Therapist Toolkit
Therapist Toolkit $245.00
128 87 60MB
English Pages [805] Year 2020
Licensure Agreement
Part 1: Assessment Tools
Table of Contents for Part 1
Assessment Tests without Answer Sheets
Pre-Therapy Testing
Depression Checklist
Anxiety Inventory
Relationship Satisfaction Scale
Assessment Tests with Answer Sheets
Depression Check list
Anxiety Inventory
Relationship Satisfaction Scale
Empathy Scale
Patient's Therapy Session Evaluation
Brief Assessment Tests For Indiviuals with Disabilities
Depression Checklist - brief version
Anxiety Inventory - brief version
Relationship Satisfaction Scale
Empathy Scale
Assessing Self-Defeating Attitudes and Beliefs
The Initial Evaluation
The Final Evaluation
DSM-IV Diagnosis
Table of Contents for DSM-IV Survey
Part 2: Treatment Tools
Table of Contents for Part 2
Overview of Part 2
How to Use the Forms & Charts for Treating Mood Problems
How to Use the Forms & Charts for Treating Relationship Problems
Summary of Cognitive Therapy Interventions
THE Forms & Charts for Treating Mood Problems
The Daily Mood Log / Triple Column
Self-Defeating Beliefs
Your Thoughts and Your Feelings
Unhappy Stick Figure
Five Steps for Feeling Good
How to Use the CBA
How to Use the Pleasure Predicting Sheet
Daily Activity Schedule
Anti-Procastination Sheet
Decision Making Form
THE Forms & Charts for Treating Relationship Problems
Relationship CBA
Revise Your Communication / Relationship Journal
Memos to Orient New Patients to Therapy
Concept of Self-Help
Make Therapy Rewarding and Successful
Specialized Memos
The Anti-Hopelessness Memo
Part 3: 1997 Upgrade
Table of Contents for Part 3
In a Hurry? Read This!
Description, Scoring and Psychometric Properties
Depression
Anxiety
Anger
Relationship Satisfaction Test
Empathy & Patient Satisfaction Scales
Full Scales
New, Experimental Scales (1997)
Answer Sheets for New Scales (1997)
Chart Records
References
Appendix
Part 4: 2016 Upgrade
Assessment Tests for Adults & Teens
Assessment Tests for Children & Adolescents
Assessment Tests for Medical Settings
Cognitive Behavior Therapy Tools
Interpersonal Therapy Tools
Memos & Administrative Tools
Motivational Tools
Other - Order forms, etc.
Reading Lists
Tools for Supervision and Teaching
Tools in Foreign Languages
French
Russian
Spanish
Two-Sided Color Cards
Common Self-Defeating Beliefs
Recovery Circle
50 Ways to Untwist Your Thinking
Perfectionism CBA
Love Addiction CBA
Why People Resist Change
Blame CBA
EAR
Feeling Word Chart
12 GOOD Reasons NOT to
Bad Communication Checklist
EAR Checklist
Depression Recovery Map
Anxiety Recovery Map
Anger Recovery Map
Habit / Addiction Recovery Map
5 Steps in Agenda Setting
Writings & Excerpts
Acceptance and Commitment In CBT
Selecting the Most EffectiveTechniques for Your Patients
Interpersonal Techniques
Suicide Assessment and Prevention
Suicide Assessment Interview
Recommend Papers

- Author / Uploaded
- David Burns
- Commentary
- decrypted from 3B542D5E0676F14698E8A2D8DCBD5503 source file
File loading please wait...
Citation preview
Licensure Agreement This license gives you permission to print the materials from this PDF for use in your psychotherapy practice. The materials are intended for use only by qualified mental health professionals. This license does NOT give you the right to reproduce these materials for other purposes including research, books, pamphlets, articles, video or audio tapes, handouts or slides for lectures or workshops. Electronic reproduction is not permitted. You will need the separate Electronic Tool Package & License. Please visit www.FeelingGood.com to purchase. Reproduction on the Internet is not permitted. Permission to use or reproduce these materials for any other purpose must be obtained in writing from David D. Burns, M. D.
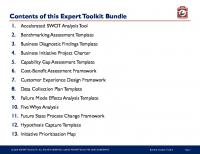
What is Included in this Therapist’s Toolkit 2020 Edition! The materials from the 400+ page 1995 Original Edition plus the upgrades from following years up until 2018. There are bookmarks for easy navigation. Look for the bookmark icon in your PDF reader app to open the navigation pane.
1995 Therapist's Toolkit Part 1 - 145 pages Assessment tools include tests for depression, anxiety, relationship satisfaction, and therapeutic empathy, along with answer sheets and scoring keys; Self-Defeating Beliefs Scale; Clinician's History form (brief and complete versions); Speedy Screening System for DSM-IV (Axes I and II); Patient's Evaluation of Therapy; and Termination Summary.
Part 2 - 129 pages Individual therapy tools include the Summary of Cognitive Interventions, Daily Mood Log with instructions, Checklist of Cognitive Distortions, Troubleshooting Guide, How to Untwist Your Thinking, Cost-Benefit Analysis (three types with instruction sheet), Daily Activity Schedule, Anti-Procrastination Sheet, and the Decision Making Form (with instruction sheet). Also included are The Concept of Self-Help Memo, How to Make Therapy Rewarding and Successful, The Anti-Hopelessness Memo, progress notes, medication records, Clinician's Data Sheet, and more. Interpersonal therapy tools include the Relationship Cost-Benefit Analysis (with instruction sheet), Revise Your Communication Style (with instructions), Good vs. Bad Communication, Bad Communication Checklist, Five Secrets of Effective Communication, Feeling Words Chart, 12 Barriers to Self-Expression, and 12 Barriers to Listening.
Part 3: 1997 Upgrade - 150 pages Includes new and improved assessment tools for: Anxiety Disorders: Generalized Anxiety Disorder, Panic Disorder, Agoraphobia, OCD, Social Phobia, PTSD Depression: Burns Depression Checklist (25-item and 5-item versions, plus assessment of suicidal urges) Relationship Problems: Relationship Satisfaction Scale (5-item version), Anger Scale, (Violent Urges Scale) Therapy Session Evaluation: Empathy Scale, Helpfulness of Session (5-item and fulllength versions) Positive Emotions: Happiness, Self-Esteem, Intimacy, Productivity, Playfulness, Freedom from Fear, Hope, Spirituality (eight 5-item scales) Self-Help Report: For tracking patients' self-help activities and psychotherapy homework Convenient Chart Records: Makes it easy to record scores and review changes over time And morel As noted, most scales come with a choice of time perspectives ("indicate how have you been feeling over the past week" vs. "indicate how you are feeling at this moment"). Many scales are available in two lengths. The full-length versions have superb reliabilities (typically 95% or better) and are suitable for comprehensive assessment. The brief, 5-item scales also have outstanding reliabilities (typically 90% or better) and are suitable for tracking symptoms on a session-by-session basis. Many scales are also formatted in large typeface to help individuals with impaired vision or reading difficulties.
Part 4: 2016 Upgrade – 376 pages The 2016 Upgrade contains 2005, 2007, 2010, and many other upgrades! It contains wonderful instruments you can use in your clinical work, including the new and improved Daily Mood Log, the new and improved Brief Mood Survey with individual and group scales, scales in Spanish, the Pain Scale, instruments for children, scales to use in medical settings, a therapy supervision scale, the 50 Ways to Untwist Your Thinking, and much more.
Plus 2016 Upgrade
2016 Upgrade Assessment Tests for Adults and Teens Assessment Tests for Children and Adolescents Assessment Tests for Medical Settings Cognitive Behavior Therapy (CBT) Tools Interpersonal Therapy (IPT) Tools Memos and Administrative Tools Motivational Tools Other – Order Forms, reading list Reading Lists Tools for Supervision and Teaching Tools in Foreign Languages Two-Sided Color Cards Writings and Excerpts from Dr. Burns Therapy Ebook
Licensure Agreement By David D. Burns, M.D.
Purchase of the Therapist’s Toolkit and / or the EASY Diagnostic System provides you with a license to photocopy the materials for use in your clinical practice. The license does NOT give you the right to reproduce these materials for other purposes including research, books, pamphlets, articles, video or audio tapes, handouts or slides for lectures or workshops. Electronic reproduction is not permitted. Reproduction or illustration on the Internet is not permitted. The Therapist’s Toolkit and EASY Diagnostic System are intended for use only by qualified mental health professionals. The license is limited to the clinician who purchased the Therapist’s Toolkit and does not extend to additional clinicians. Licenses cannot be sold or transferred to other individuals. However, licenses for additional therapists who practice together at the same location can be purchased for a modest fee. This gives additional therapists the right to use and photocopy the treatment and assessment tools in the Therapist’s Toolkit and / or the EASY Diagnostic System. Permission to use or reproduce these materials for any other purpose must be obtained in writing from David D. Burns, M.D.
Assessment Tests for Adults and Teens
1. Initial Diagnostic Assessment. Did you complete a comprehensive Axis I and Axis II diagnostic survey at the initial evaluation? 2. Clinical History. Did you flush out hidden agendas or conflicts of interest that could sabotage the treatment? Did you assess the patient's motivation and make him or her accountable? Did you ask about disability evaluations or legal entanglements, such as lawsuits, that could bias this patient's response to the treatment? Have you conceptualized the problem properly? 3. Psychotherapy Homework. Did the patient fill out the "Concept of SelfHelp Memo," along with the Self-Help Contract? Is the patient willing to do psychotherapy homework consistently between sessions? 4. Session-by-Session Testing. Do you track changes in symptoms at every therapy session, using instruments that accurately measure depression, suicidal urges, anxiety, anger, and relationship satisfaction? 5. Therapeutic Empathy. Do you have a vibrant, trusting therapeutic alliance? Does the patient feel accepted and cared about? Does the patient rate you on the Therapeutic Empathy scale after every session to indicate how warm, respectful and understanding you were? Are you getting scores of 20? 6. Therapeutic Helpfulness. Does the patient rate you on the Therapeutic Helpfulness scale after every therapy session? Does the patient feel that your interventions are relevant and helpful? 7. Agenda Setting. Invitation: Have you asked if the patient wants something more than listening and support? Specificity: Have you pinpointed one specific moment the patient wants help with? Conceptualization: Have you conceptualized the problem as an individual mood problem, relationship problem, or habit / addiction? Motivation: Have you explored Outcome and Process Resistance? Is the patient ready to change and willing to work hard, if you agree to help him or her with this problem? 8. Methods. Are you using a variety of techniques that specifically target this patient's problem? If it's an individual mood problem, are you using the Daily Mood Log and Recovery Circle, and "failing as fast as you can"? If it's a relationship problem, are you using interpersonal techniques, such as the Revise Your Communication Style form? Total
* Copyright © 2003 by David D. Burns, M.D.
2—Yes
1—Unsure
0—No
Therapist's Report Card* Instructions. Therapeutic failure usually results from the therapist errors listed below. Think of a patient you're stuck with and use checks () to indicate how well you're doing in each category.
Scoring Key: Therapist's Report Card Score
Grade
Interpretation
16
A+
Awesome! Few therapists do this well.
14 – 15
A
Very good. There's only a little bit of room for improvement.
11 – 13
B
Decent, but there are some problem areas to work on.
8 – 10
C
Not so good. There are lots of areas that need work.
4–7
D
Hmmm. What a can I say? Well, the good news is that the reasons for the therapeutic failure should be obvious, and there's lots of room for improvement!
0–3
F
Heck, we've all got to start somewhere. Furthermore, you've done an honest job of pinpointing the reasons for the therapeutic failure. There's nowhere to go but up!
Your Name:
Date:
Total
Total
Total
Total
Total
Total
Total
Total
4—Extremely
3—A lot
2—Moderately
1—Somewhat
0—Not at all
After Session 4—Extremely
3—A lot
How depressed do you feel right now? 1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life
2—Moderately
Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
1—Somewhat
Brief Mood Survey*
0—Not at all
Before Session
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life? How anxious do you feel right now? 1. Anxious 2. Frightened 3. Worrying about things 4. Tense or on edge 5. Nervous How angry do you feel right now? 1. Frustrated 2. Annoyed 3. Resentful 4. Angry 5. Irritated
1. 2. 3. 4. 5. 6. 7. 8. 9. 10.
Total
4—Extremely
3—A lot
2—Moderately
1—Somewhat
0—Not at all
4—Extremely
3—A lot
Positive Feelings: How do you feel right now? I feel worthwhile. I feel good about myself. I feel close to people. I feel I am accomplishing something. I feel motivated to do things. I feel calm and relaxed. I feel a spiritual connection to others. I feel hopeful. I feel encouraged and optimistic. My life is satisfying.
2—Moderately
Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
0—Not at all
Positive Feelings Survey*
1—Somewhat
Your answers on the following items will tend to be the opposite from your answers on the negative mood items above.
Total
* Copyright 1997 by David D. Burns, M.D. Revised, 2010.
Please fill this out BEFORE and AFTER the session. Thank you!
Page 1
1. 2. 3. 4. 5.
Therapeutic Empathy My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Total
6. 7. 8. 9. 10.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems. Total
Satisfaction with Today's Session 11. I believe the session was helpful to me. 12. Overall, I was satisfied with today's session. Total Your Commitment 13. I plan to do therapy homework before the next session. 14. I intend to use what I learned in today's session. Total Negative Feelings During the Session 15. At times, my therapist didn't seem to understand how I felt. 16. At times, I felt uncomfortable during the session. 17. I didn't always agree with my therapist. Total Difficulties with the Questions 18. It was hard to answer some of these questions honestly. 19. Sometimes my answers didn't show how I really felt inside. 20. It would be too upsetting for me to criticize my therapist. Total What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–Somewhat true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
Your Name:
Date:
Please complete the following surveys BEFORE and AFTER the session. Then complete the survey on the back AFTER the session. Thank you!
Total
Total
1. Communication and openness 2. Resolving conflicts 3. Degree of affection and caring 4. Intimacy and closeness 5. Overall satisfaction Total
* Copyright 1997 by David D. Burns, M.D. Revised 2010, 2011.
Total
4—Extremely 6—Very Satisfied
1—Moderately Dissatisfied
0—Very Dissatisfied
After Session
6—Very Satisfied
5—Moderately Satisfied
4—Somewhat Satisfied
3—Neutral
2—Somewhat Dissatisfied
Use checks () to indicate how you feel about this relationship. Please answer all 5 items.
1—Moderately Dissatisfied
How angry do you feel right now? 1. Frustrated 2. Annoyed 3. Resentful 4. Angry 5. Irritated
Put the name of an important relationship in your life:
0—Very Dissatisfied
Relationship Satisfaction * Total
3—A lot
Total
Before Session
Total
2—Moderately
1—Somewhat
0—Not at all
4—Extremely
3—A lot
2—Moderately
1—Somewhat
0—Not at all
4—Extremely
Total
How anxious do you feel right now? 1. Anxious 2. Frightened 3. Worrying about things 4. Tense or on edge 5. Nervous
5—Moderately Satisfied
Total
I feel worthwhile. I feel good about myself. I feel close to people. I feel productive. I feel motivated to do things. I feel calm and relaxed. I feel a connection to others. I feel hopeful. I feel encouraged and optimistic. My life is satisfying.
4—Somewhat Satisfied
Total
1. 2. 3. 4. 5. 6. 7. 8. 9. 10.
3—Neutral
Total
Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
After Session
2—Somewhat Dissatisfied
Total How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life?
Before Session Positive Feelings Survey*
3—A lot
2—Moderately
1—Somewhat
0—Not at all
After Session 4—Extremely
3—A lot
How depressed do you feel right now? 1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life
1—Somewhat
Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
0—Not at all
Brief Mood Survey*
2—Moderately
Before Session
1. 2. 3. 4. 5.
Therapeutic Empathy My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Total
6. 7. 8. 9. 10.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems. Total
Satisfaction with Today's Session 11. I believe the session was helpful to me. 12. Overall, I was satisfied with today's session. Total Your Commitment 13. I plan to do therapy homework before the next session. 14. I intend to use what I learned in today's session. Total Negative Feelings During the Session 15. At times, my therapist didn't seem to understand how I felt. 16. At times, I felt uncomfortable during the session. 17. I didn't always agree with my therapist. Total Difficulties with the Questions 18. It was hard to answer some of these questions honestly. 19. Sometimes my answers didn't show how I really felt inside. 20. It would be too upsetting for me to criticize my therapist. Total What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–Somewhat true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
Depression 1. 2. 3. 4. 5.
4—Extremely
Instructions. Use checks () to indicate how depressed, anxious or angry you've been feeling over the past week, including today. Please answer all the items.
3—A lot
0—Not at all
Brief Mood Survey*
2—Moderately
Date: 1—Somewhat
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges
1. Have you had any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions. Use checks () to show how satisfied or dissatisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
Scoring Keys* Depression, Anxiety, Panic, and Anger Scales
Relationship Satisfaction Scale
Score
Interpretation
Score
Satisfaction
0
no symptoms
0 - 10
extremely dissatisfied
1-2
borderline
11 - 15
very dissatisfied
3-5
mild
16 - 20
moderately dissatisfied
6 - 10
moderate
21 - 25
marginal
11 - 15
severe
26 - 28
moderately satisfied
16 - 20
extreme
29 - 30
Extremely satisfied
Therapeutic Empathy Scale* Score
Satisfaction Level
20
Excellent
19
Surprisingly, this score indicates a failure in the therapeutic alliance.
15 - 18
Not so good
10 - 14
Marginal at best
5-9
Poor
0-4
Alarming
*
Interpretation Good job! The patient appears to be very satisfied with the warmth, trust, respect, and understanding that she or he experienced during the session. A 19 seems excellent, and most therapists would be thrilled with it, but there’s a problem that needs to be addressed. It can be hard for patients to criticize therapists, and you won’t know the extent of the difficulty until you talk it over with your patient. The failure could be mild, moderate, or even severe. There’s definitely room for improvement. Scores of 18 always indicate fairly significant failures of therapeutic warmth, trust, or understanding. Scores of 15 are quite low. There are substantial and potentially serious feelings of dissatisfaction in more than one area. There are severe problems in many areas of the therapeutic alliance. Scores this low are unusual. This score nearly always indicates extreme problems in warmth, trust or understanding that need to be addressed immediately.
Copyright © 1997 by David D. Burns, MD. Revised, 2010.
Brief Mood / Survey Keys
Page 1
Scoring Key: 5–Item Depression, Anxiety, and Anger Tests Score
Interpretation
0-1
Few or no symptoms: the best possible score
2-4
Borderline symptoms
5-8
Mild symptoms
9 - 12
Moderate symptoms
13 - 16
Severe symptoms
17 - 20
Extreme symptoms
2–Item Suicidal Urges Test Item 1
Elevated scores on this item are not unusual. Most depressed patients have some suicidal thoughts or fantasies at times.
Item 2
Here, any elevated score is dangerous. This item assesses suicidal urges. You will need to do a careful suicide assessment, and may need to hospitalize the patient if he or she seems in danger of a suicide attempt.
Anyone with significant symptoms of depression, or suicidal or violent urges, should see consultation immediately with a mental health professional.
Score
5–Item Relationship Satisfaction Test (RSAT)
0-5
Extremely dissatisfied
6 - 10
Moderately dissatisfied
11 - 14
Somewhat dissatisfied
15 - 18
Neutral
19 - 22
Slightly satisfied
23 - 26
Moderately satisfied
27 - 28
Very satisfied
29 - 30
Extremely satisfied
Brief Mood / Survey Keys
Page 2
Scoring Key: Evaluation of Therapy Session Positive Feelings (Items 1 – 5) Score
Interpretation
20
Outstanding — excellent job!
19
There's a problem that should be explored.
17 - 18
Fair — but considerable room for improvement.
15 - 16
Poor — The patient doesn't feel supported or understood.
11 - 14
Warning — The patient seems very dissatisfied.
0 - 10
Extreme problems in the therapeutic alliance.
Scale
Helpfulness of the Session (Items 6 – 10)
Satisfaction with Today's Session (Items 11 – 12)
Your Commitment (Items 13 – 14)
Negative Feelings During the Session (Items 15 – 17)
Difficulties with the Questions (Items 18 – 20)
Interpretation You do not need to interpret the total score on this scale. However, the patient's responses will clearly indicate how helpful the session was. You can encourage the patient to explain which techniques were the most and least helpful. Toward the beginning of therapy, scores on this scale may indicate that the interventions are only somewhat or moderately helpful. This is normal. Once you develop a collaborative relationship, and find methods that lead to improvement, your scores will increase. It's much easier to get "perfect" scores on the Positive Feelings subscale than on the Helpfulness subscale. Again, the total score does not need interpretation, but the specific responses will clearly show how satisfied the patient felt. The responses will indicate whether patients intend to do psychotherapy homework and whether the session will have an impact on their lives. Any score of 1 ("Somewhat true") or above indicates that the patient had some negative feelings during the session. You need to explore these reactions using the Five Secrets of Effective Communication. Any score of 1 ("Somewhat true") or above indicates that the patient had trouble answering some of the items openly and honestly. If you simply ask them which items they had the most trouble with, nearly all patients will tell you! You need to be especially concerned if they had trouble with the suicidal urges questions. If patients had trouble answering the suicidal urges items honestly on the Brief Mood Survey, you will need to do a careful suicide assessment immediately. The patient may need an emergency intervention, such as hospitalization, to prevent a suicide attempt.
Brief Mood Survey / Scoring Keys
Page 1
Scoring Key: 5–Item Depression, Anxiety, and Anger Tests Score
Interpretation
0-1
Few or no symptoms: the best possible score
2-4
Borderline symptoms
5-8
Mild symptoms
9 - 12
Moderate symptoms
13 - 16
Severe symptoms
17 - 20
Extreme symptoms
2–Item Suicidal Urges Test Item 1
Elevated scores on this item are not unusual. Most depressed patients have some suicidal thoughts or fantasies at times.
Item 2
Here, any elevated score is dangerous. This item assesses suicidal urges. You should seek consultation with a mental health professional immediately.
Anyone with suicidal or violent urges should see consultation immediately with a mental health professional.
Score
5–Item Relationship Satisfaction Test (RSAT)
0-5
Extremely dissatisfied
6 - 10
Moderately dissatisfied
11 - 14
Somewhat dissatisfied
15 - 18
Neutral
19 - 22
Slightly satisfied
23 - 26
Moderately satisfied
27 - 28
Very satisfied
29 - 30
Extremely satisfied
Brief Mood Survey / Scoring Keys
Page 2
Scoring Key: Evaluation of Therapy Session Positive Feelings (Items 1 – 5) Score
Interpretation
20
Outstanding — excellent job!
19
There's a problem that should be explored.
17 - 18
Fair — but considerable room for improvement.
15 - 16
Poor — The patient doesn't feel supported or understood.
11 - 14
Warning — The patient seems very dissatisfied.
0 - 10
Extreme problems in the therapeutic alliance.
Scale
Helpfulness of the Session (Items 6 – 10)
Satisfaction with Today's Session (Items 11 – 12)
Your Commitment (Items 13 – 14)
Negative Feelings During the Session (Items 15 – 17)
Difficulties with the Questions (Items 18 – 20)
Interpretation You do not need to interpret the total score on this scale. However, the patient's responses will clearly indicate how helpful the session was. You can encourage the patient to explain which techniques were the most and least helpful. Toward the beginning of therapy, scores on this scale may indicate that the interventions are only somewhat or moderately helpful. This is normal. Once you develop a collaborative relationship, and find methods that lead to improvement, your scores will increase. It's much easier to get "perfect" scores on the Positive Feelings subscale than on the Helpfulness subscale. Again, the total score does not need interpretation, but the specific responses will clearly show how satisfied the patient felt. The responses will indicate whether patients intend to do psychotherapy homework and whether the session will have an impact on their lives. Any score of 1 ("Somewhat true") or above indicates that the patient had some negative feelings during the session. You need to explore these reactions using the Five Secrets of Effective Communication. Any score of 1 ("Somewhat true") or above indicates that the patient had trouble answering some of the items openly and honestly. If you simply ask them which items they had the most trouble with, nearly all patients will tell you! You need to be especially concerned if they had trouble with the suicidal urges questions. If patients had trouble answering the suicidal urges items honestly on the Brief Mood Survey, you will need to do a careful suicide assessment immediately. The patient may need an emergency intervention, such as hospitalization, to prevent a suicide attempt.
Brief Mood / Survey Keys
Page 1
Scoring Key: 5–Item Depression, Anxiety, and Anger Tests Score
Interpretation
0-1
Few or no symptoms: the best possible score
2-4
Borderline symptoms
5-8
Mild symptoms
9 - 12
Moderate symptoms
13 - 16
Severe symptoms
17 - 20
Extreme symptoms
2–Item Suicidal Urges Test Item 1
Elevated scores on this item are not unusual. Most depressed patients have some suicidal thoughts or fantasies at times.
Item 2
Here, any elevated score is dangerous. This item assesses suicidal urges. You will need to do a careful suicide assessment, and may need to hospitalize the patient if he or she seems in danger of a suicide attempt.
Anyone with significant symptoms of depression, or suicidal or violent urges, should see consultation immediately with a mental health professional.
Score
5–Item Relationship Satisfaction Test (RSAT)
0-5
Extremely dissatisfied
6 - 10
Moderately dissatisfied
11 - 14
Somewhat dissatisfied
15 - 18
Neutral
19 - 22
Slightly satisfied
23 - 26
Moderately satisfied
27 - 28
Very satisfied
29 - 30
Extremely satisfied
Brief Mood / Survey Keys
Page 2
Scoring Key: Evaluation of Therapy Session Positive Feelings (Items 1 – 5) Score
Interpretation
20
Outstanding — excellent job!
19
There's a problem that should be explored.
17 - 18
Fair — but considerable room for improvement.
15 - 16
Poor — The patient doesn't feel supported or understood.
11 - 14
Warning — The patient seems very dissatisfied.
0 - 10
Extreme problems in the therapeutic alliance.
Scale
Helpfulness of the Session (Items 6 – 10)
Satisfaction with Today's Session (Items 11 – 12)
Your Commitment (Items 13 – 14)
Negative Feelings During the Session (Items 15 – 17)
Difficulties with the Questions (Items 18 – 20)
Interpretation You do not need to interpret the total score on this scale. However, the patient's responses will clearly indicate how helpful the session was. You can encourage the patient to explain which techniques were the most and least helpful. Toward the beginning of therapy, scores on this scale may indicate that the interventions are only somewhat or moderately helpful. This is normal. Once you develop a collaborative relationship, and find methods that lead to improvement, your scores will increase. It's much easier to get "perfect" scores on the Positive Feelings subscale than on the Helpfulness subscale. Again, the total score does not need interpretation, but the specific responses will clearly show how satisfied the patient felt. The responses will indicate whether patients intend to do psychotherapy homework and whether the session will have an impact on their lives. Any score of 1 ("Somewhat true") or above indicates that the patient had some negative feelings during the session. You need to explore these reactions using the Five Secrets of Effective Communication. Any score of 1 ("Somewhat true") or above indicates that the patient had trouble answering some of the items openly and honestly. If you simply ask them which items they had the most trouble with, nearly all patients will tell you! You need to be especially concerned if they had trouble with the suicidal urges questions. If patients had trouble answering the suicidal urges items honestly on the Brief Mood Survey, you will need to do a careful suicide assessment immediately. The patient may need an emergency intervention, such as hospitalization, to prevent a suicide attempt.
4—Extremely
3—Very
Instructions. Use checks () to indicate how depressed, anxious or angry you've been feeling recently. Please answer all the items.
2—Moderately
Brief Mood Survey*
1—Somewhat
Date: 0—Not at all
Your name:
Depression 1. 2. 3. 4. 5.
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total Anxiety
1. 2. 3. 4. 5.
Anxious Nervous Worried Frightened or apprehensive Tense or on edge Total
1. 2.
Suicidal Urges Do you have any suicidal thoughts? Would you like to end your life? Total Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total
Total
* Copyright © 1997 by David D. Burns, M.D. Revised 2005.
6—Very
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Please answer all the items. 1. Communication and openness 2. Resolving conflicts and arguments 3. Degree of affection and caring 4. Intimacy and closeness 5. Overall satisfaction
0—Very
Put the name of someone you care about here: Use checks () to indicate how satisfied or dissatisfied you feel about this relationship.
Satisfied
Dissatisfied
5—Moderately
Relationship Satisfaction Test*
1. 2. 3. 4. 5.
4—Extremely true
3—Very true
2—Moderately true
Instructions. Use checks () to indicate how much you agree with each of the following statements. Please answer all the items.
1—Somewhat true
Brief Mood Survey (cont'd)*
Page 2
0—Not at all true
Brief Mood Survey
Special Experiences I sometimes hear voices that others do not seem to hear. Others can read my mind or insert thoughts into my mind. I believe that people are trying to control me with electricity, radio waves or other forces. I believe that people can hear my thoughts. I've been receiving special messages from the radio or TV. Total Feelings of Mistrust
1. 2. 3. 4. 5.
I believe that people are plotting against me. I believe that people are saying bad things about me. I believe that people are out to get me. I believe people want to harm me or take advantage of me. I believe that people are spying on me or trying to find out about my private life. Total
1. 2. 3. 4. 5.
Feelings of Superiority I sometimes feel far more brilliant and intelligent than others. I sometimes feel like I have special powers. I sometimes feel like a Messiah or a God. I sometimes feel far superior to others. I sometimes receive special messages from God.
1. 2. 3. 4. 5.
The doctors and nurses seem warm, supportive, and concerned. The doctors and nurses seem trustworthy. The doctors and nurses treat me with respect. The doctors and nurses do a good job of listening. The doctors and nurses understand how I feel inside. Total
* Copyright © 1997 by David D. Burns, M.D. Revised 2005.
4—Completely true
3—Very true
2—Moderately true
Instructions. Use checks () to indicate how well these statements describe your feelings about your experiences on the inpatient unit. Please answer all the items.
1—Somewhat true
Therapeutic Empathy Scale*
0—Not at all true
Total
1. Sad or down in the dumps 2. Discouraged or hopeless
4—Extremely
Please answer all the items. Depression
3—A lot
Instructions: Put a check ( ) after each item to indicate how you've been feeling over the past week, including today.
2—Moderately
Brief Mood Survey*
1—Somewhat
Page 1 0—Not at all
Brief Mood Survey Example plus Scoring Keys
3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life
Total Items 1 – 5
17
Suicidal Urges 1. Do you have any suicidal thoughts? 2. Would you like to end your life?
Total Items 1 – 2
2
Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous
Total Items 1 – 5
16
Anger 1. Frustrated
2. Annoyed
3. Resentful
4. Angry
5. Irritated
Total Items 1 – 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions: Place a check ( ) in the box that best describes how satisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
16
Total Items 1 – 5
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
17
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions: Put a check ( ) in the box that indicates how you felt about today’s session.
1–Somewhat true
Evaluation of Therapy Session*
Page 2
0–Not at all true
Brief Mood Survey Example plus Scoring Keys
Positive Feelings 1. 2. 3. 4. 5.
My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside.
Helpfulness of the Session 6. 7. 8. 9. 10.
I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems.
Satisfaction with Today's Session
11. I believe the session was helpful to me. 12. Overall, I was satisfied with today's session. Your Commitment 13. I plan to do therapy homework before the next session. 14. I intend to use what I learned in today's session.
Negative Feelings During the Session 15. At times, my therapist didn't seem to understand how I felt. 16. At times, I felt uncomfortable during the session. 17. I didn't always agree with my therapist.
Difficulties with the Questions 18. It was hard to answer some of these questions honestly. 19. Sometimes my answers didn't show how I really felt inside. 20. It would be hard for me to criticize my therapist.
What did you like the least about the session?
What did you like the best about the session?
* Copyright © 2001 by David D. Burns, M.D. Revised, 2002.
Brief Mood Survey Example plus Scoring Keys
Page 3
Scoring Key: Brief Mood Survey Score
5–Item Depression, Anxiety, and Anger Tests
0-1
Few or no symptoms: the best possible score
2-4
Borderline symptoms
5-8
Mild symptoms
9 - 12
Moderate symptoms
13 - 16
Severe symptoms
17 - 20
Extreme symptoms
2–Item Suicidal Urges Test Item 1
Elevated scores on this item are not unusual. Most depressed patients have some suicidal thoughts or fantasies at times.
Item 2
Here, any elevated score is dangerous. This item assesses suicidal urges. You will need to do a careful suicide assessment, and may need to hospitalize the patient if he or she seems in danger of a suicide attempt.
There are two additional assessment devices for suicidal urges in the Therapist's Toolkit. One is a two-page form that you fill out while interviewing the patient. You ask about urges to live, urges to die, degree of hopelessness, level of planning and preparation for a suicide attempt, presence or absence of deterrents, etc. In addition, there's a two-page self-assessment test the patient can fill out. These instruments may assist you in your evaluation of suicidal urges.
Score
5–Item Relationship Satisfaction Test (RSAT)
0-5
Extremely dissatisfied
6 - 10
Moderately dissatisfied
11 - 14
Somewhat dissatisfied
15 - 18
Neutral
19 - 22
Slightly satisfied
23 - 26
Moderately satisfied
27 - 28
Very satisfied
29 - 30
Extremely satisfied
Brief Mood Survey Example plus Scoring Keys
Page 4
Scoring Key: Evaluation of Therapy Session Positive Feelings (Items 1 – 5) Score
Interpretation
20
Outstanding — excellent job!
19
There's a problem that should be explored.
17 - 18
Fair — but considerable room for improvement.
15 - 16
Poor — The patient doesn't feel supported or understood.
11 - 14
Warning — The patient seems very dissatisfied.
0 - 10
Extreme problems in the therapeutic alliance.
Scale
Helpfulness of the Session (Items 6 – 10)
Satisfaction with Today's Session (Items 11 – 12)
Your Commitment (Items 13 – 14)
Negative Feelings During the Session (Items 15 – 17)
Difficulties with the Questions (Items 18 – 20)
Interpretation You do not need to interpret the total score on this scale. However, the patient's responses will clearly indicate how helpful the session was. You can encourage the patient to explain which techniques were the most and least helpful. Toward the beginning of therapy, scores on this scale may indicate that the interventions are only somewhat or moderately helpful. This is normal. Once you develop a collaborative relationship, and find methods that lead to improvement, your scores will increase. It's much easier to get "perfect" scores on the Positive Feelings subscale than on the Helpfulness subscale. Again, the total score does not need interpretation, but the specific responses will clearly show how satisfied the patient felt. The responses will indicate whether patients intend to do psychotherapy homework and whether the session will have an impact on their lives. Any score of 1 ("Somewhat true") or above indicates that the patient had some negative feelings during the session. You need to explore these reactions using the Five Secrets of Effective Communication. Any score of 1 ("Somewhat true") or above indicates that the patient had trouble answering some of the items openly and honestly. If you simply ask them which items they had the most trouble with, nearly all patients will tell you! You need to be especially concerned if they had trouble with the suicidal urges questions. If patients had trouble answering the suicidal urges items honestly on the Brief Mood Survey, you will need to do a careful suicide assessment immediately. The patient may need an emergency intervention, such as hospitalization, to prevent a suicide attempt.
Brief Mood Survey Example plus Scoring Keys
Page 5
Depression 1. 2. 3. 4. 5.
4—Extremely
Instructions. Use checks () to indicate how depressed, anxious or angry you've been feeling over the past week, including today. Please answer all the items.
3—A lot
0—Not at all
Brief Mood Survey*
2—Moderately
Date: 1—Somewhat
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges
1. Have you had any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5 * Copyright 1997 by David D. Burns, M.D. Revised, 2002.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions. Use checks () to show how satisfied or dissatisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
Therapeutic Empathy 1. 2. 3. 4. 5.
My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Helpfulness of the Session
6. 7. 8. 9. 10.
I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems.
11. 12.
I believe the session was helpful to me. Overall, I was satisfied with today's session.
13. 14.
I plan to do therapy homework before the next session. I intend to use what I learned in today's session.
15. 16. 17.
At times, my therapist didn't seem to understand how I felt. At times, I felt uncomfortable during the session. I didn't always agree with my therapist.
Satisfaction with Today's Session
Your Commitment
Negative Feelings During the Session
Difficulties with the Questions 18. 19. 20.
It was hard to answer some of these questions honestly. Sometimes my answers didn't show how I really felt inside. It would be too upsetting for me to criticize my therapist.
What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2003.
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1--Somewhat true
Evaluation of Therapy Session*
0--Not at all true
Page 2
Depression 1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life
Total Items 1 to 5 Suicidal Urges 1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5 Violent Urges
1. I’ve had thoughts or fantasies of hurting people. 2. I’ve had the urge to do something harmful or violent. Total Items 1 to 2
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
4—Extremely
Please answer all the items.
3—A lot
Instructions. Use checks () to indicate how you've been feeling over the past week, including today.
2—Moderately
Brief Mood Survey*
1—Somewhat
Date:
0—Not at all
Name:
Therapeutic Empathy 1. 2. 3. 4. 5.
My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Helpfulness of the Session
6. 7. 8. 9. 10.
I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems.
11. 12.
I believe the session was helpful to me. Overall, I was satisfied with today's session.
13. 14.
I plan to do therapy homework before the next session. I intend to use what I learned in today's session.
15. 16. 17.
At times, my therapist didn't seem to understand how I felt. At times, I felt uncomfortable during the session. I didn't always agree with my therapist.
Satisfaction with Today's Session
Your Commitment
Negative Feelings During the Session
Difficulties with the Questions 18. 19. 20.
It was hard to answer some of these questions honestly. Sometimes my answers didn't show how I really felt inside. It would be too upsetting for me to criticize my therapist.
What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2002.
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1--Somewhat true
Evaluation of Therapy Session*
0--Not at all true
Page 2
4—Extremely
3—A lot
Instructions. Use checks () to indicate how depressed, anxious or angry you're feeling right now, at this moment. On the Suicidal Urges scale, indicate how you've been feeling recently. Please answer all the items. Depression (How do you feel right now?)
2—Moderately
Brief Mood Survey*
1—Somewhat
Date:
0—Not at all
Name:
1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges (How have you felt recently?) 1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety (How do you feel right now?) 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger (How do you feel right now?)
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5 * Copyright 1997 by David D. Burns, M.D. Revised, 2002.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions. Use checks () to show how satisfied or dissatisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
Therapeutic Empathy 1. 2. 3. 4. 5.
My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Helpfulness of the Session
6. 7. 8. 9. 10.
I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems.
11. 12.
I believe the session was helpful to me. Overall, I was satisfied with today's session.
13. 14.
I plan to do therapy homework before the next session. I intend to use what I learned in today's session.
15. 16. 17.
At times, my therapist didn't seem to understand how I felt. At times, I felt uncomfortable during the session. I didn't always agree with my therapist.
Satisfaction with Today's Session
Your Commitment
Negative Feelings During the Session
Difficulties with the Questions 18. 19. 20.
It was hard to answer some of these questions honestly. Sometimes my answers didn't show how I really felt inside. It would be too upsetting for me to criticize my therapist.
What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2002.
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1--Somewhat true
Evaluation of Therapy Session*
0--Not at all true
Page 2
1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges (How have you felt recently?) 1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety (How do you feel right now?) 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger (How do you feel right now?)
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5 Violent Urges (How have you felt recently?)
1. I have thoughts or fantasies of hurting people. 2. I have the urge to do something harmful or violent. Total Items 1 to 2
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
4—Extremely
3—A lot
Instructions. Use checks () to indicate how depressed, anxious and angry you're feeling right now, at this moment. On the Suicidal and Violent Urges scales, indicate how you've been feeling recently. Please answer all the items. Depression (How do you feel right now?)
2—Moderately
Brief Mood Survey*
1—Somewhat
Date:
0—Not at all
Name:
Therapeutic Empathy 1. 2. 3. 4. 5.
My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Helpfulness of the Session
6. 7. 8. 9. 10.
I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems.
11. 12.
I believe the session was helpful to me. Overall, I was satisfied with today's session.
13. 14.
I plan to do therapy homework before the next session. I intend to use what I learned in today's session.
15. 16. 17.
At times, my therapist didn't seem to understand how I felt. At times, I felt uncomfortable during the session. I didn't always agree with my therapist.
Satisfaction with Today's Session
Your Commitment
Negative Feelings During the Session
Difficulties with the Questions 18. 19. 20.
It was hard to answer some of these questions honestly. Sometimes my answers didn't show how I really felt inside. It would be too upsetting for me to criticize my therapist.
What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2002.
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1--Somewhat true
Evaluation of Therapy Session*
0--Not at all true
Page 2
Brief Pain Test* 1.
Please circle the number that shows how much physical pain you feel RIGHT NOW? 0 none
2.
3
4
5 6 moderate pain
7
8 intense pain
9
10 worst
1
2 a little pain
3
4
5 6 moderate pain
7
8 intense pain
9
10 worst
Please circle the number that shows how strong your physical pain feels RIGHT NOW? 0 none
4.
2 a little pain
Please circle the number that shows how severe your physical pain is RIGHT NOW? 0 none
3.
1
1
2 a little pain
3
4
5 6 moderate pain
7
8 intense pain
9
10 worst
9
10 worst
What degree of physical pain are you experiencing RIGHT NOW? 0 none
1
2 a little pain
3
*
4
5 6 moderate pain
7
8 intense pain
Copyright © David D. Burns, M.D., 1999
Scoring Key Brief Pain Test Score
Pain Level
0
no pain
1-4
minimal
5 - 12
mild
13 - 24
moderate
25 - 36
severe
37 - 40
extreme
Pilot study at Stanford inpatient unit, N = 95: Reliability Cronbach's coefficient alpha: 99% Convergent Validity Correlation with McGill Pain Questionnaire (15-item test): r(95) = .88 (p < .0001) Correlation with McGill Pain Questionnaire (single pain intensity item): r(95) = .99 (p < .0001) Discriminant Validity Correlation with Brief Depression Test (5-item test): r() = .xx (p < .0001) Correlation with Brief Anxiety Test (5-item test): r() = .xx (p < .0001) Correlation with Brief Anger Test (5-item test): r() = .xx (p < .0001)
Chart Record*
Medication
Dose
Side Effects
Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session
1 Copyright © 2004 by David D. Burns, M.D.
Page 1
# Refills
Medication Record
# Prescribed
Commitment Negative Feelings Difficulties
Satisfaction
Helpfulness
Evaluation of Session
Empathy
Relationship Sat.
Anger
Anxiety
Date of Session
Suicidal Urges
Brief Mood Survey
Depression
Client's Name
Chart Record*
Medication
Dose
Side Effects
Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session
1 Copyright © 2004 by David D. Burns, M.D.
Page 2
# Refills
Medication Record
# Prescribed
Commitment Negative Feelings Difficulties
Satisfaction
Helpfulness
Evaluation of Session
Empathy
Relationship Sat.
Anger
Anxiety
Date of Session
Suicidal Urges
Brief Mood Survey
Depression
Client's Name
Chart Record*
Medication
Dose
Side Effects
Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session
1 Copyright © 2004 by David D. Burns, M.D.
Page 3
# Refills
Medication Record
# Prescribed
Commitment Negative Feelings Difficulties
Satisfaction
Helpfulness
Evaluation of Session
Empathy
Relationship Sat.
Anger
Anxiety
Date of Session
Suicidal Urges
Brief Mood Survey
Depression
Client's Name
Chart Record*
Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session
1 Copyright © 2004 by David D. Burns, M.D.
Page 1
Difficulties
Negative Feelings
Commitment
Satisfaction
Helpfulness
Empathy
Evaluation of Session Relationship Sat.
Anger
Anxiety
Date of Session
Suicidal Urges
Brief Mood Survey
Depression
Client's Name
Chart Record*
Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session
1 Copyright © 2004 by David D. Burns, M.D.
Page 2
Difficulties
Negative Feelings
Commitment
Satisfaction
Helpfulness
Empathy
Evaluation of Session Relationship Sat.
Anger
Anxiety
Date of Session
Suicidal Urges
Brief Mood Survey
Depression
Client's Name
Chart Record*
Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session Before Session After Session
1 Copyright © 2004 by David D. Burns, M.D.
Page 3
Difficulties
Negative Feelings
Commitment
Satisfaction
Helpfulness
Empathy
Evaluation of Session Relationship Sat.
Anger
Anxiety
Date of Session
Suicidal Urges
Brief Mood Survey
Depression
Client's Name
Date of Session
*
Copyright © 2004 by David D. Burns, M.D. Difficulties
Negative Feelings
Commitment
Satisfaction
Brief Mood Survey
Helpfulness
Empathy
Before Session
Relationship Sati'n.
Anger
Anxiety
Brief Mood Survey
Suicidal Urges
Depression
Relationship Sati'n.
Anger
Anxiety
Suicidal Urges
Depression
Client's Name
Chart Record * After Session Evaluation of Session
Date of Session
*
Copyright © 2004 by David D. Burns, M.D. Difficulties
Negative Feelings
Commitment
Satisfaction
Brief Mood Survey
Helpfulness
Empathy
Before Session
Relationship Sati'n.
Anger
Anxiety
Brief Mood Survey
Suicidal Urges
Depression
Relationship Sati'n.
Anger
Anxiety
Suicidal Urges
Depression
Client's Name
Chart Record * After Session Evaluation of Session
Date of Session
*
Page 1
Copyright © 2004 by David D. Burns, M.D.
# Prescribed / # Refills?
Side Effects
Evaluation of Session
Dose
Medication
Difficulties
Negative Feelings
Commitment
Brief Mood Survey
Satisfaction
Helpfulness
Empathy
Relationship Sat
Anger
Anxiety
Suicidal Urges
Depression
Client's Name
Chart Record * Medication Record
Date of Session
*
Page 2
Copyright © 2004 by David D. Burns, M.D.
# Prescribed / # Refills?
Side Effects
Evaluation of Session
Dose
Medication
Difficulties
Negative Feelings
Commitment
Brief Mood Survey
Satisfaction
Helpfulness
Empathy
Relationship Sat
Anger
Anxiety
Suicidal Urges
Depression
Client's Name
Chart Record * Medication Record
Date of Session
*
Page 1
Copyright © 2004 by David D. Burns, M.D.
Difficulties
Negative Feelings
Commitment
Satisfaction
Brief Mood Survey
Helpfulness
Empathy
Before Session
Relationship Sat
Anger
Anxiety
Brief Mood Survey
Suicidal Urges
Depression
Relationship Sat
Anger
Anxiety
Suicidal Urges
Depression
Client's Name
Chart Record * After Session Evaluation of Session
Date of Session
*
Page 2
Copyright © 2004 by David D. Burns, M.D.
Difficulties
Negative Feelings
Commitment
Satisfaction
Brief Mood Survey
Helpfulness
Empathy
Before Session
Relationship Sat
Anger
Anxiety
Brief Mood Survey
Suicidal Urges
Depression
Relationship Sat
Anger
Anxiety
Suicidal Urges
Depression
Client's Name
Chart Record * After Session Evaluation of Session
Fantasies 1. Sometimes I think about getting high. 2. Sometimes I daydream about getting high. 3. Sometimes I fantasize about using drugs or alcohol. 4. Sometimes I crave drugs or alcohol. 5. Sometimes I feel tempted to use drugs or alcohol. Total Items 1 to 5 Urges 6. Sometimes I have the urge to use drugs or alcohol. 7. Sometimes I really want to use drugs or alcohol. 8. Sometimes I really want to get high. 9. Sometimes it’s hard to resist the urge to use drugs or alcohol. 10. Sometimes I have to struggle with the temptation to use drugs or alcohol. Total Items 6 to 10
* Copyright 1998 by David D. Burns, M.D. Revised, 2002.
4—Completely true
3—Very true
2—Moderately true
Please answer all the items.
1—Somewhat true
Instructions. Use checks () to indicate how much each statement describes how you have been feeling in the past week, including today.
0—Not at all true
Cravings and Urges to Use*
Therapist Instructions for the Cravings and Urges to Use Scale This scale was designed for individuals receiving treatment for alcoholism or substance abuse. It's based on the assumption that the patient is trying to achieve total abstinence. Ask your patients to fill out the test each week, along with the other selfassessment tests to monitor progress. These may include the Brief Mood Survey and the Evaluation of Therapy Session form. You will notice the items don't ask about whether or not the patient actually used drugs or alcohol. They simply ask whether the patient was struggling with temptation. If the patient indicates that he or she did feel tempted to use drugs or alcohol, you can say that it's not surprising, since the urges to use drugs or alcohol can be so strong. Then you can say something like this, "I can imagine it was pretty tempting to give in to the urges. Sometimes it can be hard to resist these temptations. How many times did you use during the week?" In other words, you want to give a non-judgmental message that will make it easy for the person to own up to their substance abuse, so you can work on it in therapy. Once they've owned up to having strong urges, it becomes much easier to own up to using drugs or alcohol. You could also quantify the patient's responses along the following lines, but this type of interpretation is not really necessary for clinical use of the scale: Interpretation Score
Fantasies: Items 1 - 5
Urges: Items 6 - 10
0
No temptation
No urges
1—2
Occasional temptation
Slight urges
3—5
Significant temptation
Significant urges
6 — 10
Moderately strong temptation
Moderately strong urges
11 — 15
Very strong temptation
Very strong urges
16 — 20
Overwhelming temptation
Overwhelming urges
Please fill this out before and after the session. Thank you!
Brief Mood Survey* Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
How depressed do you feel right now? 1. 2. 3. 4. 5.
Before Session
After Session
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Date:
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem Worthless or inadequate Loss of pleasure or satisfaction in life Total
Total
Total
Total
Total
Total
Total
Total
How suicidal do you feel right now? 6. Do you have any suicidal thoughts? 7. Would you like to end your life?
How anxious do you feel right now? 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous
How angry do you feel right now? Frustrated Annoyed Resentful Angry Irritated
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total
* Copyright 1997 by David D. Burns, M.D. Revised, 2010.
Total
5—Moderately 6—Very
4—Somewhat
Satisfied
3—Neutral
2—Somewhat
1—Moderately
Dissatisfied
0—Very
6—Very
5—Moderately
4—Somewhat
Please answer all 5 items.
After Session
Satisfied
3—Neutral
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship.
2—Somewhat
Put the name of a family member here:
Before Session Dissatisfied
1—Moderately
Relationship Satisfaction*
0—Very
1. 2. 3. 4. 5.
Please fill this out before and after the session. Thank you! Relationship Satisfaction*
Before Session Dissatisfied
After Session
Satisfied
Dissatisfied
Satisfied
Total
5—Moderately 6—Very 5—Moderately 6—Very
4—Somewhat
Satisfied
3—Neutral
2—Somewhat
1—Moderately
0—Very
6—Very
5—Moderately
4—Somewhat
Dissatisfied
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total
After Session
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total
* Copyright 1997 by David D. Burns, M.D. Revised, 2010.
Total
5—Moderately 6—Very
Satisfied
4—Somewhat
2—Somewhat
1—Moderately
Dissatisfied
0—Very
6—Very
5—Moderately
4—Somewhat
Satisfied
3—Neutral
Please answer all 5 items.
2—Somewhat
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship.
1—Moderately
Put the name of a family member here:
Total
Before Session Dissatisfied
0—Very
Relationship Satisfaction*
1. 2. 3. 4. 5.
4—Somewhat
After Session
Satisfied
3—Neutral
Please answer all 5 items.
2—Somewhat
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship.
1—Moderately
Put the name of a family member here:
Total
Before Session Dissatisfied
0—Very
Relationship Satisfaction*
1. 2. 3. 4. 5.
3—Neutral
2—Somewhat
1—Moderately
0—Very
6—Very
5—Moderately
4—Somewhat
3—Neutral
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction
3—Neutral
1. 2. 3. 4. 5.
2—Somewhat
Please answer all 5 items.
1—Moderately
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship.
0—Very
Put the name of a family member here:
Please fill this out after the session. Thank you!
1. 2. 3. 4.
Therapeutic Empathy The therapist seemed warm, supportive, and concerned. The therapist treated me with respect. The therapist did a good job of listening. The therapist understood how I felt inside.
5. 6. 7. 8.
Your Participation I talked about the problems that are bothering me. I was able to express my feelings during the session. I participated actively in the session. I worked on my problems during the session.
Total
Total Helpfulness of the Session 9. 10. 11. 12.
The techniques we used were helpful. I learned some new ways to deal with my problems. The approach we used made sense. What I learned in today's session will be useful. Total Support of the Session
13. I felt close to my family members. 14. Family members were warm, supportive, and concerned. 15. I felt accepted by the other family members. Total Satisfaction with Today's Session 16. Overall, I was satisfied with today's session. Total Your Commitment 17. I plan to do therapy homework before the next session. 18. I intend to use what I learned between sessions. Total Difficulties with the Questions 19. It was hard to be completely honest on this survey. 20. It would be too upsetting for me to criticize the therapist. Total What did you like the least about the session?
What did you like the best about the session?
* Copyright © 2001 by David D. Burns, MD, Revised 2010
4--Completely true
Please answer all the items.
3--Very true
Instructions. Use checks () to indicate how you felt about today’s session.
2--Moderately true
Evaluation of Family Therapy Session*
1--Somewhat true
Date:
0--Not at all true
Name:
Please fill this out BEFORE the group begins. Thank you!
1. 2. 3. 4. 5.
4—Extremely
3—A lot
Instructions. Use checks () to indicate how depressed, anxious or angry you're feeling right now, at this moment. On the Suicidal Urges scale, indicate how you've been feeling recently. Please answer all the items. Depression (How do you feel right now?)
2—Moderately
Brief Mood Survey*
1—Somewhat
Date:
0—Not at all
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges (How have you felt recently?)
1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety (How do you feel right now?) 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger (How do you feel right now?)
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5 * Copyright 1997 by David D. Burns, M.D. Revised, 2002.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions. Use checks () to show how satisfied or dissatisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
1. 2. 3. 4. 5.
4—Extremely
3—A lot
2—Moderately
Instructions. Use checks () to indicate how depressed, anxious or angry you're feeling right now, at this moment. On the Suicidal Urges scale, indicate how you've been feeling recently. Please answer all the items. Depression (How do you feel right now?)
1—Somewhat
Brief Mood Survey*
0—Not at all
Please fill this out AT THE END of the group. Thank you!
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges (How have you felt recently?)
1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety (How do you feel right now?) 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger (How do you feel right now?)
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5 * Copyright 1997 by David D. Burns, M.D. Revised, 2002.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions. Use checks () to show how satisfied or dissatisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
Therapeutic Empathy 1. The group leader(s) seemed warm, supportive, and concerned. 2. The group leader(s) treated me with respect. 3. The group leader(s) did a good job of listening. 4. The group leader(s) understood how I felt inside. Support of the Group 5. I felt close to the other group members. 6. The group members were warm, supportive, and concerned. Your Participation 7. I talked about the problems that are bothering me. 8. I was able to express my feelings during the group. 9. I participated actively in the group. Helpfulness of the Group 10. The techniques we used were helpful. 11. I learned some new ways to deal with my problems. 12. What I learned in the session will be useful. 13. Overall, I was satisfied with today's group. Your Commitment 14. I plan to do therapy homework before the next group. 15. I intend to use what I learned between sessions. Negative Feelings During the Group 16. At times, the group leader(s) didn't seem to understand how I felt. 17. At times, I felt uncomfortable during the group. 18. I didn't always agree with the group leader(s). Difficulties with the Questions 19. It was hard to be completely honest on this survey. 20. It would be too upsetting for me to criticize the group leader(s). What did you like the least about the group?
What did you like the best about the group?
(Use reverse if you need more space) * Copyright © 2001 by David D. Burns, MD
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about today’s group session.
1--Somewhat true
Evaluation of Therapy Group*
0--Not at all true
Please fill this out AT THE END of the group. Thank you!
Please fill this out BEFORE the group begins. Thank you!
Depression: How are you feeling right now? 1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges: How have you been feeling recently? 1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety: How are you feeling right now? 1. Anxious 2. Frightened 3. Worrying about things 4. Tense or on edge 5. Nervous Total Items 1 to 5 Anger: How are you feeling right now? 1. Frustrated 2. Annoyed 3. Resentful 4. Angry 5. Irritated Total Items 1 to 5 Violent Urges: How have you been feeling recently? 1. I’ve had thoughts or fantasies of hurting people. 2. I’ve had the urge to do something harmful or violent. Total Items 1 to 2
* Copyright 1997 by David D. Burns, M.D.
4—Extremely
3—A lot
Instructions. Use checks () to indicate how depressed, anxious and angry you're feeling right now, at this moment. On the Suicidal and Violent Urges scales, indicate how you've been feeling recently. Please answer all the items.
2—Moderately
Brief Mood Survey*
1—Somewhat
Date: 0—Not at all
Name:
Depression: How are you feeling right now? 1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges: How have you been feeling recently? 1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety: How are you feeling right now? 1. Anxious 2. Frightened 3. Worrying about things 4. Tense or on edge 5. Nervous Total Items 1 to 5 Anger: How are you feeling right now? 1. Frustrated 2. Annoyed 3. Resentful 4. Angry 5. Irritated Total Items 1 to 5 Violent Urges: How have you been feeling recently? 1. I’ve had thoughts or fantasies of hurting people. 2. I’ve had the urge to do something harmful or violent. Total Items 1 to 2
* Copyright 1997 by David D. Burns, M.D.
4—Extremely
3—A lot
2—Moderately
Instructions. Use checks () to indicate how depressed, anxious and angry you're feeling right now, at this moment. On the Suicidal and Violent Urges scales, indicate how you've been feeling recently. Please answer all the items.
1—Somewhat
Brief Mood Survey*
0—Not at all
Please fill this out AT THE END of the group. Thank you!
Therapeutic Empathy 1. The group leader(s) seemed warm, supportive, and concerned. 2. The group leader(s) treated me with respect. 3. The group leader(s) did a good job of listening. 4. The group leader(s) understood how I felt inside. Your Participation 5. I talked about the problems that are bothering me. 6. I was able to express my feelings during the group. 7. I participated actively in the group. 8. I worked on my problems during the group. Helpfulness of the Group 9. The techniques we used were helpful. 10. I learned some new ways to deal with my problems. 11. The approach we used made sense. 12. What I learned in today's group will be useful. Support of the Group 13. I felt close to the other group members. 14. The group members were warm, supportive, and concerned. 15. I felt accepted by the other group members. Satisfaction with Today's Group 16. Overall, I was satisfied with today's group. Your Commitment 17. I plan to do therapy homework before the next group. 18. I intend to use what I learned between sessions. Difficulties with the Questions 19. It was hard to be completely honest on this survey. 20. It would be too upsetting for me to criticize the group leader(s). What did you like the least about the group?
What did you like the best about the group?
(Use reverse if you need more space) * Copyright © 2001 by David D. Burns, MD
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about today’s group session.
1--Somewhat true
Evaluation of Therapy Group*
0--Not at all true
Please fill this out AT THE END of the group. Thank you!
Brief Mood Survey* Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
How depressed do you feel right now? 1. 2. 3. 4. 5.
Before Session
After Session
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Date:
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total
Total
Total
Total
Total
Total
Total
Total
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life?
How anxious do you feel right now? 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous
How angry do you feel right now? Frustrated Annoyed Resentful Angry Irritated
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total
* Copyright 1997 by David D. Burns, M.D. Revised, 2004.
Total
5—Moderately 6—Very
4—Somewhat
Satisfied
3—Neutral
2—Somewhat
1—Moderately
Dissatisfied
0—Very
6—Very
5—Moderately
4—Somewhat
Please answer all 5 items.
After Session
Satisfied
3—Neutral
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship.
2—Somewhat
Put the name of someone you care about here:
Before Session Dissatisfied
1—Moderately
Relationship Satisfaction*
0—Very
1. 2. 3. 4. 5.
Therapeutic Empathy 1. The group leader(s) seemed warm, supportive, and concerned. 2. The group leader(s) treated me with respect. 3. The group leader(s) did a good job of listening. 4. The group leader(s) understood how I felt inside. Your Participation 5. I talked about the problems that are bothering me. 6. I was able to express my feelings during the group. 7. I participated actively in the group. 8. I worked on my problems during the group. Helpfulness of the Group 9. The techniques we used were helpful. 10. I learned some new ways to deal with my problems. 11. The approach we used made sense. 12. What I learned in today's group will be useful. Support of the Group 13. I felt close to the other group members. 14. The group members were warm, supportive, and concerned. 15. I felt accepted by the other group members. Satisfaction with Today's Group 16. Overall, I was satisfied with today's group. Your Commitment 17. I plan to do therapy homework before the next group. 18. I intend to use what I learned between sessions. Difficulties with the Questions 19. It was hard to be completely honest on this survey. 20. It would be too upsetting for me to criticize the group leader(s). What did you like the least about the group?
What did you like the best about the group?
* Copyright © 2001 by David D. Burns, MD, Revised 2009
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about today’s group session.
1--Somewhat true
Evaluation of Therapy Group*
0--Not at all true
Please fill this out AFTER the group. Thank you!
Brief Mood Survey* Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
How depressed do you feel right now? 1. 2. 3. 4. 5.
Before Session
After Session
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Date:
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Name:
Sad or down in the dumps Discouraged or hopeless
Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total
Total
Total
Total
Total
Total
Total
Total
Total
Total
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life?
How anxious do you feel right now? 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous
How angry do you feel right now? 1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated
How violent do you feel right now? 1. I have thoughts or fantasies of hurting people. 2. I have the urge to do something harmful or violent.
* Copyright 1997 by David D. Burns, M.D. Revised, 2004.
1. 2. 3. 4. 5.
Therapeutic Empathy My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Total
1. 2. 3. 4. 5.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems. Total
Satisfaction with Today's Session 1. I believe the session was helpful to me. 2. Overall, I was satisfied with today's session. Total Your Commitment 1. I plan to do therapy homework before the next session. 2. I intend to use what I learned in today's session. Total Negative Feelings During the Session 1. At times, my therapist didn't seem to understand how I felt. 2. At times, I felt uncomfortable during the session. 3. I didn't always agree with my therapist. Total Difficulties with the Questions 1. It was hard to answer some of these questions honestly. 2. Sometimes my answers didn't show how I really felt inside. 3. It would be too upsetting for me to criticize my therapist. Total What did you like the least about the session?
What did you like the best about the session?
* Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–Somewhat true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
Brief Mood Survey* Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
How depressed do you feel right now? 1. 2. 3. 4. 5.
Before Session
After Session
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Date:
0—Not at all 1—Somewhat 2—Moderately 3—A lot 4—Extremely
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total
Total
Total
Total
Total
Total
Total
Total
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life?
How anxious do you feel right now? 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous
How angry do you feel right now? Frustrated Annoyed Resentful Angry Irritated
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total
* Copyright 1997 by David D. Burns, M.D. Revised, 2004.
Total
6—Very Satisfied
5—Moderately Satisfied
4—Somewhat Satisfied
3—Neutral
2—Somewhat Dissatisfied
1—Moderately Dissatisfied
0—Very Dissatisfied
6—Very Satisfied
After Session 5—Moderately Satisfied
4—Somewhat Satisfied
Please answer all 5 items.
3—Neutral
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship.
0—Very Dissatisfied
Put the name of someone you care about here:
2—Somewhat Dissatisfied
Before Session
Relationship Satisfaction*
1—Moderately Dissatisfied
1. 2. 3. 4. 5.
1. 2. 3. 4. 5.
Therapeutic Empathy My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Total
6. 7. 8. 9. 10.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems. Total
Satisfaction with Today's Session 11. I believe the session was helpful to me. 12. Overall, I was satisfied with today's session. Total Your Commitment 13. I plan to do therapy homework before the next session. 14. I intend to use what I learned in today's session. Total Negative Feelings During the Session 15. At times, my therapist didn't seem to understand how I felt. 16. At times, I felt uncomfortable during the session. 17. I didn't always agree with my therapist. Total Difficulties with the Questions 18. It was hard to answer some of these questions honestly. 19. Sometimes my answers didn't show how I really felt inside. 20. It would be too upsetting for me to criticize my therapist. Total What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–Somewhat true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
Date:
Total
Total
Total
Total
Total
Total
Total
Total
4—Extremely
3—A lot
2—Moderately
0—Not at all
After Session
4—Extremely
3—A lot
How depressed do you feel right now? 1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life 0 - 4 5 - 8 9 - 11 12 - 14 15 - 17 18 - 20
2—Moderately
Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
0—Not at all
Brief Mood Survey*
1—Somewhat
Before Session
1—Somewhat
Name:
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life? How anxious do you feel right now? 1. Anxious 2. Frightened 3. Worrying about things 4. Tense or on edge 5. Nervous 0 - 4 5 - 8 9 - 11 12 - 14 15 - 17 18 - 20
1. Communication and openness 2. Resolving conflicts and arguments 3. Degree of affection and caring 4. Intimacy and closeness 5. Overall satisfaction 0 – 10 11 - 15 16 - 20 26 - 25 26 – 28 29 - 30
Total
* Copyright 1997 by David D. Burns, M.D. Revised, 2010.
Total
6—Very Satisfied
5—Moderately Satisfied
4—Somewhat Satisfied
3—Neutral
2—Somewhat Dissatisfied
1—Moderately Dissatisfied
0—Very Dissatisfied
6—Very Satisfied
5—Moderately Satisfied
4—Somewhat Satisfied
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship. Please answer all 5 items.
3—Neutral
Put the name of an important relationship in your life:
0—Very Dissatisfied
Relationship Satisfaction*
1—Moderately Dissatisfied
9 - 11 12 - 14 15 - 17 18 - 20
2—Somewhat Dissatisfied
How angry do you feel right now? 1. Frustrated 2. Annoyed 3. Resentful 4. Angry 5. Irritated 0-4 5-8
1. 2. 3. 4. 5.
Therapeutic Empathy My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Total
6. 7. 8. 9. 10.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems. Total
Satisfaction with Today's Session 11. I believe the session was helpful to me. 12. Overall, I was satisfied with today's session. Total Your Commitment 13. I plan to do therapy homework before the next session. 14. I intend to use what I learned in today's session. Total Negative Feelings During the Session 15. At times, my therapist didn't seem to understand how I felt. 16. At times, I felt uncomfortable during the session. 17. I didn't always agree with my therapist. Total Difficulties with the Questions 18. It was hard to answer some of these questions honestly. 19. Sometimes my answers didn't show how I really felt inside. 20. It would be too upsetting for me to criticize my therapist. Total What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–Somewhat true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
Date:
Total
Total
Total
Total
Total
Total
Total
Total
4—Extremely
3—A lot
2—Moderately
0—Not at all
After Session
4—Extremely
3—A lot
How depressed do you feel right now? 1. Sad or down in the dumps 2. Discouraged or hopeless 3. Low self-esteem, inferiority, or worthlessness 4. Loss of motivation to do things 5. Loss of pleasure or satisfaction in life 0 1 - 2 3 - 5 6 - 10 11 - 15 16 - 20
2—Moderately
Instructions. Use checks () to indicate how you're feeling right now. Please answer all the items.
0—Not at all
Brief Mood Survey*
1—Somewhat
Before Session
1—Somewhat
Name:
How suicidal do you feel right now? 1. Do you have any suicidal thoughts? 2. Would you like to end your life? How anxious do you feel right now? 1. Anxious 2. Frightened 3. Worrying about things 4. Tense or on edge 5. Nervous 0 1 - 2 3 - 5 6 - 10 11 - 15 16 - 20
1. Communication and openness 2. Resolving conflicts and arguments 3. Degree of affection and caring 4. Intimacy and closeness 5. Overall satisfaction 0 – 10 11 - 15 16 - 20 26 - 25 26 – 28 29 - 30
Total
* Copyright 1997 by David D. Burns, M.D. Revised, 2010.
Total
6—Very Satisfied
5—Moderately Satisfied
4—Somewhat Satisfied
3—Neutral
2—Somewhat Dissatisfied
1—Moderately Dissatisfied
0—Very Dissatisfied
6—Very Satisfied
5—Moderately Satisfied
Use checks () to indicate how satisfied or dissatisfied you feel about this relationship. Please answer all 5 items.
4—Somewhat Satisfied
Put the name of an important relationship in your life:
0—Very Dissatisfied
Relationship Satisfaction*
3—Neutral
6 - 10 11 - 15 16 - 20 1—Moderately Dissatisfied
3-5
2—Somewhat Dissatisfied
How angry do you feel right now? 1. Frustrated 2. Annoyed 3. Resentful 4. Angry 5. Irritated 0 1-2
1. 2. 3. 4. 5.
Therapeutic Empathy My therapist seemed warm, supportive, and concerned. My therapist seemed trustworthy. My therapist treated me with respect. My therapist did a good job of listening. My therapist understood how I felt inside. Total
6. 7. 8. 9. 10.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems. Total
Satisfaction with Today's Session 11. I believe the session was helpful to me. 12. Overall, I was satisfied with today's session. Total Your Commitment 13. I plan to do therapy homework before the next session. 14. I intend to use what I learned in today's session. Total Negative Feelings During the Session 15. At times, my therapist didn't seem to understand how I felt. 16. At times, I felt uncomfortable during the session. 17. I didn't always agree with my therapist. Total Difficulties with the Questions 18. It was hard to answer some of these questions honestly. 19. Sometimes my answers didn't show how I really felt inside. 20. It would be too upsetting for me to criticize my therapist. Total What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–Somewhat true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
New Psychometric Information This file contains some new psychometric information published since the completion of the 1997 Toolkit Upgrade. You will find copies of Dr. Don Beal's reports presented at the Annual Meeting of the Association for the Advancement of Behavior Therapy, Toronto, Canada, November, 1999, including: On page 2, you will find a report on the concurrent validity of the Burns Anxiety Checklist (Burns-A). In Table 2 on page 6, you will find the actual data and results, including reliability estimates. On page 3, you will find a report on the concurrent validity of the Burns Depression Checklist (Burns-D). In Table 3 on page 7, you will find the actual data and results, including reliability estimates. The means and standard deviations for the Burns-D, Burns-A, BDI, BAI, SDS (Zung Depression Scale) and SAS (Zung Anxiety Scale) in clinical and nonclinical groups appear in Table 4 on page 8. On page 4, you will find the results of a study at the Atlanta VA using a number of the brief scales. In Table 5 on page 9, you will find the discriminant validity data for the Burns-D and Burns-A in this study. On page 11, you will find a reference to a study by Cohen, Thayapran, Muhlen, Ibrahim, & Quan (1999). These investigators recently reported that scores on the 33-item Burns-A predicted symptomatic hypotension and/or bradycardia on head-up tilt table testing (HUT) in men and women with unexplained syncope. The association between Burns-A scores and subsequent symptoms was stronger in women than in men. On page 11, you will find references to several additional psychometric analyses of the Burns-D and Burns-A. These dissertations were completed under the direction of Dr. Beal, a faculty member in the Department of Psychology at Eastern Kentucky University. Many of his graduate students are involved in ongoing studies on the properties of the Burns-D, the Burns-A, and other instruments.
Update on Reliability and Validity Information
Page 2
THE CONCURRENT VALIDITY OF THE BURNS ANXIETY CHECKLIST Presented at the Annual Meeting of the Association for the Advancement of Behavior Therapy, Toronto, Canada, November, 1999 Gerlinde C. Sekirnjak and Don Beal, Eastern Kentucky University Contact: Don Beal, Department of Psychology, Eastern Kentucky University, Richmond, KY 40475. Phone (606) 622-1105; FAX (606) 622-5871. E-mail: [email protected] The availability of valid instruments to assess emotional problems is critical for systematically monitoring ongoing psychological treatment, demonstrating treatment efficacy, and carrying out epidemiological research. The purpose of the present investigation was to further assess the concurrent validity of the Burns Anxiety Checklist (Burns-A). The Burns-A is a brief self-report inventory developed to evaluate symptoms of anxiety (Burns, 1993). The Burns-A consists of 33 items assessing three dimensions of anxiety: (1) anxious feelings; (2) anxious thoughts; and (3) physical symptoms. Clients are asked to indicate how much each of the 33 symptoms has bothered them in the "last several days." A 4-point rating scale for each item indicates the severity of each symptom, from 0 ("not at all") to 3 ("a lot"). The Burns-A yields an overall anxiety score ranging from 0 to 99, determined by summing the self-ratings across all items. Method One method of establishing the concurrent validity of a psychometric instrument is to correlate the instruments' scores with other well established, valid instruments that measure the same construct the new test purports to measure (Anastasi, 1968). Thus in the present study, the scores from the Burns-A were correlated with scores from the Beck Anxiety Inventory and the Zung Self Rating Anxiety Scale. Instruments: The Beck Anxiety Inventory and the Zung Self Rating Anxiety Scale were selected as reference standards, as both have clear internal consistency, strong content validity, excellent concurrent validity, and clear discriminative validity. Thus given their wellestablished empirical support, both are seen as valid self-report measures of anxiety. Participants: Participants consisted of two groups: (1) A group of 76 undergraduate students enrolled in Psychology courses at a regional university in the southeastern United States; and (2) A group of clinic clients (N=33) from several mental health centers. Each participant was given the Burns-A, the Beck Anxiety Scale, and the Zung Self Rating Anxiety Scale. The order of administration of these instruments was varied to avoid order effects. Results and Discussion It was found that the Burns-A correlated significantly with the Beck Anxiety Inventory and the Zung Self Rating Anxiety Scale in all sets of analyses. In all cases the correlations were highly significant (p < .0001). Thus, these findings provide encouraging supportive evidence for the concurrent validity of the Burns-A.
Update on Reliability and Validity Information
Page 3
THE CONCURRENT VALIDITY OF THE BURNS DEPRESSION CHECKLIST Presented at the Annual Meeting of the Association for the Advancement of Behavior Therapy, Toronto, Canada, November, 1999 Gerlinde C. Sekirnjak and Don Beal, Eastern Kentucky University Contact: Don Beal, Department of Psychology, Eastern Kentucky University, Richmond, KY 40475. Phone (606) 622-1105; FAX (606) 622-5871. E-mail: [email protected] The availability of valid instruments to assess emotional problems is critical for systematically monitoring ongoing psychological treatment, demonstrating treatment efficacy, and carrying out epidemiological research. The purpose of the present investigation was to further assess the concurrent validity of the Burns Depression Checklist (Burns-D). The Burns-D is a brief self-report inventory developed to assess depression severity (Burns, 1989, 1993). The Burns-D consists of fifteen items assessing fifteen different dimensions of depression. Clients are asked to indicate how much each of the 15 symptoms has bothered them in the "last several days." A 4-point rating scale for each item indicates the severity of each symptom, from 0 ("not at all") to 3 ("a lot"). The Burns-D yields an overall depression score ranging from 0 to 45, determined by summing the self-ratings across all items. Method One method of establishing the concurrent validity of a psychometric instrument is to correlate the instruments' scores with other well established, valid instruments that measure the same construct the new test purports to measure (Anastasi, 1968). Thus in the present study, the scores from the Burns-D were correlated with scores from the Beck Depression Inventory and the Zung Self Rating Depression Scale. Instruments: The Beck Depression Inventory and the Zung Self Rating Depression Scale were selected as reference standards, as both have clear internal consistency, strong content validity, excellent concurrent validity, and clear discriminative validity. Thus given their wellestablished empirical support, both are seen as valid, self-report measures of depression. Participants: Participants consisted of two groups: (1) A group of 76 undergraduate students enrolled in Psychology courses at a regional university in the southeastern United States; and (2) A group of clinic clients (n=33) from several mental health centers. Each participant was given the Burns-D, the Beck Depression Scale, and the Self Rating Depression Scale. The order of administration of these instruments was varied to avoid order effects. Results and Discussion It was found that the Burns-D correlated significantly with the Beck Depression Inventory and the Zung Self Rating Depression Scale in all sets of analyses. In all cases the correlations were highly significant (p < .0001). Thus, these findings provide encouraging supportive evidence for the concurrent validity of the Burns-D.
Update on Reliability and Validity Information
Page 4
Brief Scale Reliabilities Reliabilities of the Brief Mood Survey scales, PTSD scale, and Positive Feelings scales in the recent Atlanta VA study are reported here. Cronbach’s coefficient alpha was calculated using SPSS under listwise deletion. Cronbach’s coefficient alpha is an estimate of the reliability of a scale. A scale with an alpha of .90 (90%) contains 10% error variance and is 90% reliable. Cronbach’s coefficient alpha is the correlation between the total scale score and a onedimension scale factor. The estimate of any correlation will be attenuated by range restriction. The veterans in this study were suffering from PTSD, and nearly all of them reported severe symptoms. Therefore, in many cases the ranges were restricted, and the true scale reliabilities will probably be higher than those reported here. In spite of this problem, the reliabilities of the scales are quite high. Of course, the reliability of a long scale will usually be high, even if the scale items are poor. When short scales have high reliabilities (over 85%), it's encouraging. This result indicates that the scale measures a single dimension quite accurately. The reliability analysis of the 5-item Depression scale appears in Table 1 on page 5. You will find two columns labeled "Alpha." The value of .90 in the "intake only group" means that the reliability of the brief depression test was .90 during the initial evaluation of the 79 veterans who participated in the study. You will also see a value of .92 in the 18-week study group. A subgroup of 21 veterans was tested repeatedly during the 18 weeks while participating in a treatment group, so each veteran contributed several depression tests. This is why the total N was 303 in the 18-week analysis. What do these results mean? The reliability of a test indicates how accurately the test measures one construct. We can conclude that at least 90% of the variance in the brief Depression test results from depression variance and that less than 10% of the variance in the test scores result from errors of measurement or constructs other than depression. The reliability of a test is not the same as the validity. A test could be exceedingly reliable, but not valid. In other words, the test could measure the wrong thing with great accuracy! One way to determine validity is to correlate a new test with an established test that measures the same construct. Investigators have compared the Burns Depression Checklist with other established measures of depression, like the Beck Depression Inventory, The Zung Depression Scale, the SCL-90 depression scale, and others. In all studies to date, the correlations among the measures were exceedingly high. The discriminant validity studies from the Atlanta VA appear in Table 5 on page 9.
Update on Reliability and Validity Information
Page 5
Table 1. Scale Reliabilities in the Atlanta VA Study. Group
18-week study group* Alpha
N
Intake only group** Alpha
N
Brief Mood Survey Scales (5-item scales) Depression
.92
303
.90
79
Anxiety
.94
303
.88
77
Panic
.92
302
.90
79
Anger
.97
304
.93
79
Relationship Satisfaction Scale (RSAT)
.95
296
.95
73
Empathy (positive feelings about therapist)
.99
295
.95
72
Self-Help Scale
.99
296
.95
69
Post-Traumatic Stress Disorder Scale (a 10-item scale) PTSD
.94
291
.90
77
Positive Emotion Scales (all 5-item scales)
* **
Happiness
.85
305
.93
77
Self-Esteem
.84
304
.92
76
Intimacy
.92
303
.89
78
Productivity
.87
302
.87
78
Fun
.79
299
.85
79
Hope
.93
298
.88
79
Freedom from Fear
.90
297
.86
79
Spirituality
.94
296
.91
78
This analysis included 21 veterans measured on 18 consecutive weeks. The large Ns reflect the fact that each veteran repeated the test up to 18 times. These two columns included data from 79 veterans measured at intake only.
Update on Reliability and Validity Information
Page 6
Table 2. Reliability and Concurrent Validity Data, Burns Depression Checklist (Burns-D) from the Atlanta VA and Eastern Kentucky Studies (Sekirnjak, 1998; Sekirnjak & Beal, 1999a).
Burns-D (15-item)
Burns-D (25-item)
Cronbach’s coefficient alpha
Comparison Scale
Population
N
r
p
--
BDI (Beck Depression Inventory)
76 undergraduates and 32 outpatients from community mental health centers in Eastern Kentucky (55% mood disorders, 26% substance abuse, 13% anxiety disorders, 7% other)
108
.92
< .001
--
SDS (Zung Depression Scale)
.87
< .001
0.95
SCL-90 R (depression scale)
.89
< .001
Same population
Consecutive outpatients at the Atlanta Kaiser mental health system
137
Update on Reliability and Validity Information
Page 7
Table 3. Reliability and Concurrent Validity, Burns Anxiety Inventory (Burns-A) from the Atlanta VA and Eastern Kentucky Studies (Sekirnjak, 1998; Sekirnjak & Beal, 1999b). Cronbach’s coefficient alpha
Comparison Scale
Population
N
r
p
Burns-A (25-item)
0.95
SCL-90 R (anxiety subscale)
Consecutive outpatients at the Atlanta Kaiser mental health system
131
.88
< .001
Burns-A (33-item)
--
BAI (Beck Anxiety Inventory)
76 undergraduates and 32 outpatients from community mental health centers in Eastern Kentucky (55% mood disorders, 26% substance abuse, 13% anxiety disorders, 7% other)
108
.93
< .001
Burns-A (33-item)
--
SAS (Zung Anxiety Scale)
.91
< .001
Same population
Update on Reliability and Validity Information
Page 8
Table 4. Means, Standard Deviations, T-Values, and Significance Levels for the Clinical and Nonclinical Groups in the Kentucky Study (Sekirnjak, 1998). Nonclinical (N = 76)
Clinical (N = 32)
TValue
Significance Level
Burns-D (15-item version)
10.18 (12.56)
23.91 (12.56)
5.74
0.0001
Burns-A (33-item version)
17.88 (16.35)
47.16 (24.33)
6.23
0.0001
BDI (Beck Depression Inventory)
9.11 (7.59)
23.03 (12.54)
5.83
0.0001
BAI (Beck Anxiety Inventory)
8.62 (9.43)
26.09 (15.86)
5.82
0.0001
SDS (Zung Depression Scale)
45.57 (11.51)
63.91 (16.60)
5.70
0.0001
SAS (Zung Anxiety Scale)
44.50 (12.93)
62.28 (15.05)
5.84
0.0001
Update on Reliability and Validity Information
Page 9
Table 5. Discriminant Validity for the Burns-D and Burns-A in the Atlanta Kaiser Study. Burns-D
Burns-A
Burns-D (25-item)
1.00
Burns-A (25-item)
.72 (n = 129, p < .0001)
1.00
Relationship Satisfaction Score (RSAT)
-.05 (n = 136, ns)
.01 (n = 135, ns)
SCL-Depression
.89 (n = 131, p < .0001)
.79 (n = 132, p < .0001)
SCL-Anxiety
.60 (n = 132, p < .0001)
.88 (n = 131, p < .0001)
SCL-Hostility
.42 (n = 131, p < .0001)
.57 (n = 131, p < .0001)
SCL-Agoraphobia
.43 (n = 136, p < .0001)
.58 (n = 136, p < .0001)
Update on Reliability and Validity Information
Page 10
Table 6. Correlations Among the Burns-D and Burns-A Subscales in the Atlanta Kaiser Study.*
*
Burns-A Total Score (25 items)
Burns-A Thoughts and Feelings (12 items)
Burns-A Physical Symptoms (13 items)
Burns-D total (all 25 items)
.72
.78
.57
Burns-D Thoughts and Feelings (10 items)
.66
.77
.47
Burns-D Activities (7 items)
.63
.68
.50
Burns-D Somatic (5 items)
.66
.59
.61
Burns-D Suicide (3 items)
.34
.36
.28
N = 129 to 151 for the various correlations, p < .001 for all.
Update on Reliability and Validity Information
Page 11
References Cohen, T. J., Thayapran, N., Muhlen, F. v.z., Ibrahim, B., & Quan, W. (1999). The Association of Anxiety and Neurocardiogenic Syncope During Head-Up Tilt Table Testing. (Manuscript under review.) Johnson, K. K. (2000). Concurrent Validaton of the Burns Anxiety Inventory (Burns-A) Using the Beck Anxiety Inventory (BAI) and the Profile of Mood States (POMS). Submitted to the Graduate School of Eastern Kentucky University in partial fulfillment of the requirements for the degree of Master of Science. The author reported strong and significant correlations between the Burns-A and BAI and POMS T-Scale (tension/anxiety), supporting the concurrent validity of the Burns-A. Marr, I. B. (May, 2000). Concurrent Validation of the Burns Depression Inventory (Burns-D). Submitted to the Graduate School of Eastern Kentucky University in partial fulfillment of the requirements for the degree of Master of Science. The author reported that significant correlations between the Burns-D and Beck Depression Inventory / Second Edition (BDI-II) and the Symptom-Checklist-90Revised (SCL-90-R) in a group of 91 undergraduate and 8 graduate students, supporting the concurrent validity of the Burns-D. Rabenhorst, M. M. (May, 2000). The Burns Anxiety Inventory: A Psychometric Analysis. Submitted to the Graduate School of Eastern Kentucky University in partial fulfillment of the requirements for the degree of Master of Science. The author concludes that the results of this study "support the concurrent validity of the Burns Anxiety Inventory with the Beck Anxiety Inventory and Multiple Affect Adjective Check List-Revised" in a group of 100 undergraduates. Sekirnjak, G. C. (1998). Concurrent Validation of the Burns Depression Checklist and the Burns Anxiety Inventory. Submitted to Faculty of the Graduate School of Eastern Kentucky in partial fulfillment of the requirements for Master of Science. For more information, contact Dr. Don Beale, 606-622-1105. Sekirnjak, G. C., & Beal, D. (1999a). Concurrent Validation of the Burns Depression Checklist. Presented at the Annual Meeting of the Association for the Advancement of Behavior Therapy, Toronto, Canada. Sekirnjak, G. C., & Beal, D. (1999b). Concurrent Validation of the Burns Anxiety Inventory. Presented at the Annual Meeting of the Association for the Advancement of Behavior Therapy, Toronto, Canada.
4—Extremely
3—A lot
Instructions. Use checks () to indicate how much you have experienced each symptom in the past week, including today. Please answer all the items.
2—Moderately
Post-Traumatic Stress Disorder*
1—Somewhat
Today's Date:
0—Not at all
Name:
Category A: Exposure to a Traumatic Event 1. Have you experienced or witnessed a traumatic event such as death, serious injury, or a threat to your life or someone else's? 2. Did you feel intensely afraid, helpless or horrified when this event occurred? Category B: Persistent Memories 3. 4. 5. 6. 7.
Do upsetting memories of the traumatic event come into your mind over and over? Do you have upsetting dreams about the traumatic event? Do you have flashbacks and feel like the event is happening again? Do you get upset when you think about the event or when you're reminded of it? Do you have strong physical sensations, such as increased heart rate or sweating, when you're reminded about the event? Category C: Avoidance
8. 9. 10. 11. 12. 13. 14.
Do you avoid thinking or talking about the event? Do you avoid people, things, or places that remind you of the event? Are there parts of the event you can't recall? Have you lost interest in life? Do you often feel isolated or alienated from other people? Do you feel numb or unable to experience love, pleasure and happiness? Do you often feel like you have no future? Category D: Agitation and Arousal
15. 16. 17. 18. 19.
Do you have trouble sleeping? Do you get irritable or have angry outbursts? Do you have trouble concentrating? Are you always on the lookout to make sure you don’t experience the event again? Do you get startled easily? Category E: Distress
20. How much do your reactions to this event interfere with your life? Category F: Duration How long have you experienced these kinds of symptoms? If unsure, just estimate. Years
Months
Use checks () to indicate the types of traumatic event(s) you experienced, with the dates. Traumatic Event
()
Date
Traumatic Event
Accident
War trauma
Natural disaster
Physical assault
Sexual assault
Torture
Being in prison
Serious illness
()
Other event (describe):
*
Copyright 1996 by David D. Burns, M.D. Revised, 2001, 2002.
Date
PTSD Scale
Page 2
How to Score the 20-Item PTSD Scale* Many symptoms on this scale are not specific to PTSD, and are often observed in other Axis I or Axis II disorders. I've listed these non-specific symptoms in the following table. Keep this in mind when you interpret the scores on the test. For example, a severely depressed individual could easily score 24 on this test, and still have no absolutely no history or symptoms suggesting PTSD. Someone who is depressed, anxious and angry could score a 36 or higher, and still have no specific symptoms of PTSD. Disorder
Scale items
Depression
11, 12, 13, 14, 15, 17, 20
Anxiety
12, 15, 17, 19, 20
Anger, relationship problems, mania, or personality disorders (such as BPD)
12, 13, 16, 20
Why is this? Is there something wrong with this PTSD test? Yes there is. The test is modeled after the DSM-IV Diagnostic Criteria for PTSD and is intended to assist you in screening for this disorder. However, the DSM-IV criteria contain approximately 11 symptoms that are reasonably specific to PTSD and 9 symptoms that are rather non-specific, as you've just seen. Any test that maps onto these criteria will necessarily be flawed, because the DSM-IV criteria for PTSD are flawed. The grouping categories don't always make much sense, either, and they would not hold up in a factor analysis. For example, item 7 seems to belong in category D, since it reflects agitation. However, DSM-IV places it in the Persistent Memories category, and that's why you'll find it there. You will find many other inconsistencies if you examine the test critically. However, the goal was not to create the finest possible PTSD test, but rather to create a user-friendly test that will make it easy for you to assess the DSM-IV criteria quickly and accurately. Score
Interpretation
0–2
Few or no symptoms of PTSD
3–5 6 – 10 11 – 20 21 – 40
Comment
Nine of the 20 test items assess Few, if any, symptoms of PTSD symptoms of depression, anxiety, and anger, and are not specific to PTSD. Borderline symptoms of PTSD Scores in this range may result from other disorders. The non-specific Mild symptoms of PTSD symptoms may inflate the total score. Moderate symptoms of PTSD
41 – 60
Severe symptoms of PTSD
61 – 80
Extreme symptoms of PTSD
*
Scores this high are likely to be due to PTSD.
Copyright 1996 by David D. Burns, M.D. Revised, 2001, 2002.
0–No
2–Yes
T = Testing
Use checks () to indicate whether you (or another therapist) skillfully processed the TEAM assessment tests during today’s session. Please answer all the items.
1–Maybe
Rating of Therapy Session* Complete this form after each TEAM therapy session.
Skillfully processed today’s Brief Mood Survey “before session” scores Skillfully processed last session’s Brief Mood Survey “after session” scores Skillfully processed last session’s Evaluation of Therapy Session ratings
1. 2. 3.
E = Empathy (Therapist use of Five Secrets) I was warm, supportive, and concerned. I seemed trustworthy. I treated the patient with respect. I did a good job of listening. I understood how my patient felt inside.
4. 5. 6. 7. 8.
Total A = (Paradoxical) Agenda Setting 9. 10. 11. 12. 13.
Invitation step Specificity step Conceptualization (as mood, relationship, habit, or non-problem) Assessment and management of outcome resistance Assessment and management of process resistance Total M = Methods
14. 15. 16. 17. 18.
Discussion of psychotherapy homework Selection of methods tailored to specified problem(s) Skillful use of selected method(s) during session Therapy approach optimal for the patient’s problems or concerns Meaningful psychotherapy homework was assigned Total
19.
What aspect of this session do you believe was most helpful for the patient?
20.
What mistakes did you make? What will you do differently next session?
Continue on reverse if needed. * Copyright © 2012 by David Burns, MD and Mickey Trockel, MD PhD. Revised 2013.
4–Extremely skillful
3–Very skilful
2–Moderately skilful
1–Slightly skilful
Use checks () to indicate how skillfully you (or another therapist) implemented other aspects of TEAM therapy during today’s session.
0–No / not skillful
Total
Scoring Keys Depression, Anxiety, Panic, and Anger Scales
Relationship Satisfaction Scale
Score
Interpretation
Score
Satisfaction
0
no symptoms
0 - 10
extremely dissatisfied
1-2
borderline
11 - 15
very dissatisfied
3-5
mild
16 - 20
moderately dissatisfied
6 - 10
moderate
21 - 25
marginal
11 - 15
severe
26 - 28
moderately satisfied
16 - 20
extreme
29 - 30
Extremely satisfied
Therapeutic Empathy Scale Score
Satisfaction Level
20
Excellent
19
Surprisingly, this score indicates a failure in the therapeutic alliance.
15 - 18
Not so good
10 - 14
Marginal at best
5-9
Poor
0-4
Alarming
Interpretation Good job! The patient appears to be very satisfied with the warmth, trust, respect, and understanding that she or he experienced during the session. A 19 seems excellent, and most therapists would be thrilled with it, but there’s a problem that needs to be addressed. It can be hard for patients to criticize therapists, and you won’t know the extent of the difficulty until you talk it over with your patient. The failure could be mild, moderate, or even severe. There’s definitely room for improvement. Scores of 18 always indicate fairly significant failures of therapeutic warmth, trust, or understanding. Scores of 15 are quite low. There are substantial and potentially serious feelings of dissatisfaction in more than one area. There are severe problems in many areas of the therapeutic alliance. Scores this low are unusual. This score nearly always indicates extreme problems in warmth, trust or understanding that need to be addressed immediately.
This file contains information on scoring the experimental scales in the 1997 upgrade to the Therapist's Toolkit.
Scoring Key for the 10-Item Panic Test Score
Interpretation
0
No panic
1–5
Slight feelings of panic
6 – 10
Mild panic
11 – 20
Moderate panic
21 – 30
Severe panic
31 – 40
Extreme panic
Ask the patient about the time frame that they had in mind when answering the test. Were they thinking about how they feel most of the time, or how they feel during an episode of panic? How often do they have panic episodes? How intense are they? What are they thinking about during these attacks? Remember that unlike depression, panic attacks are very episodic and develop suddenly. They usually reach a crescendo within ten minutes, and often disappear entirely within 30 to 90 minutes, leaving the victim feeling frightened, ashamed, and confused.
Scoring Keys for Experimental Scales
Page 2
Scoring Key for the 10-Item Agoraphobia Test Score
Interpretation
0
No agoraphobia
1–5
Slight feelings of agoraphobia
6 – 10
Mild agoraphobia
11 – 20
Moderate agoraphobia
21 – 30
Severe agoraphobia
31 – 40
Extreme agoraphobia
The Agoraphobia Test is not necessarily interpreted in a strictly continuous fashion, from 0 to 40, but should be viewed as a probe to determine if the patient has agoraphobic symptoms that should be explored by the therapist to confirm the diagnosis. For example, the patient could in theory answer “extremely” on the first three items, but have low answers for many of the remaining items on the test. This is because those first three items ask about agoraphobia in general, whereas many of the remaining questions ask about specific types of feared situations. Thus, the patient could score around 20 on the test, or even lower, and still be extremely agoraphobic. These are the first three items on the test: 1. Fears of being away from home alone 2. Needing a trusted companion when you are away from home 3. Fears that something terrible may happen if you are alone In all cases, your clinical judgment will help you pinpoint the diagnosis. If you ask the patient to complete the test once per week during treatment, the changes in the scores will help you track progress. Ultimately, you will want the patient's scores to fall below 5, and as close to zero as possible.
Scoring Keys for Experimental Scales
Page 3
Scoring Key for the 10-Item Social Anxiety Test Score
Interpretation
0
No social anxiety
1–5
Minimal anxiety in social situations
6 – 10
Borderline social anxiety
11 – 20
Mild social anxiety
21 – 30
Moderate social anxiety
31 – 40
Severe social anxiety
Scoring Key for the 10-Item PTSD Test Score
Interpretation
0
No symptoms of PTSD
1–5
Minimal anxiety possibly associated with a traumatic event
6 – 10
Mild symptoms of PTSD
11 – 20
Moderate symptoms of PTSD
21 – 30
Severe symptoms of PTSD
31 – 40
Extreme symptoms of PTSD
Scoring Keys for Experimental Scales
Page 4
Scoring Key for the 32-Item OCD Test, Page 1 Items 1 - 10: Obsessive Concerns Items 11 - 20: Compulsive Rituals The two ten-item scales on the first page ask about obsessions (items 1 – 10) and compulsions (items 11 – 20). You should view these tests primarily as screening tools for OCD. If one or more items are checked, you will want to confirm the diagnosis using DSM-IV criteria. The first two ten-item scales are not to be interpreted in a strictly continuous fashion. For example, a person could have only one or two obsessions and rituals and therefore have a low score on these first two subscales. Nevertheless, the person could be severely crippled by the disorder if the obsessions and compulsions are creating a tremendous disruption, as is often the case.
Scoring Key for the 32-Item OCD Test, Page 2 Items 1 - 5: Distress due to Obsessions Items 6 - 10: Distress due to Compulsions The scales on page 2 can help you assess the severity of the OCD in terms of the distress the person experiences, as well as the amount of time she or he spends each day with obsessive worrying and compulsive rituals. Thus, the two five-item scales on the second page can be administered on a weekly basis to assess progress. Each fiveitem scale can be interpreted in a continuous fashion as follows: Distress Score
Interpretation
0
No distress
1–4
Minimal distress
5–8
Mild distress
9 – 12
Moderate distress
13 – 16
Severe distress
17 – 20
Extreme distress Items 11 and 12: Time Spent
These two time scales are simple to interpret. Ideally, the time spent on obsessive worrying and compulsive rituals will decrease with treatment. These scales should be given weekly to assess progress. The goal is to get the time spent down to 0 (no time at all) or 1 (just a few minutes) using Exposure and Response Prevention, along with other treatment techniques.
Scoring Keys for Experimental Scales
Page 5
Scoring Key for the 5-Item Positive Feelings Tests, including: Self-Esteem Feeling Good about Others Happiness Productivity
Playfulness Freedom from Fear Hope Spiritual Awareness
Score
Interpretation
0–1
Extremely unhappy or negative
2–5
Very unhappy or negative; severe difficulties
6 – 10
Only somewhat positive
11 – 15
Moderately positive, but much room for improvement
16 – 18
Very positive, with some room for improvement
19 – 20
Extremely positive; the highest possible score
Scoring Keys for Experimental Scales
Page 6
Scoring Key for the Full Anger Test Items 1 - 10: Feelings of Anger and Resentment Score
Interpretation
0
No anger
1–5
Slight annoyance or irritation
6 – 10
Mild anger
11 – 20
Moderate anger
21 – 30
Severe anger
31 – 40
Extreme anger
Items 11 - 15: Violent Fantasies and Urges Instructions. Examine items 11 and 12 first. These two items ask about violent thoughts and fantasies. If either or both of these are greater than 0, the person is acknowledging some violent or aggressive fantasies. This is not unusual or necessarily a cause for alarm. Many people have violent fantasies and never act on them. Since a few people unfortunately do act on these fantasies, you will need to ask the patient for more information. Try to confirm whether she or he has any intention of acting on the fantasies, now or at any time in the future. Now examine items 13 to 15. These three items ask about violent urges and plans. Any answer greater than 0 on any of these three items could be significant. The higher the score on these items, the greater the risk, but any score above 0 requires careful interviewing by the therapist to assess the actual threat or danger. The following list of interview areas is not intended to be comprehensive but simply to give you a starting point. Ask the patient specific questions like these to assess the level of danger: Who is the intended victim(s)? What is the method of violence? How dangerous is the method (slapping vs. shooting, for example)? How powerful is the violent urge, between 0 and 100, at this moment? How powerful is the violent urge, between 0 and 100, when it is the strongest? Has the patient prepared for violence, such as buying a gun or stalking the victim? Does the patient have any plans, now or in the future, to act on these fantasies? Are there any deterrents to acting violently, such as the fear of jail or religious beliefs? What are these deterrents? How strong are they? Is there anything that might trigger the patient to act on the fantasies?
Scoring Keys for Experimental Scales
Page 7
What circumstances, if any, might make the patient feel especially angry and violent (like seeing the wife flirting with another man)? How likely is it that this will happen? Has the patient ever threatened violence, or committed violent acts, in the past? Has the patient ever abused drugs or alcohol? If so, the threat of violence will be greater. Does the patient sometimes become delusional or paranoid? Keep in mind that when a specific threat is made to another person, you may have the duty, according to the Tarasoff I ruling, to warn the potential victim. There is also the Tarasoff II ruling, which is the duty to protect the intended victim. When you are unsure about the potential for violence or your legal and ethical obligations, it would be wise to get an emergency consultation. Choose a colleague or expert who can advise you about the ethics of the situation as well as how to do a thorough and competent evaluation of the patient’s potential for violence. Remember to document your violence assessment carefully and specifically in the chart. For example, it would probably be wise to record the answer to each of the bulleted items above, along with your final assessment of the patient's potential for violence, your plan of action, and your rationale. If the person scores a zero on items 11 – 15, I would confirm this score by saying, “It looks like you have no violent fantasies or urges at all. If you did have some violent fantasies and urges, would it be easy for you to tell me about them, or would it be difficult?” The patient may say, “It would be easy.” If you are not entirely convinced, you might ask them a second question in a friendly way. You can say, "That's great. It would be hard for most people. Why would it be easy for you?" If, instead, the patient says, “It would be hard,” then this should raise your suspicion immediately that there may be violent urges the patient is hiding. Some patients may deny their violent urges. It is important for you to find this out, if possible, so you can try to assess the urgency of the situation. If the patient acknowledges it would be difficult to admit having these urges, it indicates a lack of trust in the therapist or the therapeutic situation. You might say, “It sounds like it would be pretty hard to admit to me that you felt really violent or wanted to blow someone away. What do you think would happen if you did tell me about these fantasies and urges?” You might also say, “I am assuming, then, that you may have some violent urges or fantasies, which are not unusual, but that it is hard for you to tell me about them because you are not sure you can trust me. Is this correct?” The rationale for saying, “which are not unusual” is to suggest to the patient that you are not going to be judgmental. From a therapeutic point of view, I would find it excessively stressful and unacceptable to try to treat a potentially violent outpatient who was withholding information from me. I would feel like a hostage, because at any time the patient might act out unpredictably, and I might be held accountable for that patient's actions from a medical-legal perspective. In essence, I would be assuming responsibility for a patient without being empowered to treat the patient in an adequate and effective manner. In such a situation, I would immediately obtain a consultation from a colleague with expertise in
Scoring Keys for Experimental Scales
Page 8
treating difficult patients and explore alternative treatment plans, such as hospitalization. Of course, you will need to explain to the prospective patient why you may not be able to accept him or her as a patient under these conditions, because you are not convinced you can personally deliver safe and effective treatment. Be sure, however, that you have worked with the patient to find an alternative and acceptable treatment option. You do not want to make the mistake of patient abandonment, for which you can also be sued. This topic is unfortunately difficult and anxiety provoking. I believe that many therapists avoid dealing with their patients’ anger or violent urges. These therapists may think their patients are too nice to do something violent, or they may feel uncomfortable asking such pointed questions. Our society has become increasingly violent and litigious. Unfortunately, therapists can be held accountable for the actions of their patients, even months after patients have terminated treatment. For these reasons, it is wise to learn to assess violence and violent urges effectively, even if it is a bit uncomfortable at first. When in doubt, obtain a consultation from an expert, and carefully document your own assessment, as well as the consultation, in the chart. Items 16 – 20: Difficulties with the Test Instructions. The final five items ask the patient how difficult it was to answer the items honestly. Any answer of 1 or more indicates that the patient had some trouble being completely candid. You can ask the patient about this in a tactful and respectful way. For example, item 16 reads, “I had difficulty answering some of the questions honestly.” If the patient indicated some agreement with this item, you might say, “I take it that it wasn’t always easy for you to answer these items in a completely open way. I appreciate your telling me this. I know it can be hard to talk about violent and aggressive urges. Can you tell me which items were particularly hard for you to answer?” The idea here is not to confront or challenge the patient, but to respond in a supportive and non-judgmental way so the patient will feel safe to open up a bit more. If the answer on all of the final five items was 0, you can confirm this score by saying, “I take it that it was easy for you to answer the items on the test. Is this correct?”
Therapist Instructions for the Side Effects Checklist The Side Effects Checklist will be most useful for physicians. However, you may want to monitor side effects even if you are a non-medical therapist and someone else is prescribing medications for your patients. This will give you a far better understanding of your patients' somatic complaints. Sometimes side effects result from mood problems, and sometimes they're caused by medications. In fact, any "side effect" can occur in individuals who are not taking any medications at all. For example, depression can cause fatigue, anxiety can cause dizziness and palpitations, and anger can trigger headaches or backaches. There's an innovative way to sort this out. Ask all your patients to complete the Side Effects Checklist at least once BEFORE starting any new medications. Do this even if the patient isn't taking any medications at all. After you have one or two baseline readings with the Side Effects Checklist, you can start the medication. Then ask the patient to complete the checklist at weekly intervals, or more frequently if you feel the need. Any significant change in side effects may be the result of the medication. For example, if the patient suddenly begins to report fatigue, and this symptom was not previously present, it could be the result of the drug. However, you can never be absolutely sure that a new side effect is the result of the drug. This is because patients who receive placebos also experience lots of new side effects that are indistinguishable from "real" drug side effects. If a side effect was present before the patient started the medication, and the severity does not increase, then the side effect probably did not result from the drug. This is why the baseline readings can be so helpful. Otherwise, you might falsely conclude that the drug is causing a troublesome side effect and unnecessarily reduce the dose or switch to another drug in an attempt to correct the problem. You can keep the completed copies of the checklist in the patient's chart. This will provide you with an accurate record of every side effect the patient has experienced during your work together. For convenience, you can photocopy the checklist two-sided on one piece of paper.
Mouth and Stomach 1. 2. 3. 4. 5. 6. 7. 8. 9.
Dry mouth Frequently thirsty Loss of appetite Nausea or vomiting Stomach cramps or upset stomach Increase in appetite or eating too much Weight gain or loss Constipation Diarrhea Eyes and Ears
10. 11. 12. 13.
Blurred vision Overly sensitive to light Changes in vision, such as halos around objects Ringing in your ears Skin
14. 15. 16. 17. 18.
Sweating too much Rash Excessive sunburn when exposed to sun Change in skin color Bleeding or bruising easily Sex
19. 20. 21. 22. 23.
Loss of interest in sex Difficulties getting sexually excited Difficulties getting an erection (men) Difficulties having an orgasm Difficulties with your period (women)
24. 25. 26. 27. 28.
Stimulated or overly excited Agitated or pacing about Anxious, worried or nervous Feeling strange or “spaced out” Excess energy
Stimulation and Nervousness
(Continue on reverse)
*
Copyright © 1998 by David D. Burns, M.D.
4—Extremely
3—A Lot
Instructions. Use checks () to indicate whether you've been bothered by each side effect during the past several days. Please answer all the items.
2—Moderate
Side Effects Checklist*
1—Somewhat
Date:
0—Not at All
Name:
Sleep Problems 29. 30. 31. 32. 33. 34. 35.
Feeling tired or exhausted Loss of energy Sleeping too much Trouble falling asleep Sleep that is restless or disturbed Waking up too early in the morning Nightmares or strange dreams Muscles and Coordination
36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47.
Muscle jerks or twitches Slurred speech Tremor Difficulty walking or loss of balance Feeling slowed down Stiffness of the arms, legs or tongue Feeling restless, or constantly moving your arms or legs Hand-wringing Constant, rhythmic leg jiggling Abnormal movements of your face, lips, tongue Abnormal movements of other parts of your body Muscle spasms of your tongue, jaw or neck Other
48. 49. 50. 51. 52. 53. 54. 55.
Difficulty remembering things Feeling dizzy, light-headed or faint Feeling your heart race or pound Swelling in your hands, arms, legs or feet Trouble starting urination Headache Breast swelling or enlargement Milk secretion from the nipples
Please describe any other side effects:
*
Copyright © 1998 by David D. Burns, M.D.
4—Extremely
3—A Lot
2—Moderate
(cont'd)
1—Somewhat
Side Effects Checklist*
0—Not at All
Page 2
Assessment Tests for Children and Adolescents
Date:
Total
Total
Total
Total
How anxious do you feel right now? 1. I feel scared. 2. I feel worried. 3. I feel afraid. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
How angry do you feel right now? 1. I’m mad. 2. I’m angry. 3. I’m frustrated. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
How shy have you been feeling recently? 1. I feel shy around other people. 2. I’m afraid that people will notice that I feel shy. 3. I often worry that people won’t like me because I’m shy. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
Trouble Concentrating 1. It’s hard for me to pay attention. 2. It’s hard for me to focus on things. 3. It’s hard for me to finish my work. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
Feeling Impulsive 1. I often interrupt people when we’re talking. 2. I sometimes have trouble waiting until it’s my turn. 3. I sometimes grab or touch things I’m not supposed to touch. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
Feeling Restless 1. It’s hard for me to sit still. 2. I often feel restless or squirmy. 3. People often tell me to sit still. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
How suicidal have you been feeling recently? 1. Sometimes I wish I were dead. 2. Sometimes I want to kill or hurt myself.
* Copyright 2010 by David D. Burns, M.D.
4–Completely
3–A lot
2–In between
1–A little true
How does YOUR CHILD feel?
4–Completely
3–A lot
How sad do you feel right now? 1. I feel sad and unhappy. 2. I feel like things will never get better. 3. I’m no good. 4. I feel like a loser. 5. I’m not having any fun. 0 1 - 5 6 - 10 11 - 15 16 - 20
1–A little
Instructions. Use checks () to indicate how you're feeling. Please answer all the items.
0–Not at all
Brief Mood Survey*
2–In between
How do YOU feel?
0–Not at all true
Name:
1. 2. 3. 4. 5.
Therapeutic Empathy The therapist seemed warm, supportive, and concerned. The therapist seemed trustworthy. The therapist treated me with respect. The therapist did a good job of listening. The therapist understood how I felt inside. Total
6. 7. 8. 9. 10.
Helpfulness of the Session I was able to express my feelings during the session. I talked about the problems that are bothering me. The techniques we used were helpful. The approach my therapist used made sense. I learned some new ways to deal with my problems. Total
Satisfaction with Today's Session 11. I believe the session was helpful to me. 12. Overall, I was satisfied with today's session. Total Your Commitment 13. I plan to do therapy homework before the next session. 14. I intend to use what I learned in today's session. Total Negative Feelings During the Session 15. At times, my therapist didn't seem to understand how I felt. 16. At times, I felt uncomfortable during the session. 17. I didn't always agree with my therapist. Total Difficulties with the Questions 18. It was hard to answer some of these questions honestly. 19. Sometimes my answers didn't show how I really felt inside. 20. It would be too upsetting for me to criticize my therapist. Total What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2004.
4–Completely true
3–Very true
Please answer all the items.
2–Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–Somewhat true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
Name:
Date: Before Session
After Session
Total
Total
Total
Total
Total
Total
Total
Total
Total
Total
Total
Total
Total
Total
How suicidal have you been feeling recently? 1. Sometimes I wish I were dead. 2. Sometimes I want to kill or hurt myself. How anxious do you feel right now? 1. I feel scared. 2. I feel worried. How shy do you feel right now? 1. I feel shy around other people. 2. I worry that people won’t like me because I’m shy. How angry do you feel right now? 1. I’m mad. 2. I’m angry. Trouble Concentrating 1. It’s hard for me to pay attention. 2. It’s hard for me to focus on things. Feeling Restless 1. It’s hard for me to sit still. 2. I feel restless or squirmy.
* Copyright 2010 by David D. Burns, M.D.
4–Completely
3–A lot
2–In between
1–A little
0–Not at all
4–Completely
3–A lot
2–In between
How sad do you feel right now? 1. I feel sad and unhappy. 2. I feel like things will never get better. 3. I’m no good. 4. I feel like a loser. 5. I’m not having any fun.
1–A little
Instructions. Use checks () to indicate how you're feeling. Please answer all the items.
0–Not at all
Brief Mood Survey*
Please fill this out AFTER the session. Thank you!
Total Therapist Understanding 1. My therapist understands how I’m feeling. 2. My therapist understands my problems. Total Your Satisfaction 1. The session was helpful to me. 2. I liked today's session. Total Negative Feelings During the Session 1. At times, my therapist didn't understand how I felt. 2. At times, I felt uncomfortable during the session. Total Difficulties with the Questions 1. It was hard to be honest during the session. 2. It would be upsetting to have to say bad things about my therapist. Total What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2010 by David D. Burns, M.D.
4–Completely true
3–Very true
2–In between
Talking about Feelings 1. I told my therapist how I was feeling. 2. I talked about the problems that are bothering me.
1–A little true
Instructions. Use checks () to indicate how you felt about your most recent therapy session. Please answer all the items.
0–Not at all true
Evaluation of Therapy Session*
Children’s Brief Mood Survey and Evaluation of Therapy Session Name of Scale 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15.
Sadness (Depression) Suicidal Urges Anxiety Shyness Anger Hyperactivity Trouble Concentrating Feeling Impulsive Feeling Restless Therapist Kindness Talking about Feelings Therapist Understanding Your Satisfaction Negative Feelings During the Session Difficulties with the Questions
Number of Items 5 2 3 3 3 9 3 3 3 2 2 2 2
Scale Reliability (Coefficient Alpha) .80 .90 .94 .87 .94 .86 .87 .87 .85 .97 .86 ---
New scale—currently under study. New scale—currently under study.
3
--
New scale—currently under study.
4
--
New scale—currently under study.
Comment
Includes the three subscales
These values are based on our pilot study with 62 children, and are good to excellent. In many cases, I was confronted by significant range restriction problems. For example, very few children had elevated depression scores. Range restriction causes an artificial reduction of the values of correlations, including Cronbach’s coefficient alpha, which is the reliability coefficient listed for each scale on this table. The actual reliabilities for some of the scales may be significantly higher than those listed above. Scoring Keys: At the bottom of the most of the scales on the Brief Mood Survey, you will find a scoring key that looks like something like this: 0
1- 3
4- 6
7 - 9 10 - 12
Here’s what these categories mean— 5-item scales
3-item scales
0 1-5 6 - 10 11 - 15 16 - 20
0 1–3 4–6 7–9 10 - 12
No symptoms No symptoms Minimal to borderline symptoms Mild symptoms Moderate symptoms Severe symptoms
On the Suicidal Urges scale, any elevated scores need to be explored. On the Therapist Kindness, Talking about Feelings, Therapist Understanding, and Your Satisfaction scales, any scores below perfect scores indicate significant problems in the therapeutic alliance that need to be explored, as do any scores greater than 0 on the Negative Feelings During the Session scale as well as the Difficulties with the Questions scale.
Date:
Total
Total
Total
Total
How anxious do you feel right now? 1. I feel scared. 2. I feel worried. 3. I feel afraid. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
How angry do you feel right now? 1. I’m mad. 2. I’m angry. 3. I’m frustrated. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
How shy have you been feeling recently? 1. I feel shy around other people. 2. I’m afraid that people will notice that I feel shy. 3. I often worry that people won’t like me because I’m shy. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
Trouble Concentrating 1. It’s hard for me to pay attention. 2. It’s hard for me to focus on things. 3. It’s hard for me to finish my work. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
Feeling Impulsive 1. I often interrupt people when we’re talking. 2. I sometimes have trouble waiting until it’s my turn. 3. I sometimes grab or touch things I’m not supposed to touch. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
Feeling Restless 1. It’s hard for me to sit still. 2. I often feel restless or squirmy. 3. People often tell me to sit still. 0 1 - 4 5 - 7 8 - 9 10 - 12
Total
Total
How suicidal have you been feeling recently? 1. Sometimes I wish I were dead. 2. Sometimes I want to kill or hurt myself.
* Copyright 2010 by David D. Burns, M.D.
4–Completely
3–A lot
2–In between
0–Not at all true
After Session 4–Completely
3–A lot
How sad do you feel right now? 1. I feel sad and unhappy. 2. I feel like things will never get better. 3. I’m no good. 4. I feel like a loser. 5. I’m not having any fun. 0 1 - 5 6 - 10 11 - 15 16 - 20
1–A little
Instructions. Use checks () to indicate how you're feeling. Please answer all the items.
0–Not at all
Brief Mood Survey*
2–In between
Before Session
1–A little true
Name:
Therapist Kindness 1. My therapist was nice to me. 2. My therapist listened. Total Talking about Feelings 1. I told my therapist how I was feeling. 2. I talked about the problems that are bothering me. Total Therapist Understanding 1. My therapist understands how I’m feeling. 2. My therapist understands my problems. Total Your Satisfaction 1. The session was helpful to me. 2. I liked today's session. Total Negative Feelings During the Session 1. At times, my therapist didn't understand how I felt. 2. At times, I felt uncomfortable during the session. 3. I didn't always agree with my therapist. Total 1. 2. 3. 4.
Difficulties with the Questions It’s hard to talk about my feelings and problems. It was hard to be honest during the session. It was hard to answer some of these written questions honestly. It would be upsetting to have to say bad things about my therapist. Total
What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2010 by David D. Burns, M.D.
4–Completely true
3–Very true
Please answer all the items.
2–In between
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1–A little true
Evaluation of Therapy Session*
0–Not at all true
Please fill this out AFTER the session. Thank you!
Assessment Tests for Medical Settings
1. I feel worthwhile. 2. I feel close to people. 3. People support and care about me. 4. I enjoy life. 5. I often laugh and smile. 6. I feel motivated to do things. 7. I feel productive. 8. I feel hopeful. 9. I feel peaceful. 10. My life has a deeper meaning. Total Items 1 to 10
Scoring Key Score
Interpretation
0–8
Not at all happy or fulfilled
9 – 16
Slightly happy and fulfilled
17 – 24
Moderately happy and fulfilled
25 – 31
Very happy and fulfilled
33 – 40
Extremely happy and fulfilled
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
4—Extremely
3—A lot
2—Moderately
Please answer all the items.
1—Somewhat
Instructions. Use checks () to indicate how you've been feeling over the past week, including today.
0—Not at all
Positive Feelings Test*
Please answer all the items.
4—Extremely
Instructions. Use checks () to indicate how you've been feeling over the past week, including today.
3—A lot
0—Not at all
Brief Mood Survey*
2—Moderately
Date: 1—Somewhat
Name:
Depression 1. 2. 3. 4. 5.
Sad or down in the dumps Discouraged or hopeless Low self-esteem Worthless or inadequate Loss of pleasure or satisfaction in life Total Items 1 to 5
Suicidal Urges** 1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Furious Total Items 1 to 5
Instructions. Please note that in this test, checking Not At All means that you have no positive feelings and checking Extremely means that you have strong positive feelings. Positive Feelings 1. I feel worthwhile. 2. I feel close to people. 3. People support and care about me. 4. I enjoy life. 5. I often laugh and smile. 6. I feel motivated to do things. 7. I feel productive. 8. I feel hopeful. 9. I feel peaceful. 10. My life has a deeper meaning. Total Items 1 to 10
* Copyright 1997 by David D. Burns, M.D. Revised, 2002. ** Anyone with suicidal urges should seek immediate help from a mental health professional.
Page 2 Please complete this page after your visit with your doctor.
Satisfaction with Doctor's Bedside Manner* Instructions. Use checks () to indicate how you felt about your visit with the doctor today. Please answer all 5 items.
0 Not at all true
1 2 Somewhat Moderately true true
3 Very true
4 Completely true
1. My doctor treated me with respect. 2. My doctor seemed genuinely concerned. 3. My doctor listened well. 4. My doctor was easy to talk to. 5. I was satisfied with my doctor visit. Total Items 1 to 5
Satisfaction with Diagnosis and Treatment* Instructions. Use checks () to indicate how you feel about the quality of your medical care. Please answer all 5 items.
0 Not at all true
1 2 Somewhat Moderately true true
3 Very true
1. I was satisfied with the evaluation of my symptoms and medical problems. 2. My doctor clearly explained any testing and follow-up I will need. 3. I'm confident the diagnosis was accurate. 4. I was satisfied with the explanation of the benefits and side effects of medications. 5. I believe I'm receiving good treatment. Total Items 1 to 5
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
4 Completely true
Please answer all the items.
4—Extremely
Instructions. Use checks () to indicate how you've been feeling over the past week, including today.
3—A lot
0—Not at all
Brief Mood Survey*
2—Moderately
Date: 1—Somewhat
Name:
Depression 1. 2. 3. 4. 5.
Sad or down in the dumps Discouraged or hopeless Low self-esteem Worthless or inadequate Loss of pleasure or satisfaction in life Total Items 1 to 5
Suicidal Urges** 1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Furious Total Items 1 to 5
1. 2. 3. 4. 5.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions. Use checks () to show how satisfied or dissatisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5
* Copyright 1997 by David D. Burns, M.D. Revised, 2002. ** Anyone with suicidal urges should seek immediate help from a mental health professional.
Page 2 Please complete this page after your visit with your doctor.
Satisfaction with Doctor's Bedside Manner* Instructions. Use checks () to indicate how you felt about your visit with the doctor today. Please answer all 5 items.
0 Not at all true
1 2 Somewhat Moderately true true
3 Very true
4 Completely true
1. My doctor treated me with respect. 2. My doctor seemed genuinely concerned. 3. My doctor listened well. 4. My doctor was easy to talk to. 5. I was satisfied with my doctor visit. Total Items 1 to 5
Satisfaction with Diagnosis and Treatment* Instructions. Use checks () to indicate how you feel about the quality of your medical care. Please answer all 5 items.
0 Not at all true
1 2 Somewhat Moderately true true
3 Very true
1. I was satisfied with the evaluation of my symptoms and medical problems. 2. My doctor clearly explained any testing and follow-up I will need. 3. I'm confident the diagnosis was accurate. 4. I was satisfied with the explanation of the benefits and side effects of medications. 5. I believe I'm receiving good treatment. Total Items 1 to 5
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
4 Completely true
Please answer all the questions. Depression 1. 2. 3. 4. 5.
4—Extremely
Instructions. Use checks () to indicate how you've been feeling over the past week, including today.
3—A lot
0—Not at all
Brief Mood Survey*
2—Moderately
Date:
1—Somewhat
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem Worthless or inadequate Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges
1. Do you have any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5 * Copyright 1997 by David D. Burns, M.D., revised, 2002.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
Please answer all 5 items.
1—Moderately
Instructions: Place a check ( ) in the box that best describes how satisfied you feel in your closest personal relationship.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
Positive Feelings 1. 2. 3. 4. 5.
My doctor seemed warm, supportive, and concerned. My doctor seemed trustworthy. My doctor treated me with respect. My doctor did a good job of listening. My doctor understood how I felt inside.
6. 7. 8. 9.
I was able to express my feelings during the session. I talked about the problems that are bothering me. The doctor's suggestions were helpful. I learned some new ways to deal with my problems.
Helpfulness of the Session
Explanation of My Condition and Treatment 10. 11. 12. 13.
My doctor answered my questions clearly. My doctor clearly explained my symptoms and diagnoses. S/he answered my questions about the medications I'm taking. My doctor explained any side effects of the medications.
14. 15. 16.
At times, my doctor didn't seem to understand how I felt. At times, I felt uncomfortable during the session. I didn't always agree with my doctor.
Negative Feelings During the Session
Difficulties with the Questions 17. 18.
It was hard to answer some of these questions honestly. It would be too upsetting for me to criticize my doctor. Overall Satisfaction with Today's Session
19. 20.
I believe the session was helpful to me. Overall, I was satisfied with today's session.
What did you like the least about the session?
What did you like the best about the session?
*
Copyright © 2001 by David D. Burns, M.D. Revised, 2002.
4--Completely true
3--Very true
Please answer all the items.
2--Moderately true
Instructions. Use checks () to indicate how you felt about your most recent therapy session.
1--Somewhat true
Evaluation of Therapy Session*
0--Not at all true
Page 2
Cognitive Behavior Therapy (CBT) Tools
Common Self-Defeating Beliefs* Achievement 1. Perfectionism. I must never fail or make a mistake. 2. Perceived Perfectionism. People will not love and accept me as a flawed and vulnerable human being. 3. Achievement Addiction. My worthwhileness depends on my achievements, intelligence, talent, status, income, or looks.
Love 4. Approval Addiction. I need everyone's approval to be worthwhile. 5. Love Addiction. I can't feel happy and fulfilled without being loved. If I'm not loved, then life is not worth living. 6. Fear of Rejection. If you reject me, it proves that there's something wrong with me. If I'm alone, I'm bound to feel miserable and worthless.
Submissiveness 7. Pleasing Others. I should always try to please others, even if I make myself miserable in the process. 8. Conflict Phobia. People who love each other shouldn't fight. 9. Self-Blame. The problems in my relationships are bound to be my fault.
Demandingness 10. Other-Blame. The problems in my relationships are the other person's fault.
Depression 13. Hopelessness. My problems could never be solved. I could never feel truly happy or fulfilled. 14. Worthlessness / Inferiority. I'm basically worthless, defective, and inferior to others.
Anxiety 15. Emotional Perfectionism. I should always feel happy, confident, and in control. 16. Anger Phobia. Anger is dangerous and should be avoided at all costs. 17. Emotophobia. I should never feel sad, anxious, inadequate, jealous or vulnerable. I should sweep my feelings under the rug and not upset anyone. 18. Perceived Narcissism. The people I care about are demanding, manipulative, and powerful. 19. Brushfire Fallacy. People are clones who all think alike. If one person looks down on me, the word will spread like brushfire and soon everyone will look down on me. 20. Spotlight Fallacy. Talking to people feels like having to perform under a bright spotlight on a stage. If I don't impress people by being sophisticated, witty, or interesting, they won't like me. 21. Magical Thinking. If I worry enough, everything will turn out okay.
Other
11. Entitlement. You should always treat me in the way I expect.
22. Low Frustration Tolerance. I should never be frustrated. Life should be easy.
12. Truth. I'm right and you're wrong.
23. Superman / Superwoman. I should always be strong and never be weak.
*
Copyright 2001, by David D. Burns, M.D.
Habit Cost-Benefit Analysis* List the attitude, feeling or habit you want to change: Checking my vision each day.
Advantages
Disadvantages
1. It's reassuring.
1. The odds of a real problem are low.
2. I can catch any problem early
2. The constant checking is unnecessary.
3. I can get help if I need it.
3. The anxiety is ruining my life.
40
60
* Copyright 1984 by David D. Burns, M.D.
Cost-Benefit Analysis* List the attitude, feeling or habit you want to change:
Advantages
Disadvantages
* Copyright 1984 by David D. Burns, M.D.
Cost-Benefit Analysis* List the attitude, feeling or habit you want to change:
Advantages
Disadvantages
* Copyright 1984 by David D. Burns, M.D.
Daily Mood Log Continuation Sheet* % Belief before
Negative Thoughts
*
% Belief after
Distortions
Positive Thoughts
Copyright 1984 by David D. Burns, M.D. Revised 2004.
% Belief
Daily Mood Log Continuation Sheet (cont'd) % Belief before
Negative Thoughts
% Belief after
Distortions
Positive Thoughts
% Belief
Checklist of Cognitive Distortions * 1.
All-or-Nothing Thinking. You look at things in absolute, black-and-white categories.
6.
Magnification or Minimization. You blow things way out of proportion or shrink them.
2.
Overgeneralization. You view a single negative event as a never-ending pattern of defeat.
7.
Emotional Reasoning. You reason from your feelings: “I feel like an idiot, so I must be one.”
3.
Mental filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use “shoulds,” “shouldn'ts,” “musts,” “oughts,” and “have tos.”
4.
Discounting Positives. You insist your positive qualities don't count.
9.
Labeling. Instead of saying, “I made a mistake,” you tell yourself, “I'm a jerk” or “I'm a loser.”
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Self-Blame and Other-Blame.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
*
Copyright 1984 by David D. Burns, M.D. Revised 2004.
Daily Mood Log* Situation or Event: % Before
Emotions
% After
Emotions
Sad, blue, depressed, down, unhappy
Hopeless, discouraged, pessimistic, despairing
Anxious, worried, panicky, nervous, frightened
Frustrated, stuck, thwarted, defeated
Guilty, remorseful, bad, ashamed
Angry, mad, resentful, annoyed, irritated, upset, furious
Inferior, worthless, inadequate, defective, incompetent
Other (describe)
Lonely, unloved, unwanted, rejected, alone, abandoned
Other
Embarrassed, foolish, humiliated, self-conscious
Other
% Belief before
Negative Thoughts
% Belief after
Distortions
Positive Thoughts
1.
1.
2.
2.
3.
3.
4.
4.
*
Copyright 1984 by David D. Burns, M.D. Revised 2001.
% Before
% After
% Belief
Daily Mood Log (cont’d) % Belief before
Negative Thoughts
% Belief after
Distortions
Positive Thoughts
5.
5.
6.
6.
7.
7.
8.
8.
% Belief
Checklist of Cognitive Distortions * 1.
All-or-Nothing Thinking. You look at things in absolute, black-and-white categories.
6.
Magnification or Minimization. You blow things way out of proportion or shrink them.
2.
Overgeneralization. You view a single negative event as a never-ending pattern of defeat.
7.
Emotional Reasoning. You reason from your feelings: “I feel like an idiot, so I must be one.”
3.
Mental filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use “shoulds,” “shouldn'ts,” “musts,” “oughts,” and “have tos.”
4.
Discounting Positives. You insist your positive qualities don't count.
9.
Labeling. Instead of saying, “I made a mistake,” you tell yourself, “I'm a jerk” or “I'm a loser.”
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Self-Blame and Other-Blame.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
*
Copyright 1984 by David D. Burns, M.D. Revised 2001.
Daily Mood Log* Situation or Event: % Before
Emotions
% After
Emotions
Sad, blue, depressed, down, unhappy
Hopeless, discouraged, pessimistic, despairing
Anxious, worried, panicky, nervous, frightened
Frustrated, stuck, thwarted, defeated
Guilty, remorseful, bad, ashamed
Angry, mad, resentful, annoyed, irritated, upset, furious
Inferior, worthless, inadequate, defective, incompetent
Other (describe)
Lonely, unloved, unwanted, rejected, alone, abandoned
Other
Embarrassed, foolish, humiliated, self-conscious
Other
% Belief before
Negative Thoughts
% Belief after
Distortions
Positive Thoughts
1.
100
1.
2.
100
2.
3.
80
3.
4.
100
4.
*
Copyright 1984 by David D. Burns, M.D. Revised 2001.
% Before
% After
% Belief
Daily Mood Log (cont’d) % Belief before
Negative Thoughts
5. David is not genuinely interested in me.
% Belief after
Distortions
Positive Thoughts
% Belief
5.
95
6.
6.
7.
7.
8.
8.
9.
9.
10.
10. Checklist of Cognitive Distortions *
1.
All-or-Nothing Thinking. You look at things in absolute, black-and-white categories.
6.
Magnification or Minimization. You blow things way out of proportion or shrink them.
2.
Overgeneralization. You view a single negative event as a never-ending pattern of defeat.
7.
Emotional Reasoning. You reason from your feelings: “I feel like an idiot, so I must be one.”
3.
Mental filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use “shoulds,” “shouldn'ts,” “musts,” “oughts,” and “have tos.”
4.
Discounting Positives. You insist your positive qualities don't count.
9.
Labeling. Instead of saying, “I made a mistake,” you tell yourself, “I'm a jerk” or “I'm a loser.”
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Self-Blame and Other-Blame.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
*
Copyright 1984 by David D. Burns, M.D. Revised 2001.
Daily Mood Log* Situation or Event: % Before
Emotions
% After
Emotions
Sad, blue, depressed, down, unhappy
Hopeless, discouraged, pessimistic, despairing
Anxious, worried, panicky, nervous, frightened
Frustrated, stuck, thwarted, defeated
Guilty, remorseful, bad, ashamed
Angry, mad, resentful, annoyed, irritated, upset, furious
Inferior, worthless, inadequate, defective, incompetent
Other (describe)
Lonely, unloved, unwanted, rejected, alone, abandoned
Other
Embarrassed, foolish, humiliated, self-conscious
Other
% Belief before
Negative Thoughts
% Belief after
Distortions
Positive Thoughts
1.
1.
2.
2.
3.
3.
4.
4.
*
Copyright 1984 by David D. Burns, M.D. Revised 2001.
% Before
% After
% Belief
Daily Mood Log (cont’d) % Belief before
Negative Thoughts
% Belief after
Distortions
Positive Thoughts
5.
5.
6.
6.
7.
7.
8.
8.
9.
9.
10.
10.
% Belief
Checklist of Cognitive Distortions * 1.
All-or-Nothing Thinking. You look at things in absolute, black-and-white categories.
6.
Magnification or Minimization. You blow things way out of proportion or shrink them.
2.
Overgeneralization. You view a single negative event as a never-ending pattern of defeat.
7.
Emotional Reasoning. You reason from your feelings: “I feel like an idiot, so I must be one.”
3.
Mental filter. You dwell on the negatives and ignore the positives.
8.
Should Statements. You use “shoulds,” “shouldn'ts,” “musts,” “oughts,” and “have tos.”
4.
Discounting Positives. You insist your positive qualities don't count.
9.
Labeling. Instead of saying, “I made a mistake,” you tell yourself, “I'm a jerk” or “I'm a loser.”
5.
Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Self-Blame and Other-Blame.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
*
Copyright 1984 by David D. Burns, M.D. Revised 2001.
Daily Mood Log* Upsetting Event: Emotions
% Before
% Goal
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
Embarrassed, foolish, humiliated, self-conscious
Anxious, worried, panicky, nervous, frightened
Hopeless, discouraged, pessimistic, despairing
Guilty, remorseful, bad, ashamed
Frustrated, stuck, thwarted, defeated
Inferior, worthless, inadequate, defective, incompetent
Angry, mad, resentful, annoyed, irritated, upset, furious
Lonely, unloved, unwanted, rejected, alone, abandoned
Other
Negative Thoughts
% Before
% After
Distortions
1.
2.
3.
4.
5.
* Copyright 1984 by David D. Burns, M.D. Revised 2010.
Positive Thoughts
% Goal
% After
% Belief
Daily Mood Log (cont'd) Negative Thoughts
% Before
% After
Distortions
Positive Thoughts
% Belief
6.
7.
8.
9.
10.
Checklist of Cognitive Distortions* 1. All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6. Magnification and Minimization. You blow things out of proportion or shrink them.
2. Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7. Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3. Mental Filter. You dwell on the negatives and ignore the positives.
8. Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4. Discounting the Positive. You insist that your positive qualities don't count.
9. Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5. Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright 1984 by David D. Burns, M.D. Revised 2003.
Daily Mood Log* Upsetting Event: Emotions
% Before
% Goal
% After
Emotions
% Before
Sad, blue, depressed, down, unhappy
Embarrassed, foolish, humiliated, self-conscious
Anxious, worried, panicky, nervous, frightened
Hopeless, discouraged, pessimistic, despairing
Guilty, remorseful, bad, ashamed
Frustrated, stuck, thwarted, defeated
Inferior, worthless, inadequate, defective, incompetent
Angry, mad, resentful, annoyed, irritated, upset, furious
Lonely, unloved, unwanted, rejected, alone, abandoned
Other
Negative Thoughts
% Before
% After
Distortions
1.
2.
3.
4.
5.
* Copyright 1984 by David D. Burns, M.D. Revised 2010.
Positive Thoughts
% Goal
% After
% Belief
Daily Mood Log (cont'd) Negative Thoughts
% Before
% After
Distortions
Positive Thoughts
% Belief
6.
7.
8.
9.
10.
Checklist of Cognitive Distortions* 1. All-or-Nothing Thinking. You view things in absolute, black-and-white categories.
6. Magnification and Minimization. You blow things out of proportion or shrink them.
2. Overgeneralization. You view a negative event as a never-ending pattern of defeat: "This always happens!"
7. Emotional Reasoning. You reason from your feelings: "I feel like an idiot, so I must really be one."
3. Mental Filter. You dwell on the negatives and ignore the positives.
8. Should Statements. You use shoulds, shouldn'ts, musts, oughts, and have tos.
4. Discounting the Positive. You insist that your positive qualities don't count.
9. Labeling. Instead of saying, "I made a mistake," you say, "I'm a jerk" or "I'm a loser."
5. Jumping to Conclusions. You jump to conclusions not warranted by the facts.
10. Blame. You find fault instead of solving the problem.
Mind-Reading. You assume that people are reacting negatively to you.
Self-Blame. You blame yourself for something you weren't entirely responsible for.
Fortune-Telling. You predict that things will turn out badly.
Other-Blame. You blame others and overlook ways you contributed to the problem.
* Copyright 1984 by David D. Burns, M.D. Revised 2003.
All-or-Nothing Overgeneralization Mental Filter Discounting the Positive Jumping to Conclusions Magnification & Minimization Emotional Reasoning Should Statements Labeling & Mislabeling Self-Blame Other-Blame
*Copyright © 2003 by David D. Burns, M.D.
Stimulus Control Decision-Making Form Gradual Exposure & Flooding Response Prevention Distraction Relationship CBA Revise Your Communication Style The Five Secrets One-Minute Drill Smile and Hello Practice David Letterman Technique Self-Disclosure Flirting Training Rejection Practice & Feared Fantasy
Socratic Method Thinking in Shades of Gray Process vs. Outcome Semantic Method Let's Define Terms Be Specific Self-Monitoring Negative Practice Acceptance Paradox Externalization of Voices Feared Fantasy Paradoxical Magnification Shame-Attacking Exercises Cognitive Flooding Image Substitution Memory Rescripting Hidden Emotion Downward Arrow What-If Technique Daily Activity Schedule Pleasure Predicting Sheet Little Steps for Big Feats Anti-Procrastination Sheet Cost-Benefit Analysis (CBA) Devil's Advocate Technique
Empathy Agenda Setting Straightforward Technique Double Standard Technique Examine the Evidence Experimental Technique Survey Technique Reattribution
Anti-Shyness
Interpersonal
Exposure
Motivational
Uncovering
Visual Imaging
Humorous
Role-Playing
Spiritual
Quantitative
Semantic
Logic-Based
Truth-Based
Compassionate
Basic
Selecting Techniques for Cognitive Distortions* Category of Technique
Discounting the Positive Jumping to Conclusions Mind-Reading Fortune-Telling Magnification & Minimization Emotional Reasoning Should Statements
Labeling Blame Self-Blame Other-Blame
All
Semantic Method
Depression and Anxiety Disorders
All
Habits and Addictions
* Copyright © 2004 by David D. Burns, M.D. Permission to copy or publish is strictly prohibited.
Anxiety Disorders
One-Minute Drill
The Five Secrets
Revise Your Communication Style
Interpersonal
Exposure
Relationship CBA
Rejection Practice
Flirting Training
Self-Disclosure
David Letterman Technique
Smile and Hello Practice
Cognitive
Classical
Motivational
Memory Rescripting
Image Substitution
Cognitive Flooding
Distraction
Response Prevention
Gradual Exposure and Flooding
Anti-Procrastination Sheet
Pleasure Predicting Sheet
Daily Activity Schedule
Decision-Making Form
Uncovering
Stimulus Control
Devil's Advocate Technique
Cost-Benefit Analysis (CBA)
Hidden Emotion Technique
What-If Technique
Visual Imaging
Spiritual
Role-Playing
Humor-Based
Quantitative
Semantic
Cognitive
Interpersonal Downward Arrow
Individual Downward Arrow
Cognitive Hypnosis
Humorous Imaging
Time Projection
Acceptance Paradox
Feared Fantasy
Externalization of Voices
Shame-Attacking Exercises
Paradoxical Magnification
Negative Practice / Worry Breaks
Self-Monitoring
Be Specific
Logic-Based
Truth-Based
Compassionate
Basic
Let's Define Terms
Thinking in Shades of Gray
Socratic Method
Reattribution
Survey Technique
Experimental Technique
Agenda Setting
Examine the Evidence
Mental Filter Double Standard Technique
All-or-Nothing Thinking Overgeneralization Straightforward Technique
Empathy
How to Select Techniques for Each Distortion* Interpersonal
Relationship Problems
50 Ways to Untwist Your Thinking* Basic Techniques 1.
Empathy
When you're upset, you need someone to listen and see the world through your eyes without trying to cheer you up, change you, help you, or give you advice. Although this usually won’t cure you, it’s often a necessary first step. It can be a tremendous relief to feel that someone's listening. Similarly, you can empathize when you’re trying to help a friend or family member who feels upset. Usually, all they really want is for you to be a good listener.
2.
Agenda Setting
Agenda Setting is the most basic and important technique of all. First, try to define a specific problem you want help with. It must be specific as to person, place, and time. Ask yourself, "What is the specific problem I want help with? What time of day did it happen? Where was I? Who was I interacting with? What was going on?" Second, ask yourself if you’re motivated and willing to roll up your sleeves and work on it now, rather than just talking about it endlessly. Ask yourself, "What would it be worth to me to solve this problem? How hard would I be willing to work on the solution?"
3.
Identify the Distortions
Use the Checklist of Cognitive Distortions to identify the distortions in each of your Negative Thoughts.
4.
Straightforward Technique
You try to substitute a more positive and realistic thought for each of your Negative Thoughts. Ask yourself, "Is this Negative Thought really true? Do I really believe it? Is there another way to look at the situation?"
Compassion-Based Techniques 5.
Double Standard Technique
Instead of putting yourself down, you talk to yourself in the same compassionate way you might talk to a dear friend who was upset. Ask yourself, "Would I say such harsh things to a friend with a similar problem? If not, why not? What would I say to him or her?"
Truth-Based Techniques 6.
Examine the Evidence
Instead of assuming that your Negative Thought is true, you examine the evidence for it. Ask yourself, "What are the facts? What do they show?"
7.
Experimental Technique
You do an experiment to test the validity of your Negative Thought, in much the same way that a scientist would test a theory. Ask yourself, "How could I test this Negative Thought to find out if it's really valid?"
8.
Survey Method
You do a survey to find out if your thoughts are realistic. Ask yourself, "How do other people think and feel about this? Could I ask some friends about this to get some feedback?" For example, if you believe that social anxiety is rare or shameful, simply ask several friends if they’ve ever felt that way.
9.
Reattribution
Instead of blaming yourself entirely for a problem, you can think about the many factors that contributed to it. You can also focus on solving the problem instead of blaming yourself for it. Ask yourself, "What caused this problem? What did I contribute and what did others contribute? What can I learn from the situation?"
* Copyright 2000 by David D. Burns, MD.
Fifty Ways
Page 2
Logic-Based Techniques 10. Socratic Method
Ask yourself several questions that will lead to the inconsistencies in your Negative Thoughts. For example, you might ask yourself, "When I say that I'm a 'failure at life,' do I mean that I fail at some things some of the time, or all things all of the time?" If you say, "some things some of the time," you can point out that this is true of all human beings. If you say, "all things all of the time," you can point out that this isn't true of anyone, since no one fails at everything.
11. Thinking in Shades of Gray
Instead of thinking about your problems in black-and-white categories, you evaluate them in shades of gray. When things don't work out as well as you'd hoped, you can think of the experience as a partial success or a learning opportunity. Pinpoint your specific errors instead of writing yourself off as a total failure.
12. Process Vs. Outcome
You evaluate your performance based on the process--the effort you put in-rather than the outcome. Your efforts are within your control, but the outcome is not.
Semantic Techniques 13. Semantic Method
Substitute language that is less colorful and emotionally loaded. Instead of thinking, "I shouldn’t have made that mistake," you can tell yourself, "It would be preferable if I hadn't made that mistake." This method is especially helpful for should statements and labeling.
14. Let's Define Terms
When you label yourself as "inferior" or "a fool" or "a loser," ask yourself what those labels mean. You'll see that there's no such thing as a "fool" or a "loser." Foolish behavior exists, but fools and losers do not. Ask yourself, "What's the definition of 'an inferior human being' or 'a loser'? What is my definition of someone who is hopeless? When I say I'm hopeless, what claim am I making?"
15. Be Specific
Stick with reality and avoid judgments about reality. For example, instead of thinking of yourself as totally defective, you can focus on your specific strengths and weaknesses.
Quantitative Techniques 16. Self-Monitoring
Keep track of repetitious Negative Thoughts or anxiety-producing fantasies by counting them. You can count your thoughts in a couple of different ways. You can keep a 3x5 card in your wallet or pocket. Each time you have a Negative Thought, put a tick mark on the card. Alternatively, you can use a wrist-counter like the ones golfers wear to keep track of their scores. At the end of the day, record the total on your calendar. Usually, the upsetting thoughts will diminish and disappear after about three weeks of Self-Monitoring.
17. Negative Practice
Schedule several minutes each day to worry or beat up on yourself mentally. For example, if you constantly beat up on yourself because of your shortcomings, you can schedule several five-minute periods each day to berate yourself and feel miserable. At those times, you can be as self-critical as you want and rip yourself to shreds with gusto. You can use the rest of the time for joyous, productive living.
Fifty Ways
Page 3
Philosophical / Spiritual Techniques 18. Acceptance Paradox
Instead of defending yourself against your own criticisms, you can find truth in them and accept your shortcomings with tranquility. Tell yourself, "It's true that I have many inadequacies. In fact, there is very little, if anything, about me that couldn't be improved considerably."
Role-Playing Techniques 19. Externalization of Voices
This Role-Playing technique requires two people and transforms intellectual understanding into emotional change at the gut level. It is by far the most powerful of all cognitive therapy techniques, but it can be quite challenging and even a bit upsetting at first. You and the other person take turns playing the role of your Negative Thoughts and the role of your Positive Thoughts. The person playing the Negative Thoughts attacks, and the person playing the Positive Thoughts defends. Use role-reversals when you get stuck.
20. Feared Fantasy Technique
Like the Externalization of Voices, this is a two-person technique. You and the other person act out your worst fears, such as being rejected because you aren’t smart enough or good enough. When you face your worst fear, you often gain liberation from it. Your worst fears usually don't turn out to be real monsters, but figments of your imagination that can be defeated with a little logic, compassion, and common sense.
Other Role-Playing Methods
Many techniques are more effective when used in a role-playing format. These include: the Double Standard Technique, the Devil's Advocate, the Acceptance Paradox, the Five Secrets of Effective Communication, the David Letterman Technique, and Flirting Training. Of course, you will need the help of another person, such as your therapist or a friend.
Humorous Techniques 21. Paradoxical Magnification
Instead of refuting your Negative Thoughts, you can buy into them and exaggerate them. Don't try to argue with your NTs. Instead, make them as extreme as possible. For example, if you feel inferior, you could tell yourself, “Yes, it’s true. In fact, I’m probably the most inferior person in California at this time.” Paradoxically, this humorous method can sometimes provide objectivity and relief. Of course, if you’re really feeling upset, this may have the unintended effect of making you feel even worse. If so, go on to another method.
22. Shame-Attacking Exercises
If you suffer from shyness, you probably have intense fears of looking foolish in front of other people. Shame-Attacking Exercises are a specific and potent antidote to these kinds of fears. You intentionally do something foolish in public. For example, you could stand up and loudly announce each stop on a bus or shout out the time in a crowded department store. When you make a fool of yourself on purpose, you realize that the world doesn't really come to an end, and that people don’t really look down on you. This discovery can be tremendously liberating.
Fifty Ways
Page 4
Visual Imaging Techniques 23. Cognitive Flooding
Visualize one of your worst fears, such as feeling trapped and going crazy while riding on a train. Try to endure the anxiety for as long as you can. If you become panicky, tell yourself, "Don't fight it!" Instead, try to make it even worse. Eventually, your anxiety will burn itself out, because your body simply cannot create anxiety indefinitely. You can use Cognitive Flooding when you can’t expose yourself to the thing you fear. For example, if you have a fear of flying, you can't expose yourself to an actual airplane crash in order to overcome your anxiety! However, you can confront this fear in your mind’s eye using Cognitive Flooding.
24. Image Substitution
Substitute a more positive or peaceful image for a frightening one. For example, during an airplane flight, you can fantasize landing safely or relaxing on a beach instead of picturing the plane crashing in flames.
25. Memory Rescripting
If you've been a victim of sexual or physical abuse, you may experience flashbacks and vivid memories of the traumatic episode. These mental pictures can be likened to an internal movie that accompanies the negative, self-blaming thoughts. You can edit these images in much the same way that you can change your Negative Thoughts. Editing the painful images creates a sense of mastery and helps you overcome the feelings of helplessness that result from being a victim. Exposure to the painful memories desensitizes you so that the traumatic event loses its power to upset and intimidate you.
Uncovering Techniques 26. Hidden Emotion Technique
This technique is based on the idea that when you're anxious, you may be avoiding a personal problem that you don't want to face. Bringing this problem to conscious awareness and expressing your feelings will often eliminate your anxiety. Ask yourself, "Am I focusing on my anxiety to avoid dealing with something upsetting? What's the real problem that's bothering me? Do I secretly resent my spouse or my job? Am I unhappy about being in school? How do I really feel?"
27. Individual Downward Arrow
This technique will help you pinpoint the Self-Defeating Beliefs that make you vulnerable to depression and anxiety. For example, you may be a perfectionist and base your self-esteem entirely on your accomplishments. To use this technique, draw a downward arrow under a Negative Thought and ask yourself, "Why would it be upsetting to me if this thought were true? What would it mean to me?” A new Negative Thought will come to mind. Write it down under the arrow and repeat the process several times. The NTs you generate will lead to the underlying beliefs at the core of your suffering.
28. Interpersonal Downward Arrow
This technique will help you pinpoint Self-Defeating Beliefs about intimate relationships. For example, you may believe that you always have to please other people, even at the expense of your own needs and feelings. To use this technique, draw a downward arrow under a Negative Thought and ask yourself, "If that were true, what would it tell me about the type of person s/he is, the type of person I am, or the type of relationship we have?" A new Negative Thought will come to mind. Write it down under the arrow and repeat the process several times. The additional thoughts you generate will help you uncover the beliefs that lead to problems in your relationships with other people.
Fifty Ways 29. What-If Technique
Page 5 This technique is similar to the Downward Arrow Technique, but it's geared specifically to anxiety. Draw a downward arrow under a Negative Thought and ask yourself, "What if that were true? What's the worst that could happen? What do I fear the most?" A new Negative Thought or fantasy will come to mind. Write it down under the arrow and repeat the process several times. You will generate additional thoughts until you uncover the fantasy that frightens you the most. Then you can ask yourself, "How likely is it that this would happen? And could I live with it if it did?"
Anti-Procrastination Techniques 30. Daily Activity Schedule
When you're depressed, everything seems overwhelming, and nothing seems worth doing, so you may give up on life. The Daily Activity Schedule can help you overcome do-nothingism. Record what you do each hour from the time you get up in the morning to the time you go to bed at night. Rate how satisfying each activity was on a scale from 0 (not at all satisfying) to 5 (the most satisfying). A review of the schedule will show you which activities boost your mood the most.
31. Pleasure Predicting Sheet
Schedule a series of activities with the potential for pleasure, learning, or personal growth. Indicate whom you plan to do each activity with. Include activities you can do by yourself (such as jogging) as well as activities with other people. Predict how satisfying each activity will be on a scale from 0% (the least) to 100% (the most). After you complete each activity, record how satisfying it actually turned out to be on the same scale. Now compare your actual satisfaction ratings with your predictions. Many depressed people find that lots of activities turn out to be more rewarding than they predicted. This discovery can boost your motivation. You can also compare the satisfaction you get from being alone with the satisfaction you feel from being with other people. This can help you test SelfDefeating Beliefs such as, "If I'm alone, I'm bound to feel miserable."
32. Little Steps for Big Feats
If you have trouble with procrastination, you can break large, overwhelming tasks down into small steps that you can tackle one at a time. If you tell yourself you have to clean the entire garage today, you'll never get started. Instead, break it down into small steps. Tell yourself you only have to carry two cardboard boxes out to the trash. That will feel far less overwhelming and you may end up doing a great deal more than you planned.
33. AntiProcrastination Sheet
This is similar to Little Steps for Big Feats but it’s more sophisticated. Break a large task down into small steps and predict how difficult and how satisfying each step will be on a scale from 0% to 100%. Record these predictions on the Anti-Procrastination Sheet. After completing each small step, record how difficult and satisfying it turned out to be on a scale from 0% to 100%. Now compare your predictions with the outcome. Many people discover that each small step is far easier and much more rewarding than they expected.
Fifty Ways
Page 6
Anti-Resistance Techniques 34. Straightforward Cost-Benefit Analysis (CBA)
List the advantages and disadvantages of a Negative Thought (“I’m such a loser”) or Self-Defeating Belief (“I should be perfect”). You can also do a CBA for a negative feeling (like anger, guilt, inferiority or anxiety), a habit (such as drinking, using drugs, overeating or procrastinating) or a relationship problem (such as blaming your spouse for your marital problems). In each case, ask yourself, "What are the advantages and disadvantages of this belief, feeling or habit? How will it help me, and how will it hurt me?" After you list all the advantages and disadvantages, balance them against each other on a 100-point scale so you can see whether the costs or the benefits or your mind-set are greater.
35. Paradoxical CostBenefit Analysis (CBA)
List only the advantages of a negative thought, belief, feeling, addiction, or relationship problem. The list will make you aware of all the powerful forces that keep you stuck. Ask yourself, "Given all the advantages of this thought (or attitude or behavior), why should I change?"
36. Devil's Advocate Technique
This is a Role-Playing Technique. Another person plays the role of the Devil who tempts you to drink, overeat, procrastinate, or date the wrong person. You talk back to those thoughts in real time. Role-reversals can be helpful when you get stuck. For example, if you are overweight, imagine being in a mall where fast food is sold. The Devil might say, "Gee, why don't you get one of those hot, buttery cinnamon buns? They just came out of the oven. They'd taste so good. You deserve it!" You would fight back and say, “I don’t need a cinnamon bun, and I’ll feel terrible if I give in. I’m determined to stick with my diet, and I’m looking forward to fitting into more attractive clothes.” The Devil can try to break you down again, and you will fight back. This method is surprisingly challenging, especially if the Devil is familiar with your own rationalizations and expresses them in a seductive and persuasive manner.
37. Stimulus Control
If you're trying to break a bad habit, such as alcoholism or overeating, you can reduce temptation rather than struggling with it. For example, if you drink too much, don’t go to places where alcohol is served, and get rid of all the alcoholic beverages in your house. Stimulus Control is not a complete treatment, but an important part of a more comprehensive program.
Other Motivational Techniques 38. The DecisionMaking Form
If you're having trouble making up your mind about something, you can use the Decision-Making Form. This form will show why you're getting hung up and will help you finalize your decision. The purpose of the Decision-Making Form is not to tell you what to do, but to show you what the real issues are and how you feel about them.
Fifty Ways
Page 7
Exposure Techniques for Anxiety 39. Gradual Exposure and Flooding
Gradual Exposure and Flooding are both forms of exposure therapy for anxiety disorders. When you use Gradual Exposure, you expose yourself to the thing you fear in small steps so that it won't be quite so terrifying. In contrast, when you use Flooding, you expose yourself to the thing you fear all at once. For example, if you have an elevator phobia, force yourself to get on an elevator and stay there, no matter how anxious you feel, until your fear disappears. Gradual Exposure is less traumatic, but it takes longer. Flooding is much more frightening, but it works more rapidly. Both approaches have been used successfully in the treatment of nearly all forms of anxiety.
40. Response Prevention
Response Prevention is an important key to the treatment of all forms of anxiety. It’s often combined with Exposure. For example, let's say you have a powerful urge to check the mailbox over and over after you drop a letter in. Using Response Prevention, you would drop a letter in the mailbox and walk away without checking it as you usually do. Your anxiety will temporarily get worse, and you’ll feel compelled to check it. But if you refuse to give in to the urge to check the mailbox, your anxiety will eventually disappear.
41. Distraction
If you feel anxious, you can distract yourself from your upsetting thoughts. For example, if you’re feeling anxious during an airplane flight, you can distract yourself from the frightening thoughts by concentrating on something else. For example, you could do a crossword puzzle or engage the passenger next to you in conversation. You can combine Distraction with Self-Monitoring and exposure therapy.
Interpersonal Techniques for Relationship Problems 42. Relationship CostBenefit Analysis
List the advantages and disadvantages of blaming the other person for a relationship problem. For example, if you blame the other person, you can feel self-righteous and morally superior. You won’t have to change or examine your own role in the problem. You’ll feel like truth is on your side, and you can get back at the other person without having to feel guilty. There are also a number of disadvantages. For example, you won’t be able to resolve the problem or get close to the person you’re mad at. The conflict will go on and on and you’ll feel frustrated all the time. Once you’ve listed all the advantages and disadvantages, balance them against each other on a 100-point scale. This will help you decide whether you want to maintain this mind-set.
43. Revise Your Communication Style
You can use the Revise Your Communication Style form to improve your relationships with family members, friends and colleagues. There are five steps. First, write down one thing the other person said to you. Second, write down what you said next. Third, use the "Good Vs. Bad Communication Checklist" or the "Bad Communication Checklist" to identify your communication errors. Fourth, ask yourself what the consequences of your response will be. Finally, use the "Five Secrets of Effective Communication" to generate a more effective response.
44. Five Secrets of Effective Communication
The Five Secrets can help you resolve virtually any relationship problem quickly. The acronym, EAR, will help you remember them. The E stands for Empathy and includes three listening skills: the Disarming Technique, Thought and Feeling Empathy, and Inquiry. The A stands for Assertiveness, using "I Feel" Statements. The R stands for Respect (Stroking). These techniques require considerable practice and will backfire if not done skillfully.
Fifty Ways
Page 8
45. One-Minute Drill
This technique practically ensures nearly perfect communication. It breaks the pattern of accusation and self-defense, and shifts the dialogue to the level of emotion and intimacy. You and your partner take turns playing the roles of Talker and Listener. The Talker spends 30 seconds expressing his or her feelings about a relationship problem. The Listener paraphrases what the Talker said as accurately as possible. The Talker rates the Listener's accuracy from 0% to 100%. Once the Listener receives a 95% or better rating, you can do a role-reversal.
Interpersonal Techniques for Shyness and Loneliness 46. Smile and Hello Practice
If you are shy, you can smile and say hello to 10 strangers per day. Use a 3x5 card to record how many people respond positively, neutrally, or negatively. You’ll often discover that people are much friendlier than you expected— unless you happen to live in Manhattan. I’ve tried this in Manhattan and everyone ignored me! Of course, even that can be helpful, because you quickly get over your fears of rejection.
47. David Letterman Technique
You learn how to make casual conversation using the Five Secrets of Effective Communication. The idea is to focus on the other person in a friendly way. Get them to open up, rather than feeling like you have to impress them by talking about yourself. These are the same skills used by successful talk-show hosts like David Letterman. They appear charming and relaxed because they always keep the spotlight on the other person.
48. Self-Disclosure
Instead of shamefully hiding your feelings of shyness or nervousness in a social situation, you disclose them openly. This technique requires a good sense of self-esteem to be effective.
49. Flirting Training
You learn to flirt in a light-hearted way, rather than interacting with others in an overly serious, heavy manner.
50. Rejection Practice and Rejection Feared Fantasy
If you're shy and afraid of rejection, you can accumulate as many rejections as possible in order to learn that the world doesn’t come to an end. For example, when he was young, Dr. Albert Ellis, a noted New York psychologist, asked 200 women for a date during a two-week period. All but one turned him down, and she failed to show up! Although he didn't get a date, he did conquer his fears of rejection and ultimately developed a robust social life, to say the least! You can combine this technique with the Rejection Feared Fantasy. You need a partner if you want to try this technique. Your partner will play the most rejecting, hostile person you can imagine. She or he will be far worse than any real human being would ever be, and is really just the projection of your own fears. When you confront this fantasy figure, you will discover that you had nothing to be afraid of in the first place.
50 Ways to Untwist Your Thinking* By David D. Burns, M.D. Basic Techniques 1. Empathy
When we're upset, we need someone to listen and see the world through our eyes without trying to cheer us up, help us, or give us advice. Although this won't usually lead to a cure, it can be a relief to know that someone's listening. You can learn to empathize when you're trying to help a friend or family member who feels upset. Usually, all they really want is for you to be a good listener.
2. Agenda Setting
Agenda Setting is the most basic and important technique of all. First, try to define the problem you want help with. It must be real and specific as to person, place, and time. Ask yourself, "When was I upset? What time of day was it? Where was I? Who was I interacting with? What was going on?" Now ask yourself if you're willing to roll up your sleeves and work on it now, rather than just talking about it endlessly. Ask yourself, "What would it be worth to me to solve this problem? How hard would I be willing to work on the solution?"
3. Identify the Distortions
Use the Checklist of Cognitive Distortions to identify the distortions in each negative thought.
4. Straightforward Technique
Try to substitute a more positive and realistic thought for each negative thought. Ask yourself, "Is this negative thought really true? Do I really believe it? Is there another way to look at the situation?"
Compassion-Based Techniques 5. Double Standard Technique
Instead of putting yourself down, talk to yourself in the same compassionate way you might talk to a dear friend who was upset. Ask yourself, "Would I say such harsh things to a friend with a similar problem? If not, why not? What would I say to him or her?"
Truth-Based Techniques 6. Examine the Evidence
Instead of assuming that your negative thought is true, examine the evidence for it. Ask yourself, "What are the facts? What do they show?"
7. Experimental Technique
Do an experiment to test the validity of your negative thought, in much the same way that a scientist would test a theory. Ask yourself, "How could I test this negative thought to find out if it's really true?" For example, if you believe you're on the verge of losing control and cracking up during your panic attacks, you can test this belief by trying to drive yourself crazy though willful effort. You can roll around on the floor, flail your arms and legs in the air, and speak gibberish. It can be a relief to discover that you can't go crazy, no matter how hard you try.
8. Survey Technique
Conduct a survey to find out if your thoughts are realistic. Ask yourself, "How do other people think and feel about this? Could I ask some friends and get some feedback?" For example, if you believe that social anxiety is rare or shameful, you could simply ask several friends if they've ever felt that way.
9. Reattribution
Instead of blaming yourself entirely for a problem, think about the many factors that contributed to it. Ask yourself, "What caused this problem? What did I contribute and what did others contribute? What can I learn from the situation?"
* Copyright 2004 by David D. Burns, MD. Revised 2005. Do not reproduce without written permission.
50 Ways To Untwist Your Thinking
Page 2
Logic-Based Techniques 10. Socratic Method
Ask yourself questions that will lead to the inconsistencies in your negative thoughts. For example, you might ask yourself, "When I say that I'm a 'failure at life,' do I mean that I fail at some things some of the time, or all things all of the time?" If you say, "some things some of the time," you can point out that this is true of all human beings. If you say, "all things all of the time," you can point out that this isn't true of anyone, since no one fails at everything.
11. Thinking in Shades of Gray
Instead of thinking about your problems in black-and-white categories, you can evaluate them in shades of gray. When things don't work out as well as you'd hoped, you can think of the experience as a partial success or learning opportunity. Pinpoint your specific errors instead of writing yourself off as a total failure.
Semantic Techniques 12. Semantic Method
Substitute language that's less colorful and emotionally loaded. Instead of thinking, "I shouldn't have made that mistake," you can tell yourself, "It would be preferable if I hadn't made that mistake." This method is especially helpful for Should Statements and Labeling.
13. Let's Define Terms
When you label yourself as "inferior," "a fool," or "a loser," ask yourself what those labels mean. What's the definition of "a fool" or "a loser"? When you try to define these terms, you'll discover there's no such thing as "a fool" or "a loser." Foolish behavior exists, but "fools" and "losers" do not.
14. Be Specific
Stick with reality and avoid judgments about reality. For example, instead of thinking of yourself as defective or worthless, you can focus on your specific strengths and weaknesses.
Quantitative Techniques 15. Self-Monitoring
Keep track of repetitious negative thoughts or anxiety-producing fantasies by counting them. You can keep a 3x5 card in your wallet or pocket and put a tick mark on it each time you have a negative thought. Alternatively, you can wear a wrist-counter like the ones golfers use to keep track of their scores. Record the total number of negative thoughts each day on your calendar. Often, the upsetting thoughts will diminish or disappear within two to three weeks.
16. Negative Practice / Worry Breaks
Schedule time to intentionally worry or criticize yourself. For example, if you constantly beat up on yourself because of your shortcomings, you can schedule several five-minute periods each day to berate yourself and feel miserable. At those times, you can be as self-critical as you want and rip yourself to shreds with gusto. Use the rest of your time for positive, productive living.
50 Ways To Untwist Your Thinking
Page 3
Humor-Based Techniques 17. Paradoxical Magnification
Instead of trying to refute your negative thoughts, you can buy into them and exaggerate them. Try to make them as extreme as possible. For example, if you feel inferior, you could tell yourself, "Yes, it's true. In fact, I'm probably the most inferior person in California at this time." Paradoxically, this can sometimes provide objectivity and relief. Of course, if you're really upset, this technique may have the unintended effect of making you feel even worse. If so, try another method.
18. Shame-Attacking Exercises
If you suffer from shyness, you probably have intense fears of looking foolish in front of other people. Shame-Attacking Exercises are a specific and potent antidote to these kinds of fears. You intentionally do something foolish in public so you can get over this fear. For example, you could stand up and announce each stop on a bus or shout out the time in a crowded department store. When you make a fool of yourself on purpose, you discover that the world doesn't come to an end after all, and that people don't really look down on you. This discovery can be liberating.
Role-Playing Techniques 19. Externalization of Voices
This technique transforms intellectual understanding into emotional change at the gut level. It's the most powerful of all the CBT techniques, but it can be quite challenging and even a bit upsetting at first. You and another person will take turns playing the role of your negative thoughts and the role of your positive thoughts. The person playing the negative thoughts attacks, and the person playing the positive thoughts defends. Use role-reversals when you get stuck. In the "I-I" version of the Externalization of Voices, both of you will speak in the first person, "I." In the "You-I" version, the person playing the negative thoughts will speak in the second-person, "You," and the person playing the positive thoughts will speak in the first person, "I." The "I-I" method is gentle and safe, but less effective. The "You-I" method is more intimidating and challenging, but has far greater healing power.
20. Feared Fantasy Technique
Other Role-Playing Methods
Like the Externalization of Voices, this is a two-person technique. You and the other person act out your worst fears, such as being rejected by an exceptionally hostile critic because you aren't smart enough or good enough. When you face your worst fear, you often gain liberation from it. Your worst fears don't usually turn out to be real monsters, but figments of your imagination that you can defeat with a little logic, compassion, and common sense. Many techniques are much more effective in a role-playing format. They include Cognitive Techniques like the Double Standard Technique (#5) and, Acceptance Paradox (#21), Motivational Techniques like the Devil's Advocate (#30), and Exposure Techniques like the David Letterman Technique (#43) and Flirting Training (#45). The Interpersonal Techniques, such as the Five Secrets of Effective Communication (#49) and One-Minute Drill (#50) also work extremely well in a role-playing format.
50 Ways To Untwist Your Thinking
Page 4
Philosophical / Spiritual Techniques 21. Acceptance Paradox
Instead of defending against your own self-criticisms, you can find truth in them and accept your shortcomings with tranquility. Tell yourself, "It's true that I have many inadequacies. In fact, there is very little, if anything, about me that couldn't be improved considerably."
Visual Imaging Techniques 22. Time Projection
Future Projection. If you're depressed, you can take a mental trip into the future and imagine that you've recovered. The current self who feels worthless and defeated can have a conversation with the future self who feels joy and selfesteem. The outpouring of emotion will often have a cathartic effect. Past Projection. You can also take a mental trip into your past and have a conversation with someone who hurt or abused you. This will give you the chance to express thoughts and feelings that have been bottled up and eating away at you for many years.
23. Humorous Imaging
When you feel consumed with anxiety or anger, it can sometimes help to visualize something humorous. A depressed woman obsessed about the fact that she'd gotten screwed in her divorce settlement. She could barely make ends meet, and became furious every time she fantasized about her ex-husband cavorting with his new trophy wife on his yacht and living in the lap of luxury. The constant feelings of anger and resentment were making her miserable. She found that picturing him at a board meeting in his underpants made her giggle. This was a useful antidote to the feelings of rage that were plaguing her.
24. Cognitive Hypnosis
You'll need a therapist who uses hypnosis if you want to try this technique, and you'll have to be hypnotizable—this includes about a third of us. After inducing a trance, the hypnotist may suggest that you're standing in a special library with two sets of shelves. The shelves on the left contain intensely negative books, like "The Book of Rape" and "The Book of Despair," and the shelves on the right contain positive books, like "The Book of Joy" and "The Book of Self-Esteem." When you take a book from the shelf on the left, you'll discover that it's about you. It contains descriptions of all your negative thoughts, memories, and fears. When you read from this book, you'll feel overwhelmed with feelings of depression, anxiety, hopelessness and shame. Your hypnotist will guide you as you destroy this book. You can burn it, bury it, or shred it. Then you'll find yourself in the library again, where you'll take a book from the shelf on the right. Once again, you'll discover that it's all about you, but this time, it's filled with positive messages of self-esteem, creativity, and optimism. As you read from this book, you'll be flooded with feelings of inner peace.
Other Visual Imaging Techniques
Cognitive Flooding (#39), Image Substitution (#40), and Memory Rescripting (#41) are also Visual Imaging Techniques, but they're categorized as Cognitive Exposure Techniques because they're extremely useful in the treatment of anxiety.
50 Ways To Untwist Your Thinking
Page 5
Uncovering Techniques 25. Individual Downward Arrow
Draw a downward arrow under a negative thought on your Daily Mood Log and ask yourself, "Why would it be upsetting to me if this thought were true? What would it mean to me?" A new negative thought will come to mind. Write it down under the arrow and repeat this process several times. When you review the chain of negative thoughts, along with the list of Common Self-Defeating Beliefs (SDBs), you can pinpoint the attitudes and beliefs that make you vulnerable to depression and anxiety, such as Perfectionism, the Achievement Addiction, or the Brushfire Fallacy.
26. Interpersonal Downward Arrow
Draw a downward arrow under a negative thought on your Daily Mood Log and ask yourself, "If that were true, what would it tell me about the type of person s/he is? The type of person I am? The type of relationship we have?" A new negative thought will come to mind. Write it down under the arrow and repeat this process several times. The thoughts you generate will help you uncover the SelfDefeating Beliefs that lead to problems in your relationships with other people, such as Entitlement, Truth, or Submissiveness.
27. What-If Technique
This Uncovering Technique was developed specifically for anxiety. Draw a downward arrow under a negative thought on your Daily Mood Log and ask yourself, "What if that were true? What's the worst that could happen? What do I fear the most?" A new negative thought or fantasy will come to mind. Write it down under the arrow and repeat this process several times. You'll generate additional thoughts that will lead to the fantasy that frightens you the most. Then you can ask yourself, "How likely is it that this would happen? And could I live with it if it did?"
28. Hidden Emotion Technique
This technique is based on the idea that when you're anxious, you may be avoiding a personal problem that you don't want to face. Bringing the problem to conscious awareness and expressing your feelings will often eliminate your anxiety. Ask yourself, "Am I focusing on my anxiety to avoid dealing with something upsetting? What's the real problem that's bothering me? Do I secretly resent my spouse or my job? Am I unhappy about being in school? How do I really feel?"
Motivational Techniques 29. Straightforward and Paradoxical CostBenefit Analysis (CBA)
When you do a Straightforward CBA, you list the advantages and disadvantages of a negative thought ("I'm such a loser") or Self-Defeating Belief ("I should be perfect"). You can also do a CBA for a negative feeling (like anger, guilt, inferiority or anxiety), a habit (such as drinking, using drugs, overeating or procrastinating), or a relationship problem (such as blaming your spouse for your marital problems). Ask yourself, "What are the advantages and disadvantages of this belief, feeling or habit? How will it help me, and how will it hurt me?" After you list all the advantages and disadvantages, balance them against each other on a 100-point scale so you can see whether the costs or the benefits of your mindset are greater. When you do a Paradoxical CBA, you list only the advantages of a negative thought, belief, feeling, habit, or relationship problem. Now ask yourself, "Given all these advantages, why should I change?" This will make you aware of the powerful forces that keep you stuck.
50 Ways To Untwist Your Thinking 30. Devil's Advocate Technique
Page 6
This is a Role-Playing Technique. Another person plays the role of the Devil who tempts you to drink, overeat, procrastinate, or date the wrong person. Your job is talk back to those thoughts in real time. Use role-reversals when you get stuck. For example, if you're struggling to stick with your diet, imagine being in a mall where fast food is sold. The Devil might say, "Gee, why don't you go and get one of those hot, buttery cinnamon buns? They just came out of the oven. It would taste so good. You deserve it!" You can fight back and say, "I don't need a cinnamon bun, and I'll feel terrible if I give in. I'm determined to stick with my diet, and I'm looking forward to fitting into more attractive clothes." The Devil will try to break you down again, and you can fight back. This method can be surprisingly challenging, especially if the Devil is familiar with your own rationalizations and expresses them in a seductive and persuasive manner.
31. Stimulus Control
If you're trying to break a bad habit, such as alcoholism or overeating, you can reduce temptation rather than struggling with it. For example, if you drink too much, you can get rid of all the alcoholic beverages in your house and avoid going to places where alcohol is served. Stimulus Control is not a complete treatment for any addiction, but it can be an important part of a more comprehensive program.
32. Decision-Making Form
If you're stuck on the horns of a dilemma, the Decision-Making Form can help you sort out your options and get unstuck. It won't tell you what you should do, but will show you what the real issues are and how you feel about them.
33. Daily Activity Schedule
When you're depressed, everything seems overwhelming. Nothing seems worth doing, so you may give up on life. The Daily Activity Schedule can help you overcome do-nothingism. Record what you do each hour from the time you get up in the morning to the time you go to bed at night. Rate how satisfying each activity was on a scale from 0 (not at all satisfying) to 5 (the most satisfying). A review of the schedule will show you which activities boost your mood the most.
34. Pleasure Predicting Sheet
Schedule a series of activities with the potential for pleasure, learning, or personal growth. Indicate who you plan to do each activity with. Include activities you can do by yourself (such as jogging) as well as activities with other people. Predict how satisfying each activity will be on a scale from 0% (the least) to 100% (the most). After you complete each activity, record how satisfying it actually turned out to be on the same scale. Now compare your actual satisfaction ratings with your predictions. Many depressed people find that lots of activities turn out to be more rewarding than they predicted. This discovery can boost your motivation to become more actively involved in life again. You can also compare the satisfaction you get from being alone to the satisfaction you feel from being with other people. This can help you test SelfDefeating Beliefs such as, "If I'm alone, I'm bound to feel miserable."
35. Anti-Procrastination Sheet
Rather than telling yourself you have to do everything all at once, break an overwhelming task down into tiny steps that you can tackle one step at a time. List each step in the left-hand column of the Anti-Procrastination Sheet. In the next two columns, predict how difficult and how satisfying each step will be on a scale from 0% – 100%. After completing each small step, record how difficult and how satisfying it turned out to be in the last two columns. Now compare your predictions with the outcome. Many people discover that each step is far easier and more rewarding than they expected.
50 Ways To Untwist Your Thinking Other AntiProcrastination Techniques
Page 7
Socratic Method. If you're struggling with procrastination, you can ask yourself a series of questions that will lead to the absurdity of your claim that you just "can't" seem to get started on the task you've been avoiding. First, break the task down into tiny steps. What's the first thing you'd have to do? The second thing? Then ask yourself, "What do I mean when I claim that I can't do the first step? Or the second step?" Problem-Solution Method. Schedule a time when you can do five minutes of the task you've been avoiding. Let's say you decide to start organizing the mess on your desk at 3:00 PM. Draw a line down the center of a piece of paper and list all the problems that will get in your way and all the excuses you'll give yourself for not getting started at 3:00 in the left-hand column. You might put, "A friend may call and need to talk," or "It may seem too anxiety-provoking," or "I may decide that I need to rest for a while first." You can put solutions to each problem in the right-hand column.
Classical Exposure Techniques 36. Gradual Exposure and Flooding
When you use Gradual Exposure, you expose yourself to the thing you fear in small steps. For example, if you have an elevator phobia, you could get on an elevator, go up one floor, and get off. Once you're comfortable with that, you could ride the elevator for two floors. You can gradually increase the length of time you spend in the elevator. You can use Gradual Exposure for any phobia, such as the fear of heights, needles, or dogs, as well as other forms of anxiety, such as shyness or Obsessive-Compulsive Disorder. You can also create a Fear Hierarchy, listing the least threatening situation as +1, and the most threatening as +10. You can record the type and amount of exposure you perform each day, as well as how anxious you felt, between 0% and 100%. When you use Flooding, you expose yourself to the thing you fear all at once. For example, if you have an elevator phobia, you can force yourself to get on an elevator and ride up and down, no matter how anxious you feel, until your fear disappears. Flooding is more frightening than Gradual Exposure, but it works more rapidly. Both approaches have been used successfully in the treatment of nearly all forms of anxiety, so you can use the approach that appeals to you the most.
37. Response Prevention
Response Prevention is an important key to the treatment of all forms of anxiety. It's often combined with exposure. For example, let's say you have a powerful urge to check the mailbox over and over after you drop a letter in. Using Response Prevention, you would drop the letter in the mailbox and walk away without checking it as you usually do. Your anxiety will temporarily get worse, and you'll feel compelled to check it. But if you refuse to give in to this urge, your anxiety will eventually disappear.
38. Distraction
If you feel anxious, you can distract yourself from the upsetting thoughts by concentrating intensely on something else. For the best results, you can combine Distraction with Gradual Exposure or Flooding. For example, if you feel panicky during an airplane flight, you can work on a crossword puzzle or engage the passenger next to you in conversation. Some therapists recommend moving the eyes back and forth from left to right during exposure. This is called EMDR (Eye Movement Desensitization and Reprocessing). Others recommend tapping rhythmically on some part of your body, like your clavicle or eyebrow, during exposure. This is called TFT (Thought Field Therapy). Although these techniques are controversial, there's no harm in trying them, and they might make the exposure somewhat less upsetting.
50 Ways To Untwist Your Thinking
Page 8
Cognitive Exposure Techniques 39. Cognitive Flooding
Cognitive Flooding is useful when you can't expose yourself to the thing you fear in reality. For example, if you have a fear of flying, you can't expose yourself to an actual airplane crash in order to overcome your fears! However, you can confront this fear in your mind's eye using Cognitive Flooding. Visualize your worst fear, such as feeling trapped in a plane that's crashing toward the earth in a ball of flames while all the passengers scream in terror. Try to endure the anxiety for as long as you can. If you become panicky, don't fight it! Instead, try to make the panic even worse. Eventually, the anxiety will burn itself out because your body simply cannot create anxiety indefinitely.
40. Image Substitution
Substitute a more positive or peaceful image for a frightening one. For example, during an airplane flight, you can fantasize landing safely or relaxing on a beach instead of imagining the plane crashing in flames.
41. Memory Rescripting
If you've been a victim of sexual or physical abuse, you may experience flashbacks with vivid memories of the traumatic episode. These mental pictures can be likened to a horrifying internal movie that you replay over and over, in exactly the same way every time. You can edit the frightening scenes in this movie in much the same way that you can change your negative thoughts. For example, if your best buddy was killed by a hand grenade when you were fighting together in Vietnam, horrifying memories of his body being blown apart may haunt you. You can bring him back to life in your mind's eye and tell him all the things you never got to say before he died. Then you can give him a proper burial and say goodbye. Changing the images can create a sense of mastery and help you overcome the feelings of helplessness that resulted from being a victim. In addition, the intentional exposure will desensitize you, and the traumatic memories will lose their power to intimidate you.
Other Cognitive Exposure Techniques
Negative Practice / Worry Breaks (#16), the Feared Fantasy (#20) and the Acceptance Paradox (#21) are all forms of Cognitive Exposure.
Interpersonal Exposure Techniques 42. Smile and Hello Practice
If you're shy, you can force yourself to smile and say hello to 10 or 20 strangers each day. Use a 3x5 card to record how many people respond positively, neutrally, and negatively. You'll often discover that people are much friendlier than you expected. This discovery can help you overcome your fears of rejection or looking foolish.
43. David Letterman Technique
You can learn how to make casual conversation with anyone by using the Five Secrets of Effective Communication (#49), especially the Disarming Technique, Inquiry, and Stroking. These are the same skills used by successful talk-show hosts like David Letterman and Jay Leno. They appear charming, personable and relaxed because they always keep the spotlight on the other person. Instead of trying to impress people by talking about yourself, you can focus on them in a friendly way. Find truth in what they say. Express curiosity and admiration. Ask questions and encourage them to open up. You'll find that most people are somewhat bored and lonely, and love to be the center of attention.
50 Ways To Untwist Your Thinking
Page 9
44. Self-Disclosure
Instead of shamefully hiding your feelings of shyness or nervousness in a social situation, you can disclose them openly. This technique requires a good sense of self-esteem to be effective. If it's done skillfully, it will allow you to form real relationships with people instead of trying to put on a show and pretend to be something that you're not. This technique is based on the rather unintuitive idea that shyness without shame is actually an asset, because it makes you seem more human and personable.
45. Flirting Training
You learn to flirt in a playful, light-hearted way, rather than interacting with others in such a formal, heavy manner. Paradoxically, when you lighten up and learn to stop taking people so seriously, they're more likely to find you attractive and may even start chasing you.
46. Rejection Practice
If you're shy and afraid of rejection, you can try to accumulate as many rejections as you can instead of trying so hard to find someone to love you. Although this takes tremendous courage, you'll discover that the world doesn't actually come to an end when you're rejected. Paradoxically, when you stop fearing rejection, you stop getting rejected.
Other Interpersonal Exposure Techniques
Shame-Attacking Exercises (#18) are categorized as Humor-Based Techniques, but they're also Interpersonal Exposure Techniques. The Rejection Feared Fantasy is a variation of the Feared Fantasy Technique (#20). Let's say that you're intensely shy and afraid of rejection. You can enter an Alice-inWonderland nightmare world where your worst fears come true. A friend or therapist can play the role of the most rejecting, hostile person you can imagine. She or he will be far worse than any real human being would ever be, and will try to rip you to shreds. If you respond with the Acceptance Paradox, you'll discover that you can easily handle anything the Hostile Critic throws at you without getting perturbed. Use role-reversals if you get stuck.
Interpersonal Techniques 47. Relationship CostBenefit Analysis (CBA)
List the advantages and disadvantages of blaming the other person for the problems in your relationship. You'll discover that there are lots of advantages: ● You can feel morally superior. ● You won't have to examine your own role in the problem. ● You'll feel like truth is on your side. ● You can get back at the other person without feeling guilty. ● You can feel powerful. ● You can tell your friends what a loser the other person is, and they'll probably agree with you. There may also be some disadvantages. You won't be able to resolve the problem or get close to the person you're mad at. The conflict will go on and on, and you'll feel consumed by feelings of frustration and anger. Your friends may get tired of your constant complaining. And there won't be any room for personal or spiritual growth. Once you've listed all the advantages and disadvantages on the CBA form, balance them against each other on a 100-point scale. Ask yourself whether the costs or the benefits of this mind-set are greater. If you decide to keep blaming the other person, the prognosis for the relationship will be extremely poor. The willingness to stop blaming them and examine your own role in the problem is the key to developing a more satisfying relationship.
50 Ways To Untwist Your Thinking 48. Revise Your Communication Style
Page 10
The Revise Your Communication Style form can help you improve your relationships with family members, friends and colleagues. There are five steps: Step 1. Write down one thing the other person said to you. Step 2. Write down exactly what you said next. Step 3. Analyze what you wrote down in Step 2. Was it an example of good or bad communication? Step 4. Think about the consequences of what you wrote down in Step 2. How will the other person think and feel? What will she or he say next? Will your response make the situation better or worse? Step 5. Generate a more effective response using the Five Secrets of Effective Communication.
49. Five Secrets of Effective Communication
The Five Secrets of Effective Communication can help you resolve virtually any relationship problem quickly. These techniques require considerable practice and must come from the heart or they'll backfire. 1. The Disarming Technique. Find some truth in what the other person is saying, even if it seems totally unreasonable or unfair. 2. Empathy. Try to see the world through the other person's eyes. Paraphrase their words (Thought Empathy) and acknowledge how they're probably feeling, based on what she or he said (Feeling Empathy). 3. Inquiry. Ask gentle, probing questions to learn more about what the other person is thinking and feeling. 4. "I Feel" Statements. Express your own ideas and feelings in a direct, tactful manner. Use "I Feel" Statements, such as "I'm feeling upset," rather than "You" statements, such as "You're making me furious!" 5. Stroking. Convey an attitude of respect, even if you feel angry with the other person. Find something genuinely positive to say, even in the heat of battle.
50. One-Minute Drill
You and your partner take turns playing the roles of Talker and Listener. The Talker spends 30 seconds expressing his or her feelings about a relationship problem. The Listener paraphrases what the Talker said as accurately as possible. The Talker rates the Listener's accuracy from 0% – 100%. Once the Listener receives a rating of 95% or better, you can do a role-reversal. This technique ensures nearly perfect communication. It quickly breaks the pattern of accusation, self-defense, and hostility, and shifts the dialogue to a level of greater vulnerability and intimacy.
Other Interpersonal Techniques
Interpersonal Decision-Making. When you're at odds with someone, you have three choices: you can settle for the status quo, work to make the relationship better, or leave the person you're not getting along with. Most of time, people know what they want, but sometimes it's confusing. You may ask yourself: "Should I get engaged or break up and look for someone more exciting?" Or, "Should I get divorced or try to make my marriage better?" The Decision-Making Form (#32) can help you sort out your options when you're having a tough time making up your mind. A wide variety of patterns can emerge, and each one will lead to a unique solution.
50 Ways to Untwist Your Thinking* Basic Techniques
Role-Playing 19. Externalization of Voices
Exposure Techniques Classical Exposure
1. Empathy
20. Feared Fantasy
2. Agenda Setting
Plus: Double Standard, Acceptance
36. Gradual Exposure and Flooding
3. Identify the Distortions
Paradox, Devil's Advocate, and
37. Response Prevention
4. Straightforward Technique
many of the Interpersonal Techniques
38. Distraction
Cognitive Techniques Compassion-Based 5. Double Standard Technique
Truth-Based 6. Examine the Evidence 7. Experimental Technique 8. Survey Technique 9. Reattribution
Philosophical / Spiritual 21. Acceptance Paradox
Visual Imaging
Cognitive Exposure 39. Cognitive Flooding 40. Image Substitution
22. Time Projection
41. Memory Rescripting
23. Humorous Imaging
Plus: Worry Breaks, Feared Fantasy,
24. Cognitive Hypnosis
and Acceptance Paradox
Uncovering Techniques
Interpersonal Exposure 42. Smile and Hello Practice
25. Individual Downward Arrow
43. David Letterman Technique
26. Interpersonal Downward Arrow
44. Self-Disclosure
10. Socratic Method
27. What-If Technique
45. Flirting Training
11. Thinking in Shades of Gray
28. Hidden Emotion Technique
46. Rejection Practice
Logic-Based
Semantic 12. Semantic Method 13. Let's Define Terms 14. Be Specific
Quantitative
Motivational Techniques 29. Straightforward and Paradoxical Cost-Benefit Analysis (CBA) 30. Devil's Advocate Technique
Plus: Rejection Feared Fantasy and Shame-Attacking Exercises
Interpersonal Techniques
17. Paradoxical Magnification
34. Pleasure Predicting Sheet
47. Relationship Cost-Benefit Analysis (CBA) 48. Revise Your Communication Style 49. Five Secrets of Effective Communication 50. One-Minute Drill
18. Shame-Attacking Exercises
35. Anti-Procrastination Sheet
Plus: Interpersonal Decision-Making
15. Self-Monitoring
31. Stimulus Control
16. Negative Practice / Worry Breaks
32. Decision-Making Form
Humor-Based
33. Daily Activity Schedule
* Copyright © 2004 by David D. Burns, M.D.
Basic* Techniques
Role-Playing
Other Motivational
19. Externalization of Voices
38. Decision-Making Form
1. Empathy
20. Feared Fantasy
Also: Agenda Setting and Hidden Emotion
2. Agenda Setting
Also: The Double Standard, Acceptance Paradox, Devil's Advocate, and all of the Interpersonal Techniques
3. Identify the Distortions 4. Straightforward Technique
Humorous
Cognitive Techniques
Behavioral
21. Paradoxical Magnification 22. Shame-Attacking Exercises
Compassion-Based
Visual Imaging
5. Double Standard Technique
23. Cognitive Flooding 24. Image Substitution
Truth-Based
39. Gradual Exposure and Flooding 40. Response Prevention 41. Distraction Also: Smile and Hello Practice, SelfDisclosure, Rejection Practice, ShameAttacking Exercises
25. Memory Rescripting
6. Examine the Evidence
Uncovering
7. Experimental Technique 8. Survey Technique
26. Hidden Emotion
9. Reattribution
27. Individual Downward Arrow
Cognitive Negative Practice, Cognitive Flooding, Memory Rescripting, Feared Fantasy, Acceptance Paradox
Interpersonal Techniques
28. Interpersonal Downward Arrow
Logic-Based
29. What-If Technique
10. Socratic Method
Motivational Techniques
11. Thinking in Shades of Gray 12. Process vs. Outcome
Semantic
Anti-Procrastination
13. Semantic Method
30. Daily Activity Schedule
14. Let's Define Terms
31. Pleasure Predicting Sheet
15. Be Specific
32. Little Steps for Big Feats 33. Anti-Procrastination Sheet
Quantitative
Anti-Resistance
16. Self-Monitoring 17. Negative Practice
34. Straightforward CBA
Philosophical / Spiritual 18. Acceptance Paradox
Exposure Techniques
Relationship Conflicts 42. Relationship CBA 43. Revise Your Communication 44. The Five Secrets 45. One-Minute Drill
Shyness and Loneliness 46. Smile and Hello Practice 47. David Letterman Technique 48. Self-Disclosure
35. Paradoxical CBA
49. Flirting Training
36. Devil's Advocate
50. Rejection Practice and Rejection Feared Fantasy
37. Stimulus Control
* Copyright © 2003 by David D. Burns, M.D.
Recovery Circle*
Empathy
16
15
Agenda Setting
1
14
2
13
Identify the Distortions
3
12
4
11 5
10 6 9
8
7
* Copyright 2003 © by David D. Burns, M.D.
Straightforward Technique
Recovery Circle*
32
31
17
30
18
29
19
28
20
27
21
26 25
22 24
23
* Copyright 2003 © by David D. Burns, M.D.
Recovery Circle*
16
15
1
14
2
13
3
12
4
11 5
10 6 9
8
7
* Copyright 2003 © by David D. Burns, M.D.
Recovery Circle*
32
31
17
30
18
29
19
28
20
27
21
26 25
22 24
23
* Copyright 2003 © by David D. Burns, M.D.
Interpersonal Therapy (IPT) Tools
Relationship Journal* Step 1 – S/he said: Write down exactly what the other person said. Be brief:
Step 2 – I said: Write down exactly what you said next. Be brief:
Step 3 – Good Vs. Bad Communication: Was your response an example of good or bad communication? Why? Use the EAR Checklist or the Bad Communication Checklist to analyze what you wrote down in Step 2.
Step 4 – Consequences: Did your response in Step 2 make the problem better or worse? Why?
Step 5 – Revised Version: Revise what you wrote down in Step 2. Use the “Five Secrets of Effective Communication.” If your revised response is still ineffective, try again.
*
Copyright 1991 by David D. Burns, MD. Revised, 2007.
EAR Checklist* Instructions. Review what you wrote down in Step 2. Was your statement an example of Good Communication or Bad Communication?
Good Communication
Bad Communication
Empathy
1.
You acknowledge the other person's feelings.
1. You ignore the other person's feelings.
Assertiveness
2.
You express your feelings openly and directly.
2. You fail to express your feelings openly.
Respect
3.
Your attitude is respectful and caring.
3. Your attitude is not respectful or caring.
The Bad Communication Checklist* Instructions. Review what you wrote down in Step 2 of the Relationship Journal. How many of the following communication errors can you spot?
Communication Error
()
Communication Error
1.
Truth – You insist you're "right" and the other person is "wrong."
10. Diversion – You change the subject or list past grievances.
2.
Blame – You imply the problem is the other person's fault.
11. Self-Blame – You act as if you're awful and terrible.
3.
Defensiveness – You argue and refuse to admit any imperfection.
12. Hopelessness – You claim you've tried everything and nothing works.
4.
Martyrdom – You imply that you're an innocent victim.
13. Demandingness – You complain when people aren’t as you expect.
5.
Put-Down – You imply that the other person is a loser.
14. Denial – You imply that you don't feel angry, sad or upset when you do.
6.
Labeling – You call the other person "a jerk," "a loser," or worse.
15. Helping – Instead of listening, you give advice or "help."
7.
Sarcasm – Your tone of voice is belittling or patronizing.
16. Problem Solving – You try to solve the problem and ignore feelings.
8.
Counterattack – You respond to criticism with criticism.
17. Mind-Reading – You expect others to know how you feel without telling them.
9.
Scapegoating – You imply the other person is defective or has a problem.
18. Passive-Aggression – You say nothing, pout or slam doors.
* Copyright 1991 by David D. Burns, MD. Revised 2001.
()
Feeling Words Chart* Blue
Down
Unhappy
Disheartened
Sad
Disappointed
Despairing
Low
Hurt
Lost
Dejected
Miserable
Ashamed
At fault
Bad
Responsible
Discouraged
Pessimistic
Desperate
Defeated
Inferior
Inadequate
Worthless
Flawed
Second-rate
Useless
Undesirable
Incompetent
Defective
Tired
Exhausted
Weary
Fatigued
Sleepy
Drained
Worn out
Lethargic
Wiped out
Uninterested
Bored
Turned off
Burdened
Abandoned
Alone
Rejected
Unloved
Unwanted
Isolated
Lonesome
Friendless
Worried
Afraid
Scared
Nervous
Apprehensive
Uptight
Tense
Terrified
Panicky
Fearful
Frightened
Alarmed
Foolish
Self-conscious
Flustered
Awkward
Humiliated
Mortified
Embarrassed
Timid
Overworked
Burned out
Tense
Frazzled
Pressured
Strained
Besieged
Overwhelmed
Mad
P. O.'d
Ticked off
Irate
Resentful
Irritated
Incensed
Annoyed
Upset
Furious
Enraged
Aggravated
Picked on
Put down
Insulted
Judged
Blamed
Intimidated
Defensive
Condemned
Stuck
Thwarted
Stymied
Envious
Mistrustful
Suspicious
Depressed
Depression
Guilty Hopeless
Unmotivated Lonely
Anxiety
Anxious
Shy Stressed
Anger
Angry
Criticized Frustrated Jealous
Paranoid
* Copyright 1989 by David D. Burns, M.D. Revised 1992, 2000, 2003.
F Fiivve eS Se ec crre ettss o off E Effffe ec cttiivve eC Co om mm mu un niic ca attiio on n ((E EA AR R:: ))** E = Empathy 1. The Disarming Technique (DT). Find some truth in what the other person is saying, even if it seems totally unreasonable or unfair. 2. Empathy. Put yourself in the other person's shoes and try to see the world through his or her eyes. Thought Empathy (TE). Paraphrase the other person's words. Feeling Empathy (FE). Acknowledge how the other person is probably feeling, based on what she or he said. 3. Inquiry (IN). Ask gentle, probing questions to learn more about what the other person is thinking and feeling.
A = Assertiveness 4. "I Feel" Statements (IF). Express your own ideas and feelings in a direct, tactful manner. Use "I feel" statements, such as "I feel upset," rather than "you" statements, such as "You're wrong!" or "You're making me furious!"
R = Respect 5. Stroking (ST). Convey an attitude of respect, even if you feel frustrated or angry with the other person. Find something genuinely positive to say to the other person, even in the heat of battle.
* Copyright 1991 by David D. Burns, MD. Revised 2006.
Reasons NOT to Change / David Burns, M.D.
Page 1
12 GOOD Reasons NOT to Listen* 1.
Truth
I'm right and you're wrong.
2.
Blame
It's all your fault.
3.
Defensiveness
I have every right to defend myself. You're full of B.S.
4.
Mistrust
If I listen to you, you'll take advantage of me.
5.
Denial
I'm the victim here. This problem isn't my fault.
6.
Entitlement
You should be the way I expect you to be.
7.
Control
I want to keep you in a one-down position.
8.
Power
I enjoy intimidating you. I like to keep you under my thumb.
9.
Competition
One of us must win and one of us must lose.
10. Revenge
I have the right to punish you. You deserve to suffer.
11. ProblemSolving
If we have a problem, we should try to solve it.
12. Hidden Agendas
I don't really want to get close to you.
12 GOOD Reasons NOT to Express Your Feelings* 1.
Conflict Phobia
People with good relationships should never fight or argue. Conflict is dangerous.
2.
Disclosure Phobia
I can't let you see how I feel inside.
3.
Emotional Perfectionism
I shouldn't feel the way I do. I should always feel happy and in control of my emotions.
4.
Submissiveness
I should always please you, even if I make myself miserable in the process.
5.
Approval Addiction
I can't risk criticism. I need your approval to feel happy and fulfilled.
6.
Love Addiction
I can't risk rejection. I need your love to feel happy and fulfilled.
* Copyright 1989 by David D. Burns, MD. Revised 2005.
Reasons NOT to Change / David Burns, M.D.
Page 2
12 GOOD Reasons NOT to Express Your Feelings* (cont'd) 7.
Perceived Narcissism
You're fragile. If I tell you how I feel, our relationship will fall apart.
8.
Hopelessness
I've tried everything and nothing works. You'll never change, so there's no point in trying.
9.
Pride
I'm above feeling angry. I don't want to lower myself and let you see how upset I feel.
10. Helping
I must help you if you're upset.
11. PassiveAggression
I'll punish you with silence. I'll get back at you indirectly and maintain a façade of innocence.
12. Mind-Reading
If you really loved me, you'd know what I want and how I feel without my having to tell you.
12 GOOD Reasons NOT to Treat the Other Person with Respect* 1.
Disdain
You don't deserve my respect.
2.
Condescension
I can't think of anything positive to say about you. There's nothing good about you.
3.
Hostility
I'm too angry to treat you with respect.
4.
Entitlement
You shouldn't be the way you are. I intend to punish you until you change.
5.
Blame
You're entirely to blame for our problems.
6.
Fear of Vulnerability
I don't want to look weak.
7.
Lack of Desire
I don't want to treat you with respect. I don't want to be close to you.
8.
Truth
How could I possibly treat you with respect? After all, I have to be honest!
9.
Genuineness
It would sound phony.
10. Justice
I have the right to get back at you.
11. Revenge
You've treated me poorly, so I have every right to get back at you.
12. Hopelessness
It won't do any good. You'll never change.
* Copyright 1989 by David D. Burns, MD. Revised 2005.
Relationship Cost-Benefit Analysis* Advantages of Blaming the Other Person
Disadvantages of Blaming the Other Person Easy
1.
I won't have to change.
1.
Nothing will change, and I won't learn or grow.
2.
It's familiar and easy. No hard work will be necessary.
2.
I'll become rigid and lose the capacity for flexible thinking.
3.
Everything will be predictable.
3.
Nothing will change.
Moral Superiority
4.
Truth will be on my side. I'll feel convinced that I'm right and the other person is wrong.
4.
The other person will insist that I'm wrong and that everything is my fault.
5.
I can feel self-righteous and morally superior.
5.
I won't experience any spiritual or emotional growth, and I may be involved in evil.
Self-Pity
6.
I can feel like a victim and a martyr.
6.
The role of victim can get pretty tiresome.
7.
I can feel sorry for myself.
7.
I may get addicted to self-pity.
Safe
8.
I won't have to feel vulnerable. I'll feel like I'm protecting myself. It feels safe.
8.
I may feel anxious anyway, because I'll be at war with the other person.
9.
Blaming the other person will protect my self-esteem and my pride.
9.
I'll be depriving myself of love, joy, and happiness.
Painless
10. I won't have to feel guilty or ashamed. 11. I can hide my faults and ignore my role in the problem.
12. I won't have to experience the pain and
10. I may feel guilty and ashamed anyway. 11. I'll be blind to my role in the problem and I won't learn or grow.
12. I won't experience the joy of intimacy.
humiliation of self-examination.
13. I won't have to be honest with myself.
13. I'll deny my flaws and have an overly positive view of myself.
* Copyright © 2005 by David D. Burns, M.D. Do not reproduce. In press.
Page 3 of 3
Relationship Cost-Benefit Analysis (cont'd)* Power
14. I'll feel powerful and in control. 15. I'll show that I can't be pushed around or
14. I'll be powerless to resolve the conflict. 15. The other person can control me and
taken advantage of.
push my buttons. Revenge
16. I can fantasize about getting revenge on
16. The other person may fantasize about
the other person.
getting revenge on me!
17. I can justify mean and petty behavior,
17. The other person may not put up with it
and tell myself that the other person deserves it.
and will probably retaliate.
18. I can be passive-aggressive. I can say
18. I may feel lonely and won't experience
and do nasty things to the other person behind their back.
19. I can justify having affairs and taking
real intimacy.
19. I'll be hurting the other person.
advantage of the other person in a variety of ways (e.g., financially). Drama
20. I can insist that I have the right to be
20. It can be exhausting to feel angry all the time. I also have the right to feel happy.
angry.
21. The anger will give my life purpose and meaning.
21. I'll get trapped by my anger and enmeshed in the conflict.
22. Life will seem dramatic and exciting. The conflict will make me feel special and important.
23. The hostility may create a certain kind of intense negative intimacy. It's a way of hanging on to my relationship with the other person. As long as we're fighting, I won't have to lose them.
22. Fighting can be an energy drain and a waste of time.
23. I'll be stuck and won't be able to move forward with my life.
Scapegoating
24. I can gossip about what a loser the other person is and get sympathy from other people.
25. I can scapegoat the other person and look down on them.
26. I can write the other person off as a jerk and convince myself that they're hopeless and not worth the effort.
24. People may get tired of my complaining and think of me as a whiner.
25. This may create a pattern for other relationships as well.
26. As long as I tell myself that the other person is a hopeless jerk, it will function as a self-fulfilling prophecy.
* Copyright © 2005 by David D. Burns, M.D. Do not reproduce. In press.
Page 3 of 3
Relationship Cost-Benefit Analysis (cont'd)* Distance
27. I can put up a wall and take pot shots at
27. I'll be up against the wall I've created!
the other person.
28. I can reject the other person.
28. I'll lose the chance to get close to the other person. Other Benefits
29. I can comfort myself by overeating, drinking or using drugs.
30. I can focus on winning and making the
29. The constant resentment may lead to headaches, fatigue, or high blood pressure.
30. I'll lose my creativity and spontaneity.
other person the loser.
31. I won't have to be responsible. I'll feel free to say and do whatever I want.
31. I'll constantly have to carry a heavy burden.
* Copyright © 2005 by David D. Burns, M.D. Do not reproduce. In press.
Relationship Cost-Benefit Analysis* Instructions. List all the advantages and disadvantages of blaming the other person for the problems in your relationship. Then balance the advantages against the disadvantages on a 100-point scale. Put two numbers that reflect your ratings in the circles at the bottom. For example, if the advantages of blame feel significantly greater, you might put a 70 in the circle on the left and a 30 in the circle on the right. If the disadvantages feel slightly greater, you might put a 45 in the circle on the left and a 55 in the circle on the right Advantages of Blame
Disadvantages of Blame
* Copyright 2004 by David D. Burns, M.D.
Relationship Cost-Benefit Analysis* Instructions. List all the advantages and disadvantages of blaming the other person for the problems in your relationship. Then balance them against each other and put two numbers that add up to 100 in the circles at the bottom. Advantages of Blame
Disadvantages of Blame
* Copyright 2004 by David D. Burns, M.D.
Memos and Administrative Tools
Your header with your name, degree, phone number and office address
Today’s Date
Dear _____, This is to confirm your appointment with me on XYZ date. I have enclosed several documents I’d like you to review and fill out prior to our first meeting. They will facilitate the initial evaluation, and include: The Brief Mood Survey The Administrative Memo The “Concept of Self-Help” memo The “How to Make Therapy Rewarding and Successful” memo You should be able to complete these surveys in approximately 30 to 45 minutes. If you have questions about any of these materials, I’ll be happy to address them when we meet. Thank you! Sincerely,
Your name and degree Your title
Administrative Information*
1. Initial Evaluation
The initial evaluation will be for consultation and not for treatment. I will review your history and pinpoint the kinds of problems you want help with. This will require at least two sessions, or one extended session. If I feel that I have the tools and skills to help you, I will share my treatment recommendations with you. This will probably involve talking therapy along with psychotherapy homework assignments between sessions. In some cases, medications might be helpful as well. If you decide that you would like to work with me along the lines that I suggest, I will be pleased to accept you as my patient at that time. If I feel that I do not have the tools to help you, or if the treatment methods I suggest do not appeal to you, you will be free to explore other treatment options and you will not become my patient. If you pursue treatment with another therapist, I will be happy to share the results of my evaluation with that therapist if you provide written permission for me to do so.
2. Scheduling
I schedule the next session at the start of each session because your needs for treatment may vary from week to week. If you feel extremely distressed, it might be helpful to meet more frequently, even for several days in a row, until the crisis is over. When you begin to feel better, it may be appropriate to taper sessions and meet less frequently. If you would prefer a standing appointment each week at the same time, I'd be happy to set it up for you.
3.
Most therapists schedule 50-minute sessions once a week. If you'd like to schedule extended sessions, or more frequent sessions, this may greatly speed up your recovery. Double or triple sessions can be extremely effective. Most therapists meet with patients for an hour a week, but there's never been any research that showed it was the best way to learn or grow. My experience indicates that intensive treatment often works far more quickly and can have long-lasting effects. If you'd like to set up an intensive treatment program, let me know. Surprisingly, intensive treatment can sometimes reduce the cost of treatment since the rate of recovery may be much faster.
Length and frequency of sessions
* Copyright © 2007, David D. Burns, M.D. Revised, 2009.
Needs discussion
I do not agree
Instructions. Put a check () in the column to the right of each item to indicate whether or not you understand and agree with it. If you feel confused or unsure, simply check "Needs discussion." Thank you!
I agree
This memo describes my clinic policies. A clear understanding of these arrangements can make our work together far more rewarding and helpful. If anything seems confusing or unfair, feel free to discuss your concerns with me at the initial evaluation. I'd be more than happy to review any of these topics with you and answer any questions you may have.
4.
Duration of therapy
This varies greatly from person to person. Some patients with mild problems have been helped in just a few sessions. Others with more severe difficulties may require many months of hard, persistent work before they feel better. It's difficult to predict this ahead of time.
5.
Billing
Patients pay for each session at that session. I do not send out monthly statements, but can provide you with receipts if you need them. I will not bill third parties for your therapy. If someone else, like a parent, wants to pay for your treatment, that's fine. However, they will have to pay you, so you can pay me at each session. I want to be clear that you're my boss. I'm working for you, and not someone else.
6.
Insurance policies
It will be your responsibility to submit forms to your insurance company for reimbursement. It might be a good idea to call them and ask questions like this: "How much will I be reimbursed for each therapy session? How many sessions will I be covered for?" Sometimes, the information will be different from what you expected. If your insurance company wants me to complete any forms about the treatment, I will be happy to so. I will show you the forms so you will have knowledge about any information I provide. In fact, I will ask you to send them to the insurance company yourself.
7.
Canceling sessions
I require a 24-hour notification to cancel a session for any reason. If you provide this advance notification, I will not charge you for the session. If you do not provide me with a 24-hour notification, you will be charged for the missed session. If I can fill your slot at the last minute, I will not charge you for the cancelled session, even if you give me less than 24 hours notice.
8.
Emergency phone calls
In certain cases, you may need to call me if a problem develops between sessions. For example, if you're experiencing a medication reaction or suddenly feel suicidal, I want you to call me right away. If a phone consultation is needed, I will charge for the time we spend together at my usual rate, based on the length of the call. Often, I can schedule additional sessions with you at the office within a day or two of your call if you need extra help. Sometimes, hospitalization may be helpful. I hope you will keep phone calls between sessions to a minimum, because, as you can imagine, I also need time to unwind. This allows me to be at my very best when I see you. If you think you will need to call me frequently between sessions, we should discuss this at the initial evaluation. If you believe you are having a life-threatening emergency and are unable to contact me or the psychiatrist covering for me for any reason, you should go to the nearest emergency room or call 911.
Needs discussion
I do not agree
Instructions. Put a check () in the column to the right of each item to indicate whether or not you understand and agree with it. If you feel confused or unsure, simply check "Needs discussion." Thank you!
Page 2
I agree
Administrative Information
9.
Patient confidentiality
I will not provide information about your treatment to others without your permission. Even if a family member calls to inquire about you, I cannot reveal that you are my patient, unless you give me permission to speak with them. Even then, my discussions with any third party would be limited to the specific topics you have given me permission to discuss. For this reason, if you would like me to speak with a relative, it is often preferable that we all meet together during a regular appointment. If anyone provides me with information about you, via phone call or letter, I will share that information with you. In other words, I will not keep any secrets from you or withhold any information from you. However, there are a few areas where I may be required by law to violate the rules of patient confidentiality. These include imminent threats of suicide, violence or homicide, as well as any pattern of child or senior citizen abuse that you may reveal, or that I may become aware of as we work together.
10. Suicidal feelings
Most depressed individuals struggle with suicidal thoughts and urges from time to time. I will monitor for suicidal thoughts during every therapy session. If they are present, we can discuss them in more detail. If at any time you become actively suicidal (for example, if you have a plan to commit suicide and intend to act on it), I may recommend hospitalization. This can be helpful, even life-saving. If you intend to commit suicide, but are not willing to be hospitalized voluntarily, then I am required by law to contact family members or the police to arrange an immediate evaluation for involuntary hospitalization. I'd be happy to discuss this or any policy with you in person, and to answer any questions you may have about it. If you require frequent hospitalizations despite our work together, I will refer you to a psychiatrist who specializes in inpatient treatment.
11. Violent feelings
Feelings of anger, including violent fantasies, are also common, and you can explore these feelings during therapy sessions. However, if you threaten to kill or do something violent to another person, and I feel that your threat is credible, I will be required by law to contact the authorities and to warn the potential victim. This amounts to a violation of our confidentiality but is required by law.
12. Child or adult abuse
If I discover you are abusing a child, senior citizen, or any other person, I will be required by law to report the problem to the authorities and to violate our confidentiality agreement.
Needs discussion
I do not agree
Instructions. Put a check () in the column to the right of each item to indicate whether or not you understand and agree with it. If you feel confused or unsure, simply check "Needs discussion." Thank you!
Page 3
I agree
Administrative Information
13. Meeting outside of sessions
I do not meet with patients, friends or family members of patients outside of sessions for any reason.
14. Business dealings
I do not get involved in any business dealings with patients. Our work together will focus on the problems and symptoms you need help with.
15. Disability claims and legal issues
I do not do disability evaluations or sign disability claims, since this represents a conflict of interest. If you wish to be evaluated for disability, I can suggest the names of forensic experts who can provide that service for you. I will not provide copies of my evaluation, or reports of our work together, to anyone involved in a disability claim. If you are involved in any legal action, such as a divorce proceeding or a lawsuit, I will not testify in your behalf or provide copies of my records or reports of our work together unless I am legally forced to do so by a judge. Here's the rationale for this policy. If you recover and I have to report that to someone who is providing disability payments, then you could lose that income. This conflict of interest could prevent us from working together effectively. But if I don't have any involvement in any forensic issues, we can work together toward your recovery without any competing concerns about financial gains or losses.
16. Premature termination
If you become discouraged between sessions or feel the urge to drop out of therapy for any reason, I'd strongly encourage you to come in for an additional session to discuss your feelings. This often leads to a therapeutic breakthrough. If you are not comfortable with this arrangement, and want the right to drop out between sessions, please let me know at the initial evaluation.
17. Gifts
I do not accept gifts from patients or family members of patients because this is considered an ethics violation.
18. Books or articles that you've written
Sometimes, patients give me copies of books or other materials they've written and ask me to read them between sessions. I do not read these kinds of materials between therapy sessions. However, if you feel they are relevant to my understanding of your problems or our work together, I'd be happy to review them with you during one of our sessions. In most cases, your verbal summary will be sufficient.
Needs discussion
I do not agree
Instructions. Put a check () in the column to the right of each item to indicate whether or not you understand and agree with it. If you feel confused or unsure, simply check "Needs discussion." Thank you!
Page 4
I agree
Administrative Information
19. Psychotherapy homework
I will ask you to do homework between sessions, including written assignments. These assignments can greatly enhance your understanding and speed your recovery. Generally, 10 to 20 minutes per day will be sufficient. We will review your psychotherapy homework together during sessions. If you are not willing to do psychotherapy homework, or feel you cannot do the homework for any reason, please let me know at the initial evaluation.
20. Relapse prevention
Therapy has two goals. Feeling better and getting better. Feeling better means that you overcome your symptoms and solve the problems that brought you to therapy. If you're suffering from depression or panic attacks, feeling better means that the depression and panic attacks will disappear. Feeling better is tremendously important! Getting better means that you learn the tools to deal with any emotional or relationship problems that might emerge in the future. This is vitally important because no one can be happy forever. We all run into bumps in the road from time to time. But if you know how to deal with painful mood swings or conflicts with other people, they won't be such a threat or a problem. Before we terminate, I'll need at least one final session so I can teach you some relapse prevention techniques and review our work together. Then, if you ever need a tune-up in the future, you'd be welcome to return so we can try to nip the problem in the bud right away. That will make the termination of our work therapy together more comfortable and enlightening for you, and you'll know that you can return anytime in the future if you have the need. In most cases, only a few sessions will be required to overcome a relapse, especially if we've done good work together initially.
21. HIPAA
I have received and reviewed the Privacy Practices information on page 6.
Needs discussion
I do not agree
Instructions. Put a check () in the column to the right of each item to indicate whether or not you understand and agree with it. If you feel confused or unsure, simply check "Needs discussion." Thank you!
Page 5
I agree
Administrative Information
Administrative Information
Page 6 Description of Privacy Practices
This is a summary of the clinic’s privacy practices, describing how medical information about you is used and disclosed and how you can get access to this information. If you would like more information, please feel free to discuss these matters with me personally. You can also read about The Health Insurance Portability and Accountability Act (HIPAA), which is legislation that governs the electronic transfers of health data. This information can be found on the Internet at http://www.hhs.gov/ocr/hipaa/ You have the following rights regarding your medical information: 1. You may inspect and obtain a copy of your medical records 2. You may add an addendum to or correct your medical records 3. You may request an “accounting of disclosures” of your medical information that documents any releases of your medical information 4. You may request restrictions on certain uses or disclosures of your medical information 5. You may request that we communicate with you in a certain way or at a certain location 6. You may request a full written version of the privacy practices My disclosure of your medical information will be only for the following purposes: 1. To provide you with medical treatment and services 2. To bill and receive payment for the treatment and services you receive 3. For functions necessary to run the clinic and to assure that all patients receive quality care 4. As required or permitted by law In certain situations, I may disclose your medical information without your authorization, including: 1. For worker’s compensation or similar programs 2. For public health activities (e.g. reporting abuse or reactions to medications) 3. To a health oversight agency, such as the California Department of Health Services 4. In response to a court or administrative order, subpoena, warrant or similar process 5. To law enforcement officials in certain limited circumstances 6. To a coroner, medical examiner or funeral director 7. To organizations that handle and tissue procurement or transplantation
Depression 1. 2. 3. 4. 5.
4—Extremely
Instructions. Use checks () to indicate how depressed, anxious or angry you've been feeling over the past week, including today. Please answer all the items.
3—A lot
0—Not at all
Brief Mood Survey*
2—Moderately
Date: 1—Somewhat
Name:
Sad or down in the dumps Discouraged or hopeless Low self-esteem, inferiority, or worthlessness Loss of motivation to do things Loss of pleasure or satisfaction in life Total Items 1 to 5 Suicidal Urges
1. Have you had any suicidal thoughts? 2. Would you like to end your life? Total Items 1 to 2 Anxiety 1. 2. 3. 4. 5.
Anxious Frightened Worrying about things Tense or on edge Nervous Total Items 1 to 5 Anger
1. 2. 3. 4. 5.
Frustrated Annoyed Resentful Angry Irritated Total Items 1 to 5
1. 2. 3. 4. 5.
Communication and openness Resolving conflicts and arguments Degree of affection and caring Intimacy and closeness Overall satisfaction Total Items 1 to 5 * Copyright 1997 by David D. Burns, M.D. Revised, 2002.
6—Very
5—Moderately
4—Somewhat
3—Neutral
2—Somewhat
1—Moderately
Instructions. Use checks () to show how satisfied or dissatisfied you feel in your closest personal relationship. Please answer all 5 items.
Satisfied
Dissatisfied
0—Very
Relationship Satisfaction*
Page 2
The Concept of Self-Help* The purpose of treatment is to feel better, to understand why you got depressed or anxious, and to learn to cope more effectively in the future. There are several reasons why you may feel better during therapy: 1. You may experience an emotional uplift because you solve a personal problem. 2. You may appreciate the support of a therapist who understands you and approves of you. 3. You may benefit from an antidepressant medication. 4. You may do things to help yourself between therapy sessions, such as scheduling more productive and rewarding activities, becoming more assertive with people, or recording the negative thoughts that upset you. Some of the newer forms of therapy emphasize a structured self-help program as a part of the treatment. People who do these self-help assignments between therapy sessions usually make the most rapid gains. In contrast, people who are unwilling to help themselves between sessions are often slow to improve. For this reason, it’s crucial for you to decide whether you are willing to make an effort to help yourself as a part of your treatment. Please answer the following questions and return this memo to your therapist at the next session so you can review it together.
Put a check ( ) in the box to indicate the way you think and feel. 1.
I understand that my therapist emphasizes a self-help program as a key to personal growth.
2.
I am willing to do things to help myself between therapy sessions.
yes
no
needs discussion
Please indicate how frequently you will do the self-help assignments:
Self-Help Contract In the boxes to the right, indicate how much time you will spend on the self-help assignments between sessions. 1.
How much time do you agree to spend on self-help assignments between sessions each day? (please fill in the time to the right).
2.
How many days per week are you willing to do self-help assignments between sessions?
3.
How many weeks will you continue doing the self-help assignments while you are in therapy?
* Copyright
1982 by David D. Burns, M.D. Revised, 1994.
______________ (minutes per day) ______________ (days per week) ______________ (weeks)
Therapist’s Toolkit, Part 2
Page 76
SELF-HELP FORMS AND METHODS The following is a review of some self-help methods your therapist may use. 1. Activity Schedules: A variety of forms are available to help you organize your time more productively. 2. Daily Mood Log: A journal for recording negative feelings and thoughts. 3. Checklist of Cognitive Distortions: A list of the ten types of twisted thinking that lead to depression, anxiety, guilt and anger. 4. The Pleasure Predicting Sheet: You predict the amount of satisfaction you will get from activities with the potential for pleasure, learning or growth. 5. Bibliotherapy: Your therapist may assign chapters from a self-help book. 6. Self-Assessment Tests: Your therapist may ask you to take selfassessment tests between sessions to evaluate the severity of depression or anxiety as well as the satisfaction you feel in your closest relationship. These tests can help you track your progress in therapy. 7. Therapeutic Empathy Scale: You rate your therapist’s warmth, understanding and genuineness after each session, and review this information with him or her at the beginning of the next session. 8. Communication Training: Your therapist may teach you the Five Secrets of Effective Communication. These skills can help you deal more effectively with problems in personal or professional relationships. 9. Decision-Making Form: This helps you weigh the advantages and disadvantages of various options when you face difficult personal decisions. 10. Taping Sessions: Your therapist may ask you to tape your sessions so you can listen to the tapes at home between sessions. During a productive session you may discover many exciting insights which all seem perfectly clear. An hour or two later, you may have trouble remembering what the session was about. When you listen to the tape, it all becomes clear again. Many patients report that the tapes are more helpful than the actual sessions.
The Concept of Self-Help
Page 77
25 GOOD REASONS FOR NOT DOING THE SELF-HELP ASSIGNMENTS BETWEEN SESSIONS The following are some of the reasons why you may resist doing the self-help assignments between sessions. Put a check ( ) in the box to the right that best indicates how you usually think and feel. 1.
The Love Addiction: You may feel that being loved by someone you care about is the only real key to happiness and self-esteem. Therefore, you can’t conceive of finding happiness by learning to cope with your problems on your own. Self-help techniques may seem too cold or mechanical. Do you feel like this?
2.
Perfectionism: You may feel that if you can’t do things perfectly, there’s no point in doing them at all. Does perfectionism sometimes make it hard for you to complete tasks?
3.
Fear of Disapproval: You may be afraid that your therapist will think less of you when s/he reviews your selfhelp assignments. You may think that if you make a mistake, you will appear incompetent or stupid. Do you sometimes get defensive and upset when you are criticized?
4.
Putting the Cart Before the Horse: People who procrastinate have the idea that motivation comes before action. They tell themselves, “I don’t feel like it now, so I’ll put it off until later when I’m in the mood.” But the motivation doesn’t come, and they end up doing nothing. In contrast, highly successful people know that action comes first, and motivation comes later. They get started, whether or not they “feel like it.” Once they start, they feel more motivated. Do you sometimes put things off because you don’t feel in the mood?
5.
Unexpressed Anger: You may resent something your therapist said or react negatively to his or her personality. Instead of expressing these feelings, you may avoid the problem and express your feelings indirectly--by canceling sessions at the last minute, by arguing, or by failing to complete the self-help assignments. Do you have a tendency to avoid talking things over when you’re angry with someone?
6.
Hopelessness: The prognosis when you feel depressed is excellent. Nevertheless, many people feel convinced that their problems will go on and on forever, no matter what. If you feel hopeless and demoralized, you may give up and do nothing. Then nothing changes, and you feel more convinced that you’re hopeless. Do you have any feelings of hopelessness that might make it hard for you to do the self-help assignments?
7.
Coercion Sensitivity: You may at times feel that people are trying to force you to do things. Friends or family may seem pushy and bossy. Consequently, you may dig in your heels and resist, because you don’t want them to control you. Do you sometimes feel as if people are bossing you around?
8.
Fatalism: You may feel that your moods are governed by forces beyond your control, such as hormones, fate, or God, so there may seem to be little point in trying to change the way you feel. Do you think this way?
not at all
somewhat
a lot
Therapist’s Toolkit, Part 2
Put a check ( ) in the box to the right that best indicates how you usually think and feel. 9.
Blame: Some people feel that others are to blame for their bad moods. If you feel your problems aren’t your fault, it may seem unfair that you should have to work hard to feel better. As one woman put it, “Why should I have to change!? My husband is the one who’s making me miserable!” Do you sometimes feel like someone else is to blame for the way you feel?
10. Shame or Guilt: You may have a problem that would be difficult to discuss with your therapist, such as alcoholism or drug abuse, a sexual indiscretion, violence, or an angry reaction to something the therapist said. Do you have any problems which you feel reluctant to discuss with your therapist? 11. Medical Model: If you go to the doctor because of a fever, you expect him to diagnose the illness and prescribe bed rest plus an antibiotic. By the same token, some people who are anxious or depressed feel that only a pill could make them feel better. The idea of doing self-help assignments does not make sense to them. Do you sometimes feel that only a medication could make you feel better? 12. The “Realism” of Depression: Some people are reluctant to work at getting better because they are convinced that their problems are real and that their misery is inevitable. They do not believe they have a treatable illness. Some people feel there’s no point in trying to correct the distortions in their thoughts, because they are convinced their negative thoughts are absolutely valid. Do you sometimes feel as if your negative feelings are absolutely realistic and valid? 13. Reluctance to Give Up Negative Feelings: Some people are reluctant to give up feelings of anger, guilt, depression or anxiety because they believe these feelings are beneficial to them. A psychologist with test anxiety was so petrified about flunking her licensure examination that she was unable to study for it. However, she resisted therapy because she thought her worrying would motivate her to prepare for the examination more carefully. Do you sometimes feel reluctant to give up your negative feelings? 14. Low Frustration Tolerance: Many people don’t stick with tasks if they don’t get immediate results. If they have a set-back, they give up instead of persisting. A number of ups and downs are an inevitable part of any treatment, and there will be times when you feel stuck. If you have a low frustration tolerance, you may have the urge to stop doing the assignments. Do you sometimes give up on things when you feel frustrated? 15. Superman/Superwoman: You may feel that if you ask a therapist for help, it means that you’re weak, defective or inferior. You may feel like you should be able to solve all your problems on your own. Do you sometimes feel like this? 16. Lack of Motivation: You may be in therapy because you feel pressured by someone, such as your parents, the court or your spouse. If you aren’t motivated to be in treatment, you obviously won’t want to spend time doing self-help assignments between sessions. Do you have negative feelings about being in treatment?
Page 78
not at all
somewhat
a lot
The Concept of Self-Help
Put a check ( ) in the box to the right that best indicates how you usually think and feel. 17. Feeling Over-Committed: Some people are over-committed to work and to family. You may think the selfhelp assignments will only add to your burdens instead of giving you new energy to solve your problems. Do you feel that the self-help assignments may be too much for you? 18. Resistance to “Homework:” You may have bad memories of being in school and having to do homework every night. Do you have a negative reaction to the idea of doing homework between therapy sessions, because it’s too much like being in school again? 19. Feeling Overwhelmed by Depression: Some people feel so overwhelmed by all the problems in their life that they simply don’t know where to start. Other people feel like it wouldn’t do much good just to work on one problem at a time. Do you feel as if you don’t know where to start or what problem to work on first? 20. The “Talking Cure:” Some people feel that just talking to their therapists and getting their problems off their chests should be enough to make them feel better. Others feel that if they talk about their childhood experiences, they will develop an insight that will change the way they feel. Do you feel that just talking to your therapist once a week, without doing self-help assignments, should be enough? 21. Passivity and Helplessness: Some depressed people feel passive and inadequate. They may be unaware that they control other people by acting helpless and often get rewarded for this behavior. During a marital therapy session a severely depressed woman announced: “I think I need a cigarette.” Her obedient husband immediately picked up the pack of cigarettes from the table, took one out, placed it in her mouth, and lit it for her. His obedient behavior rewarded her for acting as if she couldn’t do anything for herself and had to be waited on. Do you sometimes feel passive and helpless when you’re in a bad mood? 22. Fear of Change: In spite of their misery, some people are afraid that any change in the status quo will make things worse. Others think their identity depends on being chronically angry and depressed. Do you have any fears about changing your life? Do you sometimes feel reluctant to give up your depression or anger? 23. Self-Pity/Martyrdom: Although depression can be intensely painful, some people take pride in their suffering. As one woman put it, “I think I like being depressed and feeling sorry for myself.” Her therapist asked her to make a list of the advantages of being depressed and the disadvantages of being happy. She discovered that if she remained depressed, she would get lots of attention from her husband and wouldn’t have to do housework or look for a job, which frightened her. Paradoxically, this insight motivated her to work harder in the therapy. Do you sometimes feel sorry for yourself and reluctant to let go of your depression?
Page 79 not at all
somewhat
a lot
Therapist’s Toolkit, Part 2
Put a check ( ) in the box to the right that best indicates how you usually think and feel.
Page 80
not at all
somewhat
a lot
24. Resistance to Brief Therapy: Some people feel committed to the idea that treatment must involve years and years of exploring the past. The idea of being treated for a severe depression in a short period of time using self-help assignments may seem gimmicky. You may tend to think of any fast-acting therapy as a psychological “Band-Aid” or “The Power of Positive Thinking.” Do you sometimes feel like any short-term treatment is bound to be superficial? 25. Entitlement: Some people feel entitled to happiness and fair treatment from others. They deeply resent the implication that they are responsible for how they feel. Do you sometimes feel entitled to a better life and think you shouldn’t have to work at things so hard? 26. Other: Can you think of any other reasons for not doing the self-help assignments? Please record your ideas here:
SUMMARY After reading this memo, you may have a better understanding of the advantages and disadvantages of doing self-help assignments between therapy sessions. Indicate how you feel about this issue now. Return this memo to your therapist so you can discuss it at the next session. Put a check ( ) in the box to the right to indicate how you now think and feel. 1. I believe that the self-help assignments could be an important part of my treatment. 2. I am willing to do the self-help assignments between therapy sessions. 3. I would prefer to be referred to a therapist who does not use self-help assignments as a part of the treatment.
yes
no
needs discussion
Premature Termination In spite of your best efforts, some patients will simply drop out of therapy between sessions, and they will not agree to come in for a final session to review their feelings. Many patients are passive, passive-aggressive, or just plain irresponsible. In these cases, you can send a friendly but firm letter that will make it crystal clear that they've knowingly and willfully terminated treatment and that you are no longer engaged a therapeutic relationship with them. This is important from a legal perspective. If you don't get closure on someone who stops coming for sessions, and they act out later on, even six months down the road, you may be legally responsible for their behavior. Unfortunately, suicide attempts are common. In fact, some experts claim that as many as 10% of patients suffering from chronic depression eventually commit suicide. Although homicide is rare among depressed and anxious patients, it can also occur. Violence is probably more common among angry patients, as well as those with substance abuse or Antisocial Personality Disorder. Violence and suicide are nightmares for therapists, to say nothing of your patients and their families. On page 2, you'll find a copy of the letter I send to patients who drop out between sessions. I edit it slightly so it will sound personal and reflect the details of each situation. You can add the patient's name and include any details that may be relevant. I don't think it's necessary to send the letter via certified mail, but that's a question for your legal consultant to address. It's not usually a good idea to prescribe meds for a patient until you complete the intake evaluation, which may require a couple of sessions. At intake, you're deciding whether or not to accept the patient into treatment, and vice versa. If you prescribe medications prematurely, the patient may drop out of therapy and end up with one or more bottles of pills you've prescribed. So you're legally responsible, even though the patient is not accountable to you. Why set yourself up for that kind of anxiety? It's not good for you or the patient. Of course, there are exceptions to every rule. Sometimes, you may have to prescribe a few days or a week's worth of medication while you're completing the intake evaluation. You can minimize the problem of premature termination by taking a proper history and by using the memos in the Therapist's Toolkit, such as the Concept of Self-Help memo and the How to Make Therapy Rewarding and Successful memo. In addition, you can get patient feedback using the Before and After Session version of the Brief Mood Survey with the Evaluation of Therapy Session on the back. That way, patients will rate the session in the waiting room before leaving the office, so you'll know right away about any negative reactions they had. This information will prevent the majority of premature terminations, because you can discuss the patient's negative feelings at the beginning of the next session and get the therapy back on track. You'll also have documentation about whether they had any suicidal fantasies or urges after the session. If you discover that they've become actively suicidal, you can intervene immediately and save their life. And if they don't reveal any suicidal urges, you'll have some documentation in your chart that may protect you from a legal perspective in case something tragic does happen. If patients don't want to fill out these types of forms throughout the treatment, then I don't accept them for treatment. It's not optional. This may sound harsh, but I've discovered over the years that it pays to practice defensively.
Premature Termination
Page 2
Dear _____________, I'm concerned that you missed your most recent therapy sessions on __________________ and __________________. If you're feeling discouraged or upset about the treatment, it can be helpful to discuss those feelings face-to-face. These discussions can lead to improved teamwork and increased satisfaction with the therapy. And even if you decide to terminate the treatment, a final session will give us the chance to review what you've liked and disliked about our work together, and will allow us to work together in the future if the need arises. If you'd be willing to meet with me, please contact my office to set up a session at a time that's convenient for you. If I do not hear from you within one week, I'll assume that you've decided to terminate treatment and that you no longer wish to be my patient. In that event, I'd strongly encourage you to continue your work with another therapist, because I believe that treatment is indicated and that the prognosis is positive. If you need help finding another therapist, I'd be happy to suggest the names of several therapists whose work I respect. I'd also be willing to speak to your new therapist and summarize the work we did, including my initial history and evaluation, if you want me to do so and send me written permission to share the information with your new therapist. In addition, my records indicate that you are taking the following psychiatric medications: Medication
Current Dose
1. 2. 3. 4. 5. These medications MUST be managed by a physician. Even the decision to taper off these medications requires medical supervision. For this reason, it is mandatory for you to call me immediately or to seek consultation with another physician for ongoing medication management right away. I hope you decide to call. If I do not hear from you, I want to thank you for giving me the chance to work with you, and wish you the very best. Sincerely, Your name and degree
How to Make Therapy Rewarding and Successful * This memo contains information vital to the success of your therapy. Please read it carefully, fill out the multiple choice items, and return it to your therapist at the next session. He or she will be happy to discuss any questions you may have.
HOW CAN I TELL IF THE THERAPY IS HELPING ME? You can monitor the effectiveness of your treatment and the rate of your improvement with brief, accurate, self-assessment tests. These tests measure feelings of depression and anxiety and several other symptoms. Your therapist will provide copies of these tests for you to fill out in the waiting room prior to each appointment. This will only take a couple minutes. Show the results to your therapist at the beginning of every session. Your therapist may also ask you to take these tests again at the end of each session to measure your improvement. Leave the test for your therapist before you go home. That way, you'll both be aware of how you're responding to therapy and what techniques are working, as well as what techniques are not helping. This information will help guide the treatment in a positive direction.
HOW CAN I TELL IF I HAVE A GOOD RELATIONSHIP WITH MY THERAPIST? In therapy, it’s important to know that your therapist respects you and understands you. This doesn’t mean that therapy will always be smooth and free of conflict. In fact, a certain amount of conflict is a normal part of therapy. Sharing negative feelings openly and respectfully is invaluable and can lead to a greater sense of understanding and teamwork. The Report of Therapy Session asks you to indicate how much warmth, trust and understanding you felt from your therapist during your most recent therapy session. You can also indicate how helpful the session was and whether you had any negative feelings that you didn't get a chance to mention. Please complete the Report of Therapy Session in the waiting room after each session along with the mood tests described above. You and your therapist can discuss the results at the beginning of the next session.
* Copyright
1982 by David D. Burns, M.D. Revised, 1994, 1995, 2006.
Therapist’s Toolkit
Page 2
WHAT SHOULD I DO IF I FEEL STUCK OR IF I’M UPSET WITH MY THERAPIST? There probably will be times when you feel stuck and convinced you aren’t making any progress. You may get annoyed with something your therapist said or feel convinced that she or he doesn’t really understand how you feel inside. Frequently, these reactions will be quite justified! It can be extremely helpful to talk these feelings over with your therapist, even though it isn’t always easy. You may be afraid of conflict or concerned about hurting your therapist’s feelings. If you don't tell your therapist how you feel, the feelings may sabotage your progress. Most good therapists have enough selfesteem and objectivity to listen without getting defensive. A frank discussion of your feelings will often lead to an unexpected therapeutic breakthrough.
WHAT SHOULD I DO IF I GET TURNED OFF AND DECIDE TO DROP OUT OF THERAPY BETWEEN SESSIONS? Unfortunately, some people drop out of treatment prematurely and do not receive the benefit of the treatment. Persistence is the key to success. If you get upset and decide to drop out between sessions, it would be valuable to come for one additional session to discuss your concerns. These moments when therapy seems to be failing are often the greatest opportunities for personal growth. Frequently, you'll feel better and the therapy will get back on track. If you're still not satisfied, your therapist can help you find a referral to another therapist. Instructions. The following questionnaire describes a number of reasons people end therapy prematurely. Please use checks ( ) to indicate how you usually think and feel, and return it to your therapist at the next session.
Conflict Phobia Some people avoid conflict and sweep their feelings under the carpet. Is it hard for you to talk things over when you feel upset with someone? 1. ____ I do not find it difficult to express negative feelings. 2. ____ It’s somewhat difficult for me. 3. ____ It’s moderately difficult for me. 4. ____ It’s extremely difficult for me. If you felt mistrustful or upset with your therapist, would you be inclined to drop out of therapy between sessions? 1. ____ I would not drop out between sessions if I felt upset. 2. ____ There is a slight chance I’d drop out if I felt upset.
How to Make Therapy Rewarding and Successful
Page 3
3. ____ There’s a moderate chance I’d drop out. 4. ____ It’s very likely that I’d drop out.
Therapeutic Niceness Your therapist may be very caring, but the treatment may not be effective. Would you find it hard to criticize a therapist who was friendly and nice to you? 1. ____ I would not find it difficult to criticize a therapist who was overly nice to me. 2. ____ I would find it somewhat difficult. 3. ____ I would find it moderately difficult. 4. ____ I would find it extremely difficult. If you felt you weren’t getting anywhere and your therapist was “too nice,” would you drop out of therapy and avoid discussing this? 1. ____ I would not drop out of therapy. 2. ____ There’s a slight chance I’d drop out. 3. ____ There’s a moderate chance I’d drop out. 4. ____ It’s very likely that I’d drop out.
Financial Problems Could financial concerns make it difficult to continue your therapy? 1. ____ The cost of therapy will not be a problem for me. 2. ____ It’s somewhat likely that the cost will be a problem. 3. ____ It’s moderately likely that the cost will be a problem. 4. ____ It’s extremely likely that the cost will be a problem. If the cost of therapy became a problem, how inclined would you be to drop out of therapy between sessions without talking things over? 1. ____ Not at all likely 2. ____ Somewhat likely 3. ____ Moderately likely 4. ____ Extremely likely
Shame Many people have problems it ‘s hard to talk about, such as sexual difficulties or fantasies, sexual or physical abuse, violent or suicidal impulses, drug or alcohol abuse, rituals or habits such as binge-eating and vomiting, or illegal activities, to name just a few.
Therapist’s Toolkit
Page 4
Feelings of shame may make it hard to discuss these difficulties. You may be afraid that your therapist will judge you. You may fear that your therapist will not protect your confidentiality and will disclose your feelings to others. You may believe that if you don’t talk about your problems, they will go away sooner or later and you won’t have to face them. Do you have problems that might be hard to talk to your therapist about? 1. ____ Yes 2. ____ Maybe 3. ____ No How inclined would you be to drop out of therapy so that you don’t have to discuss these difficulties? 1. ____ Not at all likely 2. ____ Somewhat likely 3. ____ Moderately likely 4. ____ Extremely likely How helpful do you think it would be to discuss all of your problems with your therapist? 1. ____ Not helpful 2. ____ Somewhat helpful 3. ____ Moderately helpful 4. ____ Extremely helpful
Low Motivation Some people want to be in therapy, while others have mixed feelings about it. If you're not motivated to be in therapy, you may be inclined to drop out of therapy between sessions. There are many reasons that you might not want to be in therapy. You may feel skeptical that the therapy could help. You may feel that others are to blame for your problems and resent the fact that you should have to change. You may feel pressured by family members or authorities to come to treatment. You may feel that coming to therapy makes you appear weak or sick, and think you should be able to work out your problems on your own. You may be afraid that therapy will be upsetting, or think that you will have to give up something, like violence, overeating or alcohol abuse, in order to get better. How strongly do you want to be in therapy? 1. ____ In all honesty, I do not feel particularly motivated to be in therapy right now.
How to Make Therapy Rewarding and Successful
Page 5
2. ____ I feel somewhat motivated to be in therapy. 3. ____ I feel moderately motivated to be in therapy. 4. ____ I feel extremely motivated to be in therapy. If you suddenly lose the motivation to be in therapy, how inclined would you be to drop out of therapy between sessions? 1. ____ Not at all likely 2. ____ Somewhat likely 3. ____ Moderately likely 4. ____ Extremely likely
High Expectations Some people expect therapy to work rapidly and dramatically. Although this sometimes happens, most people need longer periods of time to overcome their problems. If you don't get positive results as quickly as you hoped, you may think that the therapy cannot help and have the urge to drop out. How many sessions and months do you expect your therapy will require? Take your best guess. 1. ____________
sessions
2. ____________
months
What's the maximum number of sessions and months you'd be willing to participate in therapy? 1. ____________
sessions
2. ____________
months
If you felt you weren’t making progress fast enough, would you be tempted to drop out between sessions without talking things over with your therapist? 1. ____ I would not be tempted to drop out between sessions. 2. ____ I would be somewhat likely to drop out. 3. ____ I would be moderately likely to drop out. 4. ____ I would be very likely to drop out.
Hopelessness Many individuals feel hopeless at times. Your problems might seem overwhelming and impossible to solve. You may be tempted to drop out of therapy because you believe that the treatment cannot possibly help. Do you sometimes feel hopeless and pessimistic that things could ever get better?
Therapist’s Toolkit
Page 6
1. ____ I rarely or never feel hopeless. 2. ____ I sometimes feel hopeless. 3. ____ I often feel hopeless. 4. ____ I nearly always feel hopeless. If you suddenly felt hopeless between sessions, would you feel tempted to cancel your next session and drop out of therapy? 1. ____ No, I would not drop out if I felt suddenly hopeless. 2. ____ I would be somewhat tempted to drop out. 3. ____ I would be moderately tempted to drop out. 4. ____ I would be extremely tempted to drop out.
Relapse After you improve, you may suddenly relapse and sink back into depression again and conclude, “My improvement was just a fluke. I’m basically hopeless after all. I might as well give up.” Nearly all patients experience this. It’s crucial to persist at these times, and to continue to apply the skills you are learning. If you do, there will nearly always be a second wave of improvement and you will learn how to control your moods more effectively. If you improved in therapy and then got suddenly worse, would you feel tempted to cancel your next session and drop out of therapy? 1. ____ I would not feel at all inclined to cancel my next session and drop out. 2. ____ I would feel somewhat inclined to drop out. 3. ____ I would feel moderately inclined to drop out. 4. ____ I would feel extremely inclined to drop out. If you improved and then got suddenly worse, would you meet with your therapist to discuss this problem? 1. ____ I would probably not want to meet with my therapist if I suddenly got worse. 2. ____ I would be slightly willing to meet with my therapist. 3. ____ I would be moderately willing to meet with my therapist. 4. ____ I would be very willing to meet with my therapist.
How to Make Therapy Rewarding and Successful
Page 7
Premature Recovery Sometimes people feel suddenly better and then tell themselves, “Hey, I feel great. I don’t need any more treatment.” If this happens, it would be helpful if you would meet with your therapist for one final session to review what was helpful, to bring therapy to an appropriate closure and to make plans in case you need additional sessions in the future. If you felt suddenly better, would you be tempted to drop out between sessions? 1. ____ I would not be tempted to drop out of therapy between sessions if I suddenly felt happy. 2. ____ I would be somewhat tempted to drop out. 3. ____ I would be moderately tempted to drop out. 4. ____ I would be extremely tempted to drop out. If you felt suddenly better between sessions, would you meet with your therapist again? 1. ____ I would not meet with my therapist. 2. ____ I would be somewhat inclined to meet with my therapist. 3. ____ I would be moderately inclined to meet with my therapist. 4. ____ I would definitely meet with my therapist.
Other Can you think of any other problems which might make you feel like dropping out of therapy between sessions? Please describe them here: __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________ __________________________________________________________
Therapist’s Toolkit
Page 8
SUMMARY If you were dissatisfied with your auto mechanic, you would have every right to stop going to that person, and you would have no obligation to explain why. Therapy is a little different because discussing your negative feelings can be an important part of the therapeutic process. We respect your right to terminate at any time for any reason, but hope that we will have a chance to resolve any problems before you finalize your decision. Prior to the last session, your therapist may ask you to complete a form called the Patient’s Evaluation of Therapy. On this form, you can indicate what you liked and disliked about the treatment, how much you have improved, and what further work needs to be done. Reviewing your responses with your therapist during the last session will give both of you a chance to review the therapy and bring the treatment to an appropriate closure. Perhaps you feel ready to make a commitment to talk things over with your therapist if a problem comes up between sessions. Or perhaps you still feel unsure and need to discuss this issue with your therapist. Which statement best describes how you now feel? Put a () in one of these three boxes to indicate how you feel: 1.
I'm willing to make a definite commitment to speak with my therapist in person during a regularly scheduled therapy session before I make any decision to end therapy.
2.
I'm not sure whether or not I'm willing to make that commitment.
3.
I'm not willing to make that commitment. I want the right to drop out of treatment at any time for any reason without discussing this decision with my therapist.
Keep in mind that it can sometimes be difficult to keep this commitment. If you feel upset with your therapist, you may have an overwhelming temptation to avoid talking things over face-to-face. It can require determination not to give in to this urge. The benefits of confronting the problem instead of walking away from it can be considerable.
Motivational Tools
Why Our Patients Resist* By David D. Burns, M.D. Outcome Resistance— Why Patients Cling to the Status Quo
Process Resistance— Why Patients Resist Working Hard To Change
Depression
Depression
Worthlessness. I don't deserve to feel good because I really am inferior or defective. Guilt. I don't deserve any happiness or self-esteem because I'm bad and I deserve to suffer. Realism of Depression. Life really is awful. People who feel happy are stupid and naïve. Perfectionism. If I beat up on myself relentlessly whenever I fall short, it will motivate me to achieve great things. Achievement Addiction. I couldn't possibly feel happy or fulfilled until I've accomplished something outstanding. But I've never done anything special, so I could never feel any real joy or self-esteem. Love Addiction. I couldn't possibly feel happy or fulfilled without a loving relationship. Self-Pity. I like being a victim and feeling sorry for myself. Anxiety Magical Thinking. My fears protect me or my loved ones. If I stop worrying, something terrible may happen. No Pain, No Gain. My constant worrying is the price I have to pay to do superb work. If I stop worrying, I'll get complacent and fail. Conflict / Anger Phobia. I don't want to face the problem that's triggering my anxiety in the first place.
Hopelessness. Nothing will ever change, so why try? If I don't get my hopes up, I won't be disappointed. Motivational Paralysis. I don't feel like doing any self-help assignments between sessions. I'll wait until I'm in the mood. Overwhelmed. The psychotherapy homework assignments are just too much work. I'm drowning in commitments and don't have time to do more. Entitlement. I shouldn't have to work so hard to recover. Medical Model. My doctor said that I have a chemical imbalance in my brain, so a pill should cure me. Traditional Psychiatric Model. I thought that all I had to do was come to sessions, talk about all the problems in my life, and explore the past.
Anxiety Avoidance. Facing my worst fears will be dangerous and uncomfortable. I shouldn't have to do that. There has to be an easier way. Medical Model. The ad I saw on TV said that my shyness results from a chemical imbalance in my brain, and that an antidepressant will solve the problem.
* Copyright © 2005 by David D. Burns, M.D. Do not copy or distribute without written permission.
Why Our Patients Resist (cont'd)* Outcome Resistance— Why Patients Cling to the Status Quo
Process Resistance— Why Patients Resist Working Hard To Change
Anger / Relationship Problems
Anger / Relationship Problems
Low Desire. I don't really want to get close to you. I just want to complain about you and keep you at a distance! Martyrdom / Heroism. I like the role of victim. Moral Superiority. I enjoy feeling superior and looking down on you. You're a loser. Gossip / Scapegoating. It's rewarding to talk to my friends about what a loser you are. They all agree with me, too! Power. I want to control you. Revenge. I have every right punish you because of the way you've treated me. Anger addiction. I like feeling angry and bitter. It's rewarding. Violence. Aggression is exciting. I enjoy hurting you. Self-Righteousness. I treat you badly because you deserve it. It's the right thing to do. Habits and Addictions Instant Rewards. My habit is pleasurable. Why give it up? Entitlement. I shouldn't have to change. Narcissism. I'm special. I deserve this donut (or drink). Denial. I don't have a problem! Conflict Phobia. I'd rather get high than face the problems that are bothering me.
Truth. I'm right and you're wrong. Blame. Our problems are all your fault, so why should I have to change? Pride. I can't stand the humiliation of examining my own role in the problem. Entitlement. I deserve better treatment. I shouldn't have to work so hard to solve the problems in our relationship. Fear. Something bad will happen if I try to get close to you. You might hurt me or make me look bad. It's safer to keep you at a distance. Hopelessness. You're such a stubborn, self-centered jerk that nothing could possibly work. Why should I bother to try?
Habits and Addictions Deprivation. Giving up my habit will be painful and uncomfortable. Ugh! Who wants that? Hopelessness. I've tried over and over but nothing works, so why get my hopes up? I'll just end up feeling frustrated and disappointed again.
* Copyright © 2005 by David D. Burns, M.D. Do not copy or distribute without written permission.
Addiction / Habit Log* Tempting Situation or Event:
Emotions
% Before
% After
Emotions
Tempted, excited
Inferior, worthless, inadequate, defective, incompetent
Stressed, exhausted, overwhelmed, burdened
Lonely, unloved, unwanted, rejected, alone, abandoned
Bored, uninterested, turned off
Embarrassed, foolish, humiliated, self-conscious, shy
Sad, blue, depressed, down, unhappy
Hopeless, discouraged, pessimistic, despairing
Anxious, worried, panicky, nervous, frightened
Frustrated, stuck, thwarted, defeated
Guilty, remorseful, bad, ashamed
Angry, mad, resentful, annoyed, irritated, upset, furious
Other (describe)
Other (describe)
Tempting Thoughts
% Before
% After
Distortions
Self-Control Thoughts
1.
1.
2.
2.
3.
3.
* Copyright 2001 by David D. Burns, M.D. Adapted for Addictions and Habits. Revised, 2006.
% Before
% After
% Belief
Addiction / Habit Log (cont'd) Tempting Thoughts
% Before
% After
Distortions
Self-Control Thoughts
4.
4.
5.
5.
6.
6.
% Belief
Checklist of Positive Distortions that Trigger Habits and Addictions* 1. 2. 3.
4. 5.
All-or-nothing thinking. You think of everything that you've been putting off and tell yourself how overwhelming all those tasks will be. Overgeneralization. When you slip up, you tell yourself that you've blown your diet completely and that you'll never lose weight so you might as well give up. Mental Filter. You dwell on the positives, like how good dessert will taste, and ignore the negative consequences, like feeling guilty or bloated afterwards. Discounting the Positive. You tell yourself that any little thing you do today would only be a drop in the bucket. Jumping to Conclusions. You jump to conclusions not warranted by the facts. Mind-Reading: You may assume that other people don't have to struggle with temptations, or that people who do abstain have drab, unfulfilling lives. Fortune-Telling: You tell yourself that if you take that drink, you'll feel great and all your problems will disappear. Or, you may tell yourself, "I'll just have one drink" or "one bite," but you've never stopped at just one drink or bite in the past.
6.
Magnification or Minimization. You blow things out of proportion: "This ice cream will taste so good!" 7. Emotional Reasoning. You tell yourself, "I'll clean my desk (or start my diet) when I'm more in the mood. I just don't feel like it right now." 8. Should Statements. You tell yourself, "I've had a hard day. I deserve a drink (or a nice dish of ice cream)." After you give in, you tell yourself, "I really shouldn't have slipped up." This makes you so guilty and anxious that you eat or drink even more. 9. Labeling. When you slip up, you tell yourself, "I'm such a fat pig." Then you get so upset that you decide to eat three more donuts. 10. Self-Blame and Other-Blame. You find fault with yourself, other people, or the world. Self-blame: You blame yourself for giving in to temptation. This makes you feel angry, frustrated, and guilty. Other-blame: You may tell yourself that you have "fat genes" or that it's unfair that you have to struggle with your weight. You insist that others can eat whatever they want and still be thin, so you should be able to do the same thing.
* Copyright 2001 by David D. Burns, M.D. Adapted for Addictions and Habits. Revised, 2006.
Decision-Making Form Option
Describe
A
Drop out permanently
B
Take a leave of absence Advantages of Option A
Total Points +5 +75 Disadvantages of Option A
1. No stress.
1. I'll lose 8 years of work.
2. More free time for dancing, painting and music.
2. My burned-out feelings may be temporary.
3. I can get away from my boss and coworkers.
4. May lose scientific career.
3. School loans to repay. 5. My parents will be disappointed.
4. More certainty. 9 110
1
2
70
30
10 105
5 40
75 7
6 60
25 8
130 11
70
30
3
4
55 12
1. I'll feel less stress.
1. I might not return to school.
2. I'll feel rejuvenated.
2. I'll still have loans to repay.
3. I'll have more free time.
3. I may get sick of having too much free time.
4. I'll keep my options open.
4. Might not be welcomed back. 5. My parents will still be disappointed. Advantages of Option B
Disadvantages of Option B
Decision-Making Form Option
Describe
Total Points
A
Get engaged
+20
B
Break up
+30
Advantages of Option A 1. 2. 3. 4.
Let go of my ambivalence. Move to the next stage of my life. I care very very deeply about Rasheed. Rasheed is a great person to marry and have kids with. 5. I know Rasheed, so most of the surprises are out of the closet after 4 years. 6. I don't have to start over with someone else. 7. I can start a family sooner. 8. Easier decision, require little to know deviation off current path. 9. Spend m more time with friends who have kids. 1 9 10. Have kids while my friends' kids are still the same age. 95 60 11. Give my Mom grandkids. 12. Stop the 'tick tick' fear. 13. House in Arizona. 5 35
1. Get to fall in love again. 6 65 2. Explore other men I've been interested in, one in particular. 3. Life becomes full of 130 65 unknowns again. This 11 seems exciting. 3 4. I can move to a new city. 5. I can take a shot at finding someone I feel more compatible with. 6. More excitement. 7. Not settling for what doesn't feel right. 8. Meet Mr. Right. 9. Find a person I'm more compatible with across the board.
Advantages of Option B
Disadvantages of Option A 1. I know exactly where life is going, and it's not too exciting. 2. I have to fit into Rasheed's life. (I once was OK with this.) 3. I am not sure he's "the one." 4. I might miss out on dating the right guy. 5. Not sure if we can make it work long term. I feel 70% sure we would end up divorced…yikes! 6. I'm not excited about getting engaged. 7. I can’t seem to squelch my desire to date someone else. 2 40
10 75
35 7
65 8
35 4
100 12
1. I'll have to get to know someone all over again. 2. Could get depressed. 3. May regret my decision. 4. Hurt Rasheed. 5. Hard to do. 6. Lose house in Arizona.
7. Losing best friend. 8. I spent a good deal of time getting to know Rasheed. To a certain extent, this was a waste. 9. Not sure I'm making the right decision. Will I regret this big time in 3 months? 10. Ambiguity. 11. Life becomes full of unknowns again, which can be scary. 12. Dealing with "Did I make a mistake here?" 13. I'm getting older. This means prolonging starting a family for at least 2-3 years.
Disadvantages of Option B
Decision-Making Form Option
Describe
Total Points
A B Advantages of Option A
9
Disadvantages of Option A
1
2
10
5
7
6
8
11
Advantages of Option B
3
4
12
Disadvantages of Option B
(See instructions on reverse)
Brief Instructions for Decision-Making Form Make a list of all your options and choose the best two. Call them Option A and Option B, and write them at the top of the Decision-Making Form. Then list all the advantages and disadvantages for both options in the appropriate columns. Option A: Cover the bottom half of the sheet and think exclusively about Option A. Compare the advantages and disadvantages. Which seem greater? Put two numbers that total 100 in circles 1 and 2. Take objective facts as well as subjective feelings into account. Sometimes one strong advantage may outweigh many weak disadvantages, or vice versa. If the advantages and disadvantages seem about the same, put a 50 in each circle. Option B: Cover the top half of the sheet so you can think exclusively about Option B. Repeat the procedure you used for Option A. Put two numbers that total 100 in circles 3 and 4. Advantages Comparison: Cover the right half of the sheet so you can compare the advantages of Options A and B. Ignore the disadvantages of each option. Put two numbers totaling 100 in circles 5 and 6. The option with the more desirable list of advantages gets the higher number. Disadvantages Comparison: Cover the left half of the sheet and concentrate on the disadvantages of Options A and B. Ignore the advantages. Put two numbers totaling 100 in circles 7 and 8. Assign the higher number to the disadvantages that seem worse. Calculations Advantages of Option A: The numbers in circles 1 and 5 are the advantages of Option A. Add these two numbers, and put the total in circle 9. Disadvantages of Option A: The numbers in circles 2 and 7 are the disadvantages of Option A. Add these two numbers, and put the total in circle 10. Total for Option A: Subtract the number in circle 10 from the number in circle 9. It could be a negative or positive number. Record this number at the top of the page under Total Points for Option A. Advantages of Option B: The numbers in circles 3 and 6 represent the advantages of Option B. Add them together, and put the total in circle 11. Disadvantages of Option B: The numbers in circles 4 and 8 are the disadvantages of Option B. Add them together, and put the total in circle 12. Total for Option B: Subtract the number in circle 12 from the number in circle 11. Record this number at the top of the page under Total Points for Option B. It could be a negative or positive number. Making the Decision Compare the total points for Option A and Option B. The option with the more positive number is more desirable. If one number is strongly positive and the other is negative, your decision is a "No Brainer." If both numbers are positive, this is a "Can't Lose" decision. Sometimes no single "correct" decision exists. In this situation, it's often better to make any decision and keep moving forward with your life. If, on the other hand, both numbers are negative, it's a "Can't Win" decision. This often results from depression. You may be viewing both options in a distorted, negative fashion. There may also be a more desirable third option you haven't considered. A variety of other interesting patterns may also emerge. Remember that when you use the Decision-Making Form, you don't have to feel trapped or locked in by the results. You can fill it out on several occasions until you feel comfortable with your decision.
Paradoxical Agenda Setting / Burns
Page 1
Paradoxical Agenda Setting—13 Basic Concepts and Techniques By David D. Burns, M.D.* 1. Empathy You’ll have to empathize without trying to help at the start of every therapy session, before you begin Agenda Setting. In addition, once you begin Agenda Setting, the patient might begin resist or may feel upset, angry, or overwhelmed with emotion at any time. Your best initial response will nearly always be empathy, using the Five Secrets of Effective Communication: The Disarming Technique, Thought and Feeling Empathy, Inquiry, I Feel Statements, and Stroking. Once the patient feels accepted and relax, you can go back to Agenda Setting, starting with the Invitation Step. 2. The Invitation Although the Invitation is the first step in Agenda Setting, it’s a useful motivational tool you can use at any time. It's simply some version of, "Is this problem (with your husband, your depression, your OCD, your drinking, etc.) something you'd like help with? Or did you simply want me to understand how painful this has been for you?" 3. Dangling the Carrot When you’re offering to help a patient, you can indicate optimism about what might happen if the two of you work together as a team. The way you express this will depend on your own personality, experience, and level of training, but you must offer patients something tangible if you’re asking them to work hard and engage in the therapeutic process. For example, when I’m working with a shy patient, I might say something like this: “Jim, I’d love to help you with your shyness so you can start dating and find someone to love. I’d also enjoy helping you with your public speaking. I also used to struggle with both of these problems, and now I talk to people everywhere I go, and I make my living doing public speaking around the US. Would you be interested in working on your shyness and public speaking anxiety?” 4. Sitting with Open Hands Sitting with Open Hands means that although you’re eager to help your patient, if she or he wants to change, you don’t need to help him or her. If you try to help patients who haven’t asked for help with, you’ll often run into a wall of resistance. Many therapists struggle with the idea of Sitting with Open Hands. They feel the need to jump in, trying this or that helpful technique they’ve learned about. This often results from an intense need to rescue patients and can be an expression of narcissism or codependency. Sitting with Open Hands means that we’re not experts in how people should think, feel or behave. We're not trying to sell patients on some model of ideal mental health. The patient is the boss, and we’re simply contractors. Patients have to tell us what they want help with, and how much the solution would be worth to them. When patients don’t want help, we can open our hands and let go. 5. Paradoxical Inquiry (PI) This can be helpful for Outcome and Process Resistance. When the patient resists, you can ask a paradoxical question that may lead the patient to the illogic of their resistance, rather than using * Copyright © 2010 by David D. Burns, M.D. Do not reproduce without written permission.
Paradoxical Agenda Setting / Burns
Page 2
persuasion in an attempt to change the patient's mind. For example, the patient whose describing a conflict with his brother may say, “Why should I have to change? He’s the one who’s screwed up.” Using PI you might say, “Certainly, you don’t have to change. Are you saying that you don’t want to?” PI questions must be delivered with warmth and respect. Tone of voice can make a huge difference. Avoid sarcasm. Try to see the world through the patient’s eyes, accepting the fact that she or he may not want to change, or may not want to risk changing. Your tone of voice will depend on whether you’re truly “sitting with open hands.” If your secret agenda is persuading the patient to change, then these methods will be ineffective. 6. Magic Button This is a wonderful tool for Outcome Resistance. You tell the patient to imagine there’s a Magic Button on the desk. If they push it, all their symptoms will suddenly and totally disappear with no effort at all. Most patients will say yes. Then you can point out all the reasons NOT to press the button. If you do this skillfully, the patient will often try to talk you out of them. This requires a familiarity with the most common sources of Outcome Resistance for depression, anxiety, relationship problems, and addictions, which are summarized in tables I’ve prepared for you. However, in most cases, the resistance will be somewhat unique to each patient, so you’ll have to think creatively and individualize the Magic Button for each person you work with. 7. Acid Test Most patients will immediately agree to push the Magic Button. It sounds great to have all of your negative feelings suddenly vanish, just by pushing a button. However, the patient hasn’t yet grasped what we’re really offering. We’re offering to help patients feel happy and fulfilled in spite of their problems and shortcomings. We can’t change the facts of any patient’s life in today’s session. We can only help the patient develop greater happiness and self-esteem in spite of those facts. When you do the Acid Test, you make the patient suddenly aware of the implications of pressing the Magic Button. For example, let’s say you’re treating a college freshman who was raised in Hong Kong. She’s severely depressed because she’s way behind in her studies, and she’s and procrastinating and lying around in bed instead of attending classes, taking careful notes, and studying hard. She feels lonely, ashamed, and frustrated, and constantly criticizes herself. She graduated at the top of her high school class, and her father expects her to major in electrical engineering and take over his computer chip company in Hong Kong some day. She’s perfectionistic and she’s not living up to his expectations or her own. So she says she’d gladly press the Magic Button and walk out of today’s session feeling joy and selfesteem. Then you can say, “But keep in mind that when you press the Magic Button, your feelings will change dramatically, but the facts of your life won’t change. You’ll STILL be way behind in your studies and you’ll STILL be getting Bs and Cs instead of As, but you’ll no longer be feeling depressed and worthless. Is that what you want, to be a happy mediocre student?” That’s the Acid Test. She might say “yes.” This will probably mean that she’s ready to go to work. She already understands that her relentless self-criticisms won’t help her catch up in her studies, and may even make things worse. But she’ll probably say “No! That sounds terrible. I don’t want to be happy unless I’m really doing well in my studies.” Then you might say something like this: “I think you might be telling me that you WANT to feel miserable today, as a way of punishing yourself, or motivating yourself. And it seems like you’re already doing a pretty good job of punishing yourself. So perhaps that’s not something you need help with.”
Paradoxical Agenda Setting / Burns
Page 3
Now you’ve placed her in a paradox. You can help her escape from the trap she’s fallen into with a little psycho-education, or with the Magic Dial. Like all powerful tools, this one takes practice, and must be done with genuineness and warmth or it will backfire. 8. Magic Dial This is another useful tool to melt away Outcome Resistance. When you fill out the Daily Mood Log, you ask patients to circle and rate all their negative feelings, such as inferiority, guilt, anxiety, or anger, on a scale from 0% (not at all) to 100% (the worst). Typically, these ratings will be in the range of 75% to 100%. You can point out that in many cases, negative feelings can be healthy and helpful. For example, if you’re trying to prepare for an important exam, some anxiety might motivate you to study harder. But 100% may be more than you need, and may even paralyze you. If you had a Magic Dial and could adjust your feelings to the ideal levels, what would those levels be? For example, 20% anxiety might be enough. You can both record the ideal levels (or “goals”) on the Emotions table of the Daily Mood Log. Now you have a therapy goal that won’t threaten the patient. Paradoxically, once the negative feelings start to decrease as you use techniques like the Externalization of Voices and Acceptance Paradox, the feelings will frequently drop all the way to 0%. 9. Fallback Position This is related to the concept of Sitting with Open Hands. What will you do if the patient is not ready, willing, or able to pick up and use the tools she or he needs to recover? For example, a depressed patient might be unwillingness to do psychotherapy homework (HW), or a shy, anxious patient might be unwilling to use exposure techniques until he feels more confident. This is where your “Fallback Position” comes into play. Your Fallback Position is how you make patients accountable. There are at several approaches. First, you can tell your patient that you really want to work with her, and would love to show her how to overcome the depression or crippling shyness that’s been making her life so miserable, and you feel convinced that the two of you could probably achieve those goals if you worked together. But the tools you use will not be effective without doing psychotherapy HW between sessions, such as the Daily Mood Log or Pleasure Predicting Sheet, or exposure techniques for anxiety. You could suggest that the patient might want to seek treatment for a local therapist who does not require psychotherapy HW or exposure, while at the same time emphasizing that you like her and definitely want to work with her. . . but the HW and exposure would not be negotiable. This approach is especially powerful at the initial evaluation, before you have accepted the person for treatment. The second approach may be more suitable for student therapists who have less therapeutic autonomy, as well as for clinicians who have already accepted unmotivated and resistant patients into treatment. You could say something along these lines, "I'd really love to help you with your depression, but the tools I use are not likely to be effective without the psychotherapy HW. Perhaps there’s some other problem we could work on instead." 10. Gentle Ultimatum The previous example illustrates the Gentle Ultimatum. You say, in a kindly way, “If you want me to help you with this problem, here’s what I’ll require of you. If my suggestion does not appeal to you, I can accept that. But then we’ll have to move in some new and different direction together. If you want to work with me, perhaps we could work on some other problem instead. Or, if you want help with your depression (or anxiety, or addiction, etc.) without doing the work I’m describing, perhaps a different therapist would be more suitable for you. You could point out that most therapists in the community offer long-term talk therapy without
Paradoxical Agenda Setting / Burns
Page 4
psychotherapy HW for patients with depression (anxiety, overeating, or troubled marriages.) If they feel strongly that they’re looking for that approach, you feel they have every right to pursue it—but you don’t have those kinds of skills. And while you would hate to lose them, and hope they’ll decide to work with you, they should know that the HW (or exposure, etc.) requirement would not be negotiable. You can also express the ultimatum in an apologetic way, like this: “Harold, I’d really like to help you with the PTSD, and I can see how much you’ve been suffering. But at the same time, I’m aware that recovery will require us to see a technique called Cognitive Flooding, where you to focus vividly on some of the horrible events from the past and allow yourself to feel flooded with intense anxiety, which can be tremendously uncomfortable. I’d hate to ask you to do that, but I realize that it would be absolutely necessary to defeat the horrible flashbacks that have been plaguing you. What do you think about that?” 11. Devil's Advocate Technique This is a Role-Playing Technique. Let’s say you’re working with a patient who is struggling with some habit or addiction, such as drinking too much, overeating, procrastinating, or dating the wrong person. You can ask your patient to describe a situation where she feels tempted and typically gives in to the temptation. For example, she may be struggling unsuccessfully to stick with a diet, and one extremely difficult situation might be walking through malls where fast food is sold, such as cinnamon buns. Ask her to list the tempting thoughts and list them yourself at the same time. For example: Gee, those cinnamon buns really smell terrific. They just came out of the oven, and they’d taste SO GOOD. Mmm! I’ll just go take a closer look. I really deserve one because I’ve had a tough day. I can just eat one tiny little bite. One little bite won’t hurt. I can have a salad later on so it won’t make any difference. I’m not getting anywhere in my diet anyway. I just CAN’T control myself, no matter how hard I try. Tomorrow will be a better day for dieting. Now tell her to imagine being in a mall and smelling the sweet smell of sticky cinnamon buns. Explain that you’ll play the role of the Devil and try to tempt the patient. You’ll be the voice in her mind that tries to trick her into giving in. She can play the role of the strong, self-loving, voice that resists the temptation. The Devil (initially played by the therapist) will use the second person, “You,” and the resisting voice (initially the patient) will speak in the first person, “I.” For example, as the Devil, you might say, "Gee, why don't you get one of those hot, buttery cinnamon buns? They just came out of the oven. It would taste SO GOOD, and you deserve it!" The patient might fight back and say, "I don't need a cinnamon bun, and I'll feel terrible if I give in. I'm determined to stick with my diet, and I'm looking forward to wearing more attractive clothes. I may deserve a sticky bun, but I also deserve some dignity and self-esteem." Now, as the Devil, try to tempt her with another seductive thought, giving her another chance to fight back again. Continue until the patient has convincingly defeated all the positive, tempting thoughts. If it seems clear that the patient has gotten stuck, and cannot effectively defeat one of the tempting thoughts, you can use role-reversals to model more effective responses. Alternatively, you can become
Paradoxical Agenda Setting / Burns
Page 5
the voice of the patient’s subconscious resistance, and ask, with genuine curiosity, why the patient wants to change, giving all the benefits and rewards of the habit or addiction. You can use the Devil’s Advocate Technique for patients who feel tempted by habits such as drinking, using drugs, procrastinating, dating the wrong person, having affairs, or internet pornography. This method can be surprisingly powerful, especially if you express the tempting thoughts in a seductive and convincing manner. If patients cannot defeat the Devil, the likelihood of successful treatment may be low, so the Devil’s Advocate Technique also becomes an innovative and dynamic assessment tool. 12. Straightforward / Paradoxical Cost-Benefit Analysis (CBA) Ask the patient to list the advantages and disadvantages of a Negative Thought (“I’m such a loser”), SelfDefeating Belief (“I should be perfect”) on a CBA form. You can also do a CBA for a negative feeling (like anger, guilt, inferiority or anxiety), habit (such as drinking, using drugs, overeating or procrastinating) or relationship problem (such as blaming your spouse for your marital problems). In each case, you can ask the patient, "What are the advantages and disadvantages of this belief, feeling or habit? How will it help you, and how will it hurt you?" After the patient lists all the advantages and disadvantages, ask him to balance them against each other on a 100-point scale so he can see whether the costs or the benefits or that mind-set are greater. When you do a Paradoxical CBA, you have the patient list only the advantages of a negative thought, belief, feeling, habit, or relationship problem, such as blaming your spouse or sibling for all the problems in your relationship. Now ask the patient, "Given all these advantages, why should you change?" This will make you and your patient aware of the powerful forces that keep you stuck, and will help you avoid trying to persuade a reluctant patient. Instead, the patient has to persuade you to work with him or her. 13. Externalization of Resistance When you do a Cost-Benefit Analysis, you can list all the reasons for the patient to maintain the status quo and resist change in the Advantages column. Then you can become the voice of the patient’s subconscious resistance, and verbalize all those reasons, using the second-person, “You.” For example, consider the college freshman from Hong Kong who was beating up on herself for doing poorly in her classes. With your help, she might be able to list advantages of self-criticism, depression, and shame such as these: 1. My self-criticisms show that I have a good value system and won’t let myself off the hook. 2. They show that I love my parents and honor them. 3. They may motivate me to study harder and get caught up. 4. If I’m severely depressed and ashamed, others won’t feel the need to criticize me. 5. My self-criticisms show a high degree of integrity, since I’m facing my shortcomings instead of denying them. Together, you can probably come up with even more advantages. After explaining the procedure to your patient, you can take the role of her resistance, and verbalize all the reasons NOT to change, one at a time, using the second-person, “You.” For example, you might say, “Your depression shows how much you love your parents,” or “If you feel happy, you may lose your motivation to study,” or “If you feel happy, you’ll be settling for mediocrity,” etc. Then see if she can defeat you, speaking in the first-person, “I.” If she CAN defeat you, she’ll be well along the road to recovery, although other techniques will also be needed. If she cannot defeat you, she may be saying she WANTS to remain depressed. In this case you can “sit with open hands,” and ask her if there’s something she does want help with.
The Five Steps in Agenda Setting* By David D. Burns, M.D. 1.
The Invitation. At the beginning of each session, patients need the chance to tell you how they've been feeling. After you've listened for a while, you can ask if they're ready to roll up their sleeves and get to work on the problems that are bothering them, or if they need you to listen for a while longer. This conveys the idea that listening alone won't be sufficient, and that active effort will be required if they really want to change their lives.
2.
Specificity. If the patient accepts the invitation, ask them what problem they'd like to work on first. They may want help with depression, anxiety, a marital conflict, or a bad habit. Then ask them to describe one specific moment when they were struggling with that problem. For example, can they tell you about a time when they were feeling depressed, anxious, or angry with their spouse? It could be anything, but the problem must be specific as to: Person. Who were they with? What was going on? Place. Where were they? Time. What time of day was it? Vague complaints, like "I need better self-esteem," "Life stinks," or "I think I'm codependent," won't work. The problem must be real, and it must be something that the patient wants help with.
3.
Conceptualization. Once the patient describes the problem, ask yourself what type of problem it is. Is it: An individual mood problem, such as anxiety or depression? A relationship problem, such as anger or a conflict with a family member, friend, or colleague? A habit or addiction, such as an eating disorder, drug or alcohol abuse, smoking, or procrastination? A non-problem, such as healthy sadness or grief, where no therapeutic techniques other than empathic listening are required? Some problems will fall into more than one category. For example, a woman may be depressed because of a problem in her marriage. Or, a man may be struggling with shyness and substance abuse.
4.
Motivation. Does the patient really want to get better, or does he simply want to talk about the problem while you listen? How hard will he work to solve the problem, if you agree to help him with it? How many sessions is he willing to spend on it? Will he do homework assignments between sessions? Your conceptualization of the problem will help you predict the most likely forms of resistance you're likely to run into. Depression, anxiety, anger and addictions are all associated with unique forms of Process Resistance and Outcome Resistance. Together, you and the patient can think about all the reasons why he may not want to change (Outcome Resistance) or why he may not want to do what it's going to take to get better (Process Resistance). Then you can let him try to persuade that he really does want to change, even though there are many good reasons to maintain the status quo.
5.
Methods. Depression, anxiety, anger and addictions all respond to different kinds of techniques. The techniques you use will depend on the way you conceptualize the problem.
* Copyright © 2005 by David D. Burns, M.D. Do not copy or distribute without written permission.
Other – Order Forms, reading list • • • • • •••• • • •• ••• • ••••• • •• ••• •• • •• • ••• • •• • •• • ••• • •• ••• • ••• • • • •• • • •• • • •• • • ••• • • • • • ••• •
Therapist's Toolkit and EASY Diagnostic System
Page 1
What’s the Therapist's Toolkit? By David D. Burns, M.D.
The Therapist's Toolkit includes hundreds of pages of state-of-the-art assessment and treatment tools for the mental health professional. A partial list can be found on the accompanying order form. Why purchase the Therapist's Toolkit? Many popular tests for common disorders such as depression must be purchased for approximately $1 per copy, or more. If you have a busy practice or clinic, royalty fees can run into the thousands of dollars per year—and you own nothing at the end of the year. In contrast, when you obtain the Therapist's Toolkit, you become licensed to reproduce large numbers of testing and treatment tools in your clinical practice for your entire career, so you will not have to pay royalties each time you administer a psychological test. Multi-user site licenses are also available for group practices and institutions, providing additional savings. How do these tools compare with other instruments? Many widely used assessment tests for depression, anxiety, and other disorders were created decades ago. Often, they are not user-friendly and do not have outstanding psychometric properties. The wording is frequently unclear and the response options may be frustrating as well. Sometimes, the symptom choices are inappropriate. In contrast, the instruments in the Therapist's Toolkit are exceptionally user-friendly for the clinician and patient alike, and have superb psychometric properties. Most have reliabilities above 90%, with many above 95%, and are highly correlated with other, well-established instruments. The Toolkit also includes large numbers of incredibly useful treatment tools that will enhance your work with individuals and groups, regardless of your therapeutic orientation.
What’s the EASY Diagnostic System? As mental health professionals, we have a medical / legal obligation to screen all new patients systematically and accurately for a broad range of Axis I and II disorders, to assign the diagnoses according to DSM-IV criteria, and to record the diagnoses in the chart. But everyone knows that this is virtually impossible from a practical perspective. For example, one of the most widely used structured diagnostic interviews for Axis I and II disorders can take up to three or four hours, or more. In addition, structured interviews can be exceptionally frustrating due to the dichotomous, non-intuitive nature of the DSM-IV diagnostic criteria. And the diagnoses may not be reliable due to the subjective nature of the criteria and the arbitrary cut-off points described in DSM-IV for the various “disorders.” As a result, most therapists simply ignore the diagnosis step and scribble some plausible diagnosis in the chart, such as “Adjustment Disorder with depression.” Sometimes you can get away with this, but you may set yourself up for legal or clinical problems down the road if you don’t do a comprehensive diagnostic assessment and document your findings in the chart. For example, patients with Axis II diagnoses, such as Borderline, Narcissistic, or Paranoid PD, may be clinically challenging or litigious, and many patients may have violent or suicidal urges you are not aware of, to say nothing of the predictable clinical problems associated with undiagnosed alcohol or drug abuse, or the patient’s hidden desires to maintain symptoms in order to obtain disability or win a lawsuit. What’s the solution to this problem? Over the past ten years, I have been developing, refining, and validating the EASY Diagnostic System for Axis I and Axis II. Patients can complete the Diagnostic Survey on (Continue on reverse)
Therapist's Toolkit and EASY Diagnostic System
Page 2
their own at home between sessions or in the waiting room. Most patients can easily complete the survey in 30 to 45 minutes, or less. Then you can quickly review the answers during a therapy session and tick off the pre-coded diagnoses on the Diagnostic Summary Sheet in one of three categories: Unlikely, Possible, or Probable. In addition, you will automatically document the severity of the symptoms, since all disorders are assessed with highly reliable, dimensional scales. This diagnostic system is comprehensive, quick and easy, and will provide you with a wealth of interesting and vitally important information, much of which you would not otherwise be aware of. The Diagnostic Survey includes highly reliable screening instruments for 67 of the most common Axis I and II disorders, including— All the relational Disorders: plus Anger Toward Self, Anger Toward Others, Violent Urges, and the powerful Relationship Satisfaction Scale Mood Disorders: Major Depression, Suicidal Urges, Dysthymic Disorder, Bipolar I and II Disorder, Cyclothymic Disorder Anxiety Disorders: GAD, Panic, Agoraphobia, Phobias, five types of Social Anxiety, OCD Stress and Trauma-Related Disorders: Adjustment Disorder, Acute Stress Disorder, PTSD Somatic Disorders: Body Dysmorphic Disorder, Hypochondriasis, Chronic Pain Disorder Habits and Addictions: Gambling, Drug Abuse / Dependence, Alcohol Abuse / Dependence, plus the new Cravings and Urges to Use scale Eating Disorders: Binge Eating Disorder, Bulimia (Purging and Restricting types), Anorexia Dissociative Disorders and Schizophrenia All 10 Axis II Personality Disorders: including Clusters A, B, and C by specific disorder You’ll also find a number of interesting subscales. For example, the screening for Dependent PD includes subscales for Neediness, Conflict Phobia, and the Fear of Being Alone. The Diagnostic Survey includes a superb motivational assessment instrument and screening for suicidal and violent urges, along with an assessment of the patient’s honesty and openness in filling out the survey. You’ll also receive EASY Diagnostic Guidebook with tips on how to assign diagnoses according to formal DSM-IV criteria, along with a table listing the reliabilities of all the screening instruments, and other useful tools such as the Suicidal Urges Screening Interview. You'll love the Therapist’s Toolkit and EASY Diagnostic System, and you can't beat the price. These tools will professionalize your practice, enhance your understanding of your patients, and boost your clinical effectiveness. Purchase of either includes a lifetime license for unlimited photocopying to use in your clinical work. No royalty fees! Additional details and pricing information can be found on the order forms. To request order forms for the Therapist’s Toolkit or EASY Diagnostic System, send an email to: [email protected]. Thank you!
The Therapist's Toolkit and EASY Diagnostic System are designed for qualified mental health professionals only.
Reading List / Burns
Page 1
Question 1. Are Antidepressant Medications More Effective Than Placebos? Do True Antidepressant Medications Exist? Antonuccio, D.O., Danton, W.G., & DeNelsky, G.Y. (1995). Psychotherapy versus medication for depression: Challenging the conventional wisdom with data. Professional Psychology: Research and Practice, 26, 574 - 585. Antonuccio, D.O., Burns, D., Danton, W.G., & O’Donohue, W. (2000). The Rumble in Reno: The psychosocial perspective on depression. Psychiatric Times, 17, 10-13. Web link: http://www.mhsource.com/pt/p000824.html Antonuccio, D.O., Burns, D., & Danton, W.G. (2002). Antidepressants: A triumph of marketing over science? Prevention and Treatment, 5, Article 25. Web link: http://journals.apa.org/prevention/volume5/toc-jul15-02.htm Antonuccio, D.O., Danton, W.G., DeNelsky, G.Y., Greenberg, R., & Gordon, J.S. (1999). Raising questions about antidepressants. Psychotherapy and Psychosomatics, 68, 3-14. Hypericum depression trial study group. (2002). Effect of Hypericum perforatum (St. John’s wort) in major depressive disorder: A randomized, controlled trial. Journal of the American Medical Association, 287, 1807-14. You can read a summary online at: http://www.nih.gov/news/pr/apr2002/nccam-09.htm. A full text of this article is available at: http://www.jama.com Kirsch, I. & Sapirstein, G. (1998). Listening to Prozac but Hearing Placebo: A Meta-Analysis of Antidepressant Medication. Prevention and Treatment, 1, Article 0002a. Web link: http://journals.apa.org/prevention/volume1/pre0010002a.html Kirsch, I., Moore, T. J., Scoboria, A., & Nicholls, S. S. (2002). The Emperor's New Drugs: An Analysis of Antidepressant Medication Data Submitted to the U.S. Food and Drug Administration. Prevention and Treatment, 5:23. Web link: http://journals.apa.org/prevention/volume5/pre0050023a.html The following web link will bring you to the index for Volume 5 of Prevention and Treatment, including commentaries on the lead article about antidepressants versus placebos: http://journals.apa.org/prevention/volume5/toc-jul15-02.htm Question 2. Do Antidepressants Increase the Risk of Suicide in Adolescents and Adults? Garland, E. J. (2004). Facing the evidence: antidepressant treatment in children and adolescents. Canadian Medical Association Journal, 170, 489-491.
Reading List / Burns
Page 2
Healy, D. (2003). Lines of evidence on the risk of suicide with selective serotonin reuptake inhibitors. Psychotherapy and Psychosomatics. 72, 71-79. Jureidini, N., Doecke, C.J., Mansfield, P.R., Haby, M.M., Menkes, D.B., & Tonkin, A.L. (2004) Efficacy and safety of antidepressants in children and adolescents, British Medical Journal, 328, 879-883. Khan A, Khan SR, Leventhal RM, Brown WA (2001). Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: a replication analysis of the Food and Drug Administration Database. International Journal of Neuropsychopharmacology, 4, 113-118. Khan, A., Warner, H. A., & Brown, W. A. (2000). Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: An analysis of the Food and Drug Administration database. Archives of General Psychiatry 57, 311-317. Whittington, C.J., Kendall, T., Fonagy, P., Cottrell, D, Cotgrove, A, & Boddington, E. (2004). Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. The Lancet, 363, 1341-1345. Question 3. What's the Most Effective Treatment for Anxiety Disorders? Westra, H. A., & Stewart, S. H. (1998). Cognitive behavioral therapy and pharmacotherapy: Complementary or contradictory approaches to the treatment of anxiety? Clinical Psychology Review, 18 (3), 307-340. Question 4. CBT for Depression: How Effective Is It? Antonuccio, D.O., Danton, W.G., & DeNelsky, G.Y. (1995). Psychotherapy versus medication for depression: Challenging the conventional wisdom with data. Professional Psychology: Research and Practice, 26, 574 - 585. DeRubeis, R. J., Hollon, S. D. Amsterdam, J. D., Shelton, R. C., Young, P. R., Salomon, R. M., O’Reardon, J. P., Lovett, M. L., Gladis, M. M., Brown, L. L., & Gallop, R. (2005). Cognitive Therapy vs Medications in the Treatment of Moderate to Severe Depression. Archives of General Psychiatry, 62: 409-416. Web abstract: http://archpsyc.ama-assn.org/cgi/content/abstract/62/4/409 Dobson, K.S. (1989). A meta-analysis of the efficacy of cognitive therapy for depression. Journal of Consulting and Clinical Psychology, 57(3), 414 - 419.
Reading List / Burns
Page 3
Hollon, S.D., & Beck, A.T. (1994). Cognitive and cognitive behavioral therapies. Chapter 10 in A. E. Bergin & S. L. Garfield (Eds.), Handbook of Psychotherapy and Behavioral Change (pp. 428 - 466). New York: John Wiley & Sons, Inc. Hollon, S. D., DeRubeis, R. J., Shelton, R. C., Amsterdam, J. D., Salomon, R. M., O’Reardon, J. P., Lovett, Young, P. R., Haman, K. L., Freeman, B. B., & Gallop, R. (2005). Prevention of Relapse Following Cognitive Therapy vs Medications in Moderate to Severe Depression. Archives of General Psychiatry, 62: 417-422. Web abstract: http://archpsyc.ama-assn.org/cgi/content/abstract/62/4/417 Brief summary with interview in Medical News Today on Friday, July 8, 2005: Cognitive therapy as good as antidepressants, effects last longer. Web link: http://www.medicalnewstoday.com/medicalnews.php?newsid=22319# Robinson, L.A., Berman, J.S., & Neimeyer, R.A. (1990). Psychotherapy for the treatment of depression: A comprehensive review of controlled outcome research. Psychological Bulletin, 108, 30 - 49. Question 5. Does Therapeutic Empathy Make a Difference? Burns, D. D., & Nolen-Hoeksema, S. (1992). Therapeutic empathy and recovery from depression in cognitive-behavioral therapy: A structural equation model. Journal of Consulting and Clinical Psychology, 60(3), 441 - 449. Burns, D. D., & Auerbach, A. (1996). Therapeutic Empathy in CognitiveBehavioral Therapy: Does it Really Make a Difference? Chapter 7 in Frontiers of Cognitive Therapy (P. Salkovskis, ed.) New York: Guilford Press, pp. 135 164. Krupnick, J. L. et al. (1993). The role of the therapeutic alliance in psychotherapy and psychotherapy outcome: Findings in the NIMG treatment of depression collaborative research program. Journal of Consulting and Clinical Psychology, 64(3), 636 - 643. Orlinsky, D. E., Grawe, K., & Parks, B. K. (1995). Process and outcome in psychotherapy--Noch einmal. Chapter 8 in A. E. Bergin & S. L. Garfield (Eds.), Handbook of Psychotherapy and Behavioral Change (pp. 270 - 376). New York: John Wiley & Sons, Inc. Persons, J. B., & Burns, D. D. (1985). Mechanism of action of cognitive therapy: Relative contribution of technical and interpersonal intervention. Cognitive Therapy and Research, 9(5), 539 - 551.
Reading List / Burns
Page 4
Question 6. Is Psychotherapy Homework Important? Burns, D.D. and Nolen-Hoeksema, S. (1991). Coping styles, homework compliance and the effectiveness of cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology, 59(2), 305 - 311. Burns, D.D., & Spangler, D. (2000). Does psychotherapy homework lead to improvements in depression in cognitive behavioral therapy? Or does improvement lead to increased homework compliance? Journal of Consulting and Clinical Psychology, 68(1), 46 - 59. Persons, J.B., Burns, D.D., & Perloff, J.M. (1988). Predictors of dropout and outcome in cognitive therapy for depression in a private practice setting. Cognitive Therapy and Research, 12, 557 - 575. Question 7. What's Bibliotherapy? Does it really help? Ackerson, J., Scogin, F., Lyman, R.D., & Smith, N. (1998). Cognitive bibliotherapy for mild and moderate adolescent depressive symptomatology. Journal of Consulting and Clinical Psychology, 66, 685-690. Jamison, C., and Scogin, F. (1995). Outcome of cognitive bibliotherapy with depressed adults. Journal of Consulting and Clinical Psychology, 63, 644 650. Norcross, J. C., Santrock, J. W., Campbell, L. F., Smith, T. P., Sommer, R., & Zuckerman, E. L. (2003). Authoritative Guide to Self-Help Resources in Mental Health, Revised Edition. New York: Guilford Press. Santrock, J. W., Minnett, A. M., & Campbell, B. D. (1994). The Authoritative Guide to Self - Help Books. New York: Guilford Press. Scogin, F., Hamblin, D., and Beutler, L. (1987). Bibliotherapy for depressed older adults: A self-help alternative. The Gerontologist, 27, 383 - 387 Scogin, F., Jamison, C., and Davis, N. (1990). A two-year follow-up of the effects of bibliotherapy for depressed older adults. Journal of Consulting and Clinical Psychology, 58, 665 - 667. Scogin, F., Jamison, C., Floyd, M., & Chaplin, W. (1998). Measuring learning in depression treatment: A cognitive bibliotherapy test. Cognitive Therapy and Research, 22, 475-482. Scogin, F., Jamison, C., and Gochneaut, K. (1989). The comparative efficacy of cognitive and behavioral bibliotherapy for mildly and moderately depressed older adults. Journal of Consulting and Clinical Psychology, 57, 403 - 407.
Reading List / Burns
Page 5
Smith, N. M., Floyd, M. R., Jamison, C., and Scogin, F. (1997). Three-year follow-up of bibliotherapy for depression. Journal of Consulting and Clinical Psychology, 65(2), 324 - 327. Question 8. Other Challenges to Biological Psychiatry You can find the following books online at Amazon.com and other sources: Breggin, P. C. (2001). The Anti-Depressant Fact Book: What Your Doctor Won't Tell You About Prozac, Zoloft, Paxil, Celexa, and Luvox. Cambridge, MA: Perseus Books. Eaton T. Fores Research Center Against Psychiatry. (2003). "There Are No "Chemical Imbalances." Web link: http://www.etfrc.com/ChemicalImbalances.htm Healey, D. (1991). Let them eat Prozac. Toronto: James Lorimer & Co. Valenstein, E. (2002). Blaming the Brain: The Truth About Drugs and Mental Health. New York: The Free Press. Whitaker, R. (2001). "Not So Atypical." Chapter 11 in Mad in America: Bad Science, Bad Medicine, and the Enduring Mistreatment of the Mentally Ill. Cambridge, MA: Perseus Press.
Tools for Supervision and Teaching
Workshop Evaluation Date:
Discipline: Agree Strongly
1. Overall, I was satisfied with the workshop. 2. The program was clear, understandable and well organized. 3. The handouts and overheads enhanced the program. 4. The facility was comfortable and pleasant. 5. The program was a valuable educational experience. 6. The program will be helpful in my professional work. 7. What did you like the least about the program?
8. What did you like the best about the program?
9. General comments:
Agree
Neutral
Disagree Disagree Strongly
Teaching Evaluation Your Name:
Date: Agree Strongly
Agree
Neutral
1. Overall, I was satisfied with today's seminar. 2. The seminar was a valuable educational experience. 3. The information was interesting and clearly presented. 4. The information will be helpful in my professional work. What did you like the least about the seminar?
What did you like the best about the seminar?
Other comments:
(Use reverse if you need more space)
Disagree
Disagree Strongly
Your Name:
Date:
Name of Instructor(s): Instructor Rating Scale* Instructions. Use checks () to indicate how strongly you agree with each statement about your most recent class. Please answer all the items. Positive Feelings about the Instructor 1. The instructor was friendly and supportive. 2. The instructor welcomed questions from the students. 3. The instructor kept me engaged and interested. 4. Overall, I was satisfied with this class. Negative Feelings during Class 5. Sometimes I felt uncomfortable or anxious during the class. 6. Sometimes I felt defensive or insecure during the class. 7. Sometimes I felt frustrated during the class. 8. Sometimes I felt confused during the class. Helpfulness of the Class 9. I expect to use these ideas in my clinical work. 10. What I learned in this class was useful. 11. The class was helpful to me. Difficulties with the Questionnaire 12. It was hard to be completely honest answering some questions. 13. My answers weren’t always completely honest. 14. Sometimes I did not answer the way I really felt inside. Please describe what you specifically disliked about the class? What could have been improved? Were there some things you disagreed with or did not understand?
Please describe what you specifically liked about the class? What was the most helpful? Were there some things you learned?
Use the reverse for any additional comments or suggestions you may have. * Copyright © 2010 by David D. Burns and Jacob Towery. Adapted from Burns’ Supervision Rating Scale.
Your Name: ________________________________ Today's Date: _____________ Name of Teacher or Supervisor: _________________________________________
Supervision Rating Scale* Instructions. Use checks () to indicate how strongly you agree with each statement about your most recent supervision session. Please answer all the items. Positive Feelings about the Supervision 1. I felt I could trust my supervisor. 2. My supervisor paid careful attention to what I said. 3. My supervisor critiqued my work in a sensitive manner. 4. I felt good about the supervision I received. 5. Overall, I was satisfied with my most recent supervision session. Negative Feelings during Supervision 6. Sometimes I felt uncomfortable during the supervision. 7. Sometimes I felt defensive during the supervision. 8. Sometimes I felt frustrated during the supervision. 9. Sometimes I felt anxious during the supervision. 10. Sometimes I felt insecure during the supervision. Helpfulness of the Supervision 11. I expect to use these ideas with patients I am now treating. 12. What I am learning seems useful in my clinical training. 13. My supervisor and I are working together effectively. 14. The supervision was helpful to me. 15. I felt I was learning and growing during the supervision session. Difficulties with the Questionnaire 16. It was hard to be completely honest answering some questions. 17. My answers weren’t always completely honest. 18. Sometimes I did not answer the way I really felt inside. Please describe what you specifically disliked about the supervision? What could have been improved? Were there some things you disagreed with or did not understand?
Please describe what you specifically liked about the supervision? What was the most helpful? Were there some things you learned?
*
Copyright 2009 by David D. Burns, M.D.
Your Name: ________________________________ Today's Date: ____________
Supervision Rating Scale* Instructions. Use checks () to indicate how strongly you agree with each statement about your most recent supervision session. Please answer all the items. Positive Feelings about the Supervision 1. I felt I could trust my supervisor. 2. My supervisor was warm and supportive. 3. My supervisor seemed eager to help. 4. My supervisor treated me with respect. 5. My supervisor paid careful attention to what I said. 6. My supervisor critiqued my work in a sensitive manner. 7. My supervisor seemed genuine. 8. I felt good about the supervision I received. 9. Overall, I was satisfied with my most recent supervision session. Negative Feelings during Supervision 10. Sometimes I felt criticized during the supervision. 11. Sometimes I felt intimidated during the supervision. 12. Sometimes I felt judged during the supervision. 13. Sometimes I felt uncomfortable during the supervision. 14. Sometimes I felt defensive during the supervision. 15. Sometimes I felt misunderstood during the supervision. 16. Sometimes I felt frustrated during the supervision. 17. Sometimes I felt anxious during the supervision. 18. Sometimes I felt insecure during the supervision. 19. Sometimes I felt inadequate during the supervision. Helpfulness of the Supervision 20. I was able to discuss problems important in my clinical work. 21. I received useful feedback about the individuals I am treating. 22. The approach my supervisor used made sense to me. 23. I expect to use these ideas with patients I am now treating. 24. We used the supervision time effectively. 25. What I am learning seems useful in my clinical training. 26. My supervisor and I are working together effectively. 27. The supervision was helpful to me. 28. I felt I was learning and growing during the supervision session.
*
Copyright 1998 by David D. Burns, M.D., Henny Westra, Ph.D., & Rachel Young, Ph.D. Do not reproduce without written permission.
Supervision Rating Scale* (cont'd)
Instructions. Use checks () to indicate how strongly you agree with each statement about your most recent supervision session. Please answer all the items. Difficulties with the Questionnaire 29. Sometimes I felt awkward when I answered the questions. 30. I felt uncomfortable when I answered some of the questions. 31. It was hard to be completely honest answering some questions. 32. My answers weren’t always completely honest. 33. Sometimes I did not answer the way I really felt inside. 34. Sometimes I wasn’t completely open. 35. It would be hard for me to criticize my supervisor. Please describe what you specifically disliked about the supervision? What could have been improved? Were there some things you disagreed with or did not understand?
Please describe what you specifically liked about the supervision? What was the most helpful? Were there some things you learned?
Please describe any ideas that might improve this scale or the teaching. THANK YOU!
**
Copyright 1998 by David D. Burns, M.D., Henny Westra, Ph.D., & Rachel Young, Ph.D. Do not reproduce without written permission.
Tools in Foreign Languages • • •• • •• • • •••• • • • • • ••• •
Registre de mes humeurs quotidiennes Feuille supplémentaire* % Croyance avant
Pensées négatives
*
% Croyance après
Distorsions
Pensées positives
Copyright 1984 by David D. Burns, M.D. Revised 2004.
% Croyance
Analyse coût bénéfice d’une relation* Instructions: Faites une liste de tous les avantages et désavantages de blâmer l’autre personne pour les problèmes de la relation. Puis balancer les avantages et les désavantages sur une échelle de 100 points. Placez deux nombres qui reflètent votre évaluation dans les cercles au bas de la page. Par exemple, si les avantages de blâmer semblent significativement supérieurs, vous pourriez placez 70% dans le cercle à la gauche et 30% dans le cercle à la droite. Si les désavantages vous semblent un peu plus grands, vous pourriez mettre 45% dans le cercle de gauche et 55% dans le cercle de droite. Avantages de blâmer
Désavantages de blâmer
Analyse Coût—Bénéfice* Énoncez l’attitude, le sentiment ou l’habitude que vous désirez changer:
Avantages
Désavantages
To: Dr. David Burns, M.D. From Dr. Anne Parent, Ph.D., C. Psych. & Dr. Yvonne Labelle, Ph.D., C. Psych. Re: French translation of several Therapist’s Toolkit instruments Following your workshop in Ottawa, Canada last December, I had offered to translate some of your material in French. Dr. Parent and I have been working on translating some of the tools from your current toolkit so we can extend the use of these valuable instruments to a French-speaking clientele. The following instruments (and their translated titles) have been selected for this translation: Evaluation of Therapy Session – Évaluation de la session de thérapie Brief Mood Survey (past week) – Inventaire bref de l’humeur (semaine) Brief Mood Survey (at this moment) – Inventaire bref de l’humeur (à ce moment-ci) Daily Mood Log – Registre de mes humeurs quotidiennes Daily Mood Log – continuation sheets – Registre de mes humeurs quotidiennes -feuille supplémentaire * Relationship Cost Benefit analysis – Analyse coût bénéfice (générale) Relationship Cost Benefit analysis (relationship) – Analyse coût bénéfice (relation) Relationship Cost Benefit analysis (habit) – Analyse coût bénéfice (habitude) Decision-making Form – Formule de prise de décision As we are registered psychologists and not translators, we approached it by recognizing the diversity of spoken French throughout the world. As with any language, demographic features and education level can contribute to the particular expressions used. Dr. Parent and I come from two different provinces in Canada and live in a third one and, in addition, we have lengthy experience working with French-speaking clients. It is hoped that this background will render these tools maximally useful to other clients whose mother tongue is French. Your book “Feeling Good”, already translated in French, served as a background for some of the instruments. We hope that the French versions can extend the usefulness of your tools for a wider client base. Respectfully, Dr. Yvonne Labelle Dr. Anne Parent
* We restricted the sheet to seven events since French translations often give a lengthier text.
Date:
Empathie thérapeutique
3---Beaucoup
Veuillez bien répondre à tous les items.
1---Quelque peu vrai 2---Modérément
Instructions. Servez-vous de crochets () pour décrire vos sentiments reliés à votre session de thérapie la plus récente.
0—Pas du tout
Évaluation de la session de thérapie*
4--Complètement
Nom:
1. Mon thérapeute me semblait chaleureux, intéressé et prêt à me donne du support. 2. Mon thérapeute m’inspirait confiance. 3. Mon thérapeute me démontrait du respect. 4. Mon thérapeute m’écoutait bien. 5. Mon thérapeute saisissait bien mon sentiment.
L’aide apportée par la session 6. 7. 8. 9. 10.
J’ai pu exprimer mes sentiments pendant la session. J’ai pu parler des problèmes qui me tracassent. Les suggestions apportées étaient aidantes. L’approche utilisée par mon thérapeute était compréhensible. J’ai appris de nouvelles façons pour transiger avec mes problèmes.
Satisfaction avec la session d’aujourd’hui 11. J’ai trouvé la session utile. 12. Dans l’ensemble, j’étais satisfait de la session d’aujourd’hui.
Votre engagement 13. Je projette de faire le travail thérapeutique avant ma prochaine session. 14. J’ai l’intention d’utiliser ce que j’ai appris au cours de la session.
Sentiments négatifs ressentis lors de la session 15. À certains moments, mon thérapeute ne semblait pas comprendre ce que je ressentais. 16. À certains moments, je me sentais inconfortable. 17. Je n’étais pas toujours d’accord avec mon thérapeute.
Difficultés ressenties avec les questions de cette évaluation 18. Il m’était difficile de répondre honnêtement à certaines des questions ci-haut. 19. Parfois, mes réponses ne reflétaient pas ce que je ressentais vraiment. 20. Il me serait trop dérangeant de critiquer mon thérapeute.
Ce que vous avez le moins aimé de la session :
Ce que vous avez le plus aimé de la session:
*Copyright David D. Burns, M.D. 2001; Version française 2005 Y.Labelle, Ph.D., C. Psych. , A.Parent, Ph.D., C. Psych.
4—Extrèmement
Dépression 1. 2. 3. 4. 5.
3---Beaucoup
Instructions. Servez-vous de crochets () pour décrire vos sentiments à ce moment-ci. Lorsqu’il s’agit des questions se rapportant aux impulsions suicidaires ou violentes, indiquer comment vous vous êtes senti récemment. Veuillez répondre à tous les items.
2—Modérément
Inventaire bref de l’humeur*
1—Quelque peu
Date:
0---Pas du tout
Nom:
Triste ou ayant le cafard Découragé ou sans espoir Faible estime de soi Sans valeur ou inadéquat Perte de plaisir ou de satisfaction dans la vie Total
Impulsions suicidaires 1. Avez-vous des pensées suicidaires? 2. Aimeriez-vous mettre fin à votre vie? Total
Anxiété 1. Anxieux 2. Effrayé/Épeuré 3. Inquiet de beaucoup de choses 4. Tendu(e) ou à bout 5. Nerveux Total
Colère 1. 2. 3. 4. 5.
Frustré Agacé ou contrarié Rancunier Fâché ou en colère Irrité Total
Impulsions violentes 1. Je pense ou j’imagine blesser autrui. 2. J’ai envie de blesser ou d’être violent. Total
1. 2. 3. 4. 5.
Communication et ouverture Savoir résoudre les conflits et arguments Niveau d’affection et de soin Intimité et rapprochement Satisfaction en général Total
* Copyright
1997 by David D. Burns, M.D. Revised, 2002.
6—Beaucoup
4—Quelque peu
3—Au neutre
Satisfait 2—Quelque peu
1—Modérément
Veuillez bien répondre à tous les items.
0—Beaucoup
Instructions. Servez-vous de crochets () pour exprimer votre satisfaction à l’intérieur de votre relation la plus proche.
Insatisfait
5—Modérément
Satisfaction dans une relation*
Dépression 1. 2. 3. 4. 5.
4— Extrèmement
Veuillez répondre à tous les items.
3---Beaucoup
Instructions. Servez-vous de crochets () pour décrire vos sentiments au cours de la dernière semaine, y compris aujourd’hui.
2—Modérément
Inventaire bref de l’humeur*
1—Quelque peu
Date: 0---Pas du tout
Nom:
Triste ou ayant le cafard Découragé ou sans espoir Faible estime de soi Sans valeur ou inadéquat Perte de plaisir ou de satisfaction dans la vie Total
Impulsions suicidaires 1. Avez-vous des pensées suicidaires? 2. Aimeriez-vous mettre fin à votre vie? Total
Anxiété 1. Anxieux 2. Effrayé/Épeuré 3. Inquiet de beaucoup de choses 4. Tendu(e) ou à bout 5. Nerveux Total
Colère 1. 2. 3. 4. 5.
Frustré Agacé ou contrarié Rancunier Fâché ou en colère Irrité Total
Impulsions violentes 1. Je pense ou j’imagine blesser autrui. 2. J’ai envie de blesser ou d’être violent. Total
1. 2. 3. 4. 5.
Communication et ouverture Savoir résoudre les conflits et arguments Niveau d’affection et de soin Intimité et rapprochement Satisfaction en général Total
6—Beaucoup
4—Quelque peu
3—Au neutre
Satisfait 2—Quelque peu
1—Modérément
Veuillez bien répondre à tous les items.
0—Beaucoup
Instructions. Servez-vous de crochets () pour exprimer votre satisfaction à l’intérieur de votre relation la plus proche.
Insatisfait
5—Modérément
Satisfaction dans une relation*
Registre de mes humeurs quotidiennes* Situation ou incident: % Avant
Emotions
% Après
Emotions
Triste, cafardeux, déprimé, en peine, malheureux
Sans espoir, découragé, pessimiste, désespéré
Anxieux, inquiet, en panique, nerveux, effrayé
Frustré, coincé, contrarié, vaincu
Coupable, plein de remords, mauvais, honteux
En colère,fâché,rancunier,agacé,irrité,bouleversé,furieux
Inférieur,sans valeur, inadéquat,défectueux, incompétent
Autre (décrire)
Solitaire, pas aimé, pas désiré, rejeté, seul, abandonné
Autre
Embarrassé, idiot, humilié, gêné
Autre
Pensées négatives
% Croyance avant
% Croyance après
Distorsions
Pensées positives
1.
1.
2.
2.
3.
3.
4.
4.
% Avant
% Après
% Croyance
Registre de mes humeurs quotidiennes, Feuille supplémentaire % Croyance avant
Pensées négatives
% Croyance après
Distorsions
Pensées positives
5.
5.
6.
6.
7.
7.
% Croyance
Liste de contrôle des distorsions cognitives * 1.
Mode de pensée Tout-ou-rien. Vous voyez les choses de façon absolue, en blanc ou noir.
6.
Exagération ou Minimisation. Vous gonflez les choses hors proportions ou vous les réduisez.
2.
Sur généralisation. Vous interprétez un seul incident négatif comme une suite sans fin de défaites.
7.
Résonnement émotif. Vous résonnez à partir de vos émotions: “Je me sens idiot, donc je dois être un idiot.”
3.
Filtre mental. Vous vous étendez sur le négatif et vous ignorez le positif
8.
Énoncés de devoir. Vous employez des “devrait,” “ne devrait pas,” “doit,” “aurait dû,” et “ obligé de.”
4.
Ne pas tenir compte du positif. Vous insistez sur le fait que vos qualités positives sont sans valeurs
9.
Etiquetage. Au lieu de vous dire “J’ai fait une erreur,” vous vous dites, “je suis un imbécile” ou “Je suis un perdant.”
5.
Sauter aux conclusions. Vous sautez à des conclusions non justifiées par les faits. --Lire dans les pensées. Vous présumez que les autres réagissent négativement à vous --Prédire l’avenir. Vous prédisez une tournure négative des évènements.
10. Se blâmer ou blâmer les autres. --Se blâmer. Vous vous blâmer pour une chose sans en être entièrement responsable. --Blâmer les autres. Vous blâmez les autres et fermez les yeux sur la façon dont vous avez contribué au problème.
*
Copyright 1984 by David D. Burns, M.D. Revised 2004.
Опросник депрессии Бернса* Пожалуйста укажите, поставив галочку в одной из граф в каждой строке, насколько перечисленные чувства беспокоили Вас в последние несколько дней. 0
1
2
3
4
совсем
нет
немного
средне
сильно
1. Печаль: Чувствуете ли Вы себя грустным(ой) или как в воду опущенным(ой)? 2. Обескураженность: Представляется ли Вам будущее безнадежным? 3. Низкая самооценка: Чувствуете ли Вы себя бесполезным(ой)? 4. Неполноценность: Чувствуете ли Вы себя неполноценно по отношению к другим? 5. Вина: Вините ли и критикуете ли Вы себя? 6. Нерешительность: Трудно ли Вам принимать решения? 7. Раздражительность: Часто ли Вы чувствуете себя разозленным(ой) или возмущенным(ой)? 8. Утеря интереса к жизни: Утратили ли Вы интерес к работе, увлечениям, семье или друзьям? 9. Снижение мотивации: Приходится ли Вам понастоящему заставлять себя, чтобы что-то сделать? 10. Образ себя: Чувствуете ли Вы себя старым(ой) и непривлекательным(ой)? 11. Перемены в аппетите: У Вас пропал аппетит? Переедаете ли Вы или едите постоянно? 12. Сон: Трудно ли Вам хорошо выспаться ночью? Чувствуете ли Вы себя чрезвычайно усталым(ой) и слишком много спите? 13. Утрата сексуального влечения: Утратили ли Вы интерес к сексу? 14. Озабоченность здоровьем: Вы постоянно обеспокоены своим здоровьем? 15. Порывы к самоубийству: Вас посещают мысли, что жить не стоит и лучше бы Вам умереть?
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
* Copyright 1997 by David D. Burns, M.D. Revised, 2002.
4 сильно
3 средне
2 немного
1 нет
Пожалуйста укажите, поставив галочку в одной из граф в каждой строке, насколько перечисленные чувства беспокоили Вас в последние несколько дней. Категория I.Тревожные чувства 1. Тревога, нервозность, беспокойство или страх. 2. Ощущение отчужденности или нереальностиокружающего. 3. Чувство отсоединенности от Вашего тела или его частей. 4. Внезапные и непредвиденные приступы паники. 5. Неприятное предчувствие или ощущение надвигающегося несчастья. 6. Ощущение скованности, напряженности или на грани срыва. Категория II. Тревожные мысли. 7. Трудно сконцентрироваться. 8. Мысли скачут. 9. Пугающие фантазии или мечты. 10. Чувство, что вы на грани потери контроля. 11. Страх, что Вы сходите с ума. 12. Страх, что Вы потеряете сознание и упадете в обморок. 13. Cтрахи, что Вы серьезно больны, что у Вас инфаркт, или что Вы умираете. 14. Опасения, что Вы выглядите странно или глупо. 15. Страх остаться одному(ой), забытому(ой) или брошенному(ой). 16. Страх критики или неодобрения со стороны окружающих. 17. Страх, что сейчас произойдет что-то ужасное. Категория III. Физические показатели. 18. Учащенное или сильное сердцебиение. 19. Боль, тяжесть или сдавленность в груди. 20. Покалывание или онемение пальцев рук или ног. 21. Неприятные ощущения в желудке. 22. Запор или понос. 23. Беспокойство, вздрагиваете от каждого шороха. 24. Ощущение, что Ваши мышцы напряжены. 25. Ощущение, что Вас бросает в пот, хотя вокруг не жарко. 26. Ощущение кома в горле. 27. Вы дрожите или Вас трясет. 28. Ощущение, что ноги как ватные. 29. Ощущение головокружения или потери баланса. 30. Трудно дышать, задыхаетесь. 31. Головные боли или боли в спине и шее. 32. Чувство, что Вас бросает то в жар, то в холод. 33. Чувство усталости, слабости или быстрое утомление.
0 совсем
Опросник тревожности Бернса*
PRELIMINARY VALIDATION OF THE BURNS DEPRESSION CHECKLIST AND THE BURNS ANXIETY INVENTORY WITH A RUSSIAN POPULATION Natalia Skritskaia, Hofstra University and Don Beal, Eastern Kentucky University Depression and anxiety are two of the most common problems among individuals seeking mental health services in the United States and worldwide as well. Indeed, the World Health Organization has estimated that about 340 million people in the world are affected by mood disorder at any given time and about 400 million people are affected by anxiety disorder (World Health Organization, 1997). For this reason, valid and reliable brief self-report measures of depression and anxiety for use with English speaking and non-English speaking individuals are of critical importance. The purpose of the present study is to begin the process of developing two brief self-report measures, one for depression and one for anxiety for use with Russian speaking individuals. It should be emphasized that this research project is meant to serve as a beginning study in a larger programmatic effort to develop valid and reliable versions of the Russian versions on of the Burns Depression Checklist (Burns-D) and the Burns Anxiety Inventory (Burns-A). Method One method of developing valid scales is to start from scratch, and develop a scale within the population for which the scales are to be utilized. Another valid approach is to translate an already existing instrument into the language of choice. This approach has been used with a number of already existing instruments such as the Beck Scales and the Stait-Trait Anxiety scales. The initial step in the process of developing the Russian versions of the Burns-D and the Burns-A was to translate the instruments into Russian using a highly competent bilingual professional. Then to administer both sets of scales to a group of Russian immigrants and sojourners. The rationale was that if the individuals scored similarly on both the English and the Russian versions of the Scale, then this would offer some support for the validity of the scale. Participants: Participants consisted of 30 Russian immigrants and sojourners living in the southeastern United States. These individuals were mainly university students attending the University of Kentucky and Eastern Kentucky University. The order of administration of the instruments was varied to avoid order effects. Results and Discussion It was found that the English version of the Burns-D correlated significantly with the Russian version of the Burns-D. The correlation was highly significant (p