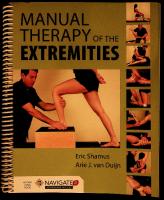
Manual Therapy of the Extremities 9781284036701, 1284036707, 9781284036718, 1284036715, 9781284083309, 1284083306, 9781284083316, 1284083314
With OCR
189 81 128MB
English Pages xvii, 352 pages : [192] Year 2017
image00345
image00350
image00351
image00352
image00353
image00354
image00355
image00356
image00357
image00358
image00359
image00360
image00361
image00362
image00363
image00364
image00365
image00366
image00367
image00368
image00369
image00370
image00371
image00372
image00373
image00374
image00375
image00376
image00377
image00378
image00379
image00380
image00381
image00382
image00383
image00384
image00385
image00386
image00387
image00388
image00389
image00390
image00391
image00392
image00393
image00394
image00395
image00396
image00397
image00398
image00399
image00400
image00401
image00402
image00403
image00404
image00405
image00406
image00407
image00408
image00409
image00410
image00411
image00412
image00413
image00414
image00415
image00416
image00417
image00418
image00419
image00420
image00421
image00422
image00423
image00424
image00425
image00426
image00427
image00428
image00429
image00430
image00431
image00432
image00433
image00434
image00435
image00436
image00437
image00438
image00439
image00440
image00441
image00442
image00443
image00444
image00445
image00446
image00447
image00448
image00449
image00450
image00451
image00452
image00453
image00454
image00455
image00456
image00457
image00458
image00459
image00460
image00461
image00462
image00463
image00464
image00465
image00466
image00467
image00468
image00469
image00470
image00471
image00472
image00473
image00474
image00475
image00476
image00477
image00478
image00479
image00480
image00481
image00482
image00483
image00484
image00485
image00486
image00487
image00488
image00489
image00490
image00491
image00492
image00493
image00494
image00495
image00496
image00497
image00498
image00499
image00500
image00501
image00502
image00503
image00504
image00505
image00506
image00507
image00508
image00509
image00510
image00511
image00512
image00513
image00514
image00515
image00516
image00517
image00518
image00519
image00520
image00521
image00522
image00523
image00524
image00525
image00526
image00527
image00528
image00529
image00530
image00531
image00532
image00533
image00534
image00535
image00536
image00537
image00538
image00539
image00540
Recommend Papers
- Author / Uploaded
- Eric Shamus
- Arie J Van Duijn
File loading please wait...
Citation preview
CY ADVANTAGE
ACCESS
Navigate 2 provides access to mobile-ready course materials that |
our
Learn. Practice. Assess. Analyze. Engage!
wew.ibleaming.com, bookstores, and retailers everywhere.
REQUIRED
will change the way you learn and access your course content.
—
fos a
=
d : oO
rr
my
: Oe
Ee
) |
Learn. Read your digital textbook online or offline, enhance your learning with
|
interactive tools, and make personal notes. The eBook provides a personal, interactive,
| |
and collaborative learning experience on computers, tablets, and mobile devices. .
-
———
7
aaa
ee
ry
pat udy
7c
-\q
Center
virtual study center. It is open during nights and weekends too!
=
a
-
fa ~
8
oar ai. . oneal =
34
—n
—
Assess. Evaluate your comprehension
of course materials in this homework and
testing center with quizzes and examinations.
ee
:
USES
Th
a
Analytics |
is
Analyze. se actionable data to determine
where to focus your study time and what ta review. It will also help you cance how to
prepare for assessments and which
tools to utilize.
learning
EE as eae
w
im¥ ElBf Fe = —.
i”
. .
za a
_
"
—w
fi. =)
oD
MM JONES & BARTLETT
‘AB: gp),
o
JONES & BARTLETT Fig
NAVIG ATE@
Jones & Bartlett Learning | 5 Wall Street | Burlin
gton, MA | 01803 phone: 1-800-832-0034 | fax: 978-443-8000 Wwe | blearnidg sees
a
— _ hae
c
Lal ic To) Mela aM
| a,
Subscription Length:
COURSE
MATERIALS
is
7
acer Tate 4
Mitie
365 days
TECHNICAL SUPPORT If you need help creating your account or technical support along the
way, please: . m Visit
SEsfae eh
@ Call Monday through Friday from 8:30 a.m. to 8:00 p.m. Eastern Standard Time at 1-978-443-5000
uw
6
S
www,jblea ng.com/techsuppo: t Email [email protected]
@
5 ore tt aaa 2 z=
3
_
“nas
MLEARN ING
nr
5 uw = a
ic
oe
Assessments
8
3 £
a)
4 a. _—_ 7 = —" ae x ;
ONLINE
:
3
Ja —
TO
=
2B Performing MET for more or fewer cycles than necessary to achieve improvements in
range of motion. Repeat the technique until there is no further relaxation of the muscle. The quality of the response usually peaks at the third cycle and will diminish thereafter if not necessary,”!
: Allowing the patient's move while the clinician
contraction, thereby not providing an “isometric” contraction but a concentric iso-
limb/lever is resisting
to the
tile cueing will assist in prevention of this problem. + The isometric contraction lasting less than 3 seconds or much longer than 5 seconds. Counting out loud to a patient may help prevent this. « The patient “pulsing” the contraction rather than maintaining a proper static contraction of the muscle. + The clinician moving to a new restrictive barrier too quickly after the isometric contraction. The restrictive barrier should not be further approached before the patient has completely finished the contraction.
| Mobilzction with Movement = 41 10
CHAPTER 1 Introduction
° ‘Once ‘the final isometric contraction’ has _ ber completed within the series of cycles, it is imperative that the clinician take the eal ver/limb. further toward the restrictive bar-
_ tier one last time prior to repositioning the lever/limb back to its neutral position. Reap‘proximating the barrier after the isometric © contraction is the most important
step in
“MET because it is what mobilizes the joint a further toward the restrictive barrier, restor-
_ ing the original range of motion of theSoy ‘muscle.
in this process that junction fires—which
when a neuromuscular occurs during a muscle
contraction—that the charge across the neuro-
muscular junction’s membrane becomes positive. At this time a “refractory period” is reached for a short period of time until the fluctuation of sodium and potassium in and out of the cell creates
a more
negative
environment
across
the membrane of the neuromuscular junction. During the refractory period the neuromuscular
junction is thought to be unable to be stimulated, i.e., the alpha and gamma motor neurons
Pay special attention to individuals with a
Indications for Muscle Energy Techniques
history of severe hypertension or recent cerebrovascular accident or myocardial -infarc-
MET can be applied to joints and muscles varying instances.
in
» To lengthen shortened, contractured, or spasmodic/strained myofascial tissues + To mobilize a joint with restricted mobility « To alter neural reflex relationships that main-
tain the muscle in a contracted state - When more invasive techniques are contraindicated, such as high-velocity low-amplitude techniques
will not be able to oppose a stretch of a muscle
‘Neurophysiological
Principles of Muscle Energy Techniques Post-isometric relaxation: The most common accepted theory of how MET has its effect on range of motion of joints and elongation of the myofascial structures is through a neurophysiological process called post-isometric relaxation. Fred Mitchell, Jr. explained the effects of MET on
the physiological
process
of action
poten-
tials across a neuromuscular junction.”” Before understanding post-isometric relaxation, it is _ important
to understand
the process
where
and
gamma
motor neuron
signals
that
would
generally oppose a stretch toward the barrier.
sition to the stretch via the alpha and gamma motor neurons, sending impulses
traction is initiated in an agonist muscle,
This reflex will always
occur unless
a neuro-
muscular junction is unable to be activated. This process indicates that during the stretching ofa muscle,
there will always
be some
oppo-
to the same
stretched muscle to contract in response to the stretch, potentially affecting the effectiveness of the stretch itself. The
process
of MET
is thought
to bypass
_ the alpha and gamma motor neuron impulses that occur when muscle spindles are activated
through
regular
muscle
stretching,
the process of post-isometric
through
relaxation.
It is
metric
pump
«
contractions.
microtorn
may
exacer-
Because
no movement
action.
Patients with suspected hemarthrosis. muscle contraction may exacerbate
of MET may
Any and
disrupt recent sutures or inter-
nal hardware placed in joints or bones. In addition, isometric contractions and breath holding inhibit venous return that is vital to the healing patients in this delicate state. MET may also precipitate internal bleeding
the restrictive barrier. However, this process is
are not sufficiently
isometric
contraction and
and precipitate negative effects. Patients with a wee deep venous thrombosis (DVT). Patients who are unwilling or unable to fol-
low verbal directions: e.g., young children, infants, or people with language barriers, hearing loss, or mental illness. Patients who have had suspected tendon avulsions from bone. The process of MET ing the tendon.
MET should be applied with caution to: Pregnant patients in their second trimester and beyond. Isometric contractions and breath holding will further reduce venous return and may exacerbate any lower extremity
edema
due
to
the
inferior
vena
cava already being compressed. + Osteoporotic patients where strong muscular contraction may avulse tendon and bone. MET is an excellent technique to use in the management of musculoskeletal joint restriction and muscle inflexibility that create pain. When
applied correctly, it can be quite effective
in improving range of motion, reducing muscle tone/spasm, reducing pain, and restoring proper joint function. The procedures of MET are phys-
iologically quite safe with applications to most clinical scenarios.
increase bleeds within joints.
allow further motion of the joint/limb/lever to
thought to occur only during a muscle contrac-
to recently or fasciae
« Post-surgical patients. The muscle activation
there
tion and the carryover effects of the antagonist
ligaments,
occurs across the joint interface, this situation does not lend itself well to removing metabolic waste and inflammatory metabolite buildup, which can occur with concentric isotonic contractions, i.e., through muscle
is a simultaneous and reflexive relaxation of that muscle’s antagonist group.” This would
inhibition post-contraction explained.
contraction
bate the inflammatory process and delay healing. In addition, inflamed muscles from an acute strain may not respond well to iso-
Golgi tendon organ reflex: The Golgi tendon organ is an inhibitory body found in the tendons sion threshold of a musculotendinous junction is reached. When it is activated, it exerts inhibitory effects on the alpha motor neurons of the musculotendinous junction, sending impulses to instruct the tendon to relax and reduce the tension in the region. Muscle fatigue theory: It is postulated that after a muscle undergoes several contract-relax cycles, it becomes fatigued allowing further stretching to the restrictive barrier without reflexive contraction of the opposing musculature.” Reciprocal inhibition: When a gentle con-
activation of the alpha and gamma motor neuTons occurs in response to this initial stretch.
« Acutely injured or painful muscles.' Further
Other Proposed Mechanisms of Muscle Energy Techniques of muscles. It is activated when the tendon ten-
muscle spindles are activated and a reflexive
MET is a contraindicated manipulative technique and should not be applied in the case of:
muscles,
a
are active when a muscle is in an active or contracted state. When muscles are stretched, the
Contraindications for Muscle Energy Techniques
muscle
muscle is maintained in a tight, spasmodic or strained state. Gamma and alpha motor neurons
because
may worsen this problem by further detach-
during this time.
It is through this process that, during a MET, specifically in the seconds following the isometric contraction of the muscle, the muscle/limb/ lever can be taken/stretched further toward the restrictive barrier without opposition of the alpha
tion
breath holding may increase blood pressure
»
in patients who have had any type of recent surgery. Patients who have undergone recent cardiac surgery or have complicated medical histories involving cardiac-related disease such as coronary artery disease or atherosclerosis.
Mobilization with Movement Mobilization manipulation
with Movement (MWM) is a technique that combines the
application of a sustained accessory joint glide with an active movement in the direction that is restricted.?”** The concept was first described by Mulligan,” with the underlying premise that slight changes in the position of the joint (“positional fault”) can lead to altered mechanics of movement leading to joint dysfunction. The following treatment concepts have been described for the application of MWM:7729.3°
~
Counterstrain Technique = «13
-
2
i
,
F
z CHAPTER Introduction
y
A specific joint dysfunction iis identified durhe patient evaluation. This dysfunction include loss of joint mobility and/or pain: with specific movements. . The passive accessory joint glide that accom-
+ S—Sustain/Skills/Sense: Sustaining of the joint glide throughout the motion is required.
The therapist needs to achieve sufficient skills in order to perform the technique appropriately and to sense patient response
throughout the application.
panies the dysfunctional movement is identi-
fied following the convex/concave rule. The application of the joint glide should be pain ea irees' The therapist investigates various combinations of parallel or perpendicular glides to find the correct treatment plane and grade of accessory movement. While the therapist sustains the accessory glide, the patient is requested to perform the dysfunctional movement, and a significant reduction in symptoms should be achieved. _ Mulligan describes PILL, an acronym for what needs to be achieved during the assess-
The
MWM
and/or painful
motion or activity is repeated by the patient while the therapist continues to maintain the appropriate accessory glide, and overpressure
is applied at end range in a pain-free manner. Mulligan also describes the CROCKS acronym for the successful techniques:*
application
of MWM
- C—Contraindications: the general contraindications for manual therapy. R—Repetitions: up to 3 sets of 10 repetitions for chronic conditions, 3 to 6 repetitions for
acute conditions,
MWM
to
reduce
musculoskeletal
3.
Diagnose the joint dysfunction limitation of movement that you intend to treat with MWM. Have the patient actively move to the barrier to the limitation of movements. The therapist performs an accessory glide
ate patient feedback
is required,
Immediespecially
in regard to pain during the application of MWM. K—Knowledge: The therapist needs to have sufficient knowledge of the anatomy and biomechanics to determine the appropriate treatment plane and accessory motions.
MWM can be applied to joints and muscles in varying instances. ¢
To lengthen shortened, contractured, or spasmodic/strained myofascial tissues that are restricting joint movement
+ To mobilize a joint with restricted mobility ¢ To alter neural reflex relationships that maintain the muscle in a contracted state
e When
more invasive techniques,
such as
high-velocity low-amplitude techniques, are contraindicated
Contraindications for MWM MWM is a contraindicated manipulative technique and should not be applied in the case of: «
Similar
contraindication
to muscle
energy
repetitions for acute conditions.
«
Times
where
the
overpressure
is not
pain
free
Errors in the
* Poor application of the direction of the accessory glide. » An inaccurate diagnosis. * Accessory glide is not sustained throughout the motion.
» The overpressure needs to be pain free.
Basic Concepts of MWM A basic concept of MWM is that there needs to be a combination of active contraction with the accessory glide to facilitate normal movement patterns and the neuromotor learning of the correct movement pattern. An example of movement with mobilization is when a patient has limited knee flexion. The
nervous
system.”
The first mechanism,
a muscular
imbalance
Theory,
resulting
from
abnormal muscle spindle activity. This increased muscle spindle activity results in a contraction of the agonist muscles, which in turn simulate the
antagonist spindles resulting in contraction of the agonist muscles, creating a neuromuscular imbalance around the joint. Application of the Counterstrain technique is purported to normalize the muscle spindle activity, thus reducing abnormal
muscle tone and improving function. The second
mechanism proposes that microcirculation in the
affected areas is restored following the placement of the muscle in a shortened position through the application of the Counterstrain technique, thus reversing ischemia and promoting the removal of metabolic waste products. Though limited evidence is present to substantiate either of these mechanisms,** a recent systematic review found low-level evidence that Counterstrain may reduce musculoskeletal pain.**
technique
Post-surgical patients where an active contraction is contraindicated
O—Overpressure: ‘is required to maintain the
gains in mobility over time. C—Communication/Cooperation:
Indications for MWM
°
Application of MWM
nomic
involves
throughout the motion. This is to be repeated for up to 3 sets of 10 repetitions for chronic conditions, 3 to 6
Common
neuromuscular activity resulting fora muscle spindles and abnormal circulation resulting in inflammatory reactions mediated by the autoalso referred to as the Proprioceptive
of MWM
4,
restricted
of
Basic Steps of the Application
and/or direction of the joint glide to evaluate previously
of
pain, mobility, and improved function.”*
2.
The
outcomes
is limited and consists primarily of case
tiveness
1.
if improvement occurs.
the
the evidence to date can be considered of low quality, there are trends that support the effec-
ment purposes: Pain-free movement and joint glide; Instant results should be present; Long Lasting results should be achieved.” needs to alter the treatment plane and grade
describing
reports and relatively small size RCTs. Although
‘ment in order to use the technique for treat-
_If improvement is not achieved, the therapist
literature
patient actively flexes the knee while the therapist performs a posterior tibial accessory glide. This facilitates the posterior motion of the concave surface on the convex surface.
1.
Counterstrain Technique Strain Counterstrain, or Counterstrain for short, is a common indirect manual technique used for the treatment of musculoskeletal pain, especially in conditions where tender points (TP) are present.*! Counterstrain, also known as positional
release technique,
was
first described
Basic Steps for the Application of the Counterstrain Technique
2.
by the
osteopathic physician Lawrence Jones, DO,
who
first described the presence of TPs. TPs are small areas (less than 1 cm) in muscles, tendons, fascia, and other types of soft tissues that are exquisitely
painful to palpation. These areas of tenderness are
often
which
in
manifested turn
may
in
hypertonic
influence
the
3.
muscles,
function
of
the joint structures that these muscles affect. To date, more than 200 TPs have been described. There are 2 proposed pathophysiological mechanisms underlying Counterstrain: abnormal
4.
Locate the tender point. Tender points are described as small zones of tense, tender, edematous muscle and fascial tissue less than 1 cm in diameter. The tender point will be used to monitor patient response during the application of the technique. The patient is placed in the position of comfort (POC), typically by shortening the tissues surrounding the TP. Typically the patient will report one specific position of maximum relief, and the therapist will feel relaxation of the TP tissues. The position of comfort is held for 90 seconds, during which time the patient remains completely relaxed and passive. The position is held for 120 seconds in areas that involve the ribs. The patient is passively, slowly returned to a neutral
position,
while
the
therapist
Myofascial ond Soft Tissue Manipulation = «15 HAPTER 1 introduction
_ monito thers TP to ensure that the tissue ‘at the TP remains relaxed. The patient —
Counterstrain is a contraindicated manipula-
is returned to the POC if abnormal tone
tive technique and should not be applied in the
returns atthe TP.
case of:
Ree
5. The therapist rechecks the tender point,
and a reduction of 70% of subjective pain and palpated tension is considered a suc-
cessful outcome?
i
7 Common Errors in the Application of Counterstrain + Inability to find the point of complete tissue - mobilization relaxation + Patient unable torelax —
+ Position not held for 90 seconds
_«
Contraindications for Counterstrain
The patient actively contracts when moving out of the position of relief
Basic Concepts of Counterstrain A basic concept of Counterstrain is that the tech-
nique is performed away from the barrier of restriction as an indirect technique. An exam-
ple of Counterstrain is when a patient has limited knee extension from a hypertonic hamstring (biceps femoris). The patient is prone with the
leg extended. The therapist palpates and finds the tender point. The therapist passively flexes the knee, rotates the tibia, and extends the hip
until the tender point is gone and no longer tender. The therapist maintains the position for 90 seconds. The therapist passively returns the leg to the extended position
and
rechecks the
tender point.
Indications for Counterstrain -Counterstrain can be applied to joints and muscles in varying instances. + To relax contractured or spasmodic/strained myofascial tissues that are restricting joint movement * To alter neural reflex relationships that maintain the muscle in a contracted state = When more invasive or direct techniques are
contraindicated, such acute muscle or soft tissue injuries
* e
Unstable fractures where all movement is contraindicated All movement that increases pain without a
point of relaxation
Myofascial and Soft Tissue
Regular — a
Manipulation There is a long history of the use of myofascial and soft tissue manipulation techniques in medicine, dating back to ancient eastern and Greek times. More contemporary forms of soft tissue treatment include Swedish massage, connective tissue mas-
\ SS
fr
Adipose
Reticular
Elastic}
Ss a
L
14
Irregular
} \,
Jae
}
sage (bindegewebsmassage) developed by the German physical therapist Elisabeth Dicke, Hoffa
FIGURE 1-9 Connective tissue types
massage, Myofascial Release (MFR), Rolfing, Alexander, Feldenkrais, and many others.** Whereas
arrangement of collagen fibers and the presence
the latter 2 approaches focus on the postural effects of soft tissue restrictions, other approaches can be classified as primarily using mechanical effects (Swedish massage, Rolfing, Structural Integration, Hoffa, MFR)
and others focus on the neurophys-
iological effects (connective tissue massage). In this text, the term myofascial manipulation refers to techniques that focus primarily on mobility of the fascial layers, whereas the term soft tissue manipulation encompasses techniques aimed at
other soft tissue structures.
of elastin and reticulin allows for significant deformation. Dense irregular connective tissue is found in joint capsules, aponeuroses, the dermis, and fascial sheets. The collagen fibers in dense irregular connective tissue are arranged in a multidirectional fashion, allowing for the absorption of multidirectional stresses. Tendons and ligaments are comprised of dense regular connective tissue. Collagen fibers in dense regular connective tissue are arranged in a parallel fashion, allowing for the absorption of unidirec-
Pathophysiology of
(see
.
The main cell type found in connective tissue is the fibroblast, which produces the components of the extracellular matrix. Fibroblasts may differentiate into specialized cells depending on the type of connective tissue. Other cells include macrophages, mast cells, plasma cells, lymphocytes, and melanocytes. The fibrillar component of the extracellular matrix consists of collagen
fibers and elastin fibers. Collagen fibers provide
tional stresses.*”*°
Anatomy and
Connective tissue consists of cells and the extracellular matrix. The extracellular matrix consists of fibrillar and interfibrillar components
Reticular fibers
Melaioscie
Elastic fibers
Connective Tissue Connective tissue is present in a wide variety
of anatomical tissues, and its structure can vary
Lymphocyte
significantly based on its specific function. Four different classes of connective tissue can be dis-
tinguished (see
Collagen fibers
;
Connective tissue proper can be classified as loose, dense irregular, and dense regular connective tissue. Loose connective tissue is found in superficial fascial sheaths, between the skin and
underlying tissues, in muscle and nerve sheaths and surrounding internal organs. The loose
Mast cell
FIGURE 1-10 Connective tissue
~ Myofesciat and Soft Tssue Manipulation
17°
CHAPTER1 Introduction.
| g . Fya eee
ERCwe ae=
2. Inflammation phase: Mast cell stimula-
tone are just as successful or more successful than techniques directed at the connective tissue of the fascia. ””
} _ Cartilage
tion results in vasodilation and release of
inflammatory mediators including cytok-
-Fiber-forming collagen eral
aaa
ines. Macrophages and neutrophils initiate debridement response. Typically lasts 24 to 48 hours.
Connective Tissue Response
ee
3.
to Injury and Immobilization The
foundational
work
of Akeson,
Amiel,
"Hyaluronic acid
e
Reduction in water content in the extracellu-
lar matrix « Reduction of PG content - Formation of cross-linking between collagen fibers and loss of critical interfiber distance
« +
FIGURE 1-11 Proteoglycan molecule the structural integrity of the connective tissue
_and are the most prevalent protein found in the body. A significant number of types of collagen have been
identified,
with
the primary
types
« Type I collagen: the most common collagen type, designed to withstand tensile forces. Found in tendons, ligaments, joint capsules,
_ bone, skin, fibrocartilage. Type II collagen: present in cartilage and nucleus pulposus of the intervertebral disc, designed to withstand compressive forces.
+ Type Ill collagen: found in muscle and tendon
sheaths,
skin, joint
capsule.
Type
III
collagen also found in healing connective tissue: after tissue damage, Type III collagen is first laid down
in a haphazard,
the water
content
of the
extracellular matrix. PGs consist of glycoaminoglycans (GAGs) attached to a core protein chain
(see TATE). Major
being:*”
-*
role in maintaining
types
of GAGs
include
chondroitin
(4 or 6) sulfate, keratin sulfate, and hyaluronan. The latter is not sulfated and can exist as a single GAG chain or can form complex PG complexes
called aggregans.* These large PGs bind water through the negatively charged GAG complexes and thus maintain the water content of the extracellular matrix. This water content is critical in maintaining normal relationships between the fibers in the extracellular matrix and preventing potential cross-linking between the collagen fibers within the matrix.
poorly
organized fashion. As healing continues, the type III collagen is replaced by more mature type I collagen during the maturation process. Elastin fibers provide connective tissue with an elastic component, and the proportion of elastin to collagen will vary depending on the elasticity required of the specific connective tissue type. The interfibrillar component of connective
tissue is composed of water, proteoglycans, and glycoproteins. Proteoglycans (PGs) play a critical
Myofascia Myofascial manipulation has 2 different theories on the possible mechanism of the effectiveness. The first is a direct technique on the mechanical properties of the connective tissue. The second is that the fascia has mechanoreceptors and
smooth muscle receptors and the technique may lower the sympathetic tone.** More physical therapists are moving to accept the second theory as therapists are find-
ing that techniques to decrease the sympathetic
Haphazard laying down of type III collagen Formation of fibrofatty infiltrates
The formation of cross-linking, loss of water content of the matrix, and the increased production of immature collagen may play an important role in the loss of soft tissue mobility in response to injury, immobilization, or abnormal stresses resulting from abnormal posture. This tissue response may lead to loss of mobility between
fascial layers, restrictions between
muscle fibers and the surrounding soft tissue, loss of mobility of nerves in their connective tis-
sue sheaths resulting in nerve entrapment, and loss of muscle play (the ability of the muscle to contract within its connective tissue sheaths) .*°
In addition, immobilized muscles lose muscle length through the loss of sarcomeres, and the resulting relative loss of length of the muscle fibers in comparison to the intramuscular connective tissue leads to an imbalance of tensile force attenuation when the muscle is placed on stretch. This altered stress pattern on the connective tissue may also lead to soft tissue dysfunction, with thickening of the endomysium and perimysium.*! Connective tissue healing takes place in the following stages:35*? 1.
Reaction phase; tissue stimulation takes place through trauma to the connective tis-
sue, resulting in the disruption of microvascular and lymphatic vessels. Vasoconstriction occurs to prevent an excessive loss of fluids.
phase:
granulation
tissue
forms, with increased vascularity of the tis-
sue. Increased fibroblastic activity occurs with the production of immature type III collagen. This phase may take 5 to 8 days in tissues with high metabolism (skin,
and
Woo investigated the response of connective tissue to immobilization*** Their findings included the following tissue responses of the periarticular soft tissue:
Proliferation
~
muscle) or up to5 weeks in low metabolic
tissue (tendons, ligaments). 4.
Maturation phase: Type Ill collagen is replaced with type I collagen, and the orga-
nization of the collagen is improved. Tissue strength increases, and tissue strength and organization can be stimulated by tissue stress. Insufficient tissue stress during this
phase can lead to formation of scar tissue or fibrosis.
Principles of Myofascial and Soft Tissue Manipulation The myofascial manipulation technique is initiated by placing the tissue under tension so that the tissue barrier is engaged. The therapist subsequently contacts the tissue proximally and distally by providing sustained pressure, and the tissue is placed under tension by separating the cephalad and caudad hands, in the direction of the fascial restriction. The direction of the force may also be in a rotational direction, depending on the specific fascial restrictions. The light pressure is maintained until tissue relaxation is achieved and the fascia elongates. The pressure may also be combined with oscillations. Other soft tissue techniques may include muscle play techniques, which can include per-
pendicular deformation,
muscle strumming, or
friction massage.***? Direct pressure to tender points or trigger points may be applied directly through the therapist’s hands or by use of rollers, balls, or other devices. Myofascial and soft tissue manipulation may also be combined with stretching techniques, including PNF. These techniques may also be performed as Self-Mobilizations.
:
ee
Basic Steps for the
Me E Application of Direct _ Myofascial Manipulation 1. The therapist palpates fascia and soft tissue i.
2
— Keylems = 19
that. have limited extensibility. The therapist uses a tissue tension tech-
patient is prone with the foot off the edge of the table. The therapist assess for fascia restriction. In direct Myofascial Mobilization, the therapist
places each hand in opposite directions to the limited fascial mobility. The patient is relaxed and the therapist places an even and opposite pressure onto the tissue of restriction. The ther-
and myofascial tissue in varying instances.
to relax
Basic Concepts of Myofascial
- To relax contractured or spasmodic/strained myofascial tissues that are restricting joint movement * To alter neural reflex relationships that maintain the muscle in a contracted state
Contraindications for
Myofascial Manipulation Myofascial
Manipulation
Manipulative
technique
is a contraindicated and
should
not
be
applied in the case of: «
Open skin lesions
» Areas of infection « Direct myofascial manipulation on acute scars (indirect myofascial techniques may be beneficial)
General Contraindications and Precautions for Manual
Manipulation
Therapy
A basic concept of Myofascial Manipulation is that the technique is performed to relax soft tissue, fascial tensions, and restrictions and allow for increased circulation of the blood and lymph flow. Fascia has mechanoreceptors and smooth
the presence of contraindications and precautions prior to the application of manual therapy. This screening needs to include the identification of potential systemic causes of musculoskel-
muscle receptors and it is also theorized that the technique lowers the sympathetic tone.
An example of Myofascial Manipulation is whena patient has limited ankle dorsiflexion from a scar of an achilles tendon repair, The
and
anticoagulant
Metallic implants, ments
Manipulation
to 5 minutes. The therapist uses both hands
« Position not held until the tissues relax * The patient actively contracts and is unable
disorders
Medically unstable
'
« Force too great or too little
Malignancy Blood-clotting
*
Myofascial Manipulation can be applied to soft
» Inappropriate direction of force
* *
It is imperative that the practitioner screens for
etal pain, disease states, fractures, etc. The type
of technique and the grade of application of that technique are important considerations in determining if a technique is contraindicated: for example, a grade IV joint manipulation may
» : » * *
Recent trauma Fracture Pregnancy Hemarthrosis Joint hypermobility/instability
« Joint inflammation
* Systemic disease
*
The direction of tension, sometimes up to 3
Common Errors in the Application of Myofascial Manipulation
this
Indications for Myofascial
opposite directions.
in opposite | directions. A light pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates. 6. In an indirect Myofascial Manipulation the technique would be to approximate the hands and remove all of the tension on the fascia.
because
technique does not put the tissue under tension. Generally, the practitioner should consider:
therapy * Bone disease (osteoporosis, osteopenia, etc.)
4.
5.
trol would not be contraindicated
apist holds until the tissue relaxes.
nique to mobilize the fascia. foe. ane therapist palpates into the soft tissue and uses the hands in opposite directions - to engage the restrictive barrier with a light force, each hand directing the force in
be contraindicated in the presence of bone disease, whereas a grade | technique for pain con-
including
F
« Systemic connective tissue diseases (RA, Marfan’s, Down, Lupus erythematosus) + Psychological factors * Pain that is not mechanically reproducible + Muscle guarding/holding
joint replace-
Key Terms Caudad: In a direction distal or toward the end, inferior.
Cephalad: In a direction toward anterior portion of the body.
the head
or
Convex/concave rule: When a convex joint surface moves upon a concave surface, a rolling of the convex surface will occur in the same direction as the osteokinematic motion, and is accompanied by a glide in the opposite direction. When the concave joint surface moves upon the convex surface, the glide will occur in the same direction as the osteokinematic motion. Counterstrain technique: An indirect where force is applied away from the barrier to unload involved tissues and resulting in a reflexive relaxation of the an increase of ROM beyond the original
technique restrictive structures, tissue and restriction.
Direct technique: A technique where the joint/
soft tissue restriction restrictive barrier.
is brought
toward
the
HVLA manipulation: In high-velocity low-amplitude (HVLA)-type techniques, the practitioner approaches the restrictive barrier in a joint and then applies a rapid, small amount of short (high-velocity low-amplitude) force to move the joint through its restrictive barrier.
Indirect
technique:
A
technique
where
the
joint/soft tissue restriction is brought away from the restrictive barrier. Manipulation: A manual therapy technique that comprises a continuum of skilled passive movements to joints and/or related soft tissues that are applied at varying speeds and amplitudes, including a small amplitude, high- wea. therapeutic movement.
Mobilization with movement (MWM): Manipulation technique that combines the application ofa sustained accessory joint glide with an active movement
in the direction that is restricted.
Muscle energy technique (MET): A direct manipulative technique where the joint or muscle is taken to the restrictive barrier of motion. The patient voluntarily activates his or her muscles when requested, from a precisely controlled position, in a specific direction, and against a distinctly executed counterforce. Myofascial manipulation: Techniques that focus primarily on mobility of the fascial layers. Soft tissue manipulation: Techniques aimed at soft tissue structures other than fascial layers.
CHAPTER T Introduction 3.
ment techniques preferred by contemporary osteopathic
" References Immediate
2015. i American Physical Therapy Association. Interactive - Guide to Physical Therapist Practice with Catalog of Tests and Measures. Rev 2nd ed. Alexandria, VA:
American Physical Therapy Association; 2003.
wn
si Levangie PK, Norkin CC. Joint Structure and Funetion: A_ Comprehensive Analysis. Sth ed: Philadelphia, PA: F. A. Davis Co; 2011. . Cyriax JH. Textbook of Orthopaedic Medicine: Diagnosis of Soft Tissue Lesions (Vol 1, 7th ed.), London; Balliére Tindall; 1978. Kaltenbomn FM, Vollowitz E, Evjenth O, Kaltenborn
TB, Morgan D. Manual Mobilization of the Joints: _ The Kaltenborn Method of Joint Examination and Treatment. 7th ed. Minneapolis, Physical Therapy Products; 2011.
MN:
17.
. van Duijn AJ, Jensen RH. Reliability of inferior glide mobility testing of the glenohumeral joint. J Man Ma-
a
Maitland
GD, Banks K, Hengeveld
E, Newton
19.
20.
viduals
with
knee
joint compression
14.
2010;11(2):179-185.
osteoarthritis
and
is
modulated
joint mobilization.
by
ea:
Ls:
Ingersoll CD, Hertel J. Immediate effects of a tibiofibular joint manipulation on lower extremity H-reflex
measurements in individuals with chronic ankle instability, J Electromyogr Kinesiol. 2011;21 (4):652-658. 16.
Martinez-Segura R, De-la-Llave-Rincén Al, OrtegaSanuney ; R, Cleland JA, Ferndndez-de-Las-Pefias C.
Dowling D. Muscle energy. In: DiGiovanna E, Schiowitz 5, Dowling D, eds. An Osteopathic Approach to Diagnosis and Treatment. 3rd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2005:83-85. DeStefano L. Greenman’s Principles of Manual Medicine. Philadelphia, PA: Lippincott, Williams & Wilkins; 2011.
24,
as.
Burns DK, Wells MR. Gross range of motion in the cervical spine: the effects of osteopathic muscle energy technique in asymptomatic subjects. J Am Osteopath Assoc. 2006;106(3):137-142. Shadmehr A, Hadian MR, Naiemi SS, Jalaie S. Hamstring flexibility in young women following passive
stretch and muscle energy technique. J Back Musculoskelet Rehabil. 2009;22(3):143-148, 26. Moore SD, Laudner KG, McLoda TA, Shaffer MA. The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. J Orthop Sports Phys Ther. 2011;41(6):400-407,
Fisher BE, Davenport TE, Kulig K, Wu AD. Identificatherapy in patients with musculoskeletal disablement; rationale and description of a clinical trial. BMC Neurology, 2009;9:20. Grindstaff TL, Beazell JR, Sauer LD, Magrum EM,
Ehrenfeuchter W. Muscle energy approach. In; Chila A, ed. Foundations of Osteopathic Medicine. 3rd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2011:682-697.
22.
J Pain.
tion of potential neuromotor mechanisms of manual
to passive cervical joint mobilisation. Man Ther. 2008;13(5):387-396. Bialosky JE, Bishop MD, George SZ, Robinson ME. Placebo response to manual therapy: something out
apy. 2011;19(1):11-19. 21.
Ther, 2011;19(3):143-151. 13. Courtney CA, Witte PO, Chmell SJ, Hornby TG. Heightened flexor withdrawal response in indi-
Schmid A, Brunner F, Wright A, Bachmann LM. Paradigm shift in manual therapy? Evidence for a
of nothing? Journal of Manual & Manipulative Ther-
Hegedus EJ, Goode A, Butler RJ, Slaven E. The neurophysiological effects of a single session of spinal joint mobilization: does the effect last? J Man Manip
Haavik-Taylor H, Murphy B. Transient modulation of intracortical inhibition following spinal manipula-
central nervous system component in the response
M.
: Bialosky JE, Bishop MD, Price DD, Robinson ME, George 5Z. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531-538.
Coronado R, Bialosky J, Bishop M, et al. The comparative effects of spinal and peripheral thrust manipulation and exercise on pain sensitivity and the
tion. ChiroprJ Aust. 2007;37(3):106-116.
nip Ther. 2001;9(2). Maitland's Vertebral Manipulation. 8th ed. Edinburgh, Scotland: Churchill Livingston Elsevier; 2014.
ge
clinical evidence. Man Ther. 2012;17(1):2-8. Wynne MM, Burns JM, Eland DC, Conatser RR, Howell JN. Effect of counterstrain on stretch reflexes, Hoffmann reflexes,
randomized clinical trial. J Orthop Sports Phys Ther. 2012;42(9):806-814.
2015345 (4):252-264. 18.
PA: Wolters Kluwer Health/Lippincott Williams & : Wilkins; 2012. . Gonnella C, Paris SV, Kutner M. Reliability in evaluating passive intervertebral motion. Phys Ther. 1982;62(4):436-444.
pain
Wong CK. Strain counterstrain: Current concepts and
Zt
Exelby L. Peripheral mobilisations with movement.
Man Ther. 1996;1(3):118-126.
28.
Vicenzino B, Paungmali A, Teys P. Mulligan’s mobilization-with-movement, positional faults and Pain
relief: current concepts from a critical review of literature. Man Ther. 2007;12(2):98-108, 29. Mulligan BR. Manual Therapy: “NAGS,” “SNAGS,” “MWMS" etc. Rev 3rd ed. Wellington, New Zealand: Plane View Services; 1995,
30. Vincenzino B, Hing W, Rivett D, Hall T. Mobilisa with Movement. Melbourne, Australia: Elsevier; oot
and
clinical
outcomes
tions in joint «contractures: changes in the reducible
cross-links in periarticular connective tissue collagen
after nine weeks of immobilization. Connect Tissue Res. 1977;5(1):15-19.
in sub-
Akeson WH, Amiel D, Woo SL. Immobility. effects on synovial joints the pathomechanics of joint contrac-
2006;106(9):547-556. 34.
Wong CK, Abraham T, Karimi P, Ow-Wing C. Strain counterstrain technique to decrease tender point palpation pain compared to control conditions: a sys-
41,
ture. Biorheology. 1980;17(1-2):95- 110. é Riezebos C, Koes E. De spierverkorting. Den Haag,
42.
the Netherlands: Stichting Haags Tijdschrift voor Fysiotherapie; 1988. Rudzinski L, Johnson G. Soft tissue mobilization in
tematic review with meta-analysis. J Bodywork Mave35.
ment Ther. 2014;18(2):165-173. Cantu RI, Gordin AJ, Stanborough RW. Myofascial Manipulation: Theory and Clinical Application. 3rd
orthopaedic manual physical therapy. In: Wise C, ed. Orthopaedic Manual Physical Therapy. Philadelphia,
ed. Austin, Texas. Pro.ed; 2011. 36.
37,
38.
Schleip R. Fascial plasticity—a new neurobiological explanation: Part 1. J Bodywork Movement Ther.
Reis
39. Akeson WH, Amiel D, Mechanic GL, Woo. SL, Harwood FL, Hamer ML. Collagen cross-li ei
jects with plantar fasciitis. J Am Osteopath Assoc.
relation to clinical outcome:a mechanistic trial using
. Paris SV, Loubert PV. Foundations of Clinical Orthoof the Musculoskeletal System. 4th ed. Philadelphia,
pressure
32.
a shoulder pain model. J Orthop Sports Phys Ther.
Orthopedic
_ paedics. St. Augustine, FL: Institute Press; 1990. . Frankel VH, Leger D, Nordin M. Basic Biomechanics
changes in widespread
sensitivity, neck pain, and cervical range of motion after cervical or thoracic thrust manipulation in patients with bilateral chronic mechanical neck pain: a
to Evidence. ‘Philadelphia, PA: E e ‘Davis Company;
10.
1974;2 (4):315-323.
physicians. J Am Osteopath Assoc. 2003 ;103 (5):219-224.
Wise clOrthopaedic ‘Manual Physical Therapy from Art
Ae
connective tissuee during contracture develop nent in the immobilized rabbit knee. Connect Tissi | Re 3
Johnson SM, Kurtz ME. Osteopathic manipulative treat-
PA: F. A. Davis; 2015:306-329. 43.
2003;7(1):11-19.
Cyriax JH, Cyriax P, Cyriax’s Illustrated Manual of Orthopaedic Medicine. 2nd ed. Oxford; Boston: But-
Shamus J, Shamus E. The management of iliotibial
terworth-Heinemann; 1996.
band syndrome with a multifaceted approach: a double case report. Int J Sports Phys Ther. 2015;10(3):378-390. Akeson WH, Woo SL, Amiel D, Matthews JV. Biomechanical and biochemical changes in the periarticular
Goodman
a
CC, Snyder TEK. Differential Diagnosis for
Physical Therapists: Screening for Referral. 5th ed. St. Louis, Mo: Saunders/Elsevier; 2013.
Shoulder — : . Chapter Outline |
INTRODUCTION Discussion of the shoulder joint biomechanics and related manual therapy information including a case study.
TECHNIQUES 2A Shoulder General Manual
Therapy Technique 2B Shoulder Flexion Manual Therapy Techniques + Joint manipulation, non-thrust - Joint manipulation, thrust
- Muscle energy technique « Mobilization with movement + Counterstrain technique
- Myofascial manipulation + Soft tissue manipulation + Self-mobilization 2C Shoulder Extension Manual Therapy Techniques + Joint manipulation, non-thrust = Joint manipulation, thrust + Muscle energy technique + Mobilization with movement + Counterstrain technique
+ Myofascial manipulation + Soft tissue manipulation
2D Shoulder Abduction Manual Therapy Techniques + + + + +
Joint manipulation, non-thrust Joint manipulation, thrust Muscle energy technique Mobilization with movement Counterstrain technique
+ Myofascial manipulation + Soft tissue manipulation + Self-mobilization 2E Shoulder Adduction Manual Therapy Techniques + Joint manipulation, non-thrust + Joint manipulation, thrust
Shoulder Internal Rotation Manual Therapy Techniques
OF
Joint manipulation, non-thrust
Joint manipulation, thrust Muscle energy technique .
Mobilization with movement
+ Counterstrain technique . .
Myofascial manipulation Soft tissue manipulation Self-mobilization
26 Shoulder External Rotation Manual Therapy Techniques Joint manipulation, non-thrust Joint manipulation, thrust
- Muscle energy technique
Muscle energy technique
: Mobilization with movement - Counterstrain technique
Counterstrain technique
+ Myofascial manipulation
Myofascial manipulation
+ Soft tissue manipulation
Soft tissue manipulation
+ Self-mobilization
Self-mobilization
Mobilization with movement
+ Self-mobilization
LEARNING OBJECTIVES Upon completion of this chapter, the reader will be able to: - Describe the anatomy and biomechanics of the joints of the shoulder complex
- Understand the state of the evidence for the use of manual therapy treatment techniques of the shoulder complex - Perform the 8 types of techniques for each of the directions of joint motion restriction : Delineate the basic steps for the application of each type of technique
“Intteduction = 25 Coracoacromial
; Acromion
‘Supraspinatus
;
tendon
for mobility and derives its structural stability
_
_
The shoulder complex is composed of the scapula,
humerus, and clavicle, with a single osseous con-
nection to the axial skeleton via the sternoclavicular the
shoulder complex has 4 articulations:
glenchumeral (GH), acromioclavicular (AC),
sternoclavicular (SC), and scapulothoracic (ST)
joints _ These 4 articulations provide for
significant
tendon (long head)
cles. The proximal segment of the GH joint is
the glenoid fossa, and the distal segment is the
Capsular
humeral head. The articular joint surface of the humeral head is significantly larger than that of the glenoid fossa.!” The congruity of the glenoid fossa with the humeral head is improved by the
Subscapularis tendon
Humeral head Humerus
shape of the articular cartilage, which is thinner
in the center, and the presence of the labrum. The labrum is attached to the peripheral margin of the glenoid
range of motion in order to provide the mobility needed for the wide range of functional activities
approximately 50%. The orientation of the glenoid fossa is somewhat variable but most often
required of the upper extremity. Considering the single articulation connecting the upper extremity
The humeral head forms an angle with the shaft
fossa and deepens
is facing lateral, slightly upward,
Subacromial bursa
Biceps
primarily from the articular ligaments and mus-
mobility of the upper extremity, allowing for movement of the upper extremity through a wide
to the axial skeleton, stabilization of the shoulder complex is accomplished primarily though mus-
—
Infraspinatus
Teres minor Muscle
muscle
the fossa by
Subacromial
and anterior.
Acromion
Glavicle
Supraspinatus tendon
of 130 to 150 degrees in the frontal plane and is
~ cle activity. This concept of dynamic stabilization allows for meeting of the contrasting demands
retroverted 30 degrees (see Malaise) 27° The GH joint has a large joint capsule, allowing for significant mobility. The capsule is loose
for mobility and stability. However, the complex arrangement and interplay of articular and contractile structures of the shoulder complex result
inferiorly and anteriorly and tight superiorly.’ The joint capsule is reinforced by 3 glenohumeral ligaments and the coracohumeral liga-
_ in an increased risk for dysfunction.? In addition
to the 4 articulations of the shoulder complex,
ment. The coracohumeral ligament is the most superior ligament and limits inferior translation
movement of the upper thoracic spine also plays
and lateral rotation in the neutral joint position.
a role in the mechanics of overhead movement. Ipsilateral rotation and extension of the upper vation; thus, examination of the upper thoracic
The superior glenohumeral ligament attaches to the superior Jabrum and the upper humeral neck and also limits inferior translation and lateral rotation. These 2 ligaments span the space
and external rotation.’ The capsular pattern of
degrees in extension. Total ROM
region should be included in the evaluation
of
between the anterior border of the supraspinatus
the GH joint is external rotation, abduction, and
is 90 to 120 degrees,
shoulder complex dysfunction.** The glenohumeral (GH) joint is a synovial,
tendon and the superior border of the subscap-
internal rotation.? The coracoacromial arch forms the roof of the glenohumeral joint and is composed of the
mately 40 degrees of external rotation. The total range of motion of rotation is dependent on the position of the humerus in the frontal plane, with
acromion,
the total ROM
thoracic spine occur at the end of shoulder ele-
multiaxial, ball-and-socket joint with 6 degrees of freedom. The GH joint is designed primarily
ularis tendon, forming the rotator cuff interval.2? The medial glenohumeral ligament runs inferior to the superior GH ligament, from the anterosuperior
Acromioclavicular (AG) joint
FIGURE2-1
———————
Acromion process
:
Glenohumeral or shoulder joint
by
Scapula
.
Humerus
bi
Anterior view of the shoulder girdle and
the clavicle including the sternum, manubrium, sternoclavicular (SC) joint, clavicle, acromioclavicular (AC) joint, acromion process, humerus, glenohumeral or shoulder joint, and the scapula
labrum
to
the
superior
aspect
of the lesser tubercle and proximal humerus. It provides anterior stability with shoulder abduction up to 60 degrees and external rotation. The inferior glenohumeral ligament complex consists of an anterior and posterior portion, with an inferior pouch in between these bands. This ligament complex forms a slinglike structure, providing for stability in the inferior direction with the arm in more than 45 degrees of abduction, whereas the anterior and posterior bands provide for stability in the anterior and posterior direction.*** The loose-packed position of the GH joint is in 40 to 55 degrees of abduction and 30 degrees of horizontal adduction, whereas
the closed-packed position is in full abduction
Biceps tendon Glenoid
AC joint
Deltoid
Glenoid labrum
Humerous Joint
capsule FIGURE2-2
Jaint
cavity
Anatomy of the glenohumeral joint
the coracoid
process,
and
the
cora-
coacromial ligament. The space between the arch and the humeral head contains the subacromial bursa, the rotator cuff tendons, and the long head of the biceps. Impingement of the structures in the subacromial space is a common source of shoulder pain and is often related
to impaired biomechanics of the shoulder girdle complex.!*? The motions of the glenohumeral joint include flexion/extension around a coronal axis, abduction/adduction around a sagittal (A-P) axis,
accompanied
in abduction by approxi-
increasing to 120 degrees with
the arm in 90 degrees abduction compared to
60 degrees with the arm in the neutral position.
During elevation of the shoulder, inferior gliding of the humeral head is needed to prevent superior translation of the humeral head as a result of the superior roll that occurs during this motion and to maintain the head of the humerus in its central position in the glenoid fossa. The rotator cuff is thought to play an important role in maintaining this central position of the humeral head and may play a role in imparting the infe-
and internal/external rotation around a vertical
rior glide of the humeral head.2#5!3:4
axis. Open-chain movement involves the convex humeral head rolling and gliding in opposite directions. The available range of motion (ROM) is approximately 120 degrees in flexion and 50
illustrates the relationship of the supraspinatus and biceps brachii tendons to the humeral head. The acromioclavicular (AC) joint is a plane
synovial joint with 6 degrees of freedom. The
Invoducion
«27
CHAPTER 2 Shoulder ‘Coracoacromial Coracoid. ligament process
Clavicle
Acromioclavicular
Coracoclavicular
ligament
ligament
Sca
—
Trapezoid
ligament
Acromioclavicular joint
Subacromial bursa
Coracoacromial ligament
Subacromial
Long head of
FIGURE2-3 The relationship of the supraspinatus and biceps brachii tendons to the humeral head
joint surfaces consist of the lateral end of the clavicle and an articular facet on the acfomion of the scapula, and there is significant variability of the shape and size of the joint surfaces.” The joint capsule is quite lax and provides little structural support. The joint has an intra-articular meniscus that gradually degenerates with age and is no longer functional after age 40. The hyaline cartilage of the joint surfaces also degenerates with age, becoming fibrocartilage by the third decade of life.** Structural support is provided by 4 ligaments: the superior and inferior acromioclavicular ligaments and the conoid and trapezoid portions of the coracoclavicular ligament. The superior AC ligament is stronger than the inferior AC ligament, and the AC ligaments control anterior-posterior motion and maintain joint approximation. The conoid ligament controls inferior-superior motion, and the trapezoid
ligament, as a function of its more horizontal orientation, controls posterior translatory forces. The coracoclavicular ligament also provides the
coupling of posterior clavicular rotation with scapular rotation during shoulder girdle eleva-
tion (see He 2%). Rotatory motions at the AC joint include upward/downward rotation, internal/external rotation, and anterior/posterior tipping of the
scapula relative to the clavicle, with a total available range of approximately 30 degrees for each
of these motions.** The loose-packed position of the AC joint is the arm at the resting position, the closed-packed position is 90 degrees of abduction, and the capsular pattern is pain and limitation end range of elevation and horizontal adduction.”® The sternoclavicular (SC) joint, a sad-
dle-shaped synovial joint, is the only direct physical link between the shoulder girdle and the axial skeleton. The joint consists of the medial end of the clavicle and a notch made up of the lateral/ proximal manubrium and the cartilage of the first rib, The 2 joint surfaces are separated by an articular disc, which increases the congruity of the 2 joint surfaces and has attachments for the
FIGURE2-4 The acromioclavicular joint
clavicle rolling and gliding in the same direction, with an available total range of 35 to 50 degrees. In addition, long axis rotation of the clavicle
movement of the distal clavicle. The costoclavicular ligament is a substantial ligament that has insertions at the inferior aspect of the medial
allows for posterior rotation of the clavicle from
clavicle and
the neutral position, with up to 50 degrees of posterior rotation possible The joint capsule envelops both joint compartments and is reinforced anteriorly and posteriorly by the sternoclavicular ligaments that limit anterior/posterior
rib.” The ligament has been described as having 2 bundles: the anterior bundle and the posterior bundle,” though other authors also describe the 2 bundles as being continuous.” The costoclavicular ligament limits clavicular elevation and
Anterior Sternoclavicular
Sternal (proximal) end
ligament
of clavicle Interclavicular
ligament
capsular ligaments.'’ The disc divides the joint
space into 2 compartments (see é During clavicular elevation and depression,
the convex medial clavicle moves on the stationary disc, with movement thus occurring in the Jateral joint compartment and the medial clavicle rolling superiorly and gliding inferiorly, with
a total available range of 55 to 60 degrees. During
clavicular protraction and retraction, the concave
ary manubrial
joint surface, with the disc and
Cartilage of
Costoclavicular ligament
disc and the distal clavicle move on the stationFIGURE2-5 The sternoclavicular joint
costochondral
ist rib Manubrium
junction of the first
“Intoducion = 29 28
CHAPTER? Shoulder
i may play a role i in imparting an inferior glide of the clavicle when the ligament is fully loaded.? The interclavicular ligament is located on the
superior manubrium, connecting the bilateral SC ; : joint at their ‘superomedial aspects.’” The liga-
ment may provide inferior and superior stability of the clavicle,’ though that function is debated _ by other authors.’” The loose-packed position of _ the SC joint is with the arm Testing at the side, ' whereas the closed-packed position is full ele-
vation and scapular protraction. The capsular pattern is pain and restriction upon joint loading in horizontal adduction and full elevation.” The scapulothoracic (ST) joint is a physiologic articulation of the thorax and the ante-
rior aspect of the scapula. Although the ST joint a true anatomical joint, motion at the ST is not joint contributes significantly to the total shoul-
der complex motion: approximately 60 degrees of the total ROM of the shoulder complex into
elevation is accounted for by the scapular move‘ment. Motion at the ST joint cannot occur independently from motion at the AC and SC joints, considering that the connection of the scapula to the axial skeleton is through the AC and SC
alongside
the body.
Although
elevation can
~ occur in any plane, the term scaption is used to
describe elevation in the plane of the scapula,
which is 30 to 45 degrees anterior to the frontal plane. Movement in this plane appears to maximize joint congruity and to have optimized joint performance while minimizing joint impinge-
ment. During elevation, coordinated movement
takes place in the 4 joints of the shoulder complex and the upper thoracic spine, which results
in an optimal relationship between the scapular and humeral alignment and optimal muscle performance.? The overall ratio of movement
between GH and ST motion, also referred to as the scapulothoracic rhythm, is 2:1; however,
the contribution of the GH and ST joints varies throughout the range. During the initial phase of elevation, the humeral head migrates superiorly to center itself in the glenoid fossa, and it remains in this centered position throughout the remaining ROM. Scapular elevation and upward rotation occurs as a result of elevation at the SC joint. The GH joint contribution to motion compared to ST motion is increased (3:1). Dur-
ing the middle phase of elevation (from 60 to
the AC joint that involve motion of the scap-
140 degrees), the relative contribution of the ST joint increases, and ST motion exceeds GH
to the clavicle, the scapula can also ula relative
motion (0.7:1). After 90 degrees of elevation,
move in upward/downward rotation, elevation/
maximal shear forces develop in the GH joint as a result of muscular activity of the deltoid and
joints. In addition to the motions described
depression,
and protraction/retraction.
at
Upward
rotation occurs during shoulder complex elevation, with a total available ROM of 60 degrees. Upward rotation is mostly a combination of at the AC and SC joints. Elevation of motions the scapula is accompanied by clavicular eleva-
tion at the SC joint. Protraction/retraction is a translation of the scapula along the shape of the convex thorax, requiring internal/external rotation at the AC joint and protraction/retraction of _ the clavicle at the SC joint. Anterior/posterior tipping of the scapula accompanies long axis rotation of the clavicle at the SC joint. Stability
of the ST joint depends to a large extent on musculature to provide for a stable base for motion
of the upper extremity,?74*°
Functional Biomechanics of
rotator cuff muscles. The humeral head remains centered in the glenoid fossa, indicating an inferior glide that occurs together with a superior roll, as a result of the activity of the rotator cuff.
The humerus also externally rotates during elevation. The relative contribution of the AC and SC joints to scapular motion shifts toward the AC joint as the angle of elevation increases, and
a posterior rotation of the clavicle occurs during scapular upward rotation. After 140 degrees of elevation, the GH contribution relative to the ST joint again increases to a 3.5:1 ratio. In addition to upward rotation of the scapula, the scapula also tips posteriorly by approximately 30 degrees and externally rotates on the thorax
throughout the range of elevation.?>* During the final phase of elevation, the upper thoracic
Shoulder Complex Elevation
spine rotates to the ipsilateral side and moves toward extension.®
Shoulder elevation refers to the movement of the upper extremity away from the resting position
The primary mover of the glenohumeral joint in elevation is the deltoid muscle, with the
anterior and middle parts of the deltoid showing
the effectiveness of manual therapy for the ©
the most activity during scaption. The deltoid is increasingly active during humeral elevation,
including rotator cuff disorders and adhesive
treatment of a variety of shoulder dysfunctions,
with peak activity at 90 degrees of abduction.
capsulitis.#
The rotator cuff shows an activation pattern similar to the deltoid muscle, with the supraspinatus muscle showing peak activity at 90 degrees of humeral abduction. The supraspinatus muscle also compresses the GH joint and guides to position the humeral head in the center of the glenoid fossa. The other rotator cuff muscles, including the subscapularis, infraspinatus, and teres minor, also gradually increase in activity
and Marinko# and Howard et al.% found evi- — dence that manual therapy of the shoulder girdle joints improved mobility and pain of the shoulder. Surenkok et al. found evidence that scapular mobilization results in decreased pain and increased mobility and physical function in patients with shoulder dysfunction.” Moore et al. studied the immediate effects ofa muscle energy technique (MET) on shoulder ROM
throughout
in overhead athletes and found that a single
the
range,
with a
peak
in activity
at 70 degrees of elevation to provide for inferior glide of the humeral head, and again at 115 degrees in order to produce humeral external rotation,””° The upper trapezius and serratus anterior muscles form a force couple with the
Systematic
application of a MET
review
by
Camarinos:
technique to the exter-
nal rotators and horizontal abductors of the shoulder resulted in increased ROM of internal rotation and horizontal adduction.”* In a study
rotation of the scapula. The role of the upper
by Djordjevic et al., mobilization with movement combined with kinesiotaping resulted in increased active ROM and decreased pain in
trapezius
patients with painful shoulders.*” Godges
lower trapezius muscle to provide for upward appears
to
be
more
critical
during
abduction of the humerus, whereas the serratus anterior appears more critical during flexion of the humerus. The rhomboid muscles act as scapular stabilizers during elevation, eccentrically controlling the scapula as it upwardly rotates.** The latissimus dorsi and pectoral muscles are prime movers of depression of the shoulder
complex, which occurs during important closed chain functional activities such as pushing up out of a chair. The teres major and rhomboid muscles work synergistically to stabilize the scapula during these activities.’ When evaluating a patient with shoulder dysfunction, it is important to assess all osteokinematic and arthrokinematic motions of the 4 shoulder girdle joints, considering the complexity of the biomechanics of the shoulder girdle. In addition, the mobility of the upper thoracic spine needs to be assessed,‘ and the cervical spine needs to be cleared as a potential source of shoulder pain. The function of the musculature needs to be examined carefully, considering the role of the musculature in movement and active stabilization of the shoulder girdle. Recent evidence indicates that manual therapy can be a useful intervention in the treatment of shoulder pain and dysfunction. A recent systematic review found level B evidence for
et al.
found that soft tissue mobilization of the subscapularis muscle in combination with PNF contract-relax techniques led to an increase in external rotation ROM and overhead reach. The authors postulated that the decreased length and tightness of subscapularis muscle results in decreased ROM in external rotation at 45 degrees abduction when compared to 90 degrees of abduction and that lengthening the muscle results in increased external rotation ROM, with similar findings reported in another study.’
Recent
evidence
also indicates
that
manual therapy directed at the upper thoracic and cervical spine can result in decreased pain and improved function of patients with shoulder dysfunction and pain.*-®2!-8 Common shoulder girdle dysfunctions that are routinely treated with manual therapy include adhesive capsulitis, shoulder impinge-
ment
(including rotator cuff pathology),
and
osteoarthritis. Adhesive capsulitis (frozen shoul-
der) has a prevalence of 2 to 5% of the general population but is significantly more prevalent in patients with thyroid
disease or diabetes melli-
tus (up to 38%). It is characterized by the presence of multiregional synovitis and frequently progresses to significant fibrosis of the joint
capsule complex, leading to significant loss of ROM.*' The loss of ROM is likely to occur in a
;
3103
irritability level! Vermeulen et al. found that high-grade mobilization techniques were more effective than low-grade mobilization techniques in restoring joint mobility and reducing _ disability in patients with adhesive capsulitis of more than 3 months in duration, with a greater than 50% loss of ROM. A recent study examined the use of end-range grade IV mobiliza‘tion techniques and scapular mobilization in patients with significant loss of ROM resulting from adhesive capsulitis and found a greater improvement in ROM, disability, and kinemat_ics compared to patients who received standard physical therapy, which included midrange mobilizations, stretching exercises, and modalities.** Johnson et al.*4 found that posterior glide mobilizations were more effective than anterior glide mobilizations in restoring external rotation _ ROM in patients with primary adhesive capsulitis. Although this finding appears to contradict the convex/concave rule, the authors postulate that asymmetrical capsular tightness may affect humeral head motion.** Tightness of the antenor capsule and the rotator cuff interval may influence the arthrokinematic glides and in this case may
prevent
the
anterior glide normally
associated with external rotation. The posteriorly directed mobilization may be more effective
in restoring anterior capsule mobility than an anteriorly directed
mobilization
and
may
thus
be more effective in restoring external rotation mobility.
Subacromial impingement syndrome (SIS) can include impingement of the structures in the subacromial space, resulting in tendinopathy of the rotator cuff tendons, rotator cuff tears, and bursitis. This impingement can be the result of altered mobility of the shoulder girdle joints. Decreased mobility of the glenohumeral joint, especially of the inferior glide accessory motion, can be a contributing factor to the development of subacromial impingement. The function of the SC and AC joints should also be
therapy in patients with SIS. These authors also
found moderate evidence supporting the use of exercise therapy in this population.”A system-
atic review by Braun and Hanchard concluded that manual therapy and exercise seem
effective
for the treatment of SIS but identified the need for further high-quality research.* Rhon et al. compared the long-term effectiveness of manual therapy to the use of corticosteroid injections and found that both groups had significant improvements in pain and function; however, the manual therapy group used significantly less follow-up healthcare services than the injection group.** Mobilization with movement and glenohumeral mobilizations in combination with a supervised
exercise program
were
found
to be
effective in decreasing pain and increasing function.*’* Tate et al. reported that a program using strengthening of the rotator cuff and scapular muscles, combined with manual therapy for posterior and inferior glides of the glenohumeral joint and the thoracic spine, resulted in symptomatic and functional improvement in patients
with SIS.
Osteoarthritis is a frequently observed pathology of the AC joint and may contribute to the development of subacromial impingement.'>!7“°
Although there is no research directly examining the effect of manual therapy in patients with AC
joint arthritis, Harris et al. reported that patients with primary AC joint pain had decreased pain and improved function following treatment with accessory joint glide techniques of the distal clavicle." There is currently insufficient evi-
dence to evaluate the effectiveness of manual therapy in the treatment of osteoarthritis of the glenohumeral joint. Shoulder pain can be a manifestation of dysfunction and disease in other anatomical structures and regions. Cervical dysfunction can be a source of referred pain to the shoulder, including
thoracic outlet syndrome and cervical tadiculopathy. Manual therapy practitioners should also perform systems screening for nonmechanical causes of shoulder pain, with emphasis on the cardiovascular, pulmonary, and upper gastrointestinal systems.”
CASE STUDY Patientis a 58-year-old female artistic painter. She paints wall murals but has been. unable todosodue | ‘to having right shoulder pain. Patient states she fell off a ladder on her shoulder 3 months ago and has difficulty raising her arm. The pertinent medical history includes insulin- -dependent diabetes. mellitus and hypothyroidism. Physical therapy examination findings are as follows: Pain at end ranges with active and passive range of motion Presence of a painful arc of 60 to 120 degrees abduction
Decreased active and passive range of motion in a capsular pattern Restricted inferior and posterior direction glides Decreased strength and poor functional reach ability above shoulder height and when reaching behind her back affecting her activities of daily living and work activities. . What is the shoulder capsular pattern?
. What diagnoses can be concluded from decreased ROM in capsular pattern of the glenohumeral joint? 3. How do you determine if the joint condition is acute, subacute, or chronic? 4, How would that information direct your joint manipulation intervention? 5° Which manual therapy techniques are appropriate for this patient, based on existing evidence? Per the evidence outlined in this chapter, the therapist may consider non-thrust joint manipulation of inferior and posterior glides, using grade Ill or IV if tolerated by the patient. MWM in the affected directions may also be considered. The patient can be instructed in self-mobilization techniques in the affected directions. Additional evidence for the use of these techniques include: A Cochrane review by Page et al*? concluded that a combination of manual therapy and exercise had short-term clinical importance in patients with adhesive capsullitis. Desjardins-Charbonneau et al.“ performed a systematic review and meta-analysis on the efficacy of manual therapy for patients with rotator cuff tendinopathy. A small statistically significant reduction in pain was found with manual therapy compared to a placebo. When adding manual therapy to an exercise program, there was a significant decrease in pain. Based on low to moderate quality evidence, manual therapy may decrease pain, but it was unclear whether it can improve function. Delgado-Gil et al. investigated the effects of mobilization with movement on pain and end range of motion with patients with impingement syndrome and found that patients receiving 4 sessions
of mobilization with movement had significantly better outcomes for pain during active flexion and external rotation.
Key Terms Acromioclavicular joint classification: synovial joint with 6 degrees of freedom.
Plane
Capsular pattern glenohumeral joint: External rotation, abduction, and internal rotation. Capsular pattern sternoclavicular joint: Pain and restriction upon joint loading in horizontal
adduction and full elevation.
Closed-packed position glenohumeral Full abduction and external rotation.
joint:
Closed-packed position sternoclavicular joint:
Full elevation and scapular protraction with 90 degrees of abduction. Glenohumeral joint classification: Synovial, multiaxial, ball-and-socket joint with 6 degrees of freedom.
dete
A recent systematic review found limited evidence supporting the effectiveness of manual
enh
ea d._ passive: ROM, as well as glenohujoint accessory motion. A recent clinical e recommends manual therapy techn pain management, improvement of. ROM, and functional improvement. Stretching exercises were also recommended and should be dosed based on the patient's tissue
_ considered, because the loss of ROM in these joints may lead to altered scapular movement. Me
pee
Aecapsular pattern, and clinicians should evaluate
)
‘References
33
~
“CHAPTER 2 Shoulder posterior shoulder tightness: a randomized controlled trial. J Orthop Sports Phys Ther. 2011;41 (6) 400-407.
Backed: posi tan glenohumeral joints 40 of to 55. degrees of abduction and 30 aoe : horizontal adduction.
‘not a true anatomical joint, motion at the ST
Loose-packed position sternoclavicular Joint: The arm resting at the side.
Sternoclavicular joint classification: Saddleshaped synovial joint with 2 degrees of freedom, clavicular head convex in the frontal plane and ‘concave in the transverse plane.
Scapulothoracic joint classification: Physiologic articulation of the thorax and the anterior ae of the scapula. Although the ST joint is
der complex motion. 28.
ose Kachingwe AF, Phillips B, Sletten E, Plunkett SW. Comparison of manual therapy techniques with
Physiol Ther. 2012;35(6):454-463. Godges JJ, Mattson-Bell M, Thorpe D, Shah D. The
impingement: a randomized controlled pilot clinical
effects of soft tissue mobilization
Te Moore KL, Agur AMR, Dalley. AF Clinically Oniented : Anatomy. 7th ed. Philadelphia, PA: Wolters Kluwer
Health/Lippincott Williams & Wilkins; 2013. Po Levangie PK, Norkin CC. Joint Structure and Func-
tule asapplied Los
PA: F. A, Davis Co; 2011. 3. Donatelli R, Physical Therapy of the Shoulder. Sth ed. St. Louis, MO: Elsevier/Churchill Livingstone; 2012. . Redman B, van Duijn A, van Duijn J, Hyatt A. Effects of lower cervical and upper thoracic mobiliza-
16. 17:
tion on shoulder range of motion limited by shoulder impingement syndrome: a case series. J Man Manip Ther. 2010;18(4):235.
NA,
Mazzocca
AD.
Biomechanics
and
treatment of acromioclavicular and sternoclavicular joint injuries. Br J Sports Med. 2010;44(5):361-369. Cyriax JH, Cyriax P. Cyriax’s Illustrated Manual of Orthopaedic Medicine. 2nd ed Oxford; Boston: But-
Med. 2014;22(3):248-252. 18.
. Strunce JB, Walker MJ, Boyles RE, Young BA. The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. J Man Manip Ther. 2009;17(4):230-236.
bility. Clin Sports Med. 2013;32(4):625-636, Cools AMJ, Struyf F, De Mey K, Maenhout A, Castelein B, Cagnie B. Rehabilitation of scapular dyski-
19.
nesis: from the office worker to the elite overhead athlete. Br J Sports Med. 2014;48(8):692-697.
- ulation on shoulder pain: a regional interdependence model. Phys Ther Rev. 2011;16(5):399-408. Magee DJ. Orthopedic Physical Assessment.
St. Louis, MO: Saunders Elsevier; 2014. . Murray IR, Goudie EB, Petrigliano FA, CM.
Functional
anatomy
and
20. 6th ed.
Robinson
biomechanics
of
shoulder stability in the athlete. Clin Sports Med.
. Cyriax JH. Textbook of Orthopaedic Medicine: Diagnosis of Soft Tissue Lesions. (Vol 1, 7th ed.). London, England; Balliére Tindall; 1978. Gebremariam L, Hay EM, van der Sande R, Rinkel WD, Koes BW, Huisstede BMA. Subacromial impingement syndrome—effectiveness of physiotherapy and manual
22.
23.
therapy. BrJ Sports Med. 2014;48(16):1202-1208. . Seitz AL, McClure PW, Finucane S, Boardman ND, Michener LA, Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clin Biomech. 2011;26(1):1-12. PM, Braman
JP.
Shoulder
24.
impingement:
25.
Schomacher J. The conyex-concave rule and the lever law. Man Ther. 2009;14(5):579-582.
. Brandt C, Sole G, Krause MW, Nel M. An evi‘dence-based review on the validity of the Kaltenborn
J Man Manip
Ther. 2009;17(4):237-246.
Brantingham
JW,
Cassa
TK,
Bonnefin
D, et al. Ma-
nipulative therapy for shoulder pain and disorders: Expansion of a systematic review. J Manipulative Physiol Ther. 2011;34(5):314-346. Camarinos J, Marinko L. Effectiveness of manual physical therapy for painful shoulder conditions: A systematic review. J Man Manip Ther. 2009;17(4):206-215.
Howard PD, Ebersole J, Lavo J, McKelvey I, Quigley L, Quirk D. The effect of shoulder mobilization/ manipulation on increasing range of motion in patients with stiff shoulders; a systematic review, Orthop Phys Ther Pract. 2013;25(1):6-9.
biomechanical considerations in rehabilitation. Man
Ther. 2011;16(1):33-39.
Walser RF, Meserve BB, Boucher TR. The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials.
26.
Surenkok O, Aytar A, Baltaci G. Acute effects of scapular mobilization in shoulder dysfunction: a dou-
ble-blind randomized placebo-controlled trial, J Sport Rehabil. 2009;18(4):493-501. Moore SD, Lau The immediate Sees
ieee
ae rgy technique on
trial. Ann
and manual
Kelley MJ. Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther.
41.
Harris
physical
42.
35.
36.
with manual physical therapy for the management
KD,
Deyle
GD,
Gill
CS. AcromioclavicuOper Tech Sports Med. NW,
Howes
RR.
Manual
therapy for injection-confirmed nonacute
acromioclavicular joint pain. J Orthop Sports Phys Ther. 2012;42(2):66-80. Goodman CC, Snyder TEK. Differential diagnosis for
physical therapists: Screening for referral. Sth ed. St. Louis, MO: Saunders/Elsevier; 2013. 43.
Page MJ, Green S, Kramer S, et al. Manual
therapy
and exercise for adhesive capsulitis (frozen shoulder). The Cochrane Database of Systematic Reviews. 2014;8:CDO11275.
44.
Desjardins-Charbonneau A, Roy J, Dionne CE, Frémont P, MacDermid JC, Desmeules F. The efficacy of manual therapy for rotator cuff tendinopathy: a systematic review and meta-analysis. J Orthop Sports
Phys Ther. 2015;45(5):330-350.
mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis, J Orthop Sports Phys Ther. 2007;37 (3):88-99. Braun C, Hanchard N. Manual therapy and exercise for impingement-related shoulder pain. Phys Ther Rev. 2010;15(2):62-83. Rhon DI, Boyles RB, Cleland JA. One-year outcome of subacromial corticosteroid injection compared
for patients with
Orthop Sports Phys Ther. 2010;40(8):474-493. Gancarczyk SM, Ahmad lar arthritis and osteolysis. 2014;22(3):214-220.
Vermeulen HM, Rozing PM, Obermann WR, le Cessie
end-range mobilization and scapular mobilization approach in a subgroup of subjects with frozen shoulder syndrome: a randomized control trial. Man Ther. 2012;17(1):47-52. Johnson AJ, Godges JJ, Zimmerman GJ, Ounanian LL. The effect of anterior versus posterior glide joint
therapy intervention
40,
Intern Med.
ized controlled trial. Phys Ther. 2006;86(3):355-368. sie Yang J, Jan M, Chang C, Lin J. Effectiveness of the
anat(BR).
a case report. J Man Manip Ther.
subacromial impingement syndrome: a case series. J
low-grade mobilization techniques in the management of adhesive capsulitis of the shoulder: random-
2009;91(12):1632-1637.
21.
2013;32(4) 607-624.
Ludewig
Sonnabend DH, Young AA. Comparative omy of the rotator cuff. J Bone Joint Surg
der impingement:
-2006;14(3):176.
1805. Bergman G, Winters JC, Groenier KH, et al. Manip-
Sci.
S, Vliet Vlieland T. Comparison of high-grade and
34.
Gebhardt TL, Whitman JM, Smith MB. Mobilization with movement as part of a comprehensive
physical therapy program for a patient with shoul-
2013;43(5):A1-A31. 32.
terworth-Heinemann; 1996. Warth RJ, Lee JT, Millett PJ. Anatomy and biome-
Degen RM, Giles JW, Thompson SR, Litchfield RB, Athwal GS. Biomechanics of complex shoulder insta-
.
31,
trial, J Man Manip Ther, 2008; 16(4): 238-247. 38.
39. Tate AR, McClure PW, Young IA, Salvatori R, Michener LA. Comprehensive impairment-based exercise
Ther
a randomized, controlled 2004;141(6):432.
chanics of the sternoclavicular joint. Oper Tech Sports
. Sueki DG, Chaconas EJ. The effect of thoracic manip-
10.
Bontempo
therapeutic exercise in the treatment of shoulder
2014;26(11):1803-
J Phys
ulative therapy in addition to usual medical care for patients with shoulder dysfunction and pain:
to the glenohumeral joint. Man Ther.
2007;12(1):3-11.
tion: A Comprehensive Analysis. 5th ed. Philadelphia,
with
proprioceptive neuromuscular facilitation on glenohumeral external rotation and overhead reach. J Orthop Sports Phys Ther. 2003;33(12):713-718. Al Dajah SB. Soft tissue mobilization and PNF improve range of motion and minimize pain level in shoulder impingement.
30.
Intern” Med.
bilization with movement and kinesiotaping compared with a supervised exercise program for painful shoulder; results of a clinical trial. J Manipulative
immediate
29.
randomized trial. Ann
2014;161(3):161-169.
Zr.) Djordjevic OC, Vukicevic D, Katunac L, Jovie S. Mo-
joint contributes significantly to the total shoul-
" References
of the unilateral shoulder impingement ‘syndrome:
4 pragmatic
45.
Delgado-Gil JA, Prado-Robles E, Rodrigues-deSouza DP, Cleland JA, Fernandez-de-Las-Penas C,
Alburquerque-Sendin F. Effects of mobilization with movement on pain and range of motion in patients with unilateral shoulder impingement syndrome: a
randomized controlled trial. J Manipulative Physiol Ther. 2015;38(4):245-252.
: =
Manual Therapy Techniques fortheShoulder CHAPTER 2 Shoulder
Manual Therapy Techniques for the Shoulder 2C Shoulder Extension Manual Therapy Techniques 2D Shoulder Abduction Manual Therapy Techniques
Rotation
Manual Manual
Therapy Therapy
The therapist can perform a thrust technique at tissue tension.
The open pack position of the shoulder is 30 degrees of shoulder flexion, 30 degrees of shoulder abduction, and 5 degrees of extemal rotation,
1, The therapist places the cephalad hand on the superior proximal humeral head and the caudad hand around the elbaw. 2. While the patient lifts the arm into 90 degrees of shoulder abduction, the patient actively circumducts the shoulder. 3. As the patient circumducts the shoulder, the therapist uses the caudad hand to distract the humerus and uses the cephalad hand to perform a circular accessory glide of the proximal humerus to facilitate the
ed
WIA
Notes: This technique can be used for the reduction of a glenohumeral dislocation as in Figure B
© fel
a
xi mls EEGES . = = is a \ aer wUUN J JJ J J
FIGURE 2-6
ae
=== a
1. The therapist places the hands above the elbow around the humerus, 2. The therapist lifts the shoulder to about 30 degrees of shoulder flexion, 30 degrees of shoulder abduction, and 5 degrees of external rotation. 3. The therapist locks the elbows at 90 degrees at their side and shifts and bodyweight away from the patient in line with the abduction of the shoulder to create traction at the shoulder, 4. The therapist maintains traction until the tissue relaxes.
ie
Therapist Position: Standing at side by the foot of the table
ad
] | i
—
Patient Position: Supine at the side of the table
ee Sneha
}
a
A.
a
oo
Fee
a
| Restricted. Motion: Limited Shoulder. Mobility
oe ee
sty
etary ca eee Gaal a nares
=n|
u eect
eral Ntn Limitation
a
L Type of Manipulation: Joint traction
-Shoulid
COO OOOO
uc sat
TINNTNINDNVO
osha
re
» » = = » = = = a) = 2 2 2 2 | oe ~~) "2 es) “2 “2 “wy 2 "2
Patient Position: Sidelying
Therapist Position: Standing in front of the patient
EE
2E Shoulder Adduction Manual Therapy Techniques
wa BE.
a) (epee es
» =
Pe
Rotation
i,
Shoulder Internal Techniques 2G Shoulder External Techniques
Shoulder Flexion Manual Therapy Techniques
obq “Restricted : Motion: inted 5Shoulder Mobility ‘
ooo
2F
2A Shoulder General Manual Therapy Techniques 2B
LIMITED SHOULDER MOBILITY
34
35
circumduction motion of the shoulder. The glide (humeral head FIGURE 2-7
convex) is performed in the opposite direction of the position the elbow is going. 4. This is repeated and performed in a rhythmic format when the arm is brought into circumduction.
Notes: This is part of the Spencer technique sequence.
Joint: Shoulder
Shoulder General Motion Limitation:
| ee Manipulation: Self-mobilization _ Restricted Motion: : Limited Shoulder.Mobility _ Patient Position: Standing 1. The patient stands bent forward to bring the trunk parallel to the
ground. The patient stands with one foot forward and one foot backward.
2. The patient lets the arm hang against gravity in a pendulum position. 3, The patient shifts bodyweight back and forth to create passive movementat the shoulder.
FIGURE 2-8
Notes: The patient can stand with the feet abducted and shift side to side. This is often termed a Codman’s or pendulum exercise.
‘
‘i
CHAPTER 2 Shoulder
37
FIGURE 2-10
Notes: This technique will be beneficial for patients with scapulothoracic dysfunction,
PEERY al ad
il
:
een
eayne Of Manipulation: Joint manipulation, se © non-thrust reas " Restricted Motion: Limited Shou idet Flexion ne
1 os Se Sl el s+.
1. The therapist lifts the humerus with the cephalad hand and stabilizes the scapula with the caudad hand, 2. The humerus should be able ta move to 120 degrees with the scapula stabilized, 3. At the tissue barrier, the therapist can create 2 progressive oscillation to manipulate the scapula in a posterior/inferior direction while stabilizing the humerus.
=
=
=
1
FIGURE 2-11
Type of Manipulation: Jointntmanipulation, :
| Joint: Shoulder Shoulder Flexion Motion Limitation
non-thrust Restricted:Motion: Limited shoulderFlexion _ Patient Position: Supine at the side of the table
Therapist Position: Standing on the same side of the patient's shoulder to be treated 1. The therapist lifts the humerus into flexion with the caudad hand and
tractions the humerus. 2. The therapist places the cephalad hand on the anterior portion of the humeral head. 3. The therapist creates a progressive oscillation with the cephalad hand
in a posterior and inferior direction on the humeral head to increase mobility of the posterior capsule.
FIGURE 2-12
LIMITED SHOULDER FLEXION
hs
3
2. The therapist places the cephalad hand around the top of the scapula from the thumb on the anterior chest wall and the fingers around to the spine of the scapula, 3. The therapist uses both hands in unison to move the scapula in all planes.
Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
Patient Position: Supine at the side of the table
a el a a
‘
w= Ralea ie
¥
'
eT:
scapula.
+ Joint: Shoulder | Shoulder Flexion Motion Limitation
heps
1. The therapist places the caudad hand around the inferior border of the
* * « ¢
a
A
a
Therapist Position: Standing in front of the patient
ae
Patient Position: Sidelying
« Mobilization with movement
=
+ non-thrust || Restricted Motion: Limited Shoulder Mobility
CE
i |
|| Type of Manipulation: Joint manipulation,
« Joint manipulation, thrust « Muscle energy technique
a
a
Toke shoutier | Shoulder General Motion Limitation
PPPITPVPINIINIIINNNNN0
ae
|
|
Notes: A patient with adhesive capsulitis would benefit from this technique.
Shoulder Flexion Manual Therapy Techniques * Joint manipulation, non-thrust
Therapist Position: Standing on the same side of the patients shoulderto be treated
a a i i i be ce
Patient Position: Supine or prone
i.
Patient Position: Seated
APRN PNNTANN NTOOOO OOOE SEEK AS nEEE as SISSIS SSS SSS
4
i
therapist palpates the anterior ribs that have therapist uses a tissue therapist palpates into
latissimus dorsi muscles, pectoralis major, limited extensibility. tension technique to mobilize the fascia. the soft tissue and uses the caudad hand
to grasp the humerus and flex the shoulder with upward traction. 5. The therapist uses the cephalad hand on the latissimus dorsi or pectoralis major to engage the restrictive barrier with a light force in the direction of tension, sometimes up to 3 to 5 minutes. The therapist uses both hands in opposite directions.
6. Alight pressure on the barriers held until the tissue barrier softens and relaxes and the myofascial unit elongates.
FIGURE 2-19 Notes: Depending on the specific muscle identified, the fiber direction will change. In Figure B. the therapist utilizes their cephalad hand to raise the arm into shoulder flexion while the caudad hand grasps onto the scapula to engage the restrictive barrier in an inferior direction.
1
LIMITED SHOULDER FLEXION
CHAPTER 2 Shoulder
ByPPR JUUUY
40
_
| |
Manual Therapy Techniques fortheShoulder
Manual Therapy Techniques fortheShoulder = CHAPTER 2 Shoulder Self soft tissue manipulation Patient Position: Standing with bodyweight on a massage ball 1. The patient places bodyweight on a massage ball with the pectoralis
muscle. 2. The patient can hold statically or rock side to side to relax the soft tissues, 3. Thisis repeated until the soft tissue relaxes.
Manual soft tissue manipulation Patient Position: Supine
Therapist Position: Standing on the involved side of the patient 1. The patient lies supine. 2. The therapist palpates the pectoralis, subscapularis, and latissimus dorsi muscles and holds deep pressure to relax the muscle. 3. The therapist can perform soft tissue manipulation with gentle strumming and lateral mobilization of the muscles and tendons, and with circular strokes to increase circulation. 4° This is repeated until the soft tissue relaxes.
FIGURE 2-20
FIGURE 2-21 Notes:A towel can be placed over the ball to soften the technique. As an alternate technique the patient can be prone over a foam roller and roll back
and forth over the latissimus dorsi or pectoralis muscles as seen in Figure C.
LIMITED SHOULDER FLEXION
42
43
met. 4. The patient can hold tension statically or rock the shoulder into flexion by keeping a hand on the floor and shifting bodyweight posteriorly to create traction on the shoulder while stretching into flexion.
Alternate Techniques: In Figure B, the patient can lie over a foam roll in line with the spine. The patient raises the shoulder to be mobilized into flexion. With the opposite hand the patient reaches around and
grasps onto the opposite scapula and mobilizes into scapular upward
rotation (Figure 8). Figure C shows the patient seated, with the involved
al
PUPP
FIGURE 2-22
ah
=
ah
jae Ee ps1,
extremity on the table. The patient bends forward to the restriction and providesa posterior glide with the opposite hand.
Shoulder Extension Manual Therapy Techniques
e Joint manipulation, non-thrust e Muscle energy technique
« Counterstrain technique « Myofascial manipulation + Soft tissue manipulation
* Mobilization with movement
* Self-mobilization
« Joint manipulation, thrust
| Type of Manipulation: joint manipulation, = Joint: Shoulder©
/ enon-thrust
aa “9 Heid
Notes: This technique can be performed with the patient seated or standing as in Figure B.
hse
j| Shoulder Abduction Motion, Limitation,
Al 5
T
FIGURE 2-37
Se
Solnts Shoulder RCIGE
Me
performs an accessory glide to take up all of the tissue tension with the cephalad hand in a lateral and inferior direction at the humeral head. 3. This is repeated and performed in a rhythmic format when the arm is brought into shoulder abduction.
»5 =)
tat
1. The therapist places the cephalad hand on superior proximal humeral head and the caudad hand on the opposite shoulder. 2. While the patient lifts the arm into shoulder abduction, the therapist
55
»
A
Therapist Position: Standing at the head of the table
BE BREESE me
Patient Position: Supine
oooce
a
— CHAPTER 2Shoulder
EE See
54
Manual Therapy Techniques for the Shoulder
Manual Therapy Techniques tor the Shoulder
57
CHAPTER 2 Shoulder
an ae
_ |
Patient Position: Sidelying
Selfsoft tissue manipulation Patient Position: Sidelying on foam roller
1. The patientis sidelying with the foam roller under the shoulder to be
Bs
|
jest
Therapist Position; Standing at the side of the table behind the patient.
mobilized. on the shoulder adductors. The 2, The patient rolls over the foam roller
patient can hold tension statically or rack back and forth to relax the soft tissues underneath as between Figures B and C
1. The patient is sidelying with the shoulder abducted.
2. The therapist palpates the latissimus dorsi muscle group for limited fascia mobility with the caudad hand facing toward the hips and the cephalad hand pulling the humerus into shoulder abduction. 3, The therapist uses a tissue tension technique to mobilize the fascia, 4, The therapist palpates into the soft tissue and engages the restrictive
barrier with a light force in the direction of tension, sometimes up to i FIGURE 2-40
:
:
3 to 5 minutes. 5. A light pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates.
Notes: The therapist can place a pillow under the thoracic spine to sidebend the patient away to reach the restrictive barrier.
Manual soft tissue manipulation Patient Position: Supine Therapist position: Standing on the side of the table
1, The patient lies supine. 2. The therapist palpates the shoulder adductor and internal rotator muscles and holds deep pressure to relax the muscle. 3. The therapist can perform soft tissue manipulation with gentle
strumming and lateral mobilization of the muscles and tendons, and with circular strokes to increase circulation. 4, This is repeated until the soft tissue relaxes.
FIGURE 2-41
FIGURE 2-41 (CONTINUED)
ball instead of the foam roller. The patient can perform the Notes: A towel can be placed for comfort. The patient can also use a massage knobby tech
as seen in Figure D. nique standing if they have enough shoulder abduction to reach the soft tissues involved
_ LIMITED SHOULDER ABDUCTION
+
56
Shoulder iques ‘Manual Terpy Technforthe mee aeCin 2E Shoulder Adduction Manual Therapy Techniques Patient Position: Seated with the arm supported at the elbowin a ‘neutral position.
:
~ 1, The patient sits with the arm abducted to 90 degrees and places @ mobilization strap around the proximal portion of the humeral head.
« Joint manipulation, non-thrust
© Counterstrain technique
e Joint manipulation, thrust « Muscle energy technique « Mobilization with movement
* Myofascial manipulation
+ Soft tissue manipulation « Self-mobilization
~ 2, The patient abducts the shoulder to the tissue barrier. The patient’
‘thigh then pulls downward on the mobilization strap with the knee or foot to createan inferior humeral glide, 3. The patient continues to increase active shoulder abduction along
witha humeral head inferior glide.
Patient Position: Sidelying atthe side of the table
Therapist Position: Standing on involved side ofthe patient 1. The therapist places the cephalad ha ndon the superior medial
humerus up into the arm pit and the caudal hand on the distal
humerusby the elbow. 2. The therapist steps or leans back to createa distal pull at the shoulder _ joint.
:
;
3. The therapist performs a lateral glide on the humerus with the cephalad hand. At the tissue barrier, the therapist can create a progressive oscillation or a sustained distraction to manipulate the
FIGURE 2-42
shoulder capsule,
FIGURE 2-43
59.
BEEGgGU
CHAPTER2Shoulder
/ Shoulder Adduction: Motion Limitation ©
Patient Position: Supine at the side of the table
an
Therapist Position: Standing on the involved side of the patient
5
aa Het ni
2. The therapist brings the shoulder up to 90 degrees shoulder flexion and steps or leans back to create a lateral pull at the shoulder joint. 3. Atthe tissue barrier, the therapist uses the cephalad hand to take up all of the tissue tension with a posterior and lateral humeral glide. At the barrier, the therapist generates a HVLA thrust gliding the humeral
DOO oooG SS | 2) Ge ee
head laterally and posteriorly.
FIGURE 2-45
i + Joint: Shoulder i
a
dpe of Manipulation: Muse: energyWRC: ' Restricted Motion: Limited shOUides Horizontal
| Adduction bi
at bo
gee at ns eam
ne reid
Sea neal
"ha ST
ho
. The therapist places a mobilization strap around the therapist's waist and around the patient's humerus, as proximal on the humerus as possible, . The therapist brings the shoulder up to 90 degrees of flexion.
iw
. The therapist places the cephalad hand on the elbow and the caudal
=
a
FIGURE 2-46
un
i
I fl f
telah
Patient Position: Supine at the side of the table
|
: \
: aL
Therapist Position: Standing on the involved side of the patient
oe |
Ti Ti ‘a
e
shoulder Adduction Motion Limitation.
=
=Ii
a
:
ia
===
FIGURE 2-44
ecto
‘
i doint Shoulder
1. The therapist places both hands on the proximal humerus.
cat
1. The therapist places the cephalad hand (hypothenar eminence) on the proximal clavicle and the caudal hand around the body and grasping the scapula, 2, The patient grasps the top of the therapist's shoulder with the dysfunctional arm. 3. The therapist steps or leans back to create protraction of the scapula. 4. The therapist performs a posterior glide on the proximal clavicle with the cephalad hand, At the tissue barrier, the therapist can create a progressive oscillation to depress the proximal clavicle.
OOOO OOee
Patient Position: Supine at the side of the table Therapist Position: Standing on the involved side of the patient
EEANNNP NNN TOTO OOOO
. ‘(Flexion), Adduction (Sternoclavicular)
=
and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review. BrJ Sports Med. 2013;47(17):1112- 1119. . Wildeman W, Moesker A, Oerlemans HM, Paassen
and function in participants with secondary carpo-
Choung S$, Kwon 0, Park K, Kim S, Cynn H. Shortterm effects of self-mobilization with a strap on pain and range of motion of the wrist joint in patients with dorsal wrist pain when weight bearing through the hand:
23.
a case series. Man
Patient Position: Seated with the elbows bent
Therapist Position: Seated at the opposite side of the table
Ther. 2013;18(6):568-572.
1, The patient's elbow is placed at 90 degrees of flexion and the wrist in
Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. Sth ed. St. Louis, MO: Saunders/Elsevier; 2013.
the 10 degree of extension.
2. The therapist places a stabilizing strap around the forearm, or the patient can place a shoulder retraction force to meet the wrist traction
force. The mobilizing strap or hand is placed at the first (proximal). carpal row,
3. The therapist or weight/pulley sustains traction in an inferior direction fora general stretch on the wrist; this may take afew seconds to a
few minutes to allow the tissues to elongate.
FIGURE 4-8
2
Se
SS
e
pares
joint. This wane canaiso be Seat with a traction thrust. the Notes: 10 degrees of wrist extension is the loose- saeli position of thesplicarll nese treatmentee orasaey to more BAK Yee neeye a to aa bea nee This Redinique can ceuseful asa sere tec
LIMITED WRIST MOBILITY
116
Manual Therapy Techniques forthe Wrist
118
119
CHAPTER4 Wrist
Type of Manipulation: Joint manipulation,
~ Joint: Wrist Wrist General Motion Limitation
non-thrust
4B
Restricted Motion; Limited Wrist Mobility Patient Position: Seated with the elbow bent Therapist Position: Seated in front of the patient
Wrist Flexion Manual Therapy Techniques « Joint manipulation, non-thrust e Joint manipulation, thrust
* Counterstrain technique
« Muscle energy technique
» Soft tissue manipulation
e Mobilization with movement
= Self-mobilization
e Myofascial manipulation
patient's wrist in all directions along a figure8 pattern assessing and
Wrist General Motion Limitation
non-thrust
Restricted Motion: Limited Wrist Mobility Patient Position: Seated with the forearm resting on the table Therapist Position; Standing or sitting in front of the patient 1. The forearm is resting on the table. 2, The therapist grasps around and stabilizes the distal ulna and radius with the cephalad hand. 3. The therapist uses the caudad hand to interlock the fingers. 4, The therapist compresses the carpal bones and gently glides in all directions along with rotation.
7
Patient Position: Seated, fingers relaxed Therapist Position: Standing on the opposite side of the table of the patient
1. The patient rests the arm on the table with the wrist hanging off on the opposite side. The fingers should be relaxed with any mobilizations to eliminate restrictions fram extrinsic flexors and extensors. The therapist places the cephalad hand just proximal to the stylaid process to stabilize the radiocarpal joint. The caudal hand/mobilizing hand of the therapist is around the proximal carpal row. The therapist distracts with the cephalad hand. 4, Adorsal glide of the proximal (first) carpal row is performed with progressive oscillation at the tissue barrier.
=F
Type of Manipulation: Joint manipulation, . Joint: Wrist
ea
iSSSS5232S5ea5
Notes: This technique can be useful as a general technique for pain relief, ta improve mobility, or as a precursor to more specific treatment techniques.
OOO OOOO
FIGURE 4-9
i
AOA TOO OT ODDO
treating for restricted movement.
Type of Manipulation: Joint manipulation, non-thrust Restricted Motion: Limited Wrist Flexion
Te PEE
FIGURE 4-11
carpal row ina Notes: The therapist can mobilize the distal carpal row by stabilizing the proximal carpal row (midcarpal joi nt} and mobilizing the distal volar (palmar) direction. See Figure B.
In addition, the individual intercarpal joints can be mobilized using intercarpal joint glides:
. Fixate capitate and glide trapezoid, scaphoid, lunate, hamate « Fixate scaphoid and glide trapezoid, trapezium, lunate
. fixate triquetrum and glide lunate, hamate, pisiform
FIGURE4-10 Notes: This technique can be useful as a general technique for pain relief, to improve mobility, or a5 a precursor to more specific treatment techniques,
LIMITED WRIST FLEXION
Joint: Wrist Wrist Flexion Motion Limitation
he
distal carpal row by placing the hypothenar eminence of each hand on both sides of the carpal row, The therapist can interlock the fingers for more control and stability over the carpal row. The therapist creates traction at the wrist and circumducts the
aw
nm
The therapist grasps the patient's hand just distal to the proximal or
a
. The elbow is placed in slight flexion.
Manual Therapy Techniques for the Wrist «121
120. CHAPTER 4Wist
_ Patient Position: Seated ona high table, palm down, fingers relaxed. Therapist Position: | Standing in i front of the patient
Patient Position: Seated at the side of the table, palm up, fingers relaxed Therapist Position: Standing on the same side of the patient’s arm to be treated
1. The therapist places both hands around the aka
1, The patient sits with the elbow bent and palmup. The wrist is just off the edge of the table. 2, The therapist places hands around each side of the patient's hand with thumbs over the proximal carpal row and distracts at the wrist. The
3. The patient isometrically contracts the wrist into extension Gir from the restrictive: barrier) for3 to 5 seconds, meeting the therapist's
force with approximately 5 Ibs of pressure, and then the patient
patient pulls the arm back to meet the traction force of the therapist
completely relaxes. 4. Upon relaxation, the therapistpushes the wrist to the new restrictive barrier of flexion. Thisis repeated until no further relaxation or
or the forearm can be strapped down to the table.
3. The therapist performs a dorsal glide of the distal carpal row to the tissue barrier, :
Sq
FIGURE 4-12
hand with
- thumbs over the carpalbones. 2. The therapist takes up thetissue |tension tothe restrictivebarrier of wrist flexion.
improvement of range of motion into flexion occurs,
4. Atthetissue barrier of the dorsal glide, the therapist creates a high-
velocity low-amplitude (HVLA) thrustin a dorsal direction.
Notes: The technique can also be performed palm down. The therapist can focus on one carpal bone by crossing the thumbs over the carpal bone to
apply a direct force.
FIGURE 4-13 Notes: This technique is useful when significant muscle quarding is present. This technique can be performed with some traction if the patient feels some impingement while going into wrist ee
ca
Manual Therapy Techniques forthe Wrist
123
CHAPTER 4 Wrist Joint: Wrist Wrist Flexion Motion Limitation
Type of Manipulation: Mobilization with
; “Joint: Wrist _ Wrist Flexion Motion Limitation
Type of Manipulation: Counterstrain technique Restricted Motion: Limited Wrist Flexion
movement Patient Position: Seated, fingers relaxed
Restricted Motion: Limited Wrist Flexion
Therapist Position: Seated on the involved side of the patient
Patient Position: Seated with the elbow bent to 90 degrees, fingers relaxed Therapist Position: Seated on the same side of the patient's wrist to be treated
1. The patient is seated with the elbow straight. The therapist palpates the wrist extensor muscles that are hypertonic. 2, The therapist presses into the muscles of discomfort and finds the most hypertonic uncomfortable point. The therapist asks the patient
1, The therapist places the cephalad hand on the proximal carpal row. The caudad hand is placed on the distal ulnar/radius to stabilize the radiocarpal joint. 2. The patient performs wrist flexion, The therapist performs an accessory glide to take up all of the tissue tension of the proximal row ina dorsal direction. 3. This is repeated until there is an increase in wrist flexion.
3. The therapist passively extends the wrist and along with a combination of ulnar and radial deviation, clockwise or counterclockwise rotation Until the palpable point is down to a 2/10 discomfort level. 4. The therapist holds the position for 90 seconds. The therapist does not
to rate the discomfort at-a 10/10.
FIGURE 4-15
need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively straightens out the wrist and rechecks the point in the original position. Ifthe point produces more than 2/10 discomfort the treatment is repeated.
Joint: Wrist Wrist Flexion Motion Limitation
ce
ee
eS el
tension, sometimes up to 3 to 5 minutes. 4. Alight pressure on the barrier is held until the tissue barrier softens
=
ee =
Notes: This can be repeated with the distal carpal row and stabilization of the proximal carpal row (see Figure 8).
1, The therapist places the cephalad hand on the dorsum of the forearm over the wrist extensors and the caudad hand around the wrist. 2. The therapist uses a tissue tension technique to mobilize the fascia. 3. The therapist palpates with the cephalad hand into the soft tissue and engages the restrictive barrier with a light force in the direction of
and relaxes and the myofascial unit elongates.
2
FIGURE 4-14
Type of Manipulation: Myofascial manipulation Restricted Motion: Limited Wrist Flexion Patient Position: Seated Therapist Position: Seated at the opposite side of the table
24
i os
Notes: There are also extensor carpometacarpal and metacarpal phalangeal points.
FIGURE 4-16
can be performed in any Notes: Technique is useful in the presence of myofascial restrictions that contribute to decreased joint mobility. This technique line of tissue tension; most of the focus is parallel to the muscle fibers of the wrist extensors.
LIMITED WRIST FLEXION
122
E
Manual Therapy Techniques forthe Wrist
125
Joint: Wrist _ Wrist Flexion Motion Limitation
Type of Manipulation: Soft tissue manipulation Restricted Motion: Limited Wrist Flexion
Joint: Wrist Wrist Flexion Motion Limitation
rt
cM
Wh iy
Type of Manipulation: Self-mobilization Restricted Motion: Limited Wrist Flexion Patient Position: Seated
Manual soft tissue manipulation
7
(KITS
te
1. The therapist flexes the patient's wrist. 2. The therapist palpates the wrist extensors and holds deep pressure, 3. The therapist can perform soft tissue manipulation with gentle strumming and lateral mobilization of the muscles and tendons, and with circular strokes to increase circulation.
mo
Patient Position: Seated Therapist Position: Standing on the involved side of the patient
utilize their mobilizing thumb on the ventral side of the wrist to create
GAT
“
a dorsal glide on the proximal row carpal bones with the thumb. 4. This can be statically held or rocked further in flexion until the tissue relaxes.
ay
Gta AUT
Self soft tissue manipulation Patient Position: Seated with bodyweight on a foam roller or massage ball 1. The patient places bodyweight with the wrist extensor muscles on the foam roller. 2. The patient can hold statically or rock back and forth to relax the soft tissues. 3. This is repeated until the muscle relaxes.
FIGURE 4-18
peel Bly fe
a
Notes: Can be combined with a muscle energy to facilitate movernent. The technique can be performed at the distal row with proximal row stabilization.
“»
C. (Ai
Tihbe Sai» Cc nh >» :
py
ie
Ce ie» c
iD
aams
c
ell i»
cali FIGURE 4-17
Notes: Technique can also be performed sitting with rolling a can or tennis ball over the wrist extensor musculature (see Figure B and C),
oll c
rg
Cc
@Cc
. The patient is seated with the wrist flexed over the table at the distal radius. _ The patient places the opposite hand of the involved extremity with the thumb on the palmar side. _ Atthe tissue barrier of wrist flexion, the patient rotates the mobilizing hand ina counterclockwise direction to increase wrist flexion and can
iH
-
7”
LIMITED WRIST FLEXION
124 = CHAPTER 4 Wrist
Manual Therapy Techniques forthe Wrist
127
«CHAPTER 4 Wrist
Joint: Wrist
Wrist Extension Motion Limitation
Joint manipulation, non-thrust Joint manipulation, thrust Muscle energy technique Mobilization with movement
Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
patient's wrist to be treated 1, The therapist places hands around the patient’s hand with a finger perpendicular to the patient's wrist at the distal carpal row.
2. The therapist tractions distally and performs a palmar (volar) glide to tissue tension. 3. At the tissue barrier, the therapist can create a HVLA thrust in a palmar
Type of Manipulation: Joint manipulation, non-thrust Restricted Motion: Limited Wrist Extension
direction.
i) ad al
Joint: Wrist: _ Wrist Extension Motion Limitation
« * + *
| Restricted Motion: Limited Wrist Extension Patient Position: Seated at the side of the table, fingers relaxed Therapist Position: Seated/standing on the same side of the
4€ Wrist Extension Manual Therapy Techniques « « « «
"Type of Manipulation: Joint manipulation, thrust
Patient Position: Seated, fingers relaxed Therapist Position: Standing on the opposite side of the table from the patent
Pee
eter)
=
4
restrictions from extrinsic flexors and extensors. . The therapist places the cephalad hand just proximal to the styloid process to stabilize the distal radius at the radiocarpal joint. The caudal hand/mobilizing hand of the therapist is around the proximal carpal row. . The therapist distracts with the cephalad hand, A palmar (volar) glide of the proximal carpal row is performed with progressive oscillation at the tissue barrier.
4
am
ww
~
fingers should be relaxed with any of the mobilizations to eliminate
Ss ey ey es Bs
_ The patient rests the arm on the table with the wrist hanging off on the opposite side or utilizes a mobilization wedae as pictured here. The
eee
Notes: The therapist can mobilize the distal row by grasping the distal carpal row and mobilizing in a palmar glide, In addition, the individual
FIGURE 4-20
intercarpal joints can be mobilized using intercarpal joint glides: - Fixate capitate and glide trapezoid, scaphoid, lunate, hamate - fixate scaphoid and glide trapezoid, trapezium, lunate
Joint: Wrist Wrist Extension Motion Limitation
Type of Manipulation: Muscle energy technique Restricted Motion: Limited Wrist Extension
» Fixate triquetrum and glide lunate, hamate, pisiform Patient Position: Seated with palm down and wrist on the table,
fingers relaxed Therapist Position: Seated/standing on the involved side of the patient
lo
pu
1, The therapist places hands around the patient's hand and wraps thumbs around the wrist . The therapist extends the wrist to the restrictive barrier of extension. . The patient isometrically contracts wrist into flexion (away from the
7
restrictive barrier) for 3 to 5 seconds, meeting the therapist's force
FIGURE 4-21
with approximately 5 Ibs of pressure, and then the patient completely relaxes. . Upon relaxation, the therapist pushes the wrist to the new restrictive barrier of extension. This is repeated until no further relaxation or improvement of range of motion into extension occurs,
‘|
LIMITED WRIST EXTENSION
126
ee
Manual Theropy Techniques forthe Wrist
+129
1. The patient is seated with the elbow flexed. The therapist palpates the wrist flexor muscles that are hypertonic. The therapist presses intothe — muscles of discomfort and finds the most bpstine uncomfortable
wrist to be treated 1. The therapist places thecephalad | hand on the proximal carpal row: The caudad hand is on the distal ulnar/radius to ane the
point. 2, The therapist asks the patient to rate the discomfortat a10/ 10.
radiocarpal joint. 2. The patient performs wrist extension. The therapistcero
3, The therapist passively flexes the elbow and flexes the wrist and compresses the wrist toward the elbow along witha combination of ulnar and radial deviation, clockwise or counterclockwise rotation until the palpable point is down toa 2/10 discomfort level,
an
accessory glideto take up all of the tissue tension of the proximal row
ina palmar (volar) direction. 3. This is repeated until there is an increase in wrist extension.
4. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds, Once the90
FIGURE 4-23
Notes: There are also interphalangeal and interasseous points.
FIGURE 4°22 Notes: This technique can be
eine at ae tba Carpal row withmpc
Carpal row stabilization.
seconds are up, the therapist passively streightens out the legsand rechecks the point in the original position. If the paint produces more than 2/10 discomfort the treatments repeated,
m
Patient Position: Seated with elbow extended, fingers relaxed ‘Therapist Position: poersaei on the same side of the patient's
‘LIMITED WR
PatientPosition:Seated with the bow foal Therapist Position: Standing on the involved side of the|patient
a
fs
128 © CHAPTERAWist
;
IST EXTENS!
of
Manual Therapy Techniques forthe Wrist
131
_ Wrist Extension Motion Limitation
vA i
Type of Manipulation: Myofascial manipulation Restricted Motion: Limited Wrist Extension Patient Position: Seated palm up Therapist Position: Seated on the opposite side of the patient 1. The therapist places the caudad hand around the wrist to stabilize the fascia. The therapist places the cephalad hand on the palmarside of the forearm pointing toward the elbow, 2. The therapist uses a tissue tension technique to mobilize the fascia.
Joint: Wrist Wrist Extension. Motion Limitation.
| Type of Manipulation: Soft tissue manipulation Restricted Motion: Limited Wrist Extension Manual soft tissue manipulation Patient Position: Supine Therapist Position: Standing on the involved side of the patient 1, The patient lies supine. 2. The therapist extends the wrist. 3. The therapist palpates the wrist flexors and holds deep pressure.
4. The therapist can perform soft tissue manipulation with gentle
3. The therapist palpates into the soft tissue and engages the restrictive
strumming and lateral mobilization of the muscles and tendons, and with circular strokes to increase circulation.
barrier with ¢ light force in the direction of tension, sometimes up to
3 to 5 minutes. 4. A light pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates. Self soft tissue manipulation Patient Position: Seated with weight on the forearm palm down on a foam roller or massage ball 1. The patient places bodyweight on the foam roller.
2. The patient can hold statically or rock back and forth to relax the soft
TSI
tissues of the wrist flexor muscles. 3. This is repeated until the muscle relaxes.
iit a a
a
Notes: A fascial technique can be performed over the carpal tunnel (Figure B)
‘ll
Te
aa
A
YUVIVITI STITT
FIGURE 4-24
L
A ri]
nine
ij li rl ’
mee. ui
iti. rs Pa |
pith
FIGURE 4-25
LIMITED WRIST EXTENSION
Joint: Wrist
SiS SoS
CHAPTER 4 Wiist
E
130
Manual Therapy Techniques forthe Wrist
133
©6CHAPTER 4 Wrist
eof
Restrict
nipulation: Sel
d Motion:
moblizetion
a
TMU ele elect) 1
ar
imited Wrist Extension
4D Ulnar Deviation Manual Therapy Techniques * Joint manipulation, non-thrust * Joint manipulation, thrust e Muscle energy technique + Mobilization with movement
Patient Position: Quadruped 1, The patient is in the quadruped position. 2, The patient places arms directly under the shoulders. 3. The patient shifts bodyweight over the wrists into wrist extension until tissue barrier is met. The patient can hold tension statically
or rock the wrist into extension by getting an increased forward Movement of bodyweight.
eT wi i ik (MN
e e eo iM! ap e jail e caored om AT
« + ¢ «
Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
Joint: Wrist it Wrist Ulnar Deviation Motion Limitation
(MTs,
Patient Position: Seated
Therapist Position: Standing at the side of the patient 1, The patient's wrist is placed in slight ulnar deviation on a mobilization
wedge. 2. The therapist places the cephalad hand around the distal ulnar radius and the caudad hand on the proximal carpal row. 3. The therapist distracts the wrist joint. 4. Atthe tissue barrier of ulnar deviation, the therapist can createa
oe
Cc, of a “»
progressive oscillation in a radial glide direction at the tissue barrier.
sil
FIGURE 4:27 Notes: The eanele cana peta the same eal
FIGU RE 4°26
_ Joint: Wrist Wrist Ulnar Deviation Motion. Limitation
Notes: The ear and or distal carpal row is tea mobilized in a ahimar sidedfiettoi This technique can also be performed standing resting the wrist on a table with elbows straight and rocking bodyweight over the wrist. This technique can also be performed in the Phalen’s test position (Figure B) by dropping elbows to increase wrist extension, When the fingers are see ee extrinsic flexors will have tissue tieet notalewing) the wrist to fully ae
on the distal row Bestabilizimg the pom imal row and a
ane Z pa TOW.
Type of Manipulation: Joint manipulation,
SE
} Restricted Motion: Limited Wrist Ulnar Deviation Patient Position: Seated at the side of the table Therapist Position: Standing on the involved side of the patient 1. Patient sits with the elbow extended.
2, The therapist stabilizes one of the carpal bones with both thumbs crossed over the fingers surrounding the wrist. 3. The therapist places traction at the wrist and ulnarly deviates to tissue tension, 4. Atthe tissue barrier, the therapist creates a HVLA thrust in a radial direction.
es
FIGURE 4-28
Notes: Thrust technique can be useful to address joint restrictions that do not respond to the application of non-thrust techniques.
LIMITED WRIST ULNAR DEVIATION
132
Manual Therapy Techniques forthe Wrist
135
CHAPTER4 Wrist
» Joint: Wrist —
o
Wrist Ulnar Deviation Motion Limitation
:
Joint: Wrist
Type of Manipulation: Muscle energy technique ‘|
Wrist Ulnar Deviation Motion Limitation
| Type ofManipulation: Counterstrain technique '
Restricted Motion: Limited Wrist Ulnar Deviation
Restricted Motion: Limited Wrist Ulnar Deviation Patient Position: Seated Therapist Position: Seated on the involved side of the patient
a
FIGURE 4-29
1, The therapist palpates the flexor and extensor carpi radialis. 2. The therapist presses into the muscles/ligaments of discomfort and finds the most hypertonic uncomfortable point. The therapist asks the patient to rate the discomfort ata 10/10. . The therapist passively flexes the elbow and radially deviates the wrist with pronation or supination until the palpable point is dawn to a 2/10 discomfort level. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively straightens out the arm and
. The therapist places the cephalad hand on the proximal carpal row and the cephalad hand on the distal ulnar and radius. The therapist distracts the wrist and ulnarly deviates the wrist to the restrictive barrier, The patient isometrically contracts the wrist into radial deviation (away from the restrictive barrier) for 3 to 5 seconds, meeting the therapist's force with 5 Ibs of pressure, and then the patient completely relaxes. . Upon relaxation, the therapist glides the talus medially and takes up the additional tissue slack to the new restrictive barrier. This is repeated until no further relaxation or improvement of range of motion into ulnar deviation occurs.
=
ha
Mm
Patient Position: Seated Therapist Position: Seated across the table from the patient
rechecks the point in the original position. If the point produces more
than 2/10 discomfort the treatment is repeated.
. The therapist places the cephalad hand around the palm of the hand.
cee}
mw
The caudad hand is placed with the webspace in a C shape around the
ulnar side of the wrist at the carpal bones. . As the patient actively ulnarly deviates the wrist, the therapist performs a radial accessory alide of the carpal bones (proximal or distal row) to take up all of the tissue tension. . Thisis repeated each time the patient actively ulnarly deviates the wrist,
FIGURE 4-30
Notes: Do not incude thumb in the grasp; the thumb is often painful for patients (also true of mobilization techniques for all of ulnar and radial deviation).
a eae
Patient Position: Seated Therapist Position: Seated
eh
Type of Manipulation: Mobilization with movement Restricted Motion: Limited Wrist Ulnar Deviation
a
Joint: Wrist ' Wrist Ulnar Deviation Motion Limitation
z
Notes: This technique is useful when joint glides are painful or significant muscle quarding is present.
FIGURE 4-31
Notes: This technique can be useful in the presence of muscle hypertonicity or myofascial restrictions.
~
LIMITED WRIST ULNAR DEVIATION
134
Manual Therapy Techniques forthe Wrist
;i aos JS SU S
CHAPTER 4 Wast
sal
ot
Patient Position: Seated Therapist Position: Seated on the involved side of the patient
we
la
. The therapist places the cephalad hand around the four fingers. The therapist places the caudad hand around the carpal bones with the thumb up along the carpal bones. . The therapist passively ulnarly deviates the patient's wrist.
fe
ms
- Patient places the hand palm up.
. At the tissue barrier, the therapist uses a tissue tension technique to
mobilize the fascia over the carpal bones in a radial direction of tissue tension. 5. The force is held until the tissue relaxes and the fascia elongates.
Type of Manipulation: Soft tissue manipulation
Wrist Ulnar Deviation Motion Limitation
Restricted Motion: Limited Wrist Ulnar Deviation
Manual soft tissue manipulation Patient Position: Seated Therapist Position: Seated on the involved side of the patient
1. The patient relaxes the wrist into slight ulnar deviation. 2. The therapist palpates the flexor or extensor carpi radialis muscle and holds deep pressure. 3. The therapist can perform soft tissue manipulation with gentle
ls,
9,
strumming and lateral mobilization of the muscles and tendons, and with circular strokes to increase circulation.
ba
Cg
= |
“s ~
fia iA a
*» *)
G
p 4 a
*
Cor FT
7
Cy
by
ar
Self soft tissue manipulation Patient Position: Seated 1. The patient places the hand on the flexor or extensor carpi radialis
musde, 2.
; G
Pa
\
yy
G
(Aili+y
teal ssues
. hold staticallyor rock back and forth to relax the soft
3. This is repeated until the soft tissue relaxes.
Cis
FIGURE 4-32
Notes: This technique can be performed on the dorsal (Figure A) or palmar (Figure B) side of the wrist.
Cc
aa»
Cc
wa
roi eet o
ve -*»
eT
o aa) Cc
rae
aii
Y
etki c a mie
”
e rie ” Cc
ih ne
"
FIGURE 4-33
|
;
Notes: The patient can rolla massage ball between the muscle and the person's body as an alternate technique (Figure C)
LIMITED WRIST ULNAR DEVIATION
Restricted Motion: Limited Wrist Ulnar Deviation
Joint: Wrist
=
_ Wrist Uinar Deviation Motion Limitation
Type of Manipulation: Myofascial manipulation
1.
;
Nad = cl1: —-—=
_ Joint: Wrist
a
|
La
=
“4
|
136
137
Manual Therapy Techniques forthe Wrst
138 CHAPTER 4Wist
Wrist Radial Deviation ¢
ae
139
oth The patient grasps the hand just proximal tothe thumb to be mobilized with the opposite hand with the thumb around the ulnar side of the carpal bones. 2. The patient ulnarly deviates the wrist until the tissue barrier is met.
~ ——
_
=
Radial Deviation Manual Therapy Techniques « Joint manipulation, non-thrust
« Joint manipulation, thrust « Muscle energy technique « Mobilization with movement
+ « + e
Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
/
"
:
3. The patient can hold tension statically or rock the wrist into ulnar ~ deviation by getting an increased radial glide on the proximal or distal carpal row.
Patient Position: Seated Therapist Position: Seated at the side ofthe patient 1. The patient's wrist is placed in slight radial deviation over a bolsteror
at the edge of the table. 2. The therapist places the cephalad hand around the distal ulnar radius and the caudad hand on the proximal carpal row. 3, The therapist distracts the wrist joint. 4. Atthe tissue barrier of radial deviation, the therapist cancreate a progressive oscillation in an ulnar glide direction at the tissue barrier. —
hc PGR
Sa
a
rare
Notes: The therapist can Prom the same technique on the
FIGURE434 0
Sees
eh
Notes: Patient can use a muscle energy vednicue tovaltate movement. The patient can also ani the self-mobilization holding onon to a wood stick and using the opposite arm to pull the wrist downward into ulnar deviation (Figures B and C). The patient can also rest his or her hand on the knee or
table with a theraband pulling the wrist toward the floor (Figure 0),
i
aE
A row by stabilizing the proximal row and ulnarly gliding the distal row.
LIMITED WRIST RADIAL DEVIATION
‘,
4E
Patient Position: Seated
Manual Therapy Techniques forthe West
141
CHAPTER 4 Wrist
Restricted Motion: im ited wrist Radial Deviation a Patient Position: Seated Therapist Position: Seated next to the patient
Patient Position: Seated at the side of the table Therapist Position: Standing on the involved side of the patient
. The therapist places the cephalad hand on the proximal or distal carpal bones and the caudal hand stabilizing the distal ulna and
1, The patient is seated with the elbow extended. hm
2. The therapist stabilizes one of the carpal bones with both thumbs crossed over with the fingers surrounding the wrist. 3. The therapist places traction at the wrist and radially deviates to tissue tension. 4. At the tissue barrier, the therapist creates a HVLA thrust in an ulnar
radius. _ The therapist distracts the wrist and radially deviates the wristto the restrictive barrier.
. The patient isometrically contracts the wrist into ulnar deviation
om
a
direction.
FIGURE 4- 37
(away from the barrier) for 3 ta S seconds with approximately 5 lbs of pressure and then the patient completely relaxes. _ Upon relaxation, the therapist radially deviates the carpal bones ta new restrictive barrier of wrist radial deviation. This is repeated until no further relaxation or improvement of range of motion into radial deviation occurs.
Notes: This techniqueis useful when joint glides are painful or significant muscle quarding is present.
Joint; Wrist Wrist Radial Deviation Motion Limitation
j Type a Manipu lation: Mobilization with _ movement =A i Restricted Motion: Limited Wrst RadialDeviation 4 Patient Position: Seated with the forearm in neutral thumb up Therapist Position: Standing 1. The therapist places the cephalad hand around the distal ulnar and
radius to stabilize. The therapist places the caudad hand over the proximal carpal row with the wrist off a mobilization wedge or edge of the table just at the proximal row. 2. The patient actively radially deviates the wrist, the therapist distracts
FIGURE4-36
Notes: Thrust technique can be useful to address joint restrictions that do nat respond to the cae ofnon-thrust Shnie The cite can also be performed with the wrist in neutral with the thumb up. The therapist would place both hands around the patient's wrist with the therapist's thumbs on the radial side of the wrist to perform a traction radial whip (traction to the fingers and radial deviation with the mobilizing thumbs from the radial side of the taba bones ioe Be
the wrist joint and performs an ulnar accessory glide of the proximal carpal row to take up all of the tissue tension. 3. This is repeated each time the patient actively radially deviates the wrist.
FIGURE 4-38 Notes: Technique is useful in the presence of muscle quarding or hypertonicity.
LIMITED WRIST RADIAL DEVIATION
140
Manual Therapy Techniques forthe Wrst
143
CHAPTER 4Wiist
“dointe wit Manual soft tissue manipulation Patient Position: Seated Therapist Position: Seated on the involved side of the patient
Patient Position: Seated
Therapist Position: Standing on the involved side of the patient
1, The therapist palpates the radial side of the pisiform (inferiorly) for the
1. The patient relaxes the wrist into slight ulnar deviation 2, The therapist palpates the flexor or extensor carpi ulnaris tendon and
wrist muscles that ulnarly deviate (extensor and flexor carpi ulnaris).
The therapist presses into the muscle of discomfort and finds the most
holds deep pressure.
mS
hypertonic uncomfortable point. The therapist asks the patient to rate the discomfort at a 10/10.
3, The therapist can perform soft tissue manipulation with gentle strumming and lateral mobilization of the muscles and tendons, and
The therapist passively ulnarly deviates the wrist with flexion and extension until the palpable point is down to a 2/10 discomfort level.
with circular strokes to increase circulation.
ta
. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds. 4. Once the 90 seconds are up, the therapist passively brings the wrist
FIGURE 4-39
to neutral and rechecks the point in the original position. If the point produces more than 2/10 discomfort the treatment is repeated.
Self soft tissue manipulation Patient Position: Seated
Notes: This technique is useful when joint glides are painful or significant muscle quarding is present,
1. The patient places a hand on the flexor or extensor carpi ulnaris
muscle, 2. The patient can hold statically or rock back and forth to relax the soft tissues 3, This is repeated until the soft tissue relaxes.
| Type of Manipulation: Myofascial manipulation __ Restricted Motion: Limited Wrist Radial Deviation Patient Position: Seated Therapist Position: Seated/standing on the involved side of the patient 1, Patient places hand in neutral, 2. The therapist places the cephalad hand around the four fingers. The therapist places the caudad hand around the carpal bones with
thumb up along the carpal bones. 3, The therapist passively radially deviates the patient's wrist. 4. Atthe tissue barrier, the therapist uses a tissue tension technique to mobilize the fascia over the carpal bones in an ulnar direction of tissue tension.
5, The force ts held until the tissue relaxes and the fascia elongates.
FIGURE 4-40 _ Notes: This technique can be performed on the dorsal or palmar side of the wrist. For all of the techniques with the palm up you may want to perform ina wrist neutral or supinated position depending on the motion. Supination is often painful and limited after Many wrist injuries because of the tension placed on the ulna and TFCC.
FIGURE 4-41
Ea celal
LIMITED WRIST RADIAL DEVIATION
(142
=
ie
qa ata
144 CHAPTEA Vist R
Hand and Patient Position: Opposite hand grasping around the hand
Fingers
1, The patient grasps the hand tobe mobilized with the opposite hand.
The mobilizing hands grasps around the fingers:with the thumb at the radial side of the carpal bones,”
2. The patient radially deviates the wrist ‘by performing a counterclockwise direction of force until tissue barrier is met. 3, The patient can hold tension statically or rock the wristinto rad ial deviation by getting an increased ulnar glide on the carpal bones,
ca
:
go pen
Chapter Outline
: af 2 inp aim
Discussion of the hand/finger/thumb joint biomechanics and related manual peop including a case study.
INTRODUCTION information — deka
TECHNIQUES - Muscle energy technique + Mobilization with movement
5B Finger and Thumb Flexion Manual
- Counterstrain technique
: Joint manipulation, non-thrust
+ Myofascial manipulation - Soft tissue manipulation
+ Joint manipulation,thrust - Muscle energy technique
Therapy Techniques + Joint manipulation, non-thrust
+ Joint manipulation, thrust
- Muscle energy technique
- Mobilization with movement » Counterstrain technique - Myofascial manipulation
+ Soft tissue manipulation = Self-mobilization 5€ Finger and Thumb Extension
Manual Therapy Techniques FIGURE 4-42
5E Finger and Thumb Adduction
5A Finger and Thumb General Manual Therapy Techniques
- Joint manipulation, non-thrust + Joint manipulation, thrust
+ Self-mobilization 5D Finger and Thumb Abduction
Manual Therapy Techniques + Joint manipulation, non-thrust Joint manipulation, thrust - Muscle energy technique Mobilization with movement + Counterstrain technique
Manual Therapy Techniques
+ Mobilization with movement * Counterstra in technique
+ Myofascial manipulation .
Soft tissue manipulation
‘Self-mobilization
Myofascial manipulation « Soft tissue manipulation + Self-mobilization
Notes: Patient can incorporate a hold-telax hela into this mobilization, This incl ue can also be performed with elastic band ora towel creating the gobi 1force ina rl pice = o B).
LEARNING OBJECTIVES Upon completion of this chapter, the reader will be able to: + Describe the anatomy and biomechanics of the joints of the hand
- Understand the state of the evidence for the use of manual therapy treatment techniques of the hand complex + Perform the 8 types of techniques for each of the directions of joint motion restriction + Delineate the basic steps for the application of each type of technique
ae af
- Inoducton VA closely resemble each other in size and is very Longitudinal _ iy
and consists of 19 bones that form 19 from p
1t
e
arch
limited in mobilityin abduction/adduction and
—_Distal
axial rotation.?* The MCP joints are stabilized by
transverse arch
radial and ulnar collateral ligaments and by the volar plate. The volar plate provides for increased
ints for each digit
joint stability and is composed of fibrocartilage that is attached to the base of the phalanx and
are the carpometacarpal
(CMC) joints, the metacarpophalangeal (MCP)
proximally blends into the volar joint capsule. The volar plates are connected to each other via
_ joints, the proximal interphalangeal (PIP) joints, r tal interphalangeal (DIP) joints, with
the deep transverse ligament. The volar plate limits hyperextension of the digit, reinforces the
ing only an interphalangeal (IP) 1-3
_
volar side of the joint capsule, and prevents the long flexor tendons from being pinched between
The CMC joints form the relatively immobile
_ proximal transverse arch of the hand, the MCP
joints contribute to the mobile distal transverse
the MCP joint surfaces. The capsule of the MCP
FIGURE5-3 The joint surfaces of the CMC | joint
arch, and the MCP, PIP, and DIP joints form the
_ longitudinal arch of the hand (see MGTUi#22). __ The carpometacarpal joints of the fingers _ are composed of the distal joint surfaces of the bones of the distal row of the wrist and the bases
of the second through fifth metacarpal bones. The second MCP joint is an articulation of the second metacarpal bone with primarily the trapezoid and secondarily the trapezium and capi-
tate bones. The third MCP joint is composed of the third metacarpal and the capitate, and the fourth MCP joint consists of the fourth metacarpal and the capitate and hamate. The fifth MCP joint consists of the fifth metacarpal and the hamate. Each of the second through fifth
metacarpals also articulates with the others at
FIGURE 5-2. The transverse and longitudinal arches of the hand
the first metacarpal is accompanied by a glide
their bases.** The CMC joints of the fingers are supported by volar and dorsal longitudinal and transverse ligaments. The deep transverse metacarpal ligament connects the bases of the second through fourth metacarpals and prevents abduc-
tion of the CMC joints. The second through fourth CMC joints are plane synovial joints with 1 degree of freedom in flexion and extension. The second and third CMC joints have little
motion. The fifth CMC joint has a saddle shape, allowing for abduction/adduction in addition to
flexion/extension, thus allowing for the combination motion of opposition.*? The CMC joint of the thumb
(CMC J) is com-
posed of the trapezium and the first metacarpal. The joint is a saddle joint with 2 degrees of freedom in flexion/extension and abduction/
/—
Metacarpals
Hamate
CMC joints
(Capitate
Trapezium
Triquetral
Trapezoid
Lunate
Scaphoid Radius
adduction. These motions, with addition of axial rotation, form the combination motion of opposition. The CMC] joint surfaces of the trapezium are concave in the sagittal plane and convex in the frontal plane. Flexion/extension of the MCP I joint occurs in a plane almost parallel to the palm around an anteroposterior axis that is somewhat oblique, while abduction/adduction occurs in plane almost
perpendicular
somewhat oblique also referred to as As a result of the and the shape of
to
the
palm,
around
a
coronal axis.? This motion is palmar abduction/adduction. orientation of the trapezium the joint surfaces, flexion/
extension of the first metacarpal is accompanied
by a glide of the metacarpal joint surface in the FIGURES-1 Joints of the hand
same direction, whereas abduction/adduction of
of the metacarpal joint surface in the opposite direction.?* Available motion at the CMC I joint is approximately 50 degrees in flexion/extension, 40
degrees
in
(palmar)
abduction/adduction,
and 15 degrees of axial rotation.**° The CMC I joint has a relatively lax joint capsule (allowing for axial rotation) and is primarily supported by the dorsoradial oblique and anterior oblique ligaments.? The loose-packed position of the joint is in the neutral position between the motions in both planes, and the closed-packed position is in full abduction and adduction. The metacarpophalangeal (MCP) joints of the fingers are composed of the relatively large convex distal joint surface of the metacarpal head and the relatively small joint concave surface on
base of the proximal phalanx (see MTaGE2m) .
The joint is a condyloid synovial joint that has 2 degrees of freedom in flexion/extension and abduction/adduction. Axial rotation of the MCP
when
II-IV joints can occur in extension,
the joint capsule is relatively slack. The MCP
joint of the thumb has joint surfaces that more
joint of the thumb is reinforced by two sesamin flexion/ oid bones. Mobility of the MCP joints
extension increases from the radial joints to the
ulnar joints: the MCP II joint has approximately
90 degrees
of flexion,
phalanx
1
es —
Extensor
tendon .
the MCP
Each IP joint is a synovial hinge joint with 1
cave surface. The joint capsule in reinforced by
a volar plate and an ulnar and radial collateral Joint capsule
Metacarpal
oe Fee _
ae Stee i
:
ce oo ENT
yi
Fibrocartilaginous
Collateral Ulnar’
Palmarplate
ligament collateral
Proximal interphalangeal joint
ligament
FIGURE 5-4 The metacarpophalangeal joint
IV
degree of freedom in flexion/extension. Similar to the surface of MCP joints, the convex proximal joint surface is larger than the distal con-
Distal interphalangeal Proximal
whereas
joint has approximately 120 degrees of flexion, allowing for optimal grip on objects held in the palm. Maximal abduction/adduction occurs in extension.2» The closed-packed position is full (hyper) extension, and the loose-packed position is in slight flexion. The capsular pattern of the MCP joint is limitation in all directions, with flexion most limited.‘ The proximal and distal interphalangeal (PIP and DIP) joints of the fingers and the interphalangeal (IP) joint of the thumb consist of the convex distal head of the proximal phalanx and the concave base of the distal phalanx (see
FIGURES-5 The interphalangeal joints
Collateral ligament
—
a.
148 CHAPTERS Handandrges ] _ Sion
adie
_to the
vailable ROM in flexion/extenincreases of the IP joints increases from the of the hand to the ulnar side, similar MCP
Distal joint
joints, with the total available range
Lateral slip
increasing from 100 degrees at the PIP II joint
_ to 135 degrees at the PIP V joint and from 80
- Proximal joint
' degrees at the PIP II joint to 90 degrees at the _ PIPV joint.? The loose-packed position of the
Central slip
_ interphalangeal joint is in slight flexion, and __ the closed-packed position is in full extension.
The capsular pattern is more restricted in flex-
_ ton than extension.*° _
The extrinsic finger flexors include the flexor
Interossel muscles
digitorum profundus and superficialis. The latter flexes the PIP and MCP joints, whereas the
Extensor
profundus, due to its insertion on the base of the distal phalanx, also flexes the DIP joints. The individual tendons of the finger flexors pass
under the flexor retinaculum and through the carpal tunnel under the transverse carpal ligament. The tendons are enveloped in tendon sheaths, and friction between the tendons
and
the surrounding structures is further decreased by the ulnar and radial bursae. Past the meta-
carpus, the flexor tendons are stabilized by 5 annular pulleys (A1-AS) (see BGI@#2H), with
the A2 and 4 pulleys preventing bowstringing between the joints and the Al, 3, and 5 pulleys
stabilizing the tendons at the level of the MCP, PIP, and DIP joints, respectively. The Al pulley
is most commonly involved in the development of trigger finger.’> The extrinsic muscles of the hand are described in Chapter 4. The extrinsic finger extensors include the extensor digitorum communis,
indices proprius,
Collateral ligament J
Proximal
DIP. PIP
Middle
joint
Distal phalanx
_
FIGURE5-7
Palmar view
tendon
The extensor tendon mechanism
and digiti minimi. The tendons of these muscles pass under the extensor retinaculum and merge with the dorsal hood at the level of the MCP joints. The central tendon portion inserts on the base of the proximal phalanx, and the terminal tendon inserts on the base of the distal phalanx
(see The intrinsic finger muscles include the dorsal and volar interossei muscles, and the lum-
bricals
(see MEQGUTEFI).
There
are 4 dorsal
interossei and 3 volar interossei (the fourth volar
interossei is most commonly named separately as the flexor polices brevis), arising from the sides of the metacarpal joints and inserting on the extensor mechanism at the proximal phalanx
and the extensor hood, with other fibers attach-
ing more distally to the lateral bands and the central tendon. The interossei can contribute to finger flexion at the MCP joints and extension at the IP joints. With the MCP joints in extension, the dorsal interossei can produce abduction at the MCP
joints and the volar interossei can produce MCP adduction.?? The lubrical muscles originate from the flexor digitorum tendons in the palm and insert on the radial sides of the lateral bands of the extensor mechanism. The lumbricals produce
MCP flexion and IP extension. Annular pulleys: A1, A2, A3, A4,. AS Cruciform pulleys: CO, C1, C2, C3
FIGURE5-6
The flexor tendon pulley system
The extrinsic thumb muscles include the flexor pollicis longus, the extensor pollicis longus, the extensor pollicis brevis, and the abductor pollicis
longus. The flexor pollicis longus tendon runs in between the two sesamoid bones and inserts
FIGURE5-8
Intrinsic hand muscles
on the base of the distal phalanx.
The extensor
pollicis longus crosses the wrist ulnarly to the extensor pollicis brevis and abductor longus and pulleys around Lister’s tubercle to the base of the distal phalanx. The extensor pollicis brevis inserts on the base of the proximal phalanx, allowing it to function as an extensor of the MCP I joint, and the abductor pollicis longus inserts on the base of the MCP | joint. Both muscles can
abduct the CMC I joint.'? The 5 intrinsic thumb muscles all originate from the carpal bones and the flexor retinaculum. These muscles include the abductor pollicis brevis, adductor pollicis, flexor pollicis brevis, and the first volar interosseus muscles, all of which insert on the base of the proximal phalanx, and
professionals such as physical therapists.” Other common pathologies include carpal tunnel syndrome, tendon pathologies such as De Quervain’s syndrome,* MCP joint dysfunction secondary to rheumatoid arthritis, and trauma. There is limited evidence available regarding the effectiveness of manual therapy interventions in the hand. A recent systematic review’ identified only two studies examining effectiveness of joint mobilization. One low-quality study examined the effectiveness of joint glides and traction to treat postfracture stiffness of the MCP joints
and found that significant short-term improvements in range of motion (ROM)
were achieved
the opponens pollicis, which inserts on the first
metacarpal (see Miiaie=m).
The hypothenar intrinsic muscles include the abductor digiti minimi, originating from the pisiform and inserting on the base of the fifth proximal phalanx, and the opponens digiti minimi and flexor digiti minimi, both originating from the hook of the hamate and the flexor retinaculum and inserting at the medial border of the fifth metacarpal (see Figure 5-9).'
Common pathologies of the hand include osteoarthritis of the joints, especially of the
the CMC | joint and the DIP and PIP joints of finger. Involvement of the CMC I joint is especially common in professions that require fre-
quent use of the hands,
including
healthcare
Opponens
digiti minimi
oi
Flexor pollicis brevis
Abductor digiti minimi brevis
Flexor digiti minimi brevis
‘
ga
7
:
me
Abductor pollicis brevis
Opponens
pollicis
FIGURES-9 The thenar and hypothenar intrinsic muscles
References 151
Srs and Finge HandR' ——'150. CHAPTE compared to a control group. Another study found that Kaltenborn A-P joint glides were ective to decrease pain in patients with CMC
joint pain. A recent survey found that manual _ therapy is routinely used in the management of
_ CMC dysfunction.” A study by Villafaiie et al." found preliminary evidence that joint mobiliza-
tion of more proximal upper extremity joints, _ including the wrist, elbow, and shoulder, may be effective in decreasing pain and increasing func-
tion in patients with secondary osteoarthritis
of CMC joints. A recent randomized controlled ‘tial found that a combination of joint mobili-
found
to be effective for the
treatment
of De
Quervain’s tenosynovitis in a single case study.® Proximal sources of hand pain and dysfunction need to be considered when examining and treating patients with hand pain.” Hand and wrist pain can result from a number of pathologies outside the anatomical area of the wrist, including cervical/thoracic radiculopathy, tho-
racic outlet syndrome,
lesions of the brachial
plexus, upper extremity nerve entrapments, etc.
more effective than sham treatment for pain in
Therefore, the entire upper quarter, including the cervical and upper thoracic spine, needs to be examined and if needed, treated as part of the patient/client management of people with hand pain and dysfunction.
there was a limited
effect for functional improve-
ment." There is emerging evidence that manual therapy may be effective in the treatment
CASE STUDY A 52-year-old female presents with right hand thumb pain. The patient states she works in an assembly line manufacturing small toys. When she works for longer than 30 minutes she is feeling pain at the base
_ of her thumb. She has not had any trauma. Pertinent medical history: osteoarthritis and atrial fibrillation. Physical therapy assessment findings include tenderness at the carpometacarpal joint on palpation, Thumb abduction and flexion active and passive range of motion is painful at end range, and palmar and ulnar direction CMC joint glides are painful in end range and restricted. Pinch and grip strength is
decreased. Upper quadrant testing is negative and the cervical spine tests are negative, and sensation testing is normal. X-ray results of the hand were negative for fracture. CMC joint space was decreased.
Questions: + What changes to the joint are anticipated with osteoarthritis? + +
What is the roll and glide direction of the CMC with thumb abduction? Whatis the roll and glide direction of the CMC with thumb flexion?
*
{sthe joint injury acute, subacute, or chronic? Describe why.
+»
How would
that information direct your joint manipulation intervention?
f
and exercise was
patients with osteoarthritis of the CMC joint, but
tive carpometacarpal osteoarthritis and found that manual therapy and exercise are an effective means of improving pain and function at short-term follow-up by patients with thumb CMC. osteoarthritis.
zation.**"'* Mobilization with movement was L
Key Terms Capsular pattern metacarpophalangeal (MCP) joints: Limitation in all directions, with flexion
most limited. Capsular pattern proximal and distal interphalangeal (PIP and DIP) joints: More restriction in flexion than extension.
Carpometacarpal (CMC) I joint: Saddle joint with 2 degrees of freedom in flexion/extension and abduction/adduction, composed
(CMC)
II-V
joints:
Com-
posed of the distal joint surfaces of the bones of the distal row of the wrist and the bases of the second through fifth metacarpal bones. The second through fourth CMC joints are plane synovial joints with 1 degree of freedom in flexion and extension. The second and third CMC joints have little motion. The fifth CMC joint has a saddle shape, allowing for abduction/adduction in
addition to flexion/extension, thus allowing for
the combination motion of opposition.
|
Closed-packed position metacarpophalangeal (MCP) joints: Full (hyper) extension.
Closed-packed position proximal and distal interphalangeal extension.
(PIP
and
DIP)
joints: Full
Loose-packed position carpometacarpal (CMC) I joint: Neutral position between the motions in both planes. Loose-packed position metacarpophalangeal (MCP) joints: Slight flexion.
Loose-packed position proximal and distal interphalangeal (PIP and DIP) joints: Slight flexion. Metacarpophalangeal (MCP) joint: A condyloid synovial joint, composed of the relatively large convex distal joint surface of the metacarpal head and the relatively small joint concave surface on base of the proximal phalanx, with 2 degrees of freedom in flexion/extension and abduction/adduction. Proximal and distal interphalangeal (PIP and DIP) joints: Synovial hinge joint with 1 degree
of freedom in flexion/extension, the convex proximal joint surface is larger than the distal concave surface.
carpometacarpal Closed-packed _ position adduction. and n abductio (CMC) I joint: Full
References 1.
Per the available evidence, non-thrust joint manipulation of CMC should be considered to decrease
pain and increase mobility and function. MWM should also be considered. The following studies may provide evidence for the selection of these techniques: + Villafane etal.’ investigated effects of central sensitization in patients with CMC arthritis and found that performing unilateral Kaltenborn mobilizations (posterior to anterior glides) exhibited bilateral effects in the increase of contralateral pressure pain thresholds, tip pinch strength, and tripod grip strength. + Villafane et al.’? investigated effects of a mobilization with movement in combination of tape support in the management of trapeziometacarpal osteoarthritis in a case study and found that 12
of the tra-
pezium and the first metacarpal. CMC I joint surfaces of the trapezium are concave in the sagittal plane and convex in the frontal plane.
Carpometacarpal
eed
zation, neural mobilization,
s the treatment of conserva+ _Bertozzi et al2° performed a systematic review and meta-analysiin
of joint glides, neural mobilization, and manual and instrument-assisted soft tissue mobili-
eee eee
ek
weekly sessions significantly reduced subjective pain reports and resulted in considerable improvement in functional and occupational task.
of carpal tunnel syndrome, including the use
2,
3, 4,
Moore
KL, Agur AMR,
Dalley AF. Clinically Oriented
Anatomy. 7th ed, Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2013. Levangie PK, Norkin CC. Joint Structure and Function: A Comprehensive Analysis. Sth ed. Philadelphia, PA: F, A. Davis Co; 2011. Duncan SFM, Saracevic CE, Kakinoki R. Biomechanics of the hand. Hand Clin, 2013;29(4):483-492. Su F, Lin C, Wang C, et al. In vivo analysis of traduring arthrokinematics joint peziometacarpal motions. Clin Biomech. multi-directional thumb 2014;29(9):1009-1015.
Magee DJ. Orthopedic Physical Assessment. 6th ed. St. Louis, MO: Saunders Elsevier; 2014. 6. Cyriax JH. Textbook of Orthopaedic Medicine: Diagnosis of Soft Tissue Lesions. (Vol 1, 7th ed.). London, England: Balliére Tindall; 1978. 7. Atkinson BW, Maher T. Thumb pain in physiotherapists: Biomechanical causes of pain and alternate methods of preventing distress in treatment. J Man Manip Ther. 2004;12(4):187-191. §. Backstrom KM. Mobilization with movement as an adjunct intervention in a patient with complicated De Quervain’s tenosynovitis: a case report... including
5.
Manual Therapy Techniques for the Hand and Fingers.
CHAPTER 5 Hand and Fingers commentary by LaStayo P with author response. J
. Burke J, Buchberger DJ, Carey-Loghmani M, Dougherty PE, Greco DS, Dishman JD. A pilot study comparing two manual therapy interventions for carpal tunnel syndrome. J Manipulative Physiol Ther.
Orthop Sports Phys Ther. 2002;32(3):86-97. Bes Heiser R, O'Brien VH, Schwartz DA. The use of joint mobilization to improve clinical outcomes in hand therapy: a systematic review of the literature. J Hand
‘Ther. 2013;26(4):297-310.
2007;30(1):50-61. 16.
Page MJ, O'Connor D, Pitt V, Massy-Westropp
hide
ercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012(6). Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. Sth ed. St. Louis, MO: Saunders/Elsevier; 2013.
18,
Villafane
10. O'Brien VH, McGaha JL. Current practice patterns in conservative thumb CMC joint care: survey results. J
11.
12.
Hand Ther, 2014;27(1):14-22. Villafafie JH, Silva GB, Chiarotto A. Effects of passive upper extremity joint mobilization on pain sensitivity and function in participants with secondary carpometacarpal. osteoarthritis: a case series. J Manipulative ‘Physiol Ther. 2012;35(9):735-742.
Fernandez
de-Las-Penas
C, Silva
thumb
The effectiveness of a manual therapy and exercise protocol in patients with thumb carpometacarpal osteoarthritis: a randomized controlled trial. J Orthop
analysis. J Phys Ther Sci. 2014;26(6):807-812. .
lative and multimodal therapy for upper extremity and disorders: a systematic review. J
carpometacarpal
osteoarthritis:
a secondary
Villafane JH, Langford D, Alguacil-Diego IM, Fernan-
20,
and the hand Patient Position: Seated with the elbow bent supported on the table
2013;12(2):79-86. Bertozzi L, Valdes K, Vanti C, Negrini 5, Pillastrini P,
Therapist Position: Seated
Villafane JH. Investigation of the effect of conserva-
Tal-Akabi A, Rushton A. An investigation to compare the effectiveness of carpal bone mobilisation and neurodynamic mobilisation as methods of
thritis: systematic
treatment for carpal tunnel syndrome. Man
Rehabil. 2015;5:1-19.
Ther.
GB,
dez-Carnero J. Management of trapeziometacarpal osteoarthritis pain and dysfunction using mobilization with movement technique in combination with kinesiology tape: a case report. J Chiropr Med.
Brantingham JW, Cassa TK, Bonnefin D, et al. ManipuManipulative Physiol Ther. 2013;36(3):143-201.
: — niques 5E Finger and Thumb Adduction Manual Thera Techniques
unilateral Kaltenborn mobilization in patients with
Villafafie JH, Cleland JA, Fernandez de-Las-Pefias C.
temporomandibular
SA Finger and Thumb ere Manual Therapy Techniques 5B Finger and Thumb Flexion Manual Therapy Techniques 5C Finger and Thumb Extension Manual Therapy Techniques
Negrini S. Contralateral sensory and motor effects of
Sports Phys Ther. 2013;43(4):204-213.
14,
JH,
N. Ex-
tive interventions in thumb carpometacarpal osteoarreview
and
meta-analysis.
at 90 degrees of flexion and the fingers 1, The patient's elbow is placed
Disabil
in 10 degrees of flexion (loase packed).
2000;5(4):214-222.
2. The therapist places the stabilizing hand just proximal to the involved joint (MCE PIP or DIP). The manipulating hand is placed just distal to the involved joint (MCP PIP or DIP). 3, The therapist bunches up the skin, takes up the capsule slack, and distracts the joint for a general mobility technique. The therapist/ patient sustains traction for a general mobility technique; this may take a few seconds to a few minutes to allow for the tissues to elongate.
FIGURES-1000
UCR
Paaal Sop TRO
ie
ONS
eS
pkentuenes
eine aa pain relief, to improve a nique can be useful as aie Notes: This technique can also be eae with a traction thrust. This tech eg — a Soe EE HAT E pesRe maby, 5a eco
aa
- LIMITED FINGER AND THUMB MOBILITY —
152
153
=
ee Hand and fingers, 154 CHAPTERS
|
ee Lcca,
Manuel Treropy Tecniques forthe Handand Fingers ee 55 ¥
rs
a
Patient Position: Seated with theelbow bent. Patient Position: Seated with the aa bentand the hand supported on the table
1, The elbow is olaced at 90 degrees of flexion.
Therapist Position: Seated at the opposite side of the table
2. The therapist places a stabilizing strap (Chinese finger trap) around the finger or thumb.
3. The patient pulls the elbow downto create some traction at the finger or thumb ora pulley weight system canbeused
1. The hand is placed in its resting position (loose packed) 2, The therapist places the cephalad (stabilizing) hand just proximal to the involved joint on the hamate (carpal bone). The caudad _ (manipulating) hand is placed just distal to the involved joint (fourth
or fifth base of the metacarpal). 3. The therapist bunches up the skin, takes up the capsule slack, and distracts the joint for a general mobility technique. This may take a few seconds to a few minutes to allow for the tissues to elongate. FIGURE 5-11 ‘Notes: This technique can assist in improving mobility at the fourth and fifth CMC joints, These joints flex and extend about 20 deqrees and internally ‘fotate about 30 degrees. These motions are necessary for fifth finger opposition and functional grasping and gripping around objects. It is important to Note that the second and third OG joints are quite inode and es not account for functional motion.
Courtesy af Ryeor Medical Services, Inc.
Comrtesyof Rycor Medical Services, tex.
FIGURES-12 Notes This role
Pecans canbe weet asa Agere
=
Sika
EIEN: for pat relief, to Ree mobility, 0 orasa nee to more
aos hee
oaEaeee
et treatmenta EC
Manual Therapy Techniques for theHand and fingers = 157 CHAPTER 5 Hand and Fingers
Type of Manipulation: Joint manipulation,
Ut eNO
—
__ non-thrust long axis rotation
¢ « « «
Mobility
¥
1. The involved joint is placed in 10 degree of flexion (loose pack).
1. The therapist places the cephalad (mani pulating) hand on the first metacarpal and the caudal (stabilizing) hand on the trapezium. 2. The therapist takes up the tissue tension to the restrictive barrier of thumb opposition by adducting and flexing the first phalanx. 3. The patient isometrically contracts the thumb into palmar abduction (away from the restrictive barrier) for3 to 5 seconds with approximately 5 Ibs of pressure and then the patient completely relaxes. 4, Upon relaxation, the therapist opposes the thumb to new restrictive
barrier. This is repeated until no further relaxation or improvement of FIGURE 5- 14
range of motion into opposition occurs.
Notes: Figure A demonstrates muscle energy for the IP joint of the thumb. This can be done at the I, MF or CMC joint of the thumb as in the pe bon ye Notes: This technique is useful when aaa muscle faring is present (e.g,, abductor pollicis brevis). This technique is useful when joint glides are painful or significant muscle quarding is present.
First CMC joint opposition is made up of two osteakinematic motions: palmar abduction (in a direction perpendicular to the palm) and flexion (a direction parallel to the palm). Therefore, both a dorsal glide (palmar abduction) and a medial glide (flexion) should be performed to improve thumb opposition. Caution should be used with this technique because the first CMC joint is typically unstable in the dorsal/radial direction
(conditions such as first CMC osteoarthritis).
| anid Thumb (MCP, IP) Flexion
Cy,
Therapist Position: Seated
G
2. The therapist places the cephalad hand just proximal to the MCP/PIP/ DIP/IP to stabilize the proximal bone. The caudal hand/mobilizing
1. The involved joint is placed in 10 degree of flexion (loose packed).
fz
1,
e}
J
-
hand of the therapist is on the distal phalange. 3, The therapist distracts with the caudal hand. 4. Apalmar glide of the phalange is performed with progressive oscillation at the tissue barrier.
FIGURE 5-15
4
Patient Position: Seated Therapist Position: Seated
non-thrustFinger (MCP. PIP. OP) Restricted Motion: Limited Fi
Patient Position: Seated with the elbow bent and the hand supported on the table
Gy
=
Type of Manipulation: Muscle energy technique ' Restricted Motion: Limited Thumb Opposition
A
Cras
ea
Joints Beeee Finger and Thumb Opposition Motion Limitation
4 Type of Manipulation: Joine manipulation, ~ Joint: Finger Finger and Thumb Flexion Motion Limitation
\
FIGURE = 3
es
TOT OO O OOO
2. The therapist places the stabilizing hand just proximal to the involved joint (MCP PIP or DIP). The manipulating hand is placed just distal to the involved joint (MCP PIP or DIP). 3, The therapist produces a distraction with the mobilizing hand while performinga rotational accessory movement in the medial or lateral direction.
Finger and Thumb Flexion Manual Therapy Techniques + Counterstrain technique Joint manipulation, non-thrust e Myofascial manipulation Joint manipulation, thrust « Soft tissue manipulation Muscle energy technique + Self-mobilization Mobilization with movement
(aS,
t
Therapist Position: Seated
=
Patient Position: Seated with the elbow bent and the hand supported on the table
‘mat)
eneral Motion Limitation
5B
' Restricted Motion: Limited Finger and Thumb
a ede
LIMITED FINGER (MCP, PIP, DIP) AND THUMB (MCP, IP) FLEXION
156
158
CHAPTER 5 Hand and Fingers
Manual Therapy Techniques for the Hand and fingers
) A AS Joint: Finger Finger and Thumb
Flexion Motion Limitation
159
~ Type of Manipulation: Joint manipulation, non-thrust Restricted Motion: Limited Thumb CMC Flexion
Joint: Finger Finger and Thumb Flexion Motion Limitation
= >
Patient Position: Seated with the elbow bent and the hand
Type of Manipulation: Muscle energy technique Restricted Motion: Limited Finger and Thumb MCP/PIP/DIP/IP Flexion Patient Position: Seated with the elbow bent and the hand supported on the table
=)
Therapist Position: Seated
supported on the table
Therapist Position: Seated
. The therapist places the cephalad (stabilizing) hand just proximal to
metacarpal is performed with progressive oscillation at the tissue
barrier. FIGURE 5-16
a pany
FIGURE 5-18
of the therapist is at the base of the phalanx just distal to the joint. _ The therapist takes up the tissue tension to the restrictive barrier of finger flexion. _ The patient isometrically contracts the finger into extension (away from the restrictive barrier) for 3 to 5 seconds, meeting the therapist's force with approximately 2 to 3 bs of pressure, and then the patient completely relaxes. _ Upon relaxation, the therapist pushes the finger to the new restrictive bartier of flexion. This is repeated until no further relaxation or improvement of range of motion into flexion occurs.
Notes: This technique is useful when significant muscle guarding is present (e.9., extensor pollicis longus).
fo
Pl
Restricted Motion: Limited Finger (MCP, PIP DIP) and Thumb (MCP. IP) Flexion Patient Position: Seated with the elbow bent Therapist Position: Seated . The patient rests the arm on the table. 2, The therapist places the cephalad (stabilizing) hand just proximal to the MCP/PIP/DIP/IP of the patient. The caudad (manipulating) hand of the therapist is at the base of the phalanx just distal to the joint. 3. The therapist flexes the MCP PIP DIP IP joint to the tissue barrier. 4. Apalmar glide of the metacarpal is performed at the tissue barrier. The therapist creates a high-velocity low-amplitude (HVLA) thrust in a palmar direction.
FIGURE 5-17
‘fi
”
1 ee” 1h
”)
Joint: Finger
Finger and Thumb Flexion Motion Limitation
Type of Manipulation: Mobilization with movement Restricted Motion: Limited Finger (MCP/PIP/DIP) and Thumb (IP) Flexion Patient Position: Seated with the wrist in neutral Therapist Position: Seated 1. The therapist places the cephalad (stabilizing) hand just proximal to the MCP/PIP/DIP/IP of the patient. The caudad (manipulating) hand
of the therapist is at the base of the phalanx just distal to the joint. 2. Asthe patient performs finger flexion, the therapist performs an accessory glide of the distal seqment in a palmar direction. 3, This is repeated until there is an increase in finger flexion.
FIGURE 5-19
LIMITED FINGER (MCP, PIP, DIP) AND THUMB (IP) FLEXION
Finger and Thumb Flexion Motion Limitation
=e
Joint: Finger
|
Type of Manipulation: Joint manipulation, thrust
Saal
saat
Notes: During CMC flexion {in a direction parallel to the palm), the metacarpal rolls and glides in the same direction.
a
4. A medial (ulnar) glide in a direction parallel to the palm of the
TEE EEE ECE REECE ee
the MCP/PIP/DIP/IP of the patient. The caudad (manipulating) hand
1, The involved thumb joint is placed in a resting position midway between abduction/adduction and flexion/extension (loose packed). 2. The therapist places the cephalad hand on the first metacarpal and the caudal on the trapezium (carpal bone). 3. The therapist distracts with the cephalad hand.
=
)
=e
Manual Therapy Techniques for the Hand and Fingers’ = 161 CHAPTER 5 Handand Fingers
' Type of Manipulation: Mobilization with
movement
d Th mb Flexion Motion Limitation iS
;
Type of Manipulation: Counterstrain technique
a
Joint: Finger
Restricted Motion: Limited Finger are TURD
Sa
Finger and Thumb Flexion Motion Limitation
Flexion
Restricted Motion: Limited Thumb CMC Flexion Patient Position: Seated palm up Patient Position: Seated with the elbow bent and the hand supported on the table
Therapist Position: Seated
Therapist Position: Seated
1. The therapist palpates the finger extensor muscle (extensor digitorum
communis—EDQ) or the thumb extensor muscle (extensor pollicis longus—EPL and brevis—EPB) that is hypertonic The therapist
1. The therapist places the cephalad (stabilizing) hand along the trapezium carpal bone. The caudad (manipulating) hand is placed just distal to the first CMC on the base of the first metacarpal.
presses into the muscle of discomfort and finds the most hypertonic uncomfortable point.
2. The therapist asks the patient to rate the discomfort ata 10/10. 3. The therapist passively extends the thumb or fingerat the MCP joint
2. As the patient performs active thumb flexion, the therapist simultaneously performs an accessory glide of the distal segment in
(proximal phalange) and compresses the thumb or finger toward the carpal bones until the palpable point is down to a 2/10 discomfort level.
the medial (ulnar) direction. 3. This is repeated until there is an increase in thumb flexion.
4. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively straightens out the thumb
FIGURE 5-20 Notes: This technique can be helpful when the patient presents with radial subluxation ae the base of the first eed be CMC osteoarthritis). The medial force aligns thejsent & cps! amotionie decreased oa
and rechecks the point in the original position. If the point produces
at the first CMC jointie 4,
more than 2/10 discomfort the treatment is repeated.
Salih be
bef TMA
FIGURE 5-21
LIMITED FINGER AND THUMB FLEXION
160
Manual Therapy Techniques tor the Hand and Fingers
+9163
CHAPTER 5 Hand and Fingers Type of Manipulation: Myofascial manipulation
Joint: Finger
Finger and Thumb Flexion Motion Limitation
Joint: Finger
Type of Manipulation: Myofascial manipulation Restricted Motion: Limited Finger and Thumb Flexion
Finger and Thumb Flexion Motion Limitation
Restricted Motion; Limited Finger and Thumb
Flexion Patient Position: Seated
Patient Position: Seated
Therapist Position: Seated . The therapist places thumbs on the dorsum of the patient's hand (over the metacarpal shafts). 2. The therapist places the fingers of one hand aver the patient's thenar eminence and the fingers of the other hand over the patient's hypothenar eminence. . The therapist mobilizes the fascia and other soft tissues on the dorsum of the hand with the thumbs while approximating the thenar and hypothenar eminences palmarly with the fingers. . The therapist engages the restrictive barrier with a light force in the direction of tension, sometimes up to 3 to.5 minutes. _ Aight pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates.
=.
Therapist Position: Seated 1. The therapist places the opposite hand around the patient's hand
(e.g., patient's right hand and therapist's left hand).
un
:-
2. The therapist uses a tissue tension technique to mobilize the fascia. The therapist uses the index finger to stabilize the proximal segment and the thumb to palpate the soft tissue, 3. The therapist engages the restrictive barrier with a light force in the direction of tension, sometimes up to 3 to 5 minutes. 4. A light pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates. FIGURE 5-23
Notes: Technique is useful in the presence of myofascial restrictions that contribute to decreased jointmobility.
file i, a id
Type of Manipulation: Soft tissue manipulation
~ Joint: Finger Finger and Thumb Flexion Motion Limitation
Restricted Motion: Limited Finger and Thumb Flexion Manual soft tissue manipulation Patient Position: Seated Therapist Position: Seated
ho
FIGURE 5-22
a
rer)
Notes: Technique is useful in the presence of myofascial restrictions that contribute to decreased joint mobility.
The therapist flexes the finger. The therapist palpates the finger extensors (EDC, EPL)/interossei and holds deep pressure. The therapist can perform soft tissue manipulation by gentle strumming and lateral mobilization of the muscles and tendons, and with circular strokes to increase circulation. This is repeated until the soft tissue relaxes.
a,
“a
FIGURE 5-24
should be performed with the patient actively Notes: Although interossei mobilization is performed passively, the lumbrical mobilization technique
extension with IP flexion). The FDP needs to be engaged in contracting due to the attachments to the flexor digitorum profundus—FOP (active MCP
order for lumbricals to havea firm anchor to be mobilized upon.
_ LIMITED FINGER AND THUMB FLEXION
162
OS
ills hathaalae
S Hand and Fnges © 164 CHAPTER Self soft tissue manipulation
Patient Position: Seated
ee
Patient Position: Seated
1, The patient compresses the finger extensor muscles with the opposite
‘
oes ae 1, The patient wears a finger flexion glove or a torque transmission
: ‘fingers. can hold statically or rock back and forth to relax the soft 2, The patient
3
in 0 degrees (IPs are the MCPs orthosis is fabricated that immobilizes
“tissues,
left free).
3. This is repeated until the soft tissue relaxes.
a
2, The patient is encouraged to actively flex at IPs throughout the day to actively mobilize the joints and mobilize the intrinsics.
"FIGURE 5-24 (CONTINUED) Notes: This technique can also be performed rollingon a tennis ball.
‘Courtesy af Patteeven Medical,
FIGURE 5-25,
Se
eee
or hypermobile joint(s) (e.g., MCP), Notes: Useful when |? motion is limited and MCP joint motion is normal or excessive. By restricting the normal finger. A relative motion orthosis single a only for or 4 through 2 you are facilitating motion at the stiffjoint(s) (e.9,, IPs). May be used grossly for fingers transmission to flex. force greater have with IPs the so digits, other the to relative extension more in may also be used to position a patient's MCP resistance. the against This can be combined with a muscle energy technique to facilitate movement where the patient works
CHAPTERS Hand and Finger
Patient Position: Seated
Patient Position: Variable
+1. The patient uses the opposite hand to flex the thumb or finger.
1. Amobilization orthosis is fabricated that mobilized the MCP(s) into
2. Thisis statically held at a point of tissue tension.
‘flexion. The orthosis may bea static-progressive, dynamic,or serial static design based on the end feel and stage of healing.
2. The patient is encouraged to wear the orthosis to passively move joints into flexion through a low-load long duration stretch to the tissues. Teal hae Batic
FIGURE 5-26 ~ Notes: A capsular end feel with slight hypomobility responds betterto dynamic mobilization (i.e., rubber bands). An abnormal capsular end feel with considerable hypomobility responds betterto a static progressive orthosis (i.e, fishing line).
FIGURE 5-27
Notes: Can be combined with a muscle energy technique to facilitate movement. This can also be performed on the fingers.
LIMITED FINGER AND THUMB FLEX
166
Manuol Therapy Techniques forthe Hand and Fingers © 167
Manual Therapy Techniques forthe Hand and Fingers
169
CHAPTERS Hand and Fingers
Type of Manipulation: Joint manipulation, thrust Restricted Motion: Limited Finger (MCP PIP DIP)
Finger and Thumb Extension Motion Limitation
and Thumb Extension (MCP, IP) Patient Position: Seated with the elbow bent and the hand supported on the table
Finger and Thumb Extension Manual Therapy Techniques » Counterstrain technique « Joint manipulation, non-thrust e Myofascial manipulation ¢ Joint manipulation, thrust
* Soft tissue manipulation
« Mobilization with movement
* Self-mobilization
Joint: Finger
Finger and Thumb Extension Motion Limitation
Type of Manipulation: Joint manipulation, non-=thrust Restricted Motion: Limited Finger (MGCP PIP, DIP) and Thumb (MCP IP) Extension
Therapist Position: Seated
Patient Position: Seated with the elbow bent and the hand supported on the table Therapist Position: Seated 1, The involved joint is placed in 10 degrees of flexion (loose packed). 2. The therapist places the cephalad (stabilizing) hand just proximal to the MCP/PIP/DIP/IP to stabilize proximal bone. The caudal
(mobilizing) hand of the therapist is on the phalange just distal to the joint. 3. The therapist distracts with the caudal hand. 4. A dorsal glide of the phalange is performed with progressive oscillation at the tissue barrier.
5
Es 2
“eae Te
——
a a ak
*
“lew ‘eh
3aaa
Soak
=
Notes: During CMC extension in a direction parallel to the palm (radial abduction), the metacarpal rolls and glides in the same direction. However, caution should be used with this technique because the first CMC joint is typically unstable in this direction (radial) with conditions such as first CMC osteoarthritis,
BPP
FIGURE 5-29
=
(carpal bone).
3. The therapist distracts with the cephalad hand. 4. A lateral (radial) glide is performed in a direction parallel to the palm of the metacarpal with progressive oscillation at the tissue barrier,
ek
metacarpal and the caudal (stabilizing) hand on the trapezium
2
1. The involved thumb joint is placed in a resting position midway between abduction/adduction and flexion/extension (loose packed). 2. The therapist places the cephalad (manipulating) hand on the first
4, Alateral (radial) glide of the phalanx is performed to the second and the third digits with progressive oscillation at the tissue barrier.
(Mil -»
5. A medial (ulnar) glide of the phalanx is performed to the third, fourth, and fifth digits with progressive oscillation at the tissue barrier.
PEER EER ER TEER
yA *»
yA
”»
of TS al ~
Notes: The patient can vee this at any of the other MCP/PIP/DIP joints. The patient can also use a pen or dowel interlaced between the other fingers to create an extension stretch.
the Metacarpal Phalangeal (MCP) Joints
supported on the table
i | IAS iB ay
FIGU RES5- 39
Type of Manipulation: Hol int mani ipulation, non-thrust Restricted Motion: Limited Finger Abduction of
CT
”
re
ea. ” ra ”
ok wu 7
Fi
aii
FIGURE 5~ 40
es Hine
he ae
Gis relative to me i a
LIMITED FINGER ABDUCTION OF THE METACARPAL PHALANGEAL (MCP) JOINTS
the MCP joint.
2. The patient can perform statically or can use a muscle energy technique.
Manual Therapy Techniques for the Hand and Fingers
CHAPTER 5 Hand and Fingers
Joint: Finger Finger and Thumb Abduction Motion Limitation
Type of Manipulation: Joint manipulation, thrust Restricted Motion: Limited Finger Abduction
(MCP) Patient Position: Seated with the elbow bent
mu
_
Therapist Position: Seated . The patient rests the arm on the table . The therapist places the stabilizing hand just proximal to the MCP.
Goh 7
Gr C-is,
creates a HVLA thrust in a lateral (radial) direction, A medial (ulnar) glide of the phalanx is performed to the third, fourth and fifth digits at the tissue barrier. At the tissue barrier, the therapist creates a HVLA thrust in a medial (ulnar) direction.
ANAAALA
FIGURE 5-42
Notes: Finger MCP abduction is relative to the third digit
+»
- The therapist stabilizes the trapezium carpal bone and the rest of the hand with the caudad hand and places the cephalad hand around the metacarpal of the thumb with the therapist’ thumb at the base of the metacarpal.
2. The therapist places traction on the thumb and abducts the thumb at the CMC joint to tissue tension. 3. At the tissue barrier, the therapist creates a HVLA thrust in a perpendicular direction away from the palm.
FIGURE 5-43
Notes: During CMC (palmar) abduction (ina direction perpendicular to the palm), the metacarpal rolls and glides in opposite directions. Thrust technique can be useful to address joint restrictions that do not respond to the application of non-thrust techniques.
Joint: Finger
Finger and Thumb Abduction Motion Limitation
Type of Manipulation: Muscle energy technique Restricted Motion: Limited Thumb CMC
Abduction (Palmar Abduction) Patient Position: Seated with the elbow bent and the hand supported on the table Therapist Position: Seated _ The therapist places the cephalad (manipulating) hand on the distal . The therapist takes up the tissue tension to the restrictive barrier of thumb palmar abduction by abducting the first CMC joint. . The patient isometrically contracts the thumb into adduction (away
phalanx and the caudad (stabilizing) hand on the first metacarpal.
4,
phalanx just distal to the joint. . The therapist abducts the MCP to the tissue barrier. A lateral (radial) glide of the phalanx is performed to the second and
DATA
fe us
The manipulating hand of the therapist is placed at the base of the
the third digits at the tissue barrier. At the tissue barrier, the therapist
PL
a
CoS,
from the restrictive barrier) for 3 to 5 seconds, meeting the therapist's force with 2 to 3 lbs of pressure, and then the patient completely relaxes. Upon relaxation, the therapist takes up the additional tissue slack to the new restrictive barrier of thumb abduction. This is repeated
FIGURE 5-44
until no further relaxation or improvement of range of mation into abduction occurs
brevis abducts the thumb Notes: This technique is useful when joint glides are painful or significant muscle guarding is present. Abductor pollicis
extension of the thumb. at the carpometacarpal joint and the metacarpophalangeal joint. It also assists in apposition and
LIMITED THUMB CMC ABDUCTION (PALMAR ABDUCTION)
Notes: During CMC palmar abduction (in a direction perpendicular to the palm), the metacarpal rolls and glides in the opposite direction. However, caution should be used with this technique because the first CMC joint is typically unstable in this direction (dorsal/radial) with conditions such as first CMC osteoarthritis.
Therapist Position: Seated
ee)
FIGURE 5-41
Cot
nm
1. The thumbs placed in its resting position (loose packed) 2. The therapist places the cephalad (stabilizing) hand on the trapezium {carpal bone) and the caudad (manipulating) hand on the base of the first metacarpal 3. The therapist distracts with the caudad (manipulating) hand. 4, A dorsal glide is performed with progressive oscillation at the tissue barrier.
Patient Position: Seated with the arm on the table palm up
has
Therapist Position: Seated
Type of Manipulation: Joint manipulation, thrust Restricted Motion: Limited CMC Thumb Abduction (Palmar Abduction)
7
Patient Position: Seated with the elbow bent and the hand supported on the table
Finger and Thumb Abduction Motion Limitation
SSssssssddddssdddUUV
Finger and Thumb Abduction Motion Limitation
Joint: Finger
179
A
Joint: Finger
Type of Manipulation: Joint manipulation, non-thrust Restricted Motion: Limited Thumb CMC Abduction (Palmar Abduction)
NOOO OOOO OL
178
un
ea
SL
Manual Therapy Techniques for the Rand and Fingers
§=181
CHAPTER 5 Hand and Fingers
Patient Position: Seated with the elbow bent and the hand supported on the table
Therapist Position: Seated
Patient Position: Seated with the elbow bent and the hand supported on the table
pee)
nm
Therapist Position: Seated . The therapist places the cephalad (stabilizing) hand along the trapezium carpal bone. The caudad (manipulating) hand is placed just distal to the first CMC on the base of the first metacarpal. _ As the patient performs active thumb palmar abduction, the therapist simultaneously performs an accessory glide of the metacarpal ina perpendicular direction toward the palm (dorsal direction) to take up all of the tissue tension. . This is repeated each time the patient actively abducts the thumb to get an increase in thumb palmar abduction. FIGURE 5-46
Notes: Caution: This technique is not appropriate for patients with a first CMC joint instability, If a patient presents with an unstable first CMC with
radial subluxation of the base of the first metacarpal (e,g., first CMC osteoarthritis), a medial (ulnar) force will better align the joint for improved motion and decreased pain.
aa
4
== _
=,
mo (ee)
Restricted Motion: Limited Thumb Abduction (Palmar Abduction) Patient Position: Seated with the elbow bent and the hand supported on the table Therapist Position: Seated _ The therapist palpates the thumb adductor muscle (Adductor Pollicis) that is hypertonic. The therapist presses into the muscle of discomfort and finds the most hypertonic uncomfortable point. _ The therapist asks the patient to rate the discomfort at a 10/10. io
Joint: Finger Finger and Thumb Abduction Motion Limitation
movement Restricted Motion: Limited Thumb CMC Abduction (Palmar Abduction)
Type of Manipulation: Counterstrain technique Joint: Finger Finger and Thumb Abduction Motion Limitation
_ The therapist passively adducts the thumb’s first CMC joint while maintaining compression until the palpable tender point is down to a
>
Type of Manipulation: Mobilization with
Notes: Finger MCP abduction is relative to the third digit.
2/10 discomfort level. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds. Once the 90
seconds are up, the therapist passively retums the thumb to neutral
5
Notes: This technique is useful when significant muscle quarding is present (e.¢., interossei).
FIGURE 5-47 |
OCCUTS.
. The therapist places the cephalad (stabilizing) hand on the metacarpal just proximal to the involved jaint (MCP). The caudad (manipulating) hand is placed on the phalange just distal to the involved joint (MCP). _ As the patient performs active finger abduction, the therapist simultaneously performs an accessory glide in the lateral (radial) direction for the second and the third digits and in the medial (ulnar) direction for the third, fourth, and fifth digits to take up all of the tissue tension, . This is repeated each time the patient actively abducts the finger to get an increase in finger abduction.
aoe
the new restrictive barrier of finger abduction. This is repeated until no further relaxation or improvement of range of motion into abduction
FIGURE 5-45
= 3333-33 3225356545522
from the restrictive barrier) for 3 to S seconds, meeting the therapist's force with 2 to 3 Ibs of pressure, and then the patient completely relaxes. . Upon relaxation, the therapist takes up the additional tissue slack to
me,
Mm pes)
. The patient isometrically contracts the finger into adduction (away
~
. The therapist places the cephalad (manipulating) hand on the distal phalanx and the caudad (stabilizing) hand on the metacarpals. . The therapist takes up the tissue tension to the restrictive barrier of finger abduction by abducting the MCP joint(s)
Type of Manipulation: Mobilization with movement Restricted Motion: Limited Finger Abduction Patient Position: Seated with the elbow bent and the hand Supported on the table
sy
Therapist Position: Seated
Joint: Finger Finger and Thumb Abduction Motion Limitation
FIGURE 5-48
Notes: Adductor pollicis adducts the thumb at the carpometacarpal joint
and rechecks the pointin the original position. Ifthe point produces more than 2/10 discomfort the treatment is repeated,
LIMITED THUMB ABDUCTION (PALMAR ABDUCTION)
Type of Manipulation: Muscle energy technique Restricted Motion: Limited Finger Abduction
F|
Joint: Finger Finger and Thumb Abduction Motion Limitation
PF PPA DTEPEE OOOO OOOO OLE OOO OOO OOOO =e OOOOH
180
Manual Therapy Techniques forthe Hand and fingers
«=. 183
CHAPTER 5 Hand and Fingers
Joint: Finger Finger and Thumb Abduction Motion Limitation
Type of Manipulation: Counterstrain technique Restricted Motion: |imited Finger Abduction
Joint: Finger
Finger and Thumb Abduction Motion Limitation
Patient Position: Seated with the elbow bent and the hand supported on the table
Manual soft tissue manipulation Patient Position: Seated with the elbow bent and the hand supported on the table
1. The patient relaxes the fingers with the palm up. 2. The therapist palpates the palmar interassei between the metacarpals using a pincher grip and holds deep pressure as in Figure A. 3, The therapist can perform soft tissue manipulation by gentle
(aa
strumming and lateral mobilization of the muscles and tendons, with ead a
i,
Patient Position: Seated with the elbow bent and the hand supported on the table
Zgagaa
Abduction
sai
Restricted Motion: Limited Finger and Thumb
Finger and Thumb Abduction Motion Limitation
are
Type of Manipulation: Myofascial mobilization Joint: Finger
SITIIIIIIIIIIS
need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively returns the digit to neutral and rechecks the point in the original position. If the point produces more than 2/10 discomfort the treatment is repeated.
FIGURE 5-49
circular strokes to increase circulation. 4. This is repeated until the soft tissue relaxes.
|
. The therapist holds the position for90 seconds. The therapist does not
Therapist Position: Seated
a
f.
La op
Therapist Position: Seated . The therapist palpates the finger adductor muscle (palmar interossel) that is hypertonic. The therapist presses into the muscle of discomfort and finds the most hypertonic uncomfortable point. . The therapist asks the patient to rate the discomfort at a 10/10. . The therapist passively adducts the finger at the MCP joint while maintaining compression until the palpable tender pointis down to.a 2/10 discomfort level.
Type of Manipulation: Soft tissue manipulation Restricted Motion: Limited Finger and Thumb Abduction
Therapist Position: Seated
wv
1. The patient places the hand palm up. 2. The therapist places the cephalad hand around a metacarpal. The therapist places the caudad hand around the adjacent metacarpal. 3. The therapist passively abducts the patient's fingers. 4. Atthe tissue barrier, the therapist uses a tissue tension technique to mobilize the fascia over the metacarpal bones in direction of tissue tension, . Alight pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates.
FIGURE 5-50 Notes: This technique can be performed on the dorsal or palmar side of the fingers,
FIGURE 5-51 Notes: A distal to proximal stroking technique can be provided along the interossei muscle bellies, The interossei can also be mobilized by placing the MCP joints in extension while simultaneously placing the IPs inflexion,
LIMITED FINGER AND THUMB ABDUCTION
5
182
184
Manual Therapy Techniques for the Hand and Fingers
CHAPTERS Hand and Fingers.
185
Patient Position: Seated with the elbow bent and the hand relaxed
1. The patient places the: opposite thumb or uses a pincher grip on theadductor pollicis muscle as seen in Figure C.
Patient Position: Seated
1. The patient grasps the hand to be mobilized with the opposite hand “with the hypothenar eminence against the MCP joints 2 to 5 inside
_ 2, The patient provides deep pressure with pincer palpation over the
palpable trigger point and it is ischemically compressed continuously _ or intermittently,
the opposite thumb at the webspace of the patient.
2. The patient abducts the thumb until the tissue barrier is met.
_ 3, Pressure is held until the pain decreases or there is a significant release.
3. The patient glides the base of the first metacarpal away from the palm in a perpendicular direction.
4, Astroking (parallel to muscle fibers) or strumming (perpendicular to
4, The patient can hold tension statically or rock the thumb into
muscle fibers) technique can also be provided along the muscle.
abduction by getting an increased glide.
FIGURE 5-51 (CONTINUED) Notes: When mobilizing the adductor pollicis, itis important not only to palmarly abduct the first CMC but also to flex the first MCP as a result of the
‘attachment into the extensor expansion. Patient can roll a massage ball under the hand as an alternate technique as seen in Figure D.
Patient Position: Variable 1. Amobilization orthosis is fabricated that mobilizes the MCP(s) into abduction. The orthosis may be'a static-progressive, dynamic, or serial static design based on the end feel and stage of healing. 2. The patient is encouraged to wear orthosis to passively move joints
into abduction through a low-load long duration stretch to the tissues.
‘Courtesy of OLE FIGURE 5-52
responds better to dynamic mobilization (j.e., rubber bands) An abnormal aclu oh feel Notes: A ee end feel with slight front progressive orthosis (ie., fishing line). The finger abduction motion may be better improved static a to with considerable hypomobility responds better through the use of a serial static orthosis.
‘Courtesy af Aapson Ovtbeties.
FIGURE > 33
Notes: The patient can wear a fabricated mobilization orthosis that mobilizes the first CMC into palmar abduction. The orthosis may bea static-progressive, dynamic, or serial static design based on the end feel and stage of healing. The patientis encouraged to wear orthosis to passively move joints into palmar abduction through a low-load long duration stretch to the tissues
feel ‘sth lot fypanaails eek better to dynamic A Nepstar mobilization (i.e., rubber bands). An abnormal capsular end feel with considerable hypomobility responds better toastaticprogressive orthosis (ie, fishing line). The palmar abduction motion may be better improved through the use ofa serial static orthosis. Caution: Do not owverstress the ulnar collateral ligament of the MCP when fabricating the orthosis.
- LIMITED THUMB ABDUCTION (PALMAR ABDUCTI
: Self soft tissue ti manipulation
Manual Therapy Techniques for the Hand and Fingers © 187 186
CHAPTER 5 Hand and Fingers
Type of Manipulation: Joi nt rranpulation, aS
Finger and Thumb Adduction
Joint: Finger Finger and Thumb Adduction Motion Limitation
5E Finger and Thumb Adduction Manual Therapy Techniques * Counterstrain technique ¢ Joint manipulation, non-thrust
« Joint manipulation, thrust + Muscle energy technique « Mobilization with movement
non-thrust Restricted Motion: li mited Thumb CMC
ane
Adduction Patient Position: Seated with the elbow bent and the hand
supported on the table
« Myofascial manipulation + Soft tissue manipulation
Therapist Position: Seated
* Self-mobilization
1. The patient rests the arm on the table 2. The therapist places the cephalad (stabilizing) hand on the trapezium
(carpal bone) and the caudad (manipulating) hand on the base of the
Type of Manipulation: Joint anipulat on,
first metacarpal 3. The therapist distracts with the cephalad hand. 4. The therapist performs a radial accessory glide away from the palm with progressive oscillation at the tissue barrier.
non-thrust Restricted Motion: Limited Finger Adduction of
Notes: finger “ cmt
is relative to the third ce
AI
theely the Pear
Be ae oc in ES
Type of Manipulation: Joint manipulation, thrust Restricted Motion: Limited Hngey MCP Adduction Patient Position: Seated with the elbow bent and the hand supported on the table Therapist Position: Seated 1, The patient rests the arm on the table 2, The therapist places the cephalad (stabilizing) hand just proximal to the MCP The caudad (manipulating) hand of the therapist is placed on the base of the phalanx just distal to the joint.
3, The therapist abducts and tractions the phalange to the tissue barrier. 4, The therapist glides the second phalanx in a medial (ulnar) glide, at the tissue barrier the therapist performs a HVLA thrust in a medial
direction. 5. The therapist glides the fourth and fifth phalanx in a lateral (radial) direction, at the tissue barrier the therapist performs a HVLA thrust in
FIGURE 5-56
alateral direction.
because adduction is typically a position of Notes: Finger MCP adduction is relative to the third digit. It is very atypical to have to use these techniques deformity.
LIMITED FINGER MCP ADDUCTION
FIGURE 5-54
en (in adirection ue
Joint: Finger
Sat ta fot bot Fe
glideof the phalanx is performed to the fourth and fifth digits with progressive oscillation at the tissue barrier.
Notes: Dery ise CMC
Finger and Thumb Adduction Motion Limitation
Ff
packed). 2. The therapist places the cephalad (stabilizing) hand just proximal to the MCP joint. The caudad (manipulating) hand of the therapist is placed at the base of the proximal phalanx just distal to the MCP joint. 3, The therapist distracts with the manipulating hand. 4. A medial (ulnar) glide of the phalanx is performed to the second digit with progressive oscillation at the tissue barrier. A lateral (radial)
: i
1. The involved finger joint is placed in 10 degrees of flexion (loose
FIGURE 5-55
me
Therapist Position: Seated
EOE
Patient Position: Seated with the elbow bent and the hand supported on the table
TN)THT
the Metacarpal Phalangeal (MCP) Joints
:
“Fing er ‘and Thumb Adduction Motion Limitation
Manual Therapy Techniques for the Hand and Fingers = 189 CHAPTER 5 Hand and Fingers
Finger and Thumb Adduction Motion Limitation
on.
Patient Position: Seated at the side of the table
ons,
in
fe ta
Mm
Therapist Position: Seated . The patient rests the arm on the table . The therapist places the cephalad hand on the metacarpal of the thumb and the caudal on the trapezium (carpal bone). . The therapist distracts with the cephalad hand.
Type of Manipulation: Mobilization with
set ~)
oes &
ce
Joint: Finger Finger and Thumb Adduction Motion Limitation
movement
Restricted Motion: Limited Thumb Adduction Patient Position: Seated with the forearm in neutral thumb up
y
Therapist Position: Seated
=) mS
Joint: Finger
gat
Type of Manipulation: Joint manipulation, thrust Restricted Motion: Limited Thumb CMC Adduction
. Aglide of the first metacarpal radially and inferiorly from the palm and is performed to the tissue barrier for increasing adduction. . Atthe tissue barrier, the therapist creates a HVLA thrust in 4 radial and inferior direction.
. The therapist places the cephalad (stabilizing) hand around the trapezium. The therapist places the caudad (manipulating) hand grasping the base of the first metacarpal. As the patient actively performs thumb adduction, the therapist distracts the thumb CMC joint and performs a radial accessory glide away from the palm of the metacarpal to take up all of the tissue tension.
we
188
_ Thisis repeated each time the patient actively adducts the thumb.
FIGURE 5-59
FIGURE 5-57
Notes: Techniques useful in the presence of muscle quarding or hypertonicity. During CMC adduction (in a direction radially to the palm), the
Joint: Finger Finger and Thumb Adduction Motion Limitation
Type of Manipulation: Muscle energy technique Restricted Motion: Limited Finger Adduction Patient Position: Seated with the elbow bent and the hand supported on the table
Type of Manipulation: Mobilization with Joint: Finger Finger and Thumb Adduction Motion Limitation
movement Restricted Motion: Limited Finger Adduction Patient Position: Seated with the elbow bent and the hand
Therapist Position: Seated
supported on the table
. The therapist places the cephalad (manipulating) hand on the distal
Therapist Position: Seated
nm
phalanges and the caudal (stabilizing) hand on the metacarpals. The therapist takes up the tissue tension to the restrictive barrier of
FIGURE 5-58
ms
. The patient isometrically contracts a finger into abduction (away from the restrictive barrier) for 3 to 5 seconds with approximately 2 to 3 Ibs of pressure and then the patient completely relaxes. . Upon relaxation, the therapist adducts the finger to new restrictive
barrier. This is repeated until no further relaxation or improvement of range of motion into adduction occurs.
Notes: This technique is useful when significant muscle quarding is present (e.9,, interossei).
wy)
fs
ee
finger adduction by adducting the second, fourth, or fifth phalanx.
FIGURE 5-60
Notes: Finger MCP adduction is relative to the third digit
The therapist places the cephalad (stabilizing) hand just proximal to the involved joint (MCP). The caudad (manipulating) hand is placed on the phalange just distal to the involved jaint (MCP). As the patient performs active finger adduction, the therapist simultaneously performs an accessory glide in the medial (ulnar) direction for the second digit and in the lateral (radial) direction for the fourth and fifth digits to take up all of the tissue tension. This is repeated until there is an increase in finger adduction.
LIMITED FINGER ADDUCTION
metacarpal rolls and glides in opposite directions.
Manual Therapy Techniques for the Hand and Fingers
191
CHAPTERS Hand and Fingers
Type of Manipulation: Myofascial manipulation Joint: Finger
Type of Manipulation: Counterstrain technique
Finger and Thumb Adduction Motion Limitation
Restricted Motion: Limited Thumb Adduction
Joint: Finger Finger and Thumb Addiction Motion Limitation
Patient Position: Seated with the elbow bent and the hand supported on the table
Restricted Motion: Limited Finger and Thumb Adduction Patient Position: Seated
Therapist Position: Seated
Therapist Position: Seated
fe tA
nm
1. The therapist palpates the thumb abductor muscle (abductor pollicis brevis) that is hypertonic. The therapist presses into the muscle of discomfort and finds the most hypertonic uncomfortable point. 2. The therapist asks the patient to rate the discomfort ata 10/10,
Therapist Position: Seated
f=
td
. The therapist palpates the finger abductor muscle (dorsal interossei)
FIGURE 5-62
that is hypertonic. The therapist presses into the muscle of discomfort and finds the most hypertonic uncomfortable point. . The therapist asks the patient to rate the discomfort at a 10/10. . The therapist passively abducts the MCP while maintaining compression until the palpable tender point is dawn toa 2/10 discomfort level. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds, Once the 90 seconds are up, the therapist passively returns the digit to neutral and rechecks the point in the original position. If the point produces more than 2/10 discomfort the treatment is repeated.
in
Joint: Finger Finger and Thumb Adduction Motion Limitation
Type of Manipulation: Soft tissue manipulation Restricted Motion: Limited Finger and Thumb
Adduction Manual soft tissue manipulation Patient Position: Seated with the elbow bent and the hand supported on the table Therapist Position: Seated The patient relaxes the thumb into slight abduction. ms
Patient Position: Seated with the elbow bent and the hand supported on the table
FIGURE 5-63
The therapist palpates the thumb abductor pollicis brevis or the opponens pollicis and holds deep pressure.
ea
Restricted Motion: Limited Finger Adduction
tension.
. Alight pressure on the barrier Is held until the tissue barrier softens and relaxes and the myofascial unit elongates.
A stroking (parallel to muscle fibers) or strumming (perpendicular to
fe
Type of Manipulation: Counterstrain technique
‘W
Joint: Finger Finger and Thumb Adduction Motion Limitation
rd
FIGURE5-61
while maintaining compression until the palpable tender point is down to a 2/10 discomfort level. 4. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively returns the thumb to neutral and rechecks the point in the original position. If the point produces more than 2/10 discomfort the treatment is repeated.
ssssII IU Sessssssss
3, The therapist passively palmarly abducts the thumb’ first metacarpal
. The patient rests the hand on the table. - The therapist places the cephalad hand around the dorsum of the thumb. The therapist places the caudad hand around the carpal bones with the thumb up along the carpal bones. . The therapist passively opposes the patient’ thumb. _ Atthe tissue barrier, the therapist uses a tissue tension technique to mobilize the fascia aver the carpal bones in an ulnar direction of tissue
muscle fibers) technique can be done along the muscle. This is repeated until the soft tissue relaxes.
Self soft tissue manipulation Patient Position: Seated 1. The patient rests hand to be treated flat on the table, The patient then places a massage ball on top of the hand over the abductor pollicis
brevis or the opponens pollicis muscle. 2. The patient can hold statically or rock back and forth to relax the soft
tissues 3. This is repeated until the soft tissue relaxes.
FIGURE 5-64
LIMITED FINGER AND THUMB ADDUCTION
190
192
a ada,
CHAPTERS Hand and Fingers.
on
5
Patient Position: Seated with the elbow bent and the hand supported on the table with the fingers grasping over the thumb
1. The patient uses their opposite thumb and index finger ina flexion and ulnar deviation direction to mobilize the thumb into adduction.
2. The patient can hold tension statically or progressive oscillate the CMC
joint.
sof
anf ITS, eoyins
erin,
Hip Chapter Outline INTRODUCTION ja Tiel
and related manual therapy information. Discussion of the hip joint biomechanics
TECHNIQUES FIGURE 5-65
Notes: The patient can incorporate a hold-relax technique into this mobilization.
6A Hip General Manual Therapy
6D Hip Abduction Manual Therapy Techniques
Techniques
68
Hip Flexion Manual Therapy Techniques
+ Joint manipulation, non-thrust
- Joint manipulation, thrust + « + +
Muscle energy technique Mobilization with movement Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
6C Hip Extension Manual Therapy Techniques - Joint manipulation, non-thrust - Joint manipulation, thrust + Muscle energy technique + Mobilization with movement - Counterstrain technique » Myofascial manipulation - Soft tissue manipulation - Self-mobilization
+ > + = + =
Joint manipulation, non-thrust Joint manipulation, thrust Muscle energy technique Mobilization with movement Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
6£ Hip Adduction Manual Therapy Techniques - Joint manipulation, non-thrust + Joint manipulation, thrust - Muscle energy technique + Mobilization with movement
+ Counterstrain technique + Myofascial manipulation + Soft tissue manipulation
+ Self-mobilization
6F Hip Internal Rotation Manual. Therapy Techniques - Joint manipulation, non-thrust
- Joint manipulation, thrust « Muscle energy technique
- Mobilization with movement - Counterstrain technique - Myofascial manipulation + Soft tissue manipulation - Self-mobilization 6G Hip External Rotation Manual
Therapy Techniques + Joint manipulation, non-thrust + Joint manipulation, thrust + Muscle energy technique
- Mobilization with movement + + + +
Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
LEARNING OBJECTIVES Upon completion of this chapter, the reader will be able to: . Describe the anatomy and biomechanics of the hip joint
of the hip . Understand the state of the evidence for the use of manual therapy treatment techniques
- Perform the 8 types of techniques for each of the directions of joint motion restriction . Delineate the basic steps for the application of each type of technique
Acetabular
anteversion angle
Breneket joint with’ three of ‘motion: flexion/extension,
( Pubofemoral fgament Pubes ligament ~
abduc-
4 sto aes weight beating ‘The congruity and stability of the joint is enhanced by the presence of the acetabular labrum, which deep_ ens the joint concavity, and provides for a seal of _ the intra-articular compartment. The labrum is innervated with free nerve endings and sensory teceptors in the superficial layer, which may play a role in nocioception and proprioception ~ of the joint. The labrum is vascularized by the articular capsule vessels in its superficial third - portion.' Blood supply to the hip joint comes
from the medial and lateral circumflex arteries and the foveal artery, a branch of the posterior division of the obturator artery that runs along the ligamentum teres to the head of the femur? The acetabular fossa is covered with hyaline cartilage and faces laterally, anteriorly, and inferiorly. The inferior orientation is approximately 35 to 40 degrees, whereas the anterior orientation is approximately 20 degrees. The femoral head is also covered with hyaline cartilage. The femoral head is considered circular, with a
smaller relative radius in women than in men.
The femoral head is attached to the femoral _ neck, which forms a 120-degree angle of inclination with the shaft of the femur in the frontal
plane and a 10- to 20-degree angle of torsion in the transverse plane (MiildUi%ell). The hip has a strong joint capsule that contributes significantly to the stability of the joint. The capsule attaches
=---=
ee
- Condylar axis
‘obturator
Lesser trochanter.
Anteversion of the femoral neck angle
canal
Obturator
Femur
| Ischium membrane
FIGURE6-2 Acetabular and femoral neck anteversion angles FIGURE6-3 proximally
around
the acetabulum
and
around the base of the femoral neck. The joint capsule is reinforced anteriorly by two intracapsular ligaments: the iliofemoral (Y) ligament and
the pubofemoral ligament, and superiorly by the
ischiofemoral ligament
(see MGQUix#0)).
The
posteroinferior portion of the capsule is relatively thin and not reinforced by ligaments.! The loose-packed position of the hip joint is 30 degrees flexion, 30 degrees abduction, and slight external
rotation,
and
the
Hip ligaments
distally
closed-packed
position is full extension, abduction, and internal rotation.’ The capsular pattern is generally described as limitations in flexion, abduction, and internal rotation, although extension may also be
limited.* When the femur moves relative to the acetabulum (open-chain movement) the femoral head will glide in an opposite direction to the osteokinematic movement of the distal femur, consistent with the convex/concave rule. With flexion and extension in a neutral position, the femoral head will spin posteriorly in the sagittal plane with flexion and anteriorly with extension. The femoral head will glide inferiorly in the frontal plane with
abduction and superiorly with adduction. An anterior glide in the transverse plane will occur with external rotation, and a posterior glide will occur with internal rotation. Normal hip joint range of motion of flexion is 120 degrees, extension 15 to 20 degrees, abduction 45 to 50 degrees, adduction 20 to 30 degrees, internal rotation 30 to 40 degrees, and external rotation 40 to 60 degrees.'* Dynamic control of the hip joint is provided by the 27 muscles that act as primary movers or stabilizers." A primary stabilizer in the frontal plane is the gluteus medius. The piriformis group
are the primary movers
into flexion and
may play a role in anterior stabilization of the joint. The lateral rotator group, including the piriformis muscle, plays a role in dynamic stabilization of the hip joint, as do the internal rotators. The gluteus maximus is the primary mover for hip extension.'=.* EGTA EGZM depicts the gluteal and deep external rotator muscles.
Due to the weight-bearing function of the hip joint, osteoarthritis (OA) is a common pathology of the hip especially as age increases. Osteoarthritis is characterized by moderate lat-
eral and/or medial hip pain with weight bearing, age of 50 years and older, a loss of internal rotation and flexion of more than 15 degrees,
and morning stiffness lasting less than 1 hour (see MGTEM).’ There is moderately strong evidence that manual therapy is effective in providing short-term pain relief, increased mobility, and improved function in patients with mild
osteoarthritis of the hip. Manual therapy can be used in conjunction with exercise therapy, functional training, and patient education in the management of osteoarthritis.’ There are a number of non-arthritic conditions that can be causes of hip pain.* A recent clinical practice guideline’ outlines these conditions, including femoroacetabular impingement, "|
Piriformis
Gluteus medius
lliofemoral lig: ament (cut)
Lunate surface of acetabulum...
_-#_ Anterior inferior iliac spine
Gluteus minimus
Acetabular labrum Fat in acetabular fossa
Superior gemellus
‘Transverse acetabular ligament
Obturator
lliofemoral
ligament (cut!
Pubofemoral ligament (cut) \
Obturator artery
Inferior
4
gemellus
exlemus
Quadratus femoris
\, Obturator membrane lechiohsrrira Ligament of head ligament (cut) of femur (cut)
FIGURE6-1 Coxofemoral joint anatomy
FIGURE 6.4 Stabilizing musculature of the hip
Gluteus maximus
196 CHAPTERGHp Sidelying * Anterior femoral non-thrust mobilization/manipulation + Hip distraction with non-thrust medial femoral glide
structural instability, labral tears, osteochondral lesions, loose bodies, ligamentum teres injuries, and infections. Manual therapy may be of ben-
«
efit for the treatment of pain and joint and/or
myofascial mobility impairments. Care should
Prone * Anterior non-thrust femoral glides
be taken to identify possible contraindications for the use of manual therapy techniques,
*
including the presence of hypermobility, and
-FIGURE6.5 Osteoarthritis of the hip joint
Hip distraction non-thrust medial glide plus abduction
Anterior non-thrust glides in figure-4 position
Hoeksma et al? performed a single-blind randomized clinical trial of 109 patients with hip osteoarthritis. They found that a manual therapy program improved pain and function more than an exercise program over a 5-week period. The manual therapy program included stretching of the shortened muscles of the hip, followed by a long-axis traction technique of the hip, followed by a high-velocity thrust. Abbott et al.!° performed a 2 x 2 factorial randomized control trial of 90 adults with only hip arthritis, 116 adults with only knee arthritis, and 52 adults with OA of both the hips and knees. They found that manual therapy was superior to exercise therapy. The combination of exercise and manual therapy did not produce additional benefits. The manual therapy provided significant improvement in symptoms 4
end-range techniques should be avoided in the presence of femoroacetabular impingement.*’ Hip pain can be a manifestation of dysfunction and disease in other anatomical structures and regions. Lumbopelvic dysfunction can be a source of referred pain to the hip, as can lumbar spinal stenosis and lumbar radiculopathy. Manual therapy practitioners should also perform systems
for patients with OA of both the hips and knees,
screening for nonmechanical causes of hip pain.!”
arthritis and lumbar stenosis, and su rgical history includes right total knee replacement. The patient likes
to play golf 3 times a week; however, in the last month the left hip pain has limited his mobility in swinging a golf club. The patient is right hand dominant. Physical therapy examination findings include pain at end _Tanges with active and passive range of motion and decreased active and passive range of motion ina capsular pattern, restricted anterior and lateral direction glides, and decreased strength. Muscle length testing shows decreased muscle length of the iliopsoas muscle.
Questions: 1. What is the capsular pattern of the hip joint?
ee
The patient is a 63-year-old male who presents with left hip pain. Pertinent medical history includes oste-
Key Terms Capsular pattern coxofemoral joint: Generally
Se Ne
| CASE STUDY
See Se
f-
described as limitations in flexion, abduction, and internal rotation, although extension may also be limited.
Coxofemoral joint description: Composed of the concave acetabulum and the convex femoral head.
Closed-packed position coxofemoral joint: Full
Loose-packed position coxofemoral joint: 30 degrees flexion, 30 degrees abduction, and slight external rotation.
extension, abduction, and internal rotation.
Primary
Coxofemoral joint classification: Diarthrodial ball-and-socket joint with 3 degrees of motion:
Support weight bearing.
abduction/adduction, flexion/extension, internal/external rotation.
function of the coxofemoral
joint:
and
2. How do you determine if the joint inflammation is acute, subacute, or chronic? 3. How would that information direct your joint manipulation intervention? 4. What exercise will be appropriate for this patient to increase iliopsoas muscle length? Provide exercise parameters.
References 2.
Levangie PK, Norkin CC. Joint Structure and Function: A Comprehensive Analysis. Sth ed. Philadelphia, PA: F. A. Davis Co; 2011. Frankel VH, Leger D, Nordin M. Basic Biomechanics
3.
PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012. Moore KL, Agur AMR, Dalley AF. Clinically Oriented
].
_ 5. What exercise will be appropriate for this patient to increase hip extension strength? Provide exercise parameters. Ina case series, MacDonald et al.® found that patients with hip osteoarthritis had a decrease in pain _ and increase in hip range of motion with manual therapy techniques and exercise. Manual therapy
techniques included the following:
Supine Long-axis non-thrust oscillations in slight abduction Progression into abduction
*
Non-thrust lateral glides of femur with a belt
+
Lateral glides with combined rotations
*
Long-axis thrust mobilization/manipulation in a loose-packed position
+
Anatomy. 7th ed. Philadelphia, PA: Wolters Kluwer
and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2009;39(4):A1-A25.
8. MacDonald CW, Whitman JM, Cleland JA, Smith M,
9,
Health/Lippincott Williams & Wilkins; 2013.
« »*
*
of the Musculoskeletal System. 4th ed. Philadelphia,
international classification of functioning, disability,
Thrust mobilization/manipulation in less abduction
Hip flexion non-thrust inferior glides
4. Magee DJ. Orthopedic Physical Assessment. 6th ed. 5.
St. Louis, MO: Saunders Elsevier; 2014. Cyriax JH. Textbook of Orthopaedic Medicine: Diagnosis
6.
Balliére Tindall; 1978. Enseki K. Nonarthritic hip joint pain, J Orthop Sports
of Soft Tissue Lesions. (Vol 1, 7th ed.). London, England:
Phys Ther, 2014;44(6):Al-A32. 7. Cibulka MT. Hip pain and mobility deficits: Hip osteoarthritis: Clinical practice guidelines linked to the
10.
Hoeksma HL. Clinical outcomes following manual physical therapy and exercise for hip osteoarthritis: a case series. J Orthop Sports Phys Ther. 2006;36(8):588-599. Hoeksma HL, Dekker J, Ronday HK, et al. Comparison of manual therapy and exercise therapy in osteoarthritis of the hip: a randomized clinical trial. Arthritis Rheum. 2004;51(5):722-729. Abbott JH, Robertson MC, Chapple C, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: Clinical effectiveness. Osteoarthr Cartil. 2013;21 (4):525-534.
Manual Therapy Techniques fortheHip
198 CHAPTER 6Hip
6E Hip Adduction Manu K Ue 6c Hip Ex nsion Rs
eay
echnigues
therapy Techniques:
6F Hip |nternal Rotation Manual Therapy Techniques 6G Hip External Rotation Manual Therapy Techniques
6D Hip Abduction Manual Therapy Techniques
Therapy Techniques
« Joint manipulation, non-thrust
* Counterstrain technique
« Joint manipulation, thrust
+ Myofascial manipulation
« Muscle energy technique + Mobilization with movement
« Soft tissue manipulation » Self-mobilization
f Joint: Hip
ca
ly Hip Flexion Motion Limitation
Patient Position: Supine at the side of the table inet
ction
Therapist Position: Standing on the same side of the patient's hip to be treated
Limited L Hip Mobility
1. The therapist lifts the thigh and places the patient's knee over the
Patient Position: Supine at the side of the table
therapist's shoulder with the other leg straight. 2. The therapist places hands at the anterior thigh crease of the hip to be mobilized.
Therapist Position: Standing at the foot of the table 1, The therapist places the hands at the distal medial and lateral malleolus.
3. While lifting the thigh with the shoulders to create increased hip flexion, the therapist places an equal and opposite counterforce at the
2, The therapist lifts the hip to about 30 deqrees of hip flexion, 30 degrees of hip abduction, and 5 degrees of external rotation.
hip with both hands. 4, Atthe tissue barrier, the therapist can createa progressive oscillation to manipulate the hip capsule in a posterior/inferior direction. The
3. The therapist locks the elbows at their side at 90 degrees and shifts
bodyweight back to create traction at the hip. 4. The therapist maintains traction until the tissue relaxes with both hands to take up tissue tension.
_—
aon
primary force is generated through the hands or use of a mobilization strap. This is an anterior to posterior/inferior direction of force.
FIGURE 6-7
Notes: The imine can use a mobilization strap around the patient's waist and table to stabilize the patient. A mobilization belts can be placed around the patient's femur and ep ist to assist in ea the femur, The strap is placed as proximal on the femur as possible. FIGURE 6- 6
Notes: The therapist can also grasp the lower leg at the femoral condyles of the knee and place the lower leq against the body under the arm. The
therapist can perform a thrust technique at tissue tension. The loose-packed position of the hip is 30 degrees of hip flexion, 30 degrees of hip abduction, an 5aaeSe of external rotation.
Joint: Hip
D
yee of Manipuiation: Joint ‘manipulation, thrust
Hip Flexion Motion Limitation
by Winer es
: Bee
eet ae
i Restricted Motion: Limited Hip Flexion: i
ae e
__
Patient Position: Supine at the side of the table
|
Therapist Position: Standing on the same side of the patient's hip to be treated 1. The therapist places the hands at the anterior thigh crease of the hip
to be treated, 2. The therapist lifts the thigh and places the knee over the therapist's
shoulder with the other leq straight. 3. While lifting the thigh, the therapist uses the shoulders to create hip flexion. 4. The therapist places an equal and opposite counterforce at the anterior
thigh crease (proximal femur) with both hands to take up tissue tension. 5. Ahigh-velocity low-amplitude (HVLA) thrustis performed at the end of tissue tension. This is an anterior to posterior/inferior direction of force, FIGURE 6-8
LIMIT HIP FLEXION ED
6B Hip Flexion Manual
©1199
Manual Therapy Techniques for the Hip + 201
CHAPTERGHip
| Joint: Hip Hip Flexion Motion Limitation
Type of Manipulation: Mobilization with | movement Restricted Motion: Limited Hip Flexion Patient Position: Quadruped on the table
KS
il
Therapist Position: Standing on the same side of the patients hip to be treated facing the hip
in a posterior and inferior direction. The therapist also presses down on the posterior ilium to stabilize the pelvis. As the patient rocks back into hip flexion, the therapist usesa hand to perform an accessory glide to take up all of the tissue tension ina posterior and inferior direction of the hip capsule. 4. This is. an anterior to inferior/pasterior direction of force at the tissue barrier. 5. This is re oe: a ce amountmee flexion is nace
ae
behind the patient orin non of the patientns be Notes: is therapist can testing
posteriorly.
Type of Manipulation: Muscle energy technique
. Hip Flexion Motion Limitation
Restricted Motion: Limited Hip Flexion Patient Position: Supine
Therapist Position: Standing/kneeling on the invalved side of the patient
7.
(AD
muscles from imu
Mp
ions
crossss:
Joint: Hip Hip Flexion Motion Limitation
: read
Type of Manipulation: Counterstrain technique Restricted Motion: Limited Hip Flexion Patient Position: Prone
“a
EEE
esi >
the hans
y
ihe
Mm
1. The therapist places both hands at the posterior distal thigh of the hip to be mobilized with the therapist's knee or strap stabilizing the opposite leg. . With the knee bent to 90 degrees the therapist lifts the thigh to the restrictive barrier of hip flexion, . The patient isometrically contracts the gluteals and hamstrings (away from the restrictive barrier) into hip extension for3 to 5 seconds, meeting the therapist's force with approximately 5 Ibs of pressure, and then the patient completely relaxes. . Upon relaxation, the therapist takes up the additional tissue slack and pushes the hip to the new restrictive barrier of hip flexion. This is repeated until no further relaxation or improvement of range of motion into hip flexion occurs.
FIGURE 6-9
Notes: The knee needs to be bent to Pere
FIGURE 6-10
Therapist Position: Standing on the side of the patient and being able to support the patient's hip and knee into extension
>
TET 9
_ The patient lies prone with the legs straight. The therapist palpates the gluteal muscles that are hypertonic. The therapist presses into the
re a Jue ~
muscles of discomfort and finds the most hypertonic uncomfortable
CAS UL a
Ete
point. The therapist asks the patient to rate the discomfort at a 10/10. . The therapist passively extends the hip and knee. . The therapist palpates the gluteal muscle and extends and rotates the hip until the palpable point is down to a 2/10 discomfort level. 4, The therapist holds the position for 90 seconds. The therapist does not need to place pressure an the point for the 90 seconds. Once the 90 seconds are up, the therapist passively straightens out the legs and rechecks the point in the original position. lfthe point produces more
iw
Sait
NN
Notes: The therapist can use a mobilization strep around the patient’s waist and around the patient’s femur. The strap is placed as Saal onthe eis pt for stabilization. aalternate pate e a oe cueaxis distraction thrust (Firome B)
Joint: Hip
therapist places a force (accessory glide) at the anterior proximal thigh
a
FIG URE : : (CONTINUED)
_ The therapist places the hand at the anterior proximal thigh (femur) into the crease of the hip to be mobilized. The opposite hand is over the posterior superior iliac spine/posterior ilium. _ While the patient sits back in quadruped to increase hip flexion, the
”~
J ue “< La vrai
Minit.
< UY an r arr at
FIGURE 6-11
ih ai) 10 Sate
the treatment is pees
tequed muscle allowing the hip to flex a greater distance. This can be Notes: This should decrease the hyp ertonicity of the e. techniqu muscles, This is an indirect
Se with the paraspinal
LIMITED HIP FLEXION
200
202
int: Hip
Hip
203
Manual Therapy Techniques forthe Hip
CHAPTER GHip :
Fis
enero:
Flexion Motion Limitation=
‘Type of Manipulation: Myofascial manipulation
:
' Restricted Motion: Limited Hip Flexion Patient Position: Prone
. - wes
Therapist Position: Standing on the side of the table
;a
1. The patient lies prone, 2. The therapist palpates the gluteal muscles that have limited extensibility. 3. The therapist usesa tissue tension technique to mobilize the fascia. 4, The therapist palpates into the soft tissue and engages the restrictive
with a light barrie r force in the direction of tension, sometimes up to 3 to.5 minutes. The therapist uses both hands in opposite directions, 5. A light pressure on the barrier is held until the tissue barrier softens
: es
ee
ee
ERNE
apmemanascaeyyt
re
ee -
ee Sar
ete pe
Type of Manipulation: Soft tissue manipulation
Hip Flexion Motion Limitation RES CRE AIO
Se
ao
Joint: Hip
E
eins
Restricted Motion: Limited Hip Flexion
ri
L—
~*y an . yy
i —
=
om
FIGURE 6-13 (CONTINUED)
G
When the tibia moves relatively to the femur (open-chain arthrokinematics), the tibial joint surface will glide in the same direction as the osteokinematic movement of the tibia, consistent with the convex/concave rule. During closed-chain arthrokinematics, the femur
will roll and glide in the opposite direction. With flexion, the femoral joint surface will glide posteriorly, and it will glide anteriorly with extension
(see SEMUT7Z). With tibial lateral rotation the
medial tibial condyle will glide anteriorly, whereas the
lateral tibial condyle
will glide
posteriorly.
The glides will occur in the opposite direction with tibial medial rotation.* Normal tibiofemoral joint range of motion of flexion is 135 degrees, extension 0 to 10 degrees, medial rotation 15 to 20 degrees, and lateral rotation 20 to 30 degrees.’ The patellofemoral joint is composed of the patella, a triangularly shaped sesamoid bone in the quadriceps
muscle,
and
the femoral
sulcus
located anteriorly on the distal femur between the medial and lateral condyles. The posterior
bod
mechanism and playsa role in tensioning of the
joint capsule? — The primary movers divided
into
of the knee can be
the flexion and extension
muscle
groups (see MEZ@UT#A). Depending on the spe-
cific anatomy, the muscles that fall into the flex-
- lliopseas (group of 2) Tensor fasciae latae
Pectinus
ion and extension group can also generate forces
in the other 2 planes of movement. The knee
‘Sartorius
tendinosus and semimembranosus muscles are
Rectus femoris
flexor group consists of 7 muscles: the semi-
— Adductor longus
located in the posteromedial thigh, the short and long head of the biceps femoris in the posterolat(8)
_FIGURE7-4 Arthrokinematic motion during closed-chain flexion (A) and extension (B)
surface of the patellais covered by thick articular cartilage and has a central ridge that corresponds with a groove in the femoral sulcus.
The articular surface has three facets, each of which contact the femoral joint surface at dif_ ferent phases of the flexion-extension range of “motion, with the most medial odd facet contact-
ing the femur only at 135 degrees of knee flex-
ion (see MGGUTSEM). The patella attaches to the
tibia via the patellar tendon.’ The patellofemoral joint is highly incongruent and depends both on active and passive stabilization mechanisms. As such, it is frequently subject to tracking prob-
lems of the patella in the femoral groove. The’ primary function of the patellofemoral joint is to improve quadriceps muscle efficiency by forming an anatomical pulley mechanism.’ It also decreases friction of the distal quadriceps
eral thigh, the sartorius and gracilis in the medial
Vastus lateralis
the posterior lower leg. All but the popliteus and short head of the biceps muscles are biarticu-
Vastus medialis
lar muscles, providing movement at the hip or ankle in addition to the knee. The knee exten-
Semimembranosus
--= Popliteus (not visible)
sor group is comprised of the quadriceps femoris muscle, with the rectus femoris as the only
biarticular muscle. The monoarticular muscles are the vastus intermedius, vastus medialis, and vastus lateralis. The four quadriceps muscles combine into the single quadriceps tendon that attaches to the proximal patella, with the patel-
lar tendon (anatomically more correctly referred to as the patellar ligament) connecting the distal patella to the proximal tibia. The vastus medialis and
lateralis also attach to the medial
Peroneus longus Tibialis anterior Posterior
FIGURE 7-6 Muscles of the anterior and posterior thigh
and lat-
eral sides of the patella and thus play an important role in the tracking of the patella. Dynamic
control of the knee joint complex is provided by
interplay between the muscles of the flexor and extensor groups.'*
Due to the weight-bearing function of the tibiofemoral joint, cartilage pathologies includ-
tis is characterized by moderate joint pain with weight bearing, age of 50 years and older, a loss of range of motion more in flexion than extension, and morning stiffness lasting less than 1 hour.*’ Chondral defects are commonly associated with ACL and other ligament injuries, likely due to the loss of static joint stability. There is moderately
FIGURE 7-5 Patellar surface contact areas during
Gracilis
thigh, and the popliteus and gastrocnemius in
ing osteoarthritis are quite prevalent (60 to 70%), especially as age increases.’ Osteoarthri-
flexion-extension
Adductor magnus
strong
evidence
that
manual
ther-
apy alone, or in combination with supervised exercise, is effective in providing short-term pain relief, increased mobility, and improved function in patients with osteoarthritis and
may delay or prevent the need for surgery.®? Manual therapy can be used in conjunction with exercise therapy, functional training, and
therapy interventions, can be of use to restore optimal joint function.’ Instability of the patella and increased joint common
are
forms
of pathology
patient education in the management of osteoarthritis.-3 In addition, manual therapy and
of the patellofemoral joint. Patellar instability
postoperative rehabilitation following surgical
function
compression
often
supervised exercise are often required as part of
results
intervention.
(including
“Common tibiofemoral meniscal
nonarthritic pathologies of the joint include ligamentous and
injuries, with injuries to these
struc-
tures often occurring simultaneously.’ Patients with ligamentous and/or meniscal pathologies are at increased risk of developing chondral lesions and osteoarthritis. Although primary management of these pathologies is often surgical, manual therapy interventions, in combination with supervised exercise and other physical
from a combination
patellar
of the the
vastus
and hypermobility
Patellar instability tracking,
of decreased
stabilizing
muscles
and
lateralis)
medialis
of the patellar retinaculum.
can result in patellar mal-
lateral subluxation,
and
lateral dislo-
cation. Increased joint compression can result from decreased mobility of the patella, tightness
of the iliotibial band, decreased muscular control due to weakness of the vastus medialis, and
increased Q-angle (see Maem) .''*" Clinical manifestations of patellofemoral dysfunction include anterior knee pain, weakness of knee
- Keylems 239 that manual therapy was superior to exercise therapy. The oraiaeion of exercise and m nual therapy did not produce additional benefits. The manual therapy intervention provided: significant improvement in symptoms for patients with OA of both the hips and knees.
extensor muscles, and joint crepitus or grinding. Prolonged patellofemoral dysfunction can result in chondral lesions and osteoarthritis.2'°
In 2000, Deyle and Henderson® performed a randomized control study examining the manual: therapy techniques at the knee that included passive physiologic and accessory joint movements
There is moderate evidence that manual therapy in conjunction with exercise therapy, func-
and soft tissue mobilization for patients with OA. The control group received only ultrasound. At
tional training, and patient education is effective in providing pain relief, increased mobility, and improved function in patients with patellofemotal dysfunction.\4!7"!9
the end of the 6-week study, 5% of the subjects in the manual therapy group underwent a total: knee arthroplasty (TKA) compared to 20% in the control group.
in 2005, Deyle et al? performed a similar study with the control group receiving a standardized home exercise program (HEP). At 4-weeks follow-up, Western Ontario and McMaster Universities -
Knee pain can be a manifestation of dysfunction and disease in other anatomical strucand
regions,
considering
the
functional
differences between the groups. Pinto et al.22 examined the economic evaluation of manual therapy exercises in addition to usual
interdependence of the lower extremity joints including the foot, ankle, and hip. Lumbopelvic dysfunction can be
care for hip and knee arthritis. The results demonstrated that manual therapy and exercise were ; ; more cost effective than usual care. Jansen et al performed a systematic review on strength training alone, exercise alone, and exer-
a source of referred pain to
the knee, including lumbar spinal stenosis and
lumbar radiculopathy. Manual therapy practi-
cise therapy with passive osteoarthritis. They found on pain compared to the Rhon et al.° researched arthritis. WOMAC scores
tioners should also perform systems screening for nonmechanical
causes
of knee
pain,
with
emphasis on the urogenital and lower intestinal systems.
manual mobilization for reducing pain and disability in people with knee that exercise therapy plus manual mobilization showed a moderate effect small effect cited for exercise therapy or strength training by themselves. manual therapy and perturbation exercises in patients with knee osteosignificantly improved after the 4-week program. They found that mean
jeniicolensieteaieclieiaalia
tures
Arthritis Index (WOMAC) scores had improved 52% in the treatment group (manual therapy and | exercise) and 26% in the control group with the HEP. At 1-year follow-up there were no significant
improvements were similar to previous manual therapy trials without the pertubation. Currier et al2* worked on developing a clinical prediction rule to identify patients with knee
FIGURE 7-7 Normal male and female Q-angles
cena
ore
w
osteoarthritis who demonstrate short-term benefits from hip mobilization. They examined 5 variables:
Hip or groin pain, anterior thigh pain, passive knee flexion less than 122 degrees, passive hip internal rotation less than 17 degrees, and pain with hip distraction. If 2 out of 5 variables were present they
CASE STUDY
Be
|
'
found that the positive likelihood ratio was 12.9 with a probability of success at 97%.
The Patient is a 68-year-old female who presents with left knee pain. Pertinent medical history includes
osteoarthritis and hypothyroidism. The patient was an active jogger up toa year ago. In the last year the knee has become stiff and painful, limiting her ability to jog or walk fast, ascend and descend stairs, and to perform any squatting activities. Physical therapy assessment findings included:
ents
}
+
Key Terms
Limited active and passive range of motion, left knee flexion with pain at endrange, andrestricted posterior tibial glide.
Capsular pattern tibiofemoral joint: Limitation
+ Left hamstring length was decreased. *
Quadriceps and hamstring strength was decreased.
*
Radiology confirmed the diagnosis of osteoarthritis (OA).
. Questions:
Closed-packed position tibiofemoral joint: Full extension.
1. What is the capsular pattern of the knee joint?
Loose-packed position tibiofemoral joint: 20 to 30 degrees of flexion.
2. How do you determine if the joint inflammation is acute, subacute, or chronic?
Open-chain
3. How would that information direct your joint manipulation intervention? 4. What exercise will be appropriate for this patient to increase hamstring muscle length? Provide
exercise parameters. _ 5. What exercise will be appropriate for this patient to increase quadriceps strength? Provide exercise parameters
_ The following studies have examined the effectiveness of manual therapy, including joint glides and mobilization with movement (MWM):
«
i
more in flexion than extension.
Abbottet al. performed a 2 x 2 factorial randomized control trial of 90 adults with only hip arthritis, 116 adults with only knee arthritis, and 52 adults with OA of both the hips and knees. They found
arthrokinematics:
When
the tibia
moves relatively to the femur (open-chain move-
ment), the tibial joint surface will glide in the same direction as the osteokinematic movement of the tibia, consistent with the convex/concave rule.
Patellofemoral joint: Composed of the patella, a triangularly shaped sesamoid bone in the
quadriceps
muscle,
and
the
femoral
sulcus
located anteriorly on the distal femur between the medial and lateral condyles.
Patellofemoral joint function: To improve quadriceps muscle efficiency by forming an anatomical pulley mechanism and decrease friction of the distal quadriceps mechanism; also plays a role in tensioning of the joint capsule.
Tibiofemoral tion between
joint
classification:
the convex
distal femur
Articulaand the
concave proximal tibia. The joint is a double condyloid joint, with 3 degrees of freedom: flexion-extension, medial-lateral abduction-adduction.
rotation,
and
Manual Therapy Techniques for the Knee ge
_ References 1. Levangie PK, Norkin cc: Joint ‘Structure aia Func-
Held in Vancouver, September 2013. BrJ Sports Med.
2014;48(6):1-5.
‘Comprehensive Analysis. 5th ed. Philadel; phia, PA:
F.A. Davis Co; 2011.
15.
‘Magee DJ. Orthopedic Physical Assessment. 6th ed.
‘St. Louis, MMO:
D, Vanden Berghe L, Cerulli G. Clinical classification
of patellofemoral pain syndrome: guidelines for non-
Saunders Elsevier; 2014.
Moore ‘EL, Agur AMR, Dalley AF. Clinically Oriented Anatomy. 7th ed. Philadelphia, PA: Wolters Kluwer : Health/Lippincott Williams & Wilkins; 2013. Frankel VH, Leger D, Nordin M. Basic Biomechanics _ of the Musculoskeletal System. 4th ed. Philadelphia, “PA: Wolters Kluwer Health/Lippincott Williams &
Wilkins; 2012. Cyriax JH. Textbook of Orthopaedic Medicine: Diagnosis
of Soft Tissue Lesions. (Vol 1, 7th ed.). London, England:
Balligre Tindall; 1978.
operative treatment. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):122-130. 16. Donatelli R, Wooden MJ. Orthopaedic Physical Therapy. 4th ed. New York, NY: Churchill Livingstone; 2010. 17. van Dijk CN, van dT. Patellofemoral pain syndrome. BMJ: British Medical Journal (International Edition).
18.
on:
Kaltenborn FM, Evjenth 0. Manual Mobilization of the Joints: Joint Examination and Basic Treatment, 6th ed., Oslo, Norway: Norli; 2007. 7. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, ‘Godges JJ. Knee pain and mobility impairments: meniscal and articular cartilage lesions. J Orthop Sports Phys Ther. 2010;40(6):A1-597. -Deyle GD, Henderson NE. Effectiveness of manual
Faltus J. Effective management of patellofemoral joint dysfunction. Athletic Therapy Today. 2009;14(6):40-42.
20.
Abbott
21.
knee pain: a randomised controlled trial. J Can ChiRhon D, Deyle G, Gill N, Rendeiro D. Manual physeek
effects of mulligan’s mobilization with movement on
12
Robertson
MC,
Chapple
C,
24,
Mia
LS
Patient Position: Seated on the table
_ Therapist Position: Seated in front of the patient
et al. Man-
Osteoarthr Cartil. 2013;21(4):525-534. Deyle GD, Allison SC, Matekel RL, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. 2005;85(12):1301-1317. Pinto D, Robertson MC, Abbott JH, Hansen P, Campbell AJ, MOA Trial Team. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee. 2: Economic evaluation alongside a randomized controlled trial. Osteoarthr Jansen EJM,
2009;7(1):45-56.
athlete. Sports Med Arthrosc. 2013;21(1):2-10. 14. Witvrouw E, Callaghan MJ, Stefanik JJ, et al. - Patellofemoral pain: consensus statement from the 3rd International Patellofemoral Pain Research Retreat
JH,
Cartil, 2013;21(10):1504-1513.
23.
ment of knee osteoarthritis. Musculoskeletal Care. 13. Adams T, Band-Entrup D, Kuhn6, etal. Physical therapy management of knee osteoarthritis in the middle-aged
MiMi
1. The therapist places hands at the anterior portion of the tibial plateau.
2. The therapist creates traction at the knee joint usinga foot strap pulling inferiorly.
randomized controlled trial. 1: Clinical effectiveness.
Topr Assoc. 2008;52(4):229-242.
knee pain and disability associated with knee osteoarthritis—a prospective case series. Physiother Theory Pract. 2013;29(2):87-95. Walsh NE, Hurley MV. Evidence based guidelines and current practice for physiotherapy manage-
niques — 7E Knee External Rotation Manual Therapy Tech: niques
ual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a
of a manual therapy knee protocol on osteoarthritic
ical therapy and perturbation exercises in knee osteoarthritis. J Man Manip Ther. 2013;21(4):220-228. li. Takasaki H, Hall T, Jull G. Immediate and short-term
7D Knee Internal Rotat an
7B Knee Flexion (including patella) Manual Therapy Techniques 7€ Knee Extension (including patella) Manual Therapy Techniques
2014;22(2):100-107.
. Pollard H, Ward G, Hoskins W, Hardy K. The effect
10.
7A Knee Genefa Manual Therapy Techniques
2008;337(7677):1006-1007. Simpson BG, Simon CB. Lower extremity thrust and non-thrust joint mobilization for patellofemoral pain syndrome: a case report. J Man Manip Ther.
19.
~ physical therapy and exercise in osteoarthritis of the knee. Ann Inter Med. 2000;132(3):173-181.
Witvrouw E, Werner S, Mikkelsen C, Van Tiggelen
MJ, de
Bie
Viechtbauer RA.
Strength
W,
Lenssen training
AF, alone,
Hendriks exercise
therapy alone, and exercise therapy with passive manual mobilisation each reduce pain and disability in people with knee osteoarthritis: a systematic review. J Physiother, 2011;57(1):11-20. Currier LL, Froehlich PJ, Carow SD, et al. Development of a clinical prediction rule to identify patients with knee pain and clinical evidence of knee osteoarthritis who demonstrate a favorable short-term response to hip mobilization. Phys Ther. 2007;87(9):1106-1119.
FIGURE 7-8
5
=
Manval Therapy Techniques forthe Knee
243
CHAPTER7 Knee
Knee Flexion Patient Position: Supine at the side of the table
7B. Knee Flexion (including patella) Manual Therapy Techniques « Counterstrain technique « Joint manipulation, non-thrust « Myofascial manipulation + Joint manipulation, thrust
s Muscle energy technique « Mobilization with movement
Therapist Position: Standing on the same side of the patient's knee to be treated
¢ Soft tissue manipulation « Self-mobilization
1. The therapist places the cephalad hand on the distal femur/anterior tibial plateau. The caudad hand holds the distal tibia. 2. The therapist lifts the leg and flexes the hip to 90 degrees and kneeto maximum flexion. 3, The therapist places a force at the distal tibia to flex the knee to the end of tissue tension. 4. Atthe tissue barrier, the therapist performs a quick high-velocity low-amplitude (HVLA) thrust.
Patient Position: Supine at the side of the table
Therapist Position: Sitting on the table on the same side of the
FIGURE
r Os
patient's knee to be treated 1. The therapist places both hands at the anterior superior portion of the
tibia. 2. The therapist lifts the leg and flexes the hip to 45 degrees and knee to 90 degrees.
3. The therapist places a posterior force at the tibial plateau pushing the tibia posteriorly.
Patient Position; Seated on the table Therapist Position: Seated in front of the patient
4. Atthe tissue barrier, the therapist can create a progressive oscillation.
5. The tibia can also havea little internal rotation to facilitate the flexion movement of the knee.
1. The therapist places hands at the anterior portion of the tibial plateau. 2. The therapist creates traction at the knee joint using a foot strap.
3. As the knee is flexed, the therapist places a posterior force at the anterior portion of the tibial plateau, 4. The therapist pushes the knee to the restrictive barrier af knee flexion. 5. The patient isometrically contracts the quadriceps (away from the restrictive barrier) into knee extension for 3 to 5 seconds, meeting the therapist's force with 5 Ibs of pressure, and then the patient completely relaxes. 6. Upon relaxation, the therapist pushes the knee into the new restrictive
barrier of flexion. This is repeated until no further relaxation or FIGURE 7-11
FIGURE 7-9 Notes: This can also be papned at deren hip and kneesae The Patient can bela be a belt. The therapist will posteriorly translate the tibia (see Figure B).
with the knee off the table, with femur stabilized with
improvement of range of motion into flexion occurs.
LIMITED KNEE FLEXION
242
Manual Therapy Techniques forthe Knee
244 = CHAPTER? Knee pera sri at el SEN
| Joint: Khe”
a
NAST
245
sacl
:
Knee Flexion Motion’ Limitation Restricted Motion Limited Knee Flexion Ses
greece
iy
Patient Position: Supine
ae
Therapist Position: Standing on the opposite side of the patient
Patient Position: Supine at the side of the table
; Be
Therapist Position: Standing on the involved side of the patient
1. The patient lies supine with the knee extended.
1. The therapist places the cranial hand at the anterior portion of the distal femurand the caudad hand on the anterior tibial plateau and flexes the hip. 2. As the patient flexes the knee the therapist performs an accessory glide to take up all of the tissue tension at the tibia pushing the tibia plateau posteriorly, 3. This is repeated until a great amount of knee flexion is obtained.
2. The therapist places the caudad hand in.a cupping C shape surrounding the superior portion of the patella. The therapist places the cephalad hand on the quadriceps muscle pointing toward the hip. 3. The therapist uses a tissue tension technique to mobilize the fascia. 4, The therapist palpates into the soft tissue and engages the restrictive barrier with a light force in the direction of tension, sometimes up to 3 to 5 minutes. The therapist uses both hands in opposite directions. 5, Aight pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates. FIGURE 7-14
Notes: This can also be ae
adding tibia internal or external rotation. The tibia is the concave surface and would move in the direction of
movement
. Joint: | Knee Knee Flexion Motion Limitation.
ad § ‘Type of Manipulation: Myorascal ranipuanon Restricted Motion: Limited Knee Flexion (Patella) Patient Position: Supine
| oes
Therapist Position: Standing on the side of the patient
of Manipulation: Counterstrain technique
| Restricted Motion: Limited Knee Flexion
1. The patient lies supine with the knee extended. 2. The therapist places the caudad hand in a cupping Cshape surrounding the superior portion of the patella.
Patient Position: Supine, legs straight
Therapist Position: Standing on the side of the patient
3. The therapist uses a tissue tension technique to mobilize the fascia. 4, The therapist palpates into the soft tissue and engages the restrictive
1. The patient lies supine with the legs straight. The therapist palpates the quadriceps that are hypertonic. The therapist presses into the muscle of discomfort and finds the most hypertonic uncomfortable point. The therapist asks the patient to rate the discomfort at a 10/10. 2. The therapist then passively hyperextends the knee and internally/’
barrier with a light force in the direction of tension, sometimes up to 3 to 5 minutes. The therapist uses both hands in opposite directions. 5. Alight pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates.
externally rotates the hips and tibia,
as
3. The therapist then palpates the quadriceps muscle and continues to move the leq until the palpable point is down to a 2/10 discomfort level. . The therapist holds the position for 90 seconds, The therapist does not need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively straightens out the leg and rechecks the point. If the point produces more than 2/10 discomfort
FIGURE 7-13
the treatment is repeated.
Notes: This should decrease the hypertonicity of the quadriceps, allowing the knee to flex a greater distance, This is an indirect technique.
FIGURE 7-15
Notes: This will improve the patella inferior motion. This technique can also be performed in sitting, The therapist can also place the cephalad hand on the quadriceps facing the hip.
i .
LIMITED KNEE FLEXION (PATELLA)
FIGURE 7- 12
247
Self soft tissue manipulation
Patient Position: Prone with bodyweight on a foam rolleror massage ball at the quadriceps Manual soft tissue manipulation
1, The patient places bodyweight with the quadriceps muscles on the
Patient Position: Supine
foam roller.
Therapist Position: Standing on the side of the table
2. The patient can hold statically or rock back and forth to relax the soft
1. The patient lies supine. 2. The therapist palpates the quadriceps muscle and holds deep pressure to relax the muscle. 3. The therapist can perform soft tissue manipulation by gentle strumming and lateral mobilization of the muscles and tendons, with
3, This is repeated until the soft tissue relaxes.
tissues of the muscles.
Circular strokes to increase circulation.
4, This is repeated until the soft tissue relaxes.
FIGURE7-16 Notes: An altemate
ee yi fee
ae can be
ee with theShen
forearm contacting the adic ps muscle, and increased muscle tension can be
a
4 ice
eekneecoe i ure a
Se
oune ellnoe eines, FIGU RE r 166 (CONTINUED
oui ae S
Pa Ce,
$m
Notes: A towel can be placed over the roller or ball to soften the technique, Patient can perform mobilization technique with both hands in standing or St!
Ss pomed
i
_ LIMITED KNEE FLEXION (PATELLA)
iques for theKn ee Manual Therapy Techniques
246 = CHAPTER7 Knee
forthe Knee Monual Therapy Techniques
ocettenion 7C Knee Extension (including patella) Manual Therapy Techniques * Counterstrain technique
+ Joint manipulation, non-thrust
3,seas
the hip and vo 10 be mobilized until tissue barer
* Joint manipulation, thrust
. Myofascial manipulation
« Muscle energy technique
« Soft tissue manipulation
- Mobilization with movement
;
_
© Self-mobilization
hepagent can hold tension statically or rock into flexion.
Patient Position: Prone with thigh supported on the table Therapist Position: aaa on the same side of the patient's knee to be treated
FIGURE7-17_—
1. The therapist places the patient's lower leq with the knee in 20
Notes: A patient can place a rolled towel in the knee crease, As the patient puts weightto create knee flexion the rolled towel pushes the femur _ anteriorly and ‘stretches the knee capsule. Aftera few capsulestretching techniques the patients repeats the knee flexion without the towel roll.
degrees of flexion with the distal hand around the distal portion of the lower leg. 2. The therapist contacts the posterior lower leg with the proximal hand, with the hypothenar eminence close to the joint line.
3. The therapist anteriorly glides the tibia to tissue tension by exerting an anterior and slightly inferior force, while performing a grade 1 distraction with the distal hand.
a ze ns
4. At the tissue barrier, the therapist can create a| progressive oscillation to manipulate the knee capsule. 5, The therapist needs to repeat the technique with tibia external
‘rotation to facilitate the screw-home mechanism by providing the
mobilizing force on the medial side of the posterior tibia.
Notes: External rotation of the tibia occurs during the last 20 degrees of knee extension and tightens bath cruciate ligaments, which allows full knee extension.
250. CHAPTER7 Knee
Manual Therapy Techniques forthe Knee
Patient Position: Supine
Patient Position: Supine at the side of the table
Therapist Position: Standing at the foot of the table
Therapist Position: Standing on the involved side of the patient
1, The therapist places both hands on the proximal tibia and stabilizes the foot between the elbow and thorax.
1. The therapist places the cranial hand distal femur and the caudad hand at posterior tibial plateau with the lower leg being held up and squeezed between the upper arm and body.
2, The patient's lower leq is placed in 20 deqrees of knee flexion.
3. The therapist extends the knee and externally rotates the tibia to
2. The patient extends the knee and the therapist rotates the tibia into external rotation. 3, With the tibia in external rotation, the therapist performs an accessory
tissue tension. 4, At the tissue barrier, the therapist performs a HVLA thrust distracting
the tibia inferiorly with external tibia rotation,
FIGURE 7-19
extension,
Patient Position: Supine Therapist Position: Standing on the involved side of the patient 1. The therapist places the cranial hand at the anterior portion of the distal femur and the caudad hand around the malleolus. 2. The therapist creates traction at the knee joint by pulling inferior on the malleolus.
3. The therapist stabilizes the femur and extends the knee by lifting the tibia to maximal knee extension to the restrictive barrier, 4. The patient isometrically contracts the hamstrings into knee flexion
(away from the restrictive barrier) for 3 to 5 seconds, meeting
FIGURE 7-20
glide to take up all of the tissue tension in a posterior direction of the femoral glide, 4, Each time the patient extends the knee the therapist externally rotates
FIGURE 7-21
Notes: Extemal rotation of the tibia occurs during the last 20 degrees of knee extension and tightens both cruciate ligaments, which allows full knee
the therapist's force with 5 Ibs of pressure, and then the patient completely relaxes. 5, Upon relaxation, the therapist pushes the knee into the new restrictive barrier extension and tibial external rotation. This is repeated until no further relaxation or improvement of range of motion into extension occurs.
‘Notes: External rotation of the tibia occurs during the last 20 degrees of knee extension ‘and tightens bothcruciate liga ments, which allows full kn ee See extension.
251
the tibia and performs a posterior accessory glide of the fernur. This is repeated until a greater amount of knee extension is obtained. eerie woe ea
CHAPTER? Knee
Manual Therapy Techniques for the Knee
Knee Extension Motion Limitation
253
Hissar
Patient Position: Prone Patient Position: Supine
Therapist Position: Standing on the involved side of the patient
Therapist Position: Standing on the side of the patient 1. The patient lies supine with the knee extended 2. The therapist places the caudad hand in a cupping C shape
surrounding the inferior portion of the patella. The therapist places the cephalad hand on the tibia pointing toward the feet.
rm
1. The patient lies prone with the legs straight. The therapist palpates the hamstring muscles that are hypertonic. The therapist presses into the muscles of discomfort and finds the most hypertonic uncomfortable point. The therapist asks the patient to rate the discomfort at a 10/10. . The therapist flexes the knee and rotates tibia until the palpable point is down to a 2/10 discomfort level. The therapist may need to also extend the hip by placing a knee under the patient's thigh and rotating the hip to get further relaxation. . The therapist holds the position for 90 seconds. Once the 90 seconds afe up, the therapist passively straightens out the leg and rechecks the point in the original position. If the point produces more than 2/10 discomfort the treatment is repeated.
3. The therapist uses a tissue tension technique to mobilize the fascia.
4. The therapist palpates into the soft tissue and engages the restrictive barrier with a light force in the direction of tension, sometimes up to 3
(os)
to.5 minutes. The therapist uses both hands in opposite directions. 5. A light pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates, FIGURE 7-23
Notes: This will allow the patella to glide superiorly,
Joint: Knee
:
|| Type of Manipulation: Myofascial manipulation
_ Knee Extension Motion Limitation:
_ Restricted Motion: Limited Knee Extension — Patient Position: Supine Therapist Position: Standing on the side of the patient 1. The patient lies supine with the knee extended and stabilizes the pelvis with a posterior pelvic tilt 2. The therapist brings the leg up in a straight leg position until the tissue barrier. The therapist places the caudad hand on the hamstrings facing the pelvis. The therapist places the cephalad hand on the hamstrings pointing toward the tibia.
FIGURE 7-22 Notes: This should decrease the hypertonicity of the hamstring muscle, allowing the knee to extend a greater distance. Ifit is the medial hamstrings, internally rotate the tibia and if the lateral hamstring, externally rotate the tibia. This is an indirect technique. This technique can be used for hypertonic hamstrings that are limiting knee extension of tibial rotation. See also the counterstrain technique for the gastrocnemius, which can also function asa knee flexor.
a }
FIGURE 7-24
3. The therapist uses a tissue tension technique to mobilize the fascia. 4, The therapist palpates into the soft tissue and engages the restrictive
barrier with a light force in the direction of tension, sometimes up to 3 to 5 minutes, The therapist uses both hands in opposite directions. 5. Alight pressure on the barrieris held until the tissue barrier softens and relaxes and the myofascial unit elongates.
LIMITED KNEE EXTENSION
252
Manual Therapy Techniques for theKnee
U
i
§=.2.55
Manual soft tissue manipulation Patient Position: Prone
Patient Position: Standing
1, The patient stands with a band or mobilization strap around the superior portion of the tibia.
Therapist Position: Standing on the involved sideof the patient
2. The patient starts with knee flexion and actively extends the knee, which will create a greater traction on the belt. The belt traction will
1, The patient lies prone.
pull the tibia anteriorly,
2. The therapist palpates the hamstrings and holds deep pressure with the knee bent (see Figure A). 3. The therapist can perform soft tissue manipulation by gentle strumming and lateral mobilization of the muscles and tendons, and
3. The patient extends the knee to be mobilized until tissue bamier is
met. 4. The patient can hold tension statically or rock the knee into extension
by getting an increased anterior glide on the tibia from the belt
with circular strokes to increase circulation. 4, This is repeated until the soft tissue relaxes.
Self soft tissue manipulation
Patient Position: Seated with bodyweight on a foam roller or massage ball (see Figure C) 1. The patient places bodyweight with the hamstring muscles on the foam roller. 2. The patient can hold statically or rock back and forth to relax the soft tissues of the hamstring muscles. 3, This is repeated until the soft tissue relaxes,
FIGURE 7-26 FIGURE 7-25
Notes: The manual technique can be performed in supine (see Figure B). A towel can be placed over the roller to soften the technique,
Notes: The patient can push the femur posteriorly while sitting, See Figure C.
LIMITED KNEE EXTENSION.
CHAPTER7 Knee
" My4M)
254
Manual Therapy Techniques tor theKnee
CHAPTER? Knee
257
women (ieee |
oineknee Se
Knee Internal Rotation
i Knee InternalRotation Motion Limitation Knee Internal Rotation Manual Therapy Techniques Joint manipulation, non-thrust Joint manipulation, thrust Muscle energy technique Mobilization with movement
e « «
Counterstrain technique Myofascial manipulation Soft tissue manipulation Self-mobilization
Patient Position: Supine
Therapist Position: Standing at the side of the table 1. The therapist places the cranial hand on the tibial plateau and the caudal hand around the malleolus. 2. The patient's lower leg is placed in 120 degrees of knee flexion.
U
« « « «
U
7D.
a
+ -non-thrust heRestricted Motion: Limited knee/Ti bial
3. The therapist internally rotates the tibia to tissue tension.
Ue U
| Type of Manipulation: Joint manipulation,
4, At the tissue barrier, the therapist performsa HVLA thrust into internal tibia rotation with the cranial hand, while the caudal hand thrusts the
wee _Internal Rotation
an anteriorly directed force with the lateral hand on the tibia when mobilizing the right knee. 4. Atthe tissue barrier, the therapist can createa progressive oscillation to manipulate the knee capsule in an internal rotary direction.
FIGURE 7-27
Notes: This can also be performed in sitting and different knee joint angles.
Notes: The therapist can place both hands on the tibial plateau and support the lower leg between the arm and body,
' Joint: Knee i Knee Internal Rotation Motion Limitation
|| Type of Manipulation: Muscle energy technique — __ | Restricted Motion: Limited Knee/Ti bial | Internal Rotation~ Patient Position: Supine Therapist Position: Standing on the involved side of the patient
mS
rotates the foot. 2. The therapist places hands at the medial and lateral tibia plateau. 3. The therapist internally rotates the tibia without motion at the femur by providing a posteriorly directed force with the medial hand and
FIGURE 7-28
we)
1. The therapist places the knee at 90 degrees of flexion and internally
. The patient lies supine and the therapist places the cephalad hand on the femoral condyles and the caudal hand on the distal tibia/fibula. . The therapist flexes the knee to 90 degrees and internally rotates the tibia to the restrictive barrier. The patient isometrically rotates the foot and lower leg into external
rotation (away from the restrictive barrier) for 3 to 5 seconds, meeting the therapist’ force with approximately 5 lbs of pressure, and then the patient completely relaxes. t.
Therapist Position: Standing at the foot of the bed
rnknuuueagseeceecccececcece.
Patient Position: Supine with knee flexed to 90 degrees
knee into flexion.
FIGURE 7-29
Notes: This can also be performed in sitting. This is an indirect technique
Upon relaxation, the therapist rotates the tibia into the new restrictive
barrierof internal rotation. This is repeated until no further relaxation or improvement of range of motion into tibial internal rotation occurs.
LIMITED KNEE/TIBIAL INTERNAL ROTATION
256
258
CHAPTER7 Knee
Manual Therapy Techniques for the Knee
259
[| Joint: eee
f Knee Internal Rotation Motion Patient Position: Prone
s
Therapist Position: Standing/seated on the involved side of the patient
— LS,
J, The patient sits with the knee bent at 90 dearees. 2. The therapist places the cranial hand at the distal portion of the femur and the caudad hand at the tibial plateau.
=,
4. As the lower leg is internally rotated, the therapist performs an accessory glide to take up all of the tissue tension and internally rotate the tibia by placing a thumb on the anterior medial surface of the tibial
ae
plateau and fingers wrapped around the fibula and tibia posteriorly.
—
ha
Le5,
3. The patient actively internally rotates the lower leq pivoting on the calcaneus,
wn
ihe,
5. This.is repeated until a greater amount of knee internal rotation is obtained.
nan
Bay
i| Type of Manipulation: Counterstrain technique-
Useey sey
| Restricted Motion: Limited Knee/Tibial
ij ry
a} | Internal Rotation
uniy
sey
Patient Position: Prone
oiey
Therapist Position: Standing on the side of the patient
uey
rey rey ey
BS
|. The patient lies prone with the legs straight. The therapist palpates the biceps femoris muscle that is hypertonic. The therapist presses into the muscles of discomfort and finds the most hypertonic uncomfortable point. The therapist asks the patient to rate the discomfortat a 10/10. The therapist flexes the knee to 90 degrees and laterally rotates the tibia until the palpable point is down toa 2/10 discomfort level. The therapist may need to compress the tibia into the femur to get further relaxation. The therapist holds the position for 90 seconds. The therapist does
nay
ce
ke
oe
not need to place pressure on the point for the 90 seconds. Once the
90 seconds are up, the therapist passively straighten out the leg and rechecks the point in the original position. If the point produces more
Le
2
than 2/10 discomfort the treatment is repeated.
os |
=
=
4. At the tissue barrier, the therapist can createa HVLA thrust in an anterior direction.
cer
|
= a
me
Type of Manipulation: Joint manipulation, thrust
Patient Position: Supine at the side of the table
|
=
barrier.
—
Therapist Position: Standing on the same side of the patient's lower leg to be treated
|
ay
Ces Al a 4 a J &
—
:
A =
Ge rine ee, i _
=
Joint: Ankle Ankle Plantarflexion Motion Limitation
. The patient lies prone with the talus and
Seu
Ci miT z
; .
|
—
Sec
Saal SE, Cire
Notes: Plantarflexion of the ankle goes along with inversion of the foot. Mnemonicis PIP: A Posterior fibular head goes with ankle Inversion and ankle Plantarflexion. Restoring mobility of the PTH should be considered when treating ankle joint restrictions.
'
ee
——,
stabilize in internal rotation and plantarflexion at the ankle.
|
Therapist Position: Standing at the foot of the table
4
=z x aa ts Mae = =
Patient Position: Prone with the foot off the table
:
gi Cc
Type of Manipulation: Joint manipulation, thrust Restricted Motion: Limited Ankle Plantarflexion (Talocrural Joint)
Joint: Ankle Ankle Plantarflexion Motion Limitation
w . _
c ia Cc
3. Atthe tissue barrier of the posterior fibula head glide, the therapist createsa progressive oscillation in a posterior direction.
S
Notes: Plantarflexion of the ankle goes along with inversion of the foot. Mnemonic is PIP: A Posterior fibular head goes with ankle Inversion and ankle Plantarflexion. Restoring mobility of the PTF! should be considered when treating ankle joint restrictions.
_ Upon relaxation, the therapist pushes the ankle to the new restrictive barrier of plantarflexion. This is repeated until no further relaxation or improvement of range of motion into dorsiflexion occurs.
FIGURE 8-23
©
Notes: This technique can also be performed in supine, This technique is useful when joint glides are painful or significant muscle guarding is present.
movement Restricted Motion: Limited Ankle Plantarflexion (Talocrural Joint)
_ Joint: Ankle Ankle Plantarflexion Motion Limitation
Patient Position: Prone with the knee bent. Therapist Position: Seated on the same side of the patient's lower leg to be treated
(ox)
The therapist places the cephalad hand on the dorsum of the foot. The caudad hand is on the calcaneous. As the patient plantarflexes the ankle, the therapist performs an
ao
mS
. The knee is bent to 90 degrees.
anteriorly, This is repeated with the patient actively plantarflexing the ankle
accessory glide to take up all of the tissue tension and glides the talus
with the therapist performing an anterior talus glide until there is an increase in plantarflexion.
Cea o
1}
Sill rl
FIGURE 8-24 4
——
:
=
oie
:
-
———
Notes: Technique is useful when joint glides are painful.
Joint: Ankle Ankle Plantarflexion Motion Limitation
/
|
x.
Joint: Ankle Ankle Plantarflexion Motion Limitation
Type of Manipulation: Counterstrain
1. The patient lies supine. 2. The therapist places the caudad hand on the dorsum of the midfoot and the cephalad hand on the anterior lower tibia. 3. The therapist uses a tissue tension technique to mobilize the fascia into plantarflexion and ankle inversion, 4. The therapist palpates into the soft tissue and engages the restrictive barrier with a light force in the direction of tension, sometimes up to.3 to S minutes. The therapist uses both hands in opposite directions.
5. Alight pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates. FIGURE 8-26 Notes: lechnique is useful in the presence of myofascial restrictions that contribute to decreased joint mobility.
Joint: Ankle
Ankle Plantarflexion Motion Limitation
e)
Patient Position: Supine
er dN
1, The patient lies supine. The therapist palpates the anterior tibialis muscle that is hypertonic. 2. The therapist presses into the muscles of discomfort and finds the mast hypertonic uncomfortable point. The therapist asks the patient to rate the discomfort ata 10/10. 3, The therapist dorsiflexes the ankle and everts the rear foot until the palpable point is down to a 2/10 discomfort level, 4, The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively Straightens out the legs and rechecks the point in the original position, Ifthe point produces more than 2/10 discomfort the treatment is repeated,
Notes: This should decrease the hypertonicity of the anterior tibialis, allowing the ankle to plantarflex a greater distance.
Patient Position: Prone Therapist Position: Standing on the involved side of the patient 1. The patient lies prone.
2, The therapist flexes the knee and dorsiflexes the ankle. 3. The therapist palpates the anterior tibialis and holds deep pressure. 4. The therapist can perform soft tissue manipulation by gentle strumming and lateral mobilization of the muscles and tendons, and with circular strokes to increase circulation.
iS
é.
Coan €
Se cc
i t
©
a,
Cnn.
ane ©
let
c 7 Kl
$
onl
3
SisLg 2
Type of Manipulation: Soft tissue manipulation Restricted Motion: Limited Ankle Plantarflexion Manual soft tissue manipulation
=i
CA Cc ar
Type of Manipulation: Myofascial manipulation Restricted Motion: Limited Ankle Plantarflexion
Therapist Position: Standing/seated at the foot of the patient
ATL, Si &,
technique Restricted Motion: Limited Ankle Plantarflexion
295
Patient Position: Supine
Si
.
Therapist Position: Standing on the involved side of the patient
es
lp
Manual Therapy Techniques for theAnkle
FIGURE 8-27
IMITED ANKLE PL ANTARFLEXION
Type of Manipulation: Mobilization with
OP OPOUPURUECRL Ett OCC leg ee ee
= CHAPTER 8 Ankle
AN\9 No AA, Banas ab
294
CHAPTERS Ankle
Self soft tissue manipulation
FEY a4! Pe » {Net Not Net et bet bed dot coe 06
Patient Position: Kneeling with bodyweight on a foam roller or massage ball 1, The patient places bodyweight with the anterior tibialis muscle on the foam roller with the hips and knees bent, 2. The patient can hold statically or rock back and forth to relax the soft
8D Ankle inversion Manual Therapy Techniques * Joint manipulation, non-thrust « Joint manipulation, thrust
+ Muscle energy technique * Mobilization with movement
Patient Position: Supine or long sitting Therapist Position: Standing at the foot of the table
woes
1, The patient’s ankle in placed in slight plantarflexion. 2, The therapist places the cephalad hand around the distal tibia and fibula and the caudad hand on the medial to posterior portion of the calcaneus. 3. The therapist distracts the subtalar joint. 4. Atthe tissue barrier of calcaneal inversion, when the calcaneus is mobilized with a medial glide on the posterior portion of the calcaneus, the therapist can create a progressive oscillation at the tissue barrier,
CoP iF
=
\
We
X
5. This can be statically held or rocked further in plantarflexion,
FIGURE 8-28
a
Notes: Can be combined with a hold-relax to facilitate movement.
+ Self-mobilization
Joint: Ankle
a
« 1D a.
=|
a ae
“L i
fot
oe
placed on the dorsum of the forefoot. 3, The patient plantarflexes the ankle. 4, At the tissue barrier, the patient pushes the ankle into plantarflexion,
‘a, 4
rand
1. The patient is seated with the leg crossed in front of them,
2. The patient places the opposite hand of the involved extremity at the calcaneus. The hand on the same side of the involved extremity is
—
Patient Position: Seated
\a 4a A
\
4
= | -, ol
estricted Motion: Limited Ankle Plantarflexion
! fet
Typeof Manipulation: Self-mobilization _
+ Myofascial manipulation « Soft tissue manipulation
ins
{
Notes: A towel can be placed over the roller or ball to soften the technique (see Figure B. and C.).
« Counterstrain technique
~ Ankle Inversion Motion Limitation~
—
eeeeel
my ‘! LOA \K yf ¥= ‘
FIGURE 8-27 (CONTINUED)
297
Ankle Inversion
==
4
tissues of the anterior tibialis muscles. 3. This is repeated until the muscle relaxes.
Manual Therapy Techniques forthe Ankle
FIGURE 8-29
Notes: Technique is useful in restoring supination mobility of the ankle/foot complex.
LIMITED ANKLE INVERSION
Ei
296
fe
SURES 0
. Patient lies on the side with the talus off the edge of the wedge or table, . The therapist stabilizes the talus with one hand and grasps the calcaneus with the other hand. . The therapist places traction on the calcaneus and then inverts the calcaneus. . Atthe tissue barrier of the calcaneus and talus, the therapist creates d HVLA thrust on the posterior portion of the calcaneous in a medial direction,
e
Notes: Thrust technique can be useful to address joint restrictions that do not respond to the application of non-thrust techniques.
fb =
i
2 ted —
At the patient actively inverts the foot, the therapist distracts the
=i
subtalar joint and performs an accessory glide of the calcaneus to
take up all of the tissue tension and glides the calcaneus with a varus stress. The anterior portion of the calcaneous is glided laterally while the This is repeated each time the patient actively inverts the foot.
posterior portion is glided medially.
FIGURE 8-32
Notes: The capsular pattern is limited inversion.
Type of Manipulation: Counterstrain technique Restricted Motion: Limited Ankle Inversion
me,
Patient Position: Supine
ve ATO
Therapist Position: Sitting on the involved side of the patient 1. The patient lies supine with the knee slightly bent. The therapist palpates the lateral calcaneus, ankle everters, and the anterior talofibular ligament. The therapist presses into the muscles/ligaments
of discomfort and finds the most hypertonic uncomfortable point. The therapist asks the patient to rate the discomfort ata 10/10.
Tk
uns 1S Py
mw
1 &
AR
$
ue
=
fils
re "|
|
. The therapist passively everts the ankle with dorsiflexion and plantarflexion until the palpable point is down toa 2/10 discomfort
level.
&
Motion into inversion occurs.
Notes: This technique is useful when joint glides are painful or significant muscle quarding is present.
Ankle Inversion Motion Limitation
ce i e
+, 5
FIGURE 8-31
. The therapist places the cranial hand on the midfoot and the caudal hand at the posterior portion of the calcaneus. . The therapist distracts the calcaneus from the talus and inverts the subtalar joint and midfoot to the restrictive barrier. . The patient isometrically contracts the foot into eversion (away from the restrictive barrier) for 3 to 5 seconds, meeting the therapist's force with 5 Ibs of pressure, and then the patient completely relaxes. . Upon relaxation, the therapist glides the anterior portion of the calcaneous laterally while the posterior portion is glided medially and takes up the additional tissue slack to the new restrictive barrier. This is repeated until no further relaxation or improvement of range of
fn NADA
-—
pes)
ns
Therapist Position: Seated or standing at the foot of the bed
e)
Joint: Ankle
ka
Patient Position: Supine
yy
. The therapist holds the position for 90 seconds. The therapist does not need to place pressure on the point for the 90 seconds, Once the
90 seconds are up, the therapist passively straightens out the leq and FIGURE 8-33
=
. The therapist places the cephalad hand around the midfoot and the heel of the caudad hand on the inferior portion of the calcaneus.
ae, a
Lael Ned
Therapist Position: Seated at the foot of the table
JAI,
Type of Manipulation: Muscle energy technique Restricted Motion: Limited Ankle Inversion
wy
==
Te
Joint: Ankle Ankle Inversion Motion Limitation
S
Patient Position: Supine
m
la
nm
Therapist Position: Standing on the uninvolved side of the patient
Type of Manipulation: Mobilization with movement Restricted Motion: Limited Ankle Inversion
hat
Patient Position: Sidelying with wedge
Joint: Ankle Ankle Inversion Motion Limitation
a
Restricted Motion: Limited Ankle Inversion
s
Type of Manipulation: Joint manipulation, thrust
Ankle Inversion Motion Limitation
Le
299
f'
=
«Joint: Ankle
or
Manual Therapy Techniques forthe Ankle
74
CHAPTERS Ankle
AYAAAAAAAAAHHHHHHNO NNOLOLOOL OLA,=_ NSO,O,O\9) AAA S3385a8) BREE! aap EC Gt bt nt be i he 60 Je le le le HLCM
298
rechecks the point in the original position. lf the point produces more than 2/10 discomfort the treatment is repeated.
Notes: Technique can be useful in the presence of muscle hypertonicity or myofascial restrictions.
==
Sometimes up to 3 to. 5 minutes. The therapist uses both hands in opposite directions.
5. A light pressure on the barrier is held until the tissue barrier softens
and relaxes and the myofascial unit elongates.
FIGURE 8-34
Joint: Ankle Ankle Inversion Motion Limitation
Type of Manipulation: Soft tissue manipulation Restricted Motion: Limited Ankle Inversion Manual soft tissue manipulation Patient Position: Supine Therapist Position; Seated at the foot of the table 1, The patient lies supine with the knee extended. 2, The therapist places their thumb and fingers around the peroneus
muscles and holds deep pressure. 3, The therapist can perform soft tissue manipulation by gentle strumming and lateral mobilization of the muscles and tendons, with circular strokes to increase circulation.
FIGURE 8-35
ee,
soft tissues of the peroneal muscles.
3. This is repeated until the soft tissue relaxes.
FIGURE 8-35 (CONTINUED) Notes: The muscles in the lateral compartment of the lower leg can restrict motion into inversion.
Joint: Ankle Ankle Inversion Motion
Limitation =
Type of Manipulation: Self-mobilization Restricted Motion: Limited Ankle Inversion Patient Position: Seated with the leg crossed over the lower leq 1. The patient crosses the leg over the thigh. 2. The patient inverts the foot by grasping the calcaneus until tissue
barrier is met. 3. The patient can hold tension statically or rock the ankle into inversion by getting an increased medial glide on the calcaneus.
FIGURE 8-36
Notes: Patient can use hald-relax technique to facilitate movement
Li M ITED ANKKLE INVERSION
Id Cet mt ot tbe 016 ee le |
a
into ankle inversion.
4. The therapist palpates into the soft tissue and engages the restrictive barrier with a light force in the direction of tension,
eee
mo
. The therapist places the cephalad hand around the malleolus to stabilize the distal tibia and fibula. The caudad hand (palm) is over the lateral posterior portion of the midfoot. 3, The therapist uses a tissue tension technique to mobilize the fascia
1. The patient places the massage roller aver the peroneal muscles. 2. The patient can hold statically or rock back and forth to relax the
DOR
. The patient is sidelying with the leg bent.
Patient Position: Seated with the knee bent and the leg internally rotated
HOA
Therapist Position: Seated on the involved side of the patient
301
Self soft tissue manipulation
Det ooo.
Patient Position: Sidelying on the uninvolved side
Manual Therapy Techniques forthe Ankle
f.
Restricted Motion:.Limited Ankle Inversion
==5
Type of Manipulation: Myofascial manipulation
a
'
CHAPTERS Ankle
Joint: Ankle Ankle Inversion Motion Limitation
i
’
HHH AHHH AH AN ANAY CAAA, ) MAAAARALAIAAASAAAAHH
300
non-thrust Restricted Motion: Limited Ankle Eversion Patient Position: Seated Therapist Position: Seated at the foot of the table 1. The patient’s ankle is in placed in slight dorsiflexion. 2. The therapist places the cephalad hand around the lateral portion of the calcaneus and the caudad hand on the medial portion of the calcaneus. 3, The therapist distracts the subtalar joint. 4. At the tissue barrier, the anterior portion of the calcaneus is
mobilized medially while the posterior portion is mobilized laterally,
ODOR DY ID DLL
i
i
=
Notes: Alternate Figure B: Patient lies supine with the leg bent over the therapist's knee. The therapist places thumbs on the medial posterior portion of the calcaneus. The therapist's fingers stabilize the talus. At the tissue barrier, the therapist creates a joint glide in a lateral direction on the posterior calcaneus. Eversion is 4 component motion of pronation of the ankle/foot complex.
N KY
FIGURE 8-37
el a
a se
Therapist Position: Standing on the involved side of the patient ]. The patient lies supine with the leg extemally rotated. 2. The therapist crosses hands with one hand on the calcaneus and the other hand on the navicular. 3. The therapist pushed hands apart to distract the calcaneus. 4. Atthe tissue barrier of the calcaneus and talus, the therapist creates a HVLA thrust in a lateral direction on the posterior calcaneus.
Notes: As an alternate technique (Figure 8), the therapist can place the thenar eminence on the medial calcaneous and the other hand thenar
eminence on the medial portion of the navicular. The therapist thrust the calcaneus in a lateral direction. This can also be performed as a cross arm technique. The joint plane is about 30 degrees anteromedial/posterolateral.
t
j q
Restricted Motion: Limited Ankle Eversion
LIMIT ED ANKLE EVERSIO
Type of Manipulation: Joint manipulation, thrust
FIGURE 8-38
|i
i
— oa omc
5. The therapist can create a progressive oscillation.
t f
OC 8 Bek
; Type of Manipulation: Joint manipulation, Joint; Ankle Ankle Eversion Motion Limitation
303
Patient Position: Supine at the side of the table.
No Meg le to af ed ot ol bE
¥
* Mobilization with movement
* Myofascial manipulation « Soft tissue manipulation » Self-mobilization
Joint: Ankle Ankle Eversion Motion Limitation
Pee eet Me
» Muscle energy technique
* Counterstrain technique
Manual Therapy Techniques for the Ankle
DA
« Joint manipulation, non-thrust * Joint manipulation, thrust
Ll =
8E Ankle Eversion Manual Therapy Techniques
te
=
‘
Ankle Eversion
BOD
i
CHAPTERS Ankle
AnnAAA AHADDA.BAGHHHHHHHHHAHHHAAAND Way ALAA4ALA, {Bea 443a: aa
302
CHAPTER 8 Ankle
Manual Therapy Techniques forthe Ankle
305
Patient Position: Supine Patient Position: Seated
Therapist Position: Seated at the foot of the bed
Therapist Position: Seated at the foot of the table
1, The therapist places the cephalad hand on the talus and midfoot and
the caudal hand at the inferior portion of the calcaneus. 2. The therapist distracts the calcaneus and everts the subtalar joint and midfoot to the restrictive barrier. 3. The patient isometrically contracts the foot into inversion (away from the barrier) for3 to 5 seconds with approximately 5 lbs of pressure and then the patient completely relaxes. 4 Upon relaxation, the therapist glides the calcaneous laterally to new restrictive barrier of ankle eversion. This is repeated until no further
1. The therapist places the cephalad hand around the lower leq and the heel of the caudad hand on the inferior portion of the calcaneus. 2. As the patient actively everts the foot, the therapist distracts the subtalar jointand performsa medial accessory glide of the calcaneus to take up all of the tissue tension and glides the calcaneus with a valgus stress. 3. The anterior joint is glided medially while the posterior jaint is glided laterally. 4. This is repeated each time the patient actively everts the foot.
relaxation or improvement of range of motion into eversion occurs. FIGURE 8-40
Notes: Technique is useful in the presence of muscle quarding or hypertonicity.
“Joint Ankle = _ Ankle Eversion Motion Limitation
Type of Manipulation: Counterstrain technique Restricted Motion: Limited Ankle Eversion = Patient Position: Supine
=
Therapist Position; Standing on the involved side of the patient
. The patient lies supine with the knee slightly bent. The therapist
FIGURE 8-39
ia
need to place pressure on the point for the 90 seconds. >
AAA
mw
Notes: This technique is useful when joint glides are painful or significant muscle quarding is present.
palpates the medial calcaneus, ankle inverters, and the deltoid ligament. The therapist presses into the muscles/ligaments of discomfort and finds the most hypertonic uncomfortable point The therapist asks the patient to rate the discomfort at a 10/10. The therapist passively inverts the ankle with dorsiflexion and plantarflexion until the palpable point is down to a 2/10 discomfort level. The therapist holds the position for 90 seconds. The therapist does not
ieee
Once the 90 seconds are up, the therapist passively straightens out the legs and rechecks the point in the original position. Ifthe point produces more than 2/10 discomfort the treatment is repeated.
Notes: This technique is useful when joint glides are painful, or sig nificant muscle quarding is present.
LIMITED ANKLE EVERSION |
304
CHAPTERS Ankle
Manual Therapy Techniques for the Ankle
307
Self soft tissue manipulation
Patient Position: Sidelying on the uninvolved side Patient Position: Supine at the side of the table
1. The patient places a ball under the posterior tibialis muscle.
Therapist Position: Standing on the involved side of the patient
2. The patient can hold statically or rock back and forth to relax the soft tissues 3. This is repeated until the muscle relaxes,
1. The patient lies supine with the leg bent. 2. The therapist places the thumbs on the medial posterior portion of the calcaneus. The therapist's fingers are wrapped around the inferior and lateral portion of the calcaneus as the therapist performs traction of the calcaneus. 3, The therapist uses a tissue tension technique to mobilize the fascia into ankle eversion. 4. The therapist palpates into the soft tissue and engages the restrictive barrier with a light force in the direction of tension, sometimes up to 3 to 5 minutes. The therapist uses both hands in opposite directions. FIGURE 8-42
Notes: The moe
FIGURE 8-43 (CONTINUED) Notes: The muscles u Me Us ial compartment can restrict motion into eversion.
5. A light pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates. a the medial compartment can restrict motion into eversion.
Joint: Ankle Ankle Eversion Motion Limitation
a Type of Manipulation:
ae
1. The patient crosses the leg over the opposite thigh. 2. The patient everts the foot by grasping the calcaneus until the tissue barrier is met. 3. The patient can hold tension statically or rock the ankle into eversion
Manual soft tissue manipulation Patient Position: Supine
by getting an increased lateral glide on the calcaneus.
Therapist Position: Standing on the involved side of the patient 1. The patient relaxes the foot into slight plantarflexion. 2. The therapist palpates the posterior tibialis tendons and holds deep
pressure, 3, The therapist can perform soft tissue manipulation by gentle
strumming and lateral mobilization of the muscles and tendons, and FIGURE 8-44
Notes: Patient can incorporate a hold-relax technique into this mobilization. FIGURE 8-43
NGatone
Patient Position: Seated with the leg crossed over the lower leg
Tipe of MaRIDUISHOR: Soft tissue ti manipu lation Restricted Motion: Limited An kle Eversion
with circular strokes to increase circulation.
s
: Restricted Motion: Limited Ankle Eversion.
LIMITED ANKLE EVERSION
306
CHAPTER
Foot Chapter Outline Introduction and discussion of the foot joint biomechanics and related manual therapy information.
9A Midfoot Pronation Manual « + + +
Therapy Techniques Joint manipulation, non-thrust Joint manipulation, thrust Muscle energy technique Mobilization with movement
- Muscle energy technique + Mobilization with movement + Counterstrain technique + Myofascial manipulation + Soft tissue manipulation - Self-mobilization
~ Counterstian technique + Myofascial manipulation + Soft tissue manipulation - Self-mobilization 9F Forefoot Plantarflexion Manual Therapy Techniques
+ Counterstrain technique
9C Forefoot General Manual
+ Joint manipulation, non-thrust
+ Myofascial manipulation = SORE monipetation
Therapy Techniques 9D Forefoot Dorsiflexion Manual
« Joint manipulation, thrust + Muscle energy technique
~ Self-mobilization 98 Midfoot Supination Manual
Therapy Techniques + Joint manipulation, non-thrust
+ Mobilization with movement - Counterstrain technique
Therapy Techniques
+ Joint manipulation, thrust
+ Myofascial manipulation
~ Joint manipulation, non-thrust
+ Muscle energy technique
« Soft tissue manipulation
+ Joint manipulation, thrust
- Mobilization with movement
+ Self-mobilization
LEARNING OBJECTIVES Upon completion of this chapter, the reader will be able to: - Describe the anatomy and biomechanics of the foot . Understand the state of the evidence for the use of manual therapy treatment techniques of the foot - Perform the 8 types of techniques for each of the directions of joint motion restriction - Delineate the basic steps for the application of each type of technique
“CHAPTER 9 Foot
Introduction
the lateral side (see MT@TZE).
supination action of the foot, resulting in increased —
_ Fibularis longus tendon
rigidity of the ankle/foot complex during the late
ints of the midfoot include the transverse
The forefoot joints include the tarsometatarsal,
stance and toe-off phases ofthe gait cycle. The tib-
_ tarsal joint’ and the intertarsal joints, includ-
the intermetatarsal, metatarsalphalangeal, and inter-
jalis posterior muscle is a prime mover for subtalar
phalangeal joints. The tarsometatarsal (Lisfranc)
and midtarsal joint supination and contributes to maintaining the longitudinal arch of the foot and controlling pronation during the stance phase. The flexor hallucis longus and digitorum longus are prime movers for flexion of the toes and contribute to maintaining the longitudinal arch.'** The peroneus longus and brevis muscles are located in the lateral compartment and are prime movers for pronation at the subtalar and midtarsal
i articulations between the navicular, cuboid, and cuneiform bones (also referred to as the cubonavicular cuneiform joint’). The transverse tarsal (midtarsal, or Chopart) joint consists of the calcaneocuboid and talonavicular joints. The joints of the midfoot together can be considered _as a functional ball and socket joint, with move-
ment occurring in response to movements of the subtalar joint (see The functionalrelationship between the talonavicular and the anterior compartment of the subtalar joint is further illustrated by the fact that these joints have a shared joint capsule. The closed-packed position of this joint is full supination, and the loose-packed position is pronation.* The joints of the midfoot are supported by the spring ligament (plantar calcaneonavicular ligament) and the short and long plantar ligaments on the plantar side, the deltoid ligament
joints are planar synovial joints, allowing for gliding motions. The closed-packed position of these joints is supination.* The metatarsophalangeal (MTP) joints are condyloid synovial joints with 2 degrees
of freedom: flexion extension and abduction/adduction. The joint surfaces of the MTP joints consist of the convex metatarsal heads and the concave bases
of the phalanxes. The closed-packed position of
joints. The insertion of the peroneus longus at the
these joints is full extension, and the loose-packed
medial cuneiform bone and the base of the first
position is 10 to 20 degrees of extension. The MTP joints
primary
have
a weight-bearing
joint being critical during the late stance and toeoff phase of the gait cycle.’ The interphalangeal joints are synovial hinge joints, allowing for flexion and extension. The closed-packed position of these joints is full extension, and the loose-packed position is slight flexion.
calcaneonavicular ligament i Short plantar ligament Calcaneal tubercle
Galcaneocuboid joint
extensor digitorum and hallucis longus are prime
movers for toe extension. The extensor hallucis
FIGURE9-2 Plantar ligaments of the foot The musculature of the ankle/foot complex plays an important role in the stability of the ankle/ amentous
— Hindfoot
Tarsometatarsal (Chopart's) joint
located in the anterior compartment include the tibialis anterior, the extensor digitorum longus, and the extensor hallucis longus muscles. The
Long plantar ligament
foot complex, in addition to the structural and lig-
Dorsal view
Transverse tarsal (Lisfranc’s) joint
metatarsal allows for a contribution to the stability of the transverse arch of the foot. The muscles
function,
with sufficient extension especially of the first MTP
— Tarsals
J
ie
on the lateral side, and the bifurcate ligament on
)
— Midfoot
/
stabilization. The
musculature
can
be
longus contributes to supination, whereas the extensor digitorum longus contributes to pronation. The tibialis anterior supinates the subtalar
and midtarsal joints. The intrinsic muscles of the foot include the flexor digitorum brevis, adductor and abductor hallucis, lumbricals, and dorsal and
divided into extrinsic and intrinsic muscles, the former having their origin in the lower leg and the lat-
plantar interossei muscles. The function of these
ter in the ankle/foot complex itself. The extrinsic muscles located in the posterior compartment of
muscles is to stabilize the toes and support the arches of the foot (see Mai) «5
the lower leg include the triceps surae, consisting
The plantar fascia is an important connective
of the gastrocnemius and the soleus muscles, the
tissue structure that acts like a windlass mechanism
tibialis posterior, the flexor digitorum longus, and
for the ankle/foot complex. It supports the longi-
flexor hallucis
of
tudinal arch, contributes to stability of the toes,
muscles results in a
and plays an important role in weight bearing. The
longus
muscles.'4
the posterior compartment
i]
Contraction
Flexor digitorum brevis tandons (cut) }| Adductor hallucis Lumbricales
-— Metatarsals
——__]
Jah4—
Flexor hallucis longus tendon (cut)
tL Flexor digitorum longus tendons Flexor hallucis brevis
| Forefoot Flexor hallucis longus tendon
— Phalanges
Abductor hallucis Abductor digiti minimi Plantar aponeurosis
(cut) FIGURE9-1 The foot is divided into a hindfoot, a midfoot, and a forefoot. The transverse tarsal (Chopart) joint separates the hingfoot from the midfoot and the tarsometatarsal (Lisfranc) joint separates the midfoot from the forefoot
Quadratus plantae
Flexor digitorum bravis
FIGURES-3
The intrinsic foot muscles
Flexor digitorum
brevis tendon (cut)
312° CHAPTERS Foot Ee
oe fascia consists of longitudinally arranged _ dense fibrous connective tissue, with type | collager fibers that resist tensile forces. The plantar ‘fascia originates from the plantar aspect of the calcaneus (the calcaneal tuberosity) and inserts distally to the plantar fibrous sheaths of the toes and
References 313 of plantar fasciitis, including the use of joint and soft-tissue manipulation to normalize mobility of
the ankle/foot joints and calf musculature.®
As a result of the weight-bearing function of _ the ankle/foot complex, the joints in this region
are prone to the development
of osteoarthritic
_ the sesamoid bones of the first toe. The plantar
changes. The first metatarsophalangeal joint is
fascia is prone to inflammatory and degenerative
often affected by osteoarthritis or gout. The joint
changes, which can affect the function of the joints
has a capsular pattern of greater limitation in extension than flexion, whereas the tarsometatarsal joint has a capsular pattern with greater
__ of the ankle/foot complex and the function of the longitudinal arch2* Decreased range of motion (ROM) of the ankle/foot complex has been found to be a risk factor for plantar fasciitis. A recent _ clinical practice guideline found strong evidence
for the use of manual therapy in the treatment
limitation in flexion than extension.?”-” Manual
therapy techniques can be effective in restoring joint mobility, thereby improving pain and function in patients with osteoarthritis of the foot.?
Key Terms Capsular pattern interphalangeal joints: More
The patient is a 23-year-old female who presents with left foot pain. The patient was playing volleyball 2weeks: ago, landed ona player's foot, and felt a pop in her left foot. Since then she has had lateral foot _ pain. Medical history is unremarkable. She states that her left foot feels painful when she put weight on ‘the lateral side and it feels like she has a pebble in her shoe. She has been unable to run or play volleyball and had to discontinue her step aerobic class. X-rays were negative. Physical therapy assessment findings include:
Gait analysis identified decreased left midfoot mobility during stand phase and decreased toe-off. Active and passive range of motion assessment demonstrates limited mobility of midfoot pronation and supination with pain at end range. Cuboid mobility assessment demonstrates limited plantar glide. Localized swelling is present at the lateral midfoot.
Questions: _1. 2. 3. 4.
What How How What
midfoot movement occurs during heelstrike, midstance, and toe-off during gait? do you determine if the joint inflammation is acute, subacute, or chronic? would that information direct your joint manipulation intervention? type of cuboid manipulation is indicated as intervention according to the evidence?
The following evidence is applicable to the treatment of the case patient: Durall" performed a literature review on the examination and treatment of cuboid syndrome. Dutall stated that unless contraindicated, manipulation of the cuboid should be considered as an initial treatment. Matthews and Claus’? described a case study where the patient had an active cuboid bone pathology demonstrated by nuclear imaging. The patient had rapid and lasting symptom resolution with joint manipulation of the cuboid. Their hypothesis was that joint mobilization acted to reverse
neurological sensitization. Jennings and Davies” used a cuboid whip manipulation on 7 patients who presented with foot pain and limited cuboid mobility. All 7 patients returned to sports activities with no recurrence of pain for the remainder of the season (average follow-up 5.7 months). Patla et al.'* used a cuboid thrust manipulation as treatment in a patient who was thought to have posterior tibialis tendinopathy and reported that the patient was pain free after one high-velocity
low-amplitude (HVLA) manipulation of the cuboid.
position
eueNapphalnee
(MTP) joint: 10 to 20 degrees of extension.
Capsular pattern midtarsal joint: Plantar flexion, supination, and adduction more than dorsiflexion.
Loose-packed position midtarsal joint: Neutral position between extremes of ROM.
Closed-packed position interphalangeal joints: Full extension.
Metatarsophalangeal (MTP) joint classification: Condyloid synovial joints with 2 degrees
Closed-packed
position
of freedom: flexion extension and abduction/
eae
(MTP) joint: Full extension.
Closed-packed
position
midtarsal
joint:
Full
supination.
adduction. The joint surfaces of the MTP joints consist of the convex metatarsal heads and the concave bases of the phalanxes. Tarsometatarsal
Closed-packed position tarsometatarsal joints: Full supination.
_ CASE STUDY
Loose-packed
restriction in flexion than extension.
(Lisfranc)
joint classification:
Planar synovial joints, allowing for gliding motions, Transverse tarsal (midtarsal,
sion; the convex proximal joint surface is larger than the distal concave surface.
of the midfoot together can be considered as a
position interphalangeal
joints:
Slight flexion.
consists
of
the
joint
classification:
Loose-packed
Joint
or Chopart)
Interphalangeal (IP) joints: Synovial hinge joint with 1 degree of freedom in flexion/exten-
calca-
neocuboid and talonavicular joints. The joints functional ball and socket joint, with movement occurring in response to movements of the subtalar joint.
References 1.
Levangie PK, Norkin CC. Joint Structure and Function: A Comprehensive Analysis. 5th ed. Philadelphia, PA: F. A. Davis Co; 2011.
. Sizer P, Phelps V, James R, Matthijs O. Diagnosis and management of the painful ankle/foot part 1: Clinical anatomy and 2003 ;3(3):238-262.
pathomechanics.
Pain
Practice.
of Soft Tissue Lesions. (Vol 1, 7th ed.). London, England: Balliére Tindall; 1978.
. Cyriax JH, Cyriax P, Cyriax’s Illustrated Manual of Medicine.
England; Boston, MA:
Sizer PS,
Phelps
V, Dedrick G, James
2nd
ed.,
Pbk.
ed.
Butterworth-Heineman;
Oxford, 1996.
R, Matthijs 0.
Tutorial diagnosis and management of the painful ankle/foot. part 2: examination, interpretation, and
Management. Pain Practice. 2003;3(4):343-374.
. Snedeker JG, Wirth SH, Espinosa N. Biomechanics of the normal and arthritic ankle joint. Foot Ankle Clin.
2012;17(4):517-528.
. Magee DJ. Orthopedic Physical Assessment, 6th ed. St. Louis, MO: Saunders Elsevier; 2014. . Moore KL, Agur AMR, Dalley AF. Clinically Oriented Anatomy. 7th ed, Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2013. . Nordin M, Frankel VH. Basic Biomechanics of the Musculoskeletal System. 4th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012. . Martin R. Heel pain: plantar fasciitis: Revision 2014. J Orthop Sports Phys Ther. 2014;44(11):A1-A33. . Cyriax JH. Textbook of Orthopaedic Medicine: Diagnosis
Orthopaedic
.
:
. Durall CJ. Examination and treatment of cuboid syn-
drome: a literature review. Sports Health. 2011;3(6): 514-519. . Matthews
ML, Claus AP. Two
examples of “cuboid
syndrome” with active bone pathology: why did manual therapy help? Manual Ther. 2014;19(5):494-498. . Jennings J, Davies GJ. Treatment of cuboid syndrome secondary to lateral ankle sprains: a case series. J Orthop Sports Phys Ther. 2005;35(7):409-415, . Patla C, Lwin J, Smith L, Chaconas E. Cuboid manipulation and exercise in the management of posterior tibialis tendinopathy: a case report. Int J Sports Phys Ther. 2015;10(3):363-370.
CHAPTER 9 foot
Manual Therapy Techniques forthefoot
Manual Therapy Techniques for the Foot Midfoot Supination Manual Therapy Techniques Forefoot General Manual Therapy Techniques
|
Midfoot Pronation Manual Therapy Techniques * Joint manipulation, non-thrust
* Counterstrain technique
= Joint manipulation, thrust * Muscle energy technique * Mobilization with movement
Myofascial manipulation * Soft tissue manipulation Self-mobilization
isonet Joint: Foot
‘
% |
_ Midfoot Pronation Motion Limitation
Patient Position: Supine with the knee bent and foot on a bolster (foam block) 5 Therapist Position: Standing at the side of the table
Midfoot Pronation 9A
Type of Manipulation: Joint manipulation, thrust 6 Restricted Motion: Limited Midfoot Pronation
9D Forefoot Dorsiflexion Manual Therapy Techniques 9E Forefoot Plantarflexion Manual Therapy Techniques
9A Midfoot Pronation Manual Therapy Techniques 9B 9C
Joint; Foot Midfoot Pronation Motion Limitation
315
a
Type of Manipulation: Joint manipulation, nonthrust Restricted Motion: Limited Midfoot Pronation Patient Position: Supine with the knee bent and foot flat on the table Therapist Position: Standing at the side of the table
J. The knee is placed into 70 to. 90 degrees of flexion. 2, The therapist places one hand along the dorsum of the foot with the opposite hand under the foot blocking the proximal bone (talus, calcaneous). The therapist can use the palm of the hand or the hypothenar eminence on the dorsal surface of the foot over the dysfunctional bone and can put a plantar force to the tissue barrier. 3, At the tissue barrier, the therapist creates a HVLA thrust. The force is
Zt ze
through the palm of the hand on the dorsum of the foot, while the opposite hand blocks the proximal bone from undemeath. —
FIGURE ana
4. The bone will mave in a plantar direction. setae
eee Oe
Es
EE
Seer
Notes: A foam block can also be used forar
Joint: Foot Midfoot Pronation Motion Limitation
1. The knee is placed into 70 to 90 degrees of flexion.
eke
ees
a
Type of Manipulation; Muscle energy technique Restricted Motion: Limited Midfoot Pronation Patient Position: Supine with the knee straight and the ankle plantarflexed
2. The therapist places one hand along the dorsum of the foot with the opposite hand under the foot blocking the proximal bone (talus). The therapist can use the palm of the hand or the hypothenar erninence on the dorsal surface of the foot over the dysfunctional bone and can
Therapist Position: Standing on the same side of the patient’s lower
leg to be treated
. The knee is placed straight and the footin 10 to 30 degrees of
put a plantar force to the tissue barrier. . At the tissue barrier, the therapist creates plantar glide mation performed with progressive oscillation. The force is through the palm of the hand on the dorsum, while the opposite hand blocks the
nm
(es
ag
on ierela su ie i ue at
proximal bone (talus, calcaneous) from underneath. ae
4. The joint glide force is directed in a plantarly direction.
plantarflexion. The therapist places the hands along the dorsum surface of the foot with the thumb over the dysfunctional joint (navicular/cuneiforms) with the thumb along the ray to be mobilized. The fingers are wrapped around to the plantar surface of the foot. The therapist distracts the midfoot to the tissue barrier. The therapist
places a plantar force with the tip of the thumb while dorsiflexing the distal portion of the ray to engage the restrictive barrier. a
FIGURE 9-6
. The patient isometrically contracts the foot into plantarflexion (away
from the restrictive barrier) for 3 to 5 seconds, meeting the therapist's force with approximately 5 lbs of pressure, and then the patient in
completely relayes.
. Upon relaxation, the therapist plantarly glides the joint and takes up the additional tissue slack into midfoot pronation to the new restrictive barrier, This is repeated until no further relaxation or improvement into dorsiflexion occurs.
FIGURE ¢a 4
Notes: A foam block can also be used for support on the “iat needed for force attenuation during stance phase.
Notes: Technique can be useful when muscle guarding or hypertonicity is present.
surface of the foot as seen in Figure B. Proper pronation of the ankle/foot complex is
LIMITED MIDFOOT PRONATION
314
316
CHAPTER 9 foot
Manual Therapy Techniques forthe Foot + 317
Joint: Foot
Type ofManipulation: Mobilization with .
it
a)
idfootaa Pronation Motion
Erie
Limitation
~. movement
:
Midfoot Pronation Motion Limitation
_ Restricted Motion: Limited Midfoot Pronation _
qd: Type of Manipulation: Counterstrain technique
_ Restricted Motion: Limited Midfoot Pronation ~ Patient Position: Prone with the knee flexed and ankle plantarflexed
Patient Position: Supine with the ankle in neutral
Therapist Position: Standing on the side of the patient
Therapist Position: Seated at the foot of the table
1, The patient lies prone with the knee flexed and the ankle plantarflexed. The therapist palpates the intrinsic foot flexor muscles. The therapist presses into the muscle of discomfort and finds the most hypertonic uncomfortable point. The therapist asks the patient to rate
1. The therapist places one hand along the dorsum of the foot with the opposite hand under or behind the foot blocking the proximal bone (talus). The therapist can use the fingers along the dorsum of the foot over the dysfunctional bone,
the discomfortat a 10/10.
force is through the fingers of the hand on the dorsum, while the opposite hand blocks the proximal bone from underneath. 4, This is repeated until the bone will move in a plantar direction more
—_—
3, At the active tissue barrier of pronation, the therapist performs an accessory glide to take up all of the tissue tension and creates plantar glide motion. This can be performed with progressive oscillation. The
Ny \
2. The patient is asked to roll their foot into pronation.
freely.
FIGURE 9-8
2. The therapist then passively flexes the forefoot and compresses the calcaneus toward the midfoot while creating supination. 3. The therapist then palpates the intrinsic muscle and continues to move the metatarsals and calcaneus until the palpable pointis down toa 2/10 discomfort level. 4. The therapist holds the position for 90 seconds. The therapist does Not need to place pressure on the point for the 90 seconds. Once the 90 seconds are up, the therapist passively straightens out the leg and rechecks the point. If the point produces more than 2/10 discomfort the treatment is repeated.
Notes: This may decrease the hypertonicity of the foot intrinsics allowing the foot to pronate a greater distance. This is an indirect technique beneficial for d rearfoot equinus deformity.
Type of Manipulation: Myofascial manipulation
Restricted Motion: Limited Midfoot Pronation Patient Position: Supine on the table Therapist Position: Seated on the involved side of the patient 1. The patient lies supine with the ankle in dorsiflexion. 2, The therapist places a thumb on the plantar fascia attachment of the calcaneus. The therapist's other thumb stabilizes over the midfoot. 3. At the tissue barrier of the calcaneus, the therapist uses a tissue tension technique to mobilize the fascia into dorsiflexion. The therapist moves from the calcaneus toward the distal metatarsals, 4. The therapist palpates into the soft tissue and engages the restrictive barrier with a light force in the direction of tension, sometimes up to 3 to 5 minutes. 5. A light pressure on the barrier is held until the tissue barrier softens and relaxes and the myofascial unit elongates.
ALOROAD
FIGURE 9-7
en
iF Fi
1
ay
Notes: The therapist can tape the rear foot so the calcaneus and talus are stabilized.
a i
FIGURE 9-9
a
i;
an) 4 TUG
Neh
Notes: Sustained pressure over time is useful. Technique can be used in the presence of restrictions of the plantar fascia and intrinsic foot muscles,
LIMITED MIDFOOT PRONATION
Joint: Foot Midfoot Pronation Motion Limitation
318 CHAPTERS Foot
Manual Therapy Techniques for the Foot ©3190
Manual soft tissue manipulation
ve
Patient Position: Prone with the knee bentat 90 degrees
1. The patient stands with the leg straight and foot flat on the side to be
Therapist Position: Stand ing on the involved side of the patient
mobilized.
2. The patient uses the opposite foot and applies weight through the
1. The patient lies prone with the knee bent to 90 degrees.
heel aver the midfoot.
e
3, The patient gently mobilizes the arch in an inferior direction toward
2. The therapist palpates the intrinsic muscles of the foot and holds deep
“pressure with the knee bent. 3. The therapist can perform soft tissue manipulation by gentle
the floor.
,
4. The patient applies weight on the jointto be mobilized until tissue barrier is met. The patient can hold tension statically or spring on the
strumming and lateral mobilization of the muscles and tendons, and
joint.
with circular strokes to increase circulation.
Tar
sa
4, Thisis repeated until the soft tissue relaxes. FIGURE 9-11
Self soft tissue manipulation Patient Position; Seated with bodyweighton a foam roller or massage ball 1, The patient places bodyweight with a foot on the ball.
2. The patient can hold statically or roll back and forth to relax the soft tissues, 3. This is repeated until the soft tissue relaxes,
FIGURE 9-10 Notes: A towel can be placed over the ball to soften the technique (Figure B). The self soft tissue technique can also be performed standing (see Figure B).
Notes: A towel can be placed on top of the foot for comfort. This technique can focus on the navicular or cunelforms. This can also be combined with hold-relax technique to facilitate movement.
320. CHAPTER 9 Foot
‘Manual Therapy Techniques for the Foot
©=321
98 Midfoot Supination Manual Therapy Techniques + Joint manipulation, non-thrust+ Joint manipulation, thrust cle energy technique -« Mobilization with movement
« Counterstrain technique
Patient Position: Supine with the kneepertare the foot resting on :
* Myofascial manipulation
the lateral border
* Soft tissue manipulation * Self-mobilization
Therapist Position: Standing on the oppose side: ofthe as
lower leg to be treated 1, The patient’s knee is placed into 70 to 00 degrees of flexion. 2. The therapist places hands on the calcaneus and the navicular bone. The arms are crossed and the fingers pointing in opposite directions. 3. At the tissue barrier, the therapist creates a HVLA thrust by stabilizing
the calcaneus and talus while thrusting the navicular in a distal and dorsal direction,
Patient Position: Prone
Therapist Position: Standing on the same side of the patient's lower
4. The bone will move dorsally.
‘leg to be treated 1. The therapist places one hand on each side of the foot.
FIGURE + 14:
2, The therapist places thumbs over the plantar surface of the foot on either side of the joint to be mobilized. The therapist mobilizes with the thumb in @ dorsal direction while the fingers of the opposite hand
block the motion of the distal bone, 3, Atthe tissue barrier, the therapist performs oscillations in a dorsal direction. FIGURE 9-12
4. The bone will move dorsally.
Notes: HVLA iste ues can be useful when patient does nat respond ta joint glide techniques. This technique can also be utilized to focus on the firstBy
_ Joint: Foot
Midfoot Supination Motion Limitation
Notes: Limited supination can contribute to excessive pronation of the foot. Full supination mobility is needed to provide a rigid lever at the end of the
Patient Position: Prone with the knee bent
pushoff phase of gait.
Therapist Position: Standing at the foot of the table 1, The patient's knee is placed into 90 degrees of flexion. 2. The therapist places hands along the lateral surfaces of the foot with the thumbs crossed on the plantar surface of the foot over the dysfunctional joint and puts a dorsal force to the restrictive barrier. 3. The patient isometrically contracts the foot into pronation (away from
_ Type of Manipulation: Joint manipulation, thrust Restricted Motion: Limited Midfoot supination ul (Cuneiform S Cuboid) Patient Position: Prone at the side of the table
the restrictive barrier) for3 to 5 seconds, meeting the therapist's force
Therapist Position: Standing on the same side of the patient's lower leq to be treated |. The patient’s knee is placed into 70 to 90 degrees of flexion off the side of the table.
2. The therapist places the hands along the lateral surfaces of the foot with thumbs crossed over on the plantar surface of the foot over the
dysfunctional bone and puts a dorsal force to the tissue barrier, 3, At the tissue barrier, the therapist creates a HVLA thrust by extending the knee and plantarflexing the ankle. With a J-stroke motion, the
FIGURE 9-13 Notes: Also referred to as a Hiss whip hes Thisiti
Type of f Manipulation: Muscle chewy i eh je Restricted Motion: Limited Midfoot Sup nation
foot is flexed and the ankle is plantarflexed; the force is through the thumbs while there is ulnar deviation at the wrists. When the wrist ulnarly deviates, it creates traction on the midfoot and forefoot. 4. The bone will move BE Nes), can also tepermedo be on iestarsomJe
yes
with approximately 5 Ibs of pressure, and then completely relaxes. 4, Upon relaxation, the therapist dorsally glides the joint and takes up the additional tissue slack into the new restrictive barrier of midfoot supination. This is repeated until no further relaxation or improvement Solas ern Pana
FIGURE 9-15
of range of motion into supination occurs.
LIMITED MIDFOOTSUPINATION
y Meee


![Manual Mobilization of the Joints, Vol 3: Traction-Manipulation of the Spine and Extremities [3]](https://ebin.pub/img/200x200/manual-mobilization-of-the-joints-vol-3-traction-manipulation-of-the-spine-and-extremities-3.jpg)
![The Mulligan concept of manual therapy [2 ed.]](https://ebin.pub/img/200x200/the-mulligan-concept-of-manual-therapy-2nbsped.jpg)
![Clinical Kinesiology - Lower extremities [V]](https://ebin.pub/img/200x200/clinical-kinesiology-lower-extremities-v.jpg)
![Clinical Kinesiology - Upper extremities [IV]](https://ebin.pub/img/200x200/clinical-kinesiology-upper-extremities-iv.jpg)



![Uncommon Ulcers of the Extremities [1st ed. 2023]
9819917816, 9789819917815](https://ebin.pub/img/200x200/uncommon-ulcers-of-the-extremities-1st-ed-2023-9819917816-9789819917815.jpg)