
Anger / Relationship Problems
Low Desire. I don't really want to get close to you. I just want to complain about you and keep you at a distance! Martyrdom / Heroism. I like the role of victim. Moral Superiority. I enjoy feeling superior and looking down on you. You're a loser. Gossip / Scapegoating. It's rewarding to talk to my friends about what a loser you are. They all agree with me, too! Power. I want to control you. Revenge. I have every right punish you because of the way you've treated me. Anger addiction. I like feeling angry and bitter. It's rewarding. Violence. Aggression is exciting. I enjoy hurting you. Self-Righteousness. I treat you badly because you deserve it. It's the right thing to do.
Habits and Addictions
Instant Rewards. My habit is pleasurable. Why give it up? Entitlement. I shouldn't have to change. Narcissism. I'm special. I deserve this donut (or drink). Denial. I don't have a problem! Conflict Phobia. I'd rather get high than face the problems that are bothering me.
Truth. I'm right and you're wrong. Blame. Our problems are all your fault, so why should I have to change? Pride. I can't stand the humiliation of examining my own role in the problem. Entitlement. I deserve better treatment. I shouldn't have to work so hard to solve the problems in our relationship. Fear. Something bad will happen if I try to get close to you. You might hurt me or make me look bad. It's safer to keep you at a distance. Hopelessness. You're such a stubborn, self-centered jerk that nothing could possibly work. Why should I bother to try?
Habits and Addictions
Deprivation. Giving up my habit will be painful and uncomfortable. Ugh! Who wants that? Hopelessness. I've tried over and over but nothing works, so why get my hopes up? I'll just end up feeling frustrated and disappointed again.
* Copyright © 2005 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
Page 5
Paradoxical Agenda Setting (PAS)—Basic Concepts and Techniques* By David D. Burns, M.D. Do You Need Paradoxical Agenda Setting? At the risk of over-simplification, we could say that there are two basic approaches to, or philosophies about, psychotherapy that I call “passive / non-specific” and “active / specific.” In non-specific psychotherapy, the patient talks and the therapist listens, asking occasional questions to guide the patient in a particular direction. There’s no psychotherapy homework, and few specific tools. The goals, too, are somewhat general, focused perhaps on personal growth. During the first half of the 20th century, most schools of psychotherapy were of the non-specific type. Psychoanalysis and psychodynamic therapy would be classic examples on non-specific therapy, as was the “Emotive / Supportive” brand of psychotherapy I was trained in as a psychiatric resident. Karl Rogers said it best when he proposed that empathy is the necessary and sufficient condition for personality change. About mid-way through the 20th century, things slowly began to change, with the emergence of numerous specific forms of psychotherapy, such as Behavior Therapy, Cognitive Therapy, and a host of others. Now the approach to treatment was completely different in at least six critical areas. First, specific “disorders” were diagnosed and the symptoms of those disorders became the target of the treatment—general growth was no longer the focus. For example, the goal of the therapy might be to eliminate the patient’s panic attacks or feelings of depression. Second, the patient’s symptoms were measured with brief, accurate assessment tests so that progress, or the lack of progress, could be tracked and documented. Third, the therapist and patient worked together actively and collaboratively, almost as co-equals. This involved a fundamental change in the nature of the therapist / patient relationship. Fourth, the therapist used specific tools such as Exposure, Response Prevention, or a large number of cognitive restructuring techniques, to facilitate change. The choice of tools depended on the nature of the patient’s symptoms. Fifth, the patient was required to do psychotherapy homework between sessions so as to accelerate learning and progress. And finally, the treatment was time-limited and brief. Although the concept of “resistance” was always important in the non-specific therapies, it loomed even larger in the emergence of the new specific therapies because of the intense emphasis on collaboration, homework, measurement, and accountability. If the patient will not pick up the tools and use them, the treatment is doomed to failure. And the failure becomes far more obvious because of the overwhelming push for rapid and measurable change. The techniques in this memo will hopefully be illuminating and of great importance to you if you are using one of the newer, specific forms of psychotherapy. But if you are doing a more non-specific type of therapy, where the patient talks and you simply listen or occasionally offer some advice, you will probably find these concepts relatively irrelevant to the type of work you do. Paradoxical Agenda Setting is designed to enhance therapeutic collaboration by reducing two powerful types of resistance, Outcome Resistance and Process Resistance. Outcome Resistance means that even though the patient may want a positive treatment outcome (e.g. help with depression, anxiety, a relationship problem, or a habit or addiction) there are likely to be many internal and external factors that * Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
6
keep the patient stuck. As a result, he or she may resist change and appear unmotivated. Often, these factors are not in the patient’s conscious awareness, but they can be brought to conscious awareness fairly easily. Process Resistance means that even if the patient does want a positive treatment outcome (e.g. recovering from depression or anxiety), she or he may not want to do what will be necessary to bring that change about. Outcome Resistance. Here are some examples of Outcome Resistance: • • • •
A depressed man may think that he deserves to suffer because he did something morally bad or failed in some way. An intensely anxious woman may feel that her anxiety serves a protective function, and may think that something terrible will happen if she gives up the compulsive worrying. A woman with a troubled relationship may not want to get close to the person that she’s complaining about and may not be asking for help. A man with a habit or addiction, like alcoholism, binge eating, or an internet porn addiction may not want to give up his greatest, and perhaps only, source of pleasure and reward in a life that feels stressful and unrewarding.
Initially, most patients won’t be aware of these outcome resistance factors. If you bring them to conscious awareness with skill and compassion, there often will be a kind of an “ah-ha” experience for patients and therapists alike. It can be extraordinarily freeing for the patient and for the therapist as well. That’s because any techniques you use to help the patient will become far more effective after you’ve melted away the patient’s resistance. Outcome Resistance may be somewhat unintuitive and difficult to grasp at first. After all, the patient is coming to sessions, and may be paying for the sessions, so we naturally conclude that he or she wants help. Most of our training is predicated on this notion as well. For example, if the patient has OCD, we may recommend Exposure and Response Prevention, or think about prescribing certain types of medications that might be helpful. But what if the patient isn’t really asking for help, or has mixed feelings about change? Then your efforts to “help” may trigger resistance. The patient may “yes-but” you, insisting that nothing could possibly help, or may simply “forget” to do the psychotherapy homework. The harder you push, the more the patient pushes back. You may conclude that the patient is being stubborn, unreasonable, or oppositional, and the patient may conclude that you just don’t care or understand. Both you and your patient may begin to feel frustrated and burned out, and a subtle struggle may evolve. The patient seems to want to talk endlessly, while you keep trying to “help.” In a moment of annoyance, you may label your patient as a “help-rejecting whiner.” Once you suddenly “see” why the patient is resisting, you will have much deeper empathy and far greater power to help the patient. Here’s a simple example. A psychologist came to me for help with test anxiety. Her licensure examination was coming up in six weeks, and she was bombarding herself with distorted thoughts, such as, “They’ll only ask about the things I don’t know and none of the things I do know.” Or, “I
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
7
just know I’m going to flunk the test.” On the Daily Mood Log, she rated her feelings of panic, anxiety, and worrying at 100%. Her negative thoughts were clearly unrealistic. In the first place, it was not true that the test would only contain questions about things she didn’t know with no questions about things she did know. In addition, although the psychology licensure examinations were challenging, she was a top student and had never once flunked a test in her entire career. Her negative thoughts were classic examples of several cognitive distortions, including “All-or-Nothing Thinking,” “Mental Filter,” “Discounting the Positive,” “Fortune-Telling,” “Emotional Reasoning,” and “Other-Blame.” There were also some hidden “Should Statements.” When I encouraged her to challenge these thoughts she became oppositional and defiant. She claimed that her negative thoughts were realistic. We began to argue about who was “right” and who was “wrong,” but that was going nowhere. At this point I had to back off, empathize, and ask myself why she was fighting me so vigorously when I was simply trying to help. My therapeutic error was a common one. I wasn’t taking Outcome Resistance into account. Although she was suffering and feeling miserable, maybe she had some good reasons for making herself anxious. I suggested we might list the advantages and disadvantages of her worrying on a Cost-Benefit Analysis form. Together, we came up with many advantages. For one thing, her self-criticisms showed that she had integrity, since the test would be difficult, and she wasn’t going to fool herself with some kind of phony Pollyanna positive thinking. The worrying also showed that she had high standards for herself, and wasn’t going to settle for mediocrity. In addition, she listed this advantage: “My worrying has always motivated me to work hard, and it’s paid off. It’s the price I’ve had to pay for my success. If I stop worrying, I may get so complacent that I’ll flunk the test.” These powerful advantages of her anxiety made it clear why she was fighting me so intensely. Then we listed several disadvantages, including this one: “My worrying has gotten so severe that I haven’t done one minute of study or preparation in the past five weeks. I’m totally stuck.” When she wrote that down, it was like turning on a light bulb in her brain. Yes, there were many advantages of worrying, but there was an elephant in the room that she’d been ignoring. We resolved this motivational impasse with the Magic Dial. I pointed out that some anxiety can be productive and healthy, but she was so anxious that she was paralyzed. I pointed out that she’d rated her anxiety at 100%, and asked how much anxiety she’d want, between 0% and 100%, if we had a Magic Dial and could set the dial to the optimal number. She said that 20% would probably be plenty. I suggested that we could work together to lower the anxiety to that level, and promised her that if the anxiety fell below 20%, I’d show her how to become more anxious so she wouldn’t get overly complacent. At this point, she was able to challenge her negative thoughts successfully. There was an immediate reduction in her anxiety, and she began studying for the test, which she passed with flying colors several weeks later. She told me that once she started studying, her anxiety actually dropped all the way to 0%. In this case, I used two PAS tools: the Cost-Benefit Analysis and the Magic Dial. If I had not used them, I don’t believe the treatment would have been nearly as effective, and may even have failed.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
8
Process Resistance. This concept is a little easier to understand. Process Resistance means that even if the patient does want a positive treatment outcome (e.g. recovering from depression or anxiety), she or he may not want to do what will be necessary to bring that change about. For example: • • • •
A depressed man may not want to do psychotherapy homework between sessions because he feels so hopeless, unmotivated, and overwhelmed. An anxious woman may not want to confront her fears using exposure techniques because the exposure seems so dangerous and terrifying. A man with a troubled marriage probably won’t want to examine his own role in the problem because he’s totally convinced the problems are all his wife’s fault. A woman with an addiction may not want to have to go through withdrawal. A student with a habit, like procrastination, may not want to face the anxiety of studying or doing the tasks he’s been putting off.
The four patterns of Outcome and Process Resistance are independent and separate from each other. Furthermore, a patient could experience either Outcome or Process Resistance for a problem, such as depression, or both, or neither. And sometimes you may conceptualize the patient’s problem as having more than one component: For example, if the patient is struggling with depression following a romantic rejection, it could be conceptualized as an individual mood problem and a personal relationship problem as well. So there could be two potential forms of Outcome Resistance and two potential forms of Process Resistance. The following chart summarizes the four key themes for Outcome and Process Resistance for depression, anxiety disorders, relationship conflicts, and habits and addictions: Depression
Anxiety
Relationship Problems
Habits / Addictions
Theme of Outcome Resistance
NonAcceptance
Magical Thinking
Not Wanting to Get Close
Pleasure / Entitlement
Theme of Process Resistance
Psychotherapy Homework (HW)
Exposure
Giving up Blame
Deprivation / Discipline
You can learn more about these eight patterns of Outcome and Process Resistance in my two-page memo entitled, “Why Our Patients Resist Change.” In addition, the one-page memo entitled “The Five Steps in Agenda Setting” will show you the overall structure of Agenda Setting during therapy sessions. Finally, the chapters and written exercises in my eBook, Tools, Not Schools, of Therapy, will be very useful. PAS may be very challenging for you to learn, for technical and emotional reasons, because you will have to let go of your own agendas and become far more aware of your blind spots and biases. It is well worth the effort, because PAS is arguably the most powerful, exciting, and liberating tool in all of psychotherapy. Below, you will find brief descriptions of Basic PAS Techniques, Techniques that Target Outcome Resistance, and Techniques that Target Process Resistance. You may notice that there is some overlap among the techniques. Some are just different ways of saying the same thing or achieving the same goal. Once you have grasped Paradoxical Agenda Setting, you may find that you will create new techniques that will be suitable to your personal therapeutic style and your treatment setting.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
9
Basic PAS Techniques
1. Empathy It is crucial to empathize without trying to “help” or “solve the problem” at the start of every therapy session, before you begin Agenda Setting. The amount of time each patient needs for empathy will vary. Some patients will be satisfied with just a few minutes of skillful listening. Other patients will need much more empathic listening and support before they’ll feel ready to role up their sleeves and get to work on one of the problems they’ve described. In addition, once you begin Agenda Setting, the patient may resist or get upset, angry, or overwhelmed with emotion at any time. Your best initial response will always be empathy, using the Five Secrets of Effective Communication: The Disarming Technique, Thought and Feeling Empathy, Inquiry, I Feel Statements, and Stroking. Once the patient feels accepted and relaxed again, you can go back to Agenda Setting, starting with the Invitation Step. Many therapists who read the two paragraphs above will feel they understand them when they don’t. When I observe seasoned or novice therapists working with real or simulated patients who express tremendous pain and suffering, the therapists nearly always jump in prematurely with reassurance or advice, without paraphrasing the patient’s words (Thought Empathy) and exploring the patient’s feelings (Feeling Empathy). Reassurance has the effect of turning the feelings off, much like a faucet, and may indirectly convey the message that the therapist is afraid of the patient’s feelings. This common error can result from a problem I call emotophobia (the therapist’s fear of intense negative feelings) as well as from codependency (the therapist’s need to help or rescue the patient). Overcoming this problem requires systematic practice as well as a significant shift in the therapist’s mindset. I have developed powerful role-playing exercises that are described in the Empathy chapters of my book: Tools, Not Schools, of Therapy. Video examples of the Empathy exercises will also be available soon at TeamTherapyTraining.com. 2. The Straightforward Invitation Although the Invitation is the first step in Agenda Setting, it’s also a useful motivational tool you can use at any time in the treatment when you suspect that motivational issues may be holding the patient back. There are two versions: the Straightforward and the Paradoxical Invitation. You can use the Straightforward Invitation when the patient is reasonably motivated and cooperative and struggling with depression and anxiety. Here’s an example: “You’ve been describing some extremely painful problems, and my heart goes out to you. I’d like to offer you more than just listening and support, and I have some wonderful tools I’d love to share with you. I have no doubt that if we work together, we can bring about some tremendous changes in your life. I’m wondering if this would be a good time for us to roll up our sleeves and get to work on one of those problems, or if you’d like to vent some more first? Talking and getting support can be tremendously important and helpful, and I don’t want to jump in before you feel ready.” This statement conveys several messages: •
I know you’re suffering.
•
I have some wonderful tools available to help you.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
10
•
The prognosis is positive.
•
A good outcome will require more than just listening.
•
I need you to confirm that you do want help, and if this is a good time to start using some of the tools.
The question here is “when do you want help” and the therapist’s working assumption is that the patient probably does want help. 3. The Paradoxical Invitation You can use the Paradoxical Invitation when the patient does not seem especially motivated to work, but instead seems to want to complain. This tool is especially important when the patient is struggling with a relationship problem, or with a habit or addiction. Here’s an example: "Is this problem (with your spouse, or your OCD, or your drinking, etc.) something you'd like help with? Or did you simply want me to understand how painful this has been for you?" The question here is “do you want help” and the therapist’s working assumption is that the patient probably does NOT want help. Essentially, you are asking the patient, in a kindly way, to lay his or her cards on the table. 4. Sitting with Open Hands Sitting with Open Hands means that although you’re eager to help your patient, if she or he wants to change, you don’t have a need to help him or her. It means that you are truly willing to have your patients remain symptomatic. For example, if a patient has OCD and is a hoarder, or washes his hands 50 times a day to prevent contamination, you are okay with that. You don’t see it as your job to persuade him to change. You are emotionally at peace with his hoarding or compulsive washing, even though this might not be your preference for him. Your job is to find out if there is something he does want help with, and not to impose treatments on him based on his diagnosis or some problem he might have. Sitting with Open Hands is important for one reason: If you try to help patients who have not asked for help, you will usually run into a wall of resistance and the therapy will be unsuccessful. Many therapists struggle with the idea of Sitting with Open Hands. They feel the need to jump in, trying some technique they think might help, without taking the time to find out what, if anything, the patient wants help with, and without resolving the patient’s Outcome and Process Resistance. While this always results, in part, from the therapist’s benevolent desire to help the patient, it can also result from an intense need to rescue patients and can be an expression of the therapist’s narcissism or codependency. Sitting with Open Hands means that we are not experts in how people should think, feel or behave. We are not trying to sell patients on some model of ideal mental health. Patients have to tell us what they want help with, and let us know how much the solution would be worth to them. When patients don’t want help, we can open our hands and let go. This is a vitally important concept. You may be reading about it without truly comprehending what it means. Or, you may understand it without being able to implement it.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
11
Sitting with Open Hands means mean letting go of your need to help. But this need to help is so basic and automatic that it’s almost like a knee-jerk reaction. We may jump in to rescue or help a patient almost without noticing what we’re doing. I have seen many therapists struggle with this tendency; some have found that personal work can help them prepare for Sitting with Open Hands. Sometimes, something inside of us may have to change before we can help our patients change. 5. Fallback Position This is related to the concept of Sitting with Open Hands. What will you do if the patient is not ready, willing, or able to pick up and use the tools she or he needs to recover? For example, a depressed patient might be unwilling to do psychotherapy homework (HW), or a shy, anxious patient might be unwilling to use exposure techniques until she feels more confident. This is where your “Fallback Position” comes into play. Your Fallback Position is how you make patients accountable. There are several approaches. First, you can tell your patient that you really want to work with her, and would love to show her how to overcome the depression or crippling shyness that’s been making her life so miserable. In addition, you feel convinced that the two of you could achieve those goals if you worked together (this is called Dangling the Carrot). But the tools you use will not be effective without doing psychotherapy HW between sessions, such as the Daily Mood Log or Pleasure Predicting Sheet, or exposure techniques for anxiety. You could suggest that the patient might want to seek treatment from a local therapist who does not require psychotherapy HW or exposure, while at the same time emphasizing that you like her and hope to work with her, but the HW and exposure would not be negotiable. This approach is especially powerful at the initial evaluation, before you have accepted the patient for treatment. The following approach may be more suitable for student therapists who have less therapeutic autonomy, as well as for clinicians who have already accepted unmotivated and resistant patients into treatment. You could say something along these lines, "I'd really love to help you with your depression, but the tools I use for depression are not likely to be effective without the psychotherapy HW. Perhaps there’s some other problem we could work on instead." Here’s another way to express a Fallback Position: "I’d really love to help you with your depression, but for us to bring about meaningful change you’ll need to do daily psychotherapy homework, and you’re saying this is too much for you right now. We could spend a few sessions just talking and I could offer you support, but I’m concerned that this may not help your symptoms of depression. And you’ve told me that you’ve had years of talk therapy, and you’re still feeling worthless and hopeless. Overcoming your depression will take quite a bit of work, but it could be life-changing, what do you think?" 6. Changing the Focus This is an advanced empathy technique that can be a vitally important PAS tools as well. Although it is extremely simply, it is surprisingly hard to grasp and implement. When you use Changing the Focus, you focus on the process, rather than the content of the interaction, or conflict, between you and the patient. In other words, you might gently point out that the two of you are arguing, or getting derailed, and not working together as a team. You bring the conflict to conscious awareness in a kindly way, so you can focus on feelings, rather than trying to figure out who's right and who's wrong. In a sense, there's an elephant in the room, but everyone's ignoring the tension pretending it isn't there. When you use Change the Focus, you point to the elephant and say, "Do you see what I see?"
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
12
Suppose, for example, that the patient has been venting and complaining about all the problems in his life, and you’ve been empathizing, using the Five Secrets of Effective Communication. After a while, you issue the Invitation Step of Agenda Setting. For example, you might ask if the patient would like some help with one of the problems he has been describing, or if he needs more time to talk while you listen and provide support. Instead of answering this question, he may simply ignore you and continue to complain. You might feel frustrated, annoyed, or shut out. Many therapists would simply repeat the question and ask if there is a problem the patient wants help with—but that ignores the tension and might lead to a power struggle, because the patient will probably continue to be slippery and avoid answering the question. That because some patients do not come to treatment for help, in the sense of working hard to solve some problem in their lives, but simply to vent, complain, and get occasional support. If you use “Changing the Focus,” you might say something like this instead: “Jim, I’m not sure if you noticed what just happened. I asked you if you wanted some help with one of the problems you’ve been describing, and it seemed to me that you didn’t answer the question, but just kept talking. Did you notice that? I’m feeling a bit awkward right now, and I’m wondering how you’re experiencing our interaction. Can you tell me what‘s going on from your perspective? Are you feeling frustrated or annoyed with me? Have I perhaps jumped in too quickly to ask if you want to work on one of the problems without providing enough warmth and support while you’ve been talking?” It’s important to deliver this type of message in a curious and supportive tone of voice, and not in a defensive or adversarial way. If you use Changing the Focus skillfully, it can have a powerful effect of ending any kind of game that’s going on between patient and therapist. Instead of playing the game, you bring the game to conscious awareness. You can use Changing the Focus whenever tension emerges during a therapy session. It is not just an Agenda Setting technique, but a more general therapeutic skill. Techniques that Target Outcome Resistance
7. Dangling the Carrot When you are offering to help a patient, you can indicate optimism about what might happen if the two of you work together as a team. The way you express this will depend on your own personality, experience, and level of training, but you must offer patients something tangible if you are asking them to work hard and engage in the therapeutic process. Successful use of this technique may serve as a “hook” to encourage the patient to commit to the necessary work to achieve recovery. For example, when I’m working with a shy patient, I might say something like this: “Jim, I’d love to help you with your shyness so you can start dating and find someone to love. I’d also enjoy helping you with your public speaking. I also used to struggle with both of these problems, and now I talk to people everywhere I go, and I make my living doing public speaking. I believe I can show you how to overcome these problems, and I have some powerful techniques to share with you. Would you be interested in working on your shyness and public speaking anxiety?” Novice and experienced therapists sometimes have trouble Dangling the Carrot because they feel insecure and aren’t convinced they really can help the patient overcome depression, panic attacks, a trouble marriage, or an addiction to alcohol. In my eBook, Tools, Not Schools of Therapy, I describe 50 powerful treatment techniques you can use to help patients with practically any kind of problem. IN * Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
13
addition, when you role-play and practice with colleagues, or get consultations on patients you feel stuck with, you will gain more confidence, since you’ll know you have many specific tools available for different kinds of problems. Then you’ll be able to offer the Invitation step and Dangle the Carrot with greater conviction. 8. The Miracle Cure This is both a data gathering step as well as a useful Agenda Setting tool that may give you some important insights about why the patient is stuck. Once the patient has described the problem (such as procrastination, feelings of inadequacy, or a troubled relationship), you can ask what a “miracle cure” might look like. You might say something like this: “Suppose today was the most amazing session, and you walked out of the session thinking that our work together had changed your life in some fantastic, wonderful way. What would that change look like? What would be different? What would the solution to this problem look like?” Of course, the way you ask this question will depend on the nature of the problem the patient wants help with. A student who procrastinates may say that he would suddenly feel motivated to study and work on his dissertation. A woman who feels inferior and inadequate may say that she’d suddenly have great accomplishments. A man with a troubled relationship with his brother might say that his brother would suddenly stop his constant criticizing, whining, and blaming. You may notice that in all of these examples, the patient is asking for magical results that we cannot provide without hard work and accountability on the part of the patient. In these instances I might say, “I’d love to offer you that kind of solution, but I can’t. What I can offer you would be quite different.” Then you could point out that the student who procrastinates isn’t entitled to feel motivated until after he’s gotten to work, and that getting to work is going to be very anxietyprovoking. At this point, you could ask if he’d be willing to tackle the task he’s been putting off in spite of how boring and anxiety-provoking it’s going to be. Or you could point out that you don’t have the magical ability to create any amazing accomplishments during today’s session for the woman who feels inferior—so that if she does want to walk out of today’s session, or any session, feeling tremendous joy and self-esteem, it will probably involve a tremendous change in her standards and expectations and ways of thinking about herself. Then you could ask if she’d be willing to do that? Would she be willing to learn how to love and accept herself as she is right now, warts and all, if you agreed to teach her how? Or, you could point out that the man with a troubled relationship with his brother would have to stop blaming his brother for the problems in their relationship and focus all of his energy on pinpointing his own role in the problem and changing himself. That’s because his brother isn’t here asking for help. You could also point out that it may seem awfully unfair that he should have to do the changing when his brother is the one who’s screwed up. You could also let him know that you’ve got some terrific tools to share with him, but if he feels strongly that he shouldn’t have to change, or doesn’t want to change, it would be entirely understandable and you’d be more than happy to work with him on some other problem instead. A colleague made this comment after reading about the Miracle Cure technique: “This is important so you don’t ASSUME that you know what your patient wants help with, or how much the patient wants his or her life improved. I have used this technique a ton and am often shocked at what the patient’s “miracle cure” would look like.”
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
14 9. Magic Button
This is another wonderful tool for Outcome Resistance. You tell the patient to imagine there’s a Magic Button on the desk. If they push it, all their symptoms will suddenly and totally disappear with no effort at all. For example, if they have been seeking treatment for feelings of depression, shame, and worthlessness, the moment they press the button they’ll immediately feel joy and self-esteem, with no effort whatsoever. They’ll walk out of today’s session in a state of euphoria. You ask them if they want to push the button. Most patients will immediately say yes. Then you can point out all the reasons NOT to press the button. This is a way of bringing their Outcome Resistance to conscious awareness. If you do this skillfully, the patient will nearly always try to convince you of all the reasons to change. Generating reasons the person may not want to push the button requires a familiarity with the eight most common sources of Outcome Resistance for depression, anxiety, relationship problems, and addictions, which I’ve summarized in the table called “Why Our Patients Resist.” However, in most cases, the resistance will be somewhat unique to each patient, so you’ll have to think creatively and individualize the Magic Button for each person you work with. You may worry that you may guess at a source of outcome resistance and be wrong. This is very common. As long as you suggest reasons not to change with empathy, humility, and curiosity, you can be creative in offering possibilities and trust that your patient will correct you if an idea does not fit. 10. Acid Test Most patients will immediately agree to push the Magic Button. It sounds great to have all of your negative feelings suddenly vanish, just by pushing a button. However, the patient hasn’t yet grasped what we’re really offering. We’re offering to help patients feel happy and fulfilled in spite of their problems and shortcomings. We can’t change the facts of any patient’s life in today’s session. We can only help the patient develop greater happiness and self-esteem in spite of those facts. When you do the Acid Test, you make the patient suddenly aware of the implications of pressing the Magic Button. For example, let’s say you’re treating a college freshman who was raised in Hong Kong. She is severely depressed because she’s way behind in her studies, and she has been procrastinating and lying around in bed instead of attending classes, taking careful notes, and studying hard. She feels lonely, ashamed, and frustrated, and constantly criticizes herself. She graduated at the top of her high school class, and her father expects her to major in electrical engineering and take over his computer chip company in Hong Kong some day. She’s perfectionistic and she’s not living up to his expectations or her own. So she says she’d gladly press the Magic Button and walk out of today’s session feeling joy and selfesteem. Then you say, “But keep in mind that when you press the Magic Button, your feelings will change dramatically, but the facts of your life won’t change. You will STILL be way behind in your studies and you will STILL be getting Bs and Cs instead of As, but you’ll no longer be feeling depressed and worthless. Is that what you want, to be a happy mediocre student?” That’s the Acid Test. She might say “yes.” This will probably mean that she’s ready to go to work talking back to her self-critical negative thoughts. She may already understand that her relentless self-criticisms won’t help her catch up in her studies, and may even make things worse. But she’ll probably say “No! That sounds terrible. I don’t want to be happy unless I’m really doing well in my studies.”
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
15
Then you might say something like this: “I think you might be telling me that you WANT to feel miserable today, as a way of punishing yourself, or motivating yourself. And it seems like you’re already doing a pretty good job of punishing yourself. So perhaps that’s not something you need help with.” Now you’ve placed her in a paradox. You can help her escape from the trap she’s fallen into with a little psycho-education, or with the Magic Dial. Like all powerful tools, this one takes practice, and must be done with genuineness and warmth or it will backfire. A colleague asked for a little clarification on why these techniques might backfire, and that’s superimportant to understand. As therapists, we are human, and it’s easy—in fact, inevitable—that we will at times feel frustrated and annoyed with patients who appear to “resist” our efforts to help them. For examples, some patients may “yes-butt” us over and over as we keep bombarding them with our “helpful” or “logical” advice. In these circumstances, you may be tempted to use PAS sarcastically, as a weapon to put the patient down, or to encourage the patient to drop out of therapy. For example, you might say, “Oh, it sounds like you really want to feel sorry for yourself, don’t you? So I guess you don’t want to get better!” Well, on some level these statements are true. We all get to feeling resentful and sorry for ourselves at times, but if you confront the patient with this in an uncompassionate manner, the patient will feel hurt and outraged, and may even drop out of therapy. PAS has to come from the heart, and it has to be done with kindness, genuineness, and compassion or it won’t be effective. PAS works best when it actually makes sense to you why the patient might not want to change, and you’ve been able to use empathy to truly understand the dangers of changing from the patient’s perspective. 11. Positive Reframing When you use this technique, you become the voice of the patient’s subconscious resistance and verbalize all the reasons NOT to change, but you cast them in a flattering light. In essence, you make the patient proud of his or her resistance. A businessman named Samuel sought treatment after ten years of depression. Prior to his depression, he had been dating a divorced woman with a teenage son named Timmy. Timmy was hanging out with the wrong crowd and getting into trouble with the law. Samuel took the boy under his wing, and was determined to change his life for the better. He taught Timmy extreme skiing, a sport Samuel excelled in. The boy feel in love with the sport and turned his life around. The bond between Samuel and Timmy was fantastic. When Samuel married Timmy’s mother, he made Timmy the best man at his wedding. One year the two were skiing together down a dangerous and challenging slope, and there was a sudden avalanche. Samuel managed to escape, but Timmy was swept off a 60 foot cliff. Samuel called for the rescue helicopter, and skied down to Timmy. Sadly, Timmy had a broken neck and died in Samuel’s arms. And for the next ten years, this negative thought continued to plague Samuel: “I killed my wife’s only son.” He felt depressed, worthless, guilty, ashamed, lonely, and hopeless. Psychotherapy and antidepressants had not helped at all. He said that friends told him he had to grieve, so he cried almost constantly for two years, but that hadn’t helped either.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
16
I asked Samuel how well he’d been functioning during those ten years of depression. He said he’d lost interest in his work, and had barely earned enough money to squeak by each year. Instead, he’d been using most of his time and energy raising money to buy wheelchairs for people in third world countries, such as Viet Nam who had lost their limbs in explosions that were caused by American landmines. He described the excitement and gratitude of the people when he would travel abroad to deliver the wheelchairs in person. Even though they were basic and inexpensive wheelchairs, they meant everything in the world to people who had lost their legs. Samuel wanted to know if there was any hope for him. I pointed out that I had many powerful techniques that we could use that would probably reduce his guilt, shame, and depression, and perhaps even make all of his negative feelings disappear entirely. And although it was hard to predict how long it would take, the change might even happen quickly, conceivably even in today’s session, which was our first. I explained, however, that I was reluctant to show Samuel how to use these techniques. Samuel was puzzled and asked why. I said, “It’s because I have so much respect for you. If this is depression, maybe the real problem isn’t the fact that you’re depressed, but the fact that the rest of the world is not. There is so much real suffering in the world, and you’re the one who’s responding to it with compassion and with your entire heart. And look at what your depression says about your relationship with you step-son. Your depression is your love for him. You’ve been keeping him alive, in your heart, the entire time. I am filled with admiration for you. Are you so sure you’re ready to let go of your depression now? Are you ready to say goodbye to Timmy?” This is an example of positive reframing, because I wanted him to feel a sense of pride in his symptoms and to see what they showed about him that was truly wonderful. This is the opposite of current approach of moist mental health professionals, who see depression as a form of pathology, rather than a sign of moral strength. And the paradox is that once the patient becomes proud of the symptoms, the resistance to change always disappears. In fact, Samuel did recover completely in that first session, using the Daily Mood Log along with basic techniques such as the Paradoxical Double Standard, Externalization of Voices and Acceptance Paradox. He came in one week later for his final session, when we did Relapse Prevention Training. Positive Reframing is not a formula or gimmick. You have to be able to see why the symptoms really do reflect something positive and admirable about the patient. Initially, this will be difficult for most therapists, because of our training. Over time, you will develop much greater skill and will be able to “see” things that may have been invisible to you in the past. 12. Magic Dial This is another useful tool to melt away Outcome Resistance. When you fill out the Daily Mood Log, you ask patients to circle and rate all their negative feelings, such as inferiority, guilt, anxiety, or anger, on a scale from 0% (not at all) to 100% (the worst). Typically, these ratings will be in the range of 75% to 100%. You can point out that in many cases, some negative feelings can be healthy and helpful. For example, if you’re trying to prepare for an important exam, some anxiety might motivate you to study harder. But 100% may be more than you need, and may even paralyze you. Here’s the kind of thing you can say to the patient: “If you had a Magic Dial and could adjust your feelings to the ideal levels, what would those levels be? For example, how much anxiety would be
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
17
enough to motivate you to study hard, so you do well on the exam? Right now, you estimate your anxiety at 95%. Would 50% be enough? Or 20%? What’s the optimal level of anxiety for you right now?” The patient might say 20%. Then you can both record the ideal level in the “Goal” column on the Emotions table of the Daily Mood Log. Now you have a therapy goal that won’t threaten the patient. I also reassure patients that if we are too successful, and the anxiety drops below the ideal level (in this case 20%), I will help them generate some anxiety once again so they don’t get too complacent, or too happy. This often triggers some laughter and relief. Paradoxically, once the negative feelings start to decrease as you use techniques like the Externalization of Voices and Acceptance Paradox, the feelings will frequently drop all the way to 0%. This is because the patient’s perceptions change so radically when they have a breakthrough that they no longer see any valid need for negative feelings. But of course, sometimes some healthy negative feelings will be indicated, so a drop to 0% is not always necessary or even desirable. 13. Straightforward / Paradoxical Cost-Benefit Analysis (CBA) Straightforward CBA. Ask the patient to list the advantages and disadvantages of believing a Negative Thought (“I’m such a loser”) or maintaining a Self-Defeating Belief (“I should be perfect”), feeling (like anger, guilt, inferiority or anxiety), relationship problem (such as blaming your spouse for your marital problems), or habit (such as drinking, using drugs, overeating or procrastinating) on a CBA form. In each case, you can ask the patient, "What are the advantages and disadvantages of this having this thought, belief, feeling or habit? How does it help you, and how does it hurt you?" After the patient lists all the advantages and disadvantages, ask him to balance them against each other on a 100-point scale so he can see whether the costs or benefits of that mind-set are greater. Paradoxical CBA. If the patient is motivated and easy to work with, the Straightforward CBA will usually be effective. If the patient seems unmotivated or oppositional, the Paradoxical CBA usually works better. When you do a Paradoxical CBA, you have the patient list only the advantages of a negative thought, belief, feeling, habit, or relationship problem, such as blaming your spouse or sibling for all the problems in your relationship. Now ask the patient, "Given all these advantages, why should you change?" This will make you and your patients aware of the powerful forces that keep them stuck, and will help you avoid trying to persuade reluctant patients. Instead, they will have to persuade you to work with them. 14. Externalization of Resistance This is a way of combining a powerful role-playing technique with the paradoxical Cost-Benefit Analysis (CBA). First, you and your patient can both list all the reasons to maintain the status quo and resist change in the Advantages column of a CBA, or you can simply list them on a piece of paper. Then you become the voice of the patient’s subconscious resistance and verbalize all those reasons NOT to change, using the second-person, “You.” For example, consider the college freshman from Hong Kong who was beating up on herself for doing poorly in her classes. With your help, she might be able to list many advantages of self-criticism, depression, and shame such as these: 1. My self-criticisms show that I have a good value system and that I won’t let myself off the hook. 2. They show that I love my parents and honor them. 3. The criticisms may motivate me to study harder and get caught up. 4. If I’m severely depressed and ashamed, others won’t feel the need to criticize me. 5. My self-criticisms show a high degree of integrity, since I’m facing my shortcomings instead of denying them. Together, you can probably come up with even more advantages.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
18
After explaining the procedure, you can play the role of her resistance, and verbalize all the reasons NOT to change, one at a time, using the second-person, “You.” For example, you might say, “Your depression shows how much you love your parents,” or “If you feel happy, you may lose your motivation to study,” or “If you feel happy, you’ll be settling for mediocrity,” etc. Then see if she can defeat you, speaking in the first-person, “I,” as she argues back against the resistance thoughts you are verbalizing. If she CAN defeat you, she’ll be well along the road to recovery, although other techniques will also be needed. If she cannot defeat you, she may be saying she WANTS to remain depressed. In this case you can “sit with open hands,” and ask her if there’s something else she does want help with instead. 15. Devil's Advocate Technique Let’s say you’re working with a patient who is struggling with some habit or addiction, such as drinking too much, overeating, procrastinating, or dating the wrong person. You can ask your patient to describe a situation where she feels tempted and typically gives in to the temptation. For example, she may be struggling unsuccessfully to stick with a diet, and one extremely difficult situation for her might be walking through the food court of a mall amid the smell of freshly baked cinnamon buns or chocolate chip cookies. Ask her to list the tempting thoughts and list them yourself at the same time. For example: • Gee, those cinnamon buns really smell terrific. • They just came out of the oven, and they’d taste SO GOOD. Mmm! • I really deserve one because I’ve had a tough day. • I can just eat one tiny little bite. One little bite won’t hurt. • I can have a salad later on so it won’t make any difference. • I’m not getting anywhere in my diet anyway. • I just CAN’T control myself, no matter how hard I try. • Tomorrow will be a better day for dieting. Now tell her to imagine being in a mall and smelling the sweet smell of sticky cinnamon buns. Explain that you’ll play the role of the Devil and try to tempt her. You’ll be the voice in her mind that tries to trick her into giving in. She can play the role of the strong, self-loving, voice that resists the temptation. The Devil (initially played by the therapist) will use the second person, “You,” and the resisting voice (initially the patient) will speak in the first person, “I.” When you use this technique, it’s important to use the patient’s exact words. Don’t get carried away using your tempting thoughts because they won’t carry any weight with the patient. That’s why it is so important to ask them to list the tempting thoughts that generally defeat them on the Addiction / Habit Log. You will need to write them down as well, so you’ll have them handy for the role playing. For example, let’s say the patient is struggling with overeating, and has written down the first four tempting thoughts on the bulleted list above. As the Devil, you might ask the patient to imagine smelling cinnamon buns at the mall. They you can say, "Gee, those hot, buttery cinnamon buns smell fantastic. They just came out of the oven. Go take a look. They’d taste SO GOOD, and you deserve one!"
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
19
The patient might fight back and say, "I don't need a cinnamon bun, and I'll feel terrible if I give in. I'm determined to stick with my diet, and I'm looking forward to wearing more attractive clothes. I may deserve a sticky bun, but I also deserve some dignity and self-esteem." Now, as the Devil, try to tempt her with another of her seductive thoughts, giving her another chance to fight back again. Continue until the patient has convincingly defeated all the tempting thoughts. If the patient gets stuck, and cannot effectively defeat one of the tempting thoughts, you can use rolereversals to model more effective responses. You can let her play the role of the Devil, and you can show her how to combat the tempting thoughts. Alternatively, you can become the voice of the patient’s subconscious resistance, and ask, with genuine curiosity, why the patient wants to change, giving all the benefits and rewards of continuing the habit or addiction. You can use the Devil’s Advocate Technique for patients who feel tempted by any kind of habit, such as drinking, using drugs, procrastinating, dating the wrong person, having affairs, or internet pornography. This method can be surprisingly powerful, especially if you express the tempting thoughts in a seductive and convincing manner. If patients cannot defeat the Devil, the likelihood of successful treatment may be low, so the Devil’s Advocate Technique also becomes an innovative and dynamic assessment tool. Techniques that Target Process Resistance
16. Gentle Ultimatum Let’s assume the patient wants help with his depression, and you’ve melted away any Outcome Resistance. You can use the Gentle Ultimatum to deal with the Process Resistance. First, you need to be clear in your own mind about what the patient will have to do to recover. For depression, Process Resistance revolves around the issue of doing psychotherapy homework. Using the Gentle Ultimatum, you might say something along these lines in a kindly way: “Pedro, I’m looking forward to working with you to overcome the feelings of depression and worthlessness that have been plaguing you for so many years. However, if you want me to help you, you’re going have to do daily psychotherapy homework for 15 to 30 minutes, even when you’re not in the mood or feel convinced that it couldn’t possibly help. It’s a little like going to a tennis coach to improve your tennis game. You’d have to practice between sessions to get the real benefit. And if you’re willing to do the homework, I believe I can show you how to change your life. That would be exciting to me. “However, if my suggestion does not appeal to you, and you don’t want to have to do psychotherapy homework, I can absolutely understand and accept that. But then we’ll have to move in a different direction together, since I don’t know how to defeat depression without the homework. If you want to continue working with me, perhaps we could work on some other problem instead. Or, if you want help with your depression without doing having to do psychotherapy homework, perhaps I could refer you to a respected colleague who doesn’t require psychotherapy homework. Of course, I’d hate to lose you as my patient, and I’m eager to work with you, but I do want to be clear that the homework requirement is not negotiable.” Or, let’s say the patient is anxious, but doesn’t want to have to use exposure. You could point out that most therapists in the community offer long-term talk therapy without exposure for patients struggling * Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
20
with anxiety. You could also say, “If you feel strongly that you’re looking for that approach, I feel that you have every right to pursue it—but I don’t have those kinds of skills.” You can emphasize that you have great respect for the patient and hope she or he will decide to work with you. You can also let the patient know that you feel convinced that you can do some tremendous work together (Dangling the Carrot again.) However, they should know that the exposure requirement would not be negotiable. You can also express the ultimatum in an apologetic way, like this: “Harold, I’d really like to help you with your PTSD, and I can see how much you’ve been suffering. But at the same time, recovery will require us to use a technique called Cognitive Flooding, where I would ask you to focus vividly on some of the horrible events from the past and allow yourself to feel flooded with intense anxiety, which can be tremendously uncomfortable. I’d hate to ask you to do that, but I realize that it would be absolutely necessary to defeat the horrible flashbacks that have been plaguing you. What do you think about that?” 17. Paradoxical Inquiry (PI) Paradoxical inquiry can be helpful for Outcome and Process Resistance. When the patient resists, you can ask a paradoxical question that may lead the patient to the irrationality of the resistance, rather than using persuasion in an attempt to change the patient's mind. For example, the patient who’s describing a conflict with his brother may say, “Why should I have to change? He’s the one who’s screwed up.” Using PI you might say, “Certainly, you shouldn’t have to change and you don’t have to change. Are you saying that you don’t want to?” You can also point out that he may be saying that he doesn’t really want to work on the relationship, and perhaps just wanted you to know how difficult and irritating his brother is. If so, you can then ask if there’s something else he’d prefer to work on. PI must be delivered with warmth, respect, and authenticity. Tone of voice can make a huge difference. Avoid sarcasm. Try to see the world through the patient’s eyes. Try to be okay with the fact that the patient may not want to change, or may not want to risk changing. If you’re not truly “sitting with open hands,” and your secret agenda is to persuade the patient to change, then this method will be ineffective.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
21
Overview of Positive Reframing By David D. Burns, M.D.* I would like to thank Drs. Steve Harris and Jill Levitt who have generously contributed to this document. The following table is designed to help you with Positive Reframing when you are doing Paradoxical Agenda Setting. When I was creating this table, I was imagining working with a patient who has a partially completed Daily Mood Log, so the assumption is that you are working with an individual mood problem. If you are working with a relationship problem or with a habit or addiction, the approach would probably be quite different, although some of these concepts might be somewhat useful. I would discourage you from using this table in a general or non-specific way. It is meant to facilitate treatment when someone has asked for help with a specific moment she or he felt upset. The Upsetting Event should be recorded at the top of the Daily Mood Log (DML). The patient will also need to circle and rate his or her negative feelings on emotions table, and list his or her negative thoughts (NTs) the NT column. These details are important, and therapist discipline in following the T.E.A.M. approach will be needed. If the patient says that he or she wants help with the problem on the Daily Mood Log, you can ask what kind of help he or she is looking for. If a miracle happened in today’s session, and the patient walked out feeling fantastic, what would happen? You may recognize this as the Miracle Cure Question. Hopefully, you can guide the patient to saying that the negative thoughts and feelings would disappear, and he or she would feel happy and joyful at the end of the session instead of feeling depressed, hopeless and worthless. Then you can ask the Magic Button question: “Let’s imagine there’s a magic button right here on the desk, and if you push it, all of your negative thoughts and feelings would instantly disappear, with no effort at all, and you’d be feeling happy and joyous. Would you push it?” Usually, the patient will say yes. Then you can say something along these lines: “Well, there is no magic button, of course, but I do have some tremendous tools we can use to reduce the negative thoughts and feelings, and they may, in fact, disappear completely. But I’m reluctant to do that just now, because we might lose something very valuable. Before we jump in and try to change things, why don’t we make a list of the advantages, or benefits, of your negative thoughts and feelings? We can also include what these negative thoughts and feelings show about you that’s positive and awesome. We can list them on a piece of paper. Does anything spring to mind?” Usually, the patient will be surprised and unable to come up with anything at first. Then I typically prime the pump by offering a couple things that the patient can buy into. For example, I might say, “Well, I can see that many of your negative thoughts are self-critical, and I’m thinking that shows that you have high standards and don’t want to settle for screwing up or falling short of your goals. Does that make sense?” Most of the time, the patient will agree, assuming your statement does ring true and isn’t just something you’ve made up that isn’t reflected in the patients’ actual negative thoughts and feelings. When the patient agrees, you can both put “high standards” as #1 on your list. Then I typically say, “And I’ll bet those high standards have often motivated you to work hard and to do your best. Is that also true?” If the patient agrees, you both add that to your list. Now the patient is in a kind of “yes” mode, and is starting to see some of the benefits and positives that are inherent in his or her suffering. The following table is intended to help you learn how to do this, since it can sometimes be very difficult for therapists to see the positives in the patient’s suffering. That’s because we’ve been trained to see the suffering as a
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
22
“problem” or “disorder” or “defect” we are trying to correct—with pills, psychotherapy, and so forth. This is just the opposite. In most cases, I’ve been able to come up with a convincing list of ten to fifteen positives that are implied by the negative thoughts and feelings on the DML. It is important that they are valid and compelling, and implied by the actual thoughts and feelings. We are not looking for general compliments or vague positives, as this will nearly always turn the patient off. That’s one reason why this technique (and every technique) can be so challenging and somewhat hard to learn. For example, in one of my trauma workshops, during a live demonstration with a participant who’d endured a number of horrific traumas, I asked the audience to participate in the Positive Reframing portion of the session. One of the audience members raised his arm and said, “This shows that you’re resilient and you’re a survivor!” This statement reflects some of the buzzwords that are currently circulating among folks who specialize in the treatment of trauma patients, but it turned the patient off, and rightly so. That’s because there was nothing on her DML that suggested she was resilient or a survivor. This approach has to be individualized, and it has to ring true. It is therapy, and not cheerleading or psychoeducation. Cheap formulas will not be effective. And that is my fear and concern about this list—that therapists may rely on it too much, rather than individualizing the intervention for the specific patient and problem that you’re dealing with. Once you’ve finished, and you have your list of positives, you can use the Magic Dial, and say something along these lines: “Now, as you can see, it might not be such a good idea to press that Magic Button and make all the negative thoughts and feelings disappear, because they are revealing so many positive things about you. In fact, as you can see, your suffering is the expression of some of the most beautiful and awesome things about you, your core values, in fact. So instead of making everything disappear, maybe we could imagine, instead, that we had a Magic Dial, and could reduce your negative feelings to some lower and more appropriate level. For example, I can see that you’ve rated your sadness and depression at 100%, and certainly some sadness is appropriate, given the fact that you’ve lost your brother (or whatever the upsetting event happens to be.) What would be an ideal level, if you could lower it to any number between 0% and 100%? How sad and depressed would you want to feel?” Typically, the patient will say something like 20%. Then you can ask him or her to put 20% in the goal column of the DML. You can do this with each category of negative feelings on the DML. You do NOT need to do this with the negative thoughts, only the feelings. Then you can say something along these lines, “Okay, let’s go ahead and reduce the feelings to these numbers. Keep in mind that the methods we’re going to use now are quite powerful, and in some cases we might overshoot. For example, you want to lower your shame to 30%, but it could go all the way to 10%, or even to 0%. But don’t worry, if the shame gets too low before the end of the session, I can help you work it back up to 30%. I wouldn’t want you to end up getting too shame-free.” That’s David’s way of doing it—your way will be different, and has to reflect your personality. But the idea is that we’ve kind of made a deal with the patient’s conscious and subconscious resistance. We’re allowing the patient to cling to some of the negative feelings, and we’ve put the patient in control of the outcome of the therapy. As the session evolves, the patient’s goals nearly always change, and they usually end up reducing most or all of the negative feelings to zero, or nearly zero. The following table only focuses on negative feelings and urges for habits and addictions. However, you can apply the same approach to Negative Thoughts, and I have a separate table (Part 2) that lists examples of this. I’m not including that here to keep it reasonable simple.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
23
Positive Reframing Ideas Feeling / Urge
Advantages What are some benefits of feeling this way? How will this type of feeling help you?
Positive Values What do these kinds of feelings show about you that is awesome and beautiful?
Sad, down, depressed, unhappy
These feelings 1. Often show that you are realistically looking at a problem or loss which has been difficult and painful for you. 2. May make you more compassionate and capable of embracing the pain of others who are suffering.
Sadness is appropriate if you’ve experienced a loss or a rejection or a failure, or simply if things haven’t been going very well for you. These feelings probably reflect your intense love of life, including your love of someone or something you have lost. The feelings may also show that you are willing to wrestle with the pain rather than running from it and living in denial.
Anxious, nervous, worried, panicky, afraid, scared
The anxiety can 1. Keep you vigilant. 2. Protect you from danger. 3. Prevent you from getting complacent and letting your guard down. 4. Motivate you to do really great work.
These feelings may show that you 1. Care deeply about being on top of things, doing a great job 2. Want to protect yourself and others from harm 3. Care greatly about what others think of you.
Guilty, bad, ashamed
These feelings remind you that you might not have been living up to your core values. For example, you may have said or done something that hurt someone during a moment of anger or frustration. The feelings can also motivate you to examine and modify your behavior and make a commitment to doing things differently next time.
These feelings often show that you 1. Have high standards and a strong moral code. 2. Hold yourself accountable instead of blaming others for your problems. 3. Are honest and willing to face your shortcomings as opposed to denying them. 4. Care about the impact of your behavior on others, and that you don’t want to hurt people. 5. Don’t want to let others down or let Are humble and have strong spiritual values.
Inferior, defective, worthless, inadequate
These feelings motivate you to examine your flaws and shortcomings, rather than denying them or settling for second best.
These feelings show that 1. You are honest and realistic, since you do, in fact, have many flaws and shortcomings. 2. You are not arrogant or overly high on yourself.
Lonely, alone, rejected, abandoned
These feelings can motivate you to reach out to others, rather than giving up on people or drifting into bitterness and cynicism.
These feelings show that you 1. Care deeply about people and value loving relationships. 2. Desire deeper and more meaningful relationships with others.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
24
These feelings could also motivate you to make personal changes (for example, losing weight or improving your flirting or communication skills) that would make you more appealing to others. Humiliated, self-conscious, embarrassed
These feelings may protect you from doing something foolish and risking disapproval from people you care about. And if you feel that you have done something foolish, these feelings may prompt you to examine and modify your behavior. These feelings may protect you from getting your hopes up and risking further hurt and disappointment. These feelings could also let you know when it is time to surrender and accept defeat graciously, so you can focus your energy on some future project. There’s no rule that says we have to succeed at everything or persist endlessly when we are stuck.
These feelings show that you 1. Value the opinions of others and want their respect. 2. Are willing to admit and examine your flaws.
Frustrated, stuck, thwarted
These feelings might motivate you to keep trying so you don’t give up. These feelings could motivate you to step back, take a break and re-evaluate a situation that isn’t going well. These feelings may give you permission to give up or leave an unhappy, unrewarding situation.
Angry, resentful, upset, hurt, enraged, furious
Sometimes, anger (at others or at yourself) can be healthy and appropriate, and can alert you that something is not right, or that you are being taken advantage of. These feelings might motivate you to take action and stick up for yourself. Anger can empower you when others are breaking the rules, trying to knock you down or hurt or exploit you.
When events or people fall short of your hopes and expectations, or when your best efforts keep falling short, frustration can be appropriate. These feelings often show that you 1. Are being honest and facing up to the negatives in your life, rather than being a Pollyanna who always looks on the bright side. 2. Have high standards and want to do quality work or experience greater success in whatever you feel stuck in. 3. Want to have a more fulfilling relationship with someone. These feelings often show that you 1. Are aware of the dark side to human nature, and that you are not in a state of denial about others’ thoughts or actions. 2. Have high standards about the way that others treat you or treat those who you care about. You can feel proud of these high standards. 3. Value fairness, kindness, honesty, integrity, or some other value that the other person has violated. 4. Really care about the other person, rather than being
Hopeless, discouraged, pessimistic, defeated
These feelings show that you: 1. Are honest and realistic, since you may have had a series of failures or disappointments, no matter how hard you tried. 2. Are intelligent and skeptical, and that you question and challenge things.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Paradoxical Agenda Setting
Urges to give in to habits and addictions, such as overeating, procrastinating, or misuse of drugs or alcohol
The habit or addiction can be very rewarding, and may in fact be your only true source of pleasure or fun. The reward will be immediate, and possibly intense. Giving in to the habit or addiction may comfort you when you are bored or upset. Some habits, such as alcohol, may increase your ability to connect with others who also drink. You may be more creative when you’re high. You can avoid negative feelings. Even the Dali Lama recently said that the purpose of life is Happiness. So you could think of your habit or addiction as a kind of spiritual commitment.
25 indifferent to the way they are behaving or treating you. The habit or addiction may show that you are a free spirit, and won’t let yourself be controlled by the overly stuffy norms of society, or by someone who is busting you and telling you to change. If the habit or addiction helps you connect with others, this shows that you care about others and want to feel close to them.
* Copyright © 2016 by David D. Burns, MD. Do not copy or distribute without written permission.
Tips on Paradoxical Agenda Setting By David D. Burns, M.D.*
Sitting with Open Hands. None of the methods I refer to as “Paradoxical Agenda Setting” will work if you have the “need” to help or motivate the patient, or if you feel the “need” to be a successful therapist. I like the image of the Buddha who sits with open hands. My own personal spin on this is that the open hands mean, “I can receive you, and show you the path to enlightenment, if you’re interested, but I can also let you go if you’re not interested in what I’m offering. My personal contentment and sense of selfesteem do not depend on you.” This means genuinely letting go of the patient, and not pushing your own agenda, if the patient resists or isn’t ready to change. Some patients are not especially motivated to be in therapy, perhaps because someone has coerced them into coming, or perhaps they are coming out of a sense of guilt or obligation. Other patients may want therapy, but only in a passive mode. They may want to talk about their problems and receive support endlessly, but they aren’t ready or willing to pick up the tools to solve these problems. I’m not eager to work with patients who are unwilling to do the work. In fact, I believe that allowing a person to complain endlessly will simply reinforce this tendency, and will actually program the brain to continue in that mode. Repeated complaining actually programs the neural circuits to do just that. I offer an active and collaborative type of therapy that focuses on learning, change and growth. I am happy to work with patients who are initially ambivalent about change if they are willing to explore their resistance and take the risks required to change their lives. If the patient is not looking for the skills that I can offer, then I can let him or her go. I don’t need to chase a reluctant patient, and I don’t need to persuade any patient to work with me. That’s the essence of Sitting with Open Hands. Paradoxically, this mindset often seems to have the opposite effect of motivating patients to want to work with me, and to be willing to work hard for recovery. But the mindset of letting go can’t be a gimmick or manipulation. You genuinely have to be willing to let go. What does this mean from a practical perspective? Well, let’s say the patient has a diagnosis of OCD. I don’t feel any duty or obligation to treat that patient’s OCD. She or he may want to have OCD. For example, hoarders may be committed to hoarding. Patients who wash their hands 100 times a day to prevent contamination may feel they are doing a good thing. Even though my perceptions may be different, I can accept the patient’s reluctance to change. What I want to know is if they do have a problem they do want help with. It can be hard to sit with open hands when you feel that you can “see” the solution to the patient’s problem(s). For example, patients will often describe conflicts with people, such as a friend, colleague, or spouse. They often describe the person they are not getting along with as a hopeless jerk, or some such term. But when the patient describes his or her interactions with the other person, you may see how the patient is actually triggering the negative behavior in the person she or he is complaining about. You may also feel convinced that changes in the patient’s attitudes and ways of interacting with the other person will probably produce dramatic and almost instantaneous changes in the troubled relationship. And yet, the patient may not be interested in what you have to offer, because she or he is not willing to let go of the problem. The conflict may be intensely rewarding to the patient. The patient *
Copyright © 2009 by David D. Burns, M.D. Revised 2011.
Paradoxical Agenda Setting Tips
Page 2
may only want you to know what a loser the other person is, but may not be at all interested in trying to bring about some changes. That’s why skillful Paradoxical Agenda Setting (PAS) skills can be challenging—and almost impossible—for many therapists to learn. We just don’t want to let go of our own agendas. We want to feel like “experts” and we want to be in control of the therapeutic relationship. There are other reasons why PAS is challenging as well. For example, you can examine your own negative thoughts that may cause feelings of panic or guilt at the thought of a patient dropping out of therapy, or not wanting to work with you. Ask yourself why this is upsetting to you, and what you’re telling yourself. You may be telling yourself that you’re a young and inexperienced therapist, and that if the patient drops out of therapy, it really will mean that you’re no good, or that you’ve failed. These kinds of thoughts link your self-esteem to the patient’s emotions and behaviors in a highly co-dependent, narcissistic way, and set yourself up for feelings of anxiety, shame, frustration, and failure. In addition, your need to help can give certain kinds of patients tremendous power over you, because they can continue to fail and it becomes your fault. The patient insists that you don’t understand and you’re not helping. You end up doing all the work while the patient does all the complaining. Your fear of failure may cause you to fail because you’re not making the patient accountable. The Magic Button. The concept of the “Magic Button” helps you with Outcome Resistance, and it works like this. You can say something along these lines to the patient: “Imagine there’s a Magic Button right here on the desk. If you push it, you’ll be instantly cured, with no effort at all, and you’ll walk out of today’s session in a state of joy, with no more depression or anxiety. Will you push that button?” The patient will usually say “Yes.” Now you can become the voice of the patient’s subconscious resistance, and verbalize all the reasons NOT to push the Magic Button. You might say something like this: “That’s great, John, but I want to be clear about something before you decide to push the button. You’ve told me that you feel severely depressed and worthless because you’ve been procrastinating and skipping classes, and not studying or doing your homework for school. As a result, you’re making C’s and B’s. But you expected to make straight A’s, and your parents expect this as well because you were a super-star in high school. “If you press the button, your depression will vanish, and you’ll walk out of today’s session feeling incredible joy and self-esteem. That probably sounds good. But it won’t change the fact that you’ve been sloughing off and getting poor grades. You see, I can probably show you how to change the way you feel today, but I can’t change the facts of your life, at least not today. The Magic Button doesn’t work like that. It only changes how you feel, and how you think about yourself and your life. “So, you’d have to agree to feel joy and self-esteem in spite of the fact that you’re not doing very well in your school work. Would you be willing to do that if I could show you how? Wouldn’t that mean you’d be settling for second-best?” This type of dialogue usually highlights the patient’s resistance and goes to the core of the problem. This patient may have value system that states, “My worth as a human being depends on my achievements. If I perform at a very high level, then I can feel happy and worthwhile, and I’ll be lovable.” But since his achievements are poor right now, he feels like he deserves to suffer. He may also believe that if he suffers enough, eventually he’ll become a super-star and get straight-A’s.
Paradoxical Agenda Setting Tips
Page 3
In my experience, it rarely works this way. Depression is the world’s greatest enemy of productivity. Depression saps your motivation and usually triggers more procrastination and failure. The patient may think that you can make him a highly motivated, straight-A student. Once you’ve done that, THEN he’ll agree to feel happy. But I’m not offering that type of solution. Instead, I reassure the patient along these lines: 1. I like you and want to work with you. 2. I have powerful tools to help you, and I’m convinced that if we work together, we will be successful. 3. If you’ll agree to overcome your depression NOW, while you’re still struggling and doing poorly in school, then I can help you boost your productivity and performance, if that’s what you’d like to do. 4. But you’ll have to agree to overcome your depression first. The Magic Dial. The concept of the “Magic Dial” can also help you overcome Outcome Resistance. It works like this. Sometimes I help the patient fill out the first few steps of the Daily Mood Log during the Empathy and Agenda Setting steps, even though we haven’t yet gotten to the Methods phase of the therapy. This helps me pinpoint exactly how the patient is thinking and feeling about some specific Upsetting Event, and I can negotiate the Outcome Resistance using the “Magic Dial.” For example, during a recent Intensive Workshop in Vancouver, I encouraged the participants to fill out their own Daily Mood Logs to get some personal experience with these methods. The Upsetting Event for one of the participants was simply “Attending the workshop.” In the emotions table, she indicated that she was feeling 100% guilty and ashamed, among other feelings as well, such as sadness. She recorded this Negative Thought, “I’m a bad mother,” which she believed 100%. It turned out that her toddler son was ill, and her husband was taking care of him while she attended the workshop. Although her son was doing fine, she felt she was abandoning him and being a selfish, bad mother by coming to the Intensive. At the same time, she was conflicted because she’d been looking forward to the Intensive for six months and said she was thrilled to be there. I pointed out that the guilt and shame she felt showed what a loving and unselfish mother she was, and that some sadness and guilt might be appropriate, because these feelings reflected her intense love for her son. I also pointed out that 100% guilt and shame might be more appropriate for a serial killer, as this was the worst guilt and shame a human being can experience. Would there be some lower level of guilt or shame that might be acceptable to her? She “got it” right away and said that maybe 20% guilt and shame would be sufficient. Then I said, “Well, then, why don’t we talk back to your negative thoughts, with the idea that we’ll lower the guilt and shame to 20%, but no lower than that? Would that make sense to you?” She was enthusiastic about this suggestion, and was easily able to talk back to her negative thoughts using the Double Standard Technique, followed by the Externalization of Voices. As a result, her belief that she was a bad, selfish, mother dropped to 0%. Paradoxically, her guilt and shame went down all the way to 0% as well, and she said that she gave herself permission to enjoy the workshop intensely. This frequently happens. Once the patient agrees to reduce the negative feelings to some reasonable level using the “Magic Dial,” they often find they can often push the feelings all the way to zero. I also used the “Magic Dial” concept with a Clinical Psychologist I treated for paralyzing test anxiety who was trying to preparing for her licensure examination. Initially, she resisted treatment because of her belief that the anxiety would help her study and perform well on the exam. But she had to admit that
Paradoxical Agenda Setting Tips
Page 4
she was so anxious, she hadn’t studied for one minute in the previous month. I asked her how much anxiety, between 0% and 100%, would be optimal, so as to motivate her to study and to perform optimally on the examination. She thought that 10 to 15% would be plenty. This opened the door to collaboration. Within a few weeks, her anxiety disappeared completely and she was studying and concentrating extremely well. She passed her exam with flying colors. The following tables highlight the most common sources of Outcome Resistance for depression, anxiety disorders, relationship problems, and habits and addictions. When you review these tables, you will begin to see why patients might want to cling to their symptoms. You will need that understanding when you are dealing with Outcome Resistance. Once you’ve reviewed these tables, I’ll give you some examples of the kinds of things you can say to patients when you’re dealing with Outcome and Process Resistance. Common Sources of Outcome Resistance* Depression
Symptom
Reasons to Maintain this Type of Symptom
Worthlessness / Defectiveness / Inferiority
These feelings may be reinforced by a sense of realism and integrity. The person who feels worthless, defective, or inferior is taking a harsh look at himself or herself and highlighting the fact the there are many flaws, shortcomings, and failures. The patient may be thinking: I really am inferior. In fact, others have achieved far more than I have. I've never done anything special, nor have I achieved my goals and dreams for my life. I really am defective. I have many shortcomings, and defects. I really am worthless. I’ve had many failures, and that means that I am a failure.
Relentless selfcriticism, selfblame, perfectionism
The patient’s relentless self-criticisms and perfectionistic standards may motivate the patient to work hard and to be productive. In addition, if the patient has excessively high standards, it shows that she or he is, in a sense, superior. After all, only an extraordinarily gifted person could be expected to be perfect. The patient may have these kinds of thoughts: Although the self-criticism makes me miserable, it’s the price I have to pay to succeed and achieve my goals. My perfectionism shows that I'm one cut above other people. I wouldn't expect other people to be perfect, but I do expect superb performance from myself because I’m a superior kind of person. If I allowed myself to feel happy right now, when I’m struggling in my career (or in school, etc.), that would mean I was settling for second best.
Feelings of guilt, shame
This negative thinking style may be reinforced by a sense of taking the moral high ground. The intense feelings of guilt and shame show that the patient is punishing himself or herself for some real or imagined wrongdoing. So by suffering, you purify yourself. The patient may be thinking: I deserve to feel bad, because I am bad (or because I've done bad things, or because I've failed, or because I hurt someone I loved). The feelings of guilt and shame show that I am a moral person with good values. If I beat up on myself, others won't have to criticize me. *
Copyright © 2009 by David D. Burns, M.D. Revised 2011.
Paradoxical Agenda Setting Tips
Page 5
Depression (cont’d)*
Hopelessness
The feelings of hopelessness may protect the patient from further disappointment and may be reinforced by a sense of realism. In addition, feelings of hopelessness can be a good weapon against intrusive friends, family members, and therapist who try to “help” without really empathizing. The patient may be thinking: If I insist that I’m hopeless, I won't get my hopes up and then get disappointed if the therapy doesn't work, or if my life doesn't improve. My hopelessness is based on the facts. After all, antidepressants haven’t helped and psychotherapy hasn’t helped. I've been depressed for years, and I’m still unhappy. The hopelessness allows me to defeat all the annoying people in my life who give me advice and try to reassure me instead of listening. The hopelessness protects me from having to try and work hard to solve my problems.
Sadness, despair
Sadness can be healthy when it’s not triggered by distorted thoughts. But the patient may have trouble distinguishing healthy sadness from depression, and may be thinking: It's appropriate to feel sad and upset in this situation. I don't deserve to be happy because I'm only getting B's, rather than A's, in school, or because I'm lazy, etc. It wouldn't be possible for someone like me to feel happy because I'm alone, or unloved, or divorced, or because I’ve been rejected by someone I loved, or because I’ve failed.
Anger, resentment, bitterness, and self-pity
Some patients oscillate between Self-Blame (“I’m no good”) and Other-Blame (“You’re no good.) The anger and cynicism may protect the patient from feeling sad, hurt, or inadequate, and may make the patient feel more empowered. In addition, self-pity can be enormously addictive. The patient may be thinking: The world is screwed up, and people really are no good, so I have every right to feel the way I do. I'm just facing the truth. If I put up a wall, I won't have to get close to you and risk being hurt. Anxiety Disorders
Type of Anxiety
Reasons to Maintain this Symptom
Generalized Anxiety
If I stop worrying about my family (or my grades, or health, or finances, etc.), something terrible may happen. My family may die, or I may not get into medical school (etc)
Shyness / Social Anxiety
If I stop worrying, I may say something inappropriate and really make a fool of myself. If I stop trying to cover up my nervousness, people will see how shy and insecure I am and look down on me.
Performance / Test Anxiety
If I stop worrying, I'll become complacent and screw things up. I won’t study enough, and I’ll blow the final exam.
*
Copyright © 2009 by David D. Burns, M.D. Revised 2011.
Paradoxical Agenda Setting Tips
Page 6
Anxiety Disorders (cont’d)*
Phobias
OCD
PTSD
Panic Attacks
All forms of anxiety
If I stop worrying about flying, I’ll start flying and the plane may crash.
If I stop worrying about contamination, and stop washing my hands 50 times a day, I will get contaminated and my children may die of leukemia. If I stop checking the stove, the house may burn down. If I stop avoiding sharp objects, I may suddenly fly out of control and kill my mother. I’m not a hoarder. I just like to collect things!
My hypervigilance will protect me from some horrible thing happening again. My anger and rage show that I won’t put up with what happened to me. It was outrageous and unfair, and I have every right to be angry.
If I stop worrying, I may really lose control and go insane. Or I may actually pass out or have a heart attack or stroke and die.
The great majority of anxious individuals are exceptionally “nice” people who are anger phobic and conflict phobic. When something happens that they find annoying or upsetting, they often sweep their negative feelings under the rug, and act exceptionally “nice.” Then the suppressed feelings come out indirectly, as panic, a phobia, or worrying, or the compulsion to wash your hands repeatedly to ward off the sense of “danger.” Then, the patient becomes so preoccupied by the anxiety symptoms that she or he completely loses track of the hidden conflict that actually triggered the anxiety in the first place. So the anxiety becomes a way of avoiding real-life problems and negative feelings. Anger / Interpersonal Problems
Reasons to Maintain this Symptom
Relationship Conflict
I don't really want to get close to X, because X is: A jerk A loser Totally self-centered To blame for the problems in our relationship Wrong Impossible to get along with
Anger / Resentment
*
I have every right to be angry at X. I shouldn't have to treat him (or her) with respect. He (or she) doesn't deserve any warmth or respect.
Copyright © 2009 by David D. Burns, M.D. Revised 2011.
Paradoxical Agenda Setting Tips
Page 7
Anger / Interpersonal Problems (cont’d)*
Blame
X really is to blame for the problems in our relationship. So why should I have to change? The blame gives me feelings of moral superiority. If I blame X, I won't have to feel guilty. If I blame X, I wont' have to change. If I blame X, I can gossip about X and get other people to side with me. If I blame X, I can be angry and get back at X. If I blame X, I can play the role of martyr or victim and feel sorry for myself.
Revenge
X deserves punishment because of everything she (or he) has done to me.
I've tried everything and nothing will work. X is a hopeless case. He (or she) will never change, so there’s no point in trying.
Interpersonal Hopelessness
Habits and Addictions Reasons to Maintain this Symptom “Drinking is the most rewarding thing in the world for me. I feel the greatest joy and happiness when I’m high. Why should I have to give this up? “Life would be drab and boring without getting high, and without looking forward to having that first cold, delicious beer when I get home from work. I deserve it, and it’s not really a problem!”
Alcohol / Drug Abuse
“I can see, on some level, that it would be great to get all caught up on things, and to have my life under complete control. And certainly, that's something I can work on at some point. But at the same time, there are lots of things I really love doing when I procrastinate, such as watching a great baseball game on TV. “And sometimes, I have other more important things to do. And even though my wife bitches Procrastination and moans about how cluttered my desk is, in reality nothing terrible seems to happen just because my desk is a mess. So it's not entirely clear why I should have to put a major effort into getting caught up on things. “I’d have to give up all kinds of activities that I really love, and I’d have to do things that make me anxious and unhappy, such as filing and trying to figure out where everything goes. I’d also have to give in to my wife's nagging. I shouldn’t have to do that!” Overeating
“Eating is fun! Dieting and Exercising suck!”
On the next two pages I’ll give you some tips on how to deal with Outcome and Process Resistance. You might want to print those pages (using two sided printing) on glossy card stock so you can refer to it when you’re working with challenging, resistant patients.
*
Copyright © 2009 by David D. Burns, M.D. Revised 2011.
Paradoxical Agenda Setting Tips
Page 8
How to Deal with Outcome Resistance* Below you’ll find examples of the kinds of things you might say when you’re working with Outcome Resistance. You can start with this type of statement: “Imagine that there’s a Magic Button on the desk. If you push it, you'll be instantly cured, with no effort on your part, and you'll walk out of today's session feeling tremendous joy and self-esteem (or without any more anxiety, anger, etc.) Will you push that button?” Most patients will say yes. Now you can add a statement like the ones in the table, depending on the type of problem the patient is struggling with. Problem
Issue
What to Say
Depression
SelfBlame
“Before you decide to push that button, let’s think about some of the reasons why you might NOT want to push it. I can think of lots of good reasons to feel depressed, (or worthless, or hopeless, etc.) For example, X, Y, and Z. Are you sure you want to press that Magic Button?”
Safety
“Are you concerned that something terrible might happen if you pushed that Magic Button and your anxiety suddenly and completely disappeared? For example, if you stopped worrying constantly about your children whenever they're away from you at school, or parties, aren't you worried that they might actually get into a horrible accident, or get kidnapped, or whatever? Isn't worrying part of what a loving mother does to protect her children? After all, this is a dangerous world that we live in, and bad things can happen if you're not vigilant.”
Relationship Problem / Anger
OtherBlame
“Do you really want to develop a more loving (or rewarding) relationship with X, given how unreasonable and irritating he (or she) is, or did you mostly just want me to know how annoying and difficult that he (or she) is?”
Habits and Addiction
Pleasure / Denial
Anxiety
*
“Are you sure you really want to give up (overeating, drinking, procrastination, etc.), given the fact that it's so incredibly rewarding to you? I'm not convinced that you should have to do that. Why should you?”
Copyright © 2009 by David D. Burns, M.D. Revised 2011.
Paradoxical Agenda Setting Tips
Page 9
How to Deal with Process Resistance* Once you’ve melted away the Outcome Resistance, and the patient seems clearly motivated to work with you, you can deal with Process Resistance. The second column in the table below highlights the key Process Resistance issue for depression, anxiety, relationship problems, and habits and addictions. When you’re addressing Process Resistance, you can start with this type of statement: “Sadly, there is no Magic Button. We'll have to do some work to achieve your goals. But the prognosis is positive, and I have many powerful tools we can use to help you overcome your depression (or anxiety, etc.)” Now you can add a statement like the ones in the table, depending on the type of problem the patient is struggling with. Problem
Issue
What to Say
Depression
Psychotherapy homework
“If I agreed to help you with your depression, would you be willing to do psychotherapy homework every day, whether or not you feel like it, and whether or not you believe it could help you?”
Anxiety
Facing your fears
“If I agreed to help you with your anxiety, would you be willing to confront your fears, using Exposure Techniques, even though this will make you feel intensely anxious at first?”
“If I agreed to help you with the problems in your relationship with X, would you be willing to give up blaming X and pinpoint your own role in the problem, and focus entirely on changing yourself instead of trying Accepting Relationship responsibility to change X?“ Problem / and changing Or, "What would it be worth to you if I could show you how to develop a Anger yourself more loving (or satisfying) relationship with X? How hard would you be willing to work? Would you be willing to experience some shame or discomfort to bring that result about?" Habits and Addiction
Giving up pleasure and facing discomfort
*
“If I agreed to help you with this problem, would you be willing to experience substantial deprivation and discomfort in order to achieve your goal of (abstinence, or weight loss, or overcoming procrastination, etc.)?”
Copyright © 2009 by David D. Burns, M.D. Revised 2011.
Agenda Setting—What to Say at Each Step* By David D. Burns, M.D. At the start of each therapy session, it’s important to empathize, using the Five Secrets of Effective Communication. When you empathize, don’t try to help the patient or to give advice. Instead, paraphrase the patient’s words (Thought Empathy), acknowledge his or her feelings (Feeling Empathy), find the truth in the statements (Disarming Technique), and gently probe for more information (Inquiry). Stroking and “I Feel” statements can be very helpful as well. Skillful empathy requires discipline and training. Most therapists wrongly believe they are empathic and have good listening skills. The use of the Empathy Scale at the end of sessions will show how your patient actually experiences you. Most therapists will get failing grades initially from most patients most of the time. With practice, your scores will improve significantly. Some patients will require just a few minutes of skillful listening. Others will need more time. At some point, when the patient feels supported and relaxed, and the emotions have been expressed and acknowledged, you can initiate the five steps of Agenda Setting, which include: •
The Invitation Step
•
Specificity
•
Conceptualization
•
Motivation
•
Methods
Here are some examples of the kinds of things you can say at each step. These words are not to be memorized or taken as gospel. Just some suggestions to help you find the words that will work for you. Invitation Step •
"You’ve mentioned problem X, and how painful that has been for you. Is that something you'd like to work on today?"
•
"Is there something you'd like my help with in today’s session?" or "Is there something you'd like to work on today?"
•
"You've mentioned a lot of important issues today. Is there one problem in particular that you'd like some help with during today’s session?"
•
“In the last fifteen minutes, you’ve shared many painful feelings, and my heart goes out to you. You’ve mentioned problems X, Y and Z, and how overwhelmed, angry, and discouraged you feel. I’d like to offer you something more than just listening and support, so we could work together to solve these problems and turn your life around. I’m convinced that’s possible, * Copyright © 2009 by David D. Burns, M.D.
What to Say
Page 2
and I’m wondering if this would be a good time for us to roll up our sleeves and get started. On the other hand, talking and sharing your feelings is vitally important. I don’t want to jump in prematurely, before you’re ready, and I don’t want to cut that process short. Can you tell me how you’re feeling right now? Would you like to focus on one of the problems you’ve described, or do you feel you need more time to talk and receive my support?” Specificity Step If the patient ignores your Invitation, or doesn’t feel ready to focus on something specific, you can empathize for a while longer, and then repeat the Invitation step. If she or he wants help, there are two levels of Specificity you can ask about. First, you can ask what problem she or he wants help with, with a simple question like this: •
“Ramesh, I’m glad you feel ready to work on something together. You mentioned lots of problems that seem important, and any of them would work well, I think. What problem would you like to work on first?”
He might want help with depression, low self-esteem, procrastination, or a marital conflict. It could be anything, including something vague, such as “I think I need help getting my life together.” Once he’s described the problem he wants help with, you can ask him to describe one specific moment when he was struggling with that problem. Make sure it’s a moment he wants help with. This is important because patients with relationship problems often describe examples of how the other person was acting like a jerk. The patient’s goal may not be to get help, but rather to get you to buy into the idea that that he or she is an innocent victim of someone else’s bad behavior. Let’s say that Ramesh tells you that he wants help with his “low self-esteem.” To focus in on an example of this problem, you might say something along these lines: •
“Ramesh, I’m glad you want help with low self-esteem because I would enjoy helping you with that. Although it’s incredibly painful to have low self-esteem, there are lots of tools we can use to help you boost your self-esteem and feel greater joy in life. But I need a bit of help from you. I’m wondering if you can describe a specific moment when you were struggling with low self-esteem. That way, I’ll have a better idea of how to help you. For example, you might be experiencing low self-esteem right now, sitting here in my office, or you might have been feeling bad about something that happened yesterday, or at any time in your life.”
Once Ramesh describes a specific moment when he was upset, you can ask him where he was, what time of day was it, and who he was interacting with. What did they say to him, and what did he say next? What was he thinking at that moment, and what was he feeling? You can use your empathy skills again (the
What to Say
Page 3
Five Secrets of Effective Communication). For example, you can summarize his statements and acknowledge how he was probably feeling (Thought and Feeling Empathy). You can find truth in what he’s saying (the Disarming Technique) and ask for more information (Inquiry). If your patient describes an individual mood problem, and the feelings have to do with depression and anxiety, you can pull out two Daily Mood Logs so and your patient can fill it out together. First, ask him to briefly describe the Upsetting Event at the top. Then ask him to circle his negative feelings and rate how strong each category is, on a scale from 0% to 100%, in the “% Now” column. Once you’ve recorded all the feelings, you can ask him to record his Negative Thoughts and indicate how strongly he believes each one, on a scale from 0% to 100%, in the “% Now” column. Your patient will need help with this process, as experience helps greatly. Make sure you fill out the DML at the same time. Your own copy of the DML allows you to review your work at the next session and you can remember exactly what the two of you talked about. Everything will be crystal clear. Relying on your therapy notes or memory will not work very well, because by the time the next session rolls around, everything becomes a blur. If the problem is a Relationship Problem, involving a conflict with another person, you would fill out the first two steps of the Relationship Journal instead of using the Daily Mood Log. Often, both sets of tools will be useful, since the problem may have individual and interpersonal components. We are not yet at the Methods stage, and you might think we are jumping the gun and using the DML or Relationship Journal prematurely. At this stage, we are simply collecting information, and the DML and Relationship Journal can be useful tools in this process. We will come back to them later on, when the patient is ready to start challenging the Negative Thoughts or learning to communicate more effectively. During the Specificity Step, it can also be helpful to ask questions along these lines: “Ramesh, let’s assume for the moment that you and I successfully solved this problem. What would the solution look like? What would change? How would things be different?” This question can be tremendously useful. For one thing, you will sometimes see why the patient is stuck, because the type of solution he or she is looking for may be extremely unrealistic or self-defeating. For example, someone who is overly submissive may think that the solution to a relationship problem involves the opposite of submissiveness, such as becoming more aggressive, demanding, or argumentative. These strategies are almost certain to stir up hostility, rather than intimacy, collaboration, or respect. Or, the person who is procrastinating may think the solution will involve developing great motivation before tackling the task he or she has been putting off. Of, a patient who is depressed may think the solution involves months or
What to Say
Page 4
even years of venting about all the problems in his or her life without having to do any psychotherapy homework between sessions. Conceptualization Step You can do this step on your own, in your head, or in collaboration with your patient. When I asked Ramesh for a specific moment he was experiencing low self-esteem, he described a conflict with his boss the previous day. He’d met with her to review his performance evaluation. She said that she’s received numerous complaints about his work from his colleagues. They said that he was defensive and hard to get along with, and that he wasn’t a good team member. Ramesh got defensive and insisted that his colleagues were jealous of him because he was from India, had dark skin, and was smarter than everyone else. At this point, his boss threatened to fire him if he didn’t shape up, and he walked out of the meeting feeling worthless. Ramesh had asked for help with his “low self-esteem.” Now that we have something specific, how would you conceptualize this problem? Here are some choices: 1. An individual mood problem, such as depression or anxiety 2. A relationship problem 3. A habit or addiction 4. A non-problem, such as uncomplicated grief Think about it for a moment before reading on, and put one or more checks () in the right hand column to indicate how you’ve conceptualized this problem. Most therapists say that Ramesh has a relationship problem, and that’s definitely true. Ramesh isn’t getting along with his boss or colleagues at work. But he’s also severely depressed and intensely anxious about losing his job, so he also has an individual mood problem. Often, your conceptualization of the specific moment the patient describes will involve two or more dimensions. I usually share my conceptualization with the patient. Here’s what I said to Ramesh: “Ramesh, I can think of several ways to look at this problem, and I’m also thinking of several different kinds of tools that could be helpful to you. First, you mentioned how anxious and worthless you felt after the meeting with your boss. We could work on overcoming those feelings, so you can get some emotional relief. Those tools can be extremely helpful, and I would love to work with you along those lines. Second, we could talk about how to handle criticism from your boss and colleagues, and how to turn criticism into praise. Those tools are very different, but they could also make a huge impact on your life.
What to Say
Page 5
“I’m wondering if this makes sense to you. Would you be looking for some help with how you feel, or help with how to turn criticism into praise, or both?” Motivation Step Ramesh has a fairly severe problem and we have some terrific tools to help him. But before we jump in and offer help, we’ll need to think about resistance. When we’re suffering, most of us have one foot in the water and one foot on the shore. Part of us wants to change, but part of us resists change and clings to the status quo. In the old days, we had some powerful motivational questions, and they’re still useful. I’ll review them first. Then I’ll give you some examples of how to incorporate the eight forms of Outcome and Process Resistance into the Motivation Step of Agenda Setting. This is a high art form that can produce spectacular and almost instantaneous changes in many patients, if done skillfully. But it is surprisingly hard for therapists to learn how to do this. Here are some general motivational questions. The first example is a woman named Sarah who was complaining about a long-standing feud with her sister. “Sarah, your conflict with your sister sounds very difficult, and you say it’s been going of for years, every since you were both quite young. You’ve told me that she’s always been jealous and critical of you, since she never got good grades and never went to college. She claims that you act superior and look down on her because you have a Ph.D. “But when you tell her that she’s wrong, and explain that you don’t look down on her, she gets more upset, and everything escalates. That must be so frustrating and draining for you. Is this conflict something you want help with, so you can develop a more loving relationship with your sister, or mainly just something you just wanted me to know about?” You might notice that this is very similar to the Invitation Step. However, many patients will bail out at this point, and tell you that they don’t actually want any help with the problem. What would you do then? Suppose Sarah says, “Why would I want a more loving relationship with someone who acts like a total, selfcentered bitch? I’ve tried everything with her, but nothing works. She’s really a hopeless case.” Think about it for a moment and jot down what you’d say to Sarah you before you continue reading:
What to Say
Page 6
My recommendation would be to accept what Sarah is saying, rather than trying to push ahead. I might simply say, “It sounds like your relationship with your sister is not something we should be working on.” Then, instead of trying to persuade her to change, which is an error that many therapists would make, you can simply empathize, using the Five Secrets of Effective Communication. You can encourage her to tell you more about how angry and hurt she feels, for example, without saying anything to try to help her. After a period of skillful listening, you can issue the Invitation Step again—you can ask her if there is something she would like help with. Here are some additional questions you could ask Sarah at the Motivation Step: •
“Sarah, who do you think should do most of the changing? You or your sister?”
•
“Who do you think is more to blame for this problem? You or your sister?”
•
“Sarah, if I agreed to help you with this conflict with your sister, what would it be worth to you? Would you willing to do psychotherapy homework five days a week, for example, focusing on how you interact with her, and learning how to respond to her critical comments in a radically different way? Or did you mainly just want to let me know how difficult and unreasonable she is?”
Here are some additional questions for any patient that you might ask at the Motivation Step: •
“What would you bring to the table if I agreed to help you with this problem (which might be depression, anxiety, a relationship problem, or an addiction)?”
•
“How important is it for you to solve this problem?”
•
“Would you be willing to do psychotherapy homework consistently between sessions if I agree to help you with this problem, even if you don’t feel like doing the homework?”
Notice that these questions have a paradoxical feel. You’re not trying to sell the patient on change. Instead, you’re encouraging the patient to sell you on the idea of working with them. This has to be done in a respectful, gentle way, with lots of Stroking and Disarming, because the patient might find these questions threatening. The slightest hint of annoyance, sarcasm, or judgment in your tone of voice could trigger a negative reaction. For example, if you are secretly annoyed with the patient, you might sound unsupportive or challenging when you ask these kinds of questions, and this might cause the patient to drop out of therapy.
What to Say
Page 7
Also, if your hidden agenda is to persuade the patient to change, these methods probably won’t be effective. The winning attitude is the idea that we’re there to serve the patient, if the patient wants help, but we are also willing to let go if the patient doesn’t want help, or if the patient isn’t willing to work hard for change. As you probably know, this mindset is called “Sitting with Open Hands.” Let’s say that you wanted to incorporate the newer concept of Paradoxical Agenda Setting, taking into account the patient’s reasons NOT to change. First, let’s review some of the most common sources of Outcome Resistance: Target
Outcome Resistance
Mood disorders. Depression, shame, selfcriticism, hopelessness, worthlessness
The self-criticisms reveal the patient’s value system; the hopelessness protects against disappointment; the relentless negative thoughts may seem to be true
Anxiety disorders. Phobias, OCD, Panic Attacks, Shyness, , GAD, PTSD, other forms of Social Anxiety, Body Dysmorphic Disorder
Magical thinking—the patient thinks the anxiety or compulsive rituals will ward off danger
Relationship problems. Anger, marital conflict, disagreements with friends or colleagues/
Giving up the intense rewards of blaming the other person, feeling “right,” feeling morally superior, or fantasizing about revenge
Habits and addictions. Procrastination, overeating, drinking or drug addiction, having affairs, shopping, internet porn addiction, or dating someone who is abusive
Giving up the tremendous physical and psychological rewards of the habit or addiction
Once you’ve conceptualize some possible reasons why your patient may NOT want to change, in spite of the miserable status quo, you’ll need to learn how to share this information with him or her in a paradoxical but respectful manner. Let’s revisit Ramesh. Here’s what I said to him at the motivation step: “Ramesh, I have some powerful tools to help you with your low selfesteem and the problems you’re encountering at work, and I’d love to work with you. I believe you’re very smart, and I like you, and it would be a joy for me to show you how to turn your life around. I have no doubt that we could do exactly that. But I’m not sure it would be the right thing to do.” Ramesh seemed taken aback. He insisted that he was tremendously interested in working with me and wanted to know what the problem was. Here’s what I said next: "Ramesh, there’s a problem I’m struggling with. You've said that your colleagues treat you unfairly and that they're jealous of you. That must feel extremely unfair, and I can imagine that you might be feeling
What to Say
Page 8
incredibly angry and frustrated with them. You’ve said that they’re jealous and talking behind your back and treating you in a shabby way. They’re bad-mouthing you, which is unfair. You’re not being paranoid— we have proof that this is going on. That’s what your boss told you. "But here’s the rub. They’re not here asking for my help. So if we work together, you're the one who will have to do all the changing. You'll have to learn to change the way you think and feel, as well as the way you communicate with them. And you’ll have to work your butt off during sessions, and you’ll have to do psychotherapy homework between sessions. But that seems rather unfair, since they're the ones who are screwing up. Do you see what I mean? Why should you have to change when they’re to blame for the problem? “What are your thoughts about this? Can you help me solve this dilemma?" I had several goals in making this statement. First, I wanted to find a grain of truth in Ramesh's complaints, so he'd feel accepted. Second, I wanted to convey liking and respect. I suspected that he had a narcissistic streak. I knew that if he felt judged or belittled, he'd probably put up a wall and drop out of therapy before we even got started. And I did like him, so my statement was genuine. But most important, I wanted to head off his resistance at the pass and let him know that he'd have to persuade me to work with him, and not vice versa. Notice that I have become the voice of Ramesh’s subconscious mind. I am verbalizing all the reasons for him not to change. When you do this skillfully, the patient will nearly always suddenly let go of the resistance and buy into the treatment program. The effect is almost as basic as the law of gravity, and the results can be spectacular. Ramesh told me that he definitely wanted to work with me, and would do practically anything if I could help him overcome the problems that had been plaguing him. I told him that was the message I was hoping for, and that I’d love to work with him. Then he broke down and cried as he confessed that he’d been lying to me. He admitted that his boss didn’t really put him on probation—she’d fired him. And he also confessed that he’d been fired six times, from six different jobs, in the past two years. He said that everywhere he went it was the same thing over and over. And if I could show him how to change his life, he’d do anything I asked him to do. Rameesh did more cognitive therapy homework than anyone I'd ever worked with, and I greatly enjoyed the work we did together, which was incredibly successful. For each patient, and for each type of problem, the statements you make during the Motivation step will be slightly different. In addition, each therapist will have his or her own style. But the ingredients will usually be similar. Here’s what I try to convey to each patient:
What to Say
Page 9
•
I’m convinced I can help you if we work together. I have some powerful tools, but the teamwork will also be crucial to our success. This is called “Dangling the Carrot.”
•
“I like you and want to work with you.” This is called “Stroking,” and it has to come from the heart. It has to be genuine or it will backfire.
•
“I can see lots of reasons NOT to change, so I need your help and guidance in how to think about this. I need you to persuade me to work with you in spite of reasons X, Y and Z.” This is the heart of Paradoxical Agenda Setting for Outcome Resistance. I call this technique “Becoming the Voice of the Patient’s Subconscious Resistance.”
•
“If you decide for any reason that you don’t want to change, or that you don’t want to do the work that will be necessary to change, I can accept that. I’m here to help you, if there’s something you want my help with, but I’m not here to impose my agenda, or anyone else’s agenda, on you.” This is called “Sitting with Open Hands.”
Let’s say you’re working with a depressed man named Jim. Jim feels depressed and worthless. He’s relentlessly self-critical, always comparing himself to others and coming up short in his mind’s eye. He constantly dwells on his failures, shortcomings, and defects. Previous therapists have not been able to help him, and he hasn’t responded to antidepressant medications. Think about Outcome Resistance. Imagine that there’s a Magic Button on your desk. If he pushes it, his depression will suddenly disappear, and he’ll walk out of today’s session with feelings of joy and self-esteem. All his self-criticisms will vanish. Will he push the Magic Button? See if you can list several reasons why he might not want to push the button. What are some reasons Jim might NOT want to change? 1. 2. 3. 4. 5. Now ask yourself what you’d say to Jim at the Motivation step of Agenda Setting. Write down your response before you continue reading. If you need more space, use a separate piece of paper:
What to Say
Page 10
Have you written something down? No? Then go back and do it! It will make a huge difference in your understanding and skill development. Even an ineffective response will be invaluable. Here’s what I might say: “Jim, you mentioned that you want help with your tendency to be relentlessly self-critical. I’d love to help you with that problem. I know from personal experience how horrible it is to feel ashamed, inadequate, or even worthless. I can’t make any promises, but if we worked together, I’m convinced that we could do some tremendous work—work that could change your life. Would that appeal to you?” Assuming he responds positively, I might say this next: “That’s great, Jim. I’m really glad you want to work with me. However, I have some concerns I’d like to share with you, and I need your guidance. For one thing, your feelings of self-criticism show me that you have a tremendous sense of integrity. You’ve told me that you’ve had a lot of failures in your life, and that your career and accomplishments haven’t really measured up to your dreams and expectations. When you look at people you know and admire, and all they’ve accomplished, you feel ashamed and tell yourself you’re inferior by comparison. Although that’s incredibly painful, it shows that you have courage, and that you’re not going to go around fooling yourself or pretending you’re something that you’re not. And it also shows that you’re humble, which is an important spiritual quality, a quality that’s especially lacking in our culture, with all our emphasis on ego and status. Can you think of some other reasons to maintain your depression?” Now you can do some brainstorming on what the depression shows about Jim that’s actually very positive. The idea is to try to sell him on the benefits of his depression. Help him see that the depression reveals things about him that are actually very admirable. This is a paradoxical strategy, since most therapists, family members, and friends have probably been trying to persuade him to change. If he starts to persuade me that he really does want to change, I might say this:
What to Say
Page 11
“I’m really glad you want to change, but I have one more problem I need your help with. Let’s imagine, just for the moment, that I could show you how to make those negative feelings disappear. In fact, let’s imagine it happened in today’s session, and you suddenly experienced joy and self-esteem and walked out of today’s session feeling fantastic, like some kind of miracle occurred. That actually could happen—I’m not sure it will happen today, but it might. Would you want that to happen?” He’ll probably say yes. Then I might say something like this: “Okay, but here’s one more thing to think about, and I want to make sure we’re on the same page. If you walked out of today’s session feeling joy and self-esteem, it would mean that you’d have to give up some of your perfectionism, and allow yourself to feel happy and fulfilled in spite of the many failures and disappointments in your life. That’s because I can’t change the facts of your life today, I can only show you how to change the way you think and feel about yourself. “I’d love to show you how to give up your perfectionism and all that selfcriticism that’s making you miserable, and I’m pretty sure I can teach you how to do that. But your perfectionism and self-criticism show that you’re not willing to settle for second best. In fact, you have incredibly high standards in a world where so many people settle for mediocrity. So I’m not convinced you’d want that kind of change, or that you should lower your standards. “Can you help me with these concerns? Before I could show you how to overcome your depression, I would need you to help me understand the justification for doing that. Are you saying that you be willing to experience joy and self-esteem TODAY, if I could show you how, in spite of the fact that you haven’t measured up to so many of your goals and expectations? “You’ve told me that you’re only average, or even below average. In a way, that’s true. You have many flaws, and so do I. I can only show you how to be a joyous, flawed and below-average person. Do you want that result? Or are you saying that you’d prefer to keep beating up on yourself, and making yourself miserable, because of your failures and shortcomings? I could understand entirely if you wanted to stay on the same track you’re on.” Notice that I’m attempting to become the voice of the patient’s subconscious resistance. He will have to persuade me to work with him. And if he decides he doesn’t want to change his self-critical tendencies or lower his perfectionistic standards, I can accept that. The above “dialogue” is long and may sound like a boring monologue! I apologize for that. You can do this interactively, as a real conversation with the patient, rather than a speech. I’m just trying to get the message across so you’ll understand it. You can bring this message to life in your own words, using your own therapeutic style.
What to Say
Page 12
My goal is not to impose my own values on my patients, but rather to find out if they have something they want help with, and if they’re willing to pay the price of bringing that change about. Once you’ve melted away the Outcome Resistance, and the patient can argue effectively against the many reasons to maintain the status quo, you can focus on Process Resistance. Is the patient willing to do what’s going to be necessary to achieve change? Simply coming to therapy sessions won’t be enough. Each type of problem will be associated with a unique form of Process Resistance. Here’s a brief summary of the most common forms of Process Resistance: Target
Process Resistance
Mood disorders. Depression, shame, selfcriticism, hopelessness, worthlessness
Patients probably won’t want to do daily psychotherapy homework, such as recording negative thoughts on the Daily Mood Log or scheduling more satisfying and productive activities on the Pleasure Predicting Sheet.
Anxiety disorders. Phobias, OCD, Panic Attacks, Shyness, , GAD, PTSD, other forms of Social Anxiety, Body Dysmorphic Disorder
Patients probably won’t want to have to use exposure techniques because it will be so anxiety-provoking.
Relationship problems. Anger, marital conflict, disagreements with friends or colleagues
Patients probably won’t want to pinpoint their own role in the problem because they’re so convinced it’s the other person’s fault. They may insist on endless blaming and complaining and fight hard against learning to change themselves.
Habits and addictions. Procrastination, overeating, drinking or drug addiction, having affairs, shopping, internet porn addiction, or dating someone who is abusive or uninterested in a committed relationship
Patients won’t want to face the anxiety, deprivation, and discomfort of withdrawal, change, or tackling chores they’ve being putting off. The love-addicted patient may not be interested in overcoming the fear of being alone.
When you’re focusing on Process Resistance, you can use the Gentle Ultimatum. For example, let’s say the patient is asking for help with shyness. I might say something like this: “Roger, I’d love to help you with the shyness you’ve been struggling with. I have lots of extremely helpful techniques to share with you, and I’m pretty sure that you’re going to enjoy most of them. For example, I might ask you to read chapters from the book, Intimate Connections, between sessions, and I’ll definitely ask you to use the Daily Mood Log to record the Negative Thoughts you have in social situations. “However, there are some techniques that you won’t like at first, because they will involve confronting your fears and experiencing tremendous anxiety. These techniques have names like Smile and Hello Practice, Self-Disclosure, the David Letterman Technique, Flirting Training,
What to Say
Page 13
Rejection Practice, and Shame Attacking Exercises. I’ll be glad to describe them and give a feel for what’s involved. Before I can agree to work with you, I’ll need to know whether you’d be willing to confront your fears and do some fairly outrageous things in order to change your life? In other words, what would it be worth to you to defeat this problem?” What you say to each patient will differ slightly, since different kinds of problems will present different kinds of Process Resistance, as you can see in the table above. In addition, your own personality and therapeutic style will differ from my own. But the basic concept will be the same—letting the patient know what will be required for successful treatment and asking if they’re willing to pay the price. If patients express reluctance or say that they can’t do what I’m asking, I don’t generally try to persuade them, since that almost never works. I simply using “Sitting with Open Hands” and ask if there’s some other kind of problem they might want to work on instead. Methods Step At the Conceptualization Step of Agenda Setting, you pinpoint the type of problem the patient wants help with. This helps you with the Motivation step, since each type of problem will be associated with its own unique form of Outcome Resistance and Process Resistance. In addition, each type of problem will usually responds to certain types of techniques, from the list of 50 techniques I have developed. Here is a brief overview. Depression: You can use •
Cognitive Techniques, such as 1. Identify the Distortions 2. The Paradoxical Double Standard Technique 3. Examine the Evidence 4. The Externalization of Voices 5. The Acceptance Paradox 6. The Individual Downward Arrow 7. The Straightforward and Paradoxical Cost-Benefit Analysis 8. Let’s Be Specific
•
Behavioral Activation Techniques, such as 1. The Daily Activity Schedule 2. The Anti-Procrastination Technique 3. The Pleasure-Predicting Sheet
Anxiety: You can use •
Cognitive Techniques, such as
What to Say
Page 14
1. The What-If Technique 2. The Feared Fantasy 3. The Experimental Technique 4. Thinking in Shades of Gray •
Exposure and Response Prevention Techniques, including 1. Classical Exposure 2. Cognitive Exposure 3. Interpersonal Exposure
•
The Hidden Emotion Technique
Anger / relationship problems: You can use Interpersonal Techniques, such as •
Interpersonal Decision-Making
•
Interpersonal Downward Arrow Technique
•
The Blame Cost-Benefit Analysis
•
The Relationship Journal
•
The Five Secrets of Effective Communication
•
The Intimacy Exercise
Habits and addictions: You can use motivational techniques, such as •
The Decision-Making Form
•
The Paradoxical Cost-Benefit Analysis
•
The Addiction / Habit Log
•
The Devil’s Advocate Technique
•
Stimulus Control
•
Relapse Prevention
If the patient is depressed, how would you select which cognitive techniques to use, from the list of 50? Put your answer here, before you continue reading:
Don’t turn the page until you’ve written something down. Thanks!
What to Say
Page 15
Answer You can select methods using the Daily Mood Log (DML) and Recovery Circle. After you fill out the first four steps of the DML (Upsetting Event, Emotions, Negative Thoughts, and Distortions), ask the patient which thought she or he wants to work on first. Write that thought in the middle of a Recovery Circle and select at least 15 techniques you can use to challenge it. You can do the Recovery Circle alone or with the help of the patient. It’s equally effective either way. I have written the list of 50 Ways to Untwist Your Thinking in consumer language, so patients can easily review it with you and pinpoint techniques they’d like to try.
Paradoxical Agenda Setting (PAS) Flowchart By David D. Burns, MD*
Theme of Outcome Resistance Theme of Process Resistance
Depression
Anxiety
Relationship Problems
Habits / Addictions
Acceptance
Magical Thinking
Not Wanting to Get Close
Pleasure / Entitlement
Psychotherapy Homework (HW)
Exposure
Giving up Blame
Deprivation / Discipline
Depression
Anxiety
Relationship Problems
Habits / Addictions
Straightforward Invitation
Paradoxical Invitation Specificity Question— Steps 1 & 2 of Relationship Journal (RJ)
Specificity Question— First 3 steps of Daily Mood Log
Techniques for Outcome Resistance
Specificity Question— Steps 1 and 2 of Habit / Addiction Log
Miracle Cure Question Interpersonal Decision-Making / Decision-Making Form
Magic Button Positive Reframing / Paradoxical Cost-Benefit Analysis
Decision-Making Form / Straightforward or Paradoxical Cost-Benefit Analysis
Externalization of Resistance
Magic Dial
Blame Cost-Benefit Analysis
Devil’s Advocate Technique
Sitting with Open Hands Dangling the Carrot
Techniques for Process Resistance
Gentle Ultimatum = HW even when not in the mood
Gentle Ultimatum = Exposure, even if frightening
Gentle Ultimatum = Pinpoint your role in the problem (Steps 3 & 4 of RJ) and work entirely on changing yourself (Step 5 of RJ)
Fallback Position Sitting with Open Hands
* Copyright © 2014 by David D. Burns, MD
Gentle Ultimatum = Daily AA or Smart Recovery Meetings / Stimulus Control / Use Habit & Addiction Log
Brief Examples of Selected PAS Techniques 1. Straightforward Invitation. “You’ve mentioned problems X, Y, and Z, and I can see how painful they are for you. I’d like to offer you more than just listening and support, and I believe we could solve these problems if we work together, I’m wondering if you’d like some help with one of them today, or if you need more time just to talk and have me listen? 2. Paradoxical Invitation. “Are you asking for help with the problem with your husband (or sister, or friend, etc.), or did you simply want me to know about how lonely and frustrated you’ve been feeling?” 3. Sitting with Open Hands. “It sounds like you aren’t asking for any help with your relationship with your husband (or your anxiety, etc.). I’m wondering if there’s anything else that’s bothering you that we could work on together?” 4. Specificity. “Can you describe one specific interaction with your husband that was upsetting to you? Write down exactly what he said to you and exactly what you said next on the Relationship Journal.” Or “Tell me about one moment when you were struggling with depression? What was going on? What were you thinking and feeling? Let’s write that down on the Daily Mood Log.” 5. Miracle Cure Question. “Let’s suppose we had a magic wand and could solve that problem, so you’d walk out of today’s session feeling fantastic. What would the solution look like? What would change?” 6. Magic Button. “Imagine that there’s a Magic Button on the table, and if you push it, all your negative feelings will disappear and you’ll walk out of today’s workshop on a real high, feeling fantastic. Will you press the button?” 7. Positive Reframing. “I’m glad you want to press that Magic Button. However, I can think of a lot of really good reasons NOT to press it. What do these negative Thoughts and feelings show about you that’s really positive and awesome?” 8. Paradoxical Cost-Benefit Analysis (CBA). “I have some terrific tools to help you, but I can think of a lot of powerful reasons NOT to give up the belief that you’re hopelessly depressed, or that you’re a loser. Why don’t we list some of them here?” 9. Magic Dial. “Given that your Negative Thoughts and feelings show so many good things about you, maybe we don’t want to get rid of them entirely. I’m wondering if there’s a lower level that would be acceptable to you. If we had a Magic Dial, and you could set the intensity at any level at all, how ashamed would you want to feel? What would be the ideal level? Let’s write that down in the Goal column on your Daily Mood Log.” Then “How depressed do you want to feel,” and “how defective,” etc. 10. Externalization of Resistance. “I’m glad that you want to improve your relationship with your sister. However,, my main concern is that she isn’t here today and you say that he’s the one who needs to change, and she’s the one who’s to blame, and not you. It would seem unfair for you to have to do all the work and all the changing. And yet, that’s the approach we’d have to take.” 11. Dangling the Carrot. “I’d love to help you with the problem with your husband and I have some excellent tools to share with you . . .” Or “I’m glad you want help with your low self-esteem, because I have some terrific tools to help you.” These kinds of statements lead into the Gentle Ultimatum. 12. Gentle Ultimatum. “If I agreed to help you develop better self-esteem, would you be willing to do written psychotherapy homework every day, even if you didn’t feel like it, for a whole month?” Or “I’d love to help you with your OCD, and I believe we could be quite successful, but I don’t know how to eliminate any form of anxiety without confronting your fears.” Or “I’d be happy to help you with your relationship with your husband, but you’d have to do psychotherapy homework every day, focusing on changing yourself, rather than trying to change him. Would you be willing to do that?” 13. Devil’s Advocate. “You’ve written down a lot of the thoughts you have when you’re tempted to (take a drink, overeat, procrastinate, etc.) For example, you tell yourself that one drink can’t hurt, that you’ll enjoy the baseball game so much more, and so forth. I’m going to play that part of your mind and try to tempt you to take a drink. See if you can defeat me.” 14. Fallback Position. You’ve been pretty clear that you’re not happy with the idea of psychotherapy homework (HW), and that’s totally understandable. Sadly, I don’t know how to treat depression without homework. In fact, I’ve never had a patient recover who refused to do HW. But I totally respect your thinking. There are lots of therapists in the community who don’t believe in the value of psychotherapy HW. Of course, I really want to work with you, and what a joy it would be to see you overcome your depression and feel joy and self-esteem again. But I want to be clear that if you do decide to work with me, the HW issue would not be negotiable.” 15. Problem-Solution Method (for procrastination). “Can you think of anything that might interfere with your plan to work on your dissertation from 6 PM to 6:05 PM tonight as you’ve agreed?’ let’s write them down on the left hand column of this ProblemSolution Sheet. Now, how are you going to solve that problem?” 16. Stubbornly Refused Technique (combined with previous technique). “Will you agree to call my office number and leave one of two messages at 6:05? You can either say ‘Mission accomplished’ or ‘I stubbornly refused.’”
* Copyright © 2014 by David D. Burns, MD
PAS for Relationship Problems
Page 1
Paradoxical Agenda Setting (PAS) for Relationship Problems: An Overview By David D. Burns, MD* This memo is just a way of putting certain PAS concepts together. In real-world situations, you will be more fluid and spontaneous, and may end up doing these steps in a different order, or in a different way. The assumption here is that you will be working with an individual with a relationship problem, and not a couple. It is more difficult to work with couples, and we can review those methods in future seminars. In addition, I am assuming you have done superb E = Empathy prior to attempting PAS. Step 1. The Invitation Step: You will most likely use the Paradoxical Invitation. If your patient indicates that she or he DOES want help with a relationship problem, here is a question you might ask. You may recognize it as the Miracle Cure question. What kind of help would you be look for? If this was a terrific session, and you walked out the door thought, “Wow, that really helped,” what kinds of changes would happen? What are you hoping for if we work on your conflict with X? I indicated above that you may have to do things in a slightly different order. For example, if the patient says that his wife (or boss or whoever) would change and stop acting like a jerk, you might have to jump right into a brief bit of Process Resistance, and point out that that person is not here asking for help, so if you were to work together on this problem, the patient would have to do the changing. Ask if the patient would be open to that. If the patient says no, you can probably give up this agenda and ask if there’s something else the patient wants help with. Step 2. Specificity: If the patient does wants to work on making the relationship better, ask him or her to fill out the first two steps of the Relationship Journal (RJ), with your help. You can explain that you need one specific example of the kinds of interactions that the patient finds troubling. Make sure that you ask the patient to give you an example of an interaction that did not go well—something that she or he needs help with. The RJ is important, because the entire conflict between the two people will be fully embedded in any one brief problematic exchange. So once you understand that brief exchange, you will really have the key to the entire problem in the relationship. And once the patient learns how to turn that one example around, he or she will probably know how to deal with any conflict with that person—or with anyone. Step 3. Conceptualization: There are two things I like to do once I’ve learned about the problem from the patient and I have an example from the RJ. First, I ask myself if the patient is involved in Self-Blame, or Other-Blame, or both. If the patient is excessively self-blaming, this will often trigger strong negative emotions such as guilt, shame, anxiety, depression, worthlessness, hopelessness, and so forth. If so, you may have to step back and do some individual mood work, using the Daily Mood Log, before working on the relationship conflict. If, contrast, the patient is involved on Other-Blame (this is the most common), I try to conceptualize how the patient sees the conflict. In other words, what is the patient’s chief complaint about the other person? Here are some common patterns: He/she never listens. He/she always has to be right. He/she won’t express his/her feelings. He/she claims I don’t love him/her. He/she constantly complains. He/she always has to get his/her way. He/she is too controlling. All he/she cares about is himself / herself.
* Copyright © 2017 by David D. Burns, MD
PAS for Relationship Problems
Page 2
He/she clams up and refuses to talk to me. This is important because when you do Step 4 of the Relationship Journal, you will usually be able to see how the patient is forcing the other person to do the exact thing that he or she is complaining about. If the word, “forcing,” is too strong for you, you could think about how the patient is triggering, or reinforcing, the problem he or she is complaining about. Step 4. Motivation: At this step, you bring Outcome and Process Resistance to conscious awareness. Although we’ve already asked the patient if he or she wants a better relationship with X, it doesn’t hurt to make sure. The following questions focus on Outcome Resistance: Do you want to talk about the problem some more, or do you want to work on developing a better relationship with X? How strong is your desire to get close to him / her? Do you sometimes have the urge just to get out of this relationship? You can also do Interpersonal Decision-Making, saying something like this: “You have three choices— you can work to make the relationship better, you can leave the relationship, or you can stay in it without trying to change anything. I’d be willing to support you with any of these options. Does one of these them appeal to you more than the others?” If the patient is strongly ambivalent, you can use the Interpersonal Decision-Making Form, as discussed in detail in a chapter in your reader. If the patient still wants to make the relationship better, you can ask questions that focus on Process Resistance: Are you ready to start working on the conflict with X right now? Is this specific example on the Relationship Journal acceptable? Would you be willing to experience some pain in order to develop a more rewarding relationship with X? Doesn’t it seem rather unfair that you will have to do all the changing when, as you say, X is the one who’s to blame? Would you be willing to examine your own role in the problem? How long would you be willing to work on solving this specific problem? (in other words, how many sessions) How hard would you be willing to work on it? If I agree to help you with this problem, how much homework would you be willing to do between sessions? Who do you think should change? You or the other person? What would it be worth to you if I agreed to show you how to change? If I agree to help you with this problem, would you be willing to assume complete responsibility for change? In your opinion, who’s more to blame for the problems in your relationship? Is it you or the other person? You can do the Blame CBA at this point if you want. Step 5. Methods: If the patient is still on board, you can continue with Steps 3 to 5 of the RJ. However, you may continue to run into fairly intense therapeutic resistance at various points. If so, you can Empathize, and then renegotiate the therapeutic agenda.
* Copyright © 2017 by David D. Burns, MD
PAS for Relationship Problems - Sample Flow (Many combinations of these elements possible!) Empathy, empathy…
Paradoxical Invitation
Interpersonal Decision Making
Talk/Support Improve Relationship Outcome Resistance: Get close? Acid test: Why? Really?
Leave Relationship
Process Resistance: Give up blame; Assume responsibility; Change first? Blame CBA
Yes / Assume responsibility Relationship Journal Daniele V. Levy, PhD, 2017
Work
No / Blame others Sit Open Hands
Empathy; DML
Status Quo Empathy; DML
PARADOXICAL INVITATION DIALETICS IN AGENDA SETTING FOR RELATIONSHIP PROBLEMS BEFORE ISSUING PARADOXICAL INVITATION
PARADOXICAL INVITATION
Patient as victim of interpersonal reality Therapist holds viewpoint of patient
Therapist validating status quo
PAS for relationship problems
…doesn’t sound like you actually want my help, right?... Therapist surfaces viewpoint of others
IF PARADOXICAL INVITATION IS ACCEPTED
Therapist inviting change Patient creating interpersonal reality
NEW Habit & Addictions Materials Including help for procrastination and difficult decisions.
Treating Addictions / Burns
Page 1
Positive and Negative Distortions* By David D. Burns, M.D.
In my book, Feeling Good, I listed ten cognitive distortions, or thinking errors, such as All-or-Nothing Thinking, Jumping to Conclusions, Should Statements, Emotional Reasoning, and Self-Blame. These negative distortions trigger negative feelings such as:
Depression Feelings of worthlessness, inferiority, and low self-esteem Hopelessness Anxiety, shyness, and panic Shame and guilty Anger and frustration
The list of negative distortions has been reproduced in hundreds of magazines and books and has been helpful to many individuals suffering from mood problems. The idea is that when you’re feeling upset, you’re often involved in a mental con, but you don’t realize it. You’re telling yourself things about yourself and the world that aren’t really true. And when you change the way you think you can change the way you feel. Most people are not aware that positive distortions can also play an important role in emotional and relationship problems, as well as habits and addictions. There are ten positive distortions that are the exact mirror images of the ten negative distortions. For example, Positive All-or-Nothing Thinking is the opposite of Negative All-or-Nothing Thinking. In both instances, you look at things in opposite, black-or-white categories, and shades of gray do not exist. In the negative version, you might think of yourself as a “loser” because your marriage broke up, or because you failed to achieve an important personal or professional goal. In the positive version, you might think of yourself as a “winner” because of some positive event or personal success. Positive distortions can be as destructive as negative distortions. When left unchecked, they can trigger mania (abnormal mood elevations), habits and addictions such as gambling and alcohol and drug abuse, and relationship problems, as well as feelings of rage, violence, and even war. For example, Hitler’s messages to the German people involved a skillful blend of positive and negative distortions. He tried to sell the German people on the idea that they were a superior race with the right or duty to exterminate Jews, mental patients, gypsies and others who were labeled as “bad” or “inferior.” Unlike the negative distortions, the positive distortions typically lead to intoxicating mood elevations so you may not be motivated to challenge them or to change the way you’re thinking. In the following table, I will define each distortion, followed by examples of the negative and positive versions.
* Copyright © 2010 by David D. Burns, M.D. Do not reproduce without permission. Revised 2014.
Treating Addictions / Burns
Page 2 Checklist of Negative and Positive Distortions*
Distortion
Negative Distortion Example
Positive Distortion Example
1. All-or-Nothing Thinking. You think about yourself or the world in black-or-white, all-or-nothing categories. Shades of gray do not exist.
When you fail, you may tell yourself that you’re a complete failure.
When you succeed, you may tell yourself that you’re a winner and feel superior.
2. Overgeneralization. You think about a negative event as a never-ending pattern of defeat or a positive event as a never-ending pattern of success.
When you’re rejected by someone you care about, you may tell yourself that you’re an unlovable loser who will be alone and miserable forever.
When you overcome an episode of depression or selfdoubt, and you’re suddenly feeling happy again, you may tell yourself that all your problems are solved and that you’ll always feel happy.
3. Mental Filter. You think exclusively about your shortcomings and ignore your positive qualities and accomplishments. Or, you dwell on the positives and overlook the negatives.
A TV talk show host told me that he typically received hundreds of enthusiastic emails from fans every day, but there was nearly always one critical email from a disgruntled viewer. He explained that he’d obsess for hours about the negative email and completely overlook the hundreds of glowing ones. As a result, he constantly struggled with feelings of anxiety and low self-esteem in spite of his tremendous ratings and popularity.
You may fantasize about how good that desert will taste, and ignore the negatives, like gaining weight and feeling guilty or bloated afterwards. Or, you may tell yourself how great you’ll feel if you have a drink, and ignore the fact you nearly always drink too much and end up with a hangover.
4. Discounting the Facts. You tell yourself that negative or positive facts don’t count, so as to maintain a universally negative or positive self-image.
Discounting the Positive: When someone genuinely compliments you, you may tell yourself they’re only saying that to make you feel good.
Discounting the Negative: When you’re trying to diet and feeling tempted by something tasty, you may tell yourself, “I’ll only have one little bite.” But you’ve probably given yourself this message on hundreds of occasions, and it has never once been accurate! During an argument, you may get defensive and insist that the other person is “wrong.” Then the conflict escalates.
5. Jumping to Conclusions. You jump to conclusions that aren’t warranted by the facts. There are two common forms: Mind-Reading, you make assumptions about how other people are thinking and feeling. Fortune-Telling, you make dogmatic negative or positive predictions about the future.
Mind-Reading: If you’re feeling shy at a party, you may tell yourself that other people don’t have to struggle with shyness or that they’d look down on you if they knew you were shy. Fortune-Telling: When you’re depressed, you may tell yourself that you’ll never recover. When you’re feeling anxious, you may tell yourself that something terrible is about to happen—“When I give my talk, my mind will go blank. I’ll look like an idiot.”
Mind-Reading: You may tell yourself that a relationship is going really well when the other person is actually feeling annoyed or unhappy with you. Fortune-Telling: You may tell yourself, "I'll just have one drink" or "one bite," when, in fact, you never stop at just one drink or bite.
* Copyright © 2010 by David D. Burns, M.D. Do not reproduce without permission. Revised 2014.
Treating Addictions / Burns
Page 3
6. Magnification and Minimization. You blow things out of proportion or shrink their importance inappropriately. This is also called the “binocular trick” because it’s like looking through the ends of a pair of binoculars, so things either look much bigger, or much smaller, than they are in reality.
When you’re procrastinating, you may think about everything that you've been putting off and tell yourself how overwhelming all those tasks will be. (Magnification) You may also tell yourself that you’re efforts today wouldn’t amount to anything anyway, so you might as well put it off. (Minimization)
When you’re trying to diet and you’re feeling tempted, you may tell yourself: "This ice cream will taste so good!" (Magnification). Will it really be that good? Will it be worth the way you’ll feel about yourself after you give in to the urge to binge?
7. Emotional Reasoning. You reason from how you feel. In point of fact, your feelings result from your thoughts, and not from what’s actually happening. If your thoughts are distorted, your feelings will be as misleading as the grotesque images you see in curved funhouse mirrors.
You may tell yourself, "I'll clean my desk (or start my diet) when I'm more in the mood. I just don't feel like it right now." Or course, the feeling never comes! When you’re depressed, you may tell yourself, “I feel like a loser, so I must really be one.” Or “I feel hopeless, so I must be hopeless.”
When you’re gambling, you may say, “I feel lucky! I just know I’m about to hit the jackpot.”
8. Should Statements. You make yourself (or others) miserable with “shoulds,” “musts” or ”ought’s.” Hidden Shoulds are implied by negative thoughts. Self-Directed Shoulds cause feelings of guilt, shame, depression, and worthlessness. Other-Directed Shoulds cause feelings of anger and trigger interpersonal conflict. World-Directed Shoulds cause feelings of frustration and entitlement.
Self-Directed Shoulds: You tell yourself that you shouldn’t have screwed up and made such a stupid mistake. Other-Directed Shoulds: You may tell yourself, “That fellow shouldn’t cut in front of me in traffic like that. I’ll show him that he can’t get away with it!” World-Directed Shoulds: “The train shouldn’t be late when I’m in such a hurry!”
Self-Directed Shoulds: When you’re feeling tempted, you may tell yourself, "I've had a hard day. I deserve a drink (or a nice dish of ice cream).” Other-Directed Shoulds: You may tell yourself that your values are the best values and that other people should think and feel the same way. World-Directed Shoulds: You may tell yourself that the world should be the way you expect it to be.
9. Labeling. You label yourself or others instead. Labeling is actually an extreme form of overgeneralization, because you see your entire self or essence as defective and globally bad, or superior.
You may label yourself or someone you’re not getting along with as “a loser” or “a jerk.” A physician slipped up on her diet and gave in to the temptation to eat a donut Then she told herself that she was “a fat pig with no will power." This thought was so upsetting that she ate six more donuts.
When you do well, you may think of yourself as special or as “a winner.” Motivational speakers, politicians, and athletic coaches often use this strategy to motivate people. But in reality, there’s no such thing as a “winner” or a “loser.” We’re all human beings, and no one can win or lose all the time.
10. Blame. You find fault with yourself (Self-Blame) or others (Other Blame).
Self-blame. If you’re depressed, you may beat up on yourself constantly and mercilessly, blaming yourself for every error and shortcoming instead of using your energy to find creative solutions to your problems.
Other-blame. During an argument, you may tell yourself that the other person is to blame for the conflict. Then you feel like an innocent victim and overlook your own role in the problem.
This distortion also triggers romantic intoxication. When you meet someone attractive, you may feel so happy and excited that you think that he or she must be wonderful—the man (or woman) of your dreams.
* Copyright © 2010 by David D. Burns, M.D. Do not reproduce without permission. Revised 2014.
Treating Addictions / Burns
Page 4
Although it is a matter of controversy, I believe that it is possible to feel joyous and enlightened without positive distortions. I’m also convinced that healthy negative emotions (such as sadness or healthy fear) can be distinguished from unhealthy negative emotions (such as clinical depression or a panic attack) by the presence or absence of negative distortions in the thoughts that trigger the feelings. In the third chapter of Feeling Good I described an experience during my medical school when I was on call for the inpatient surgical service one evening at the Stanford Hospital. One of our patients was an elderly man with a kidney tumor. We operated and successfully removed his kidney, and the prognosis seemed positive. Unfortunately, he suddenly developed an aggressive metastasis to his liver and was placed on the critical list. The metastasis was not treatable. His elderly wife stayed by his bed night and day, and wouldn’t leave the hospital. At times, she would just let her head slump next to him on the bed and fall asleep. She often stroked his head and said, “You’re still my man and I have always loved you.” One night he began to slip into a coma, so the family was notified. Nearly a dozen of them soon arrived in his room, including his children and grandchildren. One of his sons asked if I could remove the catheter from his penis, because it had been uncomfortable for him. I was pretty unsure of myself, and didn’t even know how to remove a catheter, so I checked at the nursing station, but they said it was okay and explained how to do it. I asked if this meant that he was dying, and they said he was. I went back to the room, pulled the curtain around the bed, and removed the catheter from his penis. Then I opened the curtain again. His son looked at me and asked, “Does that mean he’s going to die tonight?” I had grown attached to him because he was a very kind man who had reminded me of my grandfather. Tears were rolling down my cheeks as I said, “He’s slipping into a coma, but he can still hear you, so it’s time to say goodbye. I loved him, too.” They all gathered around his bed to comfort him. I went to the room where the residents did their charting work and began to sob. He died within an hour. To my way of thinking, the experience of profound sadness and loss, without distortions, is not depression, but rather a celebration of life. Sadness reflects our capacity for love. Healthy negative and positive emotions don’t need treatment, but are part of the richness of the human experience. Sometimes healthy negative emotions (such as grief) are complicated by negative distortions, so healthy and unhealthy feelings coexist. In this case, you can use the “Mood Journal” to pinpoint and challenge your distorted negative thoughts. In Feeling Good I also described a severely depressed, suicidal physician whose brother had committed suicide. She was telling herself: 1. His depression was my fault because our parents loved me more when we were growing up. 2. I should have known he was suicidal the night he killed himself. 3. Because I failed him, I too, deserve to die. These thoughts contained many distortions, such as Self-Blame, Should Statements, and Emotional Reasoning, as well as Mind-Reading and Fortune-Telling, since she expected herself to know how he was thinking and feeling the night he took his life. Fortunately, we were able to find a way to challenge and defeat those thoughts during her seventh therapy session. Her depression and suicidal urges vanished, and she was finally able to grieve his loss. Paradoxically, the intense depression, shame, and guilt she was feeling had prevented her from grieving his loss in a healthy way. * Copyright © 2010 by David D. Burns, M.D. Do not reproduce without permission.
T = Testing (Initial Evaluation and Session-bySession Assessment of Progress)
Treating Addictions / Burns
Page 6
0 -No
Lifetime Alcohol Screening* Have you ever used alcohol excessively? Have you ever felt that you might have a problem with alcohol? Has anyone ever suggested you might have a problem with alcohol? 4–6
7-9
Total (3 items)
Problems from Alcohol Use (Dx34 – 35)*
Instructions. Use checks () to indicate whether you've had the following kinds of problems because of alcohol. Please answer all of the items.
6
4 – Completely true
2–3
3 – Very True
1
2 – Moderately true
0
1 – Slightly true
(Page 31)
2 -3 -Probably Definitely
0 – Not at all true
1. 2. 3.
1 -Maybe
1.
Have you experienced strong cravings to drink alcohol?
2.
Have you ever spent a great deal of time using alcohol?
3.
Have you had to take more and more alcohol in order to get high?
4.
Has it ever been hard to cut down or stop drinking?
5.
Have you ever had problems at home, at school, or at work because of alcohol?
6.
Did you ever have problems in your relationships with others because you were drinking?
7.
Have you ever had blackouts or forgotten what you did when you were high on alcohol?
8.
Have you sometimes used alcohol in physically dangerous situations, such a driving?
9.
Have you ever gotten depressed or violent when you were using alcohol?
10.
Did you ever experience withdrawal symptoms when you tried to stop drinking?
11.
Have you ever continued to drink even though the alcohol was causing emotional problems, health problems, legal problems, relationship problems, or other problems?
(Page 31)
0
1–3
4 – 10
11 – 25
26 – 44
Total (10 items)
* Copyright © 1995 by David D. Burns, M.D. Revised 2006, 2009. * Copyright © 2009 by David D. Burns, M.D. Do not reproduce without permission.
28
Brief Mood Survey* Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
How depressed do you feel right now? 1. 2. 3. 4. 5.
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life
Before Session
After Session
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Page 7
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Treating Addictions / Burns
Total
Total
15
1
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life?
Total
Total
2
0
How anxious do you feel right now? 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous
Total
Total
13
2
How angry do you feel right now?
4 – Completely true
Instructions. Use checks () to indicate how you‘ve been feeling in the past week, including today. Please answer all of the items.
1
3 – Very True
Cravings and Urges to Use*
Total
8
1 – Slightly true
Total
2 – Moderately true
Frustrated Annoyed Resentful Angry Irritated
0 – Not at all true
1. 2. 3. 4. 5.
1.
Sometimes I crave drugs or alcohol.
2.
Sometimes I have the urge to use drugs or alcohol.
3.
Sometimes I really want to use drugs or alcohol.
4.
Sometimes it’s hard to resist the urge to use drugs or alcohol.
5.
Sometimes I have to struggle with the temptation to use drugs or alcohol.
Total
* Copyright
2004 by David D. Burns, M.D.
* Copyright © 2009 by David D. Burns, M.D. Do not reproduce without permission.
18
Treating Addictions / Burns
Page 8
Paradoxical Agenda Setting Exercise: A Complex Case of Alcohol Abuse with Emotional and Interpersonal Problems
A single, 40 year-old, chronically depressed divorce attorney named Janine feels devastated because her main dream in life has always been to have a baby and a family of her own. She has no steady boyfriend and is convinced that she’s too old to have a child. An uncle abused Janine when she was eight years old, but she never got any help because her parents didn’t believe her when she told them what was going on. After a few months, he moved to Seattle, but she continued to feel humiliated, ashamed, and angry. Janine is attractive and dates a fair amount, but tells you that the men always turn out to be losers. Most of them are self-centered and afraid of intimacy, so every time she gets serious they reject her or disappear. The rest are needy and desperate, so she loses respect for them and rejects them. Then they chase her and become pests. She usually takes the woman’s side in divorce cases and has the reputation of making men pay. She is quite successful and earns a great deal of money. However, her work with warring couples reinforces her cynical views of intimacy. Janine is bitter because this is a couples’ world, and people look down on you if you’re alone. For example, when she goes to restaurants, she feels intensely out of place, anxious, resentful, and uncomfortable. Janine is a wine connoisseur and comforts herself by drinking wine at night, often more than a fifth, and frequently passes out, waking up many hours later in the early morning hours on the couch. She feels intensely anxious in social situations, but sometimes goes to singles bars, gets drunk, and picks someone up, only to wake up the next morning disgusted with herself and the man she met. Janine has had more than 20 years of unsuccessful psychotherapy and antidepressant drug treatment. She tells you that no one has been able to help her. She feels hopeless. If Janine presses the Magic Button, her depression, social anxiety, bitterness, and hopelessness will suddenly disappear, along with her urges to drink, with no effort at all, and she’ll walk out of today’s session with feelings of joy and self-esteem. Will she press the Magic Button? If not, why not? List several potential sources of Outcome and Process Resistance for each problem area below. Depression and hopelessness Outcome Resistance: Why might she be reluctant to press the Magic Button? 1. 2. 3. 4. 5. Process Resistance: What will she have to do to overcome her depression? 1. 2. * Copyright © 2009 by David D. Burns, M.D. Do not reproduce without permission.
Treating Addictions / Burns
Page 9
Bitterness, anger, loneliness, and failed relationships with men Outcome Resistance: Why might she be reluctant to press the Magic Button? 1. 2. 3. 4. 5. Process Resistance: What will she have to do to overcome her bitterness and anger? 1. 2. Alcohol abuse Outcome Resistance: Why might she be reluctant to press the Magic Button? 1. 2. 3. Process Resistance: What will she have to do to overcome the alcohol abuse? 1. 2. Social anxiety / shyness Outcome Resistance: Why might she be reluctant to press the Magic Button? 1. 2. 3. 4. Process Resistance: What will she have to do to overcome her social anxiety and shyness? 1. 2.
* Copyright © 2009 by David D. Burns, M.D. Do not reproduce without permission.
Intensive Workshop / Burns
Page 10
Healing Yourself: Therapist’s Addiction / Habit Log* Think of a habit you’re trying to change, such as overeating, drinking too much, procrastination, using drugs, or smoking. Vividly imagine you’re feeling tempted to give in. For example, picture that delicious donut. Record the tempting thoughts you’d typically have in that situation. Tempting Situation or Event:
Tempting Feelings
% Now
% After
Indicate how tempted and excited you generally feel in this situation, from 0% (not at all) to 100% (overwhelming) in the “% Now” box.
Tempting Thoughts
% Before
% After
Distortions
1.
2.
3.
4.
5.
6.
* Copyright
2001 by David D. Burns, MD. Revised, 2010.
Self-Control Thoughts
% Belief
Intensive Workshop / Burns
Page 11
Healing Yourself: Therapist’s Addiction / Habit Log (cont'd)* Tempting Thoughts
% Before
% After
Distortions
Self-Control Thoughts
% Belief
7.
8.
9.
10.
Checklist of Distortions that Trigger Habits and Addictions* 1. 2. 3.
4. 5.
All-or-nothing thinking. You think of everything that you've been putting off and tell yourself how overwhelming all those tasks will be. Overgeneralization. When you slip up, you tell yourself that you've blown your diet completely and that you'll never lose weight so you might as well give up. Mental Filter. You dwell on the positives, like how good dessert will taste, and ignore the negative consequences, like feeling guilty or bloated afterwards. Discounting the Positive. You tell yourself that any little thing you do today would only be a drop in the bucket. Jumping to Conclusions. You jump to conclusions not warranted by the facts. Mind-Reading: You may assume that other people don't have to struggle with temptations, or that people who do abstain have drab, unfulfilling lives. Fortune-Telling: You tell yourself that if you take that drink, you'll feel great and all your problems will disappear. Or, you may tell yourself, "I'll just have one drink" or "one bite," but you've never stopped at just one drink or bite in the past.
* Copyright
6.
Magnification or Minimization. You blow things out of proportion: "This ice cream will taste so good!" 7. Emotional Reasoning. You tell yourself, "I'll clean my desk (or start my diet) when I'm more in the mood. I just don't feel like it right now." 8. Should Statements. You tell yourself, "I've had a hard day. I deserve a drink (or a nice dish of ice cream)." After you give in, you tell yourself, "I really shouldn't have slipped up." This makes you so guilty and anxious that you eat or drink even more. 9. Labeling. When you slip up, you tell yourself, "I'm such a fat pig." Then you get so upset that you decide to eat three more donuts. 10. Self-Blame and Other-Blame. You find fault with yourself, other people, or the world. Self-blame: You blame yourself for giving in to temptation. This makes you feel angry, frustrated, and guilty. Other-blame: You may tell yourself that you have "fat genes" or that it's unfair that you have to struggle with your weight. You insist that others can eat whatever they want and still be thin, so you should be able to do the same thing.
2001 by David D. Burns, MD. Revised, 2010.
Treating Addictions / Burns
Page 12
Relapse Prevention Daily Mood Log: Addiction* Upsetting Event: Gave in to the urge to start drinking again (or using drugs, or binging, etc.) Emotions
% Now
% Goal
% After
Emotions
% Now
Sad, blue, depressed, down, unhappy
90
Embarrassed, foolish, humiliated, self-conscious
100
Anxious, worried, panicky, nervous, frightened
100
Hopeless, discouraged, pessimistic, despairing
100
Guilty, remorseful, bad, ashamed
100
Frustrated, stuck, thwarted, defeated
100
Inferior, worthless, inadequate, defective, incompetent
100
Angry, mad, resentful, annoyed, irritated, upset, furious
100
Lonely, unloved, unwanted, rejected, alone, abandoned
75
Other
Negative Thoughts (NTs)
% Now
1. I just can’t control myself. I’ve blown it completely.
100
2. I shouldn’t have given in.
100
3. I might as well give up. Things are hopeless.
100
4. I was just fooling myself when I thought I could stop drinking.
100
5. I really am a worthless loser.
100
6. I knew the treatment (or AA, etc.) wouldn’t work.
100
% After
Distortions
Positive Thoughts (PTs)
% Goal
% After
% Belief
ection
rea
a e
"Additional" Chapters that didn't make it into the book "Feeling Great"
Endin
a its and Addictions
a e
Chapter 32. Ending Habits and Addictions— Binging, Drinking, Gambling, Pot, Porn, Procrastination, Drugs, Cell Phones, Shopping, Video Games and more Have you been struggling to overcome a bad habit or addiction? Most of us have. According to the Centers for Disease Control and Prevention (CDC), nearly 40% of the American population is obese. In addition to binging and overeating, common habits and addictions include •
drinking
•
smoking / vaping
•
drugs, including marijuana
•
gambling
•
procrastination
•
cell phones
•
social media
•
internet surfing, shopping
•
video and computer games
•
nail biting
•
sex addictions / internet porn,
•
having affairs.
Research studies on treatment or self-help programs for habits and addictions are not terribly encouraging. For example, although we all know someone who has lost weight, we know way more people who are overweight. As many as 50% of individuals who enter weight loss programs, or more, drop out, and many of those who initially lose some weight eventually gain it back, and 70% of people who enter primary residential programs for substance use disorder relapse almost immediately upon discharge. The results of research studies on just about any habit or addiction are no better. You can probably attest to this yourself if your own efforts to change have not been overly successful. I think I know why treatments for habits and addictions fail, and I think I know why you’re also feeling stuck—if that’s the case. I’ll show you, using the problem of binging / overeating. However, the same considerations will apply to any habit or addiction. There are three main reasons why you’re likely to fail in your struggle with any habit or addiction. 1. Advantages of the Habit / Addiction. Your habit or addiction is probably immensely rewarding, and the reward is usually immediate. For example, if you like to binge and overeat, it’s really soothing or even fun to binge on your favorite foods, especially if you’re feeling down, bored, anxious or hungry. And the very moment that tasty food hits your tongue, you experience immediate pleasure. Am I right?
Endin
a its and Addictions
a e
For example, you may eat when you’ve had a hard day and feel like you deserve a reward—eating gives you a little something to look forward to. In fact, eating may be the most pleasurable or greatest reward you have in your life. In fact, eating and binging may be your only true pleasure in life. In addition, we’re constantly tempted with incredible, delicious foods. We see tasty burgers in television ads, seductive foods temptingly arranged at the grocery store, and neon signs of restaurants, bakeries and fast food joints that are just about everywhere when you’re driving your car. The desire to eat is a core and overwhelming biological drive. My wife and I live near the woods, and there are quite a few wild animals around our house, especially deer, whom we love. We have apple trees and I’m always giving them apples. They really appreciate it! Do you know what the deer and other animals spend almost all of their waking time doing? Eating or searching for food. The deer are always looking for something to nibble on. The drive for food in humans is just as strong. In fact, the drive to eat is inherent in all living creatures. There are lots of other benefits of overeating, too. If you’re overweight, you may be subconsciously (or consciously) putting up a wall to ward off people who might be otherwise attracted to you. This may keep you safe, especially if you’ve been hurt, rejected, or abused by someone you loved and trusted in the past. I totally support you if this is one of your motives for overeating. It makes sense and it works. The drive for safety and protection is just as intense and basic as the drive to eat. Here’s another possible benefit. If you binge in secret, as many people do, it’s something special that you can enjoy by yourself, without having to rely on socializing with other people, and without having to risk judgment. 2. Disadvantages of Change. The positive benefits of your habit or addiction are magnified by the many disadvantages of trying to change. Giving up any habit or addiction is a tremendous pain in the butt. For example, if you want to lose weight, you’ll have to diet or cut way down on the amount you eat. You’ll also have to increase your daily exercise. Face it--that’s NO FUN! For most of us, dieting and exercise suck! It’s WAY more fun to watch TV and munch on crunchies. Why in the world would you ever want to trade the joy and gratification of binging for misery, discipline and deprivation? That’s not a good trade-off! And even if you do bite the bullet and succeed through enormous sacrifice in losing some weight, you’ll probably just gain it back later on. So, what’s the point? Finally, if you give up your habit of overeating, you may experience real grief, despair and pain because of the loss of the most supportive relationship in your life—your relationship with food that has provided security, safety, and comfort.
Endin
a its and Addictions
a e
3. Core Values. You probably haven’t thought of this, but your habit or addiction is probably an expression of your core values and shows things about you that are positive, beautiful, or even awesome. How can this possibly be? Well, if you like to binge it could show that you’re an individual, a non-conformist or rebel who doesn’t have to conform to society’s values of how people should look and behave. That’s cool in my book! Your binging may show that you want to pamper and comfort yourself when you’re upset. In fact, feeding yourself the foods you love could be thought of as a form of self-love. Eating without inhibition also shows that you view life as a kind of celebration of our existence and amazing resources. And finally, if someone is criticizing you or trying to sell you on dieting and losing weight, you can resist them and show that you’re not going to give in or let them control you. You can let them know who’s the boss and show them that you don’t have to give in to everything that people tell you to do. Are we on the same page, more or less? Now can you see why you might be failing in your own efforts to overcome your own habit or addiction? We often think of our habits and addictions as “bad” habits, or weaknesses we’ve got to “overcome” through increased “will-power” or greater self-discipline. But in reality, there are tons of really good things about our so-called “bad” habits. If you like what I’m saying, and you’re interested in learning more, I’ve got some pretty cool tools to share with you. These will probably not be the kinds of tools you’ve heard about. But I can assure you of one thing. I won’t be trying to persuade you to change! Let’s see if you want to change. On page 7 you’ll find the Positive Reframing Table for Habits and Addictions. I also called this the “Triple Paradox.” Here’s how you use it. First, select any habit that you think you think you might like to change, something that’s been bothering you. It’s okay if you’re on the fence and have mixed feelings about giving up your habit or addiction. Some apprehension, anxiety, and ambivalence are completely normal and to be expected. Start out by listing the Advantages, or benefits, of your habit or addiction in the left-hand column. You’ll find that there are many! Let’s start with drinking. Here are just a few of the many benefits. Drinking— 1. Can be relaxing. 2. Can be fun. 3. Can be a great reward after a difficult and challenging day. 4. Can be an escape from anxiety, stress, conflict, and anger. 5. Can be a great way to tune out annoying people and situations. 6. Can make it easier to hang out with others, especially if you’re socially anxious. 7. Can make parties and holidays like Thanksgiving or New Year’s Eve more fun.
Endin
a its and Addictions
a e
8. Can make watching sporting events more fun—hanging out with friends who drink, tailgating, even watching TV! 9. Can help you fit in with friends, family or colleagues who drink. 10. Can lower your inhibitions and make it easier to be wild and take risks. 11. Can make sex more likely and way more exciting. 12. Is really easy. 13. Can be tasty, especially if you have your favorite drink! 14. Is totally legal. I’ll give you another example, but I have to warn you that this example may be disturbing, especially if you have strong religious beliefs. Please be assured that my goal is not to upset or anger you. I’m not preaching or taking a moral or religious stance on this or any addiction—I’m just trying to be realistic. Let’s say that you’re addicted to internet porn. What are some of the benefits? There may be quite a few potential advantages of your addiction, including: 1. Internet porn can be incredibly exciting. 2. It’s available any time you’re horny. 3. It’s free if you avoid paid sites or services. 4. It’s quick and easy. 5. You don’t have to get entangled with other people in acting out your sexual fantasies. That could be disturbing or dangerous. 6. You can indulge any conceivable fantasy you have. 7. You won’t be judged. 8. You can watch attractive, sexy people doing wild and exciting things. 9. You can feel normal, since millions of people are probably doing the exact same thing as you, even though they usually don’t talk about it. 10. You will have a convenient sexual outlet, especially if you’ve had trouble developing a good sexual relationship with someone you love. 11. It’s anonymous. I hope it was okay to list these things! They are all super-strong motivating forces. If you try to deal with this habit without taking these factors into account, I don’t think your efforts to change are going to be effective. Next, list the Disadvantages of giving up your habit or addiction in the middle-hand column. You’ll find there are many! For example, if your habit is excessive cell phone use, the disadvantages of cutting down might include: 1. Feeling lonely
Endin
a its and Addictions
a e
2. Having to ignore your friends 3. Having to do schoolwork or other things that make you feel anxious and insecure 4. Hurting peoples’ feelings 5. Feeling lost or anxious 6. Not finding out about what’s going on 7. Missing important messages. 8. Feeling bored or having too much down time. Finally, list all the things that your habit or addiction says about you that’s positive and awesome in the right-hand column. You’ll find there are many. For example, let’s say you’re addicted to playing video games until late at night, and your parents are desperately trying to get you to stop and do your homework. What does your video gaming show about you that’s totally awesome? Here are a few possibilities. Playing video games shows that 1. You love to have fun. Too many people are workaholics, slaving away at things endlessly without really enjoying life. 2. You’re a rebel, marching to the beat of your own drum, like Bill Gates who dropped out of college to do his own thing. 3. You’re competitive, persistent, and committed to trying over and over until you win. That’s a lot like Thomas Edison who persisted in his efforts to create the light bulb. He failed over and over and over and didn’t give up until he got it right! 4. You want to follow your passion in life. You are doing what turns you on, the thing you love the most. Motivational speakers often claim that following your passion takes enormous courage and is the ultimate secret of success. 5. You want to connect with others who also love video games. Paradoxically, your video gaming shows how much you value relationships with others. 6. Video games are a great escape from uncomfortable and awkward social and professional situations. 7. Video games provide a great escape from boredom and loneliness. 8. Video games are way more fun than having to do homework or going to bed! These are just examples, and your own details will be radically different. In addition, make sure you fill out the three columns for one habit or addiction. I’ve used three habits just to give you a feel for how this method works. Do it now. List your habit / addiction at the top and fill in the three columns. Do this on paper, and not in your head. When you’re done, you can continue reading. Thanks!
Endin
a its and Addictions
a e
Positive Reframing Table for Habits and Addictions* Describe the habit / addiction you want to change:
Your habit or addiction it can be almost anything—overeating, drugs or alcohol, cell phone use, internet surfing, buying things on sale, shoplifting, procrastination, internet porn, having affairs, smoking, biting your nails, etc. Advantages What are some benefits of this habit / addiction? 1. 2. 3. 4. 5. 6. 7.
Disadvantages What are the disadvantages of trying to change or give up this habit / addiction?
Core Values What does this habit / addiction say about you and your values that’s positive and awesome?
Endin
a its and Addictions
a e
How did you do? Did you fill out the three columns of the Positive Reframing Table? If the answer is no, then we may have our answer already. Right now, you may not have the motivation to change. You can keep reading out of curiosity if you like, but at least for the moment, you seem to be on the fence, at best, about giving up your own habit or addiction. I get it! This is not a trick, and I’m not trying to manipulate you. I don’t want to tell you, or anyone, what to do or what not to do, or how to live your life. In fact, the whole point of the Positive Reframing Table is to highlight all the really GOOD reasons NOT to change. Therapists, family members, and physicians typically use the opposite strategy. They use facts, persuasion or logic in an attempt to get people give up their habits and addictions. For example, your physician might try to sell you on the dangers of obesity, like increased risk for diabetes, high blood pressure, and other medical problems. Although this approach may be helpful to some people, it often doesn’t work, and may even make the problem worse. When people try to sell me something, I have a pretty strong urge to push back. Do you feel that way, too? Now, let’s assume that you did fill out the Positive Reframing Table, and you’ve listed lots of reasons NOT to change. Are you still looking for some help? If so, that’s pretty cool, and I’d like to hear more. Why in the world would you want to give up a habit or addiction that may be intensely rewarding to you? List your reasons here. Tell me why you want to change. And if you don’t want to change, this is an exercise that you DON’T have to do!
Endin
a its and Addictions
a e
If you DID that written exercise, and argued that you DO want to change, then I’ve got some interesting next steps for you that I think you’ll enjoy. Imagine that you’re in a really tempting situation. Let’s say you’ve been drinking a lot every evening when you get home from work. Typically, you go right to the refrigerator and see a nice chilled bottle of your favorite kind of beer, with droplets of perspiration, just like the bottles you see in television advertisements for beer. Let’s imagine, too, that you’re tired and exhausted, and your favorite sports team is about to play an important game on television. Your mind might be flooded with Tempting Thoughts like these: 1. Oh, that bottle of beer looks so good! 2. I deserve a beer. I’ve had a hard day. 3. Mmm. It will taste SO GOOD! It looks so cold and delicious! 4. I’ll feel a lot better after I have a beer or two. 5. I’ll just have a couple, that can’t hurt. 6. The game on TV will be so much more fun if I can relax with a few beers. 7. My wife is always nagging me and trying to control me. I don’t have to let her tell me what to do! 8. I won’t drink tomorrow. 9. It’s not fair that I have to be the only person not drinking while watching the game. 10. No one will see me, so it doesn’t count. Of course, your own Tempting Thoughts will be different, but I think you can get the basic idea. Briefly describe your own tempting situation at the top of the Habits and Addictions Log on page 10. Then list your own Tempting Thoughts in the left-hand column. You can continue on page 11 if you need more room. At the bottom of the Habits and Addictions Log on page 11, you’ll find my list of 10 positive distortions. These positive distortions are the mirror images of the 10 negative distortions I created for my first book, Feeling Good. For example, when you walk past your favorite bakery, you may have Tempting Thoughts like these: •
“Those donuts smell SO GOOD!” This is an example of Magnification. The donuts do smell and taste good . . . but are they that good?
•
“I’ll just have one little bite.” This is an example of Fortune-Telling and Discounting the Negative, because you’re making an unrealistic positive prediction. You’re also ignoring lots of data---in reality, you’ve rarely or never stopped after “one little bite.”
• “One donut can’t hurt! I’ll have a really small dinner tonight anyway.” More FortuneTelling—you may end up binging on several donuts.
Endin
a its and Addictions
a e
a its and Addictions o Describe the Tempting Situation:
Tempting Thoughts
Distortions
Loving Thoughts
1.
1.
2.
2.
3.
3.
4.
4.
5.
5.
Continue on next page
* Copyright © 2001 by David D. Burns, M.D. Adapted for Addictions and Habits. Revised, 2006.
Endin
a its and Addictions
Tempting Thoughts
a e
Distortions
Loving Thoughts
6.
4.
7.
5.
8.
6.
Checklist of Positive Distortions that Trigger Habits and Addictions* 1. 2.
All-or-nothing thinking (AON). You think of everything that you've been putting off and tell yourself how overwhelming all those tasks will be. Overgeneralization (OG). When you slip up, you tell yourself that you've blown your diet completely and that you'll never lose weight, so you might as well give up.
3.
Mental Filter (MF). You dwell on the positives, like how good dessert will taste, and ignore the negative consequences, like feeling guilty or bloated afterwards.
4.
Discounting the Negative (DN). You tell yourself, "I'll just have one drink" or "one bite," but you've never stopped at just one drink or bite in the past.
5.
Jumping to Conclusions (JC). You jump to conclusions not warranted by the facts. • Mind-Reading (MR): You may assume that other people don't have to struggle with temptations, or that people who abstain have drab, unfulfilling lives. • Fortune-Telling (FT): You tell yourself that if you take that drink, or smoke some pot, you'll feel great and all your problems will disappear. Or, you tell yourself that getting started on the task you’re putting off will make you incredibly anxious.
6.
Magnification or Minimization (MAG / MIN). You blow things out of proportion: "This ice cream will taste so good!" 7. Emotional Reasoning (ER). You tell yourself, "I'll clean my desk (or start my diet) when I'm more in the mood. I just don't feel like it right now." Or, “I’m feeling a bit tired, so I don’t have to start cleaning the garage right now.” 8. Should Statements (AH). You tell yourself, "I've had a hard day. I deserve a drink (or a nice dish of ice cream)." After you give in, you tell yourself, "I really shouldn't have slipped up." This makes you so guilty and anxious that you eat or drink even more. 9. Labeling (LAB). When you slip up, you tell yourself, "I'm such a fat pig." Then you get so upset that you decide to eat three more donuts. Or you tell yourself, “I’m a procrastinator.” This gives you a good reason to procrastinate! 10. Self-Blame and Other-Blame. You find fault with yourself, other people, or the world. • Self-blame (SB): You blame yourself for giving in to temptation. This makes you feel angry, frustrated, and guilty. • Other-blame (OB): You may tell yourself that you have "fat genes" or that it's unfair that you have to struggle with your weight. You insist that others can eat whatever they want and still be thin, so you should be able to do the same thing.
* Copyright © 2001 by David D. Burns, M.D. Adapted for Addictions and Habits.
Revised, 2006.
Endin
a its and Addictions
a e
Positive Distortions trigger habits and addictions, but also play a key role in mania, narcissism, relationship problems, and violence. Positive distortions are more difficult to challenge than negative distortions because they are instantly rewarding and make you feel so good. Once you’ve recorded your own Tempting Thoughts, see if you can identify the Positive Distortions in them. You can record the distortions in the Distortions column, using abbreviations, like this example: Tempting Thoughts
Distortions
1. Oh, that bottle of beer looks so good! It looks just like those gorgeous frosty bottles of beer you see in TV ads!
MAG; ER; FT
1.
ER; SH; OB
2.
ER: SH
3.
2. I deserve it! I’ve had a hard day! 3. I just can’t resist it!
Loving Thoughts
Once you’ve listed the distortions in your Tempting Thoughts, see if you can combat them with Loving Thoughts in the right-hand column. Here’s an example. Tempting Thoughts
Distortions
Loving Thoughts
1. Oh, that bottle of beer looks so good! It looks just like those gorgeous frosty bottles of beer you see in TV ads!
MAG; ER; FT
1. Well, I’ve given in to the urge to get plastered just about every night for quite a while now. I think I’ll skip the beer tonight and get a really good night’s sleep for a change.
ER; SH; OB
2. I do deserve some fun and pleasure. I also deserve a break from drinking, so I can get a good night’s sleep and not wake up with a hangover. I’ll like myself a whole lot more in the morning if I skip the beer tonight. Besides, watching the game will be just as fun without the beer. I usually just fall asleep when I’m drinking.
2. I deserve it! I’ve had a hard day!
It shouldn’t be hard to come up with convincing thoughts for the right-hand column. But you and I both know that this written exercise probably won’t be enough to help you when you’re tempted. It’s a good first step, but we’re going to need something more powerful. Now for the cool part. Ask a friend or family member (or your therapist if you’re in treatment) to help you with a Devil’s Advocate role-play. Here’s how it works.
Endin
a its and Addictions
a e
Ask the other person to play the role of the Devil and tempt you to give in to the urge to drink, overeat, gamble, procrastinate, buy something on sale—whatever your Tempting Thoughts happen to be. Your friend can read your tempting thoughts out loud, using the second person, “You,” as seductively and persuasively as possible. For example, your friend, in the role of the Devil, might say, “You deserve a drink! Mmm. It would taste so good, and you’ve had a hard day!” Make sure she or he says it with gusto, with a genuine attempt to tempt you into caving in. Now you can try to defeat or crush the tempting thought, as forcefully as possible, speaking in the first-person, “I.” Don’t look at what you wrote down on paper, just do it spontaneously. The dialogue might go like this: Devil (played by your friend): Oh, that bottle of beer looks so good! It looks just like those gorgeous frosty bottles of beer you see in TV ads! You: It sure does, but I’m going to pass. Devil (played by your friend): Pass? That’s ridiculous. You deserve all the beers you want! You’ve had a hard day. Just think of how good it will taste. Mmm! You: Yes, but I deserve a good night’s sleep, too. When I get plastered, I have a terrible time sleeping and I wake up feeling lousy. Devil (played by your friend): But it will taste SO GOOD! And it looks so cold and delicious! You: I’m sure it would taste great, but I can survive without beer tonight. Devil (played by your friend): You’ll feel a lot better after a beer or two. You: That’s true, but it won’t be all that wonderful, and I’ll feel a whole lot better in the morning if I say no. Devil (played by your friend): You can just have a couple of beers, that can’t hurt. You: That’s not really true. I never stop after a couple beers. In fact, I usually keep drinking until they’re all gone. But I’m not going to do that tonight. Tonight, the answer is NO. Devil (played by your friend): The Monday night football game on TV will be so much more fun if you relax with a few beers. You: It won’t really be that much better, and to be honest, I’ll probably jut pass out and miss most of the game if I start drinking. In reality, I’ll enjoy it more if I don’t drink. And the urge will pass fairly quickly if I just say no. So, my firm and final answer is NO! Devil (played by your friend): But your wife is always nagging you and trying to control you. You don’t have to let her tell you what to do! Don’t be such a pussy. Be a man! You: A man can love his wife. I don’t have to fight her all the time. She’s genuinely concerned about my drinking. If I don’t give in to the urge to drink, I think she’ll be
Endin
a its and Addictions
a e
really proud of me. And that could be pretty cool, too. That’s how it works. You can record the Devil’s Advocate role-play on your cell phone so you can listen to it again from time to time when you get tempted. This is important. There are two keys to the success of the Devil’s Advocate Technique. First, if you can’t soundly defeat one or more of the tempting thoughts, it means you haven’t yet decided to change. Don’t ask your friend to help your or bail you out when you’re stuck. If you want to change, you will find a way to defeat all of your tempting thoughts on your own. If someone else tells you what to say, they’re “helping,” and that will only make things worse. In addition, make sure your friend really tries to seduce you with your Tempting Thoughts. He or she should verbalize them as seductively as possible, trying to break you down, trying hard to make you give in to the temptation. Otherwise, this technique won’t be effective, because the other person will be secretly trying to “help.” The effort to “help” people with habits and addictions is the cause of nearly all therapeutic failure. What can you do if you don’t want to role-play with a friend because you find it too embarrassing? Well you can still do the role-play with yourself, and you can use your cell phone for recording. First, play the role of the Devil and really try to tempt yourself by reading your tempting thoughts, one by one, using the second person, “You.” Then see if you can defeat the temptation, speaking in the first-person, “I.” Once you’ve beaten down all your tempting thoughts, you’ll be good to go. That’s about it. So, what comes next? I won’t tell you what kind of diet or exercise program to adopt, or what strategies you should use to defeat any other habit or addiction, for that matter. There are tons of tips and suggestions out there. If you’re motivated, you can find plenty of reasonable recommendations on the internet, and you can make any of them work for you if you’re motivated. But if you’re not sufficiently motivated, nothing is going to work. Motivation is the whole ball game, to be honest, and that’s what we’ve focused on in this chapter. If you’re determined to change, you will be successful! Still, there are a few additional general principles or tips that may be helpful to you. Stimulus Control No one can resist every impulse on every occasion, so if you’re constantly tempted, you’ll probably eventually give in. This is just common sense, not rocket science. Stimulus control simply means that you avoid putting yourself in danger. For example, if you’re trying to give up alcohol, could you get rid of all the alcohol in your house? Could you throw your current supply away? Then you won’t gaze with yearning as you stare at
Endin
a its and Addictions
a e
your favorite bottle of wine until you give in to the urge to open one it and pour yourself a lovely glass of wine. It’s the same with food. If you binge on ice cream after dinner, could you get rid of the ice cream in the freezer? And could you decide not to buy more when you’re at the grocery store? Because if you buy it, you’ll eat it. And don’t buy groceries when you’re hungry, either, because you’ll give in to the urge to buy the very foods you’re trying to avoid. If you want some ice cream after dinner, drive to the local ice cream store and buy a single scoop of your favorite ice cream and enjoy it. That way you won’t be sitting at home binging on vast quantities of ice cream after dinner. Replenish your Motivation We know that motivation can fluctuate faster than the stock market during a crash. Let’s say that you’ve been doing great for a while, and you’ve defeated your habit or addiction. It’s extremely likely, even a certainty, that powerful temptations will start creeping back into your mind sooner or later. Go back to the chart you filled out on page 7. Review what you wrote down and add to it if you like. Then ask yourself why in the world you’d want to continue on the straight and narrow? If you decide that you no longer want to stick with abstinence, that’s okay. Our problem is solved because you’ve decided what you want to do! Sometimes that decision will be okay, but sometimes it can be disastrous. A dear colleague who specializes in the treatment of addictions just informed me that a fellow he once knew in AA recently had a “slip” after ten years of continuous sobriety and drank himself to death. If, in contrast, you find that you still want to change, review what you wrote down on the Habits and Addictions Log on pages 10 and 11, and add to it if you want. For example, you may have some new tempting thoughts like these: •
I did a great job giving up beer (or dieting, etc.) for several days, so now I deserve to have a drink again.
•
I don’t want to be abstinent forever. I can just drink a little from time to time and that will make life way more fun.
•
It’s unfair that I should have to stop drinking entirely. Other people can drink, so why can’t I?
•
I’ve proven that I can stop drinking, so I don’t have to keep proving the same thing over and over again. And there’s a great game on TV tonight, too!
Endin
•
a its and Addictions
a e
Life sucks without alcohol.
Now identify the distortions in these Tempting Thoughts and challenge them by putting Loving Thoughts in the right-hand column of the Habits and Addictions Log. Finally, ask your friend to do the Devil’s Advocate Role play again, or listen to the recording you made when you did it the first time, or make a brand-new recording, role playing with yourself on your cell phone. Reach Out for Support and Help Habits and addictions can be very challenging, and there’s no rule that says you have to fight every battle on your own. There’s no shame in asking for help. Some people are unable to meet their goals without ongoing support and help, no matter how strong their desires to change may be. You can google 12-step programs as well as other types of support groups in your area for every conceivable habit or addiction. Alcoholics Anonymous has had a proven track record of providing free and compassionate help for enormous numbers of people for generations, and it’s just one of many programs out there. You’ll find support groups for overeaters, sex addictions, narcotics, gambling, smoking, and more. And psychotherapists or certified addiction counselors can also make a huge difference, of course! My main message is not to give up hope. Finding the right combination of professional and community support can be the key to success. Thanks so much for reading this chapter and checking out some of the new and rather different techniques I’ve developed to help combat habits and addictions. I hope you found them interesting and maybe even helpful. Let me know! Still on the Fence? In case you’re still unsure about giving up your habit or addiction, I have one more incredible tool for you. I believe it’s the most powerful tool ever developed for the treatment of habits and addictions. You can read about it in the very next chapter!
i icu t
ecisions
a e
Chapter 33. How to Make Difficult Decisions Indecisiveness about giving up habits and addictions is universal and totally understandable. There may be extremely strong reasons to change, along with overwhelming and powerful reasons not to change. It’s like the war of the worlds! I've developed an innovative method to help get unstuck and resolve your ambivalence. It's called the Decision-Making Tool. It can be tremendously illuminating when you're faced with a difficult decision. It will show you exactly why you've been stuck on the horns of a dilemma and will often help you decide what you really want to do. Take a look at the Decision-Making Tool on page 18. It might look a bit intimidating at first, but it’s not actually hard to use, it just seems that way the first time you use it because there are many little steps. Once you get used to it, you’ll find that it’s powerful and really easy, and you can use it for all sorts of difficult decisions, and not just decisions about habits and addictions. It does require a little bit of adding and subtracting—calculations that are about at the fourth and fifth grade level of difficulty. In addition, you’ll have to follow the instructions carefully, in a step-by-step manner, without rushing. That way you won’t get confused, and you’ll have a nice reward when you’re done! I’m sure you’ll find the effort worthwhile. The Decision-Making Tool is incredibly illuminating and may even save your life. For right now, we’ll just focus on its use in the treatment of habits and addictions. At the end of the chapter, I’ll show you how you can use the same tool for any difficult decision involving relationships, school, work, or just about anything. When I’m working with anyone asking for help with a habit or addiction, this is the tool I use first. It can be tremendously helpful. The purpose of the Decision-Making Tool is not to tell you what to do, but to show you what the most important issues are, and how they balance off against each other in your mind. This insight can help you decide what you really want to do. Step 1. Options The first step when you're trying to make a difficult decision is to list all your options. People often get stuck because they're trying to decide between two options. In fact, there may be many options. As a first step, list as many options as you can think of. Let’s start with a pretty common problem, overeating or binge eating, and you want to lose some weight. The first option will usually be what you’re already doing. Then, list some options. There will nearly always be lots of possibilities. Here are some possible options.
Page 17
Decision-Making Tool Option
Describe
Total Points
A B Advantages of Option A
9
Disadvantages of Option A
1
2
10
5
7
6
8
11
3
4
12
Disadvantages of Option B
Advantages of Option B
Page 18
i icu t
ecisions
a e
1. (the status quo) Eat as much as I want of whatever I want whenever I want, with no exercise. 2. Eat whatever I want but start exercising. 3. Severe calorie restriction with intense daily exercise. 4. Modest calorie restriction with modest exercise several times per week. 5. Low carb diet. 6. Caveman diet. 7. Healthy eating choices plus exercise without dieting. 8. Join a local overeaters anonymous group. 9. Try one of the weight loss programs advertised on television. 10. Do a seven-day juice cleanse. There’s nothing special about this list, and your list of options will be different from the one on this list. Let’s say you want to start out by comparing the first two options. You can call them Option A and Option B and list them at the top of the Decision-Making Tool, like this. Decision-Making Tool Option
Describe
A
Eat as much as I want whenever I want.
B
Eat as much as I want but start exercising.
Total Points
Now you’re ready to start your analysis. How would you do this for a problem like excessive drinking? A man named Tyrone told me that he’d been drinking fairly heavily every night. He said it was fun but interfered with his sleep and he woke up feeling tired and hung over. His wife had been complaining that he was no fun because he got drunk and passed out every night when he came home from his work as a welder. Tyrone’s drinking started out with a couple of beers several times a week, but now he says he’s drinking many beers pretty much every night. And on weekends, he usually starts drinking in the middle of the afternoon. His wife has been critical of him, and says he passes out each night. His doctor warned him that his liver enzymes were high, and he totaled his car one night when he was drunk. Here are five possible options he listed. 1. Keep drinking—as much as I want whenever I want. 2. Give up alcohol entirely—total abstinence. Do it on my own. 3. Join AA or another support group and try for total abstinence. 4. Go to an addiction counselor for help. Page 19
Difficult Decisions
Page 20
5. Controlled drinking / social drinking. I could try to limit the amount I drink without giving up alcohol entirely. The last option is an appealing fantasy for many people who have succumbed to heavy drinking, but it doesn’t work for many people who simply cannot drink in a controlled or moderate way. That’s because no matter how strong your intentions might be, once you start to drink, your inhibitions will go down and you’ll give in to the urge to drink more. . . and more! I asked Tyrone to choose the two best options from his list. He decided to compare the status quo with total abstinence, so he listed these as Option A and Option B at the top of the Decision-Making tool, like this. Decision-Making Tool Option
Describe
A
Drink as much as I want whenever I want.
B
Stop drinking entirely and see if I can do it on my own.
Total Points
As you can see, Step 1 isn’t very hard. All you have to do is list some options and put two that are reasonably appealing at the top of the Decision-Making Tool. As you’re about to see, the other steps aren’t difficult, either. Step 2. Advantages and Disadvantages of Option A Once you’ve selected your options, list all the advantages and disadvantages that you can think of for Option A on the top-half of the form. As you can see on page 21, Tyrone listed the many advantages for Option A, “drinking as much as I want,” in the upper lefthand quadrant of the Decision-Making Tool. Of course, the benefits of your habit or addiction will be quite different. This is just to show you how it works. When you list the Advantages of your own habit or addiction, you’ll need to be brutally honest, just like Tyrone. After all, there will be tremendous benefits of almost any habit or addiction, and if you don’t list them all, this tool won’t be effective. Next list the Disadvantages of Option A in the upper right-hand quadrant of the form. Again, try to be completely honest with yourself, since there will usually be many. You can see Tyrone’s list on page 21. As you can see, Step 2 isn’t very hard, either. Remember, this is not an attempt to persuade you to change. I’m just giving you the chance to look at things from a slightly different angle, and I think you’ll find this really interesting. It’s not going to be what you think!
Page 20
Decision-Making Tool Option
Describe
Total Points
A
Drink as much as I want whenever I want.
B
Stop drinking entirely and see if I can do it on my own. Advantages of Option A
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13.
Disadvantages of Option A
Drinking is relaxing and fun. Escape from anxiety, stress, conflict, and anger. Life is hard, and drinking is my reward. Helps me fit in with friends who drink. Makes parties and holidays more fun. It’s the best thing in my life! I like “living on the edge” and being a “bad boy.” I can rebel against people who try to control me. Sporting events on TV are more fun. Drinking lowers my inhibitions. Sex is more exciting. Drinking is legal and easy. 1 I LOVE the taste of beer! 9
5
Drinking interferes with my sleep. Wake up with a hangover. Health problems, high blood pressure. I’m drinking more and more. Problems in my marriage. Wife refuses sex when I’m plastered. I pass out and don’t even see the game I’m watching on TV. How fun can that be? 8. Weight gain. When I drink, I eat! 9. Less time with kids, always drinking. 10. Not performing well at work. 11. Poor sexual functioning, impotence. 2 10 12. Impaired immune system. 13. Less time with things I love. 14. Auto accidents. 15. Social life is reduced. 16. Guilt and shame. 7 17. Feel out of control. 18. Loss of self-respect. a. 1. 2. 3. 4. 5. 6. 7.
8
6
11
3
4
12
Disadvantages of Option B
Advantages of Option B
Page 21
Decision-Making Tool Option
Describe
A
Drink as much as I want whenever I want.
B
Stop drinking entirely and see if I can do it on my own. Advantages of Option A
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13.
Disadvantages of Option A
Drinking is relaxing and fun. Escape from anxiety, stress, conflict, and anger. Life is hard, and drinking is my reward. Helps me fit in with friends who drink. Makes parties and holidays more fun. It’s the best thing in my life! I like “living on the edge” and being a “bad boy.” I can rebel against people who try to control me. Sporting events on TV are more fun. Drinking lowers my inhibitions. Sex is more exciting. Drinking is legal and easy. 1 I LOVE the taste of beer!9
5 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17.
Total Points
Better sleep. Can lose weight. 6 Better health. Increased self-esteem. More energy. Better concentration. Better marriage. 11 3 I can say I did it! Greater enjoyment of sporting events on TV. More time for family. More time for the things I enjoy. Sense of pride all day long! I LOVE the taste of beer! More sex. Make wife happy. Good role model / increased respect. Time for other pursuits and interests.
Drinking interferes with my sleep. Wake up with a hangover. Health problems, high blood pressure. I’m drinking more and more. Problems in my marriage. Wife refuses sex when I’m plastered. I pass out and don’t even see the game I’m watching on TV. How fun can that be? 8. Weight gain. When I drink, I eat! 9. Less time with kids, always drinking. 10. Not performing well at work. 11. Poor sexual functioning, impotence. 12. Impaired immune system. 2 10 13. Less time with things I love. 14. Auto accidents. 15. Social life is reduced. 16. Guilt and shame. 17. Feel out of control. 7 18. Loss of self-respect. a. 1. Have to fight cravings. 2. Anxious at social gatherings. 8 3. Irritable. 4. No fun every night. 5. Life becomes dreary. 6. Wife wins. 7. Miss the taste of beer. 12 4 8. Nothing to look forward to. 9. Feel deprived. 10. I’m giving in, I’ve lost! 11. I’ve become a goody two-shoes. 12. Can’t hang out with friends who drink, since I’ll give in to social pressures and drink. 13. Loss of my best friend! 14. Life becomes a drudgery of work and deprivation. 15. May feel controlled and resentful. 1. 2. 3. 4. 5. 6. 7.
Disadvantages of Option B
Advantages of Option B
Page 22
i icu t
ecisions
a e
Step 3. Advantages and Disadvantages of Option B Now list all the advantages and disadvantages that you can think of for Option B on the bottom-half of the form. You can see Tyrone’s lists on page 22. You might think that the advantages and disadvantages of Option B would just be the opposite of the advantages and disadvantages of Option A, but that’s only partially true. There will be some important differences as well, and that will depend on what you chose for Option B. Don’t worry about getting it “right” or listing everything. You will probably think of many more advantages and disadvantages of both options later on, and you can add them to your lists anytime. Once you've listed all the advantages and disadvantages you can think of for both options, you're ready to weigh the options against each other. This where it will start to get really interesting, but it may seem a little complicated or intimidating the first time you do it. I guarantee it will be easy if you just follow the step-by-step instructions slowly and carefully, one step at a time. You’ll see that every step will be a snap! Step 4. Advantages vs. Disadvantages of Option A Cover up the bottom half of the Decision-Making Tool with a piece of paper so you can only see the advantages and disadvantages of Option A. I want you to ignore Option B right now. Pretend, for the moment, that Option B does not exist. Now weigh the advantages against the disadvantages of Option A on a 100-point scale. Ask yourself whether the advantages or disadvantages of Option A are greater. Put two numbers in circles 1 and 2 that add up to 100. If the Advantages seem greater, put the higher number in left hand circle (circle 1) and the lower number in the right-hand circle (circle 2.) For example, you might put 60 in circle 1 and 40 in circle 2. If the Advantages and Disadvantages seem about the same, you can put 50 / 50 in the two circles. If the Disadvantages are greater, you can put the higher number in circle 2. For example, you might put 35 circle 1 and 65 in circle 2. Remember that one strong advantage will sometimes outweigh several less important disadvantages, or vice versa. So, it’s not about the number of items, but how meaningful they are to you. Take objective and subjective factors into account. Facts are important, but your feelings are also important. In addition, don’t obsess or worry about getting it right. You can change your weightings later on. The first time you use this tool, you can just try to get a feel for how it works without feeling like anything is written in stone.
Page 23
Decision-Making Tool Option
Describe
Total Points
A
Drink as much as I want whenever I want.
B
Stop drinking entirely and see if I can do it on my own. Advantages of Option A
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14.
Disadvantages of Option A
Drinking is relaxing and fun. Escape from anxiety, stress, conflict, and anger. Life is hard, and drinking is my reward. Helps me fit in with friends who drink. Makes parties and holidays more fun. It’s the best thing in my life! I like “living on the edge” and being a “bad boy.” I can rebel against people who try to control me. Sporting events on TV are more fun. Drinking lowers my inhibitions. Sex is more exciting. Drinking is legal and easy. 1 I LOVE the taste of beer! 9 It’s my right to drink! 50
5 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17.
Better sleep. Can lose weight. 6 Better health. Increased self-esteem. More energy. Better concentration. Better marriage. 11 3 I can say I did it! Greater enjoyment of sporting events on TV. More time for family. More time for the things I enjoy. Sense of pride all day long! I LOVE the taste of beer! More sex. Make wife happy. Good role model / increased respect. Time for other pursuits and interests.
Drinking interferes with my sleep. Wake up with a hangover. Health problems, high blood pressure. I’m drinking more and more. Problems in my marriage. Wife refuses sex when I’m plastered. I pass out and don’t even see the game I’m watching on TV. How fun can that be? 8. Weight gain. When I drink, I eat! 9. Less time with kids, always drinking. 10. Not performing well at work. 11. Poor sexual functioning, impotence. 12. Impaired immune system. 2 10 13. Less time with things I love. 50 14. Auto accidents. 15. Social life is reduced. 16. Guilt and shame. 17. Feel out of control. 7 18. Loss of self-respect. a. 1. Have to fight cravings. 2. Anxious at social gatherings. 8 3. Irritable. 4. No fun every night. 5. Life becomes dreary. 6. Wife wins. 7. Miss the taste of beer. 12 4 8. Nothing to look forward to. 9. Feel deprived. 10. I’m giving in, I’ve lost! 11. I’ve become a goody two-shoes. 12. Can’t hang out with friends who drink, since I’ll give in to social pressures and drink. 13. Loss of my best friend! 14. Life becomes a drudgery of work and deprivation. 15. May feel controlled and resentful. 1. 2. 3. 4. 5. 6. 7.
Disadvantages of Option B
Advantages of Option B
Page 24
Decision-Making Tool Option
Describe
A
Drink as much as I want whenever I want.
B
Stop drinking entirely and see if I can do it on my own. Advantages of Option A
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14.
Disadvantages of Option A
Drinking is relaxing and fun. Escape from anxiety, stress, conflict, and anger. Life is hard, and drinking is my reward. Helps me fit in with friends who drink. Makes parties and holidays more fun. It’s the best thing in my life! I like “living on the edge” and being a “bad boy.” I can rebel against people who try to control me. Sporting events on TV are more fun. Drinking lowers my inhibitions. Sex is more exciting. Drinking is legal and easy. 1 I LOVE the taste of beer! 9 It’s my right to drink! 50
5
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17.
Total Points
Better sleep. Can lose weight. 6 Better health. Increased self-esteem. More energy. 40 Better concentration. Better marriage. 11 3 I can say I did it! Greater enjoyment of sporting events on TV. More time for family. More time for the things I enjoy. Sense of pride all day long! I LOVE the taste of beer! More sex. Make wife happy. Good role model / increased respect. Time for other pursuits and interests.
Drinking interferes with my sleep. Wake up with a hangover. Health problems, high blood pressure. I’m drinking more and more. Problems in my marriage. Wife refuses sex when I’m plastered. I pass out and don’t even see the game I’m watching on TV. How fun can that be? 8. Weight gain. When I drink, I eat! 9. Less time with kids, always drinking. 10. Not performing well at work. 11. Poor sexual functioning, impotence. 2 10 12. Impaired immune system. 13. Less time with things I love. 50 14. Auto accidents. 15. Social life is reduced. 16. Guilt and shame. 17. Feel out of control. 7 18. Loss of self-respect. a. 1. Have to fight cravings. 2. Anxious at social gatherings. 8 3. Irritable. 4. No fun every night. 5. Life becomes dreary. 6. Wife wins. 60 7. Miss the taste of beer. 12 4 8. Nothing to look forward to. 9. Feel deprived. 10. I’m giving in, I’ve lost! 11. I’ve become a goody two-shoes. 12. Can’t hang out with friends who drink, since I’ll give in to social pressures and drink. 13. Loss of my best friend! 14. Life becomes a drudgery of work and deprivation. 15. May feel controlled and resentful. 1. 2. 3. 4. 5. 6. 7.
Disadvantages of Option B
Advantages of Option B
Page 25
i icu t
ecisions
a e
One other point—make sure you do this on paper. Don’t try to do it in your head. That will be way too hard! You’ll get frustrated and confused and give up! Then you’ll miss out on some potentially incredible discoveries that are awaiting you! On page 24, you can see how Tyrone weighed the Advantages and Disadvantages of Option A—drinking as much as he wanted whenever he wanted. As you can see, it was really close, so he put a 50 in circle 1 and a 50 in circle 2. If Tyrone had only done a Cost-Benefit Analysis of the Advantages vs. the Disadvantages of drinking, he would have been stuck, since there didn’t appear to be any particularly compelling reasons to quit. This is exactly why lots of people can’t seem to give up their habits and addictions. You may have some thoughts about change from time to time—giving up alcohol in this situation—but you can’t come up with any really good reasons to do that! Am I right? But there may be some surprises to come! Step 5. Advantages vs. Disadvantages of Option B Cover up the top half of the Decision-Making Tool with a piece of paper so you can only see the advantages and disadvantages of Option B. I want you to ignore Option A right now. Pretend, for the moment, that Option A does not exist. Now weigh the advantages against the disadvantages of Option B on a 100-point scale, just as you did for Option A. Put two numbers in circles 3 and 4 that add up to 100. If the Advantages of Option B seem greater, put the higher number in circle 3. If the Disadvantages seem greater, put the higher number in circle 4. If they feel about the same, you can put 50 in both circles, as Tyrone did for Option A. If you look on page 25, you see that Tyrone put 40 60 in the two circles, since the disadvantages of total abstinence clearly outweighed the advantages. Note, once again, that if Tyrone had been thinking about giving up alcohol, he never would have done so, since the option was not appealing and involved the loss of many things he greatly valued. But, as I’ve mentioned, we’re not done yet. It’s about to get more interesting. Step 6. Advantages of Option A vs. Advantages of Option B Now cover the right half of the paper so you can weigh the Advantages of Option A with the Advantages of Option B. When you do this, pretend that there are no disadvantages to either option. Simply ask yourself, "Which advantages seem greater? Which benefits feel more desirable to me?" Put two numbers that add up to 100 in circles 5 and 6. Assign the larger number to the set of advantages that feels greater. I want you to decide whether the advantages of Option A or Option B seem more rewarding, assuming there are no disadvantages to either option. Page 26
Habits and Addictions
Page 27
On page28, you can see that Tyrone decided that the advantages of Option B (total abstinence) were actually greater than the advantages of Option A (continuing to drink as much as he wanted whenever he wanted), so he put a 40 in circle 5 and a 60 in circle 6. Notice that things are beginning to shift. The previous comparisons only involved Advantages vs. Disadvantages of both options, and his motivation to stop drinking did not increase at all. But when we removed the Disadvantages from the picture, the benefits of becoming a non-drinker suddenly emerged as quite a bit stronger than expected. Next, we’ll see what happens when we remove the Advantages from the picture and focus on the Disadvantages. Keep in mind that there are no “correct” ways to weigh these options. It’s totally up to you, and everyone will weight things differently. You’re in charge. If you want, you can repeat your analyses later on and you might come to a completely different conclusion. We’ll discuss that later. Step 7. Disadvantages of Option A vs. Disadvantages of Option B Now we’ll remove the Advantages from the equation and compare the Disadvantages. This can also be interesting! Cover up the left half of the Decision-Making Tool so you can compare the disadvantages of both options. Pretend there are no Advantages for either option, and ask yourself, "Which disadvantages seem greater? Which costs feel greater to me?" Put two numbers that add up to 100 in circles 7 and 8 on the right side of the Decision-Making Tool. Assign the larger number to the disadvantages that feel the worst. As you can see on page28, Tyrone felt that the disadvantages of Option A (drinking) were significantly greater than the disadvantages of Option B (abstinence), so he put a 70 in circle 7 and a 30 in circle 8. I promised you that this would be fairly easy if you just did it step-by-step. Have I been right so far? Has anything been confusing or difficult to understand? Step 8. Total Points for Option A Now we come to the interesting part. We’re going to calculate the total score for the advantages of Option A and the total score for the disadvantages of Option A. Take a close look at the upper left-hand quadrant of the Decision-Making Tool on page 28, the area for the Advantages of Option A. You will see that the two circles in the upper left-hand corner contain a 50 (in circle 1) and a 40 (in circle 5). You’ll also see circle 9, which has not yet been filled in. Circle 9 is where you put the total score for the advantages of Option A. If you add up the numbers in circles 1 and 5 (50 + 40 = 90), you’ll have the total score for the Advantages of Option A.
Page 27
Decision-Making Tool Option
Describe
A
Drink as much as I want whenever I want.
B
Stop drinking entirely and see if I can do it on my own. Advantages of Option A
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14.
Total Points
Drinking is relaxing and fun. Escape from anxiety, stress, conflict, and anger. Life is hard, and drinking is my reward. Helps me fit in with friends who drink. Makes parties and holidays more fun. It’s the best thing in my life! I like “living on the edge” and being a “bad boy.” I can rebel against people who try to control me. Sporting events on TV are more fun. Drinking lowers my inhibitions. Sex is more exciting. Drinking is legal and easy. 1 I LOVE the taste of beer! 9 It’s my right to drink! 50
5 40 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17.
Better sleep. Can lose weight. 6 60 Better health. Increased self-esteem. More energy. Better concentration. 40 Better marriage. 11 3 I can say I did it! Greater enjoyment of sporting events on TV. More time for family. More time for the things I enjoy. Sense of pride all day long! I LOVE the taste of beer! More sex. Make wife happy. Good role model / increased respect. Time for other pursuits and interests.
Advantages of Option B
Disadvantages of Option A Drinking interferes with my sleep. Wake up with a hangover. Health problems, high blood pressure. I’m drinking more and more. Problems in my marriage. Wife refuses sex when I’m plastered. I pass out and don’t even see the game I’m watching on TV. How fun can that be? 8. Weight gain. When I drink, I eat! 9. Less time with kids, always drinking. 10. Not performing well at work. 11. Poor sexual functioning, impotence. 2 10 12. Impaired immune system. 13. Less time with things I love. 50 14. Auto accidents. 15. Social life is reduced. 16. Guilt and shame. 17. Feel out of control. 75 7 18. Loss of self-respect. a. 1. Have to fight cravings. 2. Anxious at social gatherings. 25 8 3. Irritable. 4. No fun every night. 5. Life becomes dreary. 6. Wife wins. 60 7. Miss the taste of beer. 12 4 8. Nothing to look forward to. 9. Feel deprived. 10. I’m giving in, I’ve lost! 11. I’ve become a goody two-shoes. 12. Can’t hang out with friends who drink, since I’ll give in to social pressures and drink. 13. Loss of my best friend! 14. Life becomes a drudgery of work and deprivation. 15. May feel controlled and resentful. 1. 2. 3. 4. 5. 6. 7.
Disadvantages of Option B
Page 28
Decision-Making Tool Option
Describe
A
Drink as much as I want whenever I want.
-35
B
Stop drinking entirely and see if I can do it on my own.
+15
Advantages of Option A 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14.
Drinking is relaxing and fun. Escape from anxiety, stress, conflict, and anger. Life is hard, and drinking is my reward. Helps me fit in with friends who drink. Makes parties and holidays more fun. It’s the best thing in my life! I like “living on the edge” and being a “bad boy.” I can rebel against people who try to control me. Sporting events on TV are more fun. Drinking lowers my inhibitions. Sex is more exciting. Drinking is legal and easy. 1 I LOVE the taste of beer! 9 It’s my right to drink! 90
50
5 40
1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17.
Total Points
Better sleep. Can lose weight. 6 60 Better health. Increased self-esteem. More energy. 100 40 Better concentration. Better marriage. 11 3 I can say I did it! Greater enjoyment of sporting events on TV. More time for family. More time for the things I enjoy. Sense of pride all day long! I LOVE the taste of beer! More sex. Make wife happy. Good role model / increased respect. Time for other pursuits and interests.
Advantages of Option B
Disadvantages of Option A Drinking interferes with my sleep. Wake up with a hangover. Health problems, high blood pressure. I’m drinking more and more. Problems in my marriage. Wife refuses sex when I’m plastered. I pass out and don’t even see the game I’m watching on TV. How fun can that be? 8. Weight gain. When I drink, I eat! 9. Less time with kids, always drinking. 10. Not performing well at work. 11. Poor sexual functioning, impotence. 2 10 12. Impaired immune system. 13. Less time with things I love. 125 50 14. Auto accidents. 15. Social life is reduced. 16. Guilt and shame. 75 7 17. Feel out of control. 18. Loss of self-respect. a. 1. Have to fight cravings. 2. Anxious at social gatherings. 25 8 3. Irritable. 4. No fun every night. 5. Life becomes dreary. 6. Wife wins. 85 60 7. Miss the taste of beer. 12 4 8. Nothing to look forward to. 9. Feel deprived. 10. I’m giving in, I’ve lost! 11. I’ve become a goody two-shoes. 12. Can’t hang out with friends who drink, since I’ll give in to social pressures and drink. 13. Loss of my best friend! 14. Life becomes a drudgery of work and deprivation. 15. May feel controlled and resentful. 1. 2. 3. 4. 5. 6. 7.
Disadvantages of Option B
Page 29
i icu t
ecisions
a e
As you can see on page 29, Tyrone put 90 in circle 9. You’ll be doing the same thing when you work with your own Decision-Making Tool. This is probably the hardest step, but as I promised, it is really pretty easy if you concentrate and just do one thing at a time. You can calculate the total score for the disadvantages of Option A in exactly the same way. The total score for the disadvantages of Option A is the sum of the numbers in circles 2 and 7 (50 + 75 = 125) in the upper right-hand quadrant of the form, so Tyrone put 125 in circle 10, as you can see on page 29. To get the total points for Option A, you simply subtract the total disadvantages for Option A in circle 10 (125) from the total advantages for Option A in circle 9 (80). That’s because the Advantages are positive, and the Disadvantages are negative. Do you remember from middle school how to subtract? You can do it like this: Total Points for Option A 90 -125 -35
(the advantages score in circle 9) (the disadvantages score in circle 10) Total
You can that Tyrone recorded -35 at the top of the Decision-Making Tool under the Total Points for Option A. Suddenly, Option A doesn’t look very appealing! But we’re still not done. Step 9. Total Points for Option B Now let’s see what’s up for Option B, total abstinence. We’ll go through the exact same procedure. If you look in the lower left-hand quadrant on page 29, you’ll see that the two values for the Advantages of Option B are 60 (in circle 6) and 40 (in circle 3). Tyrone added them up and put 100 in circle 11. This was the total for the Advantages of Option B. Similarly, you can see that the totals for the disadvantages of Option were 60 (in circle 4) and 25 (in circle 8). Tyrone added them up and put 85 in circle 12. This was the total for the Disadvantages of Option B. Now you can see that the total points for the Advantages of Option B are 100 (in circle 11) and the total points for the Disadvantages of Option B are 85 (in circle 12). Now, how will we get the total points for Option B? You simply subtract the Disadvantages (85) from the Advantages (100), just like we did before. Here’s the calculation: Total Points for Option A 100 -85 +15
(the advantages score in circle 11) (the disadvantages score in circle 12) Total
i icu t
ecisions
a e
As you can see, Tyrone put +15 at the top of the Decision-Making Tool under the Total Points for Option A, as you can see on page 29. Step 10. Results Now we've come to the fun, easy and interesting part. We're ready to put everything together so that Tyrone can see what option is the more desirable. All Tyrone has to do is compare the total points for Option A (-35) with the total points for Option B (+15). As you can see on page 31, Option B was clearly superior, and there were actually 50 points of separation. The beauty of this method is that what appeared to be a difficult decision turned out to be a fairly obvious one. If Tyrone had examined these options separately, without using the Decision-Making Tool, he would have concluded that there was no reason to quit and he would have kept drinking. That’s because when he initially balanced the Advantages and Disadvantages of Option A, unlimited drinking, they came out 50 / 50, so there was no compelling reason to change. And believe me, you’re NOT going to give up your favorite habit without a compelling reason! When Tyrone initially balanced the Advantages and Disadvantages of Option B, total abstinence, it came out 40 / 60, which seemed very negative. So, he’s obviously not going to give up drinking based on that comparison! Unlimited Drinking vs. Total Abstinence Option A: Drinking -35
Option B: Abstinence +15
+10
0
-10
-20
-30
-40
50 Points
i icu t
ecisions
a e
But when he completed his analysis with the help of the Decision-Making Tool, abstinence suddenly appeared to be much more desirable than unlimited drinking, which appeared like a losing proposition. The comparison of two options in context will often put things in an entirely different perspective. Remember that Tyrone has only compared the first two of the five options he listed, and there were three more, including controlled drinking, joining a support group like AA, or finding an addiction counselor. He may want to use the Decision-Making Tool again, so he can compare one of those options with the current “winner.” In addition, your thinking can change a great deal from time to time. You may think of advantages or disadvantages of your options that had slipped out of your mind. You can add them and do another analysis. This may change a lot. You’re in control, and no one is trying to trap you or sell you anything. At least, I’m not! The Decision-Making Tool is not intended to make your decision for you, and it will not show you what the single most “correct” decision is. It simply shows how you're feeling at a particular point in time and helps you sort out your options more systematically. Step 9. Interpretation When you use the Decision-Making Tool, many interesting patterns can emerge. Four of the more common patterns are: •
No Brainer / Slam Dunk
•
Can't Lose
•
Can't Win
•
Fence Sitter
No Brainer / Slum Dunk. Sometimes, one option will be strongly positive, and the other option will be strongly negative. This decision is usually easy and obvious because one of your options is way better than the other option. The total score for either option can range between -200 and +200. In Tyrone’s case, one option was mildly positive (abstinence was +15) and the other option was moderately negative (unlimited drinking was -35), so there was a 50-point separation between the two options. Although Option B was the clear winner, I would not classify this as a slam dunk because the winning score for Option B was only a little above zero. Can't Lose. Here, the total scores for both options are moderately to strongly positive. For example, the total score for one Option could be +65 and the total score for the other option could be +60. What do you do? In this case, it probably won't make any difference which option you choose because they both look good.
i icu t
ecisions
a e
For example, Tyrone did a second comparison of total abstinence with an experimental trial of controlled drinking. Controlled drinking came out +85 and total abstinence was +60—both strongly positive. So he decided to try controlled drinking for a month. It was a great experiment because he was drinking heavily by the end of the month. Based on his experience, he joined AA and stopped drinking entirely. He later contacted me and said he’d become incredibly happy, although he still felt tempted to drink from time to time, which is understandable. Can't Win. In this pattern, the total scores for both options are negative. This is the opposite of the can't lose pattern. An example would be if your total score for Option A was -75 and the total score for Option B was -40. When both scores are negative, it feels like anything you do will be bad. It seems like you can't win, no matter what you do. When both options look bad, it may be because you're depressed and distorting things in a negative way. In can't win patterns, doing a Daily Mood Log can often be helpful. You may be able to pinpoint and challenge the distortions in your thoughts about one or both options. I’ll give you an example of this in a few pages. In addition, there may be other more favorable options that you haven’t considered. Fence Sitter. In a fence sitter, the total scores for both options are around zero. In this case, neither option appears to have much to offer. There are different reasons you can end up with both scores around zero. •
High-energy impasse: In a high-energy impasse, both options have strong positive and negative consequences that balance each other out. You're excited about the benefits of both options, but you're also worried about the drawbacks of both options.
•
Low-energy impasse: In a low-energy impasse, you don't feel very strongly about the advantages or disadvantages of either option.
At the start of the chapter, I promised to show you how to use this powerful tool for any difficult decision you’ve been agonizing about. It’s not just for habits and addictions. I’ll give you a couple examples involving difficult romantic problems. I once treated a gorgeous blond woman named Irene who was engaged to a dashing, high-ranking Iranian government official. They were deeply in love, a story-book romance, but there was a problem. She was from a prominent New York Jewish family and he was a devout Muslim. In addition, he wanted her to live with him in Iran following their wedding. To make matters worse, her parents were prominent supporters of Israel. A huge wedding was planned at a posh hotel in Manhattan, but there was tension in the air. Irene came to me a month before her wedding, torn with indecision and flooded with anxiety. Although she loved her fiancé dearly, she was extremely torn by the extreme cultural and religious differences. She was also afraid of the intense
i icu t
ecisions
a e
potential political conflicts between America and Iran, and was terrified about living in Iran. I helped Irene fill out the Decision-Making Tool in the office. Option A was getting married, and Option B was breaking off the engagement. Option B came out as clearly superior. In fact, it was in the Slam Dunk territory. Irene felt enormous relief but also felt sad about calling off her wedding to the man she loved so much. I reminded her that her decision did not have to be final and suggested that she could sleep on it and use the Decision-Making Tool again in the morning to see if she came to the same decision. She called me the next morning to let me know what had happened. She explained that after sleeping on it, she decided to use the Decision-Making Tool again and it came out in the opposite direction. Getting married was a huge positive and breaking up was a huge negative. She said she’d suddenly changed her mind and decided to get married after all, and felt totally happy, excited, and at peace. This often happens when you use the Decision-Making Tool, and it's a perfectly acceptable part of the decision-making process. It will get you unstuck and move you forward, but sometimes your direction will change unexpectedly, which is fine! The Decision-Making Tool allows you to list all the thoughts and circumstances that are fueling your conflicting emotions when you’re having a hard time making up your mind. Once you figure out what advantages and disadvantages feel really true and important to you, it is often easier to make a decision and come to peace with it. I mentioned that one of the possible outcomes when you use the DecisionMaking Tool is the “Can’t Win” result. That’s when both of your options look dreadful. When both options look intensely bad, it may be because you're depressed and distorting everything in a negative way. In Can't-Win patterns, cognitive therapy can often be helpful. I once treated a man named Paul who was trying to decide whether to get divorced (Option A) or stay married (Option B). Paul had a strong desire to get divorced, so Option A had many advantages. But at the same time, Paul was convinced that his friends and family would look down on him and resent him if he got divorced, so the disadvantages of this option were also great. When he completed the Decision-Making Tool, the total points for Option A came out to be strongly negative (-125). At the same time, staying married was also strongly negative. Paul and his wife fought constantly. He was clear that he had no desire whatsoever to try to resolve their problems or get closer to her. He clearly wanted out. As a result, the total points for Option B also came out to be strongly negative (-110). When you’re in a “Can’t Win” situation, it might be because of distorted thinking about one or both options. Could it be that Paul was looking at things in an unrealistically negative manner? When Paul thought about getting divorced, he
i icu t
ecisions
a e
had this Negative Thought: "I'll lose all my friends and the respect of my family if Jennie and I get divorced." This thought contained several familiar distortions, including all-or-nothing thinking, mind-reading, fortune telling, and emotional reasoning. Although getting divorced is a disappointment and a loss, Paul didn’t have any evidence that he’d lose all of his friends if he left Jennie. Paul used the Survey Technique and told several of his closest friends that his marriage was not going well and asked what they'd think of him if he and Jennie got divorced. He was surprised to discover that several of them were also experiencing marital problems and didn't feel at all judgmental. All of them said they were aware of the situation and his unhappiness and would definitely support his decision. This was a huge relief and he use the Decision-Making Tool again. This time, it was a slam dunk for divorce, so he left his wife. Sadly, I can’t tell you that every problem has a story-book ending, or that every marriage can be saved. The Decision-Making Tool will never impose any decision on you. It will show what you want, and what will work for you. Distorted thinking is not the only reason that you might find yourself in a Can'tWin situation. When both options are negative, there will sometimes be other options you haven't considered. For example, Paul might want to consider doing some couples’ therapy with Jennie or initiating a trial separation for several months. Paul compared these options with getting divorced but decided that he really did want to leave his wife. I’ve included an additional blank copy of the Decision-Making Tool on page 36, along with a one-page summary of the instructions on page 37. If you photocopy the Decision-Making Tool so you'll have one available whenever you need it.
Decision-Making Tool Option
Describe
Total Points
A B
Advantages of Option A
Disadvantages of Option A
1
9
2
10
5
7
6
8
11
3
Advantages of Option B
4
12
Disadvantages of Option B
(Instructions on reverse)
a s
a e
Decision-Making Tool: Brief Instructions Make a list of all your options and choose the best two. Call them Option A and Option B and write them at the top of the Decision-Making Tool. Then list all the advantages and disadvantages for both options in the appropriate columns. Option A: Cover the bottom half of the sheet and think exclusively about Option A. Compare the advantages and disadvantages. Which seem greater? Put two numbers that total 100 in circles 1 and 2. If the advantages and disadvantages seem about the same, put a 50 in each circle. Option B: Now cover the top half of the sheet so you can think exclusively about Option B. Repeat the procedure you used for Option A. Put two numbers that total 100 in circles 3 and 4. Advantages Comparison: Now cover the right half of the sheet so you can compare the advantages of Options A and B. Ignore the disadvantages of each option. Put two numbers totaling 100 in circles 5 and 6. The option with the more desirable list of advantages gets the higher number. Disadvantages Comparison: Cover the left half of the sheet and concentrate on the disadvantages of Options A and B. Ignore the advantages. Put two numbers totaling 100 in circles 7 and 8. Assign the higher number to the disadvantages that seem worse. Calculations Advantages of Option A: The numbers in circles 1 and 5 are the advantages of Option A. Add these two numbers, and put the total in circle 9. Disadvantages of Option A: The numbers in circles 2 and 7 are the disadvantages of Option A. Add these two numbers, and put the total in circle 10. Total Score for Option A: Subtract the number in circle 10 from the number in circle 9. It could be a negative or positive number. Record this number at the top of the page (Total Points for Option A). It will be between -200 and + 100. Advantages of Option B: The numbers in circles 3 and 6 represent the advantages of Option B. Add them together and put the total in circle 11. Disadvantages of Option B: The numbers in circles 4 and 8 are the disadvantages of Option B. Add them together and put the total in circle 12. Total for Option B: Subtract the number in circle 12 from the number in circle 11. Record this number at the top of the at the top of the page (Total Points for Option B). It will also be between -200 and + 100. Making the Decision Compare the total points for Option A and Option B. The option with the more positive number is more desirable. •
If one option is strongly positive and the other is strongly negative, your decision is a "no brainer."
•
If both numbers are positive, this is a "can't lose" decision.
•
If both numbers are negative, it's a "can't win" decision.
•
If both numbers are around zero, it’s a “fence sitter.”
A variety of other interesting patterns may also emerge. Remember that when you use the DecisionMaking Tool, you don't have to feel trapped or locked in by the results. You can fill it out on several occasions until you feel comfortable with your decision.


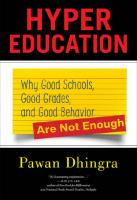
![Nanotechnology Characterization Tools for Tissue Engineering and Medical Therapy [1st ed. 2019]
9783662595961, 9783662595954, 3662595966](https://ebin.pub/img/200x200/nanotechnology-characterization-tools-for-tissue-engineering-and-medical-therapy-1st-ed-2019-9783662595961-9783662595954-3662595966.jpg)



